Abstract
Mediastinal nonseminomatous germ cell tumor (NSGCT) is rare. NSGCT shows excellent response to cisplatin-based chemotherapy. However, some tumors continue to enlarge despite normal tumor markers after chemotherapy, a rare condition called growing teratoma syndrome (GTS). Recognition of this condition is imperative for prompt surgical resection to prevent further cardiopulmonary compression and to improve survival. Multidisciplinary team meeting is important for perioperative preparation and care to improve the outcome of this high-risk surgery. Here, we report two cases of mediastinal GTS and underwent surgical resection, of which one died of pericardial decompression syndrome and the other is well.
Keywords: Growing teratoma syndrome, mediastinal germ cell tumors, nonseminomatous germ cell tumors
Primary mediastinal malignant germ cell tumor is rare and represents 1%–4% of mediastinal tumors, of which 50%–70% are nonseminomatous germ cell tumors (NSGCTs).[1] Mediastinal NSGCT occurs almost exclusively in young males and it grows rapidly which often causes compression and invasion to mediastinal structures such as airway and major vessels. NSGCT shows excellent response to cisplatin-based chemotherapy evidenced by significant reduction or normalized serum tumor markers, alpha-fetoprotein (AFP) and beta-human chorionic gonadotrophin (B-HCG), and tumor shrinkage. However, 3%–8% of cases experienced enlarging tumor with compressive symptoms despite normalization of tumor markers after chemotherapy may indicate growing teratoma syndrome (GTS).[2]
GTS encompasses three criteria: (1) normalization of previously elevated tumor markers, AFP and B-HCG, after chemotherapy, (2) an increase in tumor size during or after chemotherapy with the presence of compressive symptoms, and (3) absence of NSGCT component other than mature teratoma in histopathology of the resected tumor.[3] Although histopathologically benign, teratoma is nonchemosensitive and can be locally aggressive which results in significant morbidity by compression on the nearby structures.[2] Hence, surgery is the only curative option for GTS to prevent further cardiopulmonary deterioration.[4]
Here, we report two cases of mediastinal GTS who underwent surgical resection, of which one died of pericardial decompression syndrome (PDS) and the other is well. Both histopathology reports confirmed matured teratoma.
Case Reports
Case report 1
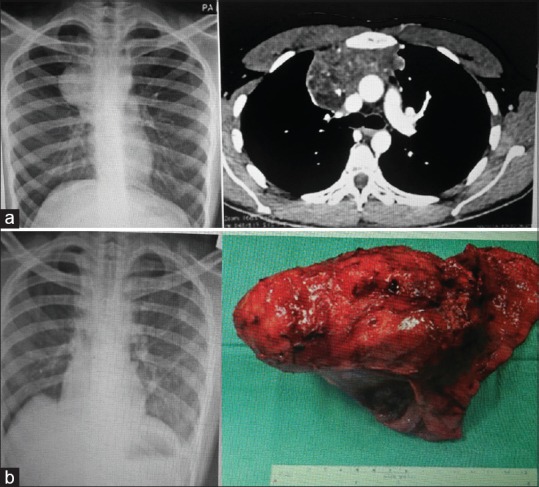
A 22-year-old male presented with cough and shortness of breath for 3 months. His chest X-ray (CXR) and computed tomography (CT) scan of the thorax showed huge mediastinal mass occupying the entire left hemithorax with mediastinal shift [Figure 1a]. His AFP and B-HCG were markedly raised. He was diagnosed with mediastinal NSGCT and underwent the first-line chemotherapy bleomycin, etoposide, and cisplatin (BEP), followed by the second line of paclitaxel, infosfamide, and cisplatin (TIP), because his tumor markers were normalized, but both tumor size and compression symptoms increased. After 4 weeks of completing chemotherapy and multidisciplinary discussion, he underwent clamshell sternothoracotomy, resection of the mediastinal tumor, pericardiectomy, and left phrenic nerve and nonanatomoical left upper lobe resection. The resected tumor size was 24 cm × 21 cm and weighed 2.6 kg [Figure 1b]. He was nursed in the intensive care unit (ICU) for 6 days. He was discharged home 3 weeks after surgery but only to readmit a week later with failure symptoms. He succumbed 2 weeks later due to acute heart failure secondary to PDS. His histopathology result revealed mature teratoma with no viable tumor.
Figure 1.

(a) Preoperative chest X-ray and computed tomography thorax, postoperative chest X-ray. (b) Resected tumor and surgical incision
Case report 2
A 20-year-old male presented with superior vena cava (SVC) syndrome, facial congestion, shortness of breath, and prominent veins over the upper chest. His CXR and CT thorax showed mediastinal mass compressing the left innominate vein and SVC [Figure 2a]. He underwent both first-line (BEP) and second-line (TIP) chemotherapy and regimens. Two weeks after the second-line chemotherapy, his AFP and B-HCG were normalized but CT thorax showed increase in tumor size and persistent SVC compression. He underwent right hemiclamshell sternothoracotomy and resection of tumor with ligation of left innominate vein 5 weeks after chemotherapy [Figure 2b]. Postoperatively, he was nursed in the ICU for a day. Other than transient left upper limb edema which resolved within 6 weeks after surgery, his recovery was unremarkable and discharged home at day 6 of surgery. His histopathology result showed matured teratoma with no viable tumor and margins consistent with fibrotic and necrotic tissue. Currently, he is 6 months after surgery with resolved SVC syndrome.
Figure 2.
(a) Preoperative chest X-ray and computed tomography thorax. (b) Postoperative chest X-ray and resected tumor
Discussion
Surgery of mediastinal GTS is challenging with significant mortality and morbidity because the surgery involves resections of the lung, phrenic nerve, pericardium, great vessels, cardiac chambers, and meticulous postoperative care including fluid balance and respiratory support.[1] It is reported 4% of operative mortality secondary to pulmonary complications.[1] More than that, patients with mediastinal NSGCT have overall poor prognosis despite treatment, with 5-year survival rate between 30% and 48%.[5]
Despite all the unfavored factors, surgery remains the only curative treatment for patients with mediastinal GTS. Early recognition of GTS and prompt referral by the oncology team for surgery are important. Kesler et al. advocated discontinuation of chemotherapy once GTS is suspected and referred for surgical resection to prevent further cardiopulmonary deterioration.[4]
These two cases of mediastinal GTS are the pioneers operated in our center to date.
A thorough preoperative plan between surgeons and anesthesiologists was agreed on to address all possibilities before surgery. Site for line placement, method of intubation and the contingency plan if airway cannot be secured, position of patient in which the surgery will be carried out, and the fluid resuscitation measures were discussed before and during the surgery.
Case 1 was readmitted 1 week after discharge for worsening orthopnea with persistent tachycardia and tachypnea. His workup for sepsis and thromboembolic event was negative. He experienced PDS, a rare complication of acute cardiac failure after decompression for cardiac tamponade,[6] whereas in case 1 decompression from the tumour. After removal of tumor, there was increased venous return that leads to expansion of the right ventricle at the expense of the left ventricle, resulting in acute left-sided cardiac failure and pulmonary edema. One-third of the patients with PDS will end up dead.[6] This is an unexpected complication despite successful surgery.
However, in Case 2, the tumor was smaller but encased the innominate vein. Resection of the left innominate vein was inevitable to make a complete oncological clearance. The resolution of ipsilateral upper limb edema was compensated by the collateral veins formed.
Recurrence rate of GTS following complete resection is as low as 4%, whereas in incomplete resection, the recurrence rate is up to 83%.[7] The two-case series demonstrated that complete surgical resection with clear margin can be accomplished despite the huge tumor size and challenging perioperative care.
In conclusion, complete surgical resection of mediastinal GTS is the mainstay of treatment and should be done in specialized centers. Early identification of patients needing surgical resection is important to prevent worsening compression effect. PDS needs to be anticipated postoperatively in patients with significant mediastinal shift due to tumor compression on the heart.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Takeda S, Miyoshi S, Ohta M, Minami M, Masaoka A, Matsuda H. Primary germ cell tumors in the mediastinum: A 50-year experience at a single Japanese institution. Cancer. 2003;97:367–76. doi: 10.1002/cncr.11068. [DOI] [PubMed] [Google Scholar]
- 2.Afifi HY, Bosl GJ, Burt ME. Mediastinal growing teratoma syndrome. Ann Thorac Surg. 1997;64:359–62. doi: 10.1016/S0003-4975(97)00581-X. [DOI] [PubMed] [Google Scholar]
- 3.Iwata H, Mori Y, Takagi H, Shirahashi K, Shinoda J, Shimokawa K, et al. Mediastinal growing teratoma syndrome after cisplatin-based chemotherapy and radiotherapy for intracranial germinoma. J Thorac Cardiovasc Surg. 2004;127:291–3. doi: 10.1016/s0022-5223(03)01300-x. [DOI] [PubMed] [Google Scholar]
- 4.Kesler KA, Patel JB, Kruter LE, Birdas TJ, Rieger KM, Okereke IC, et al. The “growing teratoma syndrome” in primary mediastinal nonseminomatous germ cell tumors: Criteria based on current practice. J Thorac Cardiovasc Surg. 2012;144:438–43. doi: 10.1016/j.jtcvs.2012.05.053. [DOI] [PubMed] [Google Scholar]
- 5.Sarkaria IS, Bains MS, Sood S, Sima CS, Reuter VE, Flores RM, et al. Resection of primary mediastinal non-seminomatous germ cell tumors: A 28-year experience at Memorial Sloan-Kettering Cancer Center. J Thorac Oncol. 2011;6:1236–41. doi: 10.1097/JTO.0b013e31821d513e. [DOI] [PubMed] [Google Scholar]
- 6.Imazio M. Pericardial decompression syndrome: A rare but potentially fatal complication of pericardial drainage to be recognized and prevented. Eur Heart J Acute Cardiovasc Care. 2015;4:121–3. doi: 10.1177/2048872614557771. [DOI] [PubMed] [Google Scholar]
- 7.Sachdeva AK, Penumadu P, Kohli P, Dubashi B, Munuswamy H. Growing teratoma syndrome in primary mediastinal germ cell tumor: Our experience. Asian Cardiovasc Thorac Ann. 2019;27:98–104. doi: 10.1177/0218492318823345. [DOI] [PubMed] [Google Scholar]


