Abstract
Purpose
We aimed to investigate the disease phenotype of Korean pediatric Crohn's disease (CD) patients at diagnosis according to the Paris classification by comparison with patients from the European multicenter 5-years recruitment of children with newly developed IBD (EUROKIDS registry).
Methods
Korean children and adolescents who had been newly diagnosed with CD at the age of <18 years during 2013–2016 were included in this multicenter retrospective study. Disease phenotype at diagnosis was classified according to the Paris classification, and compared with the published data from the EUROKIDS study.
Results
A total of 255 patients were included. The median diagnosis age was 14.7 years (range, 0.8–17.9 years). No significant difference was observed in male-to-female ratio with EUROKIDS (1.9:1 vs. 1.45:1, p=0.062). The proportion of children aged <10 years was significantly lower in Koreans (7.1% vs. 19.6%, p<0.001). Colonic disease was less prominent (10.0% vs. 27.3%, p<0.001), while upper GI involvement was more prominent in Korean children (59.3% vs. 46.2%, p<0.001). The proportion with perianal fistulizing disease at diagnosis was significantly higher in Korean patients (44.8% vs. 8.2%, p<0.001). A separate analysis of Korean patients revealed that perianal fistulizing disease at diagnosis was positively associated with male sex and body mass index z-score (odds ratio [OR]=2.12, 95% confidence interval [CI]=1.20–3.76, p=0.010; and OR=1.29, 95% CI=1.05–1.58, p=0.015, respectively).
Conclusion
Approximately half of pediatric CD patients in Korea present with perianal fistulas and/or abscesses at diagnosis, which is a distinct feature of CD in Korean children and adolescents compared to their European counterparts. An underlying genetic difference between ethnicities may play a role in this expression of different phenotypes in pediatric CD.
Keywords: Crohn disease, Fistula, Abscess, Paris, Classification, Phenotype, Korea, Europe, Pediatrics, Inflammatory bowel disease
INTRODUCTION
Crohn's disease (CD) is an inflammatory bowel disease (IBD) that can involve any area in the gastrointestinal (GI) tract from the mouth to the anus [1]. Approximately 25% of patients with CD are known to present before 20 years of age [2]. Moreover, the incidence and prevalence of pediatric CD is increasing worldwide and the age of CD diagnosis is also getting younger [3,4,5]. Meanwhile, CD is well-known as a contemporary condition of industrialized societies, and newly industrialized countries in Asia are experiencing a rapid increase in incidence [6]. Korea is also experiencing this increase in CD incidence, especially in the age group of 15–19 years [7,8].
Despite this increase, there are limited large-scale multicenter studies that have assessed the phenotype of pediatric CD in Korea according to the Paris classification based on a full evaluation of the entire GI tract. A recent multicenter study in Korea has compared the characteristics of pediatric CD with the European multicenter 5-years recruitment of children with newly developed IBD (EUROKIDS registry) [9,10]. However, only a small number of Korean patients were included in that study [9]. Moreover, disease phenotype was based on the Montreal classification, and results imply that evaluation of the upper GI (UGI) tract seems to have been insufficient in the Korean children. Considering these limitations, it is unlikely that an adequate comparison was performed with their European counterparts in that study [9]. Therefore, the aim of this study was to investigate the disease phenotype and characteristics of Korean pediatric CD patients at diagnosis by comparison with data from the EUROKIDS registry, according to the Paris classification based on a complete workup of the entire GI tract.
MATERIALS AND METHODS
Patients and study design
This study was a multicenter retrospective study conducted at the Department of Pediatrics of 10 centers in Korea; Kyungpook National University Children's Hospital, Samsung Medical Center, Severence Children's Hospital, Soonchunhyang University Bucheon Hospital, Korea University Ansan Hospital, Korea University Anam Hospital, Chungbuk National University Hospital, Samsung Changwon Hospital, Keimyung University Hospital, and Inje University Ilsan Paik Hospital. Patients included were children and adolescents who had been newly diagnosed with CD at the age of <18 years between 2013 and 2016. Patients diagnosed as ulcerative colitis (UC) or inflammatory bowel disease-unspecified (IBD-U), diagnosis age ≥18 years, and those with missing data on baseline clinicodemographics were excluded. CD was diagnosed in accordance with the revised Porto criteria of the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition [11].
Baseline clinicodemographics including sex, diagnosis age, ethnicity, first degree family history of IBD, previous surgical history before diagnosis, growth indicators were investigated in all the patients with available data. Regarding disease location and behavior, only the patients who had conducted a complete diagnostic workup of the entire GI tract according to the revised Porto criteria were included [11]. Like the inclusion criteria from the EUROKIDS study, those who had undergone UGI endoscopy, ileocolonoscopy, and adequate imaging of the small bowel by small bowel follow-through (SBFT), magnetic resonance imaging or magnetic resonance enterography (MRE), computed tomography (CT) or computed tomographic enterography (CTE), capsule endoscopy, and/or enteroscopy were considered to have conducted a complete diagnostic workup [10].
Growth indicators including z-scores for weight-for-age, height-for-age, and body mass index (BMI)-for-age were calculated using the 2017 Korean National Growth Charts for children and adolescents of the Korean Centers for Disease Control and Prevention [12].
Classification and definitions
Disease phenotype at diagnosis was classified according to the Paris classification [13], and compared with the published data from the EUROKIDS registry [10]. Disease involvement was defined as the presence of ulcers, erosions, cobblestones, and/or stenosis from the esophagus to the 2nd portion of the duodenum on UGI endoscopy, and from the terminal ileum (TI) to the rectum on ileocolonoscopy. For the remaining small bowel, disease involvement was based on findings on small bowel imaging, capsule endoscopy, and/or enteroscopy. Perianal fistulizing disease was confined to perianal fistulas and/or abscesses.
Statistical analysis
For statistical comparison between groups, a chi square test or Fisher's exact test was used for categorical variables, and a Student's t-test or Wilcoxon rank sum test was used for continuous variables. Comparative data for continuous variables are reported as median (interquartile range) or mean (standard deviation). Logistic regression analyses were performed to examine the association between variables. Univariate logistic regression analysis was first conducted to investigate the crucial odds ratio (OR) for each factor. A multivariate logistic regression analysis was then conducted using a stepwise selection procedure with a 5% significance level for a covariate to enter or remain in the model. The results were expressed as adjusted ORs with 95% confidence intervals (CIs). Data were considered to be statistically significantly different if p<0.05. Statistical analyses were carried out using R version 3.2.3 (R Development Core Team, 2015; http://www.r-project.org).
Ethical statement
This study was approved by the Institutional Review Board (IRB) of Kyungpook National University Chilgok Hospital and all other participating centers, and informed consent was waived due to the retrospective nature of this study (IRB Number 2017-06-022).
RESULTS
Baseline clinicodemographics
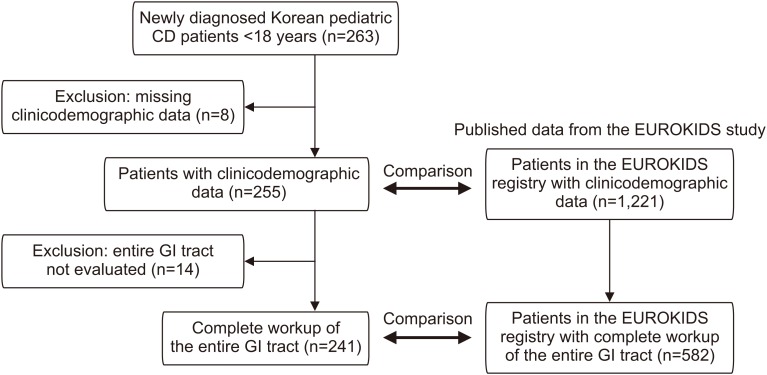
A total of 263 Korean patients had been newly diagnosed with CD at the age of <18 years between 2013 and 2016. Among them, 255 patients with available clinicodemographic data were included (Fig. 1). One-hundred sixty-seven patients (65.5%) were male, and the median age at diagnosis was 14.7 years (range, 0.8–17.9 years).
Fig. 1. Flow diagram of the study. CD: Crohn's disease, GI: gastrointestinal.
Comparison with EUROKIDS revealed that male predominance was more prominent in Koreans, although statistical significance was not observed (65.5% vs. 59.2%, p=0.062). Median age at diagnosis was also higher in Koreans than EUROKIDS (14.7 vs. 12.5 years). Other clinicodemographics and comparison with EUROKIDS are shown in Table 1.
Table 1. Baseline clinicodemographics of pediatric Crohn's disease patients in Korea and EUROKIDS at diagnosis.
| Clinicodemographics | Korea (n=255) | EUROKIDS (n=1,221) | p-value | |
|---|---|---|---|---|
| Sex | 0.062 | |||
| Male | 167 (65.5) | 723 (59.2) | ||
| Female | 88 (34.5) | 498 (41.8) | ||
| Male-to-female ratio | 1.9:1 | 1.45:1 | ||
| Age at diagnosis (yr) | 14.7 (0.8–17.9) | 12.5 (0.8–17.9) | ||
| Ethnicity | <0.001 | |||
| Asian | 255 (100.0) | 50/1,210 (4.1) | ||
| Caucasian | 0 | 1,049/1,210 (86.7) | ||
| Arab | 0 | 43/1,210 (3.6) | ||
| Africa-Caribbean | 0 | 18/1,210 (1.5) | ||
| Others | 0 | 50/1,210 (4.1) | ||
| 1st degree family history of IBD | 12 (4.7) | 129/1,193 (10.8) | 0.003 | |
| Previous bowel resection history | 4 (1.6) | N/A | ||
| Previous perianal surgery history | 61 (23.9) | N/A | ||
| Height z-score | −0.3 (−1.0–0.4) | N/A | ||
| Weight z-score | −0.9 (−1.8–−0.1) | N/A | ||
| BMI z-score | −1.1 (−1.9–−0.1) | N/A | ||
Values are presented as number (%), number only, or median (interquartile range), except for age at diagnosis which is presented as median (range).
IBD: inflammatory bowel disease, BMI: body mass index, N/A: not available.
Among the 255 Korean patients included in the study, complete workup of the entire GI tract was conducted in 241 patients (Fig. 1). Comparison of age according to the Paris classification revealed that the proportion of A1a patients (<10 years) was significantly lower in Korean children compared to EUROKIDS (7.1% vs. 19.6%, p<0.001) (Table 2).
Table 2. Comparison of pediatric Crohn's disease phenotype at diagnosis between Korea and EUROKIDS according to the Paris classification.
| Paris classification | Korea (n=241) | EUROKIDS (n=582) | p-value | |
|---|---|---|---|---|
| Diagnosis age | <0.001 | |||
| A1a | 17 (7.1) | 114 (19.6) | ||
| A1b/A2 | 224 (92.9) | 468 (80.4) | ||
| LGI tract location | <0.001 | |||
| No involvement | 2 (0.8) | 21 (3.6) | ||
| L1 | 36 (14.9) | 95 (16.3) | ||
| L2 | 24 (10.0) | 159 (27.3) | ||
| L3 | 179 (74.3) | 307 (52.8) | ||
| UGI tract location | 0.005 | |||
| No involvement | 98 (40.7) | 313 (53.8) | ||
| L4a | 61 (25.2) | 129 (22.1) | ||
| L4b | 55 (22.8) | 97 (16.7) | ||
| L4ab | 27 (11.2) | 43 (7.4) | ||
| Luminal disease behavior | 0.206 | |||
| B1 | 208 (86.3) | 477 (82.0) | ||
| B2 | 27 (11.2) | 77 (13.2) | ||
| B3/B2B3 | 6 (2.4) | 28 (4.8) | ||
| Perianal fistulizing disease | 108 (44.8) | 48 (8.2) | <0.001 | |
Values are presented as number (%).
A1a: 0–9 years, A1b: 10–16 years, A2: ≥17 years, LGI: lower gastrointestinal, UGI: upper gastrointestinal, L1: distal 1/3 ileum±limited cecal disease, L2: colonic disease, L3: ileocolonic disease, L4a: upper disease proximal to the ligament of Treitz, L4b: upper disease distal to the ligament of Treitz and proximal to the distal 1/3 ileum, L4ab: upper disease involvement in both L4a and L4b, B1: nonstricturing nonpenetrating behavior, B2: stricturing behavior, B3: penetrating behavior, B2B3: both B2 and B3.
Disease involvement across the entire GI tract
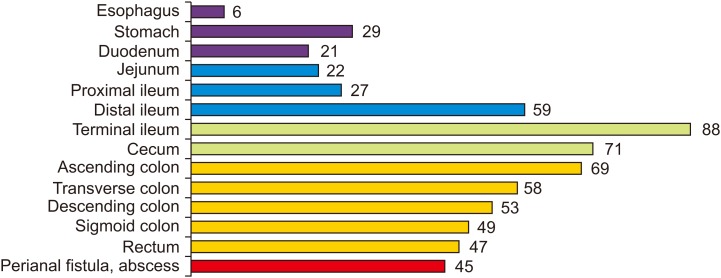
The most common location of CD involvement in Korean patients across the entire GI tract was the TI constituting 88% among the 241 patients who had completed a full workup. The proportion of patients with affected segments along the lower GI (LGI) tract showed a gradual decrease moving distally from the TI (88%) to the rectum (47%) (Fig. 2). The proportion of patients with affected segments along the UGI tract also showed a gradual decrease moving proximally from the distal ileum (59%) to the esophagus (6%), except for the stomach (29%) (Fig. 2).
Fig. 2. Proportion of disease involvement across the entire gastrointestinal tract and perianal region.
Disease phenotype according to the Paris classification
The most common disease phenotype in Korean patients according to the Paris classification was A1b, L3+L4a, B1p which constituted 12.0% (29/241) of the patients, followed by A1b, L3, B1 of 10.4% (25/241) (Table 3).
Table 3. Composition of Korean pediatric Crohn's disease phenotype at diagnosis according to the Paris classification.
| Location and behavior | Total (p) | Age | ||||
|---|---|---|---|---|---|---|
| LGI | UGI | B | A1a (p) | A1b (p) | A2 (p) | |
| L4b | B1 | 2 (0) | 2 (0) | |||
| L1 | B1 | 12 (6) | 8 (4) | 4 (2) | ||
| L1 | L4a | B1 | 5 (1) | 5 (1) | ||
| L1 | L4b | B1 | 8 (2) | 7 (2) | 1 (0) | |
| L1 | B2 | 2 (1) | 2 (1) | |||
| L1 | L4b | B2 | 4 (2) | 2 (0) | 2 (2) | |
| L1 | L4ab | B2 | 1 (0) | 1 (0) | ||
| L1 | B2B3 | 1 (0) | 1 (0) | |||
| L1 | L4b | B3 | 1 (0) | 1 (0) | ||
| L2 | B1 | 14 (6) | 4 (2) | 9 (4) | 1 (0) | |
| L2 | L4a | B1 | 6 (2) | 1 (0) | 3 (1) | 2 (1) |
| L2 | L4b | B1 | 1 (1) | 1 (1) | ||
| L2 | L4ab | B1 | 2 (0) | 2 (0) | ||
| L2 | B2 | 1 (1) | 1 (1) | |||
| L2 | L4b | B2 | 1 (1) | 1 (1) | ||
| L3 | B1 | 60 (25) | 8 (4) | 41 (16) | 11 (5) | |
| L3 | L4a | B1 | 47 (30) | 43 (29) | 4 (1) | |
| L3 | L4b | B1 | 29 (9) | 26 (8) | 3 (1) | |
| L3 | L4ab | B1 | 21 (11) | 2 (1) | 19 (10) | |
| L3 | B2 | 6 (2) | 4 (0) | 2 (2) | ||
| L3 | L4a | B2 | 4 (2) | 4 (2) | ||
| L3 | L4ab | B2 | 1 (1) | 1 (1) | ||
| L3 | L4b | B2 | 7 (3) | 6 (2) | 1 (1) | |
| L3 | B2B3 | 1 (0) | 1 (0) | |||
| L3 | L4ab | B2B3 | 1 (1) | 1 (1) | ||
| L3 | B3 | 1 (1) | 1 (1) | |||
| L3 | L4ab | B3 | 1 (1) | 1 (1) | ||
| Total | 241 (108) | 17 (7) | 192 (86) | 32 (15) | ||
LGI: lower gastrointestinal, UGI: upper gastrointestinal, B: behavior, p: perianal fistulizing disease, A1a: 0–9 years, A1b: 10–16 years, A2: ≥17 years, L1: distal 1/3 ileum±limited cecal disease, L2: colonic disease, L3: ileocolonic disease, L4a: upper disease proximal to the ligament of Treitz, L4b: upper disease distal to the ligament of Treitz and proximal to the distal 1/3 ileum, L4ab: upper disease involvement in both L4a and L4b, B1: nonstricturing nonpenetrating behavior, B2: stricturing behavior, B3: penetrating behavior, B2B3: both B2 and B3.
Comparison of LGI tract disease location according to the Paris classification showed that the proportion of patients with L2 disease was less prominent (10.0% vs. 27.3%, p<0.001) and L3 disease was more prominent in Korean children compared to EUROKIDS (74.3% vs. 52.8%, p<0.001) (Table 2). Among Korean children, isolated colonic (L2) disease was observed in 41.2% (7/17) of patients aged <10 years and 8.0% (18/224) of patients aged ≥10 years, respectively (p<0.001).
Comparison of UGI tract disease location according to the Paris classification showed that any L4 involvement was higher in Korean children compared to EUROKIDS (59.3% vs. 46.2%, p<0.001). A total 262 exams for small bowel evaluation were conducted in 241 patients. The modalities used for small bowel evaluation in Korean children were MRE in 175 patients (72.6%), CTE in 67 patients (27.8%), capsule endoscopy in 15 patients (6.2%), CT in 7 patients (2.9%), and SBFT in 5 patients (2.1%). Among Korean children, any L4 involvement was observed in 29.4% (5/17) of patients aged <10 years and 61.2% (137/224) of patients aged ≥10 years, respectively (p=0.019).
Comparison of luminal disease behavior according to the Paris classification demonstrated that there was no significant difference between Korean children and EUROKIDS (Table 2). However, perianal fistulizing disease at diagnosis was more prominent in Korean children compared to EUROKIDS (44.8% vs. 8.2%, p<0.001).
Factors associated with diagnosis age
Comparison between Korean patients aged <10 years and ≥10 years showed that patients aged <10 years had a lower height z-score at diagnosis (−0.9±1.1 vs. −0.3±1.1, p=0.029), a lower proportion of patients with any TI involvement (58.8% vs. 91.5%, p<0.001), and a lower proportion of patients with any L4 involvement (29.4% vs. 61.6%, p=0.019).
According to multivariate logistic regression analysis, any TI involvement (OR=0.15, 95% CI=0.05–0.46; p<0.001) was the only factor significantly associated with diagnosis age <10 years (Table 4).
Table 4. Factors associated with age <10 years at diagnosis in Korean patients.
| Factors | Univariate logistic regression | Multivariate logistic regression | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Sex (male vs. female) | 0.76 | 0.28–2.08 | 0.598 | |||
| 1st degree family history of IBD (yes vs. no) | 3.19 | 0.63–16.08 | 0.161 | |||
| Previous perianal surgery history | 0.64 | 0.18–2.32 | 0.500 | |||
| Height z-score | 0.61 | 0.39–0.96 | 0.031 | 0.70 | 0.43–1.14 | 0.147 |
| Weight z-score | 0.75 | 0.52–1.08 | 0.124 | |||
| BMI z-score | 0.76 | 0.50–1.15 | 0.193 | |||
| Any TI involvement (yes vs. no) | 0.13 | 0.05–0.39 | <0.001 | 0.15 | 0.05–0.46 | <0.001 |
| Any L4 involvement (yes vs. no) | 0.26 | 0.09–0.76 | 0.014 | 0.33 | 0.11–1.04 | 0.058 |
| Perianal fistulizing disease (yes vs. no) | 0.85 | 0.31–2.32 | 0.755 | |||
OR: odds ratio, CI: confidence interval, IBD: inflammatory bowel disease, BMI: body mass index, TI: terminal ileum, L4: upper disease involvement.
Factors associated with perianal fistulizing disease at diagnosis
Comparison between Korean patients with and without any perianal fistulizing disease showed that patients with perianal fistulizing disease had a higher proportion of patients with male sex (73.1% vs. 57.9%, p=0.020), a higher weight z-score (−0.7±1.3 vs. −1.1±1.3, p=0.036) and higher BMI z-score (median −0.7 vs. −1.2, p=0.009), and a higher proportion of patients with any L4a involvement [44.4% (48/108) vs. 30.1% (40/133), p=0.03] (Table 5).
Table 5. Comparison between Korean patients with and without perianal fistulizing disease at diagnosis.
| Variable | Perianal fistulizing disease | p-value | ||
|---|---|---|---|---|
| Present (n=108) | Absent (n=133) | |||
| Male | 79 (73.1) | 77 (57.9) | 0.020 | |
| Age at diagnosis (yr) | 14.6 (12.2–15.9) | 12.5 (13.0–16.2) | 0.586 | |
| 1st degree family history of IBD | 2 (1.9) | 9 (6.8) | 0.132 | |
| Previous bowel resection history | 1 (0.9) | 3 (2.3) | 0.767 | |
| Height z-score | −0.3±1.0 | −0.4±1.2 | 0.503 | |
| Weight z-score | −0.7±1.3 | −1.1±1.3 | 0.036 | |
| BMI z-score | −0.7 (−1.6–0.0) | −1.2 (−2.1–−0.3) | 0.009 | |
| LGI tract location | 0.222 | |||
| No involvement | 0 (0.0) | 2 (1.5) | ||
| L1 | 12 (11.1) | 24 (18.0) | ||
| L2 | 10 (9.3) | 14 (10.5) | ||
| L3 | 86 (79.6) | 93 (69.9) | ||
| UGI tract location | 0.076 | |||
| No involvement | 42 (38.9) | 56 (42.1) | ||
| L4a | 34 (31.5) | 27 (20.3) | ||
| L4b | 18 (16.7) | 37 (27.8) | ||
| L4ab | 14 (13.0) | 13 (9.8) | ||
| Luminal disease behavior | 0.828 | |||
| B1 | 92 (85.2) | 116 (87.2) | ||
| B2 | 13 (12.0) | 14 (10.5) | ||
| B3/B2B3 | 3 (2.8) | 3 (2.3) | ||
Values are presented as number (%), median (interquartile range), or mean±standard deviation.
IBD: inflammatory bowel disease, BMI: body mass index, LGI: lower gastrointestinal, UGI: upper gastrointestinal, L1: distal 1/3 ileum±limited cecal disease, L2: colonic disease, L3: ileocolonic disease, L4a: upper disease proximal to the ligament of Treitz, L4b: upper disease distal to the ligament of Treitz and proximal to the distal 1/3 ileum, L4ab: upper disease involvement in both L4a and L4b, B1: nonstricturing nonpenetrating behavior, B2: stricturing behavior, B3: penetrating behavior, B2B3: both B2 and B3.
According to multivariate logistic regression analysis, male sex (OR=2.12, 95% CI=1.20–3.76; p=0.010) and BMI z-score (OR=1.29, 95% CI=1.05–1.58; p=0.015) were significantly associated with the presence of perianal fistulizing disease at diagnosis (Table 6).
Table 6. Factors associated with perianal fistulizing disease at diagnosis in Korean patients.
| Factors | Univariate logistic regression | Multivariate logistic regression | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Sex (male vs. female) | 1.98 | 1.15–3.42 | 0.014 | 2.12 | 1.20–3.76 | 0.010 |
| Age <10 years (yes vs. no) | 0.85 | 0.31–2.32 | 0.755 | |||
| 1st degree family history of IBD (yes vs. no) | 0.26 | 0.06–1.23 | 0.089 | |||
| Previous bowel resection history (yes vs. no) | 0.41 | 0.04–3.95 | 0.437 | |||
| Height z-score | 1.08 | 0.86–1.37 | 0.501 | |||
| Weight z-score | 1.23 | 1.01–1.49 | 0.038 | |||
| BMI z-score | 1.25 | 1.03–1.52 | 0.022 | 1.29 | 1.05–1.58 | 0.015 |
| Any TI involvement (yes vs. no) | 1.34 | 0.58–3.09 | 0.492 | |||
| Any colon involvement (yes vs. no) | 1.94 | 0.93–4.06 | 0.077 | |||
| Any L4a involvement (yes vs. no) | 1.86 | 1.09–3.16 | 0.022 | 1.68 | 0.96–2.93 | 0.070 |
| Any L4b involvement (yes vs. no) | 0.70 | 0.41–1.20 | 0.195 | |||
| Any B2 or B3 behavior (yes vs. no) | 1.19 | 0.57–2.48 | 0.648 | |||
OR: odds ratio, CI: confidence interval, IBD: inflammatory bowel disease, BMI: body mass index, TI: terminal ileum, L4a: upper disease proximal to the ligament of Treitz, L4b: upper disease distal to the ligament of Treitz and proximal to the distal 1/3 ileum, B2: stricturing, B3: penetrating.
DISCUSSION
This was the first multicenter study in Korea to properly investigate the phenotype of pediatric CD according to the Paris classification based on a complete workup of the entire GI tract. We have revealed significant differences in several aspects of disease phenotype of Korean pediatric CD compared to the EUROKIDS registry, including diagnosis age, LGI tract location, UGI tract location, and the proportion of patients with perianal fistulizing disease. Approximately half (44.8%) of pediatric CD patients in Korea present with perianal fistulas and/or abscesses at diagnosis, which is a distinct feature of CD in Korean children and adolescents compared to their European counterparts.
To date there is insufficient data in Korea regarding the phenotypes of pediatric CD based on the Paris classification. A recent study compared the characteristics of pediatric CD with the EUROKIDS registry [9]. However, due to the small number of Korean patients (n=30), some of the results were unreliable. For example, the male-to-female ratio of Korean pediatric CD patients was 6.5:1, and 36.7% of patients had L1 disease. Moreover, only 1 patient (3.4%) had UGI tract involvement, raising the suspicion of whether a complete workup of the entire GI tract had been properly conducted. Another major limitation of that study was that phenotyping of CD was based on the Montreal classification rather than the Paris classification which is generally used for pediatric IBD [13]. Therefore, it is difficult to accept the results of that study as being representative of Korean children as well as assuming that an adequate comparison was performed with their European counterparts.
Regarding clinicodemographics at diagnosis, the proportion of children aged <10 years (A1a) was significantly lower in Koreans compared with EUROKIDS (7.1% vs. 19.6%, p<0.001). This difference may have been partially due to the difference in the ages of the study population recruited in our study and the EUROKIDS registry. While all the investigators of the participating centers in our study were responsible for the primary examination of new patients aged <18 years, approximately one-third of the participating centers in the EUROKIDS cohort reported that new patients aged >15 years were always referred to an adult gastroenterologist [10]. Meanwhile, a recent study from Israel analyzing data from adolescents who had undergone obligatory medical examination at 17 years to assess their eligibility for military service, revealed a diagnosis age of 14.2±3.2 years among 1,612 patients who had been previously diagnosed with CD [5], which is comparable to the results of our study (median 14.7 years).
Although no statistically significant difference was observed in male-to-female ratio with EUROKIDS, a higher male predominance was observed in Korean children and adolescents (1.9:1 vs. 1.45:1, p=0.062). Male predominance in the pediatric population has been reported in several population-based cohorts from Western countries [14,15,16,17]. Moreover, according to a recently published pooled analysis using population data from established cohorts from Western countries to analyze sex differences in IBD incidence according to diagnosis age, female patients had a lower risk of CD during childhood, until the age range of 10–14 years (incidence rate ratio, 0.70; 95% CI, 0.53–0.93) [18]. Thereafter, female patients had a higher risk, which was statistically significant for the age groups of 25–29 years and >35 years [18]. The authors hypothesized that sex hormones may be implicated in IBD pathogenesis [18]. However, this trend was not observed in a pooled analysis of population-based studies from the Asia-Pacific region [19]. A male predominance of CD that started in adolescence was observed to extend to past middle age of 50 years in the Asia-Pacific region [19]. This similar male predominance was also observed in a recent large scale population-based study from Korea [20]. Therefore, the higher male predominance observed in Korean children and adolescents compared to EUROKIDS in our study may be attributable to this ethnic difference for a certain sex predominance in CD.
Another observed difference was that colonic disease was less prominent in Korean children compared to EUROKIDS (10.0% vs. 27.3%, p<0.001). This seems to have been due to the relatively small proportion of patients aged <10 years. According to the EUROKIDS study, isolated colonic (L2) disease was observed in 41.2% (47/114) of children diagnosed at the age of <10 years compared with 23.8% (111/467) of those diagnosed at the age of ≥10 years (p<0.001) [10]. We also observed this finding when LGI tract location was analyzed according to diagnosis age (L2: 41.2% in A1a vs. 8.0% in A1b/A2, p<0.001). This was further confirmed by multivariate logistic regression analysis, which revealed any TI involvement (or L1 and L3 disease) as the only factor that was associated with diagnosis age <10 years (OR=0.15, 95% CI=0.05–0.46; p<0.001). Isolated colonic disease is well known to occur in younger children compared to older children or adults [2,21]. In a Scottish national cohort, children diagnosed <8 years had more L2 disease (34.0% vs. 17.7%, p=0.009), less L1 disease (39.6% vs. 60.5%, p=0.006) and less L3+L4 disease (18.9% vs. 33.6%, p=0.03) [22]. We also observed that L4 location was less prominent in patients aged <10 years (29.4% vs. 61.2%, p=0.019).
Higher rates of UGI tract involvement in Korean children is another interesting finding in this study (59.3% vs. 46.2%, p<0.001). This difference could be partially explained by the high proportion of patients in the Korean cohort undergoing advanced modalities for small bowel evaluation. Since the EUROKIDS study was conducted between 2004 to 2009, less than half of patients received advanced modalities for evaluating their small bowels [10]. Meanwhile, since the Korean cohort was conducted between 2013 to 2016, almost all the patients had undergone either an MRE, CTE, CT or capsule endoscopy for small bowel evaluation. A recent retrospective study of 594 children with CD conducted at a single center in Korea had analyzed disease phenotype at diagnosis according to the Paris classification [23]. Most of the results of that study are comparable with the results of our study: a male predominance showing a male-to-female ratio of 2.4:1, median age at CD diagnosis of 15 years, 79.3% with L3 involvement, 88.9% with B1 behavior, and 47.1% with perianal fistulizing disease. However, only 25.8% of patients had UGI tract involvement in that study, which was lower than that of our study showing 59.3%. It is unsure whether all the patients in that study had undergone a full evaluation of the entire GI tract, because the authors did not specify which exams were conducted at diagnostic evaluation. Meanwhile, full evaluation of the GI tract at diagnosis is crucial for the proper phenotyping of CD according to the Paris classification. Pediatric CD is generally comprehended as more severe and aggressive compared to adults, and small bowel lesions are known to be associated with structuring complications leading to bowel resection as well as hindering linear growth in children and adolescents [2,10,24,25]. Therefore, precise phenotyping according to the Paris classification at diagnosis may be the first step for correctly stratifying pediatric CD patients that may or may not require early treatment with biologics, in order to hit the target properly and consequently minimize bowel damage and surgery, improve quality of life, and restore linear growth in children and adolescents with CD in the era of treat-to-target [26,27,28,29,30].
The most interesting finding in this study is the significantly higher proportion of Korean patients presenting with perianal fistulizing disease at diagnosis (44.8% vs. 8.2%, p<0.001). Perianal fistulizing disease, namely perianal fistula and/or abscess, is generally well known as a complication of CD and is also a distinct feature that distinguishes CD from UC and IBD-U [31]. A recent systematic review and meta-analysis of population-based cohort studies examining the phenotype and outcome of IBD across ethnic groups have reported that perianal disease is more frequently observed in CD patients of African and/or Asian descent than CD patients of Caucasian and/or Hispanic descent [32]. Perianal fistula and/or abscess have been reported in 42–50% of Korean pediatric CD patients at diagnosis [23,33,34], and even higher in those with moderate-to-severe disease activity requiring treatment with biologics [27,35,36,37]. Meanwhile, reports from Western countries vary from 4-45% at diagnosis [21]. According to a recent study from the ImageKids study group, pediatric patients with perianal fistulizing disease during their disease course were shown to have a distinct phenotypic feature and a predisposition to a greater inflammatory burden, showing significantly worse results on laboratory tests, more extensive disease, and lower weight and height z-scores [38]. However contrary to the findings of that study, Korean patients with perianal fistulizing disease at diagnosis in our study had higher weight and BMI z-scores compared to those without perianal fistulizing disease. Recent data from the ImproveCareNow Network cohort have also shown that perianal CD is more likely to occur earlier in the disease course among Asians aged ≥10 years than in Caucasians [39]. Another study has also reported that pediatric CD patients who develop perianal fistulas and/or abscesses while on therapy for CD have a more severe phenotype and are more likely to require diverting ileostomy or colectomy compared to those who initially present with perianal fistulas and/or abscesses at diagnosis [40]. Therefore, Korean children and adolescents with perianal fistulizing disease may present with a rather milder luminal disease type compared to their Western counterparts with perianal fistulizing disease, probably because it occurs earlier in the disease course of pediatric CD.
There are some limitations of this study. First, our study was a retrospective study including only 10 tertiary centers in Korea, which may have resulted in some selection bias. Second, selection bias may have also been introduced by excluding patients who had not undergone a complete workup according to the Porto criteria for the analyses of disease location and behavior according to the Paris classification, which was also the case for the published EUROKIDS study [10]. However, only 14 out of 255 Korean patients (5.5%) were excluded, as the majority had undergone a complete workup in real-life clinical practice. Third, we were unable to compare data regarding granulomas on histology, due to the variable quality of histology reports among centers. Despite these limitations, owing to the outstanding real-life clinical performance of the pediatric gastroenterologists in our study who were capable of conducting a complete workup of the entire GI tract in most of the children as well as the excellent compliance of patients, we were able to conduct a proper comparison with the data from the EUROKIDS registry.
In conclusion, comparison of pediatric CD patients at diagnosis between our Korean cohort and the EUROKIDS registry according to the Paris classification revealed significant differences in several aspects of disease phenotype of Korean pediatric CD. The most distinct feature of CD in Korean children and adolescents compared to their European counterparts was the significantly higher presence of perianal fistulizing disease at diagnosis. An underlying genetic difference between ethnicities may play a role in the expression of different phenotypes in pediatric CD. Identification of distinct disease phenotypes and their natural disease course may lead to an understanding of different therapeutic windows of opportunity and could enable stratified and effective treatment in a timely manner, which may eventually play a role in modifying the natural disease course of pediatric CD in the era of treat-to-target.
Footnotes
Funding: This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2017R1C1B5076980).
Conflicts of Interest: The authors have no financial conflicts of interest.
References
- 1.Baumgart DC, Sandborn WJ. Inflammatory bowel disease: clinical aspects and established and evolving therapies. Lancet. 2007;369:1641–1657. doi: 10.1016/S0140-6736(07)60751-X. [DOI] [PubMed] [Google Scholar]
- 2.Rosen MJ, Dhawan A, Saeed SA. Inflammatory bowel disease in children and adolescents. JAMA Pediatr. 2015;169:1053–1060. doi: 10.1001/jamapediatrics.2015.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sýkora J, Pomahačová R, Kreslová M, Cvalínová D, Štych P, Schwarz J. Current global trends in the incidence of pediatric-onset inflammatory bowel disease. World J Gastroenterol. 2018;24:2741–2763. doi: 10.3748/wjg.v24.i25.2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ashton JJ, Cullen M, Afzal NA, Coelho T, Batra A, Beattie RM. Is the incidence of paediatric inflammatory bowel disease still increasing? Arch Dis Child. 2018;103:1093–1094. doi: 10.1136/archdischild-2018-315038. [DOI] [PubMed] [Google Scholar]
- 5.Ghersin I, Khteeb N, Katz LH, Daher S, Shamir R, Assa A. Trends in the epidemiology of inflammatory bowel disease among Jewish Israeli adolescents: a population-based study. Aliment Pharmacol Ther. 2019;49:556–563. doi: 10.1111/apt.15160. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan GG, Ng SC. Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology. 2017;152:313–21.e2. doi: 10.1053/j.gastro.2016.10.020. [DOI] [PubMed] [Google Scholar]
- 7.Jung YS, Han M, Kim WH, Park S, Cheon JH. Incidence and clinical outcomes of inflammatory bowel disease in South Korea, 2011-2014: a nationwide population-based study. Dig Dis Sci. 2017;62:2102–2112. doi: 10.1007/s10620-017-4640-9. [DOI] [PubMed] [Google Scholar]
- 8.Hong SJ, Cho SM, Choe BH, Jang HJ, Choi KH, Kang B, et al. Characteristics and incidence trends for pediatric inflammatory bowel disease in Daegu-Kyungpook province in Korea: a multi-center study. J Korean Med Sci. 2018;33:e132. doi: 10.3346/jkms.2018.33.e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee HA, Suk JY, Choi SY, Kim ER, Kim YH, Lee CK, et al. Characteristics of pediatric inflammatory bowel disease in Korea: comparison with EUROKIDS data. Gut Liver. 2015;9:756–760. doi: 10.5009/gnl14338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Bie CI, Paerregaard A, Kolacek S, Ruemmele FM, Koletzko S, Fell JM, et al. EUROKIDS Porto IBD Working Group of ESPGHAN. Disease phenotype at diagnosis in pediatric Crohn's disease: 5-year analyses of the EUROKIDS Registry. Inflamm Bowel Dis. 2013;19:378–385. doi: 10.1002/ibd.23008. [DOI] [PubMed] [Google Scholar]
- 11.Levine A, Koletzko S, Turner D, Escher JC, Cucchiara S, de Ridder L, et al. European Society of Pediatric Gastroenterology, Hepatology, and Nutrition. ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr. 2014;58:795–806. doi: 10.1097/MPG.0000000000000239. [DOI] [PubMed] [Google Scholar]
- 12.Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, et al. Committee for the Development of Growth Standards for Korean Children and Adolescents; Committee for School Health and Public Health Statistics, the Korean Pediatric Society; Division of Health and Nutrition Survey, Korea Centers for Disease Control and Prevention. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018;61:135–149. doi: 10.3345/kjp.2018.61.5.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levine A, Griffiths A, Markowitz J, Wilson DC, Turner D, Russell RK, et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis. 2011;17:1314–1321. doi: 10.1002/ibd.21493. [DOI] [PubMed] [Google Scholar]
- 14.Lophaven SN, Lynge E, Burisch J. The incidence of inflammatory bowel disease in Denmark 1980-2013: a nationwide cohort study. Aliment Pharmacol Ther. 2017;45:961–972. doi: 10.1111/apt.13971. [DOI] [PubMed] [Google Scholar]
- 15.Everhov ÅH, Olén O, Ludvigsson JF. Editorial: importance of definition of inflammatory bowel disease and an increased incidence in children. Aliment Pharmacol Ther. 2017;45:1369–1370. doi: 10.1111/apt.14035. [DOI] [PubMed] [Google Scholar]
- 16.Shivashankar R, Tremaine WJ, Harmsen WS, Loftus EV., Jr Incidence and prevalence of Crohn's disease and ulcerative colitis in Olmsted County, Minnesota from 1970 through 2010. Clin Gastroenterol Hepatol. 2017;15:857–863. doi: 10.1016/j.cgh.2016.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benchimol EI, Manuel DG, Guttmann A, Nguyen GC, Mojaverian N, Quach P, et al. Changing age demographics of inflammatory bowel disease in Ontario, Canada: a population-based cohort study of epidemiology trends. Inflamm Bowel Dis. 2014;20:1761–1769. doi: 10.1097/MIB.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 18.Shah SC, Khalili H, Gower-Rousseau C, Olen O, Benchimol EI, Lynge E, et al. Sex-based differences in incidence of inflammatory bowel diseases-pooled analysis of population-based studies from Western Countries. Gastroenterology. 2018;155:1079–89.e3. doi: 10.1053/j.gastro.2018.06.043. [DOI] [PubMed] [Google Scholar]
- 19.Shah SC, Khalili H, Chen CY, Ahn HS, Ng SC, Burisch J, et al. Sex-based differences in the incidence of inflammatory bowel diseases-pooled analysis of population-based studies from the Asia-Pacific region. Aliment Pharmacol Ther. 2019;49:904–911. doi: 10.1111/apt.15178. [DOI] [PubMed] [Google Scholar]
- 20.Park SH, Kim YJ, Rhee KH, Kim YH, Hong SN, Kim KH, et al. Songpa-Kangdong Inflammatory Bowel Disease [SK-IBD] Study Group. A 30-year trend analysis in the epidemiology of inflammatory bowel disease in the Songpa-Kangdong district of Seoul, Korea in 1986-2015. J Crohn's Colitis. 2019;13:1410–1417. doi: 10.1093/ecco-jcc/jjz081. [DOI] [PubMed] [Google Scholar]
- 21.Duricova D, Fumery M, Annese V, Lakatos PL, Peyrin-Biroulet L, Gower-Rousseau C. The natural history of Crohn's disease in children: a review of population-based studies. Eur J Gastroenterol Hepatol. 2017;29:125–134. doi: 10.1097/MEG.0000000000000761. [DOI] [PubMed] [Google Scholar]
- 22.Van Limbergen J, Russell RK, Drummond HE, Aldhous MC, Round NK, Nimmo ER, et al. Definition of phenotypic characteristics of childhood-onset inflammatory bowel disease. Gastroenterology. 2008;135:1114–1122. doi: 10.1053/j.gastro.2008.06.081. [DOI] [PubMed] [Google Scholar]
- 23.Kim HJ, Oh SH, Kim DY, Lee HS, Park SH, Yang SK, et al. Clinical characteristics and long-term outcomes of paediatric Crohn's disease: a single-centre experience. J Crohn's Colitis. 2017;11:157–164. doi: 10.1093/ecco-jcc/jjw146. [DOI] [PubMed] [Google Scholar]
- 24.Attard TM, Horton KM, DeVito K, Darbari A, Oliva-Hemker M, Thompson R, Cuffari C. Pediatric jejunoileitis: a severe Crohn's disease phenotype that requires intensive nutritional management. Inflamm Bowel Dis. 2004;10:357–360. doi: 10.1097/00054725-200407000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Cosnes J, Cattan S, Blain A, Beaugerie L, Carbonnel F, Parc R, et al. Long-term evolution of disease behavior of Crohn's disease. Inflamm Bowel Dis. 2002;8:244–250. doi: 10.1097/00054725-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Walters TD, Kim MO, Denson LA, Griffiths AM, Dubinsky M, Markowitz J, et al. PRO-KIIDS Research Group. Increased effectiveness of early therapy with anti-tumor necrosis factor-α vs an immunomodulator in children with Crohn's disease. Gastroenterology. 2014;146:383–391. doi: 10.1053/j.gastro.2013.10.027. [DOI] [PubMed] [Google Scholar]
- 27.Kang B, Choi SY, Kim HS, Kim K, Lee YM, Choe YH. Mucosal healing in paediatric patients with moderate-to-severe luminal Crohn's disease under combined immunosuppression: escalation versus early treatment. J Crohn's Colitis. 2016;10:1279–1286. doi: 10.1093/ecco-jcc/jjw086. [DOI] [PubMed] [Google Scholar]
- 28.Choi J, Kang B, Kim MJ, Sohn I, Lee HJ, Choe YH. Early infliximab yields superior long-term effects on linear growth in pediatric Crohn's disease patients. Gut Liver. 2018;12:255–262. doi: 10.5009/gnl17290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bouguen G, Levesque BG, Feagan BG, Kavanaugh A, Peyrin-Biroulet L, Colombel JF, et al. Treat to target: a proposed new paradigm for the management of Crohn's disease. Clin Gastroenterol Hepatol. 2015;13:1042–50.e2. doi: 10.1016/j.cgh.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 30.Kang B, Choe YH. Early biologic treatment in pediatric Crohn's disease: catching the therapeutic window of opportunity in early disease by treat-to-target. Pediatr Gastroenterol Hepatol Nutr. 2018;21:1–11. doi: 10.5223/pghn.2018.21.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Birimberg-Schwartz L, Zucker DM, Akriv A, Cucchiara S, Cameron FL, Wilson DC, et al. Pediatric IBD Porto group of ESPGHAN. Development and validation of diagnostic criteria for IBD subtypes including IBD-unclassified in children: a multicentre study from the Pediatric IBD Porto Group of ESPGHAN. J Crohn's Colitis. 2017;11:1078–1084. doi: 10.1093/ecco-jcc/jjx053. [DOI] [PubMed] [Google Scholar]
- 32.Shi HY, Levy AN, Trivedi HD, Chan FKL, Ng SC, Ananthakrishnan AN. Ethnicity influences phenotype and outcomes in inflammatory bowel disease: a systematic review and meta-analysis of population-based studies. Clin Gastroenterol Hepatol. 2018;16:190–7.e11. doi: 10.1016/j.cgh.2017.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim BJ, Song SM, Kim KM, Lee YJ, Rhee KW, Jang JY, et al. Characteristics and trends in the incidence of inflammatory bowel disease in Korean children: a single-center experience. Dig Dis Sci. 2010;55:1989–1995. doi: 10.1007/s10620-009-0963-5. [DOI] [PubMed] [Google Scholar]
- 34.Jin WS, Park JH, Lim KI, Tchah H, Ryoo E. Significance of perianal lesion in pediatric crohn disease. Pediatr Gastroenterol Hepatol Nutr. 2018;21:184–188. doi: 10.5223/pghn.2018.21.3.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kang B, Lee Y, Lee K, Choi YO, Choe YH. Long-term outcomes after switching to CT-P13 in pediatric-onset inflammatory bowel disease: a single-center prospective observational study. Inflamm Bowel Dis. 2018;24:607–616. doi: 10.1093/ibd/izx047. [DOI] [PubMed] [Google Scholar]
- 36.Kang B, Choi SY, Choi YO, Kim MJ, Kim K, Lee JH, et al. Subtherapeutic infliximab trough levels and complete mucosal healing are associated with sustained clinical remission after infliximab cessation in paediatric-onset Crohn's disease patients treated with combined immunosuppressive therapy. J Crohn's Colitis. 2018;12:644–652. doi: 10.1093/ecco-jcc/jjy021. [DOI] [PubMed] [Google Scholar]
- 37.Kang B, Choi SY, Choi YO, Lee SY, Baek SY, Sohn I, et al. Infliximab trough levels are associated with mucosal healing during maintenance treatment with infliximab in paediatric Crohn's disease. J Crohn's Colitis. 2019;13:189–197. doi: 10.1093/ecco-jcc/jjy155. [DOI] [PubMed] [Google Scholar]
- 38.Assa A, Amitai M, Greer ML, Castro DA, Kuint RC, Martínez-León M, et al. ImageKids Study Group. Perianal pediatric crohn disease is associated with a distinct phenotype and greater inflammatory burden. J Pediatr Gastroenterol Nutr. 2017;65:293–298. doi: 10.1097/MPG.0000000000001484. [DOI] [PubMed] [Google Scholar]
- 39.Adler J, Dong S, Eder SJ, Dombkowski KJ ImproveCareNow Pediatric IBD Learning Health System. Perianal crohn disease in a large multicenter pediatric collaborative. J Pediatr Gastroenterol Nutr. 2017;64:e117–24. doi: 10.1097/MPG.0000000000001447. [DOI] [PubMed] [Google Scholar]
- 40.Short SS, Dubinsky MC, Rabizadeh S, Farrior S, Berel D, Frykman PK. Distinct phenotypes of children with perianal perforating Crohn's disease. J Pediatr Surg. 2013;48:1301–1305. doi: 10.1016/j.jpedsurg.2013.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]