Abstract
BACKGROUND:
Health-promoting behaviors are essential beliefs and actions to develop and sustain the adolescent health; however, people with inadequate health literacy have poorer health status. This study aimed to determine the effect of a problem-based learning (PBL) health literacy program on improving health-promoting behaviors among female students (15–18 years) at high schools in 2018–2019.
METHODS:
This study was a quasi-experimental intervention one which carried out on 377 girl students using a cluster sampling method of intervention (n = 183) and control (n = 194) groups. The intervention was performed in four educational sessions of PBL health literacy program using related scenarios for 90 min. Data were collected through demographic variables, the Health Literacy Measure for Adolescents, and the Health-Promoting Lifestyle Profile II. Participants filled the questionnaires immediately and 3 months after the intervention in both the groups.
RESULTS:
There were significant differences comparing the mean score of health literacy dimensions in numeracy (P < 0.001), use (P < 0.001), communication (P < 0.001), access (P = 0.03), self-efficacy (P < 0.001), and total health literacy (P < 0.001) after intervention. These differences also observed in numeracy (P < 0.001), use (P = 0.03) and total health literacy (P < 0.001) in follow-up between the intervention and control groups. The mean scores of health-promoting lifestyle dimensions in all dimensions immediately after intervention (P < 0.001) and follow-up (P ≤ 0.006) showed significant differences between the two groups, while the intervention group revealed a higher mean scores.
CONCLUSION:
It seems that PBL health literacy and practicing real-life scenarios can improve the adolescent lifestyle. It is recommended to examine the effectiveness of the program for other health-related behaviors among other populations.
Keywords: Girl students, health literacy, health-promoting lifestyle, problem-based learning
Introduction
Health literacy is the degree to how people are able to choose, understand, process, communicate, and get information for their health.[1] In that, they have the correct judgments and make proper decisions that affect their health, disease prevention, and health promotion for maintaining or improving life quality during everyday lives.[2] According to the Center For Health Care Strategies of the United States studies, people with limited health literacy are less likely to understand and practice the provided information properly compared to those with adequate health literacy. Moreover, not only the average number of patient visits is more among them but also adopting their self-care skills and preventive care are weaker, and as a result, they will incur more medical costs.[3]
The World Health Organization (2008) reported health literacy as one of the greatest determinants of health. It also recommends that countries create the association consisting of all people for monitoring and coordination of the strategic activities of promoting health literacy in different societies.[4] People with adequate health literacy are able to show good performance in their circumstances and report better health care using acquired social cognitive skills.[5]
Adolescence is a period which changes persons’ relationships with other people and the environment dramatically[6] which also associated with physical, emotional, and evolutionary changes. Therefore, it is a very good time to equip adolescents with new and correct health information[7] to increase health literacy and improve and maintain their healthy lifestyle. Schools are one of the most important settings to implement health promotion program. For this purpose, it is necessary for the schools’ authorities to apply different educational methods which have a significant role in raising awareness of students.[8]
Nowadays, using modern educational methods has been considered. One of them is problem-based learning (PBL). PBL is a comprehensive learning strategy that the educator plays a facilitating role in learning,[9] moreover, guides learners to teamwork and encourages them to become more active.[10] Thus, teachers express real-life issues in the form of an educational scenario. It is supposed that this approach will increase self-efficacy and personal performance.[11]
Besides knowledge and attitude, students in school will learn new behaviors which can influence their health behaviors directly.[12] According to some reports, 51% of adolescents do not have good health-related behaviors.[12] Several studies showed that physical activities have an undesirable level in girl students. Some studies show that only 36% of female students have good physical activities.[12] Other studies also showed nutrition patterns of girl students in an unacceptable level.[13] Adolescence is associated with puberty which is the source of many stresses in this period. Girls are more susceptible to pubertal stress than boys, and various studies have shown a link between stress and many physical and mental illnesses.[13] Since many of the health-related behaviors develop during adolescence, establishing behavioral patterns seems very important. Further, paying attention to female health is vital because they transfer these experiences to the next generations. Intervention-based PBL method through scenarios leads to get active learning among students and put them in real-life situations to gain healthy skills to solve everyday problems, as well as provided appropriate patterns to represent healthy lifestyles.
Therefore, the primary aim of this study was to evaluate the impact of PBL and health literacy program on improving health-promotive behaviors among female students, and the second aim was to report the results to education authorities for enhancing health literacy in adolescents.
Methods
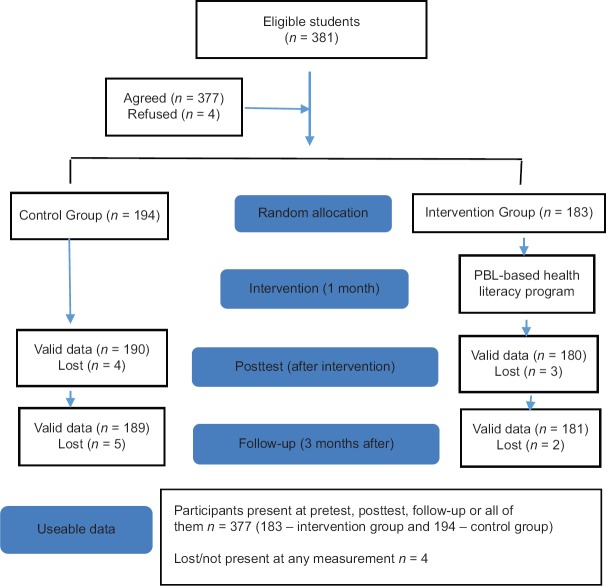
This study was a quasi-experimental one with intervention and control groups. The study population was female students in high schools in catchment areas of Tehran University of Medical Sciences (TUMS). The sample size was calculated based on the difference between health literacy scores in Eckman et al. study[8] and equaled to 360 students (180 students in each group): α = 5%, power = 90%, standard deviation in the first group = 2.2, standard deviation in the second group = 2.23, the difference observed between the two groups = 1.16, design effect = 2.1, and the probability loss percentage = 10%. Due to the difference in the number of students in each class, the sample size was 377 students who were randomly allocated to the intervention and control groups (183 in the intervention group and 194 in the control group) [Figure 1].
Figure 1.
Consort diagram of study
To collect data, a formal permission was obtained from TUMS and the General Directorate of Education Ministry. After selecting schools from education districts of 10, 11, and 17, a cluster sampling method was conducted. From each district, two schools were selected and nominated two classes from each school. To control information contaminated, each school had only one group (intervention or control).
In this study, inclusion criteria were students in Grade 10, 11, and 12 year studying in schools of selected areas of Tehran, being in the age group of 15–18 years, and volunteering to study participation. Exclusion criteria were two sessions absence from educational sessions and lack of students’ tendency to being in the study and move from living location. This study was approved by the Ethics Committee of TUMS, with ID code IR.TUMS.SPH.REC.1397.052, and was registered in the clinical trial registration database (IRCT2013213012460N16).
To data collection, a- three part self-administered questionnaire was conducted including demographic information (age, body mass index [BMI], grade, parents’ education and occupation), a standard questionnaire of the Health Literacy Measure for Adolescents (HELMA), designed and validated by Ghanbari et al.[6] consist of 44 questions in 8 domains named access, reading, understanding, appraisal, use, communication, self-efficacy, and numeracy. Moreover, standard questionnaire of the Health-Promoting Lifestyle Profile II questionnaire of Walker and Hill-Polerecky[14] conducted as the third part of questionnaire. The results are classified as inadequate (0–50), problematic (50.01–66), sufficient (66.01–84), and excellent (84.01–100). The Cronbach's (alpha) coefficient for the entire scale was 0.93. The intraclass correlation coefficient = 0.93 showed that HELMA had satisfactory stability. This instrument focused on the broader aspects of health literacy among specific subgroups of adolescents in a health-care setting.
Health-Promoting Lifestyle Profile II questionnaire of Walker and Hill-Polerecky[14] was validated by Mohamadian et al.[15] in Persian. This questionnaire contains 34 questions in four dimensions of physical activity, health responsibility, nutrition, and stress management, in which the scores range in three levels of weak (0–2), average (2–3), and good (3–4). The Cronbach's a coefficient was 0.86, and the confirmatory factor analysis produced a good estimate of fit (c2= 6.34, df = 2, P = 0.420, NFI = 0.99, CFI = 0.99, and RMSEA = 0.066).
All participants were fully informed about this study and gave written consent. Students filled the questionnaires, followed by researchers expressing the study aims to encourage them to participate. After primary analysis, the samples were randomly allocated into two groups of intervention and control. The intervention group participated in a four-session (90 min) PBL health literacy program, 1 day a week for a month, whereas the control group did not. The health literacy program designed for students consisted of a PBL intervention intended to promote the competences of participants regarding access, read, comprehension, numeracy, communication, appraisal and usage of health information, health empowerment, and health-related behaviors. We also identified health literacy issues that meet the needs of adolescent girls’ health-related behaviors [Figure 2].
Figure 2.
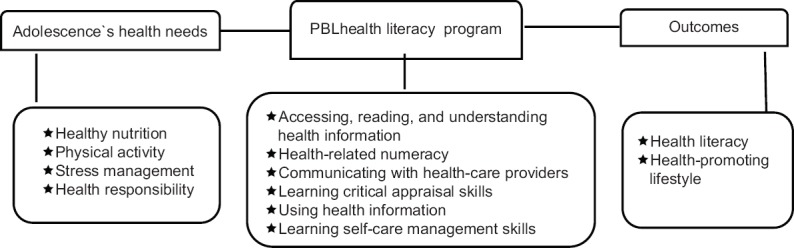
Intervention model of problem-based learning health literacy program for students
In coordination with the school principals, the curriculum for each class was held separately during school hours, and one instructor was responsible for implementing the curriculum in every six classes by visiting the schools in the school hours assigned by the school authorities.
Students randomly allocated into groups of five to six and each class included five to six groups, then working on scenarios related to health literacy and health-promoting lifestyle. This study was conducted with the aim of increasing the factors such as participation in the learning and teamwork and improving learning performance.[16] Each scenario consisted of the sections with an ill-defined or open-ended problem of a real life;[17] at the end of each section, the student had to produce hypotheses and look at the problems and trying to solve them through group discussions. The scenarios included short stories or dialogs that occur between a small number of people, and health problems of a real life were used in scenarios.
In the first session, four educational scenarios in access, reading, and understanding dimensions were presented and discussed about access, reading, and understanding health information such as prevent from pediculosis by means of access to information about it, vision problems and their impact on reading, problems related to inadequate sleep and its impact on understanding, problems related to lack of awareness of accessibility, reading and understanding health issues, and the necessity of investigating medication information from drug brochure.
In the second session, we taught scenarios related to the numeracy and communication dimensions, and discussed about the problems of communication, the need to have an effective relationship with health staff and parents to prevent puberty-related problems in girls and ways of communication. Moreover, we trained the necessity and ways of checking and calculating daily energy intake, foods’ label, and BMI to prevent health problems to the students.
In the third session, we implemented the scenarios related to the use and appraisal dimensions for students and discussed about the ways of assessing the health information, the necessity of having a critical thinking, need to use their knowledge about health issues such as daily physical activity and use methods of them in real life and healthy lifestyle.
In the fourth session, two scenarios involving self-efficacy and other dimensions were presented to students about ways to prevent noncommunicable diseases by managing stress and physical activity and healthy nutrition and responsibility for health and increasing self-efficacy and also enhance their ability to control diseases by regular checkup weight, blood sugar, and blood pressure at home.
After educational intervention, to investigate the effect of the educational program of the intervention group, all questionnaires completed by students in both the intervention and control groups. Three months after the educational intervention, all questionnaires filled by both the groups to determine the impact of the educational program and sustainability of the intervention in the intervention group.
All statistical analyses were performed at a significant level <0.05 usingSPSS (Version 25.0. Armonk, NY: IBM Corp) To compare the groups in the baseline, Chi-square test, Mann–Whitney test, and t-test were used. Relation of the variables was assessed by Spearman correlation. Repeated measures analysis of variance was used to compare the changes within each group. Generalized estimating equation (GEE) tests were used to compare the groups considering the possible correlation of the outcomes in each center. Moreover, to adjust the effect of variables which revealed to be a statistically significant difference between the intervention and control groups at baseline, another GEE analyses were used. To consider multiple comparisons, the Bonferroni method was conducted whenever needed.
Results
Table 1 shows baseline sociodemographic characteristics of students who participated in the study. The average age of participants was 16.26 ± 0.8 years. Table 1 also reveals that the intervention and control groups were not significantly different in sociodemographic characteristics except father's education.
Table 1.
Baseline of sociodemographic characteristics of participants
| Variables | Intervention, n (%) | Control, n (%) | Total, n (%) | P |
|---|---|---|---|---|
| Age (years) | ||||
| 15 | 26 (14.2) | 35 (18) | 61 (16.2) | 0.105 |
| 16 | 84 (45.9) | 95 (49) | 179 (46.9) | |
| 17 | 61 (33.3) | 56 (28.9) | 117 (31.6) | |
| 18 | 12 (6.6) | 8 (4.1) | 20 (5.3) | |
| School grade | ||||
| Tenth | 107 (58.5) | 112 (57.7) | 219 (58.1) | 0.241 |
| Eleventh | 0 | 32 (16.5) | 32 (8.5) | |
| Twelfth | 76 (41.5) | 50 (25.8) | 126 (34) | |
| Father education | ||||
| Primary | 14 (7.7) | 4 (2.1) | 18 (4.9) | 0.007 |
| Secondary | 45 (24.9) | 44 (23.3) | 89 (24.1) | |
| Diploma | 90 (49.7) | 87 (46) | 177 (47.8) | |
| Higher | 32 (17.7) | 54 (28.6) | 86 (23.2) | |
| Father job | ||||
| Employed | 155 (84.7) | 176 (90.7) | 331 (89.4) | 0.069 |
| Unemployed | 7 (3.8) | 1 (0.5) | 8 (2) | |
| Retired | 18 (9.8) | 17 (8.8) | 35 (9.2) | |
| Mother education | ||||
| Primary | 9 (5.5) | 9 (5.3) | 18 (5.4) | 0.1 |
| Secondary | 45 (24.3) | 35 (20.5) | 80 (22.4) | |
| Diploma | 97 (54.1) | 103 (53) | 200 (53.5) | |
| Higher | 29 (16) | 41 (21.2) | 70 (18.6) | |
| Mother job | ||||
| Employed | 43 (23.5) | 45 (23.2) | 89 (23.07) | 0.572 |
| Homemaker | 140 (76.5) | 149 (76.8) | 289 (76.6) | |
| BMI | ||||
| <18.5 | 40 (21.9) | 42 (21.6) | 82 (21.8) | 0.278 |
| 18.5-24.9 | 99 (54.1) | 119 (61.3) | 218 (57.8) | |
| 25-29.9 | 37 (20.2) | 22 (11.3) | 59 (15.6) | |
| >30 | 5 (2.7) | 7 (3.6) | 12 (3.2) |
BMI=Body mass index
Table 2 shows that the highest and the lowest scores of health literacy belonged to the understanding and numeracy dimensions, respectively; the mean score of students’ health literacy was in the problematic range. There was no significant difference between the intervention and control groups in the mean score of health literacy and its dimensions other than numeracy dimensions that the control group had a higher mean score (P = 0.04).
Table 2.
Changes in health literacy and its dimensions among study participants
| Variables | Mean | P* | Differences | ||||||
|---|---|---|---|---|---|---|---|---|---|
| T2−T1 | P** | T3−T1 | P** | ||||||
| Intervention, mean±SD | Control mean±SD | Intervention mean±SD | Control mean±SD | Intervention mean±SD | Control mean±SD | ||||
| Health literacy | |||||||||
| T1 | 59.1±13.0 | 61.1±12.9 | 0.106 | 6.52±1.0 | −0.01±0.34 | 0.001 | 7.36±1.0 | 1.35±0.7 | 0.001 |
| T2 | 65.6±12.4 | 61.1±12.1 | |||||||
| T3 | 66.4±14.1 | 62.5±13.4 | |||||||
| P | 0.001 | 1 | 0.001 | 0.22 | |||||
| Self-efficacy | |||||||||
| T1 | 58.1±17.5 | 60.7±17.8 | 0.137 | 6.73±1.45 | −0.42±0.327 | 0.001 | 6.25±1.54 | 3.07±1.01 | 0.426 |
| T2 | 64.9±17.6 | 60.3±17.4 | |||||||
| T3 | 64.4±18.7 | 63.8±18.1 | |||||||
| P | 0.001 | 0.481 | 0.001 | 0.009 | |||||
| Access | |||||||||
| T1 | 61.7±20.4 | 65.0±20.4 | 0.06 | 4.69±1.61 | 0.52±0.71 | 0.035 | 4.48±1.65 | 0.90±1.18 | 0.449 |
| T2 | 66.4±17.6 | 65.5±15.6 | |||||||
| T3 | 66.2±18.1 | 65.9±19.6 | |||||||
| P | 0.012 | 0.847 | 0.022 | 0.83 | |||||
| Reading | |||||||||
| T1 | 68.7±24.2 | 70.7±23.0 | 0.42 | 2.37±1.89 | −0.52±0.41 | 0.271 | 1.63±1.93 | 1.15±1.26 | 0.968 |
| T2 | 71.1±18.8 | 70.2±22.3 | |||||||
| T3 | 70.4±20.2 | 71.9±24.1 | |||||||
| P | 0.51 | 0.50 | 0.78 | 0.74 | |||||
| Understand | |||||||||
| T1 | 73.2±16.7 | 76.4±19.4 | 0.12 | −1.00±1.33 | −0.9±0.71 | 0.318 | −0.93±1.49 | −1.04±1.15 | 0.212 |
| T2 | 72.2±15.5 | 75.5±15.5 | |||||||
| T3 | 72.3±16.7 | 75.4±17.2 | |||||||
| P | 0.835 | 0.498 | 0.899 | 0.747 | |||||
| Appraisal | |||||||||
| T1 | 55.9±18.8 | 59.6±20.2 | 0.09 | 5.35±1.67 | −0.08±0.370 | 0.093 | 6.52±1.59 | 3.00±1.15 | 0.444 |
| T2 | 61.3±19.3 | 59.5±19.5 | |||||||
| T3 | 62.5±19.7 | 62.6±20.1 | |||||||
| P | 0.005 | 0.994 | 0.001 | 0.03 | |||||
| Use | |||||||||
| T1 | 48.7±19.5 | 49.5±22.3 | 0.825 | 11.25±1.65 | 0±0.70 | 0.001 | 10.5±1.66 | 2.77±1.35 | 0.030 |
| T2 | 59.9±20.2 | 49.5±21.6 | |||||||
| T3 | 59.2±22.0 | 52.3±21.7 | |||||||
| P | 0.001 | 1.00 | 0.001 | 0.121 | |||||
| Communicate | |||||||||
| T1 | 62.4±18.6 | 63.6±19.8 | 0.67 | 4.02±1.64 | −0.02±0.35 | 0.001 | 4.34±1.58 | 1.60±1.18 | 0.339 |
| T2 | 66.4±17.3 | 63.6±19.5 | |||||||
| T3 | 66.8±19.1 | 65.2±19.8 | |||||||
| P | 0.045 | 1.00 | 0.02 | 0.444 | |||||
| Numeracy | |||||||||
| T1 | 41.5±29.1 | 45.1±30.8 | 0.04 | 24.36±3.01 | 1.69±1.51 | 0.001 | 27.09±2.86 | −0.56±1.08 | 0.001 |
| T2 | 65.8±38.0 | 46.8±36.9 | |||||||
| T3 | 68.6±36.8 | 44.6±31.5 | |||||||
| P | 0.001 | 0.604 | 0.001 | 0.937 | |||||
P=Repeated measure. *T-test, **GEE. T1=Baseline, T2=After intervention, T3=Follow-up. GEE=Generalized estimating equations, SD=Standard deviation
Changes in the health literacy between the baseline (T1) and follow-up (T3) were examined. The average level of health literacy in the intervention group increased over the study period, from the baseline (T1), immediately (T2), and 3 months after the intervention (T3).
There was a significant difference in all dimensions except reading and understanding immediately and 3 months after the intervention in health literacy of the intervention group [Table 2]. In addition, there was a significant difference between the appraisal and self-efficacy dimensions in the control group at follow-up. There was a significant difference in all dimensions except reading, understanding, and appraisal immediately after intervention between the intervention and control groups. Moreover, comparing the health literacy of the intervention and control groups showed that there was a significant difference in health literacy, numeracy, and use at follow-up [Table 2].
Table 3 shows that the highest and lowest scores of health-promoting lifestyle belonged to stress management and health responsibility dimensions, respectively. The mean score of health-promoting lifestyle of participants was in the average range. There was no significant difference in health-promoting lifestyle and its dimensions between the intervention and control groups.
Table 3.
Changes in Health-Promoting Lifestyle Profile II and its dimensions among study participants
| Variables | Mean | P* | Differences | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention, mean±SD | Control, mean±SD | T2−T1 | P** | T3−T1 | P** | ||||
| Intervention, mean±SD | Control, mean±SD | Intervention, mean±SD | Control, mean±SD | ||||||
| HPLP II | |||||||||
| T1 | 2.31±0.43 | 2.32±0.46 | 0.949 | 0.40±0.03 | 0.005±0.01 | 0.001 | 0.39±0.03 | 0.03±0.02 | 0.001 |
| T2 | 2.71±0.50 | 2.32±0.44 | |||||||
| T3 | 2.7±0.52 | 2.35±0.48 | |||||||
| P | 0.001 | 0.977 | 0.001 | 0.271 | |||||
| Nutrition | |||||||||
| T1 | 2.44±0.48 | 2.43±0.49 | 0.61 | 0.39±0.04 | 0.009±0.01 | 0.001 | 0.36±0.04 | 0.02±0.02 | 0.001 |
| T2 | 2.83±0.49 | 2.44±0.48 | |||||||
| T3 | 2.81±0.51 | 2.46±0.53 | |||||||
| P | 0.001 | 0.819 | 0.001 | 0.669 | |||||
| Responsibility | |||||||||
| T1 | 2.00±0.53 | 2.04±0.62 | 0.424 | 0.55±0.04 | −0.01±0.02 | 0.001 | 0.51±0.04 | 0.06±0.03 | 0.001 |
| T2 | 2.56±0.61 | 2.03±0.57 | |||||||
| T3 | 2.52±0.61 | 2.11±0.57 | |||||||
| P | 0.001 | 0.969 | 0.001 | 0.217 | |||||
| Physical activity | |||||||||
| T1 | 2.18±0.67 | 2.11±0.65 | 0.248 | 0.45±0.04 | 0.02±0.01 | 0.001 | 0.42±0.05 | 0.10±0.03 | 0.001 |
| T2 | 2.63±0.71 | 2.13±0.64 | |||||||
| T3 | 2.60±0.68 | 2.22±0.69 | |||||||
| P | 0.001 | 0.197 | 0.001 | 0.003 | |||||
| Stress management | |||||||||
| T1 | 2.60±0.54 | 2.65±0.59 | 0.497 | 0.29±0.04 | 0.00±0.01 | 0.001 | 0.24±0.04 | −0.02±0.02 | 0.006 |
| T2 | 2.90±0.53 | 2.65±0.58 | |||||||
| T3 | 2.85±0.56 | 2.62±0.58 | |||||||
| P | 0.001 | 1.00 | 0.001 | 0.728 | |||||
*T-test, **GEE. P=Repeated measure, T1=Baseline, T2=After intervention, T3=Follow-up. GEE=Generalized estimating equations, SD=Standard deviation, HPLP II=Health-Promoting Lifestyle Profile II
Comparison of health-promoting lifestyle reveals that the intervention group had significant differences in all dimensions, immediately and 3 months after the intervention. Physical activity of the control group had a significant difference 3 months after the intervention. GEE test results showed that there was a significant difference between the intervention and control groups, immediately and 3 months after the intervention [Table 3].
Spearman correlation test indicated a statistically significant relationship between changes in health literacy and dimensions of appraisal, use, communication with health-promoting lifestyle changes, and all its dimensions at immediately after the intervention in the intervention group [Table 4].
Table 4.
Association between changes in health literacy with Health-Promoting Lifestyle Profile II among participants
| Time | HL | HPLP II | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Condition | HPLP II | Nutrition | Responsibility | Physical activity | Stress management | |||||||
| r | P | r | P | r | P | r | P | r | P | |||
| T2 | Health literacy | Intervention | 0.40 | 0.001 | 0.37 | 0.001 | 0.29 | 0.001 | 0.31 | 0.001 | 0.44 | 0.001 |
| Self-efficacy | Intervention | 0.17 | 0.021 | 0.16 | 0.028 | |||||||
| Access | Intervention | 0.23 | 0.003 | 0.17 | 0.021 | 0.22 | 0.003 | 0.22 | 0.004 | |||
| Reading | Intervention | 0.23 | 0.003 | |||||||||
| Understanding | Intervention | 0.27 | 0.001 | 0.30 | 0.001 | 0.23 | 0.002 | 0.30 | 0.001 | |||
| Appraisal | Intervention | 0.29 | 0.001 | 0.23 | 0.002 | 0.21 | 0.005 | 0.25 | 0.001 | 0.27 | 0.001 | |
| Use | Intervention | 0.42 | 0.001 | 0.30 | 0.001 | 0.39 | 0.001 | 0.29 | 0.001 | 0.26 | 0.001 | |
| Control | 0.17 | 0.016 | ||||||||||
| Communication | Intervention | 0.37 | 0.001 | 0.29 | 0.001 | 0.32 | 0.001 | 0.27 | 0.001 | 0.36 | 0.001 | |
| T3 | Health literacy | Intervention | 0.47 | 0.001 | 0.41 | 0.001 | 0.42 | 0.001 | 0.33 | 0.001 | 0.35 | 0.001 |
| Control | 0.18 | 0.035 | 0.16 | 0.039 | 0.16 | 0.042 | 0.29 | 0.001 | ||||
| Self-efficacy | Intervention | 0.21 | 0.009 | 0.20 | 0.007 | 0.21 | 0.005 | 0.22 | 0.004 | |||
| Control | 0.21 | 0.008 | 0.18 | 0.014 | 0.24 | 0.001 | 0.19 | 0.008 | ||||
| Access | Intervention | 0.29 | 0.001 | 0.20 | 0.011 | 0.27 | 0.001 | 0.27 | 0.001 | 0.25 | 0.001 | |
| Understanding | Intervention | 0.50 | 0.001 | 0.45 | 0.001 | 0.45 | 0.001 | 0.43 | 0.001 | 0.43 | 0.001 | |
| Control | 0.32 | 0.001 | 0.26 | 0.001 | 0.31 | 0.001 | 0.24 | 0.001 | 0.29 | 0.001 | ||
| Appraisal | Intervention | 0.55 | 0.001 | 0.52 | 0.001 | 0.53 | 0.001 | 0.46 | 0.001 | 0.43 | 0.001 | |
| Control | 0.40 | 0.001 | 0.31 | 0.001 | 0.44 | 0.001 | 0.31 | 0.001 | 0.35 | 0.001 | ||
| Use | Intervention | 0.62 | 0.001 | 0.58 | 0.001 | 0.60 | 0.001 | 0.57 | 0.001 | 0.42 | 0.001 | |
| Control | 0.54 | 0.001 | 0.45 | 0.001 | 0.51 | 0.001 | 0.46 | 0.001 | 0.38 | 0.001 | ||
| Communication | Intervention | 0.60 | 0.001 | 0.52 | 0.001 | 0.59 | 0.001 | 0.51 | 0.001 | 0.47 | 0.001 | |
| Control | 0.38 | 0.001 | 0.30 | 0.001 | 0.39 | 0.001 | 0.29 | 0.001 | 0.36 | 0.001 | ||
T2=Immediately after intervention, T3=Follow-up. HPLP II=Health-Promoting Lifestyle Profile II, HL=Health Literacy
Changes in self-efficacy showed a statistically significant association with changes in nutrition and physical activity. There was a statistically significant association between changes in access and understanding the dimensions with changes in health-promoting lifestyle and its dimensions except the health responsibility. There was a significant relationship between changes in reading and changes in stress management. Nevertheless, changes in numeracy had no statistically significant relationship with any dimension of health-promoting lifestyle. In addition, there was a statistically significant relationship between changes in use and changes in stress management in the control group.
Moreover, there was a statistically significant relationship between health literacy changes and its dimensions except reading and numeracy with health-promoting lifestyle changes and all of its dimensions in the intervention group, 3 months after the intervention. Changes in dimensions of understanding, appraisal, use, and communication with health-promoting lifestyle changes and all its dimensions showed a statistically significant relationship in the control group. There was a statistically significant relationship between changes in health literacy and self-efficacy with health-promoting lifestyle changes and its dimensions except stress management in the control group [Table 4].
Discussion
Immediately after the intervention and follow-up, health literacy of the intervention group increased, and the difference between the two groups was statistically significant, which was consistent with the results of the effect of educational interventions on health literacy of Panahi et al.[18] and Kahtari et al.[19] studies on students; Jahani Eftekhari et al.,[20] Solhi et al.,[21] and Tol et al.[22] studies among women; and Peyman et al.[23] study in health-care personnel.
However, this result was unlike Tsai et al. study[24] that PBL-based health literacy program had no effect on immigrant women in Taiwan, which the first reason may be due to applying more dimensions of health literacy in the present study such as use and numeracy that PBL method had more impact on them. The second reason can be the difference in scenarios, and the third reason can be due to not having a language component in the design of their intervention program for immigrants.
The study results can be provided health literacy education with the method of PBL using health-related scenario, because in this method, students learn how to get access to health information when faced with a health problem in their real life. Why and how they read, understand, and analyze health-related information and use it in daily life, learn effective communication skills with health service providers when they have health problems, can make their own health-related calculations, improve their ability to take self-care, and do health-related actions.
Although the intervention group revealed improvement in self-efficacy, differences were statistically significant between the groups immediately after the intervention but were not at follow-up. This result was statistically significantly different in the control group at follow-up that it may be due to health curriculum at schools. Some studies show that health literacy intervention programs enhance their self-efficacy,[20,21,23] whereas another study with PBL method has found no effect.[24]
The mean score of access dimension significantly increased in the intervention group, but there was a significant difference between the two groups immediately after the intervention but was not at follow-up. This study result was consistent with the result of the study by Begoray et al.[25] among students in Canada. This result may be due to factors which influenced the level of students’ access to health information, such as the amount of access to different sources and using possibility of resources for them.
The present study did not exert a positive effect on reading dimension immediately after the intervention and follow-up. This result was contrary to the result of the study by Kahtari et al.[19] that, perhaps, it was because of difference in the intervention methods. It seems that using a self-administered questionnaire for students overestimated their mastery of reading health-related issues, then, that they encountered serious problems by scenario with parts of the brochure of drug they faced with reality.
This research did not confirm an understanding dimension immediately after the intervention and follow-up. The result of this study was consistent with the results of the study by Begoray et al.[25] and was contrary to the result of the research by Kahtari et al.[19] Using a self-administered questionnaire can be a reason. Students overestimated their perception of health-related issues, which they were challenged by the scenario and they realized that had previously overestimated their ability.
There was no significant difference between the groups in the appraisal dimension immediately after the intervention and follow-up. It was unlike the Steckelberg et al.’ study[26] as a critical health literacy intervention for students in Germany. One reason for this may be that, in their study, only had been focused on this dimension of health literacy because critical health literacy skill needs more health-related information and to devote more training sessions to this topic. Another reason can be a statistically significant difference in the control group at follow-up that it may be due to health curriculum at schools.
In accordance with Kahtari et al.[19] study, the analysis showed that the mean score of use dimension increased in the intervention group, and the difference between the two groups was significant immediately after the intervention and follow-up. This result may be applied to the PBL method, which students learned by scenarios, how to use health-related information in real-life situations because the scenarios provided them with patterns appropriate to the age and position of adolescents so that they could use their health-related knowledge appropriately in life.
There was significant difference communication dimension between the groups from pretest to immediately after the intervention, but it was not at follow-up. The present study was consistent with the result of the study by Begoray et al.[25] and contrary to the result of the study by Kahtari et al.[19] The results showed that the PBL method can increase effective communication among people in a group, but various factors are influential in communication with other community members and service providers such as psychological, personality, and family.
Before educational intervention, the control group had higher scores than the intervention group in numeracy dimension. However, the score of numeracy increased in the intervention group, and there was a significant difference between the two groups immediately after the intervention and follow-up. A study by Sezginand et al.[16] in Turkey was a PBL material that had combined some of the physics subjects; it showed that this method was effective and useful and it was consistent with the result of the present study. The reason for this result can be applied to problem-based approach, because students first encountered with a problem and then solve it. Furthermore, using a scenario to teach the sciences that their usage in real life for students is not visible, because of the fascination with reading the story and working with peers in a group, can increase the interest of students in these courses.
The intervention had a significant effect on health-promoting lifestyle, and it increased in the intervention group; the difference between the two groups was significant immediately after the intervention and follow-up. The results of Eftekhari et al. among females[20] and Ahmadizade Fini.[27] on students were consistent with the present research. The reason for this result may be applied to the PBL method by the scenarios because students learned what they should do to maintain and promote their health in daily life and what behaviors they have to do and it also taught how to change behavior.
The mean score of nutrition in the intervention group was increased after the intervention, and the difference between the two groups was significant immediately after the intervention and follow-up. Vahdat-Shariatpanahi and Vahdat-Shariatpanahi study[28] also showed that the PBL method had a positive effect on improving student score in the nutrition course of midwifery students. When students learned to calculate their daily calorie intake and compare them with the most amount of calories required by a teenager in a day by the scenario, furthermore, discovered how to read food labels and check it, they can distinguish between healthy and unhealthy foods.
Physical activity increased after the intervention in the intervention group, and the difference between the groups was significant immediately after the intervention and follow-up. The results of Gholamnia-Shirvani et al.[29] study on women's physical activity were consistent with the present study. Because of using the scenario, students learned how to get the physical activity that they needed to fit, in and out of school and home. Using the PBL approach and its emphasis on real-life scenarios, students can be patterned in accordance with their age and physical and educational statuses so that they can increase their physical activity without spending time and money.
This intervention had a significant effect on health responsibility in the intervention group, and the difference between the two groups was significant immediately after the intervention and follow-up. This result was consistent with the results of Ahmadizade Fini[27] and Eftekhari et al.[20] studies. The reason for this may be the increased sensitivity of students in this regard and showing problems that will be in the future if they neglect their health.
The mean score of stress management increased after the intervention in the intervention group, and the difference between the groups was significant immediately after the intervention and follow-up. The present result was consistent with the result of the study by Skre et al.[30] of mental health literacy intervention in Norwegian and Ahmadizade Fini.[27] The reason for this can be to inform students about the effects of stress on health and illness in future and to emphasize health preferences over other issues and the impact of health on their lives and their families and to teach them ways to control stress through scenarios.
There was a significant relationship between health literacy changes and its dimensions except reading dimension and calculation with changes in health-promoting lifestyle and its dimensions, and the greatest relationship was between the changes in the use and then in dimensions of communication, appraisal, and understanding with health-promoting lifestyle changes. A study by Bayati et al.[31] on health ambassadors in health center showed a significant direct correlation of health literacy with all dimensions of health-promoting behavior before and after the intervention. A study by Chahardah-Cherik et al.[32] on diabetic patients and Aghamolaei et al.[33] among students also showed a significant relationship between all dimensions of health-promoting behaviors and health literacy.
This result shows that adolescents need a believable learning method of using health-related informations in real life, furthermore, it is a crutial neeed to have an effective communication between health professionals and them.
It also indicated the importance of empowering adolescents to understand and evaluate health-related information for promoting their lifestyle. To provide health-related information and healthy lifestyle, it should be clearly informed that teenagers can understand and evaluate subjects, and by taking into consideration their use in real life, to reach proper decision-making. It is also worthy that health information gives different ways of informing and using communication channels and social networks for adolescents.
The limitations of this study were using self-administered questionnaires and nongeneralization of results to all girl students. Moreover, this study was performed only on girl students and cannot be a complete comparison of students in both sexes.
The strengths of the study can be noted intervention which included a health literacy-based curriculum and implementation in schools. Furthermore, all dimensions of health literacy and health-promoting lifestyle instruments investigated simultaneously. Furthermore, health literacy questionnaire which used in this study, especially designed for adolescents. We implemented scenarios involving health literacy and health-promoting behaviors in a combination of both them in different dimensions appropriate to the age of adolescents in school, which can be the innovations of the present study.
Conclusion
It seems that designing intervention programs using PBL approach can lead to health-related behavior change and can provide an organized framework to health planners and health policymakers because healthy lifestyle can reduce the medical costs in modern societies. This study also showed a necessity for an innovation in the educational system. It is suggested using PBL problem-based method for teaching courses such as health-related behaviors and mathematics. Further researches are needed to develop an effective intervention to improve health-promoting behaviors among other target groups.
Financial support and sponsorship
The research has been done with the financial support of Education and Reaserch Deputy of Tehran University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This manuscript is part of a master's thesis in Health Education and Research Project approved by TUMS (Project Approval Code: 39304, IRCT2013213012460N16), whereby we thank TUMS for their financial support. The authors thank Tehran General Directorate of Education in districts of 10, 11, and 17, educational authorities of schools, and students who help the researchers to conduct the research project.
References
- 1.Khaleghparast S, Maleki A, Salesi M, Ghanbari B, Maleki M. Relationship between health literacy and adherence to treatment in cardiac patients. Iran Heart J. 2019;20:27–35. [Google Scholar]
- 2.Golluche FS, Jalili Z, Tavakoli R, Ghanbari S. The study of relationship between health literacy and nutritional practice in high school adolescents in Tehran. Iran J Health Educ Health Promot. 2017;5:224–30. [Google Scholar]
- 3.Montazeri A, Tavousi M, Rakhshani F, Azin S, Jahangiri K, Ebadi M, et al. Health literacy for Iranian adults (helia): Development and psychometric properties. Payesh.Journal of the Iranian Institute for Health Sciences Research. 2014;13:589–99. [Google Scholar]
- 4.Marmot M, Friel S, Bell R, Houweling TA, Taylor S Commission on Social Determinants of Health. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet. 2008;372:1661–9. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 5.Chang LC. Health literacy, self-reported status and health promoting behaviours for adolescents in taiwan. J Clin Nurs. 2011;20:190–6. doi: 10.1111/j.1365-2702.2009.03181.x. [DOI] [PubMed] [Google Scholar]
- 6.Ghanbari S, Ramezankhani A, Montazeri A, Mehrabi Y. Health literacy measure for adolescents (HELMA): Development and psychometric properties. PLoS One. 2016;11:e0149202. doi: 10.1371/journal.pone.0149202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hazavehei SM, Pirzadeh A, Entezari MH, Hasanzadeh A. The effect of educational program based on basnef model on the nutritional behavior of students. Zahedan J Res Med Sci. 2011;13:23–9. [Google Scholar]
- 8.Eckman MH, Wise R, Leonard AC, Dixon E, Burrows C, Khan F, et al. Impact of health literacy on outcomes and effectiveness of an educational intervention in patients with chronic diseases. Patient Educ Couns. 2012;87:143–51. doi: 10.1016/j.pec.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 9.Savery JR. Vol. 9. West Lafayette: Purdue University Press; 2015. Overview of Problem-based Learning: Definitions and Distinctions. Essential Readings in Problem-based Learning: Exploring and Extending the Legacy of Howard S. Barrows; pp. 5–15. [Google Scholar]
- 10.Noohi E, Abbaszadeh A, Madah SS, Borhani F. Collaborative learning experiences in problem-based learning (pbl) education: A qualitative study. J Qual Res Health Sci. 2013;1:255–67. [Google Scholar]
- 11.Mansoori S, Abedini-baltork M, Lashkari H, Bagheri S. Effectiveness of problem-based learning on student's academic performance: A quasi-experimental study. Res Med Educ. 2017;9:8–1. [Google Scholar]
- 12.Taymoori P, Lubans DR. Mediators of behavior change in two tailored physical activity interventions for adolescent girls. Psychol Sport Exerc. 2008;9:605–19. [Google Scholar]
- 13.Piri N, Garmaroudi G, Noori K, Azadbakht M, Hashemi S. Health-promoting behaviors among female students in primary and secondary high school levels in poldokhtar in 2014. Yafte. 2015;17:47–56. [Google Scholar]
- 14.Walker S, Hill-Polerecky D. Psychometric Evaluation of the Health-Promoting Lifestyle Profile II. Unpublished Manuscript, University of Nebraska Medical Center. 1996:120–6. [Google Scholar]
- 15.Mohamadian H, Eftekhar AH, Taghdisi MH, Mousavi GA, Sabahi BM. Psychometric properties of the health-promoting lifestyle profile (HPLP II) in a sample of iranian adolescents.Payesh. 2013;12:167–76. [Google Scholar]
- 16.Sezgin Selçuk G. A problem-based learning scenario that can be used in science teacher education. Asia Pac Forum Sci Learn Teach. 2015;16:1–26. [Google Scholar]
- 17.Şahin M. The importance of efficiency in active learning. J Turk Sci Educ. 2007;4:61–74. [Google Scholar]
- 18.Panahi R, Ramezankhani A, Tavousi M, Osmani F, Karami A, Niknami S. The effect of educational intervention on health literacy and adoption of smoking preventive behaviors among university students. J Educ Community Health. 2018;5:29–37. [Google Scholar]
- 19.Kahtari M, Farmanbar R, Kasmaei P, Omidi S. The effect of the educational intervention on health literacy level in the girl students. J Health Lit. 2017;2:187–97. [Google Scholar]
- 20.Jahani Eftekhari M, Peyman N, Doosti H. The effect of educational intervention based on the self efficacy and health literacy theory on health promoting lifestyles among female health volunteers of Neyshabur, Iran. J Health Dev. 2018;6:302–13. [Google Scholar]
- 21.Solhi M, Abbasi K, Ebadi Fard Azar F, Hosseini A. Effect of health literacy education on self-care in pregnant women: A randomized controlled clinical trial. Int J Community Based Nurs Midwifery. 2019;7:2–12. doi: 10.30476/IJCBNM.2019.40841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tol A, Pourreza A, Rahimi Foroshani A, Tavassoli E. Assessing the effect of educational program based on small group on promoting knowledge and health literacy among women with type 2 diabetes referring to selected hospitals affiliated to tehran university of medical sciences. Razi J Med Sci. 2013;19:10–19. [Google Scholar]
- 23.Peyman N, Behzad F, Taghipour A, Esmaily H. Assessment of the effect of a health literacy educational program for health personnel on promoting self-efficacy among patients with chronic diseases. Health System Research. 2016;12:350–7. [Google Scholar]
- 24.Tsai TI, Lee SD, Yu WR. Impact of a problem-based learning (PBL) health literacy program on immigrant women's health literacy, health empowerment, navigation efficacy, and health care utilization. J Health Commun. 2018;23:340–9. doi: 10.1080/10810730.2018.1445798. [DOI] [PubMed] [Google Scholar]
- 25.Begoray DL, Wharf-Higgins J, Macdonald M. High school health curriculum and health literacy: Canadian student voices. Glob Health Promot. 2009;16:35–42. doi: 10.1177/1757975909348101. [DOI] [PubMed] [Google Scholar]
- 26.Steckelberg A, Hülfenhaus C, Kasper J, Mühlhauser I. Ebm@school – A curriculum of critical health literacy for secondary school students: Results of a pilot study. Int J Public Health. 2009;54:158–65. doi: 10.1007/s00038-008-7033-1. [DOI] [PubMed] [Google Scholar]
- 27.Ahmadizade Fini E. Effect of peer education on health promoting behaviors of junior high school students. Iran J Health Educ Promot. 2015;3:105. [Google Scholar]
- 28.Vahdat-Shariatpanahi SZ, Vahdat-Shariatpanahi M. Presenting the course of nutrition as problem based learning through lecturing and its impact on the educational progression of midwifery students. J Mazandaran Univ Med Sci. 2014;22:59–63. [Google Scholar]
- 29.Gholamnia-Shirvani Z, Ghofranipour F, Gharakhanlo R, Kazemnezhad A. Improving and maintaining physical activity and anthropometric indices in females from Tehran: Application of the theory of planned behavior. J Educ Community Health. 2016;2:13–24. [Google Scholar]
- 30.Skre I, Friborg O, Breivik C, Johnsen LI, Arnesen Y, Wang CE. A school intervention for mental health literacy in adolescents: Effects of a non-randomized cluster controlled trial. BMC Public Health. 2013;13:873. doi: 10.1186/1471-2458-13-873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bayati T, Dehghan A, Bonyadi F, Bazrafkan L. Investigating the effect of education on health literacy and its relation to health-promoting behaviors in health center. J Educ Health Promot. 2018;7:127. doi: 10.4103/jehp.jehp_65_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chahardah-Cherik S, Gheibizadeh M, Jahani S, Cheraghian B. The relationship between health literacy and health promoting behaviors in patients with type 2 diabetes. Int J Community Based Nurs Midwifery. 2018;6:65–75. [PMC free article] [PubMed] [Google Scholar]
- 33.Aghamolaei T, Hosseini Z, Hosseini F, Ghanbarnejad A. The relationship between health literacy and health promoting behaviors in students. J Prev Med. 2016;3:36–43. [Google Scholar]