Abstract
Although scholars have long studied circumstances that shape prejudice, inquiry into factors associated with long-term prejudice reduction has been more limited. Using a 6-year longitudinal study of non-Black physicians in training (N = 3,134), we examined the effect of three medical-school factors—interracial contact, medical-school environment, and diversity training—on explicit and implicit racial bias measured during medical residency. When accounting for all three factors, previous contact, and baseline bias, we found that quality of contact continued to predict lower explicit and implicit bias, although the effects were very small. Racial climate, modeling of bias, and hours of diversity training in medical school were not consistently related to less explicit or implicit bias during residency. These results highlight the benefits of interracial contact during an impactful experience such as medical school. Ultimately, professional institutions can play a role in reducing anti-Black bias by encouraging more frequent, and especially more favorable, interracial contact.
Keywords: implicit bias, interracial contact, prejudice, racial bias, open data, open materials, preregistered
Among the factors that contribute to racial disparities in health, physicians’ racial biases, both explicit and implicit, play a significant role (Penner et al., 2013; Smedley, Stith, Nelson, & Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, 2003). Explicit biases represent consciously held negative attitudes and are modifiable by exposure to and consideration of new information. Implicit biases, by contrast, have been conceived of as overlearned, highly durable associations that are relatively resistant to change (Gawronski & Brannon, 2019). Although the effects of experimental interventions to reduce implicit bias rarely last beyond 24 hr (Lai et al., 2014; Lai et al., 2016), long-term personal (Turner, Hewstone, & Voci, 2007) and educational (Neto, da Conceiçao Pinto, & Mullet, 2016) experiences can have an enduring impact. In the present research, we investigated, longitudinally across a 6-year period, how personal contact with Black people before and during medical school, the medical-school racial environment, and diversity training predict non-Black U.S. physicians’ anti-Black explicit and implicit bias in their second year of residency. Understanding factors that can affect, and potentially ameliorate, biases among physicians is particularly important for improving the quality of care that Black patients receive relative to White patients and, ultimately, for reducing racial health disparities (FitzGerald & Hurst, 2017; Hall et al., 2015).
Whereas experimental interventions to change bias in a lasting way have had limited success, interracial contact, assessed in terms of both quantity (frequency of contact) and quality (favorability of contact), is consistently associated with lower levels of explicit bias (Pettigrew & Tropp, 2006) and implicit bias (Turner et al., 2007). The contact hypothesis, as traditionally conceptualized, specifies that intergroup contact improves attitudes under certain conditions (e.g., cooperative, equal-status intergroup interactions). Indeed, in earlier work using the same sample as the current study but while participants were still in medical school, we measured medical-school contact and racial attitudes. We found that non-Black medical students’ reports of higher quality interracial contact predicted both more positive explicit attitudes (Burke et al., 2017; see also Binder et al., 2009) and lower levels of implicit bias (van Ryn et al., 2015) at the end of the fourth year of medical school. Quality of contact may be a stronger predictor of racial bias than quantity of contact in medical contexts because it reflects the subjective social experience of contact. In medical contexts, quantity of contact often represents largely task-focused interactions. In general, socially oriented interactions of positive quality are more effective than task-oriented interactions at reducing prejudice (Bettencourt, Brewer, Croak, & Miller, 1992). Given that intergroup contact has been found to have long-term and generalizable effects on explicit bias (Pettigrew & Tropp, 2011; cf. Paluck, Green, & Green, 2019), we hypothesized that interracial contact during medical school, which we assessed in terms of both quality and quantity, would predict reduced explicit and implicit bias 2 years later, when participants were practicing physicians. Moreover, because work on contact theory emphasizes the importance of providing additional opportunities for contact as a way to reduce prejudice (Pettigrew & Tropp, 2011), we examined the effect of interracial contact during medical training beyond the effects of contact before medical school.
Incorporating data from medical residency had advantages over our previous research, which simultaneously assessed predictors and outcomes at the end of medical school. Methodologically, simultaneous assessment limits arguments for the causal relationships between medical-school experiences and bias compared with a fully longitudinal design (Podsakoff, MacKenzie, Lee, & Podsakoff, 2003). Theoretically, even if medical-school experiences predict bias, questions would remain about whether the effects of contact, for instance, are enduring and generalize beyond the medical-school context. Indeed, researchers have noted a lack of quality longitudinal research on the effects of interracial contact on prejudice reduction among adults (Abrams, 2010; Paluck et al., 2019). Thus, a main contribution of this investigation is the ability to predict bias from experiences measured at a separate, substantially earlier time point.
To test the role of social-influence processes on bias, we also investigated the effect of medical-school environmental factors on bias during residency. Perceptions of racial climate can critically shape prejudice by conveying norms about relations between groups (Christ et al., 2014). The role modeling of biased behaviors, such as racist remarks by other people, can also influence racial bias. Blanchard, Crandall, Brigham, and Vaughn (1994) found that White women expressed more racist views after witnessing a peer condone rather than condemn racism. Ultimately, the existence of bias in the informal curriculum, which represents norms and expectations that are absorbed outside the formal training curriculum (Hafferty, 1998), can negatively impact physicians’ racial bias. In previous work with this sample, in which experiences were assessed at the end of medical school, having heard negative comments from attending physicians or residents was related to greater explicit (Burke et al., 2017) and implicit (van Ryn et al., 2015) racial bias. We hypothesized that perceptions of a welcoming racial climate would predict less racial bias and that the observed role modeling of biased behavior in medical school would predict more racial bias during residency.
Although diversity training is one of the more common interventions suggested and implemented in organizations broadly (Dobbin & Kalev, 2016) and in medical schools specifically (Mendoza et al., 2015; Rapp, 2006), we are aware of little empirical evidence regarding a sustained effect of diversity trainings on racial bias. Most evidence points to sustained improvement in cultural knowledge or information regarding diversity (e.g., Bezrukova, Spell, Perry, & Jehn, 2016; Majumdar, Browne, Roberts, & Carpio, 2004). However, in organizational contexts, diversity trainings appear to have limited impact on subsequent managerial diversity (Kalev, Dobbin, & Kelly, 2006) and can incite backlash (Dobbin & Kalev, 2016; Legault, Gutsell, & Inzlicht, 2011) in ways that restrict their effectiveness for reducing bias. Thus, we also explored the relationship between self-reported hours of diversity training during medical school and bias during residency. Given the mixed findings in the literature, this analysis was exploratory.
Method
Participants
Participants responded to the Medical Student Cognitive Habits and Growth Evaluation (CHANGE) Study—a longitudinal study of trainees from 49 allopathic medical schools in the United States. The schools were randomly selected from strata based on geographic region (six) and status (public vs. private). The northwest region does not include any private allopathic medical schools, leaving 11 strata. The team contacted 5,823 first-year medical students at these schools (out of 8,594 total first-year students) whose contact information could be obtained from the Association of American Medical Colleges, snowball sampling, or a list purchased from a vendor. In the fall of 2010, 4,723 students (81% of those contacted) completed the baseline survey (Wave 1). In the spring of 2014, those students who had completed the baseline survey were recontacted, and 3,994 participants (85% of the original sample) completed the end-of-medical-school survey (Wave 2). In the spring of 2016, we asked those students who had completed the baseline survey to complete the second-year-of-residency survey (Wave 3). Some medical students take time to conduct research or pursue other degrees (e.g., master of public health). We included participants who were in their second year of residency at Wave 3 so the final sample had been at the medical school for a comparable amount of time and were in the same career stage, leaving 3,292 participants who had completed the survey at any of the three waves. Of these, we included the 3,134 respondents (67% of the original sample) who did not select “Black” when asked about their racial identity.
At Wave 1, participants were asked to indicate their ethnicity (Hispanic/Latino, not Hispanic/Latino, or unknown) and race (American Indian/Alaska Native, East Asian, South Asian, Black, Native Hawaiian/Pacific Islander, White, or Unknown). After excluding participants who indicated Black or African ancestry, 70% of the participants (n = 2,209) were exclusively White, 22% (n = 689) were exclusively Asian, 4% (n = 124) were multiracial without Black or African ancestry, and 0.4% (n = 10) were Native American or Pacific Islander. One hundred two participants indicated that their race or ethnicity was unknown. Participants also reported their gender (male, female, or other). At Wave 1, 51% of participants were men (n = 1,606), 49% were women (n = 1,545), 3 participants marked “other,” and 10 did not report their gender. At Wave 2, participants selected their childhood annual household income from 10 options ranging from “Less than $10,000” to “$500,000 or more.” Because the reported family income of more than a third of the participants fell into the third-to-highest category ($100,000–$249,999), we grouped participants into three categories: less than $100,000 (43%; n = 1,301), $100,000 to $249,999 (35.3%; n = 1,117), and $250,000 or more (19%; n = 591). One hundred fifty-five participants did not report their childhood annual household income.
Procedure
Participants were recruited for a study about “changes in medical students’ quality of life” and received payment for completing the survey at each wave. The surveys included a range of questions about student attitudes and opinions, well-being, and professional ambitions. We used a subset of items in the present study. The independent variables were contact with Black people, perceptions of racial climate, role modeling of racial bias, and hours of diversity training in medical school. The dependent measures were explicit and implicit racial bias during residency. The Mayo Clinic Institutional Review Board (IRB) approved this study. Per IRB guidelines, participants were allowed to skip questions without penalty; thus, not all participants completed all measures.
Racial bias
Explicit attitudes were measured at each wave using 101-point feeling thermometers (0 = very cold or unfavorable to 100 = very warm or favorable) toward Black people (“African Americans”) and White people (“Caucasians”). Implicit bias was measured at each wave using the Implicit Association Test (IAT). In one block, participants categorized images and words using one key for “Black” and “good” and another for “White” and “bad.” In another block, the categories were switched—“Black” was paired with “bad” and “White” with “good.” We used established criteria to exclude trials and participants with extremely long latencies or high error rates (Greenwald, Nosek, & Banaji, 2003). Among correct categorizations, to calculate IAT D scores, we subtracted average response times for the “Black” + “good” and “White” + “bad” blocks from average response times for the “Black” + “bad” and “White” + “good” blocks and then divided by the standard deviation of all trials. Scores ranged from −1.53 (strong preference for Black people) to 1.60 (strong preference for White people).
Contact
To measure prior quality of contact (West & Hewstone, 2012) with Black people, we asked participants at Wave 1 to indicate how favorable their interactions with Black people were before medical school on a 4-point scale (1 = very unfavorable, 2 = unfavorable, 3 = favorable, 4 = very favorable). At Wave 2, participants indicated, on the same scale, how favorable their interactions were with (a) Black medical students; (b) Black faculty, attending physicians,1 and residents; (c) Black allied health staff;2 and (d) Black clerical, administrative, and secretarial staff.3 These items exhibited high reliability (α = .88) and were averaged to create a composite score.
To measure prior quantity of contact (Eller & Abrams, 2003) with Black people, we asked participants at Wave 1 to report how much interaction they had had with Black people before medical school on a 4-point scale (1 = none, 2 = little, 3 = some, 4 = substantial). At Wave 2, participants reported, on the same scale, how much interaction they had with the groups listed above (Note 3). These items were also averaged to create a composite score (α = .82).
Medical-school environment
We examined three as-pects of the medical-school environment: racial climate, role modeling of racial bias, and hours of diversity training (Note 3). At Wave 2, participants reflected on their perceptions of the racial climate of their medical schools using a composite measure of eight items (α = .74) measured on 7-point scales ranging from strongly disagree to strongly agree. The composite consisted of three subscales: perceived learning orientation toward racial relations (Neel & Shapiro, 2012; e.g., “Students in this medical school are encouraged to learn from their mistakes in interacting with members of another race”), perceived racial tension (Reid & Radhakrishnan, 2003; e.g., “I have witnessed racial insensitivity from faculty”; reverse coded), and perceived medical-school effort (Reid & Radhakrishnan, 2003; e.g., “The medical school fosters respect for cultural differences”). The results of a confirmatory factor analysis indicated that all item loadings on the “climate” factor exceeded 0.5. A higher score indicated a more positive medical-school racial climate. At Wave 2, participants reported how often they heard professors or residents make “negative comments, disparaging remarks, or jokes” about Black patients on a 5-point scale ranging from never to very often.
Because diversity education is implemented differently across institutions (e.g., dedicated courses, integrated into other courses), our measure focused on participants’ self-reported number of hours of diversity training (Burke et al., 2017; van Ryn et al., 2015). At Wave 2, participants were able to indicate completing up to 50 hr of training related to “racial disparities and bias” during medical school.
Analytic strategy
To examine the effects of medical-school experiences on explicit and implicit bias during the second year of residency, we estimated linear mixed-effects models in Stata software (Version 16; StataCorp, 2019) using multiple imputation to account for missing data. In each model, we included sampling stratum and specified a random intercept by school. The five medical-school predictors were (a) quality of contact with Black people, (b) quantity of contact with Black people, (c) perceived racial environment, (d) observed role modeling of racial bias, and (e) reported hours of diversity training, all measured and modeled at the individual level.
For explicit bias, we conducted two primary analyses. First, we tested the separate effects of each Wave 2 predictor on Wave 3 explicit attitudes toward Black people, controlling for stratum, Wave 3 explicit attitudes toward White people, Wave 1 explicit attitudes toward Black and White people, Wave 1 amount and favorability of contact for those respective predictors, participant race, gender, and socioeconomic status. This allowed us to account for existing explicit bias against and previous contact with Black people and demographic factors (which are sometimes associated with racial attitudes; Sabin, Nosek, Greenwald, & Rivara, 2009). Second, to identify the unique effects of each predictor, we simultaneously tested all five predictors in one model, along with all the covariates and Wave 2 explicit bias. For implicit bias, we conducted comparable analyses. We report the separate effects of each Wave 2 predictor on Wave 3 pro-White implicit racial bias, as detailed above, and a model in which we simultaneously tested all predictors.
Finally, to incorporate measurements at different time points along appropriate causal pathways, we estimated a set of random-effects cross-lagged models for each type of bias, modeling effects from each measurement point, as well as repeated measures of bias. Again, we included all waves, using multiple imputation to account for missing responses and including random effects for medical school.
The analytic models that we report here were not preregistered but emerged through the review process (see osf.io/vu9xd for our preregistration and the Supplemental Material for the results of our preregistered analyses).
Results
Table 1 presents the means and standard deviations for medical-school experiences, explicit attitudes toward Blacks and Whites, explicit bias, and implicit bias at all three waves of the study. First, we explored the relationships among the variables included in this study. Second, we examined whether quality and quantity of interracial contact, perceptions of the medical-school climate, and diversity training predicted explicit and implicit bias toward Black people in physicians’ second year of residency. Data and syntax are available on the Open Science Framework at https://osf.io/78cqx/.
Table 1.
Means and Standard Deviations of Medical-School Experiences, Racial Attitudes, and Racial Bias
| Category and variable | Wave 1 (Year 1) | Wave 2 (Year 4) | Wave 3 (Residency Year 2) |
|---|---|---|---|
| Medical-school experience | |||
| Quality of contact with Black people | 3.27 (0.61)a | 3.42 (0.52)b | 3.37 (0.48) |
| Quantity of contact with Black people | 3.04 (0.78)a | 3.06 (0.66)b | 3.13 (0.60) |
| Perceived welcoming racial climate | 5.27 (0.93)b | 5.15 (0.93) | |
| Observed role modeling of racial bias | 1.74 (0.90)b | 1.73 (1.32) | |
| Hours of diversity training | 11.87 (10.03)b | 4.98 (6.61) | |
| Racial attitudes and racial bias | |||
| Explicit attitudes toward Blacks | 81.05 (19.77) | 80.59 (20.44) | 77.77 (20.96) |
| Explicit attitudes toward Whites | 85.74 (17.90) | 83.54 (19.33) | 81.27 (19.85) |
| Pro-White explicit bias | 4.69 (12.93) | 2.95 (11.89) | 3.49 (14.78) |
| Pro-White implicit bias | 0.48 (0.42) | 0.46 (0.43) | 0.45 (0.42) |
Note: Standard deviations are in parentheses.
This variable represents experience before medical school, for use as a covariate. bThis variable represents experience during medical school, for use as a predictor.
Missing-data analysis
To assess the impact of attrition, we compared non-Black participants who were in their second year of residency and completed all three waves with those who did not complete all waves. There were no significant differences in most of the predictors, covariates, or outcomes (ps = .09–.87; see the Supplemental Material available online for details). Participants who completed all three waves completed fewer hours of diversity training (M = 11.56) than those who did not (M = 14.31).
Correlations
We computed bivariate correlations to explore relationships among the study variables (see Table 2). Both higher quality and greater quantity of contact measured at the first two waves of data collection generally tended to relate to more positive attitudes toward Black people and lower levels of implicit bias at the same or subsequent waves of data collection.
Table 2.
Bivariate Correlations Among Contact With Black People, Medical-School Experiences, Explicit Attitudes, and Implicit Bias
| Variable | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Wave 1: quantity of contact with Black people | .27*** | .24*** | .13*** | .15*** | .11*** | .01 | .02 | .03 | −.01 | .01 | .03 | .18*** | .08*** | .14*** | .05** | .13*** | .04* | –.08*** | –.08*** | –.10*** |
| 2. Wave 1: quality of contact with Black people | — | .05** | .25*** | .07*** | .23*** | –.09*** | .06** | −.02 | −.03 | .07*** | .05** | .43*** | .22*** | .27*** | .12*** | .23*** | .11*** | –.12*** | –.06** | –.11*** |
| 3. Wave 2: quantity of contact with Black people | — | .19*** | .33*** | .12*** | .04* | .27*** | .17*** | −.02 | .10*** | .03 | .03 | .01 | .09*** | .05* | .07** | .01 | −.01 | –.05** | –.04* | |
| 4. Wave 2: quality of contact with Black people | — | .10*** | .33*** | –.14*** | .26*** | .07*** | –.04* | .19*** | .03 | .23*** | .16*** | .34*** | .23*** | .25*** | .17*** | –.06** | –.09*** | –.10*** | ||
| 5. Wave 3: quantity of contact with Black people | — | .25*** | −.01 | .14*** | .09*** | .06** | .24*** | .10*** | .07*** | .03 | .10*** | .06** | .06** | .02 | .00 | −.01 | .02 | |||
| 6. Wave 3: quality of contact with Black people | — | –.11*** | .21*** | .04* | –.12*** | .35*** | .10*** | .25*** | .15*** | .28*** | .19*** | .37*** | .25*** | –.06** | –.06** | –.07*** | ||||
| 7. Wave 2: role modeling of racial bias | — | –.37*** | .03 | .23*** | –.21*** | .03 | –.04* | .01 | –.10*** | −.04 | –.06** | −.02 | .03 | .05** | .02 | |||||
| 8. Wave 2: welcoming medical-school racial climate | — | .18* * * | –.13* * * | .39** * | .02 | .10** * | .11* * * | .15* * * | .15** * | .12** * | .12** * | .02 | −.03 | .01 | ||||||
| 9. Wave 2: reported hours of diversity training | — | .05* | .09*** | .24*** | .00 | −.01 | .05* | .05* | −.01 | −.02 | .02 | −.03 | .01 | |||||||
| 10. Wave 3: role modeling of racial bias | — | –.26*** | .09*** | –.04* | .01 | –.04* | .01 | –.10*** | –.05** | −.00 | .02 | .01 | ||||||||
| 11. Wave 3: welcoming medical-school racial climate | — | .19*** | .09*** | .08*** | .16*** | .13*** | .19*** | .17*** | −.02 | −.02 | −.01 | |||||||||
| 12. Wave 3: reported hours of diversity training | — | .03 | −.00 | .05* | .04 | .05** | .02 | −.03 | −.01 | –.04* | ||||||||||
| 13. Wave 1: explicit attitudes toward Blacks | — | .77*** | .48*** | .35*** | .38*** | .29*** | –.09*** | –.05** | –.07** | |||||||||||
| 14. Wave 1: explicit attitudes toward Whites | — | .36*** | .43*** | .28*** | .37*** | .02 | .02 | .01 | ||||||||||||
| 15. Wave 2: explicit attitudes toward Blacks | — | .82*** | .48*** | .36*** | –.06*** | –.06*** | –.07*** | |||||||||||||
| 16. Wave 2: explicit attitudes toward Whites | — | .36*** | .43*** | .03 | .02 | .03 | ||||||||||||||
| 17. Wave 3: explicit attitudes toward Blacks | — | .74*** | –.06** | –.06** | –.07*** | |||||||||||||||
| 18. Wave 3: explicit attitudes toward Whites | — | .03 | .02 | .03 | ||||||||||||||||
| 19. Wave 1: pro-White implicit bias | — | .32*** | .33*** | |||||||||||||||||
| 20. Wave 2: pro-White implicit bias | — | .33*** | ||||||||||||||||||
| 21. Wave 3: pro-White implicit bias | — |
Note: Correlations in boldface are statistically significant.
p < .05. **p < .01. ***p < .001.
Relationships among medical-school experiences and explicit and implicit bias during residency
We examined the relationship between contact and explicit attitudes toward Black people during residency, controlling for explicit attitudes toward White people (see Table 3). The quality of contact with Black people during medical school (Wave 2) predicted more positive explicit attitudes in residency (Wave 3) when we controlled for the quality of contact with Black people before medical school (Wave 1). Similarly, Wave 2 quantity of contact with Black people predicted positive explicit attitudes at Wave 3 when we controlled for Wave 1 quantity of contact with Black people. Thus, the quality and quantity of participants’ contact with Black people during medical school predicted explicit bias beyond contact before medical school. We further found that reporting a welcoming medical-school racial climate at Wave 2 predicted more positive explicit attitudes at Wave 3. Reporting role modeling of racial bias at Wave 2 and reported hours of diversity training at Wave 2 were unrelated to explicit attitudes at Wave 3. In a full model including all predictors and covariates and Wave 2 explicit attitudes, only Wave 2 quality of contact with Black people continued to predict more positive explicit attitudes at Wave 3. The R2 of the full model was .55.
Table 3.
Contact, Role Modeling of Racial Bias, Climate, and Diversity Training in Medical School as Predictors of Explicit and Implicit Bias Against Black People in the Second Year of Medical Residency
| Explicit bias | Implicit bias | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Individual model (ICC = 1.1e-20 to 9.9e-15)a | Full model (ICC = 3.0e to 13; R2 = .547747)b | Individual model (ICC = 6.0e-16 to 1.4e-10)c | Full model (ICC = 7.0e to 16; R2 = .169533)d | |||||||||
| Predictor | β | SE | p | β | SE | p | β | SE | p | β | SE | p |
| Wave 2: quality of contact with Black peoplee | 0.08 | 0.02 | < .001 | 0.03 | 0.02 | .025 | –0.06 | 0.02 | .002 | –0.04 | 0.02 | .024 |
| Wave 2: quantity of contact with Black peoplef | 0.04 | 0.02 | .018 | 0.01 | 0.02 | .40 | −0.02 | 0.02 | .27 | −0.01 | 0.02 | .60 |
| Wave 2: perceived welcoming racial climate | 0.04 | 0.02 | .023 | 0.01 | 0.02 | .48 | −0.01 | 0.02 | .62 | 0.02 | 0.02 | .38 |
| Wave 2: observed role modeling of racial bias | −0.03 | 0.01 | .081 | −0.00 | 0.02 | .98 | 0.02 | 0.02 | .34 | 0.01 | 0.02 | .71 |
| Wave 2: hours of diversity training | 0.00 | 0.02 | .86 | −0.01 | 0.02 | .49 | −0.00 | 0.02 | .93 | 0.01 | 0.02 | .72 |
| Wave 1: quality of contact with Black peopleg | 0.05 | 0.01 | < .001 | 0.03 | 0.01 | .040 | –0.06 | 0.02 | < .001 | −0.03 | 0.02 | .074 |
| Wave 1: quantity of contact with Black peopleh | 0.05 | 0.02 | .003 | 0.02 | 0.02 | .37 | –0.06 | 0.02 | < .001 | –0.04 | 0.02 | .033 |
| Wave 2: bias | 0.33 | 0.03 | < .001 | 0.30 | 0.03 | < .001 | 0.24 | 0.02 | < .001 | 0.23 | 0.02 | < .001 |
Note: For explicit-bias models, positive values indicate warmer attitudes (less bias) because the dependent variable was explicit attitudes toward Black people and the model controlled for explicit attitudes toward White people. For implicit-bias models, positive values indicate more bias. All predictors and dependent variables have been standardized. All models include a random intercept by school and account for the effect of stratum as a categorical predictor. All values are based on pooled estimates across multiple imputations. Values in boldface are statistically significant. ICC = intraclass correlation coefficient.
aThese columns show results for models with individual predictors of explicit attitudes toward Black people during residency, controlling for explicit attitudes toward White people during residency, baseline explicit attitudes toward Black and White people, and demographics. bThese columns show results for one model with the five predictors of attitudes toward Black people during residency, controlling for explicit attitudes toward White people during residency, baseline and end-of-medical-school explicit attitudes toward Black and White people, and demographics. cThese columns show results for models with individual predictors of Implicit Association Test (IAT) D scores, which index pro-White implicit bias, controlling for baseline IAT D score and demographics. dThese columns show results for one model with the five predictors of IAT D score, controlling for baseline and end-of-medical-school IAT D score and demographics. eThe individual predictor model controlled for baseline quality of contact with Black people. fThe individual predictor model controlled for baseline quantity of contact with Black people. gThe individual predictor model did not control for quality of contact with Black people during medical school. hThe individual predictor model did not control for quantity of contact with Black people during medical school.
In terms of implicit bias, individually and in the full model, the only Wave 2 factor that predicted less implicit bias at Wave 3 was the quality of contact with Black people during medical school. The R2 of the full model was .17. Of note, the quality and quantity of contact with Black people before medical school individually predicted explicit attitudes and implicit bias during residency. In the full models, the quality of contact with Black people before medical school continued to predict explicit attitudes during residency, and the quantity of contact with Black people before medical school continued to predict implicit bias during residency.
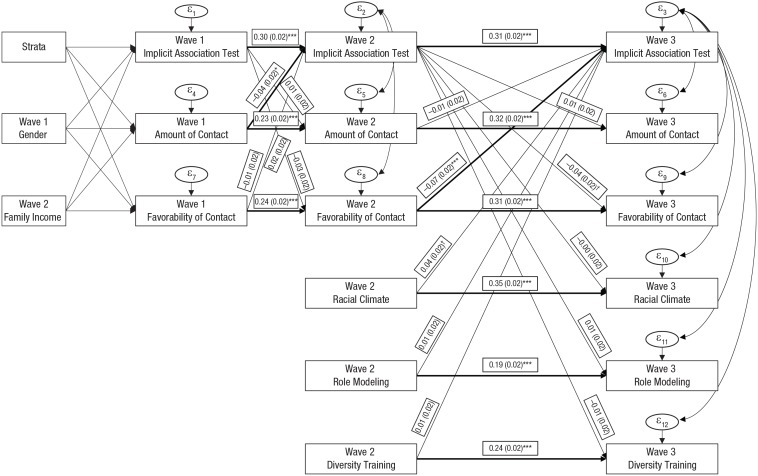
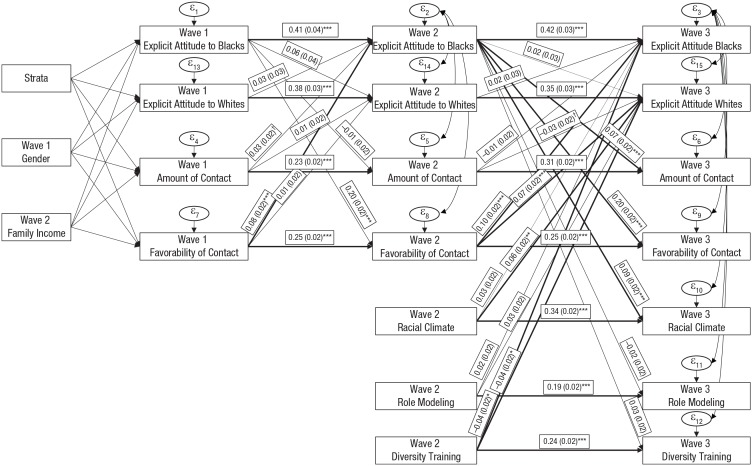
Figures 1 and 2 depict the results of the cross-lagged relationships among implicit and explicit bias (respectively) and contact, racial climate, and diversity training. They confirm our findings that the quality of contact with Black people during medical school is related to less explicit and implicit bias when other relationships are accounted for across waves. Unexpectedly, this analysis indicated that the hours of diversity training during medical school were negatively related to explicit attitudes toward both Black and White people during residency and that perceiving a welcoming medical-school racial climate was positively related to pro-White implicit bias during residency. Because these relationships were not observed in any other analyses, these two results should be interpreted cautiously. Nevertheless, we note that the negative relationship between hours of diversity training and explicit attitudes toward Black and White people could reflect the backlash that diversity training sometimes elicits (Dobbin & Kalev, 2016; Legault et al., 2011).
Fig. 1.
Cross-lagged relationships among implicit bias toward Blacks and Whites, contact, racial climate, and diversity training (N = 3,134). Values on single-headed arrows are standardized regression coefficients (with standard errors in parentheses); double-headed arrows indicate covariance. Bolded lines indicate significant relationships (*p < .05, ***p < .001); marginal significance is indicated by a dagger (p < .10).
Fig. 2.
Cross-lagged relationships among explicit attitudes, contact, racial climate, and diversity training (N = 3,134). Values on single-headed arrows are standardized regression coefficients (with standard errors in parentheses); double-headed arrows indicate covariance. Bolded lines indicate significant relationships (*p < .05, **p < .01, ***p < .001); marginal significance is indicated by a dagger (p < .10).
The cross-lagged analyses also indicate that favorable contact before medical school predicts more positive explicit attitudes toward Black people at the end of medical school, that more positive explicit attitudes at the beginning of medical school predicts more favorable contact during medical school, and that more positive explicit attitudes toward Black people at the end of medical school predict more—and more favorable—contact with Black people and more positive perceptions of the racial climate in residency. For implicit bias, more contact with Black people before medical school predicts lower pro-White implicit bias at the end of medical school, which predicts more favorable contact with Black people during residency.
Discussion
Our goal was to identify whether interracial contact and other medical-school experiences would predict non-Black physicians’ explicit and implicit bias 2 years later, during residency. Theoretically, the present work highlights the importance of considering the distinct effect of interracial contact during medical school on subsequent racial bias, beyond the effect of previous contact over the course of one’s lifetime. In the context of recent questions about the effectiveness of intergroup contact for reducing bias and the need for further experimental and longitudinal research (Paluck et al., 2019), particularly in naturalistic contexts (Paluck & Green, 2009), we provide longitudinal evidence of the relationship between the quality of interracial contact and racial bias in a large and important but difficult-to-reach sample (3,134 physicians in residency).
Previous research has suggested that contact earlier in life can have a long-term impact on implicit attitudes into adulthood (Rudman, Phelan, & Heppen, 2007). Our longitudinal study confirmed that more frequent and favorable contact with Black people before medical school continued to predict bias in residency, independently of more recent contact during medical school. However, even accounting for participants’ previous contact, we found that more favorable interracial contact during medical school further predicted less explicit and less implicit bias during residency. This effect was quite small, though. In our full model, a 1-standard-deviation change in quality of contact resulted in a 0.03-standard-deviation change in explicit attitudes and a 0.04-standard-deviation change in implicit bias. The effects were larger in the cross-lagged models: A 1-standard-deviation change in quality of contact resulted in a 0.10-standard-deviation change in explicit attitudes and a 0.07-standard-deviation change in implicit bias.
Consistent with previous work on the importance of the informal curriculum generally (Hafferty, 1998) and with medical students’ racial bias specifically (van Ryn et al., 2015), results showed that when analyzed individually, perceiving a more positive medical-school racial climate predicts less explicit (but not implicit) racial bias in residency. However, in the full model, which considered the predictors simultaneously, racial climate did not significantly predict implicit bias, and the cross-lagged analysis indicated that perceiving a more positive medical-school racial climate predicted more implicit racial bias during residency. These results suggest that although addressing racial climate has the potential to reduce bias (Christ et al., 2014), perhaps especially in the immediate environment and at least in the context of medical training and practice, personal contact is more consistently influential in shaping non-Black physicians’ long-term racial attitudes.
In contrast, in our main analyses, we found no relationship between reported hours of diversity training in medical school and explicit or implicit bias, whereas the cross-lagged analysis demonstrated a negative relationship with explicit attitudes. We note, however, that in order to assess the effect of diversity training in a way that would be comparable across medical schools, we used a metric that was rather blunt (i.e., number of hours) and may not have captured important aspects of these experiences (e.g., the nature and quality of the material presented). For example, it is possible that the focus of diversity training was to achieve cultural competence in clinical practice and not to reduce bias (our outcome measure). If the goal is simply to improve knowledge about diversity-related topics, diversity training may be an efficient strategy (Majumdar et al., 2004). Nevertheless, given the cost—around $8 billion a year by one estimate (Lipman, 2018)—and other work that has shown that diversity training has limited practical impact (Dobbin & Kalev, 2016) and evidence of backlash (Legault et al., 2011), our findings further highlight the need for evidence-based examinations of the effectiveness of diversity trainings for improving attitudes (Moss-Racusin et al., 2014). If diversity training is expected to improve intergroup attitudes and subsequently reduce biased behavior, increasing opportunities for interracial contact might be a valuable strategy to pursue as part of, or in addition to, formal diversity education.
We acknowledge that the effects of predictors on non-Black physicians’ explicit attitudes and implicit bias were statistically small, and smaller for implicit bias than for explicit bias, reflecting the generally limited malleability of implicit bias (Lai et al., 2014; Lai et al., 2016). Moreover, personal attitudes and implicit bias are generally only modest predictors of specific instances of discrimination (Kurdi et al., 2019; Oswald, Mitchell, Blanton, Jaccard, & Tetlock, 2015). Nevertheless, there is convergent evidence in medical contexts that greater physician bias—and particularly implicit bias—systematically predicts lower quality care that a physician provides to a Black patient (FitzGerald & Hurst, 2017; Hall et al., 2015; Penner et al., 2013). Given the critical importance of these medical encounters (e.g., determining the course of treatment for cancer; Penner et al., 2016), even limited reductions in physicians’ anti-Black bias have the potential to improve the health of and, potentially, save the lives of a significant number of Black people.
The present study featured a uniquely large and representative sample and included a number of relevant measures; however, there are likely other factors that might influence explicit and implicit bias. For example, one limitation of the present research is that we focused primarily on individual-level experiences and perceptions. Future research might consider how more macro and structural elements of the environment (e.g., the percentage of Black medical students or patients; an emphasis on cooperative learning exercises in a curriculum) can also influence racial bias (Christ et al., 2014), in part through the mechanisms we considered (e.g., more favorable intergroup contact, more positive intergroup environment). Understanding the medical-school experiences that have enduring effects on physicians’ explicit and implicit racial biases can inform structural-level interventions (e.g., incorporating cooperative learning tasks to promote positive contact) and policies (e.g., prohibiting open expressions of bias) that can have a cascading positive impact on the experiences and medical care of Black patients.
In conclusion, independently of the quality and quantity of contact before medical school, explicit and implicit bias at the beginning and end of medical school, perceptions of the racial environment of the medical school, and participation in diversity training, the quality of contact with Black people during medical school predicted non-Black physicians’ more positive explicit attitudes and less negative implicit bias against Black people 2 years later. These findings highlight the role that interracial contact can play in reducing racial health disparities.
Supplemental Material
Supplemental material, Onyeador_Open_Practices_Disclosure_rev for The Value of Interracial Contact for Reducing Anti-Black Bias Among Non-Black Physicians: A Cognitive Habits and Growth Evaluation (CHANGE) Study Report by Ivuoma N. Onyeador, Natalie M. Wittlin, Sara E. Burke, John F. Dovidio, Sylvia P. Perry, Rachel R. Hardeman, Liselotte N. Dyrbye, Jeph Herrin, Sean M. Phelan and Michelle van Ryn in Psychological Science
Supplemental material, Onyeador_Supplemental_Material for The Value of Interracial Contact for Reducing Anti-Black Bias Among Non-Black Physicians: A Cognitive Habits and Growth Evaluation (CHANGE) Study Report by Ivuoma N. Onyeador, Natalie M. Wittlin, Sara E. Burke, John F. Dovidio, Sylvia P. Perry, Rachel R. Hardeman, Liselotte N. Dyrbye, Jeph Herrin, Sean M. Phelan and Michelle van Ryn in Psychological Science
Supplemental material, Onyeador_Supplemental_Tables for The Value of Interracial Contact for Reducing Anti-Black Bias Among Non-Black Physicians: A Cognitive Habits and Growth Evaluation (CHANGE) Study Report by Ivuoma N. Onyeador, Natalie M. Wittlin, Sara E. Burke, John F. Dovidio, Sylvia P. Perry, Rachel R. Hardeman, Liselotte N. Dyrbye, Jeph Herrin, Sean M. Phelan and Michelle van Ryn in Psychological Science
Acknowledgments
We thank Deborah Finstad, Kristin Hardin, and Sharyn French for help with testing and data collection and Ron Lam for running the cross-lagged models and full imputation.
Attending physicians have completed training and supervise trainees in clinical settings.
Allied health staff are health professionals who are not nurses or doctors.
These items were also measured at the Wave 3 (residency) time point.
Footnotes
Action Editor: Michael Inzlicht served as action editor for this article.
Author Contributions: M. van Ryn and J. F. Dovidio developed the study concept. M. van Ryn, S. M. Phelan, S. E. Burke, and J. F. Dovidio designed the study. Testing and data collection were performed under the direction of M. van Ryn. I. N. Onyeador, N. M. Wittlin, S. E. Burke, J. F. Dovidio, S. P. Perry, R. R. Hardeman, L. N. Dyrbye, J. Herrin, S. M. Phelan, and M. van Ryn analyzed and interpreted the data. I. N. Onyeador drafted the manuscript, and the remainder of the authors provided critical revisions. All authors approved the final version of the manuscript for submission.
ORCID iD: Ivuoma N. Onyeador  https://orcid.org/0000-0002-4272-8572
https://orcid.org/0000-0002-4272-8572
Declaration of Conflicting Interests: The author(s) declared that there were no conflicts of interest with respect to the authorship or the publication of this article.
Funding: This work was supported by a National Science Foundation Directorate for Social, Behavioral and Economic Sciences Postdoctoral Research Fellowship (No. 1809370 to I. N. Onyeador); the National Institutes of Health (NIH) National Heart, Lung, and Blood Institute (Award Nos. R01HL085631 to M. van Ryn, R01HL085631-S1 to S. P. Perry, and R01HL085631-S2 and R01HL085631-S3 to R. R. Hardeman); and the NIH National Institute of Diabetes and Digestive and Kidney Diseases (Award No. K01 DK095924 to S. M. Phelan).
Supplemental Material: Additional supporting information can be found at http://journals.sagepub.com/doi/suppl/10.1177/0956797619879139
Open Practices:



All data and materials have been made publicly available via the Open Science Framework and can be accessed at https://osf.io/78cqx/. The design and analysis plans for the experiments were preregistered at https://osf.io/vu9xd. The complete Open Practices Disclosure for this article can be found at http://journals.sagepub.com/doi/suppl/10.1177/0956797619879139. This article has received the badges for Open Data, Open Materials, and Preregistration. More information about the Open Practices badges can be found at http://www.psychologicalscience.org/publications/badges.
References
- Abrams D. (2010). Processes of prejudice: Theory, evidence and intervention. Equalities and Human Rights Commission. Retrieved from https://kar.kent.ac.uk/29732/1/56_processes_of_prejudice.pdf
- Bettencourt B. A., Brewer M. B., Croak M. R., Miller N. (1992). Cooperation and the reduction of intergroup bias: The role of reward structure and social orientation. Journal of Experimental Social Psychology, 28, 301–319. doi: 10.1016/0022-1031(92)90048-O [DOI] [Google Scholar]
- Bezrukova K., Spell C. S., Perry J. L., Jehn K. A. (2016). A meta-analytical integration of over 40 years of research on diversity training evaluation. Personality and Social Psychology Bulletin, 142, 1227–1274. [DOI] [PubMed] [Google Scholar]
- Binder J., Zagefka H., Brown R., Funke F., Kessler T., Mummendey A., . . . Leyens J.-P. (2009). Does contact reduce prejudice or does prejudice reduce contact? A longitudinal test of the contact hypothesis among majority and minority groups in three European countries. Journal of Personality and Social Psychology, 96, 843–856. doi: 10.1037/a0013470 [DOI] [PubMed] [Google Scholar]
- Blanchard F. A., Crandall C. S., Brigham J. C., Vaughn L. A. (1994). Condemning and condoning racism: A social context approach to interracial settings. Journal of Applied Psychology, 79, 993–997. doi: 10.1037/0021-9010.79.6.993 [DOI] [Google Scholar]
- Burke S. E., Dovidio J. F., Perry S. P., Burgess D. J., Hardeman R. R., Phelan S. M., . . . van Ryn M. (2017). Informal training experiences and explicit bias against African Americans among medical students. Social Psychology Quarterly, 80, 65–84. doi: 10.1177/0190272516668166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christ O., Schmid K., Lolliot S., Swart H., Stolle D., Tausch N., . . . Hewstone M. (2014). Contextual effect of positive intergroup contact on outgroup prejudice. Proceedings of the National Academy of Sciences, USA, 111, 3996–4000. doi: 10.1073/pnas.1320901111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobbin F., Kalev A. (2016). Why diversity programs fail. Harvard Business Review. Retrieved from https://hbr.org/2016/07/why-diversity-programs-fail
- Eller A., Abrams D. (2003). ‘Gringos’ in Mexico: Cross-sectional and longitudinal effects of language school-promoted contact on intergroup bias. Group Processes & Intergroup Relations, 6, 55–75. doi: 10.1177/1368430203006001012 [DOI] [Google Scholar]
- FitzGerald C., Hurst S. (2017). Implicit bias in healthcare professionals: A systematic review. BMC Medical Ethics, 18(1), Article 19. doi: 10.1186/s12910-017-0179-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gawronski B., Brannon S. M. (2019). Attitudes and the implicit-explicit dualism. In Albarracín D., Johnson B. T. (Eds.), The Handbook of attitudes (2nd ed., Vol. 1, pp. 158–196). New York, NY: Taylor & Francis. [Google Scholar]
- Greenwald A. G., Nosek B. A., Banaji M. R. (2003). Understanding and using the Implicit Association Test: I. An improved scoring algorithm. Journal of Personality and Social Psychology, 85, 197–216. doi: 10.1037/0022-3514.85.2.197 [DOI] [PubMed] [Google Scholar]
- Hafferty F. W. (1998). Beyond curriculum reform: Confronting medicine’s hidden curriculum. Academic Medicine, 73, 403–407. [DOI] [PubMed] [Google Scholar]
- Hall W. J., Chapman M. V., Lee K. M., Merino Y. M., Thomas T. W., Payne B. K., . . . Coyne-Beasley T. (2015). Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: A systematic review. American Journal of Public Health, 105(12), e60–e76. doi: 10.2105/AJPH.2015.302903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalev A., Dobbin F., Kelly E. (2006). Best practices or best guesses? Assessing the efficacy of corporate affirmative action and diversity policies. American Sociological Review, 71, 589–617. doi: 10.1177/000312240607100404 [DOI] [Google Scholar]
- Kurdi B., Seitchik A. E., Axt J., Carroll T. J., Karapetyan A., Kaushik N., . . . Banaji M. (2019). Relationship between the Implicit Association Test and intergroup behavior: A meta-analysis. American Psychologist, 74, 569–586. doi: 10.1037/amp0000364 [DOI] [PubMed] [Google Scholar]
- Lai C. K., Marini M., Lehr S. A., Cerruti C., Shin J.-E. L., Joy-Gaba J. A., . . . Nosek B. A. (2014). Reducing implicit racial preferences: I. A comparative investigation of 17 interventions. Journal of Experimental Psychology: General, 143, 1765–1785. doi: 10.1037/a0036260 [DOI] [PubMed] [Google Scholar]
- Lai C. K., Skinner A. L., Cooley E., Murrar S., Brauer M., Devos T., . . . Nosek B. A. (2016). Reducing implicit racial preferences: II. Intervention effectiveness across time. Journal of Experimental Psychology: General, 145, 1001–1016. doi: 10.1037/xge0000179 [DOI] [PubMed] [Google Scholar]
- Legault L., Gutsell J. N., Inzlicht M. (2011). Ironic effects of antiprejudice messages: How motivational interventions can reduce (but also increase) prejudice. Psychological Science, 22, 1472–1477. doi: 10.1177/0956797611427918 [DOI] [PubMed] [Google Scholar]
- Lipman J. (2018, January 25). How diversity training infuriates men and fails women. Time. Retrieved from http://time.com/5118035/diversity-training-infuriates-men-fails-women/
- Majumdar B., Browne G., Roberts J., Carpio B. (2004). Effects of cultural sensitivity training on health care provider attitudes and patient outcomes. Journal of Nursing Scholarship, 36, 161–166. doi: 10.1111/j.1547-5069.2004.04029.x [DOI] [PubMed] [Google Scholar]
- Mendoza F. S., Walker L. R., Stoll B. J., Fuentes-Afflick E., Geme J. W. S., Cheng T. L., . . . Sectish T. C. (2015). Diversity and inclusion training in pediatric departments. Pediatrics, 135, 707–713. doi: 10.1542/peds.2014-1653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss-Racusin C. A., van der Toorn J., Dovidio J. F., Brescoll V. L., Graham M. J., Handelsman J. (2014). Scientific diversity interventions. Science, 343, 615–616. doi: 10.1126/science.1245936 [DOI] [PubMed] [Google Scholar]
- Neel R., Shapiro J. R. (2012). Is racial bias malleable? Whites’ lay theories of racial bias predict divergent strategies for interracial interactions. Journal of Personality and Social Psychology, 103, 101–120. [DOI] [PubMed] [Google Scholar]
- Neto F., da Conceiçao Pinto M., Mullet E. (2016). Can music reduce anti-dark-skin prejudice? A test of a cross-cultural musical education programme. Psychology of Music, 44, 388–398. [Google Scholar]
- Oswald F. L., Mitchell G., Blanton H., Jaccard J., Tetlock P. E. (2015). Using the IAT to predict ethnic and racial discrimination: Small effect sizes of unknown societal significance. Journal of Personality and Social Psychology, 108, 562–571. doi: 10.1037/pspa0000023 [DOI] [PubMed] [Google Scholar]
- Paluck E. L., Green D. P. (2009). Prejudice reduction: What works? A review and assessment of research and practice. Annual Review of Psychology, 60, 339–367. doi: 10.1146/annurev.psych.60.110707.163607 [DOI] [PubMed] [Google Scholar]
- Paluck E. L., Green S. A., Green D. P. (2019). The contact hypothesis re-evaluated. Behavioural Public Policy, 3, 129–158. doi: 10.1017/bpp.2018.25 [DOI] [Google Scholar]
- Penner L. A., Dovidio J. F., Gonzalez R., Albrecht T. L., Chapman R., Foster T., . . . Eggly S. (2016). The effects of oncologist implicit racial bias in racially discordant oncology interactions. Journal of Clinical Oncology, 34, 2874–2880. doi: 10.1200/JCO.2015.66.3658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner L. A., Hagiwara N., Eggly S., Gaertner S. L., Albrecht T. L., Dovidio J. F. (2013). Racial healthcare disparities: A social psychological analysis. European Review of Social Psychology, 24, 70–122. doi: 10.1080/10463283.2013.840973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettigrew T. F., Tropp L. R. (2006). A meta-analytic test of intergroup contact theory. Journal of Personality and Social Psychology, 90, 751–783. doi: 10.1037/0022-3514.90.5.751 [DOI] [PubMed] [Google Scholar]
- Pettigrew T. F., Tropp L. R. (2011). When groups meet: The dynamics of intergroup contact. Philadelphia, PA: Psychology Press. [Google Scholar]
- Podsakoff P. M., MacKenzie S. B., Lee J.-Y., Podsakoff N. P. (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology, 88, 879–903. doi: 10.1037/0021-9010.88.5.879 [DOI] [PubMed] [Google Scholar]
- Rapp D. E. (2006). Integrating cultural competency into the undergraduate medical curriculum. Medical Education, 40, 704–710. doi: 10.1111/j.1365-2929.2006.02515.x [DOI] [PubMed] [Google Scholar]
- Reid L. D., Radhakrishnan P. (2003). Race matters: The relation between race and general campus climate. Cultural Diversity and Ethnic Minority Psychology, 9, 263–275. [DOI] [PubMed] [Google Scholar]
- Rudman L. A., Phelan J. E., Heppen J. B. (2007). Developmental sources of implicit attitudes. Personality and Social Psychology Bulletin, 33, 1700–1713. doi: 10.1177/0146167207307487 [DOI] [PubMed] [Google Scholar]
- Sabin J., Nosek B. A., Greenwald A. G., Rivara F. P. (2009). Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. Journal of Health Care for the Poor and Underserved, 20, 896–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley B. D., Stith A. Y., Nelson A. R., & Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. (2003). Unequal treatment: Confronting racial and ethnic disparities in healthcare. Washington, DC: National Academy Press. [PubMed] [Google Scholar]
- StataCorp. (2019). Stata Statistical Software: Version 16 [Computer software]. College Station, TX: Author. [Google Scholar]
- Turner R. N., Hewstone M., Voci A. (2007). Reducing explicit and implicit outgroup prejudice via direct and extended contact: The mediating role of self-disclosure and intergroup anxiety. Journal of Personality and Social Psychology, 93, 369–388. doi: 10.1037/0022-3514.93.3.369 [DOI] [PubMed] [Google Scholar]
- van Ryn M., Hardeman R., Phelan S. M., Burgess D. J., Dovidio J. F., Herrin J., . . . Przedworski J. M. (2015). Medical school experiences associated with change in implicit racial bias among 3547 students: A medical student CHANGES Study report. Journal of General Internal Medicine, 30, 1748–1756. doi: 10.1007/s11606-015-3447-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- West K., Hewstone M. (2012). Culture and contact in the promotion and reduction of anti-gay prejudice: Evidence from Jamaica and Britain. Journal of Homosexuality, 59, 44–66. doi: 10.1080/00918369.2011.614907 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Onyeador_Open_Practices_Disclosure_rev for The Value of Interracial Contact for Reducing Anti-Black Bias Among Non-Black Physicians: A Cognitive Habits and Growth Evaluation (CHANGE) Study Report by Ivuoma N. Onyeador, Natalie M. Wittlin, Sara E. Burke, John F. Dovidio, Sylvia P. Perry, Rachel R. Hardeman, Liselotte N. Dyrbye, Jeph Herrin, Sean M. Phelan and Michelle van Ryn in Psychological Science
Supplemental material, Onyeador_Supplemental_Material for The Value of Interracial Contact for Reducing Anti-Black Bias Among Non-Black Physicians: A Cognitive Habits and Growth Evaluation (CHANGE) Study Report by Ivuoma N. Onyeador, Natalie M. Wittlin, Sara E. Burke, John F. Dovidio, Sylvia P. Perry, Rachel R. Hardeman, Liselotte N. Dyrbye, Jeph Herrin, Sean M. Phelan and Michelle van Ryn in Psychological Science
Supplemental material, Onyeador_Supplemental_Tables for The Value of Interracial Contact for Reducing Anti-Black Bias Among Non-Black Physicians: A Cognitive Habits and Growth Evaluation (CHANGE) Study Report by Ivuoma N. Onyeador, Natalie M. Wittlin, Sara E. Burke, John F. Dovidio, Sylvia P. Perry, Rachel R. Hardeman, Liselotte N. Dyrbye, Jeph Herrin, Sean M. Phelan and Michelle van Ryn in Psychological Science