Abstract
Background
Academic emergency medicine is a constant balance between efficiency and education. We developed a new model called swarming, where the bedside nurse, resident, and attending/fellow simultaneously evaluate the patient, including initial vital signs, bedside triage, focused history and physical examination, and discussion of the treatment plan, thus creating a shared mental model.
Objectives
To combine perceptions from trainee physicians, supervising physicians, nurses, and families with in vivo measurements of emergency department swarms to better conceptualize the swarming model.
Methods
This mixed methods study was conducted using a convergent design. Qualitative data from focus groups with nurses, residents, and attendings/fellows were analyzed using directed content analysis. Swarming encounters were observed in real time; durations of key aspects and family satisfaction scores were analyzed using descriptive statistics. The qualitative and quantitative findings were integrated a posteriori.
Results
From the focus group data, 54 unique codes were identified, which were grouped together into five larger themes. From 39 swarms, mean (±SD) time (minutes) spent in patient rooms: nurses = 6.8 (±3.0), residents = 10.4 (±4.1), and attendings/fellows = 9.4 (±4.3). Electronic documentation was included in 67% of swarms, and 39% included orders initiated at the bedside. Mean (±SD) family satisfaction was 4.8 (±0.7; Likert scale 1–5).
Conclusions
Swarming is currently implemented with significant variability but results in high provider and family satisfaction. There is also consensus among physicians that swarming improves trainee education in the emergency setting. The benefits and barriers to swarming are underscored by the unpredictable nature of the ED and the observed variability in implementation. Our findings provide a critical foundation for our efforts to refine, standardize, and appraise our swarming model.
Background
Emergency medicine in the academic setting involves a constant balance between efficiency and education. In the age of ever‐increasing volumes and emergency department (ED) overcrowding, the tension between these two priorities becomes particularly palpable.1 The serial model of patient evaluation, in which the trainee physician evaluates patients first before presenting to a supervising physician, further compounds this issue.2 While this traditional model of patient care has been held as a criterion standard for trainee education and autonomy, it is inherently inefficient and does not allow for active bedside learning3 and conscious role modeling,4, 5 concepts that have emerged as important for medical education in the emergency setting. Existing emergency medicine literature describes a number of methods to improve front‐end operations in the ED, including immediate bedding of patients and placing physicians in triage.6 Although there is evidence to suggest that these processes improve efficiency,7, 8 the issue of resident education in the emergency setting is seldom addressed within these interventions. One example of simultaneously integrating education and efficiency can be found in the family‐centered rounds literature, which has demonstrated improved staff understanding of the medical plan9 without significantly increasing rounding time.10 This model allows for team reflexivity, which entails group reflection and adaptation before, during, and after a patient encounter.11 Compared to the inpatient setting, however, the ED treats the undifferentiated patient with whom there is no prior relationship or existing plan, which limits the comparisons that can be made to this well‐established model of care.
With the competing goals of efficiency and education in mind, our pediatric academic ED underwent a sweeping process redesign in November 2016. During this intensive 5‐day period, we created a new model which included quick sorting of patients into tracks, rapid bedding without traditional triage, zoning of physicians, and increasing bed turnovers by moving patients into treatment‐in‐progress and discharge areas. A key component of the redesign that addressed both front‐end efficiency and trainee education was the concept of “swarming.”12
Importance
Swarming is a novel model that facilitates the immediate evaluation of a patient simultaneously by the bedside nurse, resident, and senior ED physician (attending or fellow).12 The bedside nurse performs an intake assessment including initial vital signs, while the physicians begin a focused history and physical. At the end of this encounter a plan is discussed with both family and nursing, and electronic documentation and orders are initiated. This approach, which embraces team reflexivity13 and mirrors the one often used in the management of critically ill and trauma patients, helps to develop a shared mental model14 for optimizing communication, care, and learning.
Following the process redesign which included the implementation of swarming, we saw significant decreases in length of stay (LOS), door‐to‐provider times, and left‐without‐being‐seen rates.12 However, due to the novelty of this approach and the lack of well‐defined best practices, significant variability in receptivity among staff and implementation continued to occur. To eventually develop best practices and evaluate the effects of swarming, the first step was to characterize the variation that currently exists and understand any potential barriers to consistent implementation.
Goals of This Investigation
The objective of this study was to combine perceptions from physicians, nurses, and families with in vivo measurements of ED swarms to better conceptualize the swarming model. In doing so, we sought to answer the following questions: What factors do physicians and nurses perceive as barriers to swarming implementation? What is the degree of family satisfaction with swarming encounters? What are the interactions that occur during swarming and what are their durations? Given the novelty of this approach, having the ability to triangulate the quantitative characteristics of the swarm with the perceptions of clinicians and families was essential for a comprehensive understanding of the model.
Methods
Study Design and Setting
We conducted a mixed methods study using the convergent design.15, 16 This approach involves separate qualitative and quantitative data collection, wherein the two data sets are collected around the same time and one does not influence the other; the data sets are then independently analyzed and results are coalesced to attain a convergent interpretation of the phenomenon of interest. All aspects of the study were carried out at the Children's Hospital Los Angeles ED, a tertiary care academic pediatric ED with over 95,000 visits per year.
Selection of Participants
Focus groups were conducted to collect qualitative data; this method was chosen with the expectation that interaction among the members of each group would enrich the information collected. For the focus group portion of the study, a purposive sampling17 strategy was used; individuals with experience relevant to the swarming context were approached for participation to generate a content‐rich sample. This included resident physicians, attending physicians, fellows, and nurses. Resident physicians were contacted by e‐mail and asked to volunteer for focus group participation. Residents who were working in the ED at the time of the focus groups were also invited to attend. For the attending and fellow physicians as well as the nurses, focus groups were conducted during regular staff meeting times. All participants were consented prior to the start of each session and participation was completely voluntary.
There is currently no consensus on sample size conventions for mixed methods studies;15 it has been suggested, therefore, that the sampling strategy and size estimates should be based on the specific research question and should support feasibility. As a result, a minimum number of 30 swarms were deemed as a feasible convenience sample size for direct observation. Patients were enrolled during times when research staff were available, from mornings to early evenings. Patients that were excluded from this phase of the study included critical (Emergency Severity Index [ESI] level 1) patients, where it was not feasible to consent families prior to initiating evaluation and treatment. Non–English‐speaking patients and families were also excluded, as the presence or use of an interpreter could change the durations of various aspects of the swarm.
Measurements
Separate focus groups (nurses, resident physicians, and attending/fellow physicians) were conducted to facilitate open and unhindered conversation about swarming. Focus groups were conducted in a semistructured format, with a research staff moderator there to guide discussion as needed. Because the principal investigator (JLP) is a physician, the decision was made to have non‐clinical research staff serve as moderators to encourage neutrality and open discussion, therefore increasing the trustworthiness of the collected data. Each participant was given a handout with several prompts, including asking about general perceptions of swarming as well as benefits of and barriers to the swarming model (see Data Supplement S1, Appendix S1, available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1002/aet2.10388/full). Moderators probed participants as necessary to optimize discussion time. All focus groups were audio recorded and then transcribed, removing identifying information during the transcription process.
During the observational portion of the study, a research team member recorded the duration of key aspects of the swarming encounter using a multitimer digital stopwatch (see Table 1 for a list of these timed variables and associated definitions). In addition, it was noted whether electronic documentation was started and whether orders were placed at the bedside during the swarming encounter. Thereafter, research staff administered a brief questionnaire with the family, where they explained the new swarming model and then asked a few questions regarding perceptions of the encounter, including a 5‐point Likert scale to measure overall satisfaction (see Data Supplement S1, Appendix S2). Research staff also collected general information about the visit from the patient's electronic medical record, including ESI acuity level, LOS at which swarming was initiated, chief complaint, and final diagnosis. Our mixed methods study was approved by the Institutional Review Board at our hospital.
Table 1.
Names and Definitions of Variables That Were Timed During Direct Observation of Swarming Encounter
| RN in room | Total time that bedside nurse was present in the room |
| Resident MD in room | Total time that the resident physician was present in the room |
| Attending MD in room | Total time that the supervising (attending or fellow) physician was present in the room |
| Resident MD history | Amount of time resident spent asking questions directly to the patient/family |
| Attending MD history | Amount of time attending or fellow spent asking questions directly to the patient/family |
| RN vitals and assessment | Total time for the nurse to do initial vital signs and physical assessment of patient for nursing intake |
| Resident MD physical exam | Amount of time resident physician is examining patient |
| Attending MD physical exam | Amount of time attending or fellow is examining patient |
| Resident MD discusses plan | Total duration of time where resident is explaining assessment and/or plan to the patient and family |
| Attending MD discusses plan | Total duration of time where attending or fellow is explaining assessment and/or plan to the patient and family |
Data Analysis
To establish trustworthiness of qualitative findings,18 the decision was made to have two coders: one clinician (JLP) with relevant clinical swarming experience, and one non‐clinical research staff member (ARS) with qualitative coding expertise. Directed content analysis was used to analyze focus group data.19 This strategy begins with deductive coding, which integrates codes from relevant literature, followed by inductive coding, which involves the creation of de novo codes as the coder goes through the transcript line by line. For our purposes, an initial code list was derived from literature pertinent to swarming, including ED front‐end operations, ED process improvement, and FCR.2, 6, 7, 8, 9, 10, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30
Deductive coding was conducted initially: short portions of the same focus group transcripts were independently coded using the literature‐based code list, after which the coders met and built consensus. This process was continued in an iterative fashion until all transcripts were coded using the literature‐based codes. Throughout the process the code list was edited to include definitions, and unused codes were ultimately deleted. Inductive coding was subsequently performed: all transcripts were again independently reviewed line by line and new codes were created when appropriate. The process of building consensus was repeated, with frequent meetings between the coders to review and reconcile all new codes. Any coding discrepancies were resolved through discussion with a third member of the study group, the senior author on this study (DRL). Once the code list was finalized, codes were grouped into themes and subthemes, and the frequency of each code within each transcript was recorded. The complete coding structure is available in Figure 1.
Figure 1.
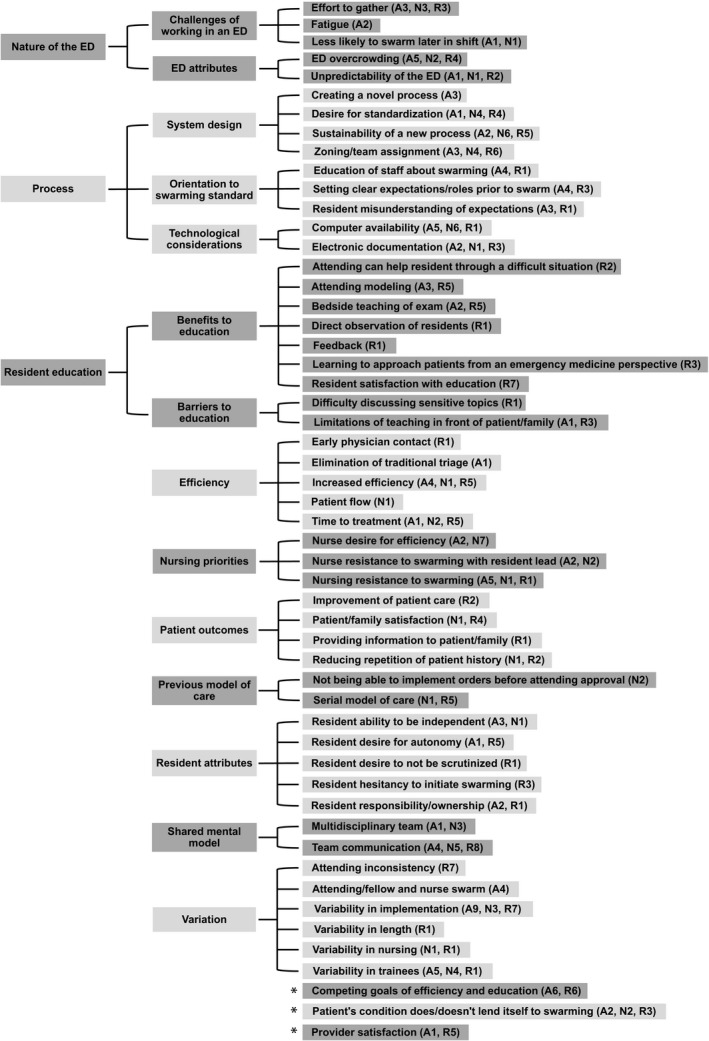
Themes, subthemes, and codes as derived from qualitative directed content analysis. The frequency of each code is listed after code title, divided into attending/fellow (A), nursing (N), and resident (R) focus groups. Total number of participants of each type: 14 attending/fellow physicians, seven nurses, and 11 resident physicians.
Descriptive statistics were used for all time duration data collected from direct observation of swarming encounters. Mean family satisfaction scores were computed.
Results
Characteristics of Study Subjects
There was one attending and fellow focus group with 14 participants, which included nine attending physicians and five fellow physicians. There was one nurse focus group with seven nurses, including both long‐term and traveling nurses. Two focus groups took place with resident physicians, with seven and four participants, respectively. All resident physicians were pediatric residents based at our home institution (external rotating residents were not able to be included due to scheduling). In all groups, there was a mix of staff that had experienced our previous serial model of care prior to the redesign and those who had not. The length of the focus groups varied from approximately 13 to 21 minutes.
For the direct observations, 39 swarming encounters were ultimately included in the analysis. The mean (±SD) age of patients in this group was 6.23 (±5.24) years (median = 5.02 years, range = 2 months to 17 years). Of all encounters, 21% were categorized as ESI level 2, 64% were ESI level 3, and 15% were ESI level 4.
Qualitative Results
The coding process yielded 54 unique codes, and the total coding structure (Figure 1) is summarized in the following five sections, with representative quotes from the focus groups included in Table 2.
Table 2.
Representative Quotations From Focus Groups
| Inherent qualities of the ED |
“The busier the ED the less swarming, so early shifts or later in your overnight shift I find myself swarming but if it's mid shift and it's crazy, you can't find everybody to swarm at the same time.” (attending/fellow) “The swarming is great, and I believe it should continue, but I just don't know if it's possible to swarm on every patient, because it's just not practical. It gets busy, and there's more than one of us usually at a station … The attending can't be in both places at the same time.” (resident) |
| System implementation |
“There are a lot of residents, it's hard for us to continue to orient people to the swarm, it's also something that's changing, and so there are a lot of residents who don't understand that the beginning and point of the swarm is to get the initial, I call it the primary survey of the visit. It's not to do everything.” (attending/fellow) “And when we first started this process as well, everyone was very diligent … I think it's just we've gotten, in the year, we've gotten away from both the logistics of it and then also the way in which we're approaching the assessment.” (nurse) |
| Variability |
“It depends on the time of day, depends on the physician, the nurse, depends on the patient.” (nurse) “I also haven't seen it consistently done. It depends on how busy it is, it also depends on the attending you work with. I think some do it more than others.” (resident) “I like that variability. And I don't know if it's necessarily the intent, but the practicality makes it so, and I think it kind of addresses your autonomy vs. learning from mentorship and watching your attending.” (resident) |
| Efficiency vs. education |
“I've been told that [residents] like how we talk to families, like even in a difficult patient setting or family interaction, even just what they need to do to follow up or reasons to come back. So, they have said they like that component of the swarm, seeing how we manage the patient differently than they would.” (attending/fellow) “From a resident education perspective, we are being taught to actually think like emergency medicine physicians.” (resident) “The focus of my education is still more on the recognition and … less so the efficiency and the throughput part of it, so maybe sometimes that's the down side I see at my point of training, like having that opportunity to see the patient by myself and kind of think through it, rather than how fast we can get through it.” (resident) |
| Outcomes |
“And we can get things started, we don't have to now wait for orders, things are much more timely.” (nurse) “Patients seem happier because they're being seen faster, and they don't have to repeat their story over and over again to multiple people.” (resident) “I really appreciate the communication we have with the nursing staff in this model.” (resident) |
Inherent Qualities of the ED
Participants in all focus groups discussed how attributes that are perceived as unique to the ED often influence their ability to swarm. Overcrowding and unpredictability, which are inherent to the ED, as well as the effort required to gather swarming participants, were noted as challenges. Furthermore, fatigue was stated as being a barrier to swarming, and both attending physicians and nurses mentioned that they are less likely to swarm at the end of their shifts. Additionally, all staff recognized technological considerations, such as the availability of computers for electronic documentation, and physician zoning, as they relate to the swarming process.
System Implementation
Given the ED context, participants noted the difficulty involved in creating and sustaining a new model like swarming. In light of the frequent rotation of new residents in the ED, all physicians recognized the need for setting clear expectations about individual roles prior to swarming. Staff unanimously expressed a desire for greater standardization, mentioning the need for further clarification on implementation. Participants from all groups mentioned that there are certain patient conditions and chief complaints that lend themselves best to the swarming model.
Variability
A common theme that emerged from all of the focus groups was the variability with which swarming is implemented. Participants noted variation in length of the swarming encounter, as well as variability in execution depending on the specific nurses or physicians who are involved. Specifically, resident physicians noted inconsistency in how each attending physician carries out the swarming model, with discussion of how this impacts their understanding of a swarming standard.
Efficiency Versus Education
Perspectives on the optimal balance of efficiency and education in ED swarms varied significantly from group to group. Although there was consensus among all focus groups that swarming reduced time to treatment and increased overall ED efficiency, all groups noted that nurses were often resistant to the swarming process. Nurses expressed that their efficiency was their ultimate priority and as a result noted that staying in the patient room for the entire swarming encounter was often difficult for them. Both nurses and attending physicians specified that nurses are hesitant to participate in swarming when it is led by a resident physician; these two groups agreed, furthermore, that when a full team swarm is not feasible, their preferred alternative is a nurse‐fellow/attending swarm. For residents, on the other hand, the preferred alternative is a resident‐nurse swarm.
Residents discussed two barriers to education, namely the potential limitations of teaching directly in front of the patient/family and the difficulty of discussing sensitive topics. However, residents also recognized educational advantages to swarming, including attending role modeling, bedside teaching, directed feedback, and learning how to approach patients from an emergency medicine perspective. Residents spoke about the importance of functioning autonomously and taking ownership of patient care but expressed dissensus concerning the extent to which swarming helped or hindered those priorities. All physicians, including both supervising and trainee physicians, acknowledged that swarming has helped to develop a consistent shared mental model of patient care through improvement of multidisciplinary team engagement and team communication.
Outcomes
There were a number of comments made in all focus groups about positive outcomes related to swarming. Staff noted that, in addition to the overall improvement in patient care, patients and families were more satisfied with swarming in contrast to the serial model of care. They also mentioned that swarming facilitates the provision of timely and accurate information to the family and that families appreciate not having to repeat information multiple times. Notably, there was consensus among the physician focus groups about the high degree of overall provider satisfaction with swarming.
Quantitative Results
For those swarming encounters included in the direct observation portion of the study, the initial evaluation occurred at a mean (±SD) of 21.2 (±11.2) minutes after patient arrival (median = 18 minutes, range = 3‐54 minutes). During the swarming encounter, on average, the nurses spent a mean (±SD) 6.8 (±3.0) minutes in the patient room, the attending/fellow physicians spent a mean (±SD) of 9.4 (±4.3) minutes, and the resident physicians spent a mean (±SD) of 10.4 (±4.1) minutes (for all the time durations of the key aspects of the swarming encounter, see Table 3 for the means and SDs and Figure 2 for the medians and interquartile ranges).
Table 3.
Time Durations of Key Aspects of the Swarming Encounter (Minutes)
| Mean | SD | Minimum | Maximum | |
|---|---|---|---|---|
| RN in room | 6.8 | 3.0 | 2.0 | 13.7 |
| Resident MD in room | 10.4 | 4.1 | 2.9 | 18.9 |
| Attending MD in room | 9.4 | 4.3 | 2.9 | 19.2 |
| Resident MD history | 3.1 | 2.5 | 0.1 | 14.3 |
| Attending MD history | 1.7 | 1.7 | 0 | 9.5 |
| RN vitals and assessment | 3.1 | 1.8 | 0 | 9.1 |
| Resident MD physical examination | 2.1 | 1.6 | 0 | 6.3 |
| Attending MD physical examination | 1.2 | 0.9 | 0 | 3.8 |
| Resident MD discusses plan | 0.6 | 1.0 | 0 | 4.5 |
| Attending MD discusses plan | 1.3 | 1.5 | 0 | 7.7 |
Figure 2.
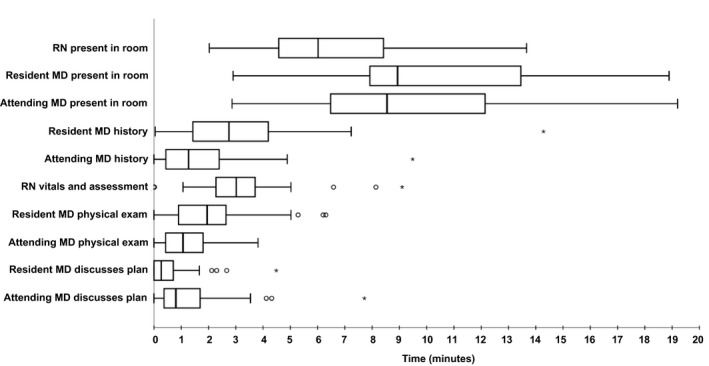
Median time duration for key aspects of the swarming encounter with interquartile range (IQR). Across the boxplots, circles are outliers (values greater than [IQR × 1.5] + 75th percentile, or less than [IQR × 1.5] − 25th percentile), and asterisks are extreme outliers (values greater than [IQR × 3] + 75th percentile). “Attending MD” in this setting refers to either the attending or fellow physician who was functioning in a supervisory role during the swarming encounter.
During the 39 observed swarming encounters, 67% included electronic documentation that was started by one of the physicians, 39% included orders that were placed at the bedside, 67% included direct communication from the resident to the attending/fellow, 67% included direct communication from the attending/fellow to the resident, 13% included direct communication from the resident to the nurse, and 31% included direct communication from the attending or fellow to the nurse. On the questionnaire completed with the family after the encounter, mean (±SD) overall satisfaction was 4.8 (±0.7) on a 5‐point Likert scale.
Synthesis of Results
The perspectives shared during the focus groups can be used to better understand and interpret the quantitative results and vice versa. A theme frequently mentioned in the focus groups was the variability with which swarming is implemented. This was supported by the quantitative data, particularly in the wide SDs of the time durations of key swarming aspects. Of note, in the qualitative data, the resident physicians specifically discussed how the attending or fellow physicians varied in their implementation of swarming. Such variations included whether the supervising physicians remained in the room throughout the complete evaluation, whether they started electronic documentation or orders, or whether the senior physician took the lead in determining or explaining the plan to the family or let the resident guide this final aspect of the swarm. In particular, these inconsistencies of the supervising physicians as perceived by the trainees may have important implications on the educational effects of swarming. Staff unanimously noted the need for greater standardization of the swarming model.
During the focus groups, it was noted that nurses sometimes hesitate to swarm and the nurses themselves expressed that their own efficiency is of primary concern. These results converge with the finding that nurses spent the least time on average in the patient rooms during swarming. Although all swarming team members started out in the room together, nurses were more likely to leave before the other clinicians.
The quantitative results showed inconsistent durations of time spent in discussion between members of the care team during swarms, which could be interpreted as markers of poor team communication. However, in the qualitative portion of the study, the idea emerged that swarming often results in improvements in team communication and the creation of a shared mental model of care. This may be explained by the simultaneous presence of all providers in the room who have increased knowledge of the assessment and care plan as a result of hearing each other speak directly with the family.
The availability of computers for electronic documentation was a factor discussed in the focus groups as being influential in the swarming model. This idea was reflected in the quantitative data, where the frequency of electronic orders placed at the bedside varied significantly from one swarm to the next.
Finally, the average level of family satisfaction with swarming encounters was notably high. This converged with the perspectives in the focus groups, where both nurses and physicians mentioned that families appreciate not having to repeat information multiple times and are generally satisfied with the swarming model.
Discussion
We embarked upon this investigation to describe and further conceptualize swarming, a new model to improve both efficiency and education in the academic emergency setting. The unique challenge of balancing these priorities in the ED has given rise to multiple innovative teaching strategies, which have been described in previous literature.31 Correspondingly, the results of our qualitative data reflect a general consensus that swarming improves education. Trainee physicians specifically noted the benefits of bedside teaching, attending role modeling, and feedback. While the literature supports the advantages of these educational tools, there are also caveats. Bedside teaching should be active,3 role modeling must be done in a conscious manner where the trainee analyzes the behaviors they witness,4 and feedback should be learner‐centered and ideally in real time.32 As a team‐based model where teacher and learner concurrently provide patient care, swarming is poised to embrace these best practices.
While there are multiple educational advantages of swarming, these may come at the cost of decreased resident autonomy, while acknowledging that supervising and trainee physicians may have different perceptions of the amount of autonomy provided in a clinical setting.33 Indeed, as reported in one family‐centered rounds (FCR) study, senior residents often perceive decreased autonomy,22 and specific strategies can be employed to promote the autonomy of the resident physician in this team model. Setting clear expectations and defining responsibilities prior to the patient encounter are strategies that emerged from our results and are consistent with published FCR findings.21
Our results also showed a consensus amongst team members that swarming increased efficiency compared to the traditional serial model of care. A number of studies show increased efficiency with changes in front‐end operations, mostly focusing on rapid triage and physician/provider in triage.6, 7, 8, 26, 28 At the same time, a systematic review showed no statistically significant decrease in LOS with team triage,30 and other studies show improvements only with certain patient acuity levels.29, 34 Although this study on swarming was not designed to quantify an improvement in efficiency metrics, our findings showed an average time commitment of approximately 10 minutes for the physicians, suggesting that a substantial amount can be accomplished in regard to patient care, communication, and education in a relatively short time frame.
Several differences exist between the swarming model and front‐end operational interventions. In many of the physician‐in‐triage or team triage models, the team that performs the initial assessment is typically not the definitive treatment team.8, 28, 29, 30, 34 When one provider sees a patient in triage, with a different provider for the remainder of the ED stay, this increases hand‐offs and may also increase the diagnostic studies ordered by the initial triage provider.29 In the swarming model, the team responsible for the initial assessment is the primary care team for the patient.
Another difference is the extent to which trainee education is incorporated. The majority of front‐end operations do not include trainee physicians, with the exception of one team triage study that showed overall improvement in quality and efficiency with both a junior and senior physician present.27 The swarming model was designed expressly with the intention of integrating trainee education.
Although involvement of trainee physicians in the ED has been associated with increased LOS,2 an observational study of FCR showed that teaching behaviors, outside of directly teaching the physical examination, did not have a statistically significant effect on rounding time.10 This may indicate that the serial model of care traditionally used in the academic ED setting—where many aspects of history, physical examination, and assessment are repeated at separate times by training and supervising providers—may be the cause of the increased LOS seen with trainee involvement, rather than the educational activities themselves.
One of the purposes of this investigation was to conceptualize swarming to establish a foundation and clarify future directions for research. A potential area of investigation involves best practices in swarming. This study will assist us in standardizing this model, which is critical for consistent training and education of staff. At the same time, there may be certain types of patients or complaints or certain environmental factors within the ED that lend themselves more toward successful use of the swarming model. With further research, we hope to delineate the circumstances where a more uniform swarming model would be appropriate and the conditions under which intentional exceptions or variations may be made.
We also plan to evaluate the effects of swarming in comparison to the traditional serial model of care with regard to efficiency and education. Since there are times in the ED when we are simultaneously utilizing swarming with some patients and traditional serial care with others, there exists an opportunity to directly compare these two models while other environmental factors are consistent. We plan to measure specific efficiency metrics such as door‐to‐physician time, time to orders, time to treatment, and overall LOS.
Finally, we plan to evaluate the effect of swarming on tangible educational outcomes. This study has highlighted specific areas of trainee education that may be particularly affected by swarming, such as role modeling, bedside teaching, and resident autonomy. In future investigations, we aim to measure these outcomes, gathering information to formalize educational best practices in the swarming model.
Limitations
For the observational portion of the study, swarms were conveniently sampled based on when a provider decided to swarm for a patient evaluation and when research staff was available; these encounters tended to occur during less busy times in the ED, most often in the morning. As a result, there was some selection bias in favor of visits that occurred during morning hours.
The decision was made to exclude non–English‐speaking patients from the study because the presence of an interpreter could change the durations of various components of the swarm. This choice, however, resulted in the exclusion of Spanish‐speaking patients/families, which compose approximately one‐third of our ED patient population. The patient/family satisfaction questionnaire was completed with a research staff member present, which could have induced social desirability bias in families and therefore affected their responses.
For the qualitative portion of the study, focus groups were not of homogenous size due to scheduling constraints for certain participants. Additionally, the choice was made to have research staff moderate the nurse and resident focus groups, since moderation by the principal investigator (a physician) could have influenced responses. Having different individuals moderate the various focus groups may have led to slight differences in response types, although there were also benefits to having research staff moderate these groups, including more open discussion and subsequently more trustworthy qualitative data. Furthermore, it is possible that participants with strongly positive or negative opinions about swarming may have been more likely to volunteer to participate in focus groups, thereby introducing some bias.
Of note, due to scheduling constraints we were unable to include rotating resident physicians from other institutions so only pediatric residents based at our institution were involved. Residents from external programs, which include pediatrics, family medicine, and emergency medicine, may have brought different perspectives to the focus group about swarming, especially with regard to its educational impact. Despite best efforts to facilitate open conversation by all participants, we cannot exclude the possibility that members of the focus groups may have censored comments due to existing relationships with other participants.
Conclusions
Swarming was created as a novel model in an attempt to balance our clinical and educational missions, two priorities that are truly at the core of academic emergency medicine. This investigation sought to better conceptualize the approach by combining perceptions from physicians, nurses, and families with in vivo measurements of swarming encounters. We ultimately found multiple benefits and barriers, which are underscored by both the inherent variability in the ED and the observed variability in the implementation of swarming. The findings presented here provide a critical foundation for our future efforts to refine, standardize, and appraise our swarming model.
Supporting information
Appendix S1. Questionnaires used in staff focus groups.
Appendix S2. Questionnaire used in brief family interview.
AEM Education and Training 2020;4:43–53
Presented at the Pediatric Academic Societies Annual Meeting, Toronto, Ontario, Canada, May 2018.
Author contributions: JLP and DRL conceptualized and designed the study; ARS and PKP contributed to the study design; JLP and DRL supervised the conduct of the study and data collection and also actively collected data; JLP, ARS, and PKP performed the data analyses; JLP drafted the manuscript and all authors contributed substantially to its revision; and JLP takes responsibility for the manuscript as a whole.
The authors have no relevant financial information or potential conflicts of interest to disclose.
Supervising Editor: Sorabh Khandelwal, MD
[This article was modified on October 23, 2019, after initial online publication to correct the degree information of the last author.]
References
- 1. Croskerry P, Chisholm C, Vinen J, Perina D. Quality and education. Acad Emerg Med 2002;9:1108–15. [DOI] [PubMed] [Google Scholar]
- 2. James C, Harper M, Johnston P, Sanders B, Shannon M. Effect of trainees on length of stay in the pediatric emergency department. Acad Emerg Med 2009;16:859–65. [DOI] [PubMed] [Google Scholar]
- 3. Merritt C, Munzer BW, Wolff M, Santen SA. Not another bedside lecture: active learning techniques for clinical Instruction. AEM Educ Train 2018;2:48–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sternszus R, MacDonald ME, Steinert Y. Resident role modeling: “it just happens.” Acad Med 2016;91:427–32. [DOI] [PubMed] [Google Scholar]
- 5. Benbassat J. Role modeling in medical education: the importance of a reflective imitation. Acad Med 2014;89:550–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wiler JL, Gentle C, Halfpenny JM, et al. Optimizing emergency department front‐end operations. Ann Emerg Med 2010;55:142–160.e1. [DOI] [PubMed] [Google Scholar]
- 7. Chan TC, Killeen JP, Kelly D, Guss DA. Impact of rapid entry and accelerated care at triage on reducing emergency department patient wait times, lengths of stay, and rate of left without being seen. Ann Emerg Med 2005;46:491–7. [DOI] [PubMed] [Google Scholar]
- 8. Rutman LE, Migita R, Woodward GA, Klein EJ. Creating a leaner pediatric emergency department: how rapid design and testing of a front‐end model led to decreased wait times. Pediatr Emerg Care 2015;31:395–8. [DOI] [PubMed] [Google Scholar]
- 9. Rosen P, Stenger E, Bochkoris M, Hannon MJ, Kwoh CK. Family‐centered multidisciplinary rounds enhance the team approach in pediatrics. Pediatrics 2009;123:e603–8. [DOI] [PubMed] [Google Scholar]
- 10. Bhansali P, Birch S, Campbell JK, et al. A time‐motion study of inpatient rounds using a family‐centered rounds model. Hosp Pediatr 2013;3:31–8. [DOI] [PubMed] [Google Scholar]
- 11. Schmutz JB, Eppich WJ. Promoting learning and patient care through shared reflection. Acad Med 2017;92:1555–63. [DOI] [PubMed] [Google Scholar]
- 12. Perniciaro J, Liu D, Liu D. Swarming: A new model to optimize efficiency and education in an academic emergency department. Ann Emerg Med 2017;70:435–6. [DOI] [PubMed] [Google Scholar]
- 13. Schmutz JB, Eppich WJ. When I say … team reflexivity. Med Educ 2019;53:545–6. [DOI] [PubMed] [Google Scholar]
- 14. Lowe DJ, Ireland AJ, Ross A, Ker J. Exploring situational awareness in emergency medicine: developing a shared mental model to enhance training and assessment. Postgrad Med J 2016;92:653–8. [DOI] [PubMed] [Google Scholar]
- 15. Burrows TJ. A Preliminary Rubric Design to Evaluate Mixed Methods Research [dissertation]. Blacksburg, VA: Virginia Polytechnic Institute and State University, 2013. [Google Scholar]
- 16. Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research, 3rd ed Los Angeles, CA: SAGE Publications, 2018. [Google Scholar]
- 17. Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Heal 2015;42:533–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Forman J, Damschroder L. Qualitative content analysis In: Jacoby L, Siminoff LA, editors. Empirical Methods for Bioethics: A Primer. Oxford, UK: Elsevier, 2007. [Google Scholar]
- 19. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. [DOI] [PubMed] [Google Scholar]
- 20. Yen K, Gorelick MH. Strategies to improve flow in the pediatric emergency department. Pediatr Emerg Care 2007;23:745–52. [DOI] [PubMed] [Google Scholar]
- 21. Beck J, Kind T, Meyer R, Bhansali P. Promoting resident autonomy during family‐centered rounds: a qualitative study of resident, hospitalist, and subspecialty Physicians. J Grad Med Educ 2016;8:731–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rappaport DI, Ketterer TA, Nilforoshan V, Sharif I. Family‐centered rounds: views of families, nurses, trainees, and attending physicians. Clin Pediatr (Phila) 2012;51:260–6. [DOI] [PubMed] [Google Scholar]
- 23. DeBehnke D, Decker MC. The effects of a physician‐nurse patient care team on patient satisfaction in an academic ED. Am J Emerg Med 2002;20:267–70. [DOI] [PubMed] [Google Scholar]
- 24. McCarthy ML, Ding R, Zeger SL, et al. A randomized controlled trial of the effect of service delivery information on patient satisfaction in an emergency department fast track. Acad Emerg Med 2011;18:674–85. [DOI] [PubMed] [Google Scholar]
- 25. Spaite DW, Bartholomeaux F, Guisto J, et al. Rapid process redesign in a university‐based emergency department: decreasing waiting time intervals and improving patient satisfaction. Ann Emerg Med 2002;39:168–77. [DOI] [PubMed] [Google Scholar]
- 26. Doyle SL, Kingsnorth J, Guzzetta CE, Jahnke SA, McKenna JC, Brown K. Outcomes of implementing rapid triage in the pediatric emergency department. J Emerg Nurs 2012;38:30–5. [DOI] [PubMed] [Google Scholar]
- 27. Burström L, Nordberg M, Örnung G, et al. Physician‐led team triage based on lean principles may be superior for efficiency and quality? A comparison of three emergency departments with different triage models. Scand J Trauma Resusc Emerg Med 2012;20:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Burström L, Engström ML, Castrén M, Wiklund T, Enlund M. Improved quality and efficiency after the introduction of physician‐led team triage in an emergency department. Ups J Med Sci 2016;121:38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lauks J, Mramor B, Baumgartl K, Maier H, Nickel CH, Bingisser R. Medical team evaluation: effect on emergency department waiting time and length of stay. PLoS One 2016;11:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ming T, Lai A, Lau P. Can team triage improve patient flow in the emergency department? A systematic review and meta‐analysis. Adv Emerg Nurs J 2016;38:233–50. [DOI] [PubMed] [Google Scholar]
- 31. Chan TM, Van Dewark K, Sherbino J, Lineberry M. Coaching for chaos: a qualitative study of instructional methods for multipatient management in the emergency department. AEM Educ Train 2019;3:145–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McGhee J, Crowe C, Kraut A, et al. Do emergency medicine residents prefer resident‐initiated or attending‐initiated feedback? AEM Educ Train 2017;1:15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Biondi EA, Varade WS, Garfunkel LC, et al. Discordance between resident and faculty perceptions of resident autonomy: can self‐determination theory help interpret differences and guide strategies for bridging the divide? Acad Med 2015;90:462–71. [DOI] [PubMed] [Google Scholar]
- 34. Li J, Caviness AC, Patel B. Effect of a triage team on length of stay in a pediatric emergency department. Pediatr Emerg Care 2011;27:687–92. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Questionnaires used in staff focus groups.
Appendix S2. Questionnaire used in brief family interview.


