Abstract
This study aimed to elucidate the role of long non-coding RNA activated by transforming growth factor-β (lncRNA-ATB) in ovarian cancer and its underlying mechanisms of action. Expression levels of lncRNA-ATB in ovarian cancer cell line SKOV3 and in a healthy human ovarian cell line were compared using reverse transcription-quantitative polymerase chain reaction (RT-qPCR). The results indicated that lncRNA-ATB was expressed at significantly higher levels in SKOV3 cells compared with the healthy cell line. After downregulation of lncRNA-ATB expression in SKOV3 cells using lncRNA-ATB-short hairpin RNA, cell proliferation, apoptosis, invasion and migration were assessed using Cell counting kit-8, Live Dead staining, Transwell assay and wound healing assay, respectively. RT-qPCR and western blotting were used to quantify the expression of signal transducer and activator of transcription 3 (STAT3), phosphorylated (p)-STAT3, and the additional epithelial to mesenchymal transition (EMT)-related proteins E-cadherin and vimentin in SKOV3 cells. LncRNA-ATB downregulation significantly reduced SKOV3 cell proliferation, invasion and migration, promoted apoptosis, decreased the expression of p-STAT3 and vimentin, and increased E-cadherin expression. Taken together, these results suggest that lncRNA-ATB downregulation can inhibit ovarian cancer cell proliferation, invasion and migration, and promote cell apoptosis. Lnc-RNA-ATB may therefore be a new target for ovarian cancer treatment.
Keywords: ncRNA-ATB, ovarian cancer, proliferation, apoptosis, metastasis
Introduction
Ovarian cancer is one of the most common causes of gynecological reproductive system tumors (1). There are approximately 299,000 new cases of ovarian cancer and 152,000 related deaths each year, accounting for the seventh highest incidence among female malignant tumors (2). Most patients are already at an advanced stage by the time of diagnosis, and the 5-year survival rate of advanced ovarian cancer is less than 30% (3). Only 15% of patients are diagnosed at an early stage (stage 1) with a 5-year survival rate of 92% (4). In recent years, much research has focused on the development of new potential ovarian cancer targeted therapies (5–7).
Long non-coding RNAs (lncRNAs) are a class of RNAs with a length of more than 200 nucleotides that lack a meaningful open reading frame (8). LncRNAs participate extensively in embryonic development, apoptosis, cell cycle regulation, tumor formation and other biological processes (9–12). Previous studies have found that lncRNA plays an important role in tumor metastasis, and abnormal expression of many lncRNAs is directly related to tumor metastasis or recurrence (13–15). LncRNA activated by transforming growth factor-β (lncRNA-ATB) is part of a family of lncRNAs, which can regulate the invasion and metastasis of various tumor cells, such as intestinal cancer and liver cancer, by regulating cell phenotype switching (16–18). However, there have been no reports on the role of lncRNA-ATB in ovarian cancer. This study therefore aimed to investigate the role of lncRNA-ATB in ovarian cancer cells and to further explore the underlying mechanisms of its action.
Materials and methods
Cell culture and treatments
Ovarian cancer cell line SKOV3 (cat no. ATCC® HTB-77™) was obtained from American Type Culture Collection. Non-tumorous human ovarian surface epithelial cells (HOSEpiC; cat no. BNCC340096) were purchased from the BeNa Culture Collection (Suzhou Bei Na Chuanglian Biotechnology Co., Ltd.). SKOV3 and HOSEpiC cells were cultured in complete Dulbecco's Modified Eagle Medium (DMEM)/nutrient mixture F12 (Gibco, Thermo Fisher Scientific, Inc.) including 10% FBS (Gibco; Thermo Fisher Scientific, Inc.) and 1% penicillin-streptomycin solution at 37°C in a 5% CO2 incubator.
Cell transfection
LncRNA-ATB-shRNA and the negative control of lncRNA-ATB-shRNA (lncRNA-ATB-NC) were purchased from Biomics (Biomics Biotechnologies, Co., Ltd.). A total of 1 µg LncRNA-ATB-NC or 1 µg lncRNA-ATB-shRNA were transfected into SKOV3 cells using Lipofectamine 2000 (Invitrogen, Thermo Fisher Scientific, Inc.) according to the manufacturer's instructions. Total RNA was extracted from the cells 48 h after transfection, and the expression of lncRNA-ATB was detected using reverse transcription-quantitative PCR (RT-qPCR) to determine the transfection efficiency. Cells without any treatment Were considered as the control.
CCK-8 assay
The CCK-8 method was used to determine SKOV3 cell proliferative ability. A cell suspension at a concentration of 1×104/ml was prepared and 100 µl of this suspension was added to each well of a 96-well plate. Cells were then cultured for 12, 24 or 48 h, respectively, before 10 µl CCK-8 reagent (Sigma-Aldrich; Merck KGaA) was added to each well. After 2 h of incubation absorbance at a wavelength of 450 nm was measured using the FLUOstar® Omega Microplate Reader (BMG Labtech GmbH). This experiment was repeated three times.
Flow cytometry analysis
SKOV3 cells of different groups (control: Cells without any treatment, lncRNA-ATB-NC and lncRNA-ATB-shRNA respectively) were harvested using 0.2% trypsin, washed with phosphate buffered saline (PBS) and then fixed with 70% ethanol overnight at 4°C. The number of apoptotic cells was quantified using the AnnexinV-FITC/PI kit (cat no. 70-AP101-100; MultiSciences) according to the manufacturer's instructions. Cell apoptosis rate was measured using a FACS Calibur flow cytometer (BD Biosciences) and the data were analyzed using FlowJo software (version 7.6.1; FlowJo LLC). The assay was performed in triplicate.
Transwell assay
A transwell invasion assay was used to determine cell invasion ability. Polycarbonate filters (8-µm pore size; Corning Inc.) with Matrigel (BD Biosciences) were used in the transwell migration assay. A total of 200 µl DMEM (supplemented with 0.1% FBS) containing 1×105 SKOV3 cells was added to the upper chamber while 600 µl DMEM supplemented with 10% FBS was added to the lower chamber. After incubation for 48 h, any SKOV3 cells that had invaded into the lower chamber were fixed with 100% methanol at room temperature for 20 min, stained with 0.1% crystal violet at 37°C for 20 min, and counted using an upright microscope (magnification, ×200; five randomly-selected fields per chamber). Each transwell assay was repeated in five independent experiments.
Scratch wound healing assay
SKOV3 cells from different treatment groups (control, lncRNA-ATB-NC and lncRNA-ATB-shRNA, respectively) were seeded onto six-well plates (5×105 cells/well) and cultured until they reached 80–90% confluence. Scratch wounds were created in the monolayer of confluent SKOV3 cells using a 200 µl pipette tip. The wounded cells were then incubated at 37°C with 5% CO2 for 24 h. Wound healing was measured using ImageJ software version 1.46 (National Institutes of Heath) and images were captured using a phase-contrast microscope at two time points, immediately after scratching and after 24-h incubation. Data were presented as wound width (at 24 h)/wound width (at 0 h) ×100%.
RT-qPCR
Total RNA was isolated from cells using an EASYspin Plus tissue/cell RNA extraction kit (Aidlab Biotechnologies, Co. Ltd.) according to the manufacturer's instructions. RNA was reverse-transcribed into cDNA using a Transcriptor First Strand cDNA Synthesis kit (Roche Diagnostics) following the manufacturer's instructions. qPCR was performed on a LightCycler 480 system (Roche Diagnostics) using Fast SYBR Green Master Mix (Roche Diagnostics) as per the manufacturer's instructions. The sequences of RT-qPCR primers were obtained as required and listed as following: GAPDH forward, 5′-CTTTGGTATCGTGGAAGGACTC-3′; reverse, 5′-GTAGAGGCAGGGATGATGTTCT-3′; lncRNA- ATB forward, 5′-TCTGGCTGAGGCTGGTTGAC-3′; reverse, 5′-ATCTCTGGGTGCTGGTGAAGG-3′; STAT3 forward, 5′-ACAGCAGGATGGCCAGGTTGC-3′; reverse, 5′-TCTGTCTGGTGGCTGCTGCCT-3′; E-Cadherin forward, 5′-AGCCATGTACGTTGCTATCC-3′; reverse, 5′-CGTAGCACAGCTTCTCCTTAAT-3′; Vimentin forward, 5′-GCTGCAGGCCCAGATTCA-3′; reverse, 5′-TTCATACTGCTGGCGCACAT-3′. The following thermocycling conditions were used for PCR: Initial denaturation at 95°C for 45 sec, followed by 40 cycles of 95°C for 10 sec and 52°C for 35 sec. The relative expression ratio of target genes was calculated using the 2−∆∆Cq method (19).
Western blotting
Cells were washed twice with PBS, then lysed in RIPA buffer (cat. no. P0013B; Beyotime Institute of Biotechnology). Protein concentration was measured using a BCA assay kit (Thermo Fisher Scientific, Inc.). The cell lysates (30 µg/lane) were separated on 12% SDS polyacrylamide gels and transferred onto PVDF membranes (Bio-Rad Laboratory, Inc.). After blocking of non-specific binding with TBS-T (0.1% Tween) containing 5% non-fat milk for 1 h at room temperature, the membranes were incubated with the primary antibodies at 4°C overnight. Then, the membranes were incubated with horseradish peroxidase (HRP)-conjugated goat anti-rabbit secondary antibody (cat no. 7074; 1:2,000; Cell Signaling Technology, Inc.) for 2 h at room temperature. Finally, the protein bands were detected using the ChemiDOC™ system (Bio-Rad, Hercules, CA) following the manufacturer's protocol. The primary antibodies: Anti-STAT3 (1:1,000; cat no. 12640), anti-p-STAT3 (1:1,000; cat no. 9145), anti-E-cadherin (1:1,000; cat no. 3195), anti-vimentin (1:1,000; cat no. 5741) and anti-GAPDH (cat no. 5174) were purchased from Cell Signaling Technology, Inc. Protein bands were analyzed using ImageJ version 1.49 software (National Institute of Health).
Statistical analysis
Statistical analysis was performed using GraphPad Prism version 5.0 (GraphPad Software, Inc.). The tests performed were one-way ANOVA followed by Tukey's post-hoc test or a Student's t-test as appropriate. Data are presented as the mean ± SD. P<0.05 was considered to indicate a statistically significant difference.
Results
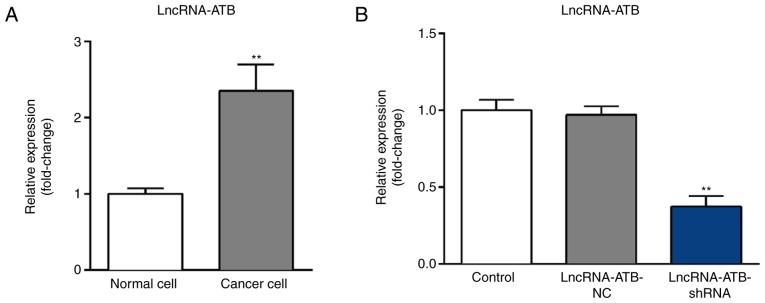
LncRNA-ATB is highly expressed in ovarian cancer cell line SKOV3
Expression levels of lncRNA-ATB in SKOV3 and HOSEpiC cells were measured using RT-qPCR. The results indicated that when compared with HOSEpiC cells, lncRNA-ATB was significantly upregulated in SKOV3 cells (Fig. 1A). To further investigate the role of lncRNA-ATB in ovarian cancer, lncRNA-ATB-shRNA or lncRNA-ATB-NC were transfected into SKOV3 cells. RT-qPCR results revealed that compared with the control group, lncRNA-ATB-shRNA significantly decreased the expression of lncRNA-ATB in SKOV3 cells (Fig. 1B).
Figure 1.
Expression of lncRNA-ATB in ovarian cancer cell line SKOV3. (A) RT-qPCR was used to detect the levels of lncRNA-ATB in SKOV3 cells and HOSEpiCs. (B) LncRNA-ATB-NC or lncRNA-ATB-shRNA was transfected into SKOV3 cells for 48 h, and the expression of lncRNA-ATB in SKOV3 cells was detected by RT-qPCR. Data were presented as the mean ± SD. Each experiment was repeated three times. **P<0.01 vs. control group. HOSEpiC, human ovarian surface epithelial cell; lncRNA-ATB, long non-coding RNA-activated by transforming growth factor-β; lncRNA-ATB-NC, long non-coding RNA-activated by transforming growth factor-β-negative control; RT-qPCR, reverse transcription-quantitative polymerase chain reaction; SKOV3, ovarian cancer cell line.
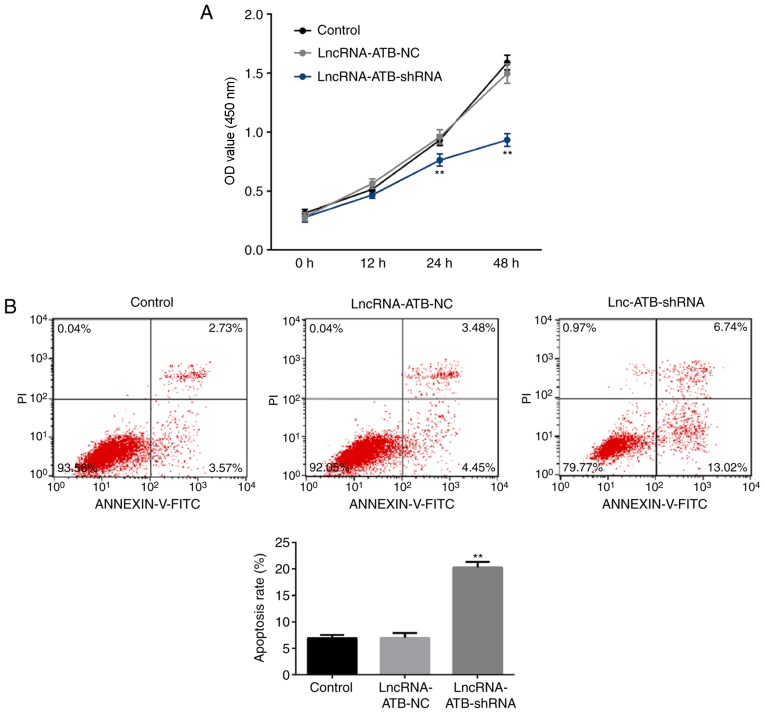
LncRNA-ATB downregulation reduces proliferation and induces apoptosis in SKOV3 cells
A CCK-8 assay was used to analyze cell proliferation and flow cytometry was used to analyze apoptosis. The results revealed that when compared with the control group, lncRNA-ATB-shRNA significantly reduced the proliferative ability of SKOV3 cells at the 24 and 48 h time points (Fig. 2A) and promoted apoptosis (Fig. 2B).
Figure 2.
Effect of lncRNA-ATB downregulation on SKOV3 cell proliferation and apoptosis. LncRNA-ATB-NC or lncRNA-ATB-shRNA was transfected into SKOV3 cells for 48 h. (A) Cell counting kit-8 assay was used to detect cell proliferation ability. (B) Flow cytometry was used to detect the apoptosis level. Data are presented as the mean ± SD. Each experiment was repeated three times. **P<0.01 vs. control group. LncRNA-ATB, long non-coding RNA-activated by transforming growth factor-β; lncRNA-ATB-NC, long non-coding RNA-activated by transforming growth factor-β-negative control; SKOV3, ovarian cancer cell line; PI, propidium iodide.
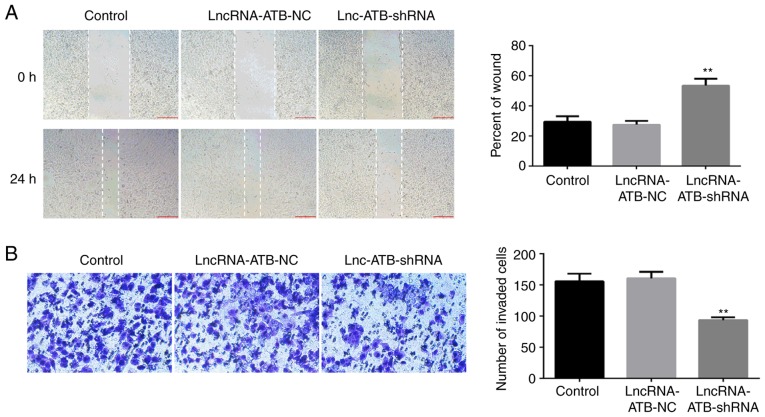
LncRNA-ATB downregulation reduces migration and invasion of SKOV3 cells
To study the effect of lncRNA-ATB downregulation on ovarian cancer cell migration and invasion, scratch wound healing and transwell assays were performed. The results revealed that when compared with the control group, lncRNA-ATB-shRNA significantly reduced the migration (Fig. 3A) and invasion ability (Fig. 3B) of SKOV3 cells.
Figure 3.
Effects of lncRNA-ATB downregulation on SKOV3 cell invasion and migration. (A) LncRNA-ATB-NC or lncRNA-ATB-shRNA was transfected into SKOV3 cells for 48 h, then scratch wound healing assay was used to detect cell migration ability. (B) Transwell assay was used to detect cell invasion ability (magnification, ×200). Data are presented as the mean ± SD. **P<0.01 vs. control group. lncRNA-ATB, long non-coding RNA-activated by transforming growth factor-β; lncRNA-ATB-NC, long non-coding RNA-activated by transforming growth factor-β-negative control; SKOV3, ovarian cancer cell line.
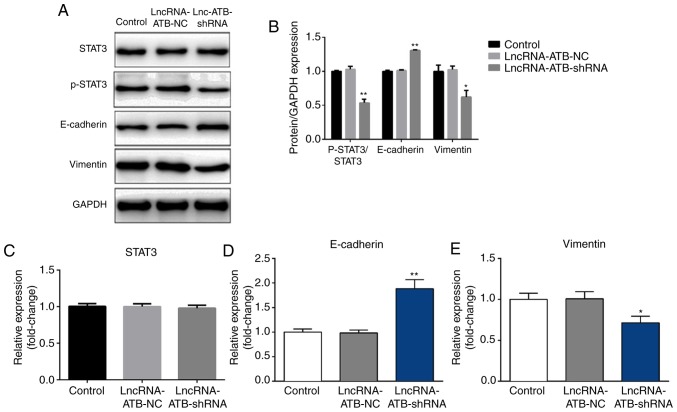
LncRNA-ATB downregulation significantly reduces the phosphorylation of STAT3, increases E-cadherin expression and decreases vimentin expression in SKOV3 cells
The effect of lncRNA-ATB downregulation on ovarian cancer cell epithelial to mesenchymal transition (EMT) was examined through analysis of the expression of EMT-related proteins (E-cadherin and vimentin) in SKOV3 cells. Transfection with lncRNA-ATB-shRNA significantly increased E-cadherin protein and mRNA expression (Fig 4A, B and D), and decreased vimentin protein and mRNA expression (Fig. 4A, B and E).
Figure 4.
Effect of lncRNA-ATB downregulation on the expression of epithelial to mesenchymal transition-related proteins and the STAT3 pathway activity in SKOV3 cells. (A) LncRNA-ATB-NC or lncRNA-ATB-shRNA was transfected into SKOV3 cells for 48 h, then western blotting was used to detect the protein level of p-STAT3, STAT3, E-cadherin and vimentin in SKOV3 cells. (B) Western blotting results were quantified. RT-qPCR was used to detect the mRNA expression of (C) STAT3, (D) E-cadherin and (E) vimentin in SKOV3 cells. Data are presented as the mean ± SD. Each experiment was repeated three times. *P<0.05 and **P<0.01 vs. control group. E-cadherin, epithelial cadherin; lncRNA-ATB, long non-coding RNA-activated by transforming growth factor-β; lncRNA-ATB-NC, long non-coding RNA-activated by transforming growth factor-β-negative control; SKOV3, ovarian cancer cell line; STAT-3, signal transducer and activator of transcription 3; p-STAT-3, phosphorylated signal transducer and activator of transcription 3.
Finally, to explore the molecular mechanisms behind the role of lncRNA-ATB in ovarian cancer, the STAT3 pathway was studied via analysis of the phosphorylation of STAT3 using western blotting. The results suggested that lncRNA-ATB-shRNA significantly inhibited the phosphorylation of STAT3 (Fig. 4A and B), but had no significant effect on STAT3 expression (Fig. 4A and C).
Discussion
Ovarian cancer, the most lethal of all gynecological malignancies, ranks as the fifth leading cause of cancer deaths in women (1,2). The prognosis of ovarian cancer is generally poor due to the lack of clear symptoms and effective screening and diagnostic methods, especially for identifying early stages of the disease. For this reason the identification of better tumor bio-markers to predict the prognosis of ovarian cancer has attracted the attention of oncologists (20–25). Increasing evidence suggests that lncRNAs play vital roles in tumorigenesis and the invasion and metastasis of cancer (26–28). Several studies have evaluated the prognostic value of lncRNA-ATB expression in human cancer (29,30). These previous studies (26–30) indicated that lncRNA-ATB may serve important roles in ovarian cancer. In the present study, lncRNA-ATB was significantly upregulated in ovarian cancer cells compared with healthy ovarian cells, suggesting the possible involvement of lncRNA-ATB in ovarian cancer development. Furthermore, lncRNA-ATB downregulation effectively reduced the proliferative, invasive and migratory capabilities of ovarian cancer cells and significantly increased apoptosis. These data indicate that lncRNA-ATB may promote cell proliferation, invasion and migration, and inhibit cell apoptosis in ovarian cancer cells.
The discovery of EMT, as a mechanism that allows cancer cells to dedifferentiate and acquire enhanced migratory and invasive properties, has had a significant impact on cancer research (31,32). EMT describes the process whereby epithelial cells undergo multiple biological changes and transform into interstitial tissues with strongly invasive characteristics (33,34). Current research indicates that there are three types of EMT, EMT associated with embryo implantation, EMT associated with tissue fibrosis and remodeling characteristics, and EMT associated with strong carcinogenic effects (35). Tumor cells contribute to the formation of fibrosis through the EMT process and affect the secretion pattern of cytokines to promote tumorigenesis (36). Moreover, in EMT, initially inactive polarized epithelial cells dissolve their own intercellular junctions to form independent, depolarized and active metastatic mesenchymal cells (37,38). For example, the expression and function of E-cadherin linked to epithelial cells can be lost, while N-cadherin, which induces adhesion to mesenchymal cells is induced (39). EMT is an important process for cancer cell migration and metastasis and can be induced by various transcription factors and signal transduction factors (37–39). In the current study, the effect of lncRNA-ATB downregulation on ovarian cancer cell EMT was examined through assessment of the expression of EMT-related proteins (E-cadherin and vimentin) in SKOV3 cells. This study showed that lncRNA-ATB downregulation may inhibit ovarian cancer cell EMT.
STAT3 enhances various signaling pathways involved in the regulation of cell growth, invasion and EMT, and is recognized as a key target for cancer treatment (40–42). The STAT3 signaling pathway plays an important role in ovarian cancer progression (43–45). In order to explore the molecular mechanism behind the role of lncRNA-ATB in ovarian cancer, the STAT3 pathway was analyzed. lncRNA-ATBA downregulation significantly reduced STAT3 activation, indicating that lncRNA-ATB may act on ovarian cancer cells at least partly through influencing the STAT3 signaling pathway activation.
In conclusion, this study demonstrated that lncRNA-ATB was highly expressed in ovarian cancer cells, and that its downregulation effectively inhibited ovarian cancer cell proliferation, invasion, and migration and induced cell apoptosis. These effects might be mediated by the regulation of the STAT3 signaling pathway. Therefore, lncRNA-ATB may be a new therapeutic target for the treatment of ovarian cancer. However, this study only includes a preliminary analysis. To clarify the role of lncRNA-ATB in ovarian cancer, further research is needed. The role of lncRNA-ATB in other ovarian cancer cell lines and in ovarian cancer in vivo should be studied. These issues will be addressed in future studies.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data sets used and/or generated during the current study are available from the corresponding author on reasonable request.
Authors' contributions
DY and XZ contributed to study design, data collection, statistical analysis, data interpretation and manuscript preparation. YZ, HQ, HW, CH, XL, TG and ML contributed to data collection and statistical analysis. HY and JY contributed to study design, data interpretation and manuscript preparation.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Webb PM, Jordan SJ. Epidemiology of epithelial ovarian cancer. Best Pract Res Clin Obstet Gynaecol. 2017;41:3–14. doi: 10.1016/j.bpobgyn.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Reid BM, Permuth JB, Sellers TA. Epidemiology of ovarian cancer: A review. Cancer Biol Med. 2017;14:9–32. doi: 10.20892/j.issn.2095-3941.2016.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pierredon S, Ribaux P, Tille JC, Petignat P, Cohen M. Comparative secretome of ovarian serous carcinoma: Gelsolin in the spotlight. Oncol Lett. 2017;13:4965–4973. doi: 10.3892/ol.2017.6096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Howlader N, Noone A, Krapcho M, Neyman N, Aminou R, Waldron W, Altekruse SF, Kosary CL, Ruhl J, Tatalovich Z, et al. SEER Cancer Statistics Review, 1975–2008, National Cancer Institute [Google Scholar]
- 5.Grunewald T, Ledermann JA. Targeted Therapies for Ovarian Cancer. Best Pract Res Clin Obstet Gynaecol. 2017;41:139–152. doi: 10.1016/j.bpobgyn.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 6.Kim JY, Cho CH, Song HS. Targeted therapy of ovarian cancer including immune check point inhibitor. Korean J Intern Med. 2017;32:798–804. doi: 10.3904/kjim.2017.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brasseur K, Gévry N, Asselin E. Chemoresistance and targeted therapies in ovarian and endometrial cancers. Oncotarget. 2017;8:4008–4042. doi: 10.18632/oncotarget.14021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lintner NG, Cate J. Regulating the ribosome: A spotlight on RNA dark matter. Mol Cell. 2014;54:1–2. doi: 10.1016/j.molcel.2014.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ponting CP, Oliver PL, Rei W. Evolution and functions of long noncoding RNAs. Cell. 2009;136:629–641. doi: 10.1016/j.cell.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Cesana M, Cacchiarelli D, Legnini I, Santini T, Sthandier O, Chinappi M, Tramontano A, Bozzoni I. A long noncoding RNA controls muscle differentiation by functioning as a competing endogenous RNA. Cell. 2011;147:358–369. doi: 10.1016/j.cell.2011.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kitagawa M, Kitagawa K, Kotake Y, Niida H, Ohhata T. Cell cycle regulation by long non-coding RNAs. Cell Mol Life Sci. 2013;70:4785–4794. doi: 10.1007/s00018-013-1423-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang XM, Yang GL, Le XH, et al. Expression profiles of long non-coding RNA in HCC patients suffering hepatitis B liver cirrhosis. J Zhengzhou Univ (Med Sci) 2015;50:194–198. [Google Scholar]
- 13.Yu T, Zhao Y, Hu Z, Li J, Chu D, Zhang J, Li Z, Chen B, Zhang X, Pan H, et al. MetaLnc9 facilitates lung cancer metastasis via a PGK1-activated AKT/mTOR pathway. Cancer Res. 2017;77:5782–5794. doi: 10.1158/0008-5472.CAN-17-0671. [DOI] [PubMed] [Google Scholar]
- 14.Su W, Xu M, Chen X, Chen N, Gong J, Nie L, Li L, Li X, Zhang M, Zhou Q. Long noncoding RNA ZEB1-AS1 epigenetically regulates the expressions of ZEB1 and downstream molecules in prostate cancer. Mol Cancer. 2017;16:142. doi: 10.1186/s12943-017-0711-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dey BK, Mueller AC, Dutta A. Long non-coding RNAs as emerging regulators of differentiation, development, and disease. Transcription. 2014;5:e944014. doi: 10.4161/21541272.2014.944014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iguchi T, Uchi R, Nambara S, Saito T, Komatsu H, Hirata H, Ueda M, Sakimura S, Takano Y, Kurashige J, et al. A long noncoding RNA, lncRNA-ATB, is involved in the progression and prognosis of colorectal cancer. Anticancer Res. 2015;35:1385–1388. [PubMed] [Google Scholar]
- 17.Fu N, Zhao SX, Kong LB, Du JH, Ren WG, Han F, Zhang QS, Li WC, Cui P, Wang RQ, et al. LncRNA-ATB/microRNA-200a/β-catenin regulatory axis involved in the progression of HCV-related hepatic fibrosis. Gene. 2017;618:1–7. doi: 10.1016/j.gene.2017.07.072. [DOI] [PubMed] [Google Scholar]
- 18.Ke L, Xu SB, Wang J, Jiang XL, Xu MQ. High expression of long non-coding RNA ATB indicates a poor prognosis and regulates cell proliferation and metastasis in non-small cell lung cancer. Clin Transl Oncol. 2017;19:599–605. doi: 10.1007/s12094-016-1572-3. [DOI] [PubMed] [Google Scholar]
- 19.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 20.Chen S, Zhang L, Yan G, Cheng S, Fathy AH, Yan N, Zhao Y. Neutrophil-to-lymphocyte ratio is a potential prognostic biomarker in patients with ovarian cancer: A Meta-analysis. Biomed Res Int. 2014;2017:7943467. doi: 10.1155/2017/7943467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang J, Zhao Y, Qi R, Zhu X, Huang C, Cheng S, Wang S, Qi X. Prognostic role of podocalyxin-like protein expression in various cancers: A systematic review and meta-analysis. Oncotarget. 2017;8:52457–52464. doi: 10.18632/oncotarget.14199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou Y, Cheng S, Chen S, Zhao Y. Prognostic and clinicopathological value of SIRT3 expression in various cancers: A systematic review and meta-analysis. OncoTargets Ther. 2018;11:2157–2167. doi: 10.2147/OTT.S157836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhou Y, Cheng S, Fathy AH, Qian H, Zhao Y. Prognostic value of platelet-tolymphocyte ratio in pancreatic cancer: A comprehensive meta-analysis of 17 cohort studies. OncoTargets Ther. 2018;11:1899–1908. doi: 10.2147/OTT.S154162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhao Y, Si G, Zhu F, Hui J, Cai S, Huang C, Cheng S, Fathy AH, Xiang Y, Li J. Prognostic role of platelet to lymphocyte ratio in hepatocellular carcinoma: A systematic review and meta-analysis. Oncotarget. 2017;8:22854–22862. doi: 10.18632/oncotarget.22557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Song X, Yao H, Liu J, Wang Q. The prognostic value of long noncoding RNA Sox2ot expression in various cancers: A systematic review and meta-analysis. Clin Chim Acta. 2018;484:52–59. doi: 10.1016/j.cca.2018.05.038. [DOI] [PubMed] [Google Scholar]
- 26.Hu Y, Chen HY, Yu CY, Xu J, Wang JL, Qian J, Zhang X, Fang JY. A long non-coding RNA signature to improve prognosis prediction of colorectal cancer. Oncotarget. 2014;5:2230–2242. doi: 10.18632/oncotarget.1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beckedorff FC, Amaral MS, Deocesano-Pereira C, Verjovski-Almeida S. Long non-coding RNAs and their implications in cancer epigenetics. Biosci Rep. 2013;33(pii):e00061. doi: 10.1042/BSR20130054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gutschner T, Diederichs S. The hallmarks of cancer: A long non-coding RNA point of view. RNA Biol. 2012;9:703–719. doi: 10.4161/rna.20481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen Y, Wei G, Xia H, Tang Q, Bi F. Long noncoding RNAATB promotes cell proliferation, migration and invasion in gastric cancer. Mol Med Rep. 2018;17:1940–1946. doi: 10.3892/mmr.2017.8077. [DOI] [PubMed] [Google Scholar]
- 30.Fu XM, Guo W, Li N, Liu HZ, Liu J, Qiu SQ, Zhang Q, Wang LC, Li F, Li CL. The expression and function of long noncoding RNA lncRNA-ATB in papillary thyroid cancer. Eur Rev Med Pharmacol Sci. 2017;21:3239–3246. [PubMed] [Google Scholar]
- 31.Karlsson MC, Gonzalez SF, Welin J, Fuxe J. Epithelial-mesenchymal transition in cancer metastasis through the lymphatic system. Mol Oncol. 2017;11:781–791. doi: 10.1002/1878-0261.12092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liao TT, Yang MH. Revisiting epithelial-mesenchymal transition in cancer metastasis: The connection between epithelial plasticity and stemness. Mol Oncol. 2017;11:792–804. doi: 10.1002/1878-0261.12096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davis FM, Azimi I, Faville RA, Peters AA, Jalink K, Putney JW, Jr, Goodhill GJ, Thompson EW, Roberts-Thomson SJ, Monteith GR, et al. Induction of epithelial-mesenchymal transition (EMT) in breast cancer cells is calcium signal dependent. Oncogene. 2014;33:2307–2316. doi: 10.1038/onc.2013.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoshida T, Ozawa Y, Kimura T, Sato Y, Kuznetsov G, Xu S, Uesugi M, Agoulnik S, Taylor N, Funahashi Y, Matsui J. Eribulin mesilate suppresses experimental metastasis of breast cancer cells by reversing phenotype from epithelial-mesenchymal transition (EMT) to mesenchymal-epithelial transition (MET) states. Br J Cancer. 2014;110:1497–1505. doi: 10.1038/bjc.2014.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Qu C, Zhang W, Zheng G, Zhang Z, Yin J, He Z. Metformin reverses multidrug resistance and epithelial-mesenchymal transition (EMT) via activating AMP-activated protein kinase (AMPK) in human breast cancer cells. Mol Cell Biochem. 2014;386:63–71. doi: 10.1007/s11010-013-1845-x. [DOI] [PubMed] [Google Scholar]
- 36.Vetuschi A, Pompili S, Flati V, Berardinis LD, Di Gregorio J, Latella G, Sferra R. Epithelial-to-Mesenchimal Transition (EMT) in experimental intestinal fibrosis. Italian J Anatomy Embryology. 2015;120:58. [Google Scholar]
- 37.Yang Y, Gao M, Lin Z, Chen L, Jin Y, Zhu G, Wang Y, Jin T. DEK promoted EMT and angiogenesis through regulating PI3K/AKT/mTOR pathway in triple-negative breast cancer. Oncotarget. 2017;8:98708–98722. doi: 10.18632/oncotarget.21864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ma Z, Xin Z, Hu W, Jiang S, Yang Z, Yan X, Li X, Yang Y, Chen F. Forkhead box O proteins: Crucial regulators of cancer EMT. Semin Cancer Biol. 2018;50:21–31. doi: 10.1016/j.semcancer.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 39.Zuo L, Zhao H, Yang R, Wang L, Ma H, Xu X, Zhou P, Kong L. Lamin A/C might be involved in the EMT signalling pathway. Gene. 2018;663:51–64. doi: 10.1016/j.gene.2018.04.040. [DOI] [PubMed] [Google Scholar]
- 40.Zhao J, Du P, Cui P, Qin Y, Hu C, Wu J, Zhou Z, Zhang W, Qin L, Huang G. LncRNA PVT1 promotes angiogenesis via activating the STAT3/VEGFA axis in gastric cancer. Oncogene. 2018;37:4094–4109. doi: 10.1038/s41388-018-0250-z. [DOI] [PubMed] [Google Scholar]
- 41.Egusquiaguirre SP, Yeh JE, Walker SR, Liu S, Frank DA. The STAT3 Target Gene TNFRSF1A Modulates the NF-κB Pathway in Breast Cancer Cells. Neoplasia. 2018;20:489–498. doi: 10.1016/j.neo.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bournazou E, Bromberg J. Targeting the tumor microenvironment: JAK-STAT3 signaling. JAKSTAT. 2013;2:e23828. doi: 10.4161/jkst.23828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen L, Wang J, Wu J, Zheng Q, Hu J. Indirubin suppresses ovarian cancer cell viabilities through the STAT3 signaling pathway. Drug Des Devel Ther. 2018;12:3335–3342. doi: 10.2147/DDDT.S174613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jia ZH, Jia Y, Guo FJ, Chen J, Zhang XW, Cui MH. Phosphorylation of STAT3 at Tyr705 regulates MMP-9 production in epithelial ovarian cancer. PLoS One. 2017;12:e0183622. doi: 10.1371/journal.pone.0183622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saini U, Naidu S, ElNaggar AC, Bid HK, Wallbillich JJ, Bixel K, Bolyard C, Suarez AA, Kaur B, Kuppusamy P, et al. Elevated STAT3 expression in ovarian cancer ascites promotes invasion and metastasis: A potential therapeutic target. Oncogene. 2017;36:168–181. doi: 10.1038/onc.2016.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data sets used and/or generated during the current study are available from the corresponding author on reasonable request.