Abstract
Recently, we have described physiological expression patterns of NKL homeobox genes in early hematopoiesis and in subsequent lymphopoiesis. We identified nine genes which constitute the so-called NKL-code. Aberrant overexpression of code-members or ectopically activated non-code NKL homeobox genes are described in T-cell leukemia and in T- and B-cell lymphoma, highlighting their oncogenic role in lymphoid malignancies. Here, we introduce the NKL-code in normal hematopoiesis and focus on deregulated NKL homeobox genes in B-cell lymphoma, including HLX, MSX1 and NKX2-2 in Hodgkin lymphoma; HLX, NKX2-1 and NKX6-3 in diffuse large B-cell lymphoma; and NKX2-3 in splenic marginal zone lymphoma. Thus, the roles of various members of the NKL homeobox gene subclass are considered in normal and pathological hematopoiesis in detail.
Keywords: homeobox, homeodomain, NKL-code
1. Hematopoiesis and B-Cell Development
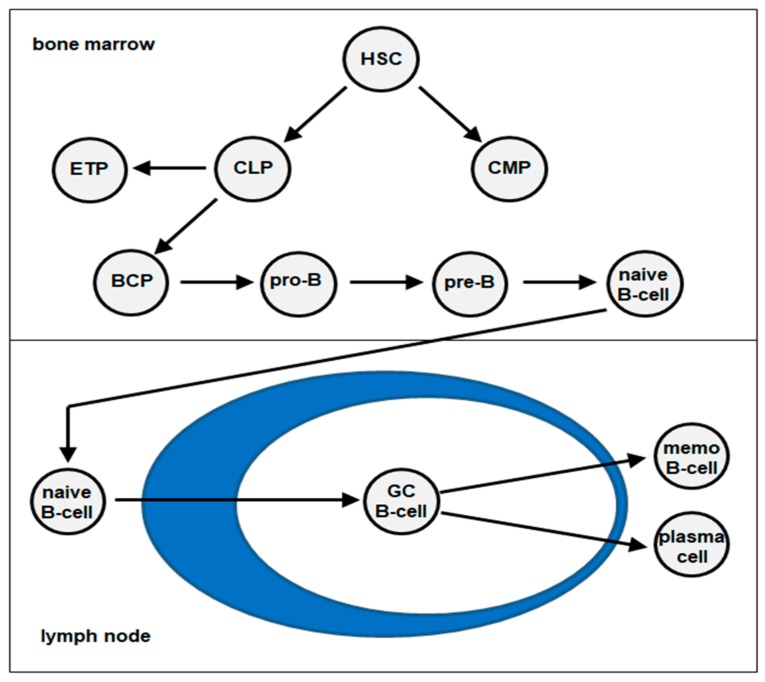
The process of hematopoiesis is responsible for the production of all types of blood cells. Hematopoietic stem and progenitor cells (HSCs) generate common myeloid and lymphoid progenitors (CMP and CLP) which, respectively, represent the starting points for the myeloid and lymphoid cell lineages. The latter produces all types of lymphocytes comprising B-cells, T-cells, natural killer (NK)-cells and innate lymphoid cells. Early B-cell development, which includes the rearrangements of the B-cell receptor genes (immunoglobulin heavy chain, IGH), takes place in the bone marrow and begins with the CLP-derived B-cell progenitor (BCP). BCPs differentiate via the pro-B-cell and pre-B-cell stages into naïve B-cells. In contrast, early T-cell progenitors (ETP) migrate into the thymus to complete their differentiation. For the final differentiation steps to memory B-cells (memo B-cell) and plasma cells via the stage of germinal center (GC) B-cells, naïve B-cells migrate from the bone marrow into lymph nodes, the spleen and other lymphoid tissues [1,2,3] (Figure 1). In these compartments, additional molecular alterations occur, like somatic hypermutation and class switching of the IGH genes. These alterations are performed at the DNA level and the process of class switching is additionally connected with gene rearrangements.
Figure 1.
Schematic presentation of B-cell development. Hematopoietic stem cell (HSC), common myeloid progenitors (CMP), common lymphoid progenitors (CLP), early T-cell progenitors (ETP), B-cell progenitor (BCP), germinal center (GC).
The main regulatory steps of lymphopoiesis including B-cell development are controlled at the transcriptional level [3,4]. Accordingly, several transcription factors (TFs), like BCL6, EBF1, MYB, PAX5, PRDM1 (alias name: BLIMP1) and TCF3 (E2A), are members of a B-cell specific regulatory network which orchestrates basic differentiation processes [5,6,7]. TCF3 plays a prominent role in the development of all types of lymphocytes, while EBF1 and PAX5 are master factors of the B-cell lineage. BCL6 and PRDM1 inhibit each other and are involved in differentiation processes taking place in the GC. Provoked by aberrant chromosomal rearrangements or gene mutations, deregulations of these developmental TFs are thought to contribute to the generation of B-cell malignancies [8,9]. Abnormal rearrangements of the IGH genes represent a frequent mechanism of oncogene activation, while deregulated hypermutation is known to be responsible for many gene mutations.
2. Classification of Homeobox Genes
Homeobox genes encode TFs, which regulate fundamental processes in development and differentiation in both embryogenesis and the adult. They share the conserved 180 bp long homeobox, which encodes the homeodomain at the protein level. This domain consists of 60 amino acid residues and mediates specific interactions with DNA, chromatin, non-coding (nc)RNA and cooperating TFs, thus representing a common platform of their gene regulatory activities [10].
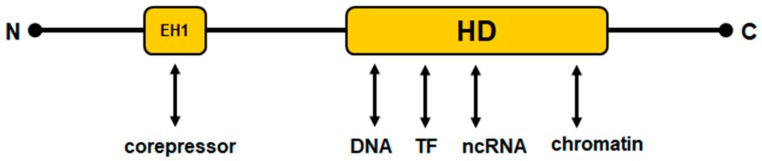
The subgroup of NK-like homeobox genes, which were later called NKL homeobox genes, have been reported for the first time by Nirenberg and Kim (abbreviated as NK) in the fruit fly Drosophila. In this invertebrate organism, the subgroup members are arranged in a cluster consisting of six genes [11]. Additional orthologous genes have since been identified and the group extended. These studies indicated that this clustering represents the ancient gene order, which is now just barely visible in vertebrates [12]. Thus, in contrast to the still-clustered HOX-genes, NKL homeobox genes show only relicts of a clustered arrangement in humans. In addition to their conserved homeodomain, NKL homeodomain proteins share a short, conserved sequence in their N-terminal part, which has been termed the engrailed-homology motif (EH1) [13,14]. This motif performs physical interactions with corepressors of the groucho family, thus mediating transcriptional inhibition [15]. Figure 2 depicts a schematic structure of NKL homeodomain proteins. Most NKL homeobox genes are functionally associated with mesodermal development, possibly displaying their ancient function [16]. A systematic classification of all 235 human homeobox genes has generated a panel of eleven classes and several subclasses. Main classes are called antennapedia (ANTP) and paired box (PRD), comprising 150 genes. Other classes identified are CERS, CUT, HNF, LIM, POU, PROS, SINE, TALE, and ZF. Accordingly, NKL homeobox genes represent a subclass of the ANTP class and contain 48 members in humans [17].
Figure 2.
Schematic structure of NKL homeodomain proteins. HD: conserved homeodomain consisting of 60 amino acid residues; EH1: conserved engrailed-homology domain consisting of about eight amino acid residues. The N- and C-terminal parts show no sequence conservation. The EH1 domain and the homeodomain interact with particular components of the gene regulatory machinery.
3. NKL Homeobox Genes in Hematopoiesis
3.1. NKL-Code in Developing Lymphocytes
In 2003, we identified the aberrantly expressed homeobox gene NKX2-5 (CSX1) in two different T-cell acute lymphoblastic leukemia (T-ALL) derived cell lines, which became activated via the chromosomal rearrangement t(5;14)(q35;q32) [18]. This gene was the third homeobox oncogene identified in this disease after the initial reports of TLX1 (HOX11) and TLX3 (HOX11L2) in 1991 and 2001, respectively [19,20,21]. We recognized that all three genes are members of the same group of NKL homeobox genes and suggested that these related genes may thus perform similar oncogenic effects [18]. To date, 24 aberrantly activated NKL homeobox genes have been described in T-ALL patients, representing the largest group of oncogenes in this malignancy [22,23]. These oncogenes additionally include MSX1, NKX2-1, NKX3-1, and NKX3-2 [24,25,26,27,28,29]. Mechanisms of aberrant gene activation are presented by chromosomal rearrangements and deregulated activites of TFs, chromatin factors, and signalling pathways [18,24,27,30]. Furthermore, deregulated NKL homeobox genes play a significant role in T-cell lymphoma as well, underlining their oncogenic potential in T-cells [31].
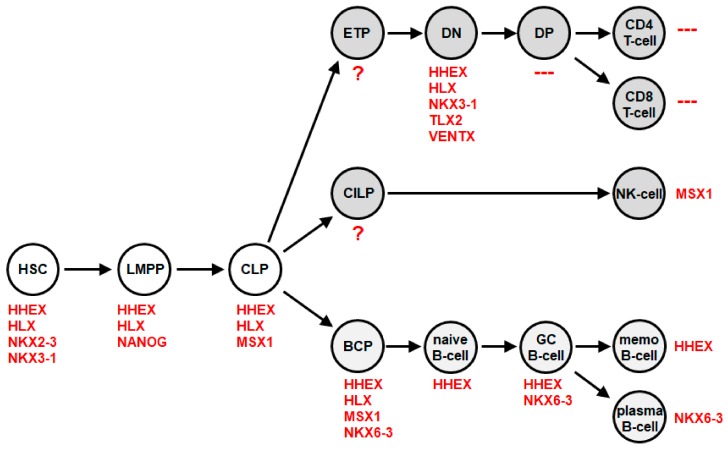
Then, we analyzed the physiological activity of NKL homeobox genes in early hematopoiesis and T-cell development. This exercise revealed nine members, comprising HHEX, HLX, MSX1, NANOG, NKX2-3, NKX3-1, NKX6-3, TLX2, and VENTX (Figure 3). They showed a specific expression pattern in stem cells, progenitor cells and immature thymocytes, but not in mature T-cells, which tested negative. We named this pattern and the respective genes the NKL-code [22]. This code demonstrated that most NKL homeobox oncogenes in T-ALL are ectopically expressed. For example, NKX2-5 is normally expressed in the developing heart and spleen but not in any hematopoietic cell [32]. Furthermore, MSX1 is normally expressed in hematopoietic progenitors, including CLP and BCP in addition to mature NK-cells, but not in the T-cell lineage (Figure 3). Accordingly, MSX1 is an oncogene in T-ALL and a tumor suppressor in NK-cell leukemia [24,33,34]. HLX (HLX1, H2.0 or HB241) was the first described NKL homeobox gene that is physiologically expressed in hematopoietic cells, including myeloid and B-cells, but not in T-cells [35]. These data support the reported expression pattern of NKL-code members and highlight their functional role in leukemia.
Figure 3.
The NKL-code in lymphopoiesis This diagram depicts activities of NKL homeobox genes during early hematopoiesis and lymphopoiesis, including the development of T-cells, NK-cells and B-cells. Each cell/stage is labelled with the accordingly expressed NKL homeobox genes. BCP: B-cell progenitor, CILP: common innate lymphoid progenitor, CLP: common lymphoid progenitor, DN: double negative, DP: double positive, ETP: early T-cell progenitor, GC B-cell: germinal center B-cell, HSC: hematopoietic stem cell, LMPP: lymphoid primed multipotent progenitor, memo B-cell: memory B-cell.
Additional gene codes containing NKL homeobox genes have been published for the developing neural tube, pharyngeal region, and teeth [36,37,38]. The code members for the neural tube comprise DBX1, DBX2, NKX2-2, NKX6-1, and NKX6-2 [36]. In the pharyngeal region, the gene code consists exclusively of all six DLX family members, while in developing teeth, BARX1, DLX1, DLX2, MSX1, and MSX2 create a code [37,38]. Most of those NKL homeobox gene code members are regulated by signalling pathways and perform cross-reactivity. In the neural tube, the hedgehog- and BMP-pathways are regulated by ligand gradients which are created in opposite directions, thus regulating NKL homeobox gene activities [36]. Therefore, differentiation processes are frequently controlled by particular NKL homeobox genes, via formation of a code.
3.2. B-Cell Associated NKL Homeobox Genes In Normal Development
In 2018, we reported an extended version of the NKL-code, which included developing and mature B-cells [39]. This study revealed four NKL homeobox genes expressed in the B-cell lineage, namely HHEX, HLX, MSX1, and NKX6-3 (Figure 3). BCPs express HHEX, HLX, MSX1, and NKX6-3, while mature memory B-cells express just HHEX, and mature plasma cells NKX6-3. Thus, at each stage of physiological B-cell differentiation, particular NKL homeobox genes are active, generating a specific pattern. Moreover, as described for other NKL homeobox gene codes, hematopoietic NKL-code members show cross-reactivity as well: HHEX and HLX repress MSX1 and NKX6-3; NKX6-3 represses MSX1; and MSX1 activates NKX6-3 [39].
Two of these genes, HLX and HHEX (HEX or PRH), represent the first described non-HOX homeobox genes expressed in hematopoietic cells [35,40]. Expression analyses of these two genes revealed activity in B-cells and myeloid cells, while T-cells were described to be negative [35,41,42,43]. Moreover, downregulation of HHEX was shown to be crucial for normal T-cell differentiation [44]. Of note, the data failed to detect HHEX in plasma cells, consistent with our screening data for the NKL-code [39,43]. Accordingly, analysis of HHEX-knockout mice showed reduced numbers of both mature and pre-B-cells, demonstrating the importance of HHEX for B-cell development [45,46]. Forced expression of HLX in hematopoietic progenitors enhanced myeloid differentiation but arrested the development of B-cells at the pro-B-cell stage and of T-cells at the CD4/CD8 double-positive stage [41,47]. In TH1-cells, HLX is induced by the TF TBX21 (TBET) and thereby involved in the expression of interferon gamma IFNG [48,49]. However, in NK-cells, HLX performs negative regulation of IFNG, demonstrating context-dependent control of target genes [50]. Collectively, these data highlight HHEX and HLX as important regulators of hematopoiesis, including B-cell differentiation.
HHEX: In addition to their activity in developing B-cells, the four NKL-code members HHEX, HLX, MSX1, and NKX6-3 are involved in the differentiation of other tissues and organs as well. HHEX is expressed in parts of the early embryo, including the chorion and yolk sac, later in primordia of the liver and the thyroid, and then in fetal liver, thyroid and lung [51,52]. HHEX is also expressed in the 3rd pharyngeal pouch, which generates the thymus, and in primordia of the pancreas and the gallbladder [53]. Furthermore, HHEX plays a role in vascular and lymphatic development [54]. The expression of HHEX was also detected in normal breast tissue [55]. Accordingly, HHEX performs tumor suppressor activities in breast cancer [56]. In the embryonal anterior endoderm which generates the lung, thyroid, pancreas, and the liver, HHEX is regulated by a complex network which includes the BMP- and WNT-signalling pathways and the TFs LIM1, NODAL, OTX2, and VENTX [57]. Components of this network may play a regulatory role in the hematopoietic system, as well.
HLX: The embryonal expression pattern of HLX indicates some degree of overlap with HHEX, as shown in the foregut, liver, gallbladder, and lung. In addition, the splanchnic mesoderm and mesenteric tissues tested positive for HLX activity in the embryo [58]. HLX is also expressed in the placenta, and controls the switch from white to brown adipose tissue [59,60]. Furthermore, HLX is involved in the differentiation of embryonal stem cells into the intestinal lineage [61]. A screening in induced pluripotent stem cells (iPSCs) for genes regulating pluripotency revealed HHEX and HLX [62]. Thus, both genes are involved in pluripotency and reprogramming, highlighting their potential in cell differentiation processes [62].
MSX1: In early embryogenesis, MSX1 is expressed in the neural plate border region and is thus involved in the generation of neural crest cells and the preplacodal ectoderm [63,64,65,66]. These cells generate a multiplicity of tissues and structures which are fundamental for vertebrate development and evolution. Later on, MSX1 is expressed in neural crest cells and their derived tissues, including the teeth [67,68]. MSX1 also plays a role in the development of craniofacial structures and neural tissues, including the brain [69,70,71]. Accordingly, mutations in the MSX1 gene are frequently found to be connected to particular malformations of craniofacial tissues. Furthermore, MSX1 is expressed in the mammary gland [72]. Functionally, MSX1 is able to dedifferentiate cells. In muscle cells, it has been shown that MSX1 dedifferentiates myotubes by repressing the muscle master factor MYOD and the muscle-specific myogenin [73,74]. These data compellingly demonstrated the developmental potential of this TF.
NKX6-3: Finally, NKX6-3 is expressed in the developing stomach and hindbrain [75,76,77]. Depleting mutations of NKX6-3 in gastric epithelial cells result in the activation of APOBEC family members, which, in turn, enhance the generation of additional mutations and, subsequently, gastric cancer [76]. In addition to MSX1, NKX6-3 is expressed in the neural plate border region as well. Knockdown and overexpression experiments indicated a dominant role of NKX6-3 in the development of neural crest cells [78]. NKX6-3 was able to induce an ectopically neural crest when overexpressed, while NKX6-3 knockdown generated defects in the neural crest [78]. Taken together, experimental data of MSX1 and NKX6-3 highlight the importance and impact of NKL homeobox genes for these pluripotent cells.
Regulation of different developmental processes by the same pathways and TFs, including homeodomain proteins, is a frequent observation in embryogenesis [79]. For example, NKL homeobox gene NKX2-5 basically regulates the development of both heart and spleen [32,80,81]. Therefore, aberrant activities of developmental homeodomain TFs may recapitulate these tissue-specific operations ectopically or at the wrong stage of differentiation, which may lead to tumorigenesis. NKL homeobox gene NKX3-1 performs master gene activities in the development of the prostate and plays a role in the early stages of hematopoiesis, showing physiological activity in different tissues [22,28]. NKL homeobox gene NKX2-5 represents a master gene for the development of the heart in vertebrates and thereby regulates the expression of specific target genes, including MEF2C [80]. This function is reactivated in T-ALL and mediates the ectopic deregulation of MEF2C, which constitutes a major oncogene in this malignancy [18,25,82,83]. Thus, consideration of known physiological operations of aberrantly activated NKL-code members and non-members may reveal findings of clinical importance. The druggability of NKL homeobox genes in particular, and of TFs in general, is difficult to define, but their regulated genes may represent suitable and effective targets for therapy [84].
3.3. Deregulated NKL Homeobox Genes In B-Cell Malignancies
Developmental arrest is a main and widespread feature of cancer cells [85,86,87]. As shown by Allen and coworkers in 1995, forced expression of HLX in hematopoietic progenitors resulted in developmental arrest of pro-B-cells [47]. Therefore, this experiment represents the first hint of the oncogenic potential of NKL homeobox genes in B-cells. Ferrando and coworkers correlated aberrant expression of NKL homeobox gene TLX1 with the developmental arrest of malignant thymocytes at the double-positive stage in T-ALL [88]. Thus, the correlation of aberrantly expressed NKL homeobox genes with particular stages of differentiation from lymphocytes highlights the developmental impact of this gene subclass in lymphoid tumors. Recently, we screened deregulated NKL homeobox genes in a variety of B-cell malignancies, which included Hodgkin lymphoma (HL), follicular lymphoma (FL), diffuse large B-cell lymphoma (DLBCL), hairy cell leukemia (HCL), mantle cell lymphoma (MCL), and splenic marginal zone lymphoma (SMZL). This study revealed 13 aberrantly overexpressed NKL homeobox genes (Table 1), supporting the relevance of this gene group for B-cell cancers [39]. In the following, we discuss in more detail seven selected NKL homeobox genes which have been studied by us and others in B-cell lymphomas, both in primary cells and in cell lines.
Table 1.
NKL homeobox gene expression in normal B-cell development and B-cell lymphomas.
| Gene | HSC | LMPP | CLP | DN | DP | BCP | NB | GCB | MB | PC | HL | FL | DLBCL | HCL | MCL | SMZL |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HHEX | ||||||||||||||||
| HLX | ||||||||||||||||
| MSX1 | ||||||||||||||||
| NANOG | ||||||||||||||||
| NKX2-3 | ||||||||||||||||
| NKX3-1 | ||||||||||||||||
| NKX6-3 | ||||||||||||||||
| TLX2 | ||||||||||||||||
| VENTX | ||||||||||||||||
| BARX2 | ||||||||||||||||
| DLX1 | ||||||||||||||||
| EMX2 | ||||||||||||||||
| NKX2-1 | ||||||||||||||||
| NKX2-2 | ||||||||||||||||
| NKX3-2 |
Physiologically expressed genes are indicated in red, deregulated gene activities detected in patients are indicated in orange. BCP: B-cell progenitor, CLP: common lymphoid progenitor, DLBCL: diffuse large B-cell lymphoma, DN: double negative, DP: double positive, FL: follicular lymphoma, GCB: germinal center B-cell, HCL: hairy cell leukemia, HL: Hodgkin lymphoma, HSC: hematopoietic stem cell, LMPP: lymphoid primed multipotent progenitor, MB: memory B-cell, NB: naive B-cell, PC: plasma cell, MCL: mantle cell lymphoma, SMZL: splenic marginal zone lymphoma. This table is modified as described previously [39].
HLX: HLX is a member of the hematopoietic NKL-code and is expressed in early hematopoiesis and BCPs [22,39]. Aberrant expression of HLX has been found in HL, FL, MCL, and SMZL [39]. HLX is part of a regulatory network consisting of B-cell associated NKL-code members HHEX, MSX1 and NKX6-3 [39]. Aberrant overexpression of HLX in HL cell line L-540 mediated downregulation of MSX1 and NKX6-3, in addition to B-cell factors BCL11A and SPIB, and of pro-apoptotic factor BCL2L11 (BIM) [89]. These regulatory relationships may underlie the described differentiation arrest in immature B-cells after forced expression of HLX [47]. Furthermore, they enhance survival of the tumor cells which represent a main property of HL [89]. ChIP-seq data from ENCODE indicated HLX as target gene of STAT3, which is a transcriptional mediator of several signalling pathways [90]. Accordingly, aberrant activation of STAT3 by JAK2-mediated phosphorylation and/or HDAC-mediated deacetylation contributes to enhanced HLX expression in HL [89]. Acetylation of STAT3 was shown to regulate its nuclear localization, representing an additional level of gene regulation which depends on the activity of acetylating and deacetylating enzymes. Of note, HDACs are druggable enzymes and, thus, potential targets for rational therapies to inhibit STAT3-signalling. Taken together, HLX is embedded in major oncogenic disturbances of HL, including aberrant signalling and apoptosis.
MSX1: MSX1 is normally expressed in CLPs and BCPs and downregulated in the course of B-cell development [39]. Aberrantly overexpressed MSX1 in HL cell line L-1236 inhibited the expression of the B-cell factor ZHX2, probably using histone H1 as co-repressor [91,92]. Silencing of ZHX2 may contribute to the deregulated B-cell phenotype in HL. In ovarian cancer cells, MSX1 performs inhibition of cyclin D1 (CCND1) in addition to other cyclins and cell cycle regulators, while, in primary mesenchymal and epithelial progenitor cell types, MSX1 activates CCND1 [93,94]. These data reflect a balanced interplay between proliferation and differentiation. Accordingly, an inhibitory impact of MSX1 on CCND1 expression was lost in MCL cells containing chromosomal translocation t(11;14)(q13;q32). This genomic rearrangement separates the regulatory MSX1 binding site from the coding part of CCND1 [95]. Therefore, this oncogenic alteration disturbs the indicated balanced interplay and may support CCND1-mediated cell proliferation in MCL.
NKX2-1: NKX2-1 (TTF1) expression has been identified in the DLBCL cell line SU-DHL-5, representing the first documentation of an aberrantly activated NKL homeobox gene in B-cell malignancies [30]. Patient data indicated NKX2-1 deregulation in about 5% of DLBCL cases [30,39]. While, in T-ALL, a chromosomal translocation aberrantly activated NKX2-1 in SU-DHL-5 cells, TF HEY1 and chromatin factors KMT2A (MLL,) and particular histones, are involved in NKX2-1 deregulation [25,30]. KMT2A overexpression in this cell line was correlated with a chromosomal duplication at 11q23 and overexpression of histone H2B, with a chromosomal abnormality at 6p22 [30]. Normally, NKX2-1 is expressed in the embryonal thyroid, lung and brain but not in hematopoietic cells and tissues at any time [96]. Thus, NKX2-1 is ectopically activated in different lymphoid malignancies.
NKX2-2: Similar to NKX2-1, NKX2-2 is ectopically activated in lymphoid tumors, including T-ALL and HL [22,25,97]. In both classical and nodular lymphocyte predominant HL, about 12% of the patients express NKX2-2 [97]. NKX2-2-expressing HL cell line DEV served as a model to reveal aberrant mechanisms of activation. Normally, NKX2-2 is expressed in the brain and pancreas [98,99]. Accordingly, aberrant reactivation of neural pathways and TFs, including IL17RB, FOXG1, FLI1 and NEUROD1, were found to be responsible for NKX2-2 expression in cell line DEV [97]. Of note, IL17RB is targeted by chromosomal translocation t(3;14)(p21;q32). Furthermore, IL17RB activator DAZAP2 is overexpressed via a chromosomal duplication at 12p13, while the gene encoding its repressor, SMURF2, is deleted at 17q24. Thus, three different chromosomal aberrations contribute to activated IL17RB-signalling and subsequent NKX2-2 transcription [97]. Therefore, NKX2-2 expression in HL exemplifies that ectopic reactivation of particular developmental pathways and factors may result in aberrant expression of NKL homeobox genes in B-cell malignancies.
NKX2-3: NKX2-3 is normally expressed in HSCs, thus representing a hematopoietic stem cell factor [22]. In addition, NKX2-3 acts as a master gene for the embryonal development of the spleen [100]. Thus, NKX2-3 is closely associated with the differentiation of hematopoietic cells and tissues. However, in advanced hematopoietic stages or mature blood cells NKX2-3 is silenced. In SMZL, NKX2-3 is aberrantly activated by chromosomal translocation t(10;14)(q24;q32), juxtaposing the locus of this NKL homeobox gene to that of IGH [101]. Downstream analyses indicated aberrant activation of B-cell receptor signalling, enhanced expression of integrins, adhesion factor MADCAM1, and of chemokine receptor CXCR4 [101]. These features may underlie malignant transformation and homing of the tumor cells to the spleen and lymph nodes. In addition to SMZL, aberrant expression of NKX2-3 has been detected in DLBCL, FL, MCL, chronic lymphoid leukemia, and multiple myeloma (MM) [101]. Furthermore, deregulated expression of NKX2-3 has been associated with Crohn disease, ulcerative colitis and inflammatory bowel disease [102]. These diseases originate from immunological disturbances which may share certain pathological aspects with particular B-cell malignancies.
NKX6-3: NKX6-3 is a member of the NKL-code and normally expressed in BCPs, GC B-cells and plasma cells [39]. This pattern indicates important functions for the differentiation of B-cells and the status of plasma cells. Aberrant overexpression of NKX6-3 was detected in FL, DLBCL and MCL patients [39]. DLBCL cell line DOHH-2 showed overexpression of NKX6-3 that was mediated by aberrant BMP-signaling and enhanced activity of chromatin factor AUTS2 [39]. Interestingly, infection of this cell line with Epstein–Barr virus (EBV) resulted in enhanced expression of HLX via STAT3 which in turn repressed NKX6-3 [103]. The EBV-encoded factors LMP1 and LMP2A were shown to mediate STAT3 activation in this cell line. These data may explain the described malignant associations of EBV and B-cell lymphomas [104].
BARX2: BARX2 is normally expressed during embryogenesis in several tissues, including the nervous system, Rathke´s pouch and submandibular glands, and in the adult ovarian epithel [105,106,107]. However, BARX2 is not expressed in developing or adult hematopoietic cells or tissues. Aberrant activity of BARX2 has been found in HCL and MCL patients [39]. Furthermore, BARX2 and NKX2-3 were the only NKL homeobox genes aberrantly expressed in MM [101,108]. Interestingly, except for BARX2, MM and primary effusion lymphoma cell lines lacked activity of any NKL-code member, indicating aberrant downregulation of HHEX and NKX6-3. Thus, in mature B-cell malignancies, NKL homeobox genes may perform tumor suppressor activity.
3.4. Cell Lines as Models for Deregulated NKL Homeobox Genes
Cell lines represent experimental models for that tumor type from which they were derived. Of note, it is of fundamental importance to use authenticated, well characterized, and annotated cell lines to be able to extrapolate cell line data to particular cancers, including B-cell malignancies. We have evaluated and systematically listed hematopoietic cell lines which meet these criteria [109]. In addition, we reviewed cell lines derived from several entities of B-cell malignancies, including B-cell precursor-leukemia, MM, primary effusion lymphoma, primary mediastinal B-cell lymphoma, double-hit B-cell lymphoma, and HL, to highlight appropriate models for particular tumors [110,111,112,113,114,115]. Here, we presented data obtained from both patients and cell lines. Deregulated NKL homeobox genes were usually identified in patients and subsequently investigated in cell lines, analyzing mechanisms of deregulation and downstream activities. Table 2 shows malignant B-cell lines and corresponding aberrant NKL homeobox gene activities to help identify models which would be suitable for the type of cancer and/or the gene of interest.
Table 2.
Aberrantly expressed NKL homeobox genes in malignant B-cell lines.
| Gene | Cell Line | Disease | Remarks | Reference |
|---|---|---|---|---|
| HHEX | ||||
| HLX | L-540 DOHH-2 OCI-LY19 NU-DHL-1 SEM |
HL DLBCL DLBCL DLBCL BCP-ALL |
elevated STAT3 activity EBV-mediated STAT3 activation |
[79] [35,94] [99] [99] [99] |
| MSX1 | L-1236 GRANTA-519 JEKO-1 REC-1 |
HL MCL MCL MCL |
cofactor H1C, target ZHX2 t(11;14)(q13;q32) activates CCND1 t(11;14)(q13;q32) activates CCND1 t(11;14)(q13;q32) activates CCND1 |
[82] [85] [85] [85] |
| NANOG | ||||
| NKX2-3 | ||||
| NKX3-1 | ||||
| NKX6-3 | DOHH-2 | DLBCL | repressed by HLX | [35,94] |
| TLX2 | ||||
| VENTX | SEM | BCP-ALL | [99] | |
| BARX2 | RPMI-8226 | MM | [99] | |
| DLX1 | ||||
| EMX2 | ||||
| NKX2-1 | SU-DHL-5 | DLBCL | KMT2A, H2B | [86] |
| NKX2-2 | DEV | HL | activated by IL17RB-signalling | [88] |
| NKX3-2 |
This table lists B-cell lines in which particular NKL homeobox genes are overexpressed. Additionally, the corresponding disease and potentially relevant information are given. The abbreviations are explained in Table 1.
4. Conclusions
NKL homeobox genes are physiologically expressed in hematopoiesis including B-cell development, in a specific pattern which we have termed the NKL-code. Aberrant activities of these basic developmental regulators are involved in the pathogenesis of B-cell malignancies. The knowledge of their pathophysiological activity and the understanding of their function may contribute to improved diagnostics and novel therapies in the future. Finally, in this field of research, validated cell lines represent informative models to explore the landscape of NKL homeobox genes.
Author Contributions
S.N. wrote the manuscript. H.G.D. revised and edited the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Melchers F. Checkpoints that control B cell development. J. Clin. Invest. 2015;125:2203–2210. doi: 10.1172/JCI78083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shlomchik M.J., Weisel F. Germinal center selection and the development of memory B and plasma cells. Immunol. Rev. 2012;247:52–63. doi: 10.1111/j.1600-065X.2012.01124.x. [DOI] [PubMed] [Google Scholar]
- 3.Boller S., Grosschedl R. The regulatory network of B-cell differentiation: A focused view of early B-cell factor 1 function. Immunol. Rev. 2014;261:102–115. doi: 10.1111/imr.12206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rothenberg E.V. Transcriptional control of early T and B cell developmental choices. Annu. Rev. Immunol. 2014;32:283–321. doi: 10.1146/annurev-immunol-032712-100024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Méndez A., Mendoza L. A network model to describe the terminal differentiation of B cells. PLoS Comput. Biol. 2016;12:e1004696. doi: 10.1371/journal.pcbi.1004696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith E., Sigvardsson M. The roles of transcription factors in B lymphocyte commitment, development, and transformation. J. Leukoc. Biol. 2004;75:973–981. doi: 10.1189/jlb.1103554. [DOI] [PubMed] [Google Scholar]
- 7.Nutt S.L., Kee B.L. The transcriptional regulation of B cell lineage commitment. Immunity. 2007;26:715–725. doi: 10.1016/j.immuni.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 8.Ma E.S. Recurrent cytogenetic abnormalities in Non-Hodgkin’s lymphoma and chronic lymphocytic leukemia. Methods Mol. Biol. 2017;1541:279–293. doi: 10.1007/978-1-4939-6703-2_22. [DOI] [PubMed] [Google Scholar]
- 9.Bödör C., Reiniger L. Catalog of genetic progression of human cancers: Non-Hodgkin lymphoma. Cancer Metastasis Rev. 2016;35:109–127. doi: 10.1007/s10555-016-9608-2. [DOI] [PubMed] [Google Scholar]
- 10.Bürglin T.R., Affolter M. Homeodomain proteins: An update. Chromosoma. 2016;125:497–521. doi: 10.1007/s00412-015-0543-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim Y., Nirenberg M. Drosophila NK-homeobox genes. Proc. Natl. Acad. Sci. USA. 1989;86:7716–7720. doi: 10.1073/pnas.86.20.7716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pollard S.L., Holland P.W. Evidence for 14 homeobox gene clusters in human genome ancestry. Curr. Biol. 2000;10:1059–1062. doi: 10.1016/S0960-9822(00)00676-X. [DOI] [PubMed] [Google Scholar]
- 13.Smith S.T., Jaynes J.B. A conserved region of engrailed, shared among all en-, gsc-, Nk1-, Nk2- and msh-class homeoproteins, mediates active transcriptional repression in vivo. Development. 1996;122:3141–3150. doi: 10.1242/dev.122.10.3141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nagel S., Venturini L., Przybylski G.K., Grabarczyk P., Meyer C., Kaufmann M., Battmer K., Schmidt C.A., Drexler H.G., Scherr M., et al. NK-like homeodomain proteins activate NOTCH3-signaling in leukemic T-cells. BMC Cancer. 2009;9:371. doi: 10.1186/1471-2407-9-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jennings B.H., Ish-Horowicz D. The Groucho/TLE/Grg family of transcriptional co-repressors. Genome Biol. 2008;9:205. doi: 10.1186/gb-2008-9-1-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garcia-Fernàndez J. The genesis and evolution of homeobox gene clusters. Nat. Rev. Genet. 2005;6:881–892. doi: 10.1038/nrg1723. [DOI] [PubMed] [Google Scholar]
- 17.Holland P.W., Booth H.A., Bruford E.A. Classification and nomenclature of all human homeobox genes. BMC Biol. 2007;5:47. doi: 10.1186/1741-7007-5-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nagel S., Kaufmann M., Drexler H.G., MacLeod R.A. The cardiac homeobox gene NKX2-5 is deregulated by juxtaposition with BCL11B in pediatric T-ALL cell lines via a novel t(5;14)(q35.1;q32.2) Cancer Res. 2003;63:5329–5334. [PubMed] [Google Scholar]
- 19.Hatano M., Roberts C.W., Minden M., Crist W.M., Korsmeyer S.J. Deregulation of a homeobox gene, HOX11, by the t (10;14) in T cell leukemia. Science. 1991;253:79–82. doi: 10.1126/science.1676542. [DOI] [PubMed] [Google Scholar]
- 20.Bernard O.A., Busson-LeConiat M., Ballerini P., Mauchauffé M., Della Valle V., Monni R., Nguyen Khac F., Mercher T., Penard-Lacronique V., Pasturaud P., et al. A new recurrent and specific cryptic translocation, t (5;14)(q35;q32), is associated with expression of the Hox11L2 gene in T acute lymphoblastic leukemia. Leukemia. 2001;15:1495–1504. doi: 10.1038/sj.leu.2402249. [DOI] [PubMed] [Google Scholar]
- 21.MacLeod R.A., Nagel S., Kaufmann M., Janssen J.W., Drexler H.G. Activation of HOX11L2 by juxtaposition with 3′-BCL11B in an acute lymphoblastic leukemia cell line (HPB-ALL) with t (5;14)(q35;q32.2) Genes Chromosomes Cancer. 2003;37:84–91. doi: 10.1002/gcc.10194. [DOI] [PubMed] [Google Scholar]
- 22.Nagel S., Pommerenke C., Scherr M., Meyer C., Kaufmann M., Battmer K., MacLeod R.A., Drexler H.G. NKL homeobox gene activities in hematopoietic stem cells, T-cell development and T-cell leukemia. PLoS ONE. 2017;12:e0171164. doi: 10.1371/journal.pone.0171164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Villarese P., Lours C., Trinquand A., Le Noir S., Belhocine M., Lhermitte L., Cieslak A., Tesio M., Petit A., LeLorch M., et al. TCRα rearrangements identify a subgroup of NKL-deregulated adult T-ALLs associated with favorable outcome. Leukemia. 2018;32:61–71. doi: 10.1038/leu.2017.176. [DOI] [PubMed] [Google Scholar]
- 24.Nagel S., Ehrentraut S., Meyer C., Kaufmann M., Drexler H.G., MacLeod R.A. Repressed BMP signaling reactivates NKL homeobox gene MSX1 in a T-ALL subset. Leuk. Lymphoma. 2015;56:480–491. doi: 10.3109/10428194.2014.924119. [DOI] [PubMed] [Google Scholar]
- 25.Homminga I., Pieters R., Langerak A.W., De Rooi J.J., Stubbs A., Verstegen M., Vuerhard M., Buijs-Gladdines J., Kooi C., Klous P., et al. Integrated transcript and genome analyses reveal NKX2-1 and MEF2C as potential oncogenes in T cell acute lymphoblastic leukemia. Cancer Cell. 2011;19:484–497. doi: 10.1016/j.ccr.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 26.Soulier J., Clappier E., Cayuela J.M., Regnault A., García-Peydró M., Dombret H., Baruchel A., Toribio M.L., Sigaux F. HOXA genes are included in genetic and biologic networks defining human acute T-cell leukemia (T-ALL) Blood. 2005;106:274–286. doi: 10.1182/blood-2004-10-3900. [DOI] [PubMed] [Google Scholar]
- 27.Kusy S., Gerby B., Goardon N., Gault N., Ferri F., Gérard D., Armstrong F., Ballerini P., Cayuela J.M., Baruchel A., et al. NKX3.1 is a direct TAL1 target gene that mediates proliferation of TAL1-expressing human T cell acute lymphoblastic leukemia. J. Exp. Med. 2010;207:2141–2156. doi: 10.1084/jem.20100745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nagel S., Ehrentraut S., Tomasch J., Lienenklaus S., Schneider B., Geffers R., Meyer C., Kaufmann M., Drexler H.G., MacLeod R.A. Transcriptional activation of prostate specific homeobox gene NKX3-1 in subsets of T-cell lymphoblastic leukemia (T-ALL) PLoS ONE. 2012;7:e40747. doi: 10.1371/journal.pone.0040747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nagel S., Meyer C., Kaufmann M., Zaborski M., MacLeod R.A.F., Drexler H.G. Aberrant activity of NKL homeobox gene NKX3-2 in a T-ALL subset. PLoS ONE. 2018;13:e0197194. doi: 10.1371/journal.pone.0197194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nagel S., Ehrentraut S., Tomasch J., Quentmeier H., Meyer C., Kaufmann M., Drexler H.G., MacLeod R.A. Ectopic expression of homeobox gene NKX2-1 in diffuse large B-cell lymphoma is mediated by aberrant chromatin modifications. PLoS ONE. 2013;8:61447. doi: 10.1371/annotation/3989404d-132f-4f07-a39e-c060d9094611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nagel S., Pommerenke C., MacLeod R.A.F., Meyer C., Kaufmann M., Fähnrich S., Drexler H.G. Deregulated expression of NKL homeobox genes in T-cell lymphomas. Oncotarget. 2019;10:3227–3247. doi: 10.18632/oncotarget.26929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kasahara H., Bartunkova S., Schinke M., Tanaka M., Izumo S. Cardiac and extracardiac expression of Csx/Nkx2.5 homeodomain protein. Circ. Res. 1998;82:936–946. doi: 10.1161/01.RES.82.9.936. [DOI] [PubMed] [Google Scholar]
- 33.Nagel S., Pommerenke C., Meyer C., Kaufmann M., Drexler H.G., MacLeod R.A. Deregulation of polycomb repressor complex 1 modifier AUTS2 in T-cell leukemia. Oncotarget. 2016;7:45398–45413. doi: 10.18632/oncotarget.9982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nagel S., Pommerenke C., Meyer C., Kaufmann M., MacLeod R.A.F., Drexler H.G. NKL homeobox gene MSX1 acts like a tumor suppressor in NK-cell leukemia. Oncotarget. 2017;8:66815–66832. doi: 10.18632/oncotarget.18609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allen J.D., Lints T., Jenkins N.A., Copeland N.G., Strasser A., Harvey R.P., Adams J.M. Novel murine homeo box gene on chromosome 1 expressed in specific hematopoietic lineages and during embryogenesis. Genes Dev. 1991;5:509–520. doi: 10.1101/gad.5.4.509. [DOI] [PubMed] [Google Scholar]
- 36.Lewis K.E. How do genes regulate simple behaviours? Understanding how different neurons in the vertebrate spinal cord are genetically specified. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2006;361:45–66. doi: 10.1098/rstb.2005.1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Depew M.J., Simpson C.A., Morasso M., Rubenstein J.L. Reassessing the Dlx code: The genetic regulation of branchial arch skeletal pattern and development. J. Anat. 2005;207:501–561. doi: 10.1111/j.1469-7580.2005.00487.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McCollum M.A., Sharpe P.T. Developmental genetics and early hominid craniodental evolution. Bioessays. 2001;23:481–493. doi: 10.1002/bies.1068. [DOI] [PubMed] [Google Scholar]
- 39.Nagel S., MacLeod R.A.F., Meyer C., Kaufmann M., Drexler H.G. NKL homeobox gene activities in B-cell development and lymphomas. PLoS ONE. 2018;13:e0205537. doi: 10.1371/journal.pone.0205537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Crompton M.R., Bartlett T.J., MacGregor A.D., Manfioletti G., Buratti E., Giancotti V., Goodwin G.H. Identification of a novel vertebrate homeobox gene expressed in haematopoietic cells. Nucleic Acids Res. 1992;20:5661–5667. doi: 10.1093/nar/20.21.5661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bedford F.K., Ashworth A., Enver T., Wiedemann L.M. HEX: A novel homeobox gene expressed during haematopoiesis and conserved between mouse and human. Nucleic Acids Res. 1993;21:1245–1249. doi: 10.1093/nar/21.5.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Manfioletti G., Gattei V., Buratti E., Rustighi A., De Iuliis A., Aldinucci D., Goodwin G.H., Pinto A. Differential expression of a novel proline-rich homeobox gene (Prh) in human hematolymphopoietic cells. Blood. 1995;85:1237–1245. doi: 10.1182/blood.V85.5.1237.bloodjournal8551237. [DOI] [PubMed] [Google Scholar]
- 43.Mack D.L., Leibowitz D.S., Cooper S., Ramsey H., Broxmeyer H.E., Hromas R. Down-regulation of the myeloid homeobox protein Hex is essential for normal T-cell development. Immunology. 2002;107:444–451. doi: 10.1046/j.1365-2567.2002.01523.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bogue C.W., Zhang P.X., McGrath J., Jacobs H.C., Fuleihan R.L. Impaired B cell development and function in mice with a targeted disruption of the homeobox gene Hex. Proc. Natl. Acad. Sci. USA. 2003;100:556–561. doi: 10.1073/pnas.0236979100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jackson J.T., Nasa C., Shi W., Huntington N.D., Bogue C.W., Alexander W.S., McCormack M.P. A crucial role for the homeodomain transcription factor Hhex in lymphopoiesis. Blood. 2015;125:803–814. doi: 10.1182/blood-2014-06-579813. [DOI] [PubMed] [Google Scholar]
- 46.Allen J.D., Adams J.M. Enforced expression of Hlx homeobox gene prompts myeloid cell maturation and altered adherence properties of T cells. Blood. 1993;81:3242–3251. doi: 10.1182/blood.V81.12.3242.3242. [DOI] [PubMed] [Google Scholar]
- 47.Allen J.D., Harris A.W., Bath M.L., Strasser A., Scollay R., Adams J.M. Perturbed development of T and B cells in mice expressing an Hlx homeobox transgene. J. Immunol. 1995;154:1531–1542. [PubMed] [Google Scholar]
- 48.Mullen A.C., Hutchins A.S., High F.A., Lee H.W., Sykes K.J., Chodosh L.A., Reiner S.L. Hlx is induced by and genetically interacts with T-bet to promote heritable T (H) 1 gene induction. Nat. Immunol. 2002;3:652–658. doi: 10.1038/ni807. [DOI] [PubMed] [Google Scholar]
- 49.Zheng W.P., Zhao Q., Zhao X., Li B., Hubank M., Schatz D.G., Flavell R.A. Up-regulation of Hlx in immature Th cells induces IFN-gamma expression. J. Immunol. 2004;172:114–122. doi: 10.4049/jimmunol.172.1.114. [DOI] [PubMed] [Google Scholar]
- 50.Becknell B., Hughes T.L., Freud A.G., Blaser B.W., Yu J., Trotta R., Mao H.C., Caligiuri de Jesús M.L., Alghothani M., Benson D.M., Jr., et al. Hlx homeobox transcription factor negatively regulates interferon-gamma production in monokine-activated natural killer cells. Blood. 2007;109:2481–2487. doi: 10.1182/blood-2006-10-050096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Keng V.W., Fujimori K.E., Myint Z., Tamamaki N., Nojyo Y., Noguchi T. Expression of Hex mRNA in early murine postimplantation embryo development. FEBS Lett. 1998;426:183–186. doi: 10.1016/S0014-5793(98)00342-1. [DOI] [PubMed] [Google Scholar]
- 52.Bort R., Signore M., Tremblay K., Martinez Barbera J.P., Zaret K.S. Hex homeobox gene controls the transition of the endoderm to a pseudostratified, cell emergent epithelium for liver bud development. Dev. Biol. 2006;290:44–56. doi: 10.1016/j.ydbio.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 53.Bogue C.W., Ganea G.R., Sturm E., Ianucci R., Jacobs H.C. Hex expression suggests a role in the development and function of organs derived from foregut endoderm. Dev. Dyn. 2000;219:84–89. doi: 10.1002/1097-0177(2000)9999:9999<::AID-DVDY1028>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 54.Gauvrit S., Villasenor A., Strilic B., Kitchen P., Collins M.M., Marín-Juez R., Guenther S., Maischein H.M., Fukuda N., Canham M.A., et al. HHEX is a transcriptional regulator of the VEGFC/FLT4/PROX1 signaling axis during vascular development. Nat. Commun. 2018;9:2704. doi: 10.1038/s41467-018-05039-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Puppin C., Puglisi F., Pellizzari L., Manfioletti G., Pestrin M., Pandolfi M., Piga A., Di Loreto C., Damante G. HEX expression and localization in normal mammary gland and breast carcinoma. BMC Cancer. 2006;6:192. doi: 10.1186/1471-2407-6-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kershaw R.M., Roberts D., Wragg J., Shaaban A.M., Humphreys E., Halsall J., Price L., Bicknell R., Gaston K., Jayaraman P.S. Proline-Rich Homeodomain protein (PRH/HHEX) is a suppressor of breast tumour growth. Oncogenesis. 2017;6:e346. doi: 10.1038/oncsis.2017.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rankin S.A., Kormish J., Kofron M., Jegga A., Zorn A.M. A gene regulatory network controlling hhex transcription in the anterior endoderm of the organizer. Dev. Biol. 2011;351:297–310. doi: 10.1016/j.ydbio.2010.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lints T.J., Hartley L., Parsons L.M., Harvey R.P. Mesoderm-specific expression of the divergent homeobox gene Hlx during murine embryogenesis. Dev. Dyn. 1996;205:457–470. doi: 10.1002/(SICI)1097-0177(199604)205:4<457::AID-AJA9>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 59.Huang L., Pan D., Chen Q., Zhu L.J., Ou J., Wabitsch M., Wang Y.X. Transcription factor Hlx controls a systematic switch from white to brown fat through Prdm16-mediated co-activation. Nat. Commun. 2017;8:68. doi: 10.1038/s41467-017-00098-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yuen N., Brennecke S.P., Umstad M.P., Yong H.E.J., Borg A.J., Rajaraman G., Kalionis B., Murthi P. Expression of homeobox gene HLX and its downstream target genes are altered in placentae from discordant twin pregnancies. Twin Res. Hum. Genet. 2018;21:42–50. doi: 10.1017/thg.2017.66. [DOI] [PubMed] [Google Scholar]
- 61.Cao L., Gibson J.D., Miyamoto S., Sail V., Verma R., Rosenberg D.W., Nelson C.E., Giardina C. Intestinal lineage commitment of embryonic stem cells. Differentiation. 2011;81:1–10. doi: 10.1016/j.diff.2010.09.182. [DOI] [PubMed] [Google Scholar]
- 62.Yamakawa T., Sato Y., Matsumura Y., Kobayashi Y., Kawamura Y., Goshima N., Yamanaka S., Okita K. Screening of human cDNA library reveals two differentiation-related genes, HHEX and HLX, as promoters of early phase reprogramming toward pluripotency. Stem. Cells. 2016;34:2661–2669. doi: 10.1002/stem.2436. [DOI] [PubMed] [Google Scholar]
- 63.Pla P., Monsoro-Burq A.H. The neural border: Induction, specification and maturation of the territory that generates neural crest cells. Dev Biol. 2018;444:S36–S46. doi: 10.1016/j.ydbio.2018.05.018. [DOI] [PubMed] [Google Scholar]
- 64.Li Y., Zhao D., Horie T., Chen G., Bao H., Chen S., Liu W., Horie R., Liang T., Dong B., et al. Conserved gene regulatory module specifies lateral neural borders across bilaterians. Proc. Natl. Acad. Sci. USA. 2017;114:E6352–E6360. doi: 10.1073/pnas.1704194114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Maharana S.K., Schlosser G. A gene regulatory network underlying the formation of pre-placodal ectoderm in Xenopus laevis. BMC Biol. 2018;16:79. doi: 10.1186/s12915-018-0540-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schlosser G., Ahrens K. Molecular anatomy of placode development in Xenopus laevis. Dev. Biol. 2004;271:439–466. doi: 10.1016/j.ydbio.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 67.Phan M., Conte F., Khandelwal K.D., Ockeloen C.W., Bartzela T., Kleefstra T., Van Bokhoven H., Rubini M., Zhou H., Carels C.E. Tooth agenesis and orofacial clefting: Genetic brothers in arms? Hum. Genet. 2016;135:1299–1327. doi: 10.1007/s00439-016-1733-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lan Y., Jia S., Jiang R. Molecular patterning of the mammalian dentition. Semin. Cell Dev. Biol. 2014;25–26:61–70. doi: 10.1016/j.semcdb.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ishii M., Han J., Yen H.Y., Sucov H.M., Chai Y., Maxson R.E., Jr. Combined deficiencies of Msx1 and Msx2 cause impaired patterning and survival of the cranial neural crest. Development. 2005;132:4937–4950. doi: 10.1242/dev.02072. [DOI] [PubMed] [Google Scholar]
- 70.Bach A., Lallemand Y., Nicola M.A., Ramos C., Mathis L., Maufras M., Robert B. Msx1 is required for dorsal diencephalon patterning. Development. 2003;130:4025–4036. doi: 10.1242/dev.00609. [DOI] [PubMed] [Google Scholar]
- 71.Ramos C., Robert B. msh/Msx gene family in neural development. Trends Genet. 2005;21:624–632. doi: 10.1016/j.tig.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 72.Friedmann Y., Daniel C.W. Regulated expression of homeobox genes Msx-1 and Msx-2 in mouse mammary gland development suggests a role in hormone action and epithelial-stromal interactions. Dev. Biol. 1996;177:347–355. doi: 10.1006/dbio.1996.0168. [DOI] [PubMed] [Google Scholar]
- 73.Hughes S.M. Muscle development: Reversal of the differentiated state. Curr. Biol. 2001;11:R237–R239. doi: 10.1016/S0960-9822(01)00114-2. [DOI] [PubMed] [Google Scholar]
- 74.Odelberg S.J., Kollhoff A., Keating M.T. Dedifferentiation of mammalian myotubes induced by msx1. Cell. 2000;103:1099–1109. doi: 10.1016/S0092-8674(00)00212-9. [DOI] [PubMed] [Google Scholar]
- 75.Yoon J.H., Choi W.S., Kim O., Choi S.S., Lee E.K., Nam S.W., Lee J.Y., Park W.S. NKX6.3 controls gastric differentiation and tumorigenesis. Oncotarget. 2015;6:28425–28439. doi: 10.18632/oncotarget.4952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yoon J.H., Kim O., Eun J.W., Choi S.S., Ashktorab H., Smoot D.T., Nam S.W., Park W.S. Multiple genetic mutations caused by NKX6.3 depletion contribute to gastric tumorigenesis. Sci. Rep. 2018;8:17609. doi: 10.1038/s41598-018-35733-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hafler B.P., Choi M.Y., Shivdasani R.A., Rowitch D.H. Expression and function of Nkx6.3 in vertebrate hindbrain. Brain Res. 2008;1222:42–50. doi: 10.1016/j.brainres.2008.04.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang Z., Shi Y., Zhao S., Li J., Li C., Mao B. Xenopus Nkx6.3 is a neural plate border specifier required for neural crest development. PLoS ONE. 2014;9:e115165. doi: 10.1371/journal.pone.0115165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Carroll S.B. Evo-devo and an expanding evolutionary synthesis: A genetic theory of morphological evolution. Cell. 2008;134:25–36. doi: 10.1016/j.cell.2008.06.030. [DOI] [PubMed] [Google Scholar]
- 80.Tanaka M., Chen Z., Bartunkova S., Yamasaki N., Izumo S. The cardiac homeobox gene Csx/Nkx2.5 lies genetically upstream of multiple genes essential for heart development. Development. 1999;126:1269–1280. doi: 10.1242/dev.126.6.1269. [DOI] [PubMed] [Google Scholar]
- 81.Koss M., Bolze A., Brendolan A., Saggese M., Capellini T.D., Bojilova E., Boisson B., Prall O.W., Elliott D.A., Solloway M., et al. Congenital asplenia in mice and humans with mutations in a Pbx/Nkx2-5/p15 module. Dev. Cell. 2012;22:913–926. doi: 10.1016/j.devcel.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nagel S., Meyer C., Quentmeier H., Kaufmann M., Drexler H.G., MacLeod R.A. MEF2C is activated by multiple mechanisms in a subset of T-acute lymphoblastic leukemia cell lines. Leukemia. 2008;22:600–607. doi: 10.1038/sj.leu.2405067. [DOI] [PubMed] [Google Scholar]
- 83.Nagel S., Venturini L., Meyer C., Kaufmann M., Scherr M., Drexler H.G., Macleod R.A. Transcriptional deregulation of oncogenic myocyte enhancer factor 2C in T-cell acute lymphoblastic leukemia. Leuk. Lymphoma. 2011;52:290–297. doi: 10.3109/10428194.2010.537003. [DOI] [PubMed] [Google Scholar]
- 84.Bradner J.E., Hnisz D., Young R.A. Transcriptional Addiction in Cancer. Cell. 2017;168:629–643. doi: 10.1016/j.cell.2016.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.O’Neil J., Look A.T. Mechanisms of transcription factor deregulation in lymphoid cell transformation. Oncogene. 2007;26:6838–6849. doi: 10.1038/sj.onc.1210766. [DOI] [PubMed] [Google Scholar]
- 86.Eswaran J., Sinclair P., Heidenreich O., Irving J., Russell L.J., Hall A., Calado D.P., Harrison C.J., Vormoor J. The pre-B-cell receptor checkpoint in acute lymphoblastic leukaemia. Leukemia. 2015;29:1623–1631. doi: 10.1038/leu.2015.113. [DOI] [PubMed] [Google Scholar]
- 87.Tomolonis J.A., Agarwal S., Shohet J.M. Neuroblastoma pathogenesis: Deregulation of embryonic neural crest development. Cell Tissue Res. 2018;372:245–262. doi: 10.1007/s00441-017-2747-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ferrando A.A., Neuberg D.S., Staunton J., Loh M.L., Huard C., Raimondi S.C., Behm F.G., Pui C.H., Downing J.R., Gilliland D.G., et al. Gene expression signatures define novel oncogenic pathways in T cell acute lymphoblastic leukemia. Cancer Cell. 2002;1:75–87. doi: 10.1016/S1535-6108(02)00018-1. [DOI] [PubMed] [Google Scholar]
- 89.Nagel S., Pommerenke C., Meyer C., Kaufmann M., MacLeod R.A.F., Drexler H.G. Aberrant expression of NKL homeobox gene HLX in Hodgkin lymphoma. Oncotarget. 2018;9:14338–14353. doi: 10.18632/oncotarget.24512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.ENCODE Project Consortium An integrated encyclopedia of DNA elements in the human genome. Nature. 2012;489:57–74. doi: 10.1038/nature11247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lee H., Habas R., Abate-Shen C. MSX1 cooperates with histone H1b for inhibition of transcription and myogenesis. Science. 2004;304:1675–1678. doi: 10.1126/science.1098096. [DOI] [PubMed] [Google Scholar]
- 92.Nagel S., Schneider B., Meyer C., Kaufmann M., Drexler H.G., Macleod R.A. Transcriptional deregulation of homeobox gene ZHX2 in Hodgkin lymphoma. Leuk. Res. 2012;36:646–655. doi: 10.1016/j.leukres.2011.10.019. [DOI] [PubMed] [Google Scholar]
- 93.Park J., Park K., Kim S., Lee J.H. Msx1 gene overexpression induces G1 phase cell arrest in human ovarian cancer cell line OVCAR3. Biochem. Biophys. Res. Commun. 2001;281:1234–1240. doi: 10.1006/bbrc.2001.4474. [DOI] [PubMed] [Google Scholar]
- 94.Hu G., Lee H., Price S.M., Shen M.M., Abate-Shen C. Msx homeobox genes inhibit differentiation through upregulation of cyclin D1. Development. 2001;128:2373–2384. doi: 10.1242/dev.128.12.2373. [DOI] [PubMed] [Google Scholar]
- 95.Nagel S., Ehrentraut S., Meyer C., Kaufmann M., Drexler H.G., MacLeod R.A. Oncogenic deregulation of NKL homeobox gene MSX1 in mantle cell lymphoma. Leuk. Lymphoma. 2014;55:1893–1903. doi: 10.3109/10428194.2013.864762. [DOI] [PubMed] [Google Scholar]
- 96.Lazzaro D., Price M., De Felice M., Di Lauro R. The transcription factor TTF-1 is expressed at the onset of thyroid and lung morphogenesis and in restricted regions of the foetal brain. Development. 1991;113:1093–1104. doi: 10.1242/dev.113.4.1093. [DOI] [PubMed] [Google Scholar]
- 97.Nagel S., MacLeod R.A.F., Pommerenke C., Meyer C., Kaufmann M., Drexler H.G. NKL homeobox gene NKX2-2 is aberrantly expressed in Hodgkin lymphoma. Oncotarget. 2018;9:37480–37496. doi: 10.18632/oncotarget.26459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Barth K.A., Wilson S.W. Expression of zebrafish nk2.2 is influenced by sonic hedgehog/vertebrate hedgehog-1 and demarcates a zone of neuronal differentiation in the embryonic forebrain. Development. 1995;121:1755–1768. doi: 10.1242/dev.121.6.1755. [DOI] [PubMed] [Google Scholar]
- 99.Sussel L., Kalamaras J., Hartigan-O’Connor D.J., Meneses J.J., Pedersen R.A., Rubenstein J.L., German M.S. Mice lacking the homeodomain transcription factor Nkx2.2 have diabetes due to arrested differentiation of pancreatic beta cells. Development. 1998;125:2213–2221. doi: 10.1242/dev.125.12.2213. [DOI] [PubMed] [Google Scholar]
- 100.Pabst O., Zweigerdt R., Arnold H.H. Targeted disruption of the homeobox transcription factor Nkx2-3 in mice results in postnatal lethality and abnormal development of small intestine and spleen. Development. 1999;126:2215–2225. doi: 10.1242/dev.126.10.2215. [DOI] [PubMed] [Google Scholar]
- 101.Robles E.F., Mena-Varas M., Barrio L., Merino-Cortes S.V., Balogh P., Du M.Q., Akasaka T., Parker A., Roa S., Panizo C., et al. Homeobox NKX2-3 promotes marginal-zone lymphomagenesis by activating B-cell receptor signalling and shaping lymphocyte dynamics. Nat. Commun. 2016;7:11889. doi: 10.1038/ncomms11889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Vojkovics D., Kellermayer Z., Kajtár B., Roncador G., Vincze Á., Balogh P. Nkx2-3-A slippery slope from development through inflammation toward hematopoietic malignancies. Biomark. Insights. 2018;13:1–6. doi: 10.1177/1177271918757480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Nagel S., Uphoff C.C., Dirks W.G., Pommerenke C., Meyer C., Drexler H.G. Epstein-Barr virus (EBV) activates NKL homeobox gene HLX in DLBCL. PLoS ONE. 2019;14:e0216898. doi: 10.1371/journal.pone.0216898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Shannon-Lowe C., Rickinson A.B., Bell A.I. Epstein-Barr virus-associated lymphomas. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2017;372:1732. doi: 10.1098/rstb.2016.0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jones F.S., Kioussi C., Copertino D.W., Kallunki P., Holst B.D., Edelman G.M. Barx2, a new homeobox gene of the Bar class, is expressed in neural and craniofacial structures during development. Proc. Natl. Acad. Sci. USA. 1997;94:2632–2637. doi: 10.1073/pnas.94.6.2632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Naka T., Yokose S. Immunohistochemical localization of barx2 in the developing fetal mouse submandibular glands. Acta Histochem. Cytochem. 2009;42:47–53. doi: 10.1267/ahc.08027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sellar G.C., Li L., Watt K.P., Nelkin B.D., Rabiasz G.J., Stronach E.A., Miller E.P., Porteous D.J., Smyth J.F., Gabra H. BARX2 induces cadherin 6 expression and is a functional suppressor of ovarian cancer progression. Cancer Res. 2001;61:6977–6981. [PubMed] [Google Scholar]
- 108.Quentmeier H., Pommerenke C., Dirks W.G., Eberth S., Koeppel M., MacLeod R.A.F., Nagel S., Steube K., Uphoff C.C., Drexler H.G. The LL-100 panel: 100 cell lines for blood cancer studies. Sci. Rep. 2019;9:8218. doi: 10.1038/s41598-019-44491-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Drexler H.G. Guide to Leukemia-Lymphoma Cell Lines. 2nd ed. DSMZ; Braunschweig, Germany: 2010. [Google Scholar]
- 110.Matsuo Y., Drexler H.G. Establishment and characterization of human B cell precursor-leukemia cell lines. Leuk. Res. 1998;22:567–579. doi: 10.1016/S0145-2126(98)00050-2. [DOI] [PubMed] [Google Scholar]
- 111.Drexler H.G., Matsuo Y. Malignant hematopoietic cell lines: In vitro models for the study of multiple myeloma and plasma cell leukemia. Leuk. Res. 2000;24:681–703. doi: 10.1016/S0145-2126(99)00195-2. [DOI] [PubMed] [Google Scholar]
- 112.Carbone A., Cesarman E., Gloghini A., Drexler H.G. Understanding pathogenetic aspects and clinical presentation of primary effusion lymphoma through its derived cell lines. AIDS. 2010;24:479–490. doi: 10.1097/QAD.0b013e3283365395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Drexler H.G., Ehrentraut S., Nagel S., Eberth S., MacLeod R.A. Malignant hematopoietic cell lines: In vitro models for the study of primary mediastinal B-cell lymphomas. Leuk. Res. 2015;39:18–29. doi: 10.1016/j.leukres.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 114.Drexler H.G., Eberth S., Nagel S., MacLeod R.A. Malignant hematopoietic cell lines: In vitro models for double-hit B-cell lymphomas. Leuk. Lymphoma. 2016;57:1015–1020. doi: 10.3109/10428194.2015.1108414. [DOI] [PubMed] [Google Scholar]
- 115.Drexler H.G., Pommerenke C., Eberth S., Nagel S. Hodgkin lymphoma cell lines: To separate the wheat from the chaff. Biol. Chem. 2018;399:511–523. doi: 10.1515/hsz-2017-0321. [DOI] [PubMed] [Google Scholar]