Highlights
-
•
The electronic medical record alert improved screening for HCV and HIV.
-
•
91% of HCV and 100% of HIV positive patients were linked into care.
-
•
Low post-intervention screening rates suggest additional interventions are required.
Keywords: Human immunodeficiency virus, Hepatitis C, Electronic medical record alert, Screening, Linkage to care
Abstract
Societal and economic burdens of hepatitis C virus (HCV) and human immunodeficiency virus (HIV) continue to grow. The Centers for Disease Control and Prevention recommends a one-time HCV screen for individuals in the Baby Boomer population (those born between 1945 and 1965) and a one-time HIV screen for all individuals between ages 13–64 years regardless of risk factors, with more frequent screening for both conditions based on individual risk factors.
This study took place at Atrium Health, a healthcare system with approximately 12 million patient encounters per year. The aims of this study were to assess the impact of the HCV and HIV electronic medical record (EMR) alerts recently implemented on screening rates and linkage to care.
Data were collected from 12 primary care practices. Implementation of EMR alerts increased HCV and HIV screening from 1,934 of 59,632 (3.2%) to 13,726 of 60,422 (22.7%) and 6,950 of 112,813 (6.2%) to 12,379 of 109,173 (11.3%) respectively. The HCV screening resulted in an increase of patients with antibody positive results having a subsequent RNA test from 68% (122/179) to 98% (430/442). 74 of 81 (91%) of HCV and 15 of 15 (100%) of HIV positive patients were linked into care.
The addition of an EMR alert was associated with improved screening for HCV and HIV in primary care practices. Screening all patients decreases testing stigma since there is a lowered risk of disease transmission for those who test positive. However, post-intervention screening rates indicate further opportunities exist for additional interventions to increase screening rates.
1. Introduction
In the US, it is estimated that approximately 2.4 million people have chronic hepatitis C virus (HCV) and up to 75% of those people with chronic HCV are unaware that they are infected (Edlin et al., 2015, Hofmeister et al., 2019, Centers for Disease Control and Prevention, 2018). Half of cases are related to intravenous drug use, and the remainder from blood transfusions, sexual contact, tattoos, and medical procedures (Smith et al., 2012, Armstrong et al., 2006, Rein et al., 2011). Most patients were infected between 1960 and 1980, and consequently “Baby Boomers” born between 1945 and 1965 account for the majority of all chronic HCV infections in adults (Smith et al., 2012). To improve quality of life and prevent transmission, the Centers for Disease Control and Prevention (CDC) recommends a one-time HCV blood test to screen all adults born between 1945 and 1965 (Smith et al., 2012). U.S. Preventive Services Task Force (USPSTF) has also made draft recommendations for a one time HCV blood test to screen all adults 18-79 (United States Preventive Services Task Force, 2019). <20% of Baby Boomers have been screened for HCV as of 2015 (Jemal and Fedewa, 2017).
Recently, increased screening and the development of effective antiviral treatments have led to marked improvements in HCV patient outcomes. Current treatments with direct-acting antiviral agents (DAAs) are highly efficacious with sustained virologic response (SVR) rates of >95% for the vast majority of patients (Barth, 2015, Jacobson et al., 2017). However, even when patients received appropriate treatments, delayed access to care is associated with a 5–20% increased risk for liver cirrhosis, putting them at high risk for additional complications like hepatocellular carcinoma (HCC) (Barth, 2015). It has been previously shown that HCV alerts can improve screening rates in primary care (Konerman et al., 2017, Al-Hihi et al., 2017).
For human immunodeficiency virus (HIV) infection, the CDC estimates that greater than 1.2 million persons aged 13 years and older are living with HIV in the United States, including 14% whose infections have not been diagnosed (Centers for Disease Control and Prevention, 2019). The 2015 national HIV/AIDS strategy has a goal to increase the percentage of people living with HIV who know their status from 85.8% in 2016 to 90% (Centers for Disease Control and Prevention, 2015). In 2006, the CDC guidelines recommended universal screening for persons aged 13–64 years. The CDC also recommends that clinicians screen asymptomatic sexually active men who have sex with men (MSM) at least annually. Furthermore, clinicians should consider the benefits of more frequent screening (e.g. once every 3 or 6 months) for individuals including MSM at increased risk for HIV Infection.
A new federal action initiative for HIV, “Ending the HIV Epidemic: A Plan for America,” set a goal of a 75% reduction in new HIV infections during the next five years and a 90% drop within a decade. The plan emphasizes early diagnosis, rapid treatment, prevention including use of pre-exposure prophylaxis (PrEP), as well as rapid detection and response to emerging clusters of HIV infection. Mecklenburg County in Charlotte, NC, is one of 48 priority counties in the United States. More than 50% of new HIV diagnoses occurred in these 48 counties (Fauci et al., 2019, Eisinger et al., 2019). The Mecklenburg County Health Department (MCHD) facilitated the development of a community plan entitled “Getting to Zero” for Charlotte-Mecklenburg, also emphasizing improved diagnosis and linkage to care for residents of Charlotte and the surrounding area (Mecklenburg County Health Department, 2018).
Electronic medical record (EMR) technologies (e.g., electronic alerts, checklists, and decision support systems) are increasingly promoted as innovative platforms to streamline preventive health programs and improve compliance with clinical guidelines (Herwehe et al., 2012, Konerman et al., 2017, Lin et al., 2017, United States Department of Health & Human Services, 2018). To leverage the full potential of EMR tools, they must be user-friendly, efficient (i.e. limited to a few clicks), and fit seamlessly into the clinical workflow. Here we describe the design and implementation of EMR alerts to streamline the HCV and HIV screening processes in primary care settings within a large, integrated healthcare system along with an educational and linkage to care support program detailing disease epidemiology, screening recommendations, and algorithms to guide screening efforts. The screening algorithms are designed to minimize additional burden on providers as they increase volume of HCV and HIV screening.
2. Methods
This pre/post study took place at Atrium Health (formerly Carolinas HealthCare System) a large, non-profit, vertically integrated healthcare system with approximately 12 million patient encounters per year across the Southeast United States. The 12 practices chosen for the study included those with high numbers of patients born between 1945 and 1965 including 5 safety net practices serving predominantly Medicaid and uninsured patients, located in and around the metropolitan area of Charlotte, NC. Here we describe pre/post year-over-year comparisons for the HCV and HIV alerts, screening, and linkage to care. Following a positive HCV or HIV test, patients are contacted to schedule an appointment with a primary care provider to inform them of their diagnosis. The patients are scheduled for continued care by their primary care physician, or they are referred to a hepatologist or infectious disease specialist in the healthcare system. Linkage to care for this study is defined as the completion of a first medical visit after diagnosis into primary or specialty care. While we expect to have a follow up visit within one month after diagnosis, there is no timeframe in this study for linkage to care for the first medical visit after diagnosis.
Atrium Health has used Cerner as its EMR since 2004 (Cerner - Millennium version). This program has a multitude of built-in health maintenance categories with alerts that prompt providers to perform various guideline-recommended screenings. HCV and HIV alerts were activated in 2016 and 2017 respectively. For both alerts, discussions were held by the Quality Committee that is responsible for coordinating clinical metrics, between healthcare system administration, infectious disease physicians, primary care, the information systems department, and quality improvement personnel. The algorithms are designed to minimize additional burden on providers (Kershaw et al., 2018, Moyer and Force USPST, 2013). Once activated, the alerts were seen in 200 + primary care practices within the healthcare system and are currently still active as of the writing of this paper.
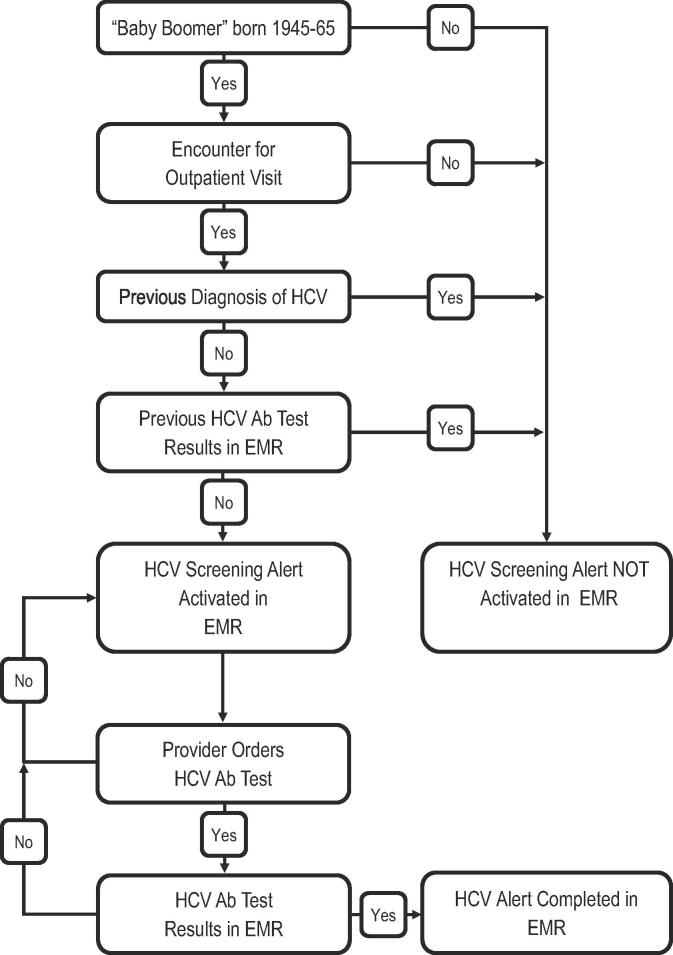
Firstly, the HCV alert prompted primary care providers to perform HCV screening for patients seen in primary care clinics: 1) born between 1945 and 1965; 2) lacked a prior diagnosis of HCV infection; and 3) lacked prior documentation of HCV antibody testing. As well as identifying patients with HCV in the primary care setting, the EMR provides a streamlined referral process to specialty care for newly diagnosed patients. For HCV, the alert was initially activated at one residency primary care location within the healthcare system for five months along with Plan-Do-Study-Act (PDSA) cycles including resident lectures, public education posters placed in the clinic in both English and Spanish languages, and a reminder flyer placed into patient charts placed outside the exam room. After showing the proportion of patients receiving screening during the trial period increased from 30% to 60%, the alert was turned on system-wide in May 2016. The logic for the HCV alert is as follows (Fig. 1): when patients present to primary care, an EMR algorithm identifies Baby Boomer adult patients, excluding them if they have a prior HCV diagnosis or if HCV screening or diagnostic testing has already been documented in the EMR. When the provider sees the alert, the provider is encouraged to notify the patient about the HCV screening test. To comply with the alert requirements, either an HCV test will be ordered, and results documented in the EMR thereby satisfying the alert, or if the patient refuses, the alert will remain active in their health maintenance module until satisfied as above. The alert is automatically canceled if a hospice care diagnosis is entered into the EMR.
Fig. 1.
Algorithm used in the Electronic Medical Record (EMR) to determine process for an HCV Screening in Primary Care within Atrium Health, 2019.
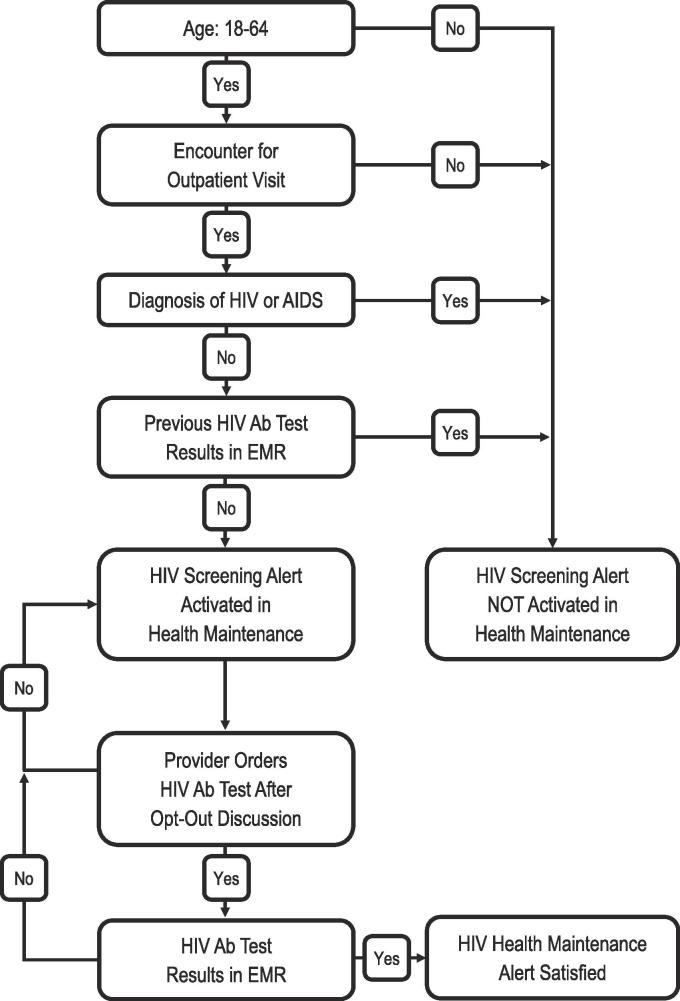
Secondly, the HIV alert, (Fig. 2), prompted providers to screen adult patients (age 18–64 years), who meet the eligibility criteria for a once in a lifetime HIV screening, and no prior HIV diagnosis or test documented in the EMR. Since October 2017, the alert appears on the ambulatory summary page in the health maintenance section of the EMR and does not include a risk factor-based screen other than age. The alert was restricted to age 18–64 years rather than the CDC recommended guideline of 13–64 years based on concerns regarding extremely low prevalence of HIV in patients < 18 years of age within the healthcare system. When the provider sees the alert, they are encouraged to notify the patient of the screening test using opt-out language. To comply with the alert requirements, either a test will be ordered, and results documented in the EMR thereby satisfying the alert, or if the patient refuses, the alert will remain active in their health maintenance module until satisfied as above. As with HCV, the alert is automatically canceled if a hospice care diagnosis is entered into the EMR.
Fig. 2.
Algorithm used in the Electronic Medical Record (EMR) to determine process for an HIV Screening in Primary Care with Atrium Health, 2019.
Statistical analyses were performed using R v3.43 (R Foundation for Statistical Computing, Vienna, Austria). Data were grouped into two time periods: 1) the 12-month time period preceding alert activation; and 2) the 12-month time period after alert activation. The mean proportion of patients who received screening in each time period was compared using a chi square test. The study was approved by the Atrium Health IRB as quality improvement on 07/15/2016.
In addition to alert activation, 10 of the 12 practices received an in-person provider peer-to-peer educational program with updates on the alerts, disease epidemiology, screening recommendations, and algorithms to guide screening efforts to supplement HCV and HIV screening and linkage to care for positive patients. The training received by the practices did not include the PDSA cycle. However, practices were encouraged to tailor their screening methods to meet the needs of their patients. The remaining 2 practices chose to receive the presentation materials by email either due to time constraints or expression of little need for the educational session. We followed up with practices a year later to present the results of their practice in comparison to the total screening for all practices in the overall project.
3. Results
Overall there was a statistically significant increase in the proportion of patients receiving screenings after the implementation of the alerts for patients seen at the 12 practices evaluated. Out of 59,632 eligible patients, 1,934 (3.2%) were adequately screened for HCV the year prior to the EMR alert. This increased to 22.7% (13,726 patients screened out of 60,422 total eligible patients) after the EMR alert was instituted. Out of 112,813 eligible patients, 6,950 (6.2%) were adequately screened for HIV the year prior to the EMR alert. This increased to 11.3% (12,379 patients screening out of 109,173 total eligible patients) after the EMR alert was instituted.
3.1. HCV screening results
Numbers of primary care patients who were eligible for screening, completed screening of antibody tests, were RNA positive, and linked into care across differing demographic groups one-year prior and one-year post initiation of a Baby Boomer HCV alert are shown in Table 1. In the 12 months prior to activation of the HCV alert from May 2015 to April 2016, 1,934 of 59,632 (3.2%) patients were screened at the 12 practices. In the 12 months following the HCV alert from May 2016 to April 2017, 13,726 of 60,422 (22.7%) patients were screened at the 12 practices, a 19.5% absolute increase compared to the year prior (p < 0.001, Table 1). The HCV screening resulted in an increase of antibody positive results having an RNA test performed from 68% (122/179) to 98% (430/442). Before the alert, 66 RNA positive HCV patients were detected increasing to 81 with the alert, and linkage to care increased from 59 (89%) to 74 (92%) patients post alert.
Table 1.
Numbers of primary care patients one-year prior and one-year post initiation of a hepatitis C virus alert for baby boomers born 1945–1965.
| Table 1. | Eligible for Screening | Completed Ab Test (% of Eligible)a | Ab+(RNA Tested) | RNA Positive (Linked to Care) | ||||
|---|---|---|---|---|---|---|---|---|
| HCV Alert | Pre-Alert | Post-Alert | Pre-Alert | Post-Alert | Pre-Alert | Post-Alert | Pre-Alert | Post-Alert |
| Total | 59 632 | 60 422 | 1 934 (3.2) | 13 726 (22.7) | 172(122) | 442(430) | 66(59) | 81(74) |
| Race | ||||||||
| African American | 25% | 25% | 36% | 31% | 52% (48%) | 54%(55%) | 59%(61%) | 60%(58%) |
| 14 908 | 15 106 | 696 (4.7) | 4 255 (28.2) | 89(58) | 240(2 3 5) | 39(36) | 49(43) | |
| White | 61% | 61% | 56% | 62% | 38%(45%) | 40%(40%) | 30%(31%) | 33%(35%) |
| 36 376 | 36 857 | 1 083 (2.9) | 8 510 (23.1) | 66(55) | 175(1 7 1) | 20(18) | 27(26) | |
| Asian | 1% | 1% | 2% | 1% | 2%(2%) | 2%(2%) | 2%(2%) | 1%(0%) |
| 596 | 604 | 39 (6.5) | 137 (22.3) | 4(2) | 8(7) | 1(1) | 1(0) | |
| Other/Unknown | 13% | 13% | 6% | 6% | 8%(6%) | 4%(4%) | 9%(6%) | 6%(7%) |
| 7 752 | 7 855 | 116 (1.5) | 824 (10.5) | 13(7) | 19(17) | 6(4) | 4(5) | |
| Gender | ||||||||
| Male | 40% | 40% | 45% | 42%b | 59%(61%) | 52%(52%) | 67%(66%) | 57%(57%) |
| 23 853 | 24 169 | 870 (3.6) | 5 765 (23.9) | 102(74) | 230(2 2 4) | 44(39) | 46(42) | |
| Female | 60% | 60% | 55% | 58%b | 40%(39%) | 48%(48%) | 34%(34%) | 43%(43%) |
| 35 779 | 36 253 | 1 064 (3.0) | 7 961 (22.0) | 70(48) | 212(2 0 6) | 22(20) | 35(32) | |
| Age | 59.0 | 60.0 | 58.2 | 60.4 | 58.0(57.8) | 60.8(60.6) | 56.9(57.9) | 60.3(60.8) |
| Payor | ||||||||
| Medicaid | 3% | 3% | 5% | 3% | 24%(22%) | 10%(10%) | 21%(21%) | 11%(10%) |
| 1 789 | 1 813 | 97 (5.4) | 412 (22.7) | 41(27) | 44(42) | 14(12) | 9(7) | |
| Medicare | 24% | 25% | 21% | 23% | 18%(20%) | 14%(14%) | 18%(21%) | 19%(17%) |
| 14 312 | 15 106 | 406 (2.8) | 3 157 (20.9) | 31(24) | 61(60) | 12(12) | 15(13) | |
| Commercial | 65% | 66% | 63% | 69% | 31%(34%) | 57%(58%) | 32%(33%) | 54%(55%) |
| 38 761 | 39 879 | 1 218 (3.1) | 9 471 (23.7) | 54(42) | 253(251) | 21(19) | 44(41) | |
| Self-Pay/Other | 8% | 6% | 11% | 5% | 27%(24%) | 19%(18%) | 29%(25%) | 16%(18%) |
| 4 770 | 3 624 | 213 (4.4) | 686 (18.9) | 46(29) | 84(77) | 19(16) | 13(13) | |
Change from pre-alert (aAll variables except for Gender = p < 0.001; b = p < 0.1); Baseline May 2015 - April 2016; Y1 May 2016 - April 2017, Atrium Health.
Notably, when looking at screening rates broken down into different demographics, African American patients increased screening rates from 4.7% to 28.2% (p < 0.001) and Caucasian 2.9% to 23.1% (p < 0.001). Additionally, males increased their screening rates from 3.6% to 23.9% (p < 0.001) and females 3.0% to 22.0% (p < 0.001). All categories of payor status showed significantly increased screening rates post the EMR alert (p < 0.001). Notably, lower proportions of African American patients (36% v 31%) and higher proportions of Caucasian (56% vs 62%) patients completed HCV screening after the alert (p < 0.001). However, proportions of African American patients who completed screening before and after the EMR alert were still significantly higher than the eligible patient populations. Additionally, a lower proportion of males (45% vs 42%) and a higher proportion of females (55% vs 58%) completed the screening after the alert (p < 0.05). Finally, the payor status proportions of the eligible patient populations screened were also significantly different before and the alert as well.
3.2. HIV screening results
Table 2 outlines the numbers of primary care patients who were eligible for screening (patients aged 18–64 years), completed screening (eligible patients), completed screening (all patients regardless of age), were viral load positive, and linked to care across differing demographic groups one year prior and one-year post initiation of an HIV alert for adults age 18–64. From October 2016 to September 2017, the 12 months prior to activation of the HIV alert, 6,950 of 112,813 (6.2%) eligible patients were screened at the 12 practices. In the 12 months following activation of the HIV alert from October 2017 to September 2018, 12,379 of 109,173 (11.3%) eligible patients were screened at the 12 practices, a 5.1% absolute increase compared to the year prior (p < 0.001).
Table 2.
Numbers of primary care patients one-year prior and one-year post initiation of an HIV alert for eligible adults age 18–64 and all patient regardless of age.
| Table 2. | Eligible for Screening | Completed Screening (% of Eligible Patients) | Completed Screening(All Patients) | Viral Load Positive(All Patients) | Linked to Care (All Patients) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| HIV Alert | Pre-Alert | Post-Alerta | Pre-Alert | Post-Alertb | Pre-Alert | Post-Alertb | Pre-Alert | Post-Alert | Pre-Alert | Post-Alert |
| 112 813 | 109 173 | 6 950 (6.2) | 12 379 (11.3) | 7 105 | 13 370 | 19 | 15 | 17 | 15 | |
| Race | ||||||||||
| African American | 26% | 26% | 58% | 48% | 58% | 45% | 74% | 60% | 76% | 60% |
| 29 331 | 28 385 | 4 031 (13.7) | 5 942 (20.9) | 4 121 | 6 017 | 14 | 9 | 13 | 9 | |
| Caucasian | 54% | 53% | 25% | 34% | 26% | 33% | 21% | 20% | 24% | 20% |
| 60 919 | 57 862 | 1 738 (2.8) | 4 209 (7.3) | 1 847 | 4 412 | 4 | 3 | 4 | 3 | |
| Asian | 2% | 2% | 1% | 2% | 1% | 2% | 0% | 0% | 0% | 0% |
| 2 256 | 2 183 | 70 (3.1) | 248 (11.3) | 71 | 267 | 0 | 0 | 0 | 0 | |
| Other/Unknown | 18% | 19% | 16% | 16% | 15% | 20% | 5% | 20% | 0% | 20% |
| 20 307 | 20 743 | 1 111 (5.5) | 1 980 (9.5) | 1 066 | 2 674 | 1 | 3 | 0 | 3 | |
| Gender | ||||||||||
| Male | 38% | 39% | 39% | 43% | 40% | 43% | 74% | 80% | 82% | 80% |
| 42 869 | 42 577 | 2 711 (6.3) | 5 323 (12.5) | 2 842 | 5 749 | 14 | 12 | 14 | 12 | |
| Female | 62% | 61% | 61% | 57% | 60% | 57% | 26% | 20% | 18% | 20% |
| 69 944 | 66 596 | 4 240 (6.1) | 7 056 (10.6) | 4 263 | 7 621 | 5 | 3 | 3 | 3 | |
| Age | 43.3 | 44.0 | 38.3 | 42.7 | 40.0 | 43.6 | 31.1 | 44.2 | 30.8 | 44.2 |
| Payor | ||||||||||
| Medicaid | 6% | 7% | 18% | 14% | 17% | 14% | 21% | 27% | 29% | 27% |
| 6 769 | 7 642 | 1 251 (18.5) | 1 733 (22.7) | 1 208 | 1 872 | 4 | 4 | 5 | 4 | |
| Medicare | 4% | 3%*** | 2% | 4% | 4% | 4% | 0% | 7% | 0% | 7% |
| 4 513 | 3 275 | 139 (3.1) | 495 (15.1) | 284 | 535 | 0 | 1 | 0 | 1 | |
| Commercial | 79% | 65%*** | 56% | 54% | 56% | 54% | 63% | 33% | 59% | 33% |
| 89 122 | 70 962 | 3 892 (4.3) | 6 685 (9.4) | 3 979 | 7 220 | 12 | 5 | 10 | 5 | |
| Self-Pay/Other | 11% | 25% | 24% | 28% | 23% | 28% | 16% | 33% | 12% | 33% |
| 12 409 | 27 294 | 1 668 (13.4) | 3 466 (12.7) | 1 634 | 3 743 | 3 | 5 | 2 | 5 | |
Change from pre-alert (a = p < 0.001 for Payor only; b = p < 0.001 for all variables); Baseline Oct 2016 – Sept 2017; Y1 Oct 2017 – Sept 2018, Atrium Health.
Similarly to HCV, for HIV, African American patients increased screening rates from 13.7% to 20.9% (p < 0.001) and Caucasians increased from 2.8% to 7.3% (p < 0.001). Both females and males increased screening rates (6.3% vs 12.5%) and (6.1% to 10.6%) respectively (p < 0.001). Finally, by average age, eligible patients screened after the alert were slightly older (40.0 v 43.6 years; p < 0.001). Similar difference was observed for all patients who completed screening.
The racial proportions screened before and after the alert were also significantly different than the eligible populations within the 12 practices before and after the alert. There were a higher proportion of males (40% vs 43%) and a lower proportion of females (60% vs 57%) for all patients who completed the screening after the alert (p < 0.001). Similar differences in gender proportions were observed for eligible patients who completed screening. All patients screened were on average older after the alert (40.0 v 43.6; p < 0.001). A similar difference in ages was observed for eligible patients who completed screening. The payor status proportions of the eligible populations were also significantly different before and after the alert as well. A similar difference in payor status proportions was also observed for both eligible patients and all patients screened.
The percentage linked into care improved from 90% to 100% with all 15 newly diagnosed HIV patients linked after the alert. Although Mecklenburg County had a high diagnosis rate, the practices in this study had a slight decrease in new diagnoses (17 prior year, 15 post year) which is in line with a slight downward trend in new diagnoses across both the state and metropolitan area of Charlotte seen since 2016 (Centers for Disease Control and Prevention, 2018).
4. Limitations
The results of this analysis have several limitations. Atrium Health has 1.2 million primary care patients and the screening data presented here represents less than 10 percent of the primary care population of the healthcare system. Practices receiving the educational program were selected based on having the highest number of patients who fell into the Baby Boomer cohort, a number not representative of all practices in the system. In addition, the results only apply to the patients who were seen within Atrium Health and any other screening and/or linkage to care information outside the healthcare system was not included. These results apply to patients living in a large, Southeast, metropolitan region and are not applicable to other regions of the United States. Impact of the educational program could not be evaluated separately from the impact of the alert. The tests highlighted in the algorithms developed were identified as the ones used by Atrium Health for HCV and HIV testing. Other tests such as antibody and RNA testing are available and may be utilized by other healthcare facilities. While the linkage to care rates are high, this may be influenced by the low overall number of positive patients.
5. Discussion and conclusion
In line with previous studies in primary care (Federman et al., 2017, Goel et al., 2017, Kershaw et al., 2018, Marcelin et al., 2016, Centers for Disease Control and Prevention, 2019), the addition of an EMR alert was associated with improved screening for HCV and HIV in primary care practices within a large healthcare system. As compared to another urban healthcare system in Kansas City, KS, their absolute increase in HCV screenings was 25% in the birth cohort as compared to 19% in North Carolina (Al-Hihi et al., 2017). Our increase in screening rates for HCV were more in line with a study in two New York City practices where absolute increase in screening rates increased 20% compared to 19% in North Carolina (Goel et al., 2017). As compared to a Midwest study, their absolute increase in HIV screenings was 1.5% as compared to 5.1% in North Carolina. Another study in another urban healthcare system in Boston, MA had an absolute increase in HIV screenings of 15% (Kershaw et al., 2018).
Because of the concern of alert fatigue and maintaining the response time of EMRs, making changes to the EMR to include these screening alerts requires institutional committee reviews that require multiple levels of approvals before alerts can be activated (Sittig and Singh, 2012). However, once these institutional requirements are met, EMR alerts enhance routine HCV and HIV screening within medical settings and provide an opportunity to screen all who access the healthcare system without the need for the patient to acknowledge risk.
At a population level, screening all patients decreases stigma associated with being testing, as well as allowing for improved outcomes and lowered risk of disease transmission for those who test positive. Additionally, for the individual who tests positive within an integrated healthcare system with streamlined connection to specialty care, this enhanced support allows for high rates of linkage to care. Interventions such as EMR alerts, educational programs, coordinated mental health, substance abuse, and hepatitis treatment services, have been shown to independently improve HCV treatment uptake, adherence, and cure compared to usual care (Zhou et al., 2016).
For patients testing positive for the HCV antibody, subsequent RNA testing is necessary to determine current infection status. Unfortunately, this two-step process has associated inefficiencies such as the patient not returning for follow-up which can lead to incomplete testing for accurate diagnosis of HCV (McGibbon et al., 2013). Possible improvements would be implementation of reflex HCV RNA testing. Although not yet addressed by the US Preventive Services Task Force, the European Association for the Study of the Liver gives a grade B1 recommendation that reflex testing for HCV RNA in patients found to be HCV antibody-positive should be applied to increase linkage to care (European Association for the Study of the Liver, 2018). Reflex testing allows infection status to be determined without requiring a follow-up visit for blood draw and streamlines the process of ensuring that patients who screen HCV antibody-positive get the additional testing necessary; and patients with positive RNA can be immediately counseled about measures for protecting their liver and begin evaluation for antiviral treatment (McGibbon et al., 2013, Casas et al., 2018).
This study adds to the evidence on large-scale use of EMR alerts and offers other healthcare systems evidence that such large-scale alert implementation and education support can significantly improve outcomes through screening and linkage to care for infectious diseases.
Stakeholder engagement was key throughout the design and implementation of this initiative. Key stakeholders were providers who lent their medical and clinical expertise and the healthcare system quality team who championed the alert activation through partnership with EMR technology.
EMR modifications along with availability of connect-to-care partners within a large, vertically integrated healthcare system can significantly enhance screening and linkage to care for patients with HCV and HIV, however, the low post-intervention screening rates indicate there are additional interventions required to increase screening rates further.
CRediT authorship contribution statement
Hazel Tapp: Conceptualization, Methodology, Writing - original draft, Supervision, Funding acquisition. Thomas Ludden: Formal analysis, Writing - review & editing. Lindsay Shade: Resources, Writing - review & editing, Project administration. Jeremy Thomas: Data curation, Writing - review & editing. Sveta Mohanan: Writing - review & editing. Michael Leonard: Writing - review & editing.
Acknowledgements
Several people have provided support for the work in this project. Internal Medicine residents Drs. Andrew Simmelink and Linsey Spence provided evidence to support the HCV alert activation and Dr. Scott Furney requested for the HCV alert to be activated. Support was received from Gilead Sciences, Inc., through their FOCUS Program (Frontlines of Communities in the United States). FOCUS is a public health initiative that enables partners to develop and share best practices in routine blood-borne virus (HIV, HCV, HBV) screening, diagnosis, and linkage to care in accordance with screening guidelines promulgated by the U.S. Centers for Disease Control and Prevention (CDC), the U.S. Preventive Services Task Force (USPSTF), and state and local public health departments. FOCUS funding supports HIV, HCV, and HBV screening and linkage to the first medical appointment after diagnosis. FOCUS partners do not use FOCUS awards for activities beyond linkage to the first medical appointment.
Contributor Information
Hazel Tapp, Email: Hazel.Tapp@atriumhealth.org.
Thomas Ludden, Email: tom.ludden@atriumhealth.org.
Lindsay Shade, Email: Lindsay.shade@atriumhealth.org.
Jeremy Thomas, Email: Jeremy.thomas@atriumhealth.org.
Sveta Mohanan, Email: sveta.mohanan@atriumhealth.org.
Michael Leonard, Email: Michael.leonard@atriumhealth.org.
References
- Al-Hihi E., Shankweiler C., Stricklen D., Gibson C., Dunn W. Electronic medical record alert improves HCV testing for baby boomers in primary care setting: adults born during 1945–1965. BMJ Open Quality. 2017;6(2):e000084-e. doi: 10.1136/bmjoq-2017-000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong G.L., Wasley A., Simard E.P., McQuillan G.M., Kuhnert W.L., Alter M.J. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann. Int. Med. 2006;144(10):705–714. doi: 10.7326/0003-4819-144-10-200605160-00004. [DOI] [PubMed] [Google Scholar]
- Barth H. Hepatitis C virus: is it time to say goodbye yet? Perspectives and challenges for the next decade. World J. Hepatol. 2015;7(5):725–737. doi: 10.4254/wjh.v7.i5.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casas P., Navarro D., Aguilera A., Garcia F. A pilot study on the implementation of reflex testing for the diagnosis of active hepatitis C virus infection. Enferm Infecc Microbiol. Clin. 2018;37(5):348–349. doi: 10.1016/j.eimc.2018.05.005. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2015. National HIV/AIDS Strategy: National HIV/AIDS Strategy: Updated to 2020. Available from: <https://www.hiv.gov/federal-response/national-hiv-aids-strategy/nhas-update>.
- Centers for Disease Control and Prevention, 2018. Hepatitis C Questions and Answers for Health Professionals. US Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta. Available from: <https://www.cdc.gov/hepatitis/hcv/hcvfaq.htm>.
- Centers for Disease Control and Prevention, 2018. HIV Surveillance Report. Available from: <http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html>.
- Centers for Disease Control and Prevention, 2019. HIV Surveillance Report. Available from: <https://www.cdc.gov/hiv/statistics/overview/index.html>.
- Edlin B.R., Eckhardt B.J., Shu M.A., Holmberg S.D., Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology (Baltimore, Md) 2015;62(5):1353–1363. doi: 10.1002/hep.27978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisinger R.W., Dieffenbach C.W., Fauci A.S. HIV Viral Load and Transmissibility of HIV Infection: Undetectable Equals Untransmittable. JAMA. 2019;321(5):451–452. doi: 10.1001/jama.2018.21167. [DOI] [PubMed] [Google Scholar]
- European Association for the Study of the Liver EASL Recommendations on Treatment of Hepatitis C. J. Hepatol. 2018;69(2):461–511. doi: 10.1016/j.jhep.2018.03.026. [DOI] [PubMed] [Google Scholar]
- Fauci A.S., Redfield R.R., Sigounas G., Weahkee M.D., Giroir B.P. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321(9):844–845. doi: 10.1001/jama.2019.1343. [DOI] [PubMed] [Google Scholar]
- Federman A.D., Kil N., Kannry J., Andreopolous E., Toribio W., Lyons J. An electronic health record-based intervention to promote hepatitis C virus testing among adults born between 1945 and 1965: a cluster-randomized trial. Med. Care. 2017;55(6):590–597. doi: 10.1097/MLR.0000000000000715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel A., Sanchez J., Paulino L., Feuille C., Arend J., Shah B. A systematic model improves hepatitis C virus birth cohort screening in hospital-based primary care. J. Viral Hepatitis. 2017;24(6):477–485. doi: 10.1111/jvh.12669. [DOI] [PubMed] [Google Scholar]
- Herwehe J., Wilbright W., Abrams A., Bergson S., Foxhood J., Kaiser M. Implementation of an innovative, integrated electronic medical record (EMR) and public health information exchange for HIV/AIDS. J. Am. Med. Inf. Assoc.: JAMIA. 2012;19(3):448–452. doi: 10.1136/amiajnl-2011-000412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmeister M.G., Rosenthal E.M., Barker L.K., Rosenberg E.S., Barranco M.A., Hall E.W. Estimating Prevalence of Hepatitis C Virus Infection in the United States. Hepatology. 2019;69(3):1020–1031. doi: 10.1002/hep.30297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson I.M., Lawitz E., Gane E.J., Willems B.E., Ruane P.J., Nahass R.G. Efficacy of 8 Weeks of Sofosbuvir, Velpatasvir, and Voxilaprevir in Patients With Chronic HCV Infection: 2 Phase 3 Randomized Trials. Gastroenterology. 2017;153(1):113–122. doi: 10.1053/j.gastro.2017.03.047. [DOI] [PubMed] [Google Scholar]
- Jemal A., Fedewa S.A. Recent hepatitis C virus testing patterns among baby boomers. Am. J. Preventive Med. 2017;53(1):e31–e33. doi: 10.1016/j.amepre.2017.01.033. [DOI] [PubMed] [Google Scholar]
- Kershaw C., Taylor J.L., Horowitz G., Brockmeyer D., Libman H., Kriegel G. Use of an electronic medical record reminder improves HIV screening. BMC Health Serv. Res. 2018;18(1):14. doi: 10.1186/s12913-017-2824-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konerman M.A., Thomson M., Gray K., Moore M., Choxi H., Seif E. Impact of an electronic health record alert in primary care on increasing hepatitis c screening and curative treatment for baby boomers. Hepatology. 2017;66(6):1805–1813. doi: 10.1002/hep.29362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J., Mauntel-Medici C., Heinert S., Baghikar S. Harnessing the power of the electronic medical record to facilitate an opt-out HIV screening program in an urban academic emergency department. J. Public Health Manag. Pract. 2017;23(3):264–268. doi: 10.1097/PHH.0000000000000448. [DOI] [PubMed] [Google Scholar]
- Marcelin J.R., Tan E.M., Marcelin A., Scheitel M., Ramu P., Hankey R. Assessment and improvement of HIV screening rates in a Midwest primary care practice using an electronic clinical decision support system: a quality improvement study. BMC Med. Inf. Decis. Making. 2016;16(1):76. doi: 10.1186/s12911-016-0320-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGibbon E., Bornschlegel K., Balter S. Half a diagnosis: gap in confirming infection among hepatitis C antibody-positive patients. The Am. J. Med. 2013;126(8):718–722. doi: 10.1016/j.amjmed.2013.01.031. [DOI] [PubMed] [Google Scholar]
- Mecklenburg County Health Department, 2018. Getting to Zero Mecklenburg: A Community Plan to Reduce New Cases of HIV in Mecklenburg County. Available from: <https://www.mecknc.gov/HealthDepartment/CDControl/HIVSTDSurveillance/Documents/Getting%20to%20Zero%20Mecklenburg.pdf>.
- Moyer V.A., Force USPST Screening for hepatitis C virus infection in adults: U.S. Preventive Services Task Force recommendation statement. Ann. Int. Med. 2013;159(5):349–357. doi: 10.7326/0003-4819-159-5-201309030-00672. [DOI] [PubMed] [Google Scholar]
- Rein D.B., Wittenborn J.S., Weinbaum C.M., Sabin M., Smith B.D., Lesesne S.B. Forecasting the morbidity and mortality associated with prevalent cases of pre-cirrhotic chronic hepatitis C in the United States. Digestive and Liver Dis. 2011;43(1):66–72. doi: 10.1016/j.dld.2010.05.006. [DOI] [PubMed] [Google Scholar]
- Sittig D.F., Singh H. Electronic health records and national patient-safety goals. The New England J. Med. 2012;367(19):1854–1860. doi: 10.1056/NEJMsb1205420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B.D., Morgan R.L., Beckett G.A., Falck-Ytter Y., Holtzman D., Teo C.G. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945–1965. MMWR Recommendations and reports: morbidity and mortality weekly report Recommendations and reports. Centers for Disease Control. 2012;61(RR-4):1–32. [PubMed] [Google Scholar]
- United States Department of Health & Human Services, 2018. Office of the National Coordinator for Health Information Technology. HealthIT.gov. Available from: <http://www.healthit.gov/providers-professionals/benefitselectronic-health-records-ehrs>.
- United States Preventive Services Task Force Draft Recommendation Statement: Hepatitis C Virus Infection in Adolescents and Adults: Screening. 2019. https://www.uspreventiveservicestaskforce.org/Page/Document/draft-recommendation-statement/hepatitis-c-screening1
- Zhou K., Fitzpatrick T., Walsh N., Kim J.Y., Chou R., Lackey M. Interventions to optimise the care continuum for chronic viral hepatitis: a systematic review and meta-analyses. The Lancet Infect. Dis. 2016;16(12):1409–1422. doi: 10.1016/S1473-3099(16)30208-0. [DOI] [PubMed] [Google Scholar]