Abstract
Background: Several anatomical variations of the median nerve recurrent motor branch have been described. No previous reports have described the anatomical variation of the ulnar nerve with respect to transverse carpal ligament. In this article, we present a patient with symptomatic compression of the ulnar nerve found to occur outside the Guyon canal due to a transligamentous course through the distal transverse carpal ligament. Methods: A 59-year-old, right-hand-dominant male patient presented with right hand pain, subjective weakness, and numbness in both the ulnar and the median nerve distributions. Electromyography revealed moderate demyelinating sensorimotor median neuropathy at the wrist and distal ulnar sensory neuropathy. At the time of planned carpal tunnel and Guyon canal release, a transligamentous ulnar nerve sensory common branch to the fourth webspace was encountered and safely released. Results: There were no surgical complications. The patient’s symptoms of numbness in the median and ulnar nerve distribution clinically improved at his first postoperative visit. Conclusions: We have identified a case of transligamentous ulnar nerve sensory branch encountered during carpal tunnel release. To our knowledge, this has not been previously reported. While the incidence of this variant is unknown, hand surgeons should be aware of this anatomical variant as its location puts it at risk of iatrogenic injury during open and endoscopic carpal tunnel release.
Keywords: compression neuropathy, ulnar nerve, transligamentous, carpal tunnel, ulnar sensory branch
Introduction
Anatomical variations in the course of the median nerve in relation to transverse carpal ligament including intraligamentous, transligamentous, and subligamentous courses have been described.1 It is critical that surgeons are aware of these differences to safely perform surgery near the wrist, including open and endoscopic carpal tunnel release. Compression of the ulnar nerve within the Guyon canal is common and alternatively has been reported to arise from anomalous origin of the abductor digiti minimi muscle.2 No previous reports of a transligamentous or an intraligamentous ulnar nerve were identified on a PubMed literature search. Here, we report a case of a symptomatic intraligamentous ulnar nerve sensory branch and possible clinical implications.
Case Presentation
A 59-year-old, right-hand-dominant male patient presented with a 1-year history of persistent and progressive subjective right hand pain, weakness, and numbness. He specifically reported numbness in all right hand digits, most severe in the ring and small fingers, and endorsed frequent nighttime pain that would awaken him from sleep. Conservative measures including night splinting had failed to improve his symptoms. A Tinel’s sign was present over the median nerve proximal to the transverse carpal ligament and over the area of the Guyon canal but absent over the cubital tunnel. Two-point discrimination was 7 mm in all digits, and light touch in the distribution of the dorsal ulnar cutaneous branch was subjectively normal. Electromyography revealed evidence of moderate sensorimotor median neuropathy at the wrist without active denervation and distal ulnar sensory neuropathy, with demyelination and no obvious neuropathy at the level of the cubital tunnel.
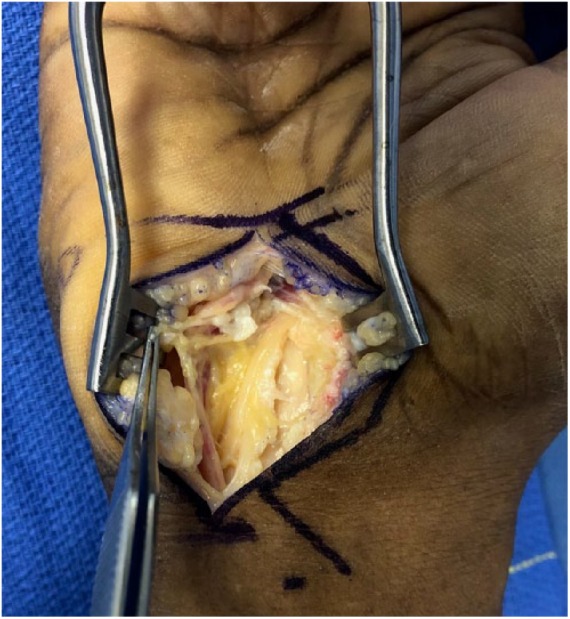
An open carpal tunnel and release of the Guyon canal was planned. After division of the palmar fascia, blunt dissection was performed to the level of the transverse carpal ligament. A structure arising from the ulnar side of the wrist was noted to enter the distal third of the carpal ligament in line with the radial aspect of the ring finger (Figure 1). The structure was followed proximally and was noted to arise from the ulnar nerve. The deep motor branch was decompressed and found to be unremarkable. The transverse carpal tunnel was then released until the level of the intraligamentous nerve was dissected out and followed distally where its course was consistent with the common sensory branch to the ring and small fingers (Figure 2). The remainder of the carpal ligament was then released, and no anomalous recurrent median nerve branches were seen. The patient’s postoperative course was uneventful, and he reported significant improvement in right hand pain as well as median and ulnar hypoesthesia at his first follow-up visit.
Figure 1.
Aberrant transligamentous ulnar nerve sensory branch entering the distal transverse carpal ligament.
Figure 2.

Appearance of transligamentous branch after dissection out of the ligament, completion of carpal tunnel release, and exploration of deep motor branch.
Discussion
Anatomical variants of the distal median and ulnar nerves have been reported in the literature, including subligamentous, preligamentous, and transligamentous median recurrent motor nerve branching patterns,1,3 duplicate thenar motor branches,1 accessory median nerve branches proximal to the carpal tunnel,4 a distal ulnar nerve loop, 5 an ulnar nerve within the carpal tunnel causing compression on the median nerve,6 and compression of the ulnar nerve by anomalous heads of the abductor digiti minimi muscle.2 A complete understanding of these variants is essential to prevent inadvertent iatrogenic injury during open or endoscopic carpal tunnel release or other wrist surgery.
Typically, the ulnar nerve enters the hand via the Guyon canal, coursing between pisiform and hamate as it divides into deep and superficial branches. The superficial branch, which provides sensory branches to the ulnar small finger and a common digital nerve that supplies the ulnar ring and radial small fingers, courses deep to the palmar fascia, with the ulnar artery above the level of the pisohamate ligament. In this case, a nerve arising from the sensory branch pierced the palmar fascia before entering the distal third of the transverse carpal ligament, running within the ligament for a distance of approximately 5 mm. To our knowledge, there have been no previous reports of anatomical variants of the ulnar nerve with respect to the transverse carpal ligament.
While the incidence of this variant is unknown, its intraligamentous course and location in line with the ring finger puts it at a higher risk of iatrogenic injury during open or endoscopic carpal tunnel release. Hand surgeons should be aware of this possibility and should exercise caution when performing open or endoscopic carpal tunnel release in patients with associated ulnar nerve sensory symptoms thought to arise from compression at the level of the Guyon canal.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from the individual participant included in this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Kyle J Chepla  https://orcid.org/0000-0002-6641-9774
https://orcid.org/0000-0002-6641-9774
References
- 1. Al-Qattan MM. Variations in the course of the thenar motor branch of the median nerve and their relationship to the hypertrophic muscle overlying the transverse carpal ligament. J Hand Surg Am. 2010;35(11):1820-1824. [DOI] [PubMed] [Google Scholar]
- 2. Netscher D, Cohen V. Ulnar nerve compression at the wrist secondary to anomalous muscles: a patient with a variant of abductor digiti minimi. Ann Plast Surg. 1997;39(6):647-651. [DOI] [PubMed] [Google Scholar]
- 3. Henry BM, Zwinczewska H, Roy J, et al. The Prevalence of Anatomical Variations of the Median Nerve in the Carpal Tunnel: a Systematic Review and Meta-Analysis. PLoS ONE. 2015;10(8):e0136477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lanz U. Anatomical variations of the median nerve in the carpal tunnel. J Hand Surg Am. 1977;2(1):44-53. [DOI] [PubMed] [Google Scholar]
- 5. Patel M, Iwanaga J, Oskouian RJ, Tubbs RS. Variant Distal Ulnar Nerve Loop: a Previously Undescribed Anatomical Finding. Cureus. 2018;10(5):e2604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Galzio RJ, Magliani V, Lucantoni D, D’Arrigo C. Bilateral anomalous course of the ulnar nerve at the wrist causing ulnar and median nerve compression syndrome. Case Report. J Neurosurg. 1987;67(5):754-756. [DOI] [PubMed] [Google Scholar]


