Abstract
Prostate cancer affects African Americans disproportionately by exhibiting greater incidence, rapid disease progression, and higher mortality when compared to their Caucasian counterparts. Additionally, standard treatment interventions do not achieve similar outcome in African Americans compared to Caucasian Americans, indicating differences in host factors contributing to racial disparity. African Americans have allelic variants and hyper-expression of genes that often lead to an immunosuppressive tumor microenvironment, possibly contributing to more aggressive tumors and poorer disease and therapeutic outcomes than Caucasians. In this review, we have discussed race-specific differences in external factors impacting internal milieu, which modify immunological topography as well as contribute to disparity in prostate cancer.
Keywords: racial disparity, immunity, African American, Caucasian
1. Introduction
Cancer-associated racial disparities have been recognized by the scientific community since the early 1970s. African Americans (AAs) are more likely to develop cancer and show worse prognosis compared to Caucasian Americans (CAs) [1,2]. Differences in the incidence and outcome of cancer among different ethnicities add a layer to an already complex disease. The fact that standard treatment options offered in clinics fail to provide similar outcomes in different ethnic groups suggests that differences in the biology of cancer contribute to racial disparities in therapeutic outcome. Moreover, several inter-related factors, such as socio-economic status (SES), lifestyle, and various cultural aspects influence biology and physiology. These factors together affect the probability and course of disease progression, while differences in these aspects maintain race-specific gaps in incidence, progression and therapeutic outcomes of cancer. Intriguingly, even after normalizing for the socio-economic factors and healthcare inequalities, racial disparities in disease and therapeutic outcome exist.
Studies have shown that Gleason score and levels of prostate specific antigen (PSA), a biomarker for prostate cancer [2,3,4], may be higher in AA prostate cancer (PCa) patients in comparison to their CA counterparts. Metastatic progression [5] and recurrence [6] is higher in AA men in comparison to other Americans. In addition, localized advanced stage PCa is potentially more aggressive in AA men in comparison to CA [7]. They are two times more likely to die of PCa than CA men [1,8]. In 2019, 202,260 new cases and 73,030 cancer-related deaths were expected to occur among AAs, with PCa being the most common cancer among AA men [1]. This disparity in mortality increases to greater than fourfold in younger men [8]. Furthermore, AA men are more likely to be diagnosed at a younger age than CA man [8,9]. Post-treatment progression-free survival is shorter in AA in comparison to CA [10]. Even after prostatectomy, AA patients have a lower three-year disease-free survival rate than CA men [2]. Worldwide incidence of PCa has been suggested to be highest in African and Jamaican men [11,12]; therefore, this observed disparity is likely attributed to predisposed genetic susceptibility.
This emphasizes the significance of addressing the differences in host factors in improving our understanding of this multifactorial issue. Studies related to HIV, birth outcomes and graft/transplant have suggested immunological differences among AAs and CAs [13,14,15,16,17,18]. Immunology and oncology have a longstanding relationship. Therefore, in this review, we discuss the race specific differences in host factors, which define the immunological landscape in PCa, and their impact on PCa racial disparity.
1.1. Immune System and Cancer
Genetic diversity in the world’s population is largely attributable to geographic differentials in allele frequencies [19,20]. Populations of African descent have more nucleotide diversity and rare alleles when compared to populations of European and Asian decent [20]. Specifically, immune adaptations suited to ancestral environments influence cancer risk between AAs and CAs [21,22], implying that the erosion in adaptive and innate immune surveillance could be a key player in PCa disparity.
1.2. Innate and Adaptive Immune Surveillance
Hosts’ internal defense systems consist of innate and adaptive immune responses. The innate response is immediate, less specific, and is followed by the antigen-specific adaptive response [23]. Complement systems function to remove infectious particles out of the body and bridges the innate and adaptive arms of the immune system [24,25,26]. This intricate system orchestrates the anti-tumorigenic actions by direct elimination of tumor cells based on the expression of tumor-specific antigens (TSAs) and by suppression of viral infections protecting the host from virus-induced tumors [27]. It prevents formation of an inflammatory microenvironment conducive for tumorigenesis (acute inflammation is a characteristic of cancer) [28,29,30,31]. Compelling evidence using carcinogen-induced and spontaneous cancer in immune-deficient mice suggests synergistic involvement of both innate and adaptive immune systems in preventing cancer development [32,33,34,35]. Simply put, developing (non-syngeneic) tumors in immune competent hosts is very difficult, and immunosurveillance is the most important process by which a healthy host gets rid of transformed cells.
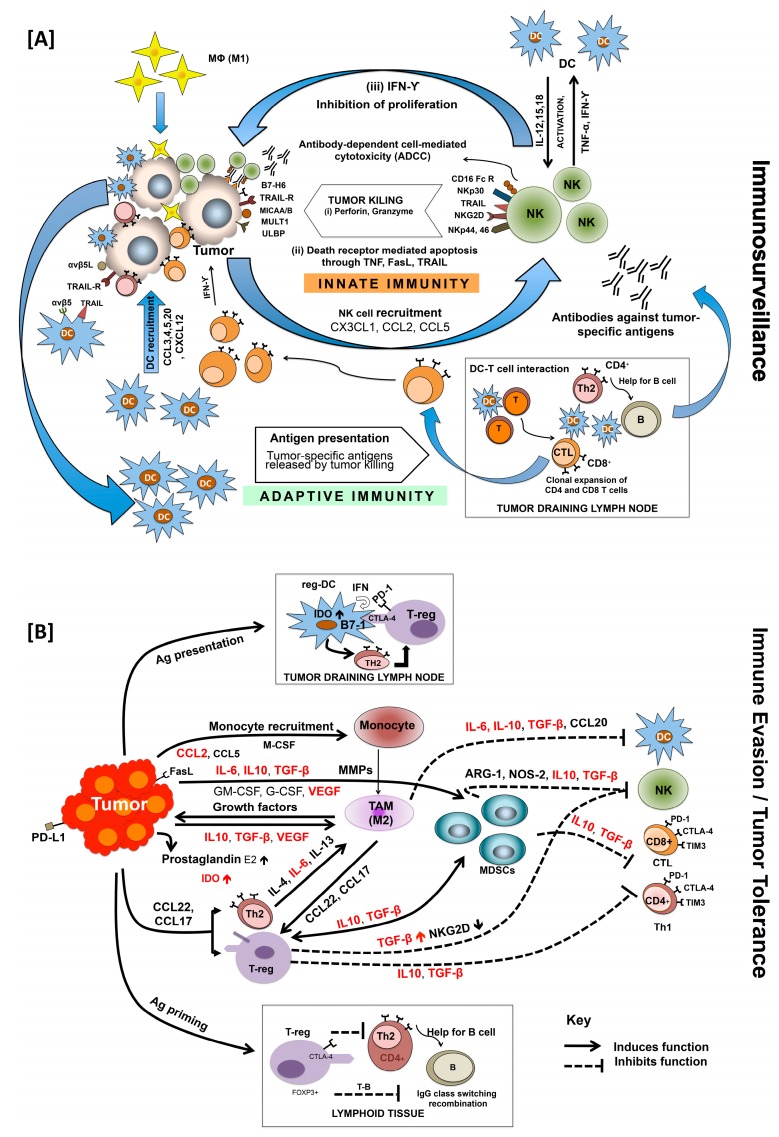
Natural killer (NK) cells are among the first innate immune cells that respond to inflammation and cancer. Activated NK cells eliminate target cancer cells by either secreting perforin or granzyme or by apoptosis mediated through interaction of TNF, FasL, and TRAIL with corresponding death receptors (Figure 1A) [36]. Activation of NK cell depends on the balance of their activating (NKG2D) and inhibitory receptor (KIR). Cytokines, such as IL-2, IL-12, IL-15, IFN-α, and IFN-β, are required for NK cell activation [36,37]. Tumor cell killing by NK cells offers a TSA-enriched environment for dendritic cells (DCs), another subset of innate immunity that plays an important role in tumor cell clearance, either directly or through activation of adaptive immune responses. Several complementary mechanisms help DCs to capture NK cell-induced TSAs, which are then processed and bound to MHC-I/II molecules during their journey to draining lymph nodes (DLNs) [38]. Besides, TSAs can also directly reach lymph node-resident DCs through lymph [39]. These antigen-loaded lymph node-resident DCs are the first to present antigenic peptides to naïve CD4+ T-cells leading to T-cell priming and IL-2 production, facilitating their proliferation and expansion. Subsequently, activated DCs from peripheral tissues migrate to lymph nodes and interact with these activated CD4+ T-cells, facilitating their conversion to effector T-cells (Figure 1A). It is important to mention here that immature, non-activated DCs that present self-antigens to T-cells bring about immune tolerance by T-cell deletion or by suppressor T-cell differentiation [40]. Upon interaction with mature DCs, naïve CD4+ T-cells differentiate into effector T-cells that include T-helper (Th1, Th2, Th17 or T-follicular helper (Tfh)) cells. These cells help in differentiation of B-cells into antibody-secreting cells as well as in generation of regulatory T (Treg) cells. Naïve CD8+ T-cells, on the other hand, differentiate into effector cytotoxic T-lymphocytes (CTLs). Tissue-localized DCs can also be polarized into distinct effector phenotypes by interaction with other cells of innate immunity via the release of IFNs, TNFs, and other cytokines [41,42,43,44,45,46,47]. Much like DCs, macrophages are phagocytic cells that reside in many tissues, recognize TSAs, and produce high levels of cytokines including chemokines that function as the alert signals for the immune system [48]. Activation of innate immunity promotes various inflammatory reactions and triggers the release of inflammatory cytokines as well as other inflammatory mediators [48,49]. In context to cancer, there are reports suggesting anti- as well as pro-oncogenic roles of innate immunity. Contrary to the physiological role, a plethora of evidence suggests the role of the immune system in the establishment of tumor cells and their subsequent progression. This, however, is due to the manipulation of the immune system by transformed cells, their escape from immune surveillance, and which eventually makes the disease clinically significant [50]. All this raises questions regarding the effectiveness of immunity against spontaneously arising tumors, spiking interest in immunotherapy for cancer [51].
Figure 1.
Immunosurveillance, evasion, and tolerance in cancer. Innate and adaptive immune systems work in consortium to eliminate cancer cells before their clinical appearance (A). Innate immune cells (NK) interact with neoplastic cells through their surface receptors (NKG2D, NKp30, NKp44, NKp46, CD16) and kill them by (i) release of cytotoxic granules (perforin, granzyme) in the vicinity; (ii) death (TNF, FasL, TRAIL) receptor-mediated apoptosis; and (iii) secretion of IFN-ϒ which inhibits proliferation of tumor cells by activating M1 macrophages (Mϕ) and DCs as well as Th1 cells of adaptive immune system. Dendritic cells (DCs), recruited at the tumor site, present tumor-specific antigens released by tumor killing. Antigen presenting DCs interact with naive T-cells in tumor draining lymph nodes facilitating clonal expansion of CD4+ and CD8+ T-cells which then differentiate into antigen-specific effector T-cells: T-helper cells (Th1, Th2, Th17) and cytotoxic T-cell lymphocytes (CTL), respectively. DCs also control the humoral part of adaptive immunity either by directly interacting with B cells or through CD4+ helper T-cell by differentiating B cells into antibody secreting cells. In addition to immune surveillance failure, cancer progress by evading immune attack (B). Immune pressure selects poorly immunogenic tumor cells, not recognized by effector cells of innate and adaptive immunity. These immune-evasive cells modulate TME further to make it more immunosuppressive by activating accessory cells: regulatory T-cells (T-regs), tumor-associated macrophages (TAMs), regulatory dendritic cells (reg-DCs), and myeloid-derived suppressor cells (MDSCs). The combined activity of these immune suppressor cells regulates tumor growth, survival, migration, and invasion by changing the hormone, growth factor, and cytokine profile of TME. Levels of cytokines involved in immune suppression and evasion and which are higher in AA are highlighted in red.
1.3. Immunological Landscape and Cancer Progression
Cancer develops either by remaining less immunogenic and unnoticed or by bending the immune system for its benefit. This dynamic “cancer immune-editing” process is characterized by changes in the immunogenicity of tumor cells along with changes in the immunological landscape leading to escape from immune surveillance. Low antigen expression, recruitment of suppressive immune cells, and production of immune modulating factors, ultimately resulting in alteration of the immune microenvironment are some of the mechanisms by which tumors escape immune attack [24,25,26,52]. Cancer immunoediting begins with clonal selection of less immunogenic cancer cells while the innate and adaptive immune system eliminates the more immunogenic cells. This results in the immune selection of poorly immunogenic tumor cell variants and eventually supporting cancer progression by the following “immune sculpting” phase. During immuno-sculpting, selected cancer cells that are tolerant of immune attack, after exposure to the effector immune cells, steer the immune response by production of selective cytokines for recruitment of suppressive immune cells and facilitate proliferation after escaping elimination [53].
Myeloid-derived suppressor cells (MDSCs), regulatory T-cells (Treg/CD4+CD25+FOXP3+), and tumor-associated macrophages (TAMs) (Figure 1B) are tumor-modified immune cells that hinder the clearance of cancer cells locally and even in distant organs [53,54]. Myeloid-derived suppressor cells are composed of a heterogeneous population of immature myeloid cells that abrogate innate and adaptive immune responses [55,56,57,58]. Immature myeloid cells give rise to macrophages, DCs, and granulocytes, all of which are essential for normal function of the immune system; however, these cells can be converted into potent immune suppressors in a tumor microenvironment (TME) [59]. Expansion of a pool of immature myeloid cells is capable of inhibiting an antigen-specific CD8+ T-cell response in cancer patients and tumor-bearing mice [58]. Myeloid-derived suppressor cells suppress T-cell proliferation and cytotoxicity, induce the expansion of Tregs, and block NK cell activation by expressing suppressive factors such as arginase-1, ROS, and iNOS [60]. Treg cells are normally responsible for preventing excessive immune reactivity and maintaining the immune balance [60] but also support tumor progression [61]. They inhibit the activity of a variety of immune cells through contact-dependent mechanisms or by secreting immunosuppressive cytokines [60]. Tregs are capable of inhibiting the anti-cancer functions of T-cells [62], NK cells [62], and B-cells [63]. Additionally, TAMs are a subset of macrophages which play a significant role in tumor immune evasion, angiogenesis, and metastasis. Evidence suggests that macrophages polarize into immunosuppressive M2 macrophages upon exposure to M2 differentiation factors produced by the tumor immune microenvironment (TIME) [64]. These macrophage subset can contribute to cancer progression by producing soluble factors like TGF-β and IL-10 that promote tumor growth and/or help tumor cells evade from host immune surveillance [64,65,66,67,68,69]. Lastly, cancer-associated fibroblasts (CAFs), also known as activated fibroblasts, myofibroblasts, or tumor-associated fibroblasts, have been investigated for their pro-tumorigenic capabilities [70]. These cells have recently been reported to modulate the immune system through secretion of TGF-β and other immune suppressive cytokines, creating an immunosuppressive environment [70]. All these changes in the TIME are brought about by combined actions of hormones and cytokines secreted by different cells in and around the tumor.
1.4. Racial Differences in Hormonal Status Impacting Immune System and Prostate Cancer
Steroid hormones significantly affect immunity by regulating the activity of lymphocytes (T- and B-cells), monocytes, and NK cells [71]. In fact, there is a direct correlation between a healthy immune response and hormonal balance of the body. Interplay of sex hormones and immunity is well studied and is rendered responsible for sex-based differences in immune responses [72,73]. Thus, immune response against cancer is also highly influenced by hormonal milieu and vice versa.
Expression of androgen receptors (ARs) by various immune cell lineages [74,75,76] and the fact that androgen plays a major role in the regulation of both innate and adaptive immune response [77] implies that differences in androgen signaling could also lead to PCa disparity. It regulates the proliferation, maturation, function, and chemokine-mediated recruitment of neutrophils. Deficiency in ARs leads to significant neutropenia, while insufficient testosterone causes a mild reduction in neutrophils. Testosterone dampens the activation of macrophages and DCs as well as suppresses the production of pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) by these cells [77,78,79]. On the other hand, it promotes activation of regulatory MDSCs and Tregs [80]. Castration-based studies also revealed a significant increase in MHC-II expression and co-stimulatory molecules by cDCs (cytotoxic DC) [81]. Further, androgen deprivation causes thymic enlargement in males, facilitating an increased peripheral T-cell population [82,83,84,85,86,87].
The level of cytokines that governs the Th1:Th2 ratio determines the risk of several types of cancer. A higher Th1:Th2 ratio prevents tumor development, whereas a Th2 polarized immune system promotes tumor development. Androgen (testosterone) inhibits Th1 differentiation as well as production of pro-inflammatory cytokines (IFN-γ, TNF-α/β) and decreases IL-12-mediated induction of Th1 phenotype [88]. Th effect of androgen on Th1 differentiation is governed by upregulation of Ptpn1 (protein tyrosine phosphatase, non-receptor type 1) that is involved in IL-12-induced phosphorylation of STAT4 via inactivation of Jak2 and Tyk2 kinases [88,89]. PCa patients undergoing androgen ablation therapy have decreased expression of Ptpn1 in their T-cells, further showing a direct correlation between androgen and Th1 response. Testosterone is also shown to promote Th2 differentiation and IL-10 production by these cells. In turn, IL-10 has an anti-inflammatory effect and facilitates the expansion of Tregs. Altogether, these changes suppress anti-tumor immune response [90,91,92,93]. In addition to favoring PCa by impacting Th1/Th2 imbalance, this male sex hormone also regulates humoral immune response by affecting B-cell development in a negative manner. Testosterone promotes TGF-β secretion from bone marrow stromal cells which reduces IL-7-mediated proliferation and differentiation of B-cells [76,82,94,95]. Therefore, a higher androgen level impacts PCa outcome negatively. This is also evident from the studies that demonstrate that treating lymphocytes from female mice with testosterone weakened their proliferative response to antigens and caused poorer antigen presentation capability in comparison to normal controls [80,96,97]. While females having significantly lower levels of testosterone are more prone to autoimmune diseases than men, hypogonadism in men leads to increased incidence of autoimmunity implying the immunosuppressive role of androgen [72,73,98,99]. Thus, testosterone plays a major role in cancer incidence and prognosis by manipulating the immune system making males more susceptible to cancer and secondary malignancies compared to females [76,82,94,95,100]. Elevated testosterone levels have not only been shown to increase the risk of sex-specific cancers, but the male–female incidence rate ratio is also high in cancers not specific to sex. Although there are few conflicting reports, PCa risk and development have been linked to elevated testosterone levels [98,99,100,101]. Of particular interest is the fact that AA men have higher circulating testosterone concentrations, along with a greater DHT/testosterone ratio when compared with CA men, which may explain the underlying differences in PCa incidence among these two races [102,103,104,105,106,107]. Furthermore, AAs have increased sex hormone-binding globulin, which increases production of cAMP, a co-activator of the testosterone receptor [108,109,110]. However, contradicting studies about significant difference in serum testosterone levels between AA and CA men exist [111,112]. This also signifies the importance of studying androgen independency observed in castration-resistant prostate cancer (CRPC). This will allow fishing out biomolecules (like cytokines, chemokines and growth factors) that serve as alternate mediators/activators of AR signaling and which are different between the two racial groups.
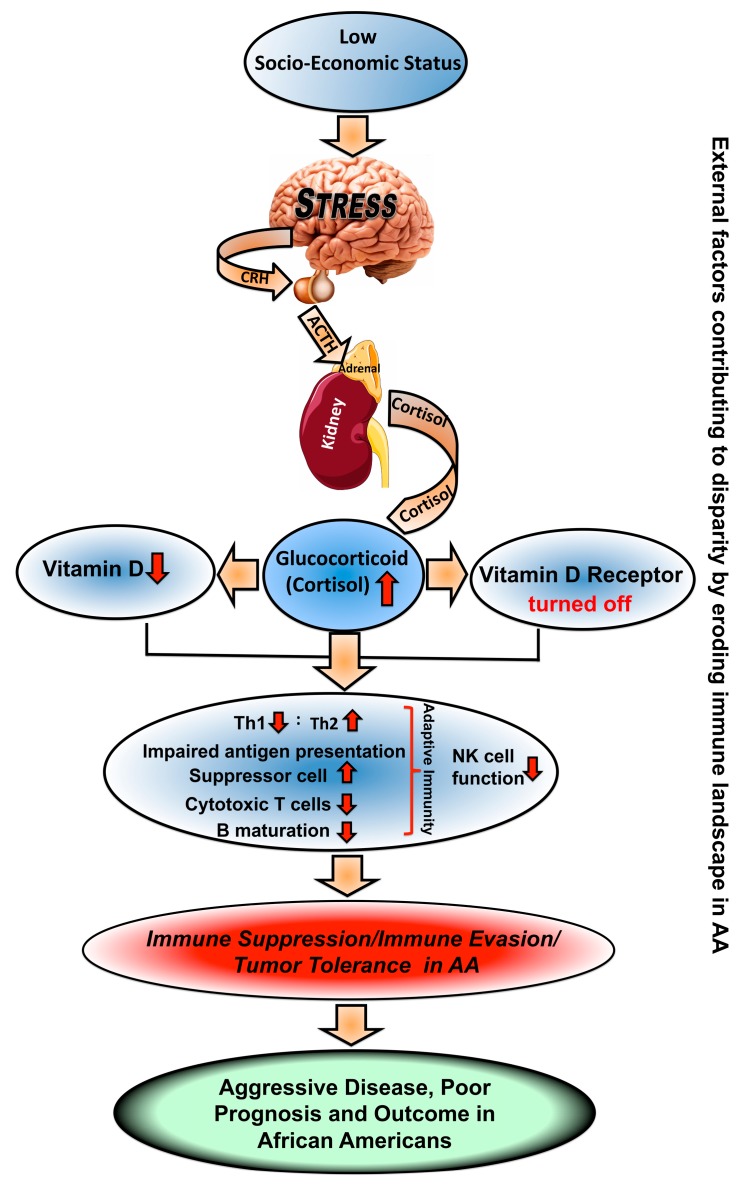
In addition to testosterone, glucocorticoid also modulates immune function. It can act as an immune stimulant however, when it is consistently high, as found with low SES [113], it becomes immune suppressive. Those AAs belonging to lower SES will have increased cortisol and hence will be more prone to tumor-induced immune suppression. Glucocorticoid levels regulate transcription of various genes, such as histone acetylation in the promoter region of perforin and granzyme B, thereby affecting NK cell cytotoxicity [114] as well as CTLs. Thus, changes in this hormone will have a global effect on host immunity [115]. It is also known that high glucocorticoid levels lead to the resistance of immune cells to immune stimulants that further deteriorate defense against cancer. Considering the structural similarity and, hence, the shared target genes between glucocorticoid and androgen receptors, it would not be surprising if glucocorticoid underlies castration resistance in PCa [116] and its associated disparities.
Vitamin D and its derivatives are another closely related class of hormones, which could significantly impact cancer-immune regulation. Also, the fact that almost all immune cells, including monocytes, macrophages, DCs, and activated lymphocytes, express VDR (Vitamin D receptors) clearly suggests an immuno-modulatory role of Vitamin D. Vitamin D exerts its effects on immunity, in addition to regulating calcium and bone homeostasis, by binding of its biologically active metabolite 1,25-dihydroxyvitamin D3 (1,25(OH)-2D) to specific intracellular VDR. 1,25(OH)-2D inhibits the production of inflammatory cytokines, such as IL-1, IL-6, IL-8, IL-12, and TNF-α, by monocytes [117]. It prevents differentiation and maturation of DCs, restricting them to their immature phenotype as evidenced by the reduced expression of MHC-II molecules, co-stimulatory molecules, and IL-12 [118]. However, at local chronic inflammation sites, elevated 1,25(OH)-2D levels augment IL-1 production and MHC-II expression in an autocrine or paracrine fashion thereby enhancing antigen presentation by tissue monocytes/macrophages. Interestingly, high levels of 1,25(OH)-2D also adversely affect adaptive immunity. It inhibits B-cell proliferation and differentiation, suppresses T-cell proliferation, decreases the Th1:Th2 ratio leading to reduced inflammation, shifts away from inflammatory Th17 phenotype, and enhances the development and function of Treg cells [119,120,121,122,123]. These pleotropic effects of Vitamin D culminate in increased production of anti-inflammatory cytokines (IL-10) and decreased production of inflammatory cytokines (IL-21, IL-17). Vitamin D supplementation suppresses IL-6, IL-8 and TNF-α in prostate epithelial cells while expression of TNF-α and PTGS2 (COX-2) is greatly reduced in stromal cells [124]. 1,25(OH)-2D inhibits NF-κB by inducing IκBα; this, in turn, prevents subsequent expression of IFN-β and CXCL10 [125]. Based on its preferential suppressive effect on CXC chemokines, Vitamin D is suggested to reduce recruitment and activation of T-cells [126]. Thus, deficiency of Vitamin D in cancer patients may affect macrophage infiltration by regulating the expression of chemokines in adipocytes.
Despite the well-established immunomodulatory function of Vitamin D on a variety of immune cells and the experimental evidence suggesting an association of lower Vitamin D levels with cancer prognosis and anti-proliferative action on cancer cells, direct correlation with anti-cancer immunity are scarce. Occurrence and mortality rates of bladder, breast, colon, endometrial, lung, ovarian, pancreatic, prostate, rectal, testicular, vaginal cancer, Hodgkin lymphoma, and melanoma negatively correlate with serum Vitamin D [127]. Particularly, in the case of PCa, reduced serum Vitamin D is associated with advanced stage, higher tumor grade, and mortality [128,129,130,131]. Levels of PTGS2 that are significantly higher in PCa are suppressed with 1,25(OH)-2D treatment [132,133,134]. 1,25(OH)-2D also inhibits NF-kB signaling by preventing its interaction with DNA response elements responsible for IL-8 production, suppressing angiogenesis in PCa [135]. Since, in healthy prostate, Vitamin D inhibits the production of pro-inflammatory cytokines responsible for PCa initiation and subsequent progression, chronic Vitamin D deficiency in AAs may create a pro-inflammatory TME that may be responsible for aggressive PCa in these patients compared to their CA counterparts [136,137]. Nonetheless, Vitamin D-mediated molecular pathways and associated inflammation in PCa still need to be explored.
1.5. Racial Differences in Cytokine Profiles in Prostate Cancer
Cytokines are hormone-like messengers which act to regulate the development and expression of a broad array of immune responses described above. These molecules serve as means of communication in coordinating the adaptive and innate immune response. These are a heterogeneous group of soluble small proteins (5–20 kDa) including interleukins (ILs), interferons (IFNs), tumor necrosis factors (TNFs), colony-stimulating factors, growth factors, and chemokines. Many of the key drivers of neoplastic progression, such as neutrophils, MDSCs, TAMs, and Tregs cells, work by secretion of pro-inflammatory cytokines, including IL-1, IL-6, TNF, and TGF-β (Figure 1B), providing a basis for a link between inflammation and cancer [138,139,140,141,142,143]. Several cytokine polymorphisms have been associated with cancer incidence [144]. Alleles associated with increased cytokine production are more frequently found in AA [145,146,147,148,149,150].
Pro-inflammatory cytokine, IL-6, is involved in the regulation of various cellular functions, i.e., proliferation, apoptosis, angiogenesis, differentiation, and regulation of immune response. It is thought to be associated with faster tumor progression, decreased effectiveness of therapy, increased relapse, and decreased survival. Indeed, the poor outcome of many cancer patients is closely associated with elevated serum levels of IL-6. Enhanced IL-6 signaling has been found to be responsible for cancer development and tumor progression in many human cancers including lung, liver, breast, ovarian, pancreatic, prostate, glioma, lymphoma, melanoma, renal, and colorectal cancers [151,152]. It has also been reported to play a key role in chemoresistance in most cancers by maintaining residual tumor cells causing tumor relapse. Its expression can also be linked to the stage, size, and metastasis of tumors affecting the overall survival of the patients. Level of IL-6 also correlates with SES and it significantly differs among healthy AAs and CAs [153]. Serum IL-6 level-based cancer prognosis in the Multi-Ethnic Cohort Study revealed association with significantly poor survival in AAs (Hazard ratio: 2.71) compared to CAs (Hazard ratio: 1.71) [154,155]. Gene expression profiling showed significant differences in levels of pro-inflammatory cytokines (IL-1β, IL-6, and IL-8) in AA and CA PCa patients, which potentially accounts for the observed disparity in PCa. Besides, stromal compartment also showed differential expression of many immune-related genes, mainly involved in cytokine-mediated pathways [156]. In fact, Giangreco et al. found ~18 fold higher IL-6 expression in PCa-associated stroma compared to benign epithelium [124]. This inflammatory microenvironment of stroma regulates the differentiation and proliferation of PCa epithelial cells and also mediates immune response. Probably, a heightened pro-inflammatory stromal microenvironment is responsible for aggressive PCa in AAs compared to CAs. Moreover, chronic inflammation may set the stage for epigenetic changes and genomic instability which may further promote aggressive PCa in AAs. The frequencies of alleles responsible for upregulating pro-inflammatory cytokines are significantly higher in AAs than in CAs. The human IL-6 gene on chromosome 7p21-24 has a common G/C polymorphism of the IL-6 promoter region on position −174 upstream of the transcription start site that impacts serum cytokine levels [157,158]. Data demonstrate a strong association of the −174 G/C polymorphism with the aggressiveness and recurrence of PCa [159]. Higher IL-6 levels and, hence, IL-6 transcription activity was found with G allele homozygosity compared to C allele homozygosity [160]. It is reported that the IL6-174 G/G genotype was much more common among AAs than CAs [147,148,149]. One report suggests that the −174 C/C genotype in AAs could be a strong predictor of aggressive metastatic disease, whereas the G/G genotype in this racial group could suggest an increased risk of cancer [161]. Further, IL-6 has been identified as a major regulator of the balance between regulatory Treg and T helper cells [162]. It also regulates initiation and maturation of Th2 cells along with IL-4 [163]. Elevated IL-6 has been shown to contribute to TAM infiltration [164] and MDSC induction [165] (Figure 1B). It maintains the pro-tumorigenic milieu of immune cells in the TME by supporting angiogenesis as well as evasion of immune surveillance. Additionally, IL-6 induces the transcription of C-reactive protein (CRP) [166], an inflammatory effector that has been reported to have higher circulating levels observed in AAs [167,168]. Over a period of time, these heightened levels have been linked to poor clinical outcomes and increased incidence in various malignancies. In contrast, Heikkilä K et al. [169] conducted a systematic review on CRP and found that CRP did not play a causal role in cancer. Evidence highlighting the anti-tumor role of IL-6 associated with maneuvering of T-cell immunity has come up [59,139,142,144,170,171,172,173,174,175,176]. However, it is the pro-tumorigenic role of IL-6 that links chronic inflammation to tumorigenesis and subsequent metastatic progression [147,148,149,150] that becomes the major factor governing PCa disparity.
Promoter polymorphism of IL-10 may influence tumor development by altering its levels in serum or the TIME. Elevated IL-10 in cancer is associated with TAM infiltration (Figure 1B), downregulating pro-inflammatory cytokines, MHC class II molecules, and co-stimulatory proteins [177,178,179]. The prominence of cancer risk related to IL-10 alleles and its protein expression is not fully understood and varies among different types of cancers [180]. For example, the IL-10−592 polymorphism is associated with a protective effect against non-cardia gastric cancer [181]. There was no effect of the IL-10−1082 G/A polymorphism on cervical cancer risk but there was a clear association with the IL-10−592 C/A polymorphism [182]. In BrCa, the IL-10−592 A/A is associated with reduced susceptibility [183], whereas in PCa, IL-10−819 C and IL-10−592 C polymorphisms may be associated with aggressiveness [184]. Genotypes (IL-10−819 T/T, IL-10−592A/A, and IL-10−1082 A/A) that are associated with lower IL-10 production are three-fold higher in AAs [149,150]. To the contrary, AAs may express higher levels of the allele (−3575T) associated with increased production of IL-10 [147,148,185] when compared to CAs.
Apart from interleukins, interferons are another important set of immune regulatory cytokines that affect immune responses. Though conventionally known for its anti-tumor properties, interferon-gamma (IFN-γ) has pro-tumorigenic roles as well [186]. The contrasting roles of IFN-γ depend on cellular and microenvironmental factors. It plays an important role in tumor surveillance by upregulating MHC-I and thereby increasing immunogenicity of cancer cells. It activates macrophages to secrete chemokines which recruit cytotoxic T-lymphocytes (CTLs) to the site of inflammation culminating into tumor elimination. However, the cancer-promoting role of IFN-γ is attributed to its suppressive effects on CTL and NK cell activity. It also attenuates myeloid cell and neutrophil infiltration into TIME [186]. Studies have found that AAs do not differentially express IFN-γ when compared to other populations; however, there are significant differences in allelic and genotypic frequencies [148]. When compared to CAs AAs are more likely to express the IFN-γ AA genotype [187,188]. This genotype is associated with decreased IFN-γ production [189,190,191]. However, several studies have reported higher mRNA expression of IFN-γ in AAs [147,192,193]. Hence, the precise role of IFNs in PCa disparity is debatable at present and needs further investigation.
Of note is the fact that cytokines associated with both Th1 and Th2 are found to be very high in African adults as opposed to their European counterparts [194]. Also, variants in the Th1-related cytokine genes (IL-12β and IFN-γ), which reduce the severity of malaria, are likely among AAs [195,196]. Single Nucleotide polymorphisms associated with Th1-related cytokines and their receptors IL-15, IL-15RA, and IFNGR2 have been found associated with BrCa risk in AA women [197]. Interestingly, Kimball et al. [198] found that AAs have a greater Th1 response but less IL-10 than healthy CAs in a hepatitis-related study.
Another cytokine that acts as a double-edged sword, having both a tumor suppression as well as progression role, is TGF-β. It regulates tumor growth by arresting cells in G1 phase during the early stages of tumorigenesis [199] and inhibits the clonal expansion and cytolytic activity of NK cells and CTLs (Figure 1B) thereby promoting tumor progression [200]. Signaling triggered by TGF-β also plays a significant role in immunoediting by promoting a Th2 phenotype of T-cells. It also channelizes MDSCs to secrete pro-angiogenic chemokines (Figure 1B) [201,202,203,204,205,206]. Evidence also suggests that TGF-β may promote tumorigenesis by inducing epithelial-to-mesenchymal transition, interfering with cell adhesion, and increasing cell invasiveness. Increased expression of the isoform TGF-β3 has also been speculated to contribute to the migration and invasion of PCa cells. More specifically, evidence confers that TGF-β is an important promoter of malignant cell growth [207,208]. It upregulates Foxp3 which is essential for the development and function of Tregs (Figure 1B) [209,210] and it is also capable of hampering the function of DCs (Figure 1B) [211]. There is a great deal of evidence suggesting the overexpression of TGF-β among AAs [212,213,214,215,216,217]. Profiling of TGF-β1 in AAs revealed overexpression of circulating proteins as well as mRNA levels compared to their CA counterparts. This implies that AAs have a more immunosuppressive environment compared to CA, which may contribute to disparity in PCa.
Vascular endothelial growth factor VEGF, a proficient angiogenic cytokine, is also known for its immunosuppressive function. Hypoxia-induced HIF-1α (hypoxia-induced factor-1α) in the TIME is a principle regulator of VEGF expression by monocytes. Hypoxic conditions also upregulate the expression of pro-angiogenic as well as pro-inflammatory factors (TNF, IL-1, IL-6, and IL-8) via HIF-1α and NFκB signaling [218]. The release of IL-6, IL-8, and CXCL1 from endothelial cells is enhanced by VEGF through an autocrine effect thus creating a pro-inflammatory environment responsible for tumor progression [219]. Interestingly, the expression of VEGF can itself be induced by inflammatory cytokines: TNF-α, IL-1β, IL-6, and IL-8, suggesting a positive feedback loop [218]. It induces COX2 (cyclooxygenase2) expression in endothelial cells via p38 and JNK pathways [220]. Further, it also acts as a chemo-attractant for macrophages in the TME, and these tumor-guided macrophages are themselves a good source of VEGF, MMPs, and M-CSF/CSF1 (Figure 1B). Thus, VEGF contributes significantly in the development of immune tolerance. African Americans have significantly high VEGF [221,222], which may be the reason why AA PCa patients develop immune tolerance sooner than CAs and suffer more aggressive PCa.
1.6. Immune-Based Strategies Available to Treat Prostate Cancer and Their Impact on Reducing Disparity
With the current knowledge of disarrayed host immune systems contributing significantly to PCa progression, outcome, and associated disparity, novel therapies are being designed to overcome immune tolerance, restore Th1 response, and activate CTL to treat PCa. Although long-term studies are imperative, the initial results of these immune therapies sound promising. A CAR–T-cell therapy targeting prostate-specific membrane antigen-II (PSMA-II) showed promising results in a PCa mice model [223]. A phase I CAR-T-cell clinical trial targeting PSMA after non-myeloablative conditioning and IL-2 administration showed reduction in PSA levels [224]. Another phase I CAR–T-cell therapy directed against PSMA showed tolerability and systemic persistence of about two weeks [225]. However, the most successful and recently approved sipuleucel-T, an autologous cellular immunotherapy for CRPC, reduced the risk of death among patients with metastatic CRPC and improved the median overall survival (OS) by 4.1 months versus a placebo in the pivotal phase of the three-trial Immunotherapy for Prostate Adenocarcinoma Treatment study (IMPACT; NCT00065442) [226]. Remarkably, AA men showed an unexpectedly higher survival advantage in the PROCEED trial for receiving immunotherapy for metastatic CRPC [227]. As compared to a placebo, sipuleucel-T led to an overall survival (OS) of 20 months based on the randomized trial [228] with OS 9.3 months longer in AAs than CAs. Such better response by AAs further substantiates the significance of considering immunological differences in patients of African Ancestry before determining the treatment course.
2. Conclusions
Incidence and mortality associated with PCa is declining in the US, yet AAs continue to have higher mortality rates associated with aggressive disease. The growing literature reviewed in this article provides strong evidence that there is differential immune response among patients of different racial groups. Genetic predisposition in immune modifiers in AAs contributes to their poorer prognosis. Socio-economic status-associated differences in hormone profiles and cytokines involved in immune evasion and tumor tolerance in men of different descent might be significant contributors to racial disparity in PCa (Figure 2). Therefore, it is also imperative to consider the SES of participants of the clinical trial before concluding that immune-based therapies, such as sipuleucel-T, show better outcomes in AA PCa patients.
Figure 2.
Immune landscape modifiers and cancer disparity: socioeconomic status-associated stress impacts on cortisol and Vitamin D and Vitamin D receptors. These are involved in eroding the immunological landscape by decreasing the Th1:Th2 ratio, impairing antigen presentation and NK cell function. Such changes favor aggressive disease and poor outcome in African American men. CRH, corticotropin releasing hormone; ACTH, adrenocorticotropic hormone.
Author Contributions
Each author has made substantial contributions to the completion of this review; has approved the submitted version; and agrees to be personally accountable for the author’s own contributions and for any questions related to the content of the review. Contributions are: Conceptualization, S.S.; Writing—Original Draft Preparation, J.K.T.; Writing–Figures Preparation, N.K.; Writing, Review, and Editing, H.M.
Funding
This study was supported in part by the funds (CA180212, CA179701, CA169716 and CA118638) from NCI. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.DeSantis C.E., Miller K.D., Goding Sauer A., Jemal A., Siegel R.L. Cancer statistics for African Americans, 2019. CA Cancer J. Clin. 2019;69:211–233. doi: 10.3322/caac.21555. [DOI] [PubMed] [Google Scholar]
- 2.Latini D.M., Elkin E.P., Cooperberg M.R., Sadetsky N., Duchane J., Carroll P.R. Differences in clinical characteristics and disease-free survival for Latino, African American, and non-Latino white men with localized prostate cancer: Data from CaPSURE. Cancer. 2006;106:789–795. doi: 10.1002/cncr.21675. [DOI] [PubMed] [Google Scholar]
- 3.Pettaway C.A., Troncoso P., Ramirez E.I., Johnston D.A., Steelhammer L., Babaian R.J. Prostate specific antigen and pathological features of prostate cancer in black and white patients: A comparative study based on radical prostatectomy specimens. J. Urol. 1998;160:437–442. doi: 10.1016/S0022-5347(01)62919-7. [DOI] [PubMed] [Google Scholar]
- 4.Powell I.J., Bock C.H., Ruterbusch J.J., Sakr W. Evidence supports a faster growth rate and/or earlier transformation to clinically significant prostate cancer in black than in white American men, and influences racial progression and mortality disparity. J. Urol. 2010;183:1792–1796. doi: 10.1016/j.juro.2010.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsodikov A., Gulati R., de Carvalho T.M., Heijnsdijk E.A.M., Hunter-Merrill R.A., Mariotto A.B., de Koning H.J., Etzioni R. Is prostate cancer different in black men? Answers from 3 natural history models. Cancer. 2017;123:2312–2319. doi: 10.1002/cncr.30687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Powell I.J., Banerjee M., Novallo M., Sakr W., Grignon D., Wood D.P., Pontes J.E. Prostate cancer biochemical recurrence stage for stage is more frequent among African-American than white men with locally advanced but not organ-confined disease. Urology. 2000;55:246–251. doi: 10.1016/S0090-4295(99)00436-7. [DOI] [PubMed] [Google Scholar]
- 7.Moses K.A., Chen L.Y., Sjoberg D.D., Bernstein M., Touijer K.A. Black and White men younger than 50 years of age demonstrate similar outcomes after radical prostatectomy. BMC Urol. 2014;14:98. doi: 10.1186/1471-2490-14-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelly S.P., Rosenberg P.S., Anderson W.F., Andreotti G., Younes N., Cleary S.D., Cook M.B. Trends in the Incidence of Fatal Prostate Cancer in the United States by Race. Eur. Urol. 2017;71:195–201. doi: 10.1016/j.eururo.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parker P.M., Rice K.R., Sterbis J.R., Chen Y., Cullen J., McLeod D.G., Brassell S.A. Prostate cancer in men less than the age of 50: A comparison of race and outcomes. Urology. 2011;78:110–115. doi: 10.1016/j.urology.2010.12.046. [DOI] [PubMed] [Google Scholar]
- 10.Chornokur G., Dalton K., Borysova M.E., Kumar N.B. Disparities at presentation, diagnosis, treatment, and survival in African American men, affected by prostate cancer. Prostate. 2011;71:985–997. doi: 10.1002/pros.21314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karakas C., Wang C., Deng F., Huang H., Wang D., Lee P. Molecular mechanisms involving prostate cancer racial disparity. Am. J. Clin. Exp. Urol. 2017;5:34–48. [PMC free article] [PubMed] [Google Scholar]
- 12.McGinley K.F., Tay K.J., Moul J.W. Prostate cancer in men of African origin. Nat. Rev. Urol. 2016;13:99–107. doi: 10.1038/nrurol.2015.298. [DOI] [PubMed] [Google Scholar]
- 13.Barnes K.C. Genetic epidemiology of health disparities in allergy and clinical immunology. J. Allergy Clin. Immunol. 2006;117:243–254. doi: 10.1016/j.jaci.2005.11.030. [DOI] [PubMed] [Google Scholar]
- 14.Johnson A.H., Rosen-Bronson S., Hurley C.K. Heterogeneity of the HLA-D region in American blacks. Transplant. Proc. 1989;21:3872–3873. [PubMed] [Google Scholar]
- 15.Kaul R., Cohen C.R., Chege D., Yi T.J., Tharao W., McKinnon L.R., Remis R., Anzala O., Kimani J. Biological factors that may contribute to regional and racial disparities in HIV prevalence. Am. J. Reprod. Immunol. 2011;65:317–324. doi: 10.1111/j.1600-0897.2010.00962.x. [DOI] [PubMed] [Google Scholar]
- 16.Kerman R.H., Kimball P.M., Van Buren C.T., Lewis R.M., Kahan B.D. Possible contribution of pretransplant immune responder status to renal allograft survival differences of black versus white recipients. Transplantation. 1991;51:338–342. doi: 10.1097/00007890-199102000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Milford E.L., Ratner L., Yunis E. Will transplant immunogenetics lead to better graft survival in blacks? Racial variability in the accuracy of tissue typing for organ donation: The fourth American workshop. Transplant. Proc. 1987;19:30–32. [PubMed] [Google Scholar]
- 18.Nguyen D.P., Genc M., Vardhana S., Babula O., Onderdonk A., Witkin S.S. Ethnic differences of polymorphisms in cytokine and innate immune system genes in pregnant women. Obstet. Gynecol. 2004;104:293–300. doi: 10.1097/01.AOG.0000133486.85400.5e. [DOI] [PubMed] [Google Scholar]
- 19.Miller J.F., Sadelain M. The journey from discoveries in fundamental immunology to cancer immunotherapy. Cancer Cell. 2015;27:439–449. doi: 10.1016/j.ccell.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 20.Winkler C. Is there a genetic basis for health disparities in human immunodeficiency virus disease? Mt. Sinai J. Med. N. Y. 2010;77:149–159. doi: 10.1002/msj.20172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carlson C.S., Thomas D.J., Eberle M.A., Swanson J.E., Livingston R.J., Rieder M.J., Nickerson D.A. Genomic regions exhibiting positive selection identified from dense genotype data. Genome Res. 2005;15:1553–1565. doi: 10.1101/gr.4326505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tishkoff S.A., Williams S.M. Genetic analysis of African populations: Human evolution and complex disease. Nat. Rev. Genet. 2002;3:611–621. doi: 10.1038/nrg865. [DOI] [PubMed] [Google Scholar]
- 23.Gong Z., Quan L., Yao S., Zirpoli G., Bandera E.V., Roberts M., Coignet J.G., Cabasag C., Sucheston L., Hwang H., et al. Innate immunity pathways and breast cancer Risk in African American and European-American women in the Women’s Circle of Health Study (WCHS) PLoS ONE. 2013;8:e72619. doi: 10.1371/journal.pone.0072619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aranda F., Llopiz D., Diaz-Valdes N., Riezu-Boj J.I., Bezunartea J., Ruiz M., Martinez M., Durantez M., Mansilla C., Prieto J., et al. Adjuvant combination and antigen targeting as a strategy to induce polyfunctional and high-avidity T-cell responses against poorly immunogenic tumors. Cancer Res. 2011;71:3214–3224. doi: 10.1158/0008-5472.CAN-10-3259. [DOI] [PubMed] [Google Scholar]
- 25.Bianchi G., Borgonovo G., Pistoia V., Raffaghello L. Immunosuppressive cells and tumour microenvironment: Focus on mesenchymal stem cells and myeloid derived suppressor cells. Histol. Histopathol. 2011;26:941–951. doi: 10.14670/hh-26.941. [DOI] [PubMed] [Google Scholar]
- 26.Ilkovitch D., Lopez D.M. Immune modulation by melanoma-derived factors. Exp. Dermatol. 2008;17:977–985. doi: 10.1111/j.1600-0625.2008.00779.x. [DOI] [PubMed] [Google Scholar]
- 27.Raval R.R., Sharabi A.B., Walker A.J., Drake C.G., Sharma P. Tumor immunology and cancer immunotherapy: Summary of the 2013 SITC primer. J. Immunother. Cancer. 2014;2:14. doi: 10.1186/2051-1426-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Annunziato F., Romagnani C., Romagnani S. The 3 major types of innate and adaptive cell-mediated effector immunity. J. Allergy Clin. Immunol. 2015;135:626–635. doi: 10.1016/j.jaci.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 29.Karachaliou N., Cao M.G., Teixido C., Viteri S., Morales-Espinosa D., Santarpia M., Rosell R. Understanding the function and dysfunction of the immune system in lung cancer: The role of immune checkpoints. Cancer Biol. Med. 2015;12:79–86. doi: 10.7497/j.issn.2095-3941.2015.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pandolfi F., Cianci R., Pagliari D., Casciano F., Bagala C., Astone A., Landolfi R., Barone C. The immune response to tumors as a tool toward immunotherapy. Clin. Dev. Immunol. 2011;2011:894704. doi: 10.1155/2011/894704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yatim K.M., Lakkis F.G. A brief journey through the immune system. Clin. J. Am. Soc. Nephrol. 2015;10:1274–1281. doi: 10.2215/CJN.10031014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Iheagwara U.K., Beatty P.L., Van P.T., Ross T.M., Minden J.S., Finn O.J. Influenza virus infection elicits protective antibodies and T-cells specific for host cell antigens also expressed as tumor-associated antigens: A new view of cancer immunosurveillance. Cancer Immunol. Res. 2014;2:263–273. doi: 10.1158/2326-6066.CIR-13-0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klein G. Tumor antigens. Annu. Rev. Microbiol. 1966;20:223–252. doi: 10.1146/annurev.mi.20.100166.001255. [DOI] [PubMed] [Google Scholar]
- 34.Olsen L., Campos B., Winther O., Sgroi D.C., Karger B.L., Brusic V. Tumor antigens as proteogenomic biomarkers in invasive ductal carcinomas. BMC Med Genom. 2014;7(Suppl. 3):S2. doi: 10.1186/1755-8794-7-S3-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smyth M.J., Dunn G.P., Schreiber R.D. Cancer immunosurveillance and immunoediting: The roles of immunity in suppressing tumor development and shaping tumor immunogenicity. Adv. Immunol. 2006;90:1–50. doi: 10.1016/s0065-2776(06)90001-7. [DOI] [PubMed] [Google Scholar]
- 36.Waldhauer I., Steinle A. NK cells and cancer immunosurveillance. Oncogene. 2008;27:5932–5943. doi: 10.1038/onc.2008.267. [DOI] [PubMed] [Google Scholar]
- 37.Storkus W.J., Alexander J., Payne J.A., Dawson J.R., Cresswell P. Reversal of natural killing susceptibility in target cells expressing transfected class I HLA genes. Proc. Natl. Acad. Sci. USA. 1989;86:2361–2364. doi: 10.1073/pnas.86.7.2361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smyth M.J., Cretney E., Kelly J.M., Westwood J.A., Street S.E., Yagita H., Takeda K., van Dommelen S.L., Degli-Esposti M.A., Hayakawa Y. Activation of NK cell cytotoxicity. Mol. Immunol. 2005;42:501–510. doi: 10.1016/j.molimm.2004.07.034. [DOI] [PubMed] [Google Scholar]
- 39.Trombetta E.S., Mellman I. Cell biology of antigen processing in vitro and in vivo. Annu. Rev. Immunol. 2005;23:975–1028. doi: 10.1146/annurev.immunol.22.012703.104538. [DOI] [PubMed] [Google Scholar]
- 40.Itano A.A., Jenkins M.K. Antigen presentation to naive CD4 T-cells in the lymph node. Nat. Immunol. 2003;4:733–739. doi: 10.1038/ni957. [DOI] [PubMed] [Google Scholar]
- 41.Albert M.L., Pearce S.F., Francisco L.M., Sauter B., Roy P., Silverstein R.L., Bhardwaj N. Immature dendritic cells phagocytose apoptotic cells via alphavbeta5 and CD36, and cross-present antigens to cytotoxic T lymphocytes. J. Exp. Med. 1998;188:1359–1368. doi: 10.1084/jem.188.7.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heath W.R., Carbone F.R. Cross-presentation, dendritic cells, tolerance and immunity. Annu. Rev. Immunol. 2001;19:47–64. doi: 10.1146/annurev.immunol.19.1.47. [DOI] [PubMed] [Google Scholar]
- 43.Banchereau J., Steinman R.M. Dendritic cells and the control of immunity. Nature. 1998;392:245–252. doi: 10.1038/32588. [DOI] [PubMed] [Google Scholar]
- 44.Cheng P., Zhou J., Gabrilovich D. Regulation of dendritic cell differentiation and function by Notch and Wnt pathways. Immunol. Rev. 2010;234:105–119. doi: 10.1111/j.0105-2896.2009.00871.x. [DOI] [PubMed] [Google Scholar]
- 45.Steinman R.M. Decisions about dendritic cells: Past, present, and future. Annu. Rev. Immunol. 2012;30:1–22. doi: 10.1146/annurev-immunol-100311-102839. [DOI] [PubMed] [Google Scholar]
- 46.Steinman R.M., Banchereau J. Taking dendritic cells into medicine. Nature. 2007;449:419–426. doi: 10.1038/nature06175. [DOI] [PubMed] [Google Scholar]
- 47.Ueno H., Schmitt N., Klechevsky E., Pedroza-Gonzalez A., Matsui T., Zurawski G., Oh S., Fay J., Pascual V., Banchereau J., et al. Harnessing human dendritic cell subsets for medicine. Immunol. Rev. 2010;234:199–212. doi: 10.1111/j.0105-2896.2009.00884.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aderem A. Role of Toll-like receptors in inflammatory response in macrophages. Crit. Care Med. 2001;29:S16–S18. doi: 10.1097/00003246-200107001-00008. [DOI] [PubMed] [Google Scholar]
- 49.Medzhitov R., Janeway C., Jr. Innate immunity. N. Engl. J. Med. 2000;343:338–344. doi: 10.1056/NEJM200008033430506. [DOI] [PubMed] [Google Scholar]
- 50.Dunn G.P., Old L.J., Schreiber R.D. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21:137–148. doi: 10.1016/j.immuni.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 51.Swann J.B., Smyth M.J. Immune surveillance of tumors. J. Clin. Investig. 2007;117:1137–1146. doi: 10.1172/JCI31405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gajewski T.F., Meng Y., Harlin H. Immune suppression in the tumor microenvironment. J. Immunother. 2006;29:233–240. doi: 10.1097/01.cji.0000199193.29048.56. [DOI] [PubMed] [Google Scholar]
- 53.Zitvogel L., Tesniere A., Kroemer G. Cancer despite immunosurveillance: Immunoselection and immunosubversion. Nat. Rev. Immunol. 2006;6:715–727. doi: 10.1038/nri1936. [DOI] [PubMed] [Google Scholar]
- 54.Kerkar S.P., Restifo N.P. Cellular constituents of immune escape within the tumor microenvironment. Cancer Res. 2012;72:3125–3130. doi: 10.1158/0008-5472.CAN-11-4094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marigo I., Dolcetti L., Serafini P., Zanovello P., Bronte V. Tumor-induced tolerance and immune suppression by myeloid derived suppressor cells. Immunol. Rev. 2008;222:162–179. doi: 10.1111/j.1600-065X.2008.00602.x. [DOI] [PubMed] [Google Scholar]
- 56.Medina-Echeverz J., Eggert T., Han M., Greten T.F. Hepatic myeloid-derived suppressor cells in cancer. Cancer Immunol. Immunother. CII. 2015;64:931–940. doi: 10.1007/s00262-015-1736-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Montero A.J., Diaz-Montero C.M., Kyriakopoulos C.E., Bronte V., Mandruzzato S. Myeloid-derived suppressor cells in cancer patients: A clinical perspective. J. Immunother. 2012;35:107–115. doi: 10.1097/CJI.0b013e318242169f. [DOI] [PubMed] [Google Scholar]
- 58.Bronte V., Serafini P., Apolloni E., Zanovello P. Tumor-induced immune dysfunctions caused by myeloid suppressor cells. J. Immunother. 2001;24:431–446. doi: 10.1097/00002371-200111000-00001. [DOI] [PubMed] [Google Scholar]
- 59.Gabrilovich D.I., Ostrand-Rosenberg S., Bronte V. Coordinated regulation of myeloid cells by tumours. Nat. Rev. Immunol. 2012;12:253–268. doi: 10.1038/nri3175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Colombo M.P., Piconese S. Regulatory-T-cell inhibition versus depletion: The right choice in cancer immunotherapy. Nat. Rev. Cancer. 2007;7:880–887. doi: 10.1038/nrc2250. [DOI] [PubMed] [Google Scholar]
- 61.Whiteside T.L. Regulatory T-cell subsets in human cancer: Are they regulating for or against tumor progression? Cancer Immunol. Immunother. CII. 2014;63:67–72. doi: 10.1007/s00262-013-1490-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zou W. Regulatory T-cells, tumour immunity and immunotherapy. Nat. Rev. Immunol. 2006;6:295–307. doi: 10.1038/nri1806. [DOI] [PubMed] [Google Scholar]
- 63.Ghiringhelli F., Menard C., Martin F., Zitvogel L. The role of regulatory T-cells in the control of natural killer cells: Relevance during tumor progression. Immunol. Rev. 2006;214:229–238. doi: 10.1111/j.1600-065X.2006.00445.x. [DOI] [PubMed] [Google Scholar]
- 64.Mantovani A., Sica A. Macrophages, innate immunity and cancer: Balance, tolerance, and diversity. Curr. Opin. Immunol. 2010;22:231–237. doi: 10.1016/j.coi.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 65.Sinha P., Clements V.K., Ostrand-Rosenberg S. Interleukin-13-regulated M2 macrophages in combination with myeloid suppressor cells block immune surveillance against metastasis. Cancer Res. 2005;65:11743–11751. doi: 10.1158/0008-5472.CAN-05-0045. [DOI] [PubMed] [Google Scholar]
- 66.Mantovani A., Sozzani S., Locati M., Allavena P., Sica A. Macrophage polarization: Tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol. 2002;23:549–555. doi: 10.1016/S1471-4906(02)02302-5. [DOI] [PubMed] [Google Scholar]
- 67.Satoh T., Kidoya H., Naito H., Yamamoto M., Takemura N., Nakagawa K., Yoshioka Y., Morii E., Takakura N., Takeuchi O., et al. Critical role of Trib1 in differentiation of tissue-resident M2-like macrophages. Nature. 2013;495:524–528. doi: 10.1038/nature11930. [DOI] [PubMed] [Google Scholar]
- 68.Hussein M.R. Tumour-associated macrophages and melanoma tumourigenesis: Integrating the complexity. Int. J. Exp. Pathol. 2006;87:163–176. doi: 10.1111/j.1365-2613.2006.00478.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Solinas G., Germano G., Mantovani A., Allavena P. Tumor-associated macrophages (TAM) as major players of the cancer-related inflammation. J. Leukoc. Biol. 2009;86:1065–1073. doi: 10.1189/jlb.0609385. [DOI] [PubMed] [Google Scholar]
- 70.Harper J., Sainson R.C. Regulation of the anti-tumour immune response by cancer-associated fibroblasts. Semin. Cancer Biol. 2014;25:69–77. doi: 10.1016/j.semcancer.2013.12.005. [DOI] [PubMed] [Google Scholar]
- 71.Casto J.M., Nolan V., Jr., Ketterson E.D. Steroid hormones and immune function: Experimental studies in wild and captive dark-eyed juncos (Junco hyemalis) Am. Nat. 2001;157:408–420. doi: 10.1086/319318. [DOI] [PubMed] [Google Scholar]
- 72.Cutolo M., Sulli A., Capellino S., Villaggio B., Montagna P., Seriolo B., Straub R.H. Sex hormones influence on the immune system: Basic and clinical aspects in autoimmunity. Lupus. 2004;13:635–638. doi: 10.1191/0961203304lu1094oa. [DOI] [PubMed] [Google Scholar]
- 73.Whitacre C.C. Sex differences in autoimmune disease. Nat. Immunol. 2001;2:777–780. doi: 10.1038/ni0901-777. [DOI] [PubMed] [Google Scholar]
- 74.Chen W., Beck I., Schober W., Brockow K., Effner R., Buters J.T., Behrendt H., Ring J. Human mast cells express androgen receptors but treatment with testosterone exerts no influence on IgE-independent mast cell degranulation elicited by neuromuscular blocking agents. Exp. Dermatol. 2010;19:302–304. doi: 10.1111/j.1600-0625.2009.00969.x. [DOI] [PubMed] [Google Scholar]
- 75.Mantalaris A., Panoskaltsis N., Sakai Y., Bourne P., Chang C., Messing E.M., Wu J.H. Localization of androgen receptor expression in human bone marrow. J. Pathol. 2001;193:361–366. doi: 10.1002/1096-9896(0000)9999:9999<::AID-PATH803>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 76.Viselli S.M., Reese K.R., Fan J., Kovacs W.J., Olsen N.J. Androgens alter B cell development in normal male mice. J. Cell. Immunol. 1997;182:99–104. doi: 10.1006/cimm.1997.1227. [DOI] [PubMed] [Google Scholar]
- 77.Muller W., Groothuis T.G., Kasprzik A., Dijkstra C., Alatalo R.V., Siitari H. Prenatal androgen exposure modulates cellular and humoral immune function of black-headed gull chicks. Proc. Biol. Sci. 2005;272:1971–1977. doi: 10.1098/rspb.2005.3178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Corcoran M.P., Meydani M., Lichtenstein A.H., Schaefer E.J., Dillard A., Lamon-Fava S. Sex hormone modulation of proinflammatory cytokine and C-reactive protein expression in macrophages from older men and postmenopausal women. J. Endocrinol. 2010;206:217–224. doi: 10.1677/JOE-10-0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Corrales J.J., Almeida M., Miralles J.M., Orfao A. Persistence of androgenic effects on the production of proinflammatory cytokines by circulating antigen-presenting cells after withdrawal of testosterone treatment in aging type 2 diabetic men with partial androgen deficiency. Fertil. Steril. 2009;92:311–319. doi: 10.1016/j.fertnstert.2008.05.040. [DOI] [PubMed] [Google Scholar]
- 80.Trigunaite A., Dimo J., Jorgensen T.N. Suppressive effects of androgens on the immune system. Cell. Immunol. 2015;294:87–94. doi: 10.1016/j.cellimm.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 81.Koh Y.T., Gray A., Higgins S.A., Hubby B., Kast W.M. Androgen ablation augments prostate cancer vaccine immunogenicity only when applied after immunization. Prostate. 2009;69:571–584. doi: 10.1002/pros.20906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ellis T.M., Moser M.T., Le P.T., Flanigan R.C., Kwon E.D. Alterations in peripheral B cells and B cell progenitors following androgen ablation in mice. Int. Immunol. 2001;13:553–558. doi: 10.1093/intimm/13.4.553. [DOI] [PubMed] [Google Scholar]
- 83.Henderson J. On the relationship of the thymus to the sexual organs: I. The influence of castration on the thymus. J. Physiol. 1904;31:222–229. doi: 10.1113/jphysiol.1904.sp001032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Heng T.S., Goldberg G.L., Gray D.H., Sutherland J.S., Chidgey A.P., Boyd R.L. Effects of castration on thymocyte development in two different models of thymic involution. J. Immunol. 2005;175:2982–2993. doi: 10.4049/jimmunol.175.5.2982. [DOI] [PubMed] [Google Scholar]
- 85.Olsen N.J., Kovacs W.J. Evidence that androgens modulate human thymic T-cell output. J. Investig. Med. 2011;59:32–35. doi: 10.2310/JIM.0b013e318200dc98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Roden A.C., Moser M.T., Tri S.D., Mercader M., Kuntz S.M., Dong H., Hurwitz A.A., McKean D.J., Celis E., Leibovich B.C., et al. Augmentation of T-cell levels and responses induced by androgen deprivation. J. Immunol. 2004;173:6098–6108. doi: 10.4049/jimmunol.173.10.6098. [DOI] [PubMed] [Google Scholar]
- 87.Sutherland J.S., Goldberg G.L., Hammett M.V., Uldrich A.P., Berzins S.P., Heng T.S., Blazar B.R., Millar J.L., Malin M.A., Chidgey A.P., et al. Activation of thymic regeneration in mice and humans following androgen blockade. J. Immunol. 2005;175:2741–2753. doi: 10.4049/jimmunol.175.4.2741. [DOI] [PubMed] [Google Scholar]
- 88.Kissick H.T., Sanda M.G., Dunn L.K., Pellegrini K.L., On S.T., Noel J.K., Arredouani M.S. Androgens alter T-cell immunity by inhibiting T-helper 1 differentiation. Proc. Natl. Acad. Sci. USA. 2014;111:9887–9892. doi: 10.1073/pnas.1402468111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Myers M.P., Andersen J.N., Cheng A., Tremblay M.L., Horvath C.M., Parisien J.P., Salmeen A., Barford D., Tonks N.K. TYK2 and JAK2 are substrates of protein-tyrosine phosphatase 1B. J. Biol. Chem. 2001;276:47771–47774. doi: 10.1074/jbc.C100583200. [DOI] [PubMed] [Google Scholar]
- 90.Coombes J.L., Siddiqui K.R., Arancibia-Carcamo C.V., Hall J., Sun C.M., Belkaid Y., Powrie F. A functionally specialized population of mucosal CD103+ DCs induces Foxp3+ regulatory T-cells via a TGF-beta and retinoic acid-dependent mechanism. J. Exp. Med. 2007;204:1757–1764. doi: 10.1084/jem.20070590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dalal M., Kim S., Voskuhl R.R. Testosterone therapy ameliorates experimental autoimmune encephalomyelitis and induces a T helper 2 bias in the autoantigen-specific T lymphocyte response. J. Immunol. 1997;159:3–6. [PubMed] [Google Scholar]
- 92.Guilliams M., Crozat K., Henri S., Tamoutounour S., Grenot P., Devilard E., de Bovis B., Alexopoulou L., Dalod M., Malissen B. Skin-draining lymph nodes contain dermis-derived CD103(-) dendritic cells that constitutively produce retinoic acid and induce Foxp3(+) regulatory T-cells. Blood. 2010;115:1958–1968. doi: 10.1182/blood-2009-09-245274. [DOI] [PubMed] [Google Scholar]
- 93.Tang S., Moore M.L., Grayson J.M., Dubey P. Increased CD8+ T-cell function following castration and immunization is countered by parallel expansion of regulatory T-cells. Cancer Res. 2012;72:1975–1985. doi: 10.1158/0008-5472.CAN-11-2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Frey-Wettstein M., Craddock C.G. Testosterone-induced depletion of thymus and marrow lymphocytes as related to lymphopoiesis and hematopoiesis. Blood. 1970;35:257–271. doi: 10.1182/blood.V35.3.257.257. [DOI] [PubMed] [Google Scholar]
- 95.Tang J., Nuccie B.L., Ritterman I., Liesveld J.L., Abboud C.N., Ryan D.H. TGF-beta down-regulates stromal IL-7 secretion and inhibits proliferation of human B cell precursors. J. Immunol. 1997;159:117–125. [PubMed] [Google Scholar]
- 96.Albertsmeier M., Pratschke S., Chaudry I., Angele M.K. Gender-Specific Effects on Immune Response and Cardiac Function after Trauma Hemorrhage and Sepsis. Viszeralmedizin. 2014;30:91–96. doi: 10.1159/000360149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Canguven O., Albayrak S. Do low testosterone levels contribute to the pathogenesis of asthma? Med. Hypotheses. 2011;76:585–588. doi: 10.1016/j.mehy.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 98.French M.A., Hughes P. Systemic lupus erythematosus and Klinefelter’s syndrome. Ann. Rheum. Dis. 1983;42:471–473. doi: 10.1136/ard.42.4.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jimenez-Balderas F.J., Tapia-Serrano R., Fonseca M.E., Arellano J., Beltran A., Yanez P., Camargo-Coronel A., Fraga A. High frequency of association of rheumatic/autoimmune diseases and untreated male hypogonadism with severe testicular dysfunction. Arthritis Res. 2001;3:362–367. doi: 10.1186/ar328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Klap J., Schmid M., Loughlin K.R. The relationship between total testosterone levels and prostate cancer: A review of the continuing controversy. J. Urol. 2015;193:403–413. doi: 10.1016/j.juro.2014.07.123. [DOI] [PubMed] [Google Scholar]
- 101.Hsing A.W., Comstock G.W. Serological precursors of cancer: Serum hormones and risk of subsequent prostate cancer. Cancer Epidemiol. Biomarkers Prev. 1993;2:27–32. [PubMed] [Google Scholar]
- 102.Cartwright R.A., Gurney K.A., Moorman A.V. Sex ratios and the risks of haematological malignancies. Br. J. Haematol. 2002;118:1071–1077. doi: 10.1046/j.1365-2141.2002.03750.x. [DOI] [PubMed] [Google Scholar]
- 103.Cook M.B., Dawsey S.M., Freedman N.D., Inskip P.D., Wichner S.M., Quraishi S.M., Devesa S.S., McGlynn K.A. Sex disparities in cancer incidence by period and age. Cancer Epidemiol. Biomarkers Prev. 2009;18:1174–1182. doi: 10.1158/1055-9965.EPI-08-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Devarahally S.R., Severson R.K., Chuba P., Thomas R., Bhambhani K., Hamre M.R. Second malignant neoplasms after primary central nervous system malignancies of childhood and adolescence. Pediatric Hematol. Oncol. 2003;20:617–625. doi: 10.1080/08880010390243031. [DOI] [PubMed] [Google Scholar]
- 105.Edgren G., Liang L., Adami H.O., Chang E.T. Enigmatic sex disparities in cancer incidence. Eur. J. Epidemiol. 2012;27:187–196. doi: 10.1007/s10654-011-9647-5. [DOI] [PubMed] [Google Scholar]
- 106.Pearce M.S., Parker L. Childhood cancer registrations in the developing world: Still more boys than girls. Int. J. Cancer. 2001;91:402–406. doi: 10.1002/1097-0215(200002)9999:9999<::AID-IJC1048>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 107.Molife R., Lorigan P., MacNeil S. Gender and survival in malignant tumours. Cancer Treat. Rev. 2001;27:201–209. doi: 10.1053/ctrv.2001.0220. [DOI] [PubMed] [Google Scholar]
- 108.Ross R., Bernstein L., Judd H., Hanisch R., Pike M., Henderson B. Serum testosterone levels in healthy young black and white men. J. Natl. Cancer Inst. 1986;76:45–48. [PubMed] [Google Scholar]
- 109.Ross R.K., Bernstein L., Lobo R.A., Shimizu H., Stanczyk F.Z., Pike M.C., Henderson B.E. 5-alpha-reductase activity and risk of prostate cancer among Japanese and US white and black males. Lancet. 1992;339:887–889. doi: 10.1016/0140-6736(92)90927-U. [DOI] [PubMed] [Google Scholar]
- 110.Wu A.H., Whittemore A.S., Kolonel L.N., John E.M., Gallagher R.P., West D.W., Hankin J., Teh C.Z., Dreon D.M., Paffenbarger R.S., Jr. Serum androgens and sex hormone-binding globulins in relation to lifestyle factors in older African-American, white, and Asian men in the United States and Canada. Cancer Epidemiol. Biomarkers Prev. 1995;4:735–741. [PubMed] [Google Scholar]
- 111.Winters S.J., Brufsky A., Weissfeld J., Trump D.L., Dyky M.A., Hadeed V. Testosterone, sex hormone-binding globulin, and body composition in young adult African American and Caucasian men. Metab. Clin. Exp. 2001;50:1242–1247. doi: 10.1053/meta.2001.26714. [DOI] [PubMed] [Google Scholar]
- 112.Kubricht W.S., 3rd, Williams B.J., Whatley T., Pinckard P., Eastham J.A. Serum testosterone levels in African-American and white men undergoing prostate biopsy. Urology. 1999;54:1035–1038. doi: 10.1016/S0090-4295(99)00290-3. [DOI] [PubMed] [Google Scholar]
- 113.Cavigelli S.A., Chaudhry H.S. Social status, glucocorticoids, immune function, and health: Can animal studies help us understand human socioeconomic-status-related health disparities? Horm. Behav. 2012;62:295–313. doi: 10.1016/j.yhbeh.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 114.Eddy J.L., Krukowski K., Janusek L., Mathews H.L. Glucocorticoids regulate natural killer cell function epigenetically. Cell. Immunol. 2014;290:120–130. doi: 10.1016/j.cellimm.2014.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Maranville J.C., Baxter S.S., Torres J.M., Di Rienzo A. Inter-ethnic differences in lymphocyte sensitivity to glucocorticoids reflect variation in transcriptional response. Pharm. J. 2013;13:121–129. doi: 10.1038/tpj.2011.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lin K.-T., Wang L.-H. New dimension of glucocorticoids in cancer treatment. Steroids. 2016;111:84–88. doi: 10.1016/j.steroids.2016.02.019. [DOI] [PubMed] [Google Scholar]
- 117.Almerighi C., Sinistro A., Cavazza A., Ciaprini C., Rocchi G., Bergamini A. 1Alpha,25-dihydroxyvitamin D3 inhibits CD40L-induced pro-inflammatory and immunomodulatory activity in human monocytes. Cytokine. 2009;45:190–197. doi: 10.1016/j.cyto.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 118.Piemonti L., Monti P., Sironi M., Fraticelli P., Leone B.E., Dal Cin E., Allavena P., Di Carlo V. Vitamin D3 affects differentiation, maturation, and function of human monocyte-derived dendritic cells. J. Immunol. 2000;164:4443–4451. doi: 10.4049/jimmunol.164.9.4443. [DOI] [PubMed] [Google Scholar]
- 119.Boonstra A., Barrat F.J., Crain C., Heath V.L., Savelkoul H.F., O’Garra A. 1alpha,25-Dihydroxyvitamin d3 has a direct effect on naive CD4(+) T-cells to enhance the development of Th2 cells. J. Immunol. 2001;167:4974–4980. doi: 10.4049/jimmunol.167.9.4974. [DOI] [PubMed] [Google Scholar]
- 120.Chen S., Sims G.P., Chen X.X., Gu Y.Y., Chen S., Lipsky P.E. Modulatory effects of 1,25-dihydroxyvitamin D3 on human B cell differentiation. J. Immunol. 2007;179:1634–1647. doi: 10.4049/jimmunol.179.3.1634. [DOI] [PubMed] [Google Scholar]
- 121.Lemire J.M., Adams J.S., Sakai R., Jordan S.C. 1 alpha,25-dihydroxyvitamin D3 suppresses proliferation and immunoglobulin production by normal human peripheral blood mononuclear cells. J. Clin. Investig. 1984;74:657–661. doi: 10.1172/JCI111465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Mattner F., Smiroldo S., Galbiati F., Muller M., Di Lucia P., Poliani P.L., Martino G., Panina-Bordignon P., Adorini L. Inhibition of Th1 development and treatment of chronic-relapsing experimental allergic encephalomyelitis by a non-hypercalcemic analogue of 1,25-dihydroxyvitamin D(3) Eur. J. Immunol. 2000;30:498–508. doi: 10.1002/1521-4141(200002)30:2<498::AID-IMMU498>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 123.Tang J., Zhou R., Luger D., Zhu W., Silver P.B., Grajewski R.S., Su S.B., Chan C.C., Adorini L., Caspi R.R. Calcitriol suppresses antiretinal autoimmunity through inhibitory effects on the Th17 effector response. J. Immunol. 2009;182:4624–4632. doi: 10.4049/jimmunol.0801543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Giangreco A.A., Dambal S., Wagner D., Van der Kwast T., Vieth R., Prins G.S., Nonn L. Differential expression and regulation of vitamin D hydroxylases and inflammatory genes in prostate stroma and epithelium by 1,25-dihydroxyvitamin D in men with prostate cancer and an in vitro model. J. Steroid Biochem. Mol. Biol. 2015;148:156–165. doi: 10.1016/j.jsbmb.2014.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hansdottir S., Monick M.M., Lovan N., Powers L., Gerke A., Hunninghake G.W. Vitamin D decreases respiratory syncytial virus induction of NF-kappaB-linked chemokines and cytokines in airway epithelium while maintaining the antiviral state. J. Immunol. 2010;184:965–974. doi: 10.4049/jimmunol.0902840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Selvaraj P., Harishankar M., Singh B., Banurekha V.V., Jawahar M.S. Effect of vitamin D3 on chemokine expression in pulmonary tuberculosis. Cytokine. 2012;60:212–219. doi: 10.1016/j.cyto.2012.06.238. [DOI] [PubMed] [Google Scholar]
- 127.Grant W.B., Peiris A.N. Differences in vitamin D status may account for unexplained disparities in cancer survival rates between African and white Americans. Derm. Endocrinol. 2012;4:85–94. doi: 10.4161/derm.19667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Gilbert R., Metcalfe C., Fraser W.D., Donovan J., Hamdy F., Neal D.E., Lane J.A., Martin R.M. Associations of circulating 25-hydroxyvitamin D with prostate cancer diagnosis, stage and grade. Int. J. Cancer. 2012;131:1187–1196. doi: 10.1002/ijc.27327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Murphy A.B., Nyame Y., Martin I.K., Catalona W.J., Hollowell C.M., Nadler R.B., Kozlowski J.M., Perry K.T., Kajdacsy-Balla A., Kittles R. Vitamin D deficiency predicts prostate biopsy outcomes. Clin. Cancer Res. 2014;20:2289–2299. doi: 10.1158/1078-0432.CCR-13-3085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Shui I.M., Mucci L.A., Kraft P., Tamimi R.M., Lindstrom S., Penney K.L., Nimptsch K., Hollis B.W., Dupre N., Platz E.A., et al. Vitamin D-related genetic variation, plasma vitamin D, and risk of lethal prostate cancer: A prospective nested case-control study. J. Natl. Cancer Inst. 2012;104:690–699. doi: 10.1093/jnci/djs189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Steck S.E., Arab L., Zhang H., Bensen J.T., Fontham E.T., Johnson C.S., Mohler J.L., Smith G.J., Su J.L., Trump D.L., et al. Association between Plasma 25-Hydroxyvitamin D, Ancestry and Aggressive Prostate Cancer among African Americans and European Americans in PCaP. PLoS ONE. 2015;10:e0125151. doi: 10.1371/journal.pone.0125151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gupta S., Srivastava M., Ahmad N., Bostwick D.G., Mukhtar H. Over-expression of cyclooxygenase-2 in human prostate adenocarcinoma. Prostate. 2000;42:73–78. doi: 10.1002/(SICI)1097-0045(20000101)42:1<73::AID-PROS9>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 133.Kirschenbaum A., Klausner A.P., Lee R., Unger P., Yao S., Liu X.H., Levine A.C. Expression of cyclooxygenase-1 and cyclooxygenase-2 in the human prostate. Urology. 2000;56:671–676. doi: 10.1016/S0090-4295(00)00674-9. [DOI] [PubMed] [Google Scholar]
- 134.Moreno J., Krishnan A.V., Swami S., Nonn L., Peehl D.M., Feldman D. Regulation of prostaglandin metabolism by calcitriol attenuates growth stimulation in prostate cancer cells. Cancer Res. 2005;65:7917–7925. doi: 10.1158/0008-5472.CAN-05-1435. [DOI] [PubMed] [Google Scholar]
- 135.Bao B.Y., Yao J., Lee Y.F. 1alpha, 25-dihydroxyvitamin D3 suppresses interleukin-8-mediated prostate cancer cell angiogenesis. Carcinogenesis. 2006;27:1883–1893. doi: 10.1093/carcin/bgl041. [DOI] [PubMed] [Google Scholar]
- 136.Grant W.B., Peiris A.N. Possible role of serum 25-hydroxyvitamin D in black-white health disparities in the United States. J. Am. Med Dir. Assoc. 2010;11:617–628. doi: 10.1016/j.jamda.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 137.Hollis B.W., Marshall D.T., Savage S.J., Garrett-Mayer E., Kindy M.S., Gattoni-Celli S. Vitamin D3 supplementation, low-risk prostate cancer, and health disparities. J. Steroid Biochem. Mol. Biol. 2013;136:233–237. doi: 10.1016/j.jsbmb.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 138.Coussens L.M., Zitvogel L., Palucka A.K. Neutralizing tumor-promoting chronic inflammation: A magic bullet? Science. 2013;339:286–291. doi: 10.1126/science.1232227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Hanahan D., Coussens L.M. Accessories to the crime: Functions of cells recruited to the tumor microenvironment. Cancer Cell. 2012;21:309–322. doi: 10.1016/j.ccr.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 140.Mantovani A., Allavena P., Sica A., Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–444. doi: 10.1038/nature07205. [DOI] [PubMed] [Google Scholar]
- 141.Naugler W.E., Karin M. The wolf in sheep’s clothing: The role of interleukin-6 in immunity, inflammation and cancer. Trends Mol. Med. 2008;14:109–119. doi: 10.1016/j.molmed.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 142.Rose-John S. IL-6 trans-signaling via the soluble IL-6 receptor: Importance for the pro-inflammatory activities of IL-6. Int. J. Biol. Sci. 2012;8:1237–1247. doi: 10.7150/ijbs.4989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Swartz M.A., Iida N., Roberts E.W., Sangaletti S., Wong M.H., Yull F.E., Coussens L.M., DeClerck Y.A. Tumor microenvironment complexity: Emerging roles in cancer therapy. Cancer Res. 2012;72:2473–2480. doi: 10.1158/0008-5472.CAN-12-0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Calhoun E.S., McGovern R.M., Janney C.A., Cerhan J.R., Iturria S.J., Smith D.I., Gostout B.S., Persing D.H. Host genetic polymorphism analysis in cervical cancer. Clin. Chem. 2002;48:1218–1224. [PubMed] [Google Scholar]
- 145.Chen H., Wilkins L.M., Aziz N., Cannings C., Wyllie D.H., Bingle C., Rogus J., Beck J.D., Offenbacher S., Cork M.J., et al. Single nucleotide polymorphisms in the human interleukin-1B gene affect transcription according to haplotype context. Hum. Mol. Genet. 2006;15:519–529. doi: 10.1093/hmg/ddi469. [DOI] [PubMed] [Google Scholar]
- 146.Cox E.D., Hoffmann S.C., DiMercurio B.S., Wesley R.A., Harlan D.M., Kirk A.D., Blair P.J. Cytokine polymorphic analyses indicate ethnic differences in the allelic distribution of interleukin-2 and interleukin-6. Transplantation. 2001;72:720–726. doi: 10.1097/00007890-200108270-00027. [DOI] [PubMed] [Google Scholar]
- 147.Hassan M.I., Aschner Y., Manning C.H., Xu J., Aschner J.L. Racial differences in selected cytokine allelic and genotypic frequencies among healthy, pregnant women in North Carolina. Cytokine. 2003;21:10–16. doi: 10.1016/S1043-4666(02)00489-1. [DOI] [PubMed] [Google Scholar]
- 148.Hoffmann S.C., Stanley E.M., Cox E.D., DiMercurio B.S., Koziol D.E., Harlan D.M., Kirk A.D., Blair P.J. Ethnicity greatly influences cytokine gene polymorphism distribution. Am. J. Transplant. 2002;2:560–567. doi: 10.1034/j.1600-6143.2002.20611.x. [DOI] [PubMed] [Google Scholar]
- 149.Ness R.B., Haggerty C.L., Harger G., Ferrell R. Differential distribution of allelic variants in cytokine genes among African Americans and White Americans. Am. J. Epidemiol. 2004;160:1033–1038. doi: 10.1093/aje/kwh325. [DOI] [PubMed] [Google Scholar]
- 150.Zabaleta J., Schneider B.G., Ryckman K., Hooper P.F., Camargo M.C., Piazuelo M.B., Sierra R.A., Fontham E.T., Correa P., Williams S.M., et al. Ethnic differences in cytokine gene polymorphisms: Potential implications for cancer development. Cancer Immunol. Immunother. CII. 2008;57:107–114. doi: 10.1007/s00262-007-0358-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Heikkila K., Ebrahim S., Lawlor D.A. Systematic review of the association between circulating interleukin-6 (IL-6) and cancer. Eur. J. Cancer. 2008;44:937–945. doi: 10.1016/j.ejca.2008.02.047. [DOI] [PubMed] [Google Scholar]
- 152.Lippitz B.E. Cytokine patterns in patients with cancer: A systematic review. Lancet Oncol. 2013;14:e218–e228. doi: 10.1016/S1470-2045(12)70582-X. [DOI] [PubMed] [Google Scholar]
- 153.Carroll J.F., Fulda K.G., Chiapa A.L., Rodriquez M., Phelps D.R., Cardarelli K.M., Vishwanatha J.K., Cardarelli R. Impact of race/ethnicity on the relationship between visceral fat and inflammatory biomarkers. Obesity. 2009;17:1420–1427. doi: 10.1038/oby.2008.657. [DOI] [PubMed] [Google Scholar]
- 154.Enewold L., Mechanic L.E., Bowman E.D., Zheng Y.L., Yu Z., Trivers G., Alberg A.J., Harris C.C. Serum concentrations of cytokines and lung cancer survival in African Americans and Caucasians. Cancer Epidemiol. Biomarkers Prev. 2009;18:215–222. doi: 10.1158/1055-9965.EPI-08-0705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Kinoshita T., Ito H., Miki C. Serum interleukin-6 level reflects the tumor proliferative activity in patients with colorectal carcinoma. Cancer. 1999;85:2526–2531. doi: 10.1002/(SICI)1097-0142(19990615)85:12<2526::AID-CNCR6>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 156.Kinseth M.A., Jia Z., Rahmatpanah F., Sawyers A., Sutton M., Wang-Rodriguez J., Mercola D., McGuire K.L. Expression differences between African American and Caucasian prostate cancer tissue reveals that stroma is the site of aggressive changes. Int. J. Cancer. 2014;134:81–91. doi: 10.1002/ijc.28326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Bowcock A.M., Kidd J.R., Lathrop G.M., Daneshvar L., May L.T., Ray A., Sehgal P.B., Kidd K.K., Cavalli-Sforza L.L. The human “interferon-beta 2/hepatocyte stimulating factor/interleukin-6” gene: DNA polymorphism studies and localization to chromosome 7p21. Genomics. 1988;3:8–16. doi: 10.1016/0888-7543(88)90152-8. [DOI] [PubMed] [Google Scholar]
- 158.Fishman D., Faulds G., Jeffery R., Mohamed-Ali V., Yudkin J.S., Humphries S., Woo P. The effect of novel polymorphisms in the interleukin-6 (IL-6) gene on IL-6 transcription and plasma IL-6 levels, and an association with systemic-onset juvenile chronic arthritis. J. Clin. Investig. 1998;102:1369–1376. doi: 10.1172/JCI2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Tan D., Wu X., Hou M., Lee S.O., Lou W., Wang J., Janarthan B., Nallapareddy S., Trump D.L., Gao A.C. Interleukin-6 polymorphism is associated with more aggressive prostate cancer. J. Urol. 2005;174:753–756. doi: 10.1097/01.ju.0000168723.42824.40. [DOI] [PubMed] [Google Scholar]
- 160.Pereira D.S., Garcia D.M., Narciso F.M., Santos M.L., Dias J.M., Queiroz B.Z., Souza E.R., Nobrega O.T., Pereira L.S. Effects of 174 G/C polymorphism in the promoter region of the interleukin-6 gene on plasma IL-6 levels and muscle strength in elderly women. Braz. J. Med. Biol. Res. 2011;44:123–129. doi: 10.1590/S0100-879X2010007500152. [DOI] [PubMed] [Google Scholar]
- 161.Mandal S., Abebe F., Chaudhary J. -174G/C polymorphism in the interleukin-6 promoter is differently associated with prostate cancer incidence depending on race. Genet. Mol. Res. GMR. 2014;13:139–151. doi: 10.4238/2014.January.10.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Fujimoto M., Nakano M., Terabe F., Kawahata H., Ohkawara T., Han Y., Ripley B., Serada S., Nishikawa T., Kimura A., et al. The influence of excessive IL-6 production in vivo on the development and function of Foxp3+ regulatory T cells. J. Immunol. 2011;186:32–40. doi: 10.4049/jimmunol.0903314. [DOI] [PubMed] [Google Scholar]
- 163.Kidd P. Th1/Th2 balance: The hypothesis, its limitations, and implications for health and disease. Altern. Med. Rev. 2003;8:223–246. [PubMed] [Google Scholar]
- 164.Pei B.X., Sun B.S., Zhang Z.F., Wang A.L., Ren P. Interstitial tumor-associated macrophages combined with tumor-derived colony-stimulating factor-1 and interleukin-6, a novel prognostic biomarker in non-small cell lung cancer. J. Thorac. Cardiovasc. Surg. 2014;148:1208–1216. doi: 10.1016/j.jtcvs.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 165.Wu C.T., Hsieh C.C., Lin C.C., Chen W.C., Hong J.H., Chen M.F. Significance of IL-6 in the transition of hormone-resistant prostate cancer and the induction of myeloid-derived suppressor cells. J. Mol. Med. 2012;90:1343–1355. doi: 10.1007/s00109-012-0916-x. [DOI] [PubMed] [Google Scholar]
- 166.Voleti B., Agrawal A. Regulation of basal and induced expression of C-reactive protein through an overlapping element for OCT-1 and NF-kappaB on the proximal promoter. J. Immunol. 2005;175:3386–3390. doi: 10.4049/jimmunol.175.5.3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Khera A., McGuire D.K., Murphy S.A., Stanek H.G., Das S.R., Vongpatanasin W., Wians F.H., Jr., Grundy S.M., de Lemos J.A. Race and gender differences in C-reactive protein levels. J. Am. Coll. Cardiol. 2005;46:464–469. doi: 10.1016/j.jacc.2005.04.051. [DOI] [PubMed] [Google Scholar]
- 168.Reiner A.P., Beleza S., Franceschini N., Auer P.L., Robinson J.G., Kooperberg C., Peters U., Tang H. Genome-wide association and population genetic analysis of C-reactive protein in African American and Hispanic American women. Am. J. Hum. Genet. 2012;91:502–512. doi: 10.1016/j.ajhg.2012.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Heikkila K., Ebrahim S., Lawlor D.A. A systematic review of the association between circulating concentrations of C reactive protein and cancer. J. Epidemiol. Community Health. 2007;61:824–833. doi: 10.1136/jech.2006.051292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Angell H., Galon J. From the immune contexture to the Immunoscore: The role of prognostic and predictive immune markers in cancer. Curr. Opin. Immunol. 2013;25:261–267. doi: 10.1016/j.coi.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 171.Chen Q., Fisher D.T., Clancy K.A., Gauguet J.M., Wang W.C., Unger E., Rose-John S., von Andrian U.H., Baumann H., Evans S.S. Fever-range thermal stress promotes lymphocyte trafficking across high endothelial venules via an interleukin 6 trans-signaling mechanism. Nat. Immunol. 2006;7:1299–1308. doi: 10.1038/ni1406. [DOI] [PubMed] [Google Scholar]
- 172.Chen Q., Wang W.C., Bruce R., Li H., Schleider D.M., Mulbury M.J., Bain M.D., Wallace P.K., Baumann H., Evans S.S. Central role of IL-6 receptor signal-transducing chain gp130 in activation of L-selectin adhesion by fever-range thermal stress. Immunity. 2004;20:59–70. doi: 10.1016/S1074-7613(03)00358-3. [DOI] [PubMed] [Google Scholar]
- 173.Fisher D.T., Chen Q., Skitzki J.J., Muhitch J.B., Zhou L., Appenheimer M.M., Vardam T.D., Weis E.L., Passanese J., Wang W.C., et al. IL-6 trans-signaling licenses mouse and human tumor microvascular gateways for trafficking of cytotoxic T-cells. J. Clin. Investig. 2011;121:3846–3859. doi: 10.1172/JCI44952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Fridman W.H., Pages F., Sautes-Fridman C., Galon J. The immune contexture in human tumours: Impact on clinical outcome. Nat. Rev. Cancer. 2012;12:298–306. doi: 10.1038/nrc3245. [DOI] [PubMed] [Google Scholar]
- 175.Mikucki M.E., Fisher D.T., Ku A.W., Appenheimer M.M., Muhitch J.B., Evans S.S. Preconditioning thermal therapy: Flipping the switch on IL-6 for anti-tumour immunity. Int. J. Hyperther. 2013;29:464–473. doi: 10.3109/02656736.2013.807440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Vardam T.D., Zhou L., Appenheimer M.M., Chen Q., Wang W.C., Baumann H., Evans S.S. Regulation of a lymphocyte-endothelial-IL-6 trans-signaling axis by fever-range thermal stress: Hot spot of immune surveillance. Cytokine. 2007;39:84–96. doi: 10.1016/j.cyto.2007.07.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Esquivel-Velazquez M., Ostoa-Saloma P., Palacios-Arreola M.I., Nava-Castro K.E., Castro J.I., Morales-Montor J. The role of cytokines in breast cancer development and progression. J. Interferon Cytokine Res. 2015;35:1–16. doi: 10.1089/jir.2014.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Hedrich C.M., Bream J.H. Cell type-specific regulation of IL-10 expression in inflammation and disease. Immunol. Res. 2010;47:185–206. doi: 10.1007/s12026-009-8150-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Shrestha S., Wiener H.W., Aissani B., Song W., Shendre A., Wilson C.M., Kaslow R.A., Tang J. Interleukin-10 (IL-10) pathway: Genetic variants and outcomes of HIV-1 infection in African American adolescents. PLoS ONE. 2010;5:e13384. doi: 10.1371/journal.pone.0013384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Howell W.M., Rose-Zerilli M.J. Interleukin-10 polymorphisms, cancer susceptibility and prognosis. Fam. Cancer. 2006;5:143–149. doi: 10.1007/s10689-005-0072-3. [DOI] [PubMed] [Google Scholar]
- 181.Pan X.F., Yang S.J., Loh M., Xie Y., Wen Y.Y., Tian Z., Huang H., Lan H., Chen F., Soong R., et al. Interleukin-10 gene promoter polymorphisms and risk of gastric cancer in a Chinese population: Single nucleotide and haplotype analyses. Asian Pac. J. Cancer Prev. APJCP. 2013;14:2577–2582. doi: 10.7314/APJCP.2013.14.4.2577. [DOI] [PubMed] [Google Scholar]
- 182.Ni J., Ye Y., Teng F., Wu Q. Interleukin 10 polymorphisms and cervical cancer risk: A meta-analysis. Int. J. Gynecol. Cancer. 2013;23:126–133. doi: 10.1097/IGC.0b013e318274b1a2. [DOI] [PubMed] [Google Scholar]
- 183.Langsenlehner U., Krippl P., Renner W., Yazdani-Biuki B., Eder T., Köppel H., Wascher T.C., Paulweber B., Samonigg H. Interleukin-10 promoter polymorphism is associated with decreased breast cancer risk. Breast Cancer Res. Treat. 2005;90:113–115. doi: 10.1007/s10549-004-3607-7. [DOI] [PubMed] [Google Scholar]
- 184.Shao N., Xu B., Mi Y.Y., Hua L.X. IL-10 polymorphisms and prostate cancer risk: A meta-analysis. Prostate Cancer Prostatic Dis. 2011;14:129–135. doi: 10.1038/pcan.2011.6. [DOI] [PubMed] [Google Scholar]
- 185.Gibson A.W., Edberg J.C., Wu J., Westendorp R.G., Huizinga T.W., Kimberly R.P. Novel single nucleotide polymorphisms in the distal IL-10 promoter affect IL-10 production and enhance the risk of systemic lupus erythematosus. J. Immunol. 2001;166:3915–3922. doi: 10.4049/jimmunol.166.6.3915. [DOI] [PubMed] [Google Scholar]
- 186.Zaidi M.R., Merlino G. The two faces of interferon-gamma in cancer. Clin. Cancer Res. 2011;17:6118–6124. doi: 10.1158/1078-0432.CCR-11-0482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Delaney N.L., Esquenazi V., Lucas D.P., Zachary A.A., Leffell M.S. TNF-alpha, TGF-beta, IL-10, IL-6, and INF-gamma alleles among African Americans and Cuban Americans. Report of the ASHI Minority Workshops: Part IV. Hum. Immunol. 2004;65:1413–1419. doi: 10.1016/j.humimm.2004.07.240. [DOI] [PubMed] [Google Scholar]
- 188.Govan V.A., Carrara H.R., Sachs J.A., Hoffman M., Stanczuk G.A., Williamson A.L. Ethnic differences in allelic distribution of IFN-g in South African women but no link with cervical cancer. J. Carcinog. 2003;2:3. doi: 10.1186/1477-3163-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Asderakis A., Sankaran D., Dyer P., Johnson R.W., Pravica V., Sinnott P.J., Roberts I., Hutchinson I.V. Association of polymorphisms in the human interferon-gamma and interleukin-10 gene with acute and chronic kidney transplant outcome: The cytokine effect on transplantation. Transplantation. 2001;71:674–677. doi: 10.1097/00007890-200103150-00018. [DOI] [PubMed] [Google Scholar]
- 190.Ben-Ari Z., Mor E., Papo O., Kfir B., Sulkes J., Tambur A.R., Tur-Kaspa R., Klein T. Cytokine gene polymorphisms in patients infected with hepatitis B virus. Am. J. Gastroenterol. 2003;98:144–150. doi: 10.1111/j.1572-0241.2003.07179.x. [DOI] [PubMed] [Google Scholar]
- 191.Lio D., Marino V., Serauto A., Gioia V., Scola L., Crivello A., Forte G.I., Colonna-Romano G., Candore G., Caruso C. Genotype frequencies of the +874T-->A single nucleotide polymorphism in the first intron of the interferon-gamma gene in a sample of Sicilian patients affected by tuberculosis. Eur. J. Immunogenet. 2002;29:371–374. doi: 10.1046/j.1365-2370.2002.00327.x. [DOI] [PubMed] [Google Scholar]
- 192.Park N.J., Kang D.H. Inflammatory cytokine levels and breast cancer risk factors: Racial differences of healthy Caucasian and African American women. Oncol. Nurs. Forum. 2013;40:490–500. doi: 10.1188/13.ONF.40-05AP. [DOI] [PubMed] [Google Scholar]
- 193.Wallace T.A., Prueitt R.L., Yi M., Howe T.M., Gillespie J.W., Yfantis H.G., Stephens R.M., Caporaso N.E., Loffredo C.A., Ambs S. Tumor immunobiological differences in prostate cancer between African-American and European-American men. Cancer. Res. 2008;68:927–936. doi: 10.1158/0008-5472.CAN-07-2608. [DOI] [PubMed] [Google Scholar]
- 194.Wilfing A., Winkler S., Schrattbauer K., Willheim M., Baier K., Aichelburg A., Muller T., Graninger W., Kremsner P.G. African-European differences in the capacity of T-cell cytokine production. Am. J. Trop. Med. Hyg. 2001;65:504–509. doi: 10.4269/ajtmh.2001.65.504. [DOI] [PubMed] [Google Scholar]
- 195.Barreiro L.B., Quintana-Murci L. From evolutionary genetics to human immunology: How selection shapes host defence genes. Nat. Rev. Genet. 2010;11:17–30. doi: 10.1038/nrg2698. [DOI] [PubMed] [Google Scholar]
- 196.Kwiatkowski D.P. How malaria has affected the human genome and what human genetics can teach us about malaria. Am. J. Hum. Genet. 2005;77:171–192. doi: 10.1086/432519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Quan L., Gong Z., Yao S., Bandera E.V., Zirpoli G., Hwang H., Roberts M., Ciupak G., Davis W., Sucheston L., et al. Cytokine and cytokine receptor genes of the adaptive immune response are differentially associated with breast cancer risk in American women of African and European ancestry. Int. J. Cancer. 2014;134:1408–1421. doi: 10.1002/ijc.28458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Kimball P., Elswick R.K., Shiffman M. Ethnicity and cytokine production gauge response of patients with hepatitis C to interferon-alpha therapy. J. Med. Virol. 2001;65:510–516. doi: 10.1002/jmv.2065. [DOI] [PubMed] [Google Scholar]
- 199.Buenemann C.L., Willy C., Buchmann A., Schmiechen A., Schwarz M. Transforming growth factor-beta1-induced Smad signaling, cell-cycle arrest and apoptosis in hepatoma cells. Carcinogenesis. 2001;22:447–452. doi: 10.1093/carcin/22.3.447. [DOI] [PubMed] [Google Scholar]
- 200.Akhurst R.J., Derynck R. TGF-beta signaling in cancer--a double-edged sword. Trends Cell Biol. 2001;11:S44–S51. doi: 10.1016/s0962-8924(01)02130-4. [DOI] [PubMed] [Google Scholar]
- 201.Carmeliet P., Jain R.K. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011;473:298–307. doi: 10.1038/nature10144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Izhak L., Wildbaum G., Jung S., Stein A., Shaked Y., Karin N. Dissecting the autocrine and paracrine roles of the CCR2-CCL2 axis in tumor survival and angiogenesis. PLoS ONE. 2012;7:e28305. doi: 10.1371/journal.pone.0028305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Ma J., Wang Q., Fei T., Han J.D., Chen Y.G. MCP-1 mediates TGF-beta-induced angiogenesis by stimulating vascular smooth muscle cell migration. Blood. 2007;109:987–994. doi: 10.1182/blood-2006-07-036400. [DOI] [PubMed] [Google Scholar]
- 204.Meulmeester E., Ten Dijke P. The dynamic roles of TGF-beta in cancer. J. Pathol. 2011;223:205–218. doi: 10.1002/path.2785. [DOI] [PubMed] [Google Scholar]
- 205.Verbeke H., Struyf S., Laureys G., Van Damme J. The expression and role of CXC chemokines in colorectal cancer. Cytokine Growth Factor Rev. 2011;22:345–358. doi: 10.1016/j.cytogfr.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 206.Yang L., Pang Y., Moses H.L. TGF-beta and immune cells: An important regulatory axis in the tumor microenvironment and progression. Trends Immunol. 2010;31:220–227. doi: 10.1016/j.it.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Chang T.P., Poltoratsky V., Vancurova I. Bortezomib inhibits expression of TGF-beta1, IL-10, and CXCR4, resulting in decreased survival and migration of cutaneous T-cell lymphoma cells. J. Immunol. 2015;194:2942–2953. doi: 10.4049/jimmunol.1402610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Engels E.A., Jennings L., Kemp T.J., Chaturvedi A.K., Pinto L.A., Pfeiffer R.M., Trotter J.F., Acker M., Onaca N., Klintmalm G.B. Circulating TGF-beta1 and VEGF and risk of cancer among liver transplant recipients. Cancer Med. 2015;4:1252–1257. doi: 10.1002/cam4.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Jarnicki A.G., Lysaght J., Todryk S., Mills K.H. Suppression of antitumor immunity by IL-10 and TGF-beta-producing T cells infiltrating the growing tumor: Influence of tumor environment on the induction of CD4+ and CD8+ regulatory T cells. J. Immunol. 2006;177:896–904. doi: 10.4049/jimmunol.177.2.896. [DOI] [PubMed] [Google Scholar]
- 210.Takatori H., Kawashima H., Matsuki A., Meguro K., Tanaka S., Iwamoto T., Sanayama Y., Nishikawa N., Tamachi T., Ikeda K., et al. Helios Enhances Treg Cell Function in Cooperation With FoxP3. Arthritis. Rheum. 2015;67:1491–1502. doi: 10.1002/art.39091. [DOI] [PubMed] [Google Scholar]
- 211.Ahn Y.H., Hong S.O., Kim J.H., Noh K.H., Song K.H., Lee Y.H., Jeon J.H., Kim D.W., Seo J.H., Kim T.W. The siRNA cocktail targeting interleukin 10 receptor and transforming growth factor-beta receptor on dendritic cells potentiates tumour antigen-specific CD8(+) T-cell immunity. Clin. Exp. Immunol. 2015;181:164–178. doi: 10.1111/cei.12620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Fantasia J., Lin C.B., Wiwi C., Kaur S., Hu Y.P., Zhang J., Southall M.D. Differential levels of elastin fibers and TGF-beta signaling in the skin of Caucasians and African Americans. J. Dermatol. Sci. 2013;70:159–165. doi: 10.1016/j.jdermsci.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 213.Huan Y., DeLoach S., Daskalakis C., Dunn S.R., Sharma K., Falkner B. Regulation of transforming growth factor-beta1 by insulin in prediabetic African Americans. Kidney Int. 2010;78:318–324. doi: 10.1038/ki.2010.109. [DOI] [PubMed] [Google Scholar]
- 214.Kupfer S.S., Skol A.D., Hong E., Ludvik A., Kittles R.A., Keku T.O., Sandler R.S., Ellis N.A. Shared and independent colorectal cancer risk alleles in TGFbeta-related genes in African and European Americans. Carcinogenesis. 2014;35:2025–2030. doi: 10.1093/carcin/bgu088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Silver R.M., Bogatkevich G., Tourkina E., Nietert P.J., Hoffman S. Racial differences between blacks and whites with systemic sclerosis. Curr. Opin. Rheumatol. 2012;24:642–648. doi: 10.1097/BOR.0b013e328356d9dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Suthanthiran M., Khanna A., Cukran D., Adhikarla R., Sharma V.K., Singh T., August P. Transforming growth factor-beta 1 hyperexpression in African American end-stage renal disease patients. Kidney Int. 1998;53:639–644. doi: 10.1046/j.1523-1755.1998.00858.x. [DOI] [PubMed] [Google Scholar]
- 217.Suthanthiran M., Li B., Song J.O., Ding R., Sharma V.K., Schwartz J.E., August P. Transforming growth factor-beta 1 hyperexpression in African-American hypertensives: A novel mediator of hypertension and/or target organ damage. Proc. Natl. Acad. Sci. USA. 2000;97:3479–3484. doi: 10.1073/pnas.050420897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Angelo L.S., Kurzrock R. Vascular endothelial growth factor and its relationship to inflammatory mediators. Clin. Cancer Res. 2007;13:2825–2830. doi: 10.1158/1078-0432.CCR-06-2416. [DOI] [PubMed] [Google Scholar]
- 219.Hao Q., Wang L., Tang H. Vascular endothelial growth factor induces protein kinase D-dependent production of proinflammatory cytokines in endothelial cells. Am. J. Physiol. Cell Physiol. 2009;296:C821–C827. doi: 10.1152/ajpcell.00504.2008. [DOI] [PubMed] [Google Scholar]
- 220.Wu G., Luo J., Rana J.S., Laham R., Sellke F.W., Li J. Involvement of COX-2 in VEGF-induced angiogenesis via P38 and JNK pathways in vascular endothelial cells. Cardiovasc. Res. 2006;69:512–519. doi: 10.1016/j.cardiores.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 221.Lindner R., Sullivan C., Offor O., Lezon-Geyda K., Halligan K., Fischbach N., Shah M., Bossuyt V., Schulz V., Tuck D.P., et al. Molecular phenotypes in triple negative breast cancer from African American patients suggest targets for therapy. PLoS ONE. 2013;8:e71915. doi: 10.1371/journal.pone.0071915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.VanCleave T.T., Moore J.H., Benford M.L., Brock G.N., Kalbfleisch T., Baumgartner R.N., Lillard J.W., Jr., Kittles R.A., Kidd L.C. Interaction among variant vascular endothelial growth factor (VEGF) and its receptor in relation to prostate cancer risk. The Prostate. 2010;70:341–352. doi: 10.1002/pros.21067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Zhong X.S., Matsushita M., Plotkin J., Riviere I., Sadelain M. Chimeric antigen receptors combining 4-1BB and CD28 signaling domains augment PI3kinase/AKT/Bcl-XL activation and CD8+ T-cell-mediated tumor eradication. Mol. Ther. Nucleic Acids. 2010;18:413–420. doi: 10.1038/mt.2009.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Junghans R.P., Ma Q., Rathore R., Gomes E.M., Bais A.J., Lo A.S., Abedi M., Davies R.A., Cabral H.J., Al-Homsi A.S., et al. Phase I Trial of Anti-PSMA Designer CAR-T Cells in Prostate Cancer: Possible Role for Interacting Interleukin 2-T Cell Pharmacodynamics as a Determinant of Clinical Response. Prostate. 2016;76:1257–1270. doi: 10.1002/pros.23214. [DOI] [PubMed] [Google Scholar]
- 225.Slovin S.F., Wang X., Hullings M., Arauz G., Bartido S., Lewis J.S., Schöder H., Zanzonico P., Scher H.I., Riviere I. Chimeric antigen receptor (CAR+) modified T-cells targeting prostate specific membrane antigen (PSMA) in patients (pts) with castrate metastatic prostate cancer (CMPC) J. Clin. Oncol. 2013;31:TPS3115. doi: 10.1200/jco.2013.31.6_suppl.72. [DOI] [Google Scholar]
- 226.Kantoff P.W., Higano C.S., Shore N.D., Berger E.R., Small E.J., Penson D.F., Redfern C.H., Ferrari A.C., Dreicer R., Sims R.B., et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N. Engl. J. Med. 2010;363:411–422. doi: 10.1056/NEJMoa1001294. [DOI] [PubMed] [Google Scholar]
- 227.Jim Kling Largest Race-Based Survival Advantage to Date Seen in Men Receiving Sipuleucel-T for Prostate Cancer. [(accessed on 24 October 2019)]; Available online: https://www.cancernetwork.com/asco-prostate-cancer/largest-race-based-survival-advantage-date-seen-men-receiving-sipuleucel-t-mcrpc.
- 228.Anassi E., Ndefo U.A. Sipuleucel-T (provenge) injection: The first immunotherapy agent (vaccine) for hormone-refractory prostate cancer. Pharm. Ther. 2011;36:197–202. [PMC free article] [PubMed] [Google Scholar]