Abstract
INTRODUCTION:
Protection against financial risks is one of the important goals of the health system. The present study aims to determine the rate of exposure to catastrophic expenditures in the insured inpatients.
METHODS:
The present study was cross-sectional one which is conducted in 2016. The statistical population comprised all the insured patients presenting to a private hospital in Qom who presented to the hospital within 4 months from December 2015 to March 2016. Random convenience sampling method was used, and the sample size was estimated at 267 people using Cochran formula. A questionnaire was employed for data gathering. Data were analyzed using Chi-square test and logistic regression using SPSS software version 20.
RESULS:
Patients exposed to catastrophic expenditures of treatment accounted for the 54.8% of the cases. The highest rate of being exposed to the catastrophic expenditures was related to the insured patients of the Universal Health Insurance Fund (UHIF). People with rural insurance, on average, paid the highest cost of treatment in the hospital. The surgical ward and critical care unit accounted for the biggest percentage of the patients who incurred catastrophic expenditures. Being rural, longer length of stay, lower education of the head of the household, lack of supplementary insurance coverage, and being in UHIF coverage have a substantial relationship with being exposed to catastrophic expenditures.
DISCUSSION:
The socioeconomic status of the insured people in the UHIF and the Rural Insurance Fund was worse than other funds in terms of less utilization and higher rate of exposure to catastrophic expenditures, and this issue requires the adoption of specific targeted policies for these groups in respect with reducing out-of-pocket payments through mechanism such as stepwise copayments, maximum out-of-pocket limit, fee exemptions or waiver and providing supplementary insurance to reduce the exposure to catastrophic expenditures.
Keywords: Catastrophic expenditures, health insurance, hospital, Iran, private
Introduction
Despite attempts made in the field of fair health security of health services, it is still observed that health security of health services in developing countries takes place with the dominance of out-of-pocket payments and the relative shortage of prepayment mechanisms, such as taxes and health insurance. Unfortunately, one of the adverse results of such financing method includes the ocurrence catastrophic expenditures when households are exposed to illness.[1] In health economics literature, the catastrophic expenditures of health services are defined as the amount of expenditure spent on health services that exceed a certain level of income.[2]
According to the World Health Organization, households with a health expenditure of more than 40% of their affordance level are considered as exposed to the catastrophic expenditures. The household's capacity to pay to the household income is minus the costs of livelihood or in fact the cost of food.[3,4] Because of the high cost of health care needs, nearly 44 million households, i.e., more than 150 million people worldwide are incurred by the catastrophic expenditures on health, and more than 100 million people are pushed to poverty line due to the catastrophic expenditures.[5,6]
One of the three functional goals of each health system is protecting against financial risks, and due to the effect of this goal on the other two (health status, customer satisfaction), healthcare policy-makers today need to give more attention to this issue, and that lack of financial protection in health is recognized as the disease of health systems. The clearest sign is that households are suffering not merely from the burden of illness, but also from economic poverty, i.e., being exposed to the catastrophic expenditures and poverty caused by health financing.[7]
Discussions on health services financing mixture have always been one of the primary challenges facing health system planners and policy-makers, particularly in developing countries.[8] Paying for health care is a source of concern for households in many nations of the globe, as it often happens unpredictably, and if it is not properly covered, costs can be threatening even for high-income families. The ratio of costs in relation to the income may be too high, leading to catastrophic financial harm for the household or pushing households into poverty trap.[9] Many households refuse to pursue and meet their health needs due to the lack of financial resources to afford their expenses, which can deteriorate the health of the individual and society in general.[6]
The most significant and widespread reforms of the health sector over the past decades in the country were adopted in 2014 as Health Transformation Plan (HTP) with a large budget. In the first step of HTP, and with regard to the policies developed to implement this national program throughout the country, the first protection step for people against health spending was formed with a reduction in payments from 40% to 10% only in governmental hospital. Then, in the second step of HTP, by reviewing the relative values of health services, it was stipulated that patients with basic health insurance should pay only 6% of the amount of the bill on the basis of the tariff and the approved price. Furthermore, people who refered to the hospital through the referral system include villagers, nomads, and residents of cities under 20,000 population (with a rural insurance) pay 3% of the cost of the service (although then it returned to previous rate of 10%). Moreover, in the free insurance coverage plan, those who were not covered by any of the basic health insurance were covered by the Iran health insurance organization without a premium.[10]
The present study aims to determine the rate of patients’ exposure to catastrophic expenditures in the insured patients of different health insurance organizations’ funds in Qom province and to evaluate the current status of the insured patients’ affordability after 1 year of HTP implementation in a private hospital. The current study deals with the insurer's vision to the vulnerability of the insured against catastrophic expenditures of treatment. This issue indicates the financial protection stutus of the insured in the health system, which is a distinctive feature and innovation of the present study.
Methods
The present study was cross-sectional one which is conducted in 2016. The statistical population includes all the insured patients who come to a private hospital in Qom who presented to the hospital within 4 months from December 2015 to March 2016.The hospital is a general private center. The importance of being general reflects the distribution of rates of exposure to catastrophic expenditures in terms of sickness and hospitalization ward, which provides the insurer with a really significant finding considering the necessity of formulating prevention policies. The importance of admission to a private hospital is due to the lack of financial affordability of the patient to pay private tariffs on the one hand and high rates of admission to private hospitals, especially in the deficiency of government facilities in intensive beds. In addition, other study showed that due to an increase in the level of basic insurance coverage after HTP, and therefore demand stimulation in the public sector and lack of growth in services supply, many of the patients are inevitably referred to the private sectors with much higher expenditure, which is likely to be effective in increase of out of pocket (OOP) and exposure rate to catastrophic health expenditure (CHE).[11] The inclusion criteria for getting into the study were hospitalized during the period from December 2015 to March 2016 and willingness to complete the questionnaire with informed consent. The costly wards of the hospital, including special wards (intensive care unit [ICU], critical care unit [CCU], ICU-open heart [OH]), surgical wards, angiography, as well as lower cost wards including internal Medicine Department (three internal wards) were chosen as research environments. Sampling of costly wards of the hospital was done on the number of beds, availability of volunteers to participate in the survey, and culmination of the questionnaire.
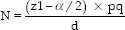
The number of insured people admitted to the hospital is 400/month, where approximately 1200 insured people were taken to the infirmary in the above 3 months. Since there was no exact data on the rate of incidence of catastrophic expenditures among the insured patients in general hospitals of Qom, the rate of occurrence of these costs was considered as 50% (P = 50%). In the next step, considering the confidence interval 95% (α =0.05) and the accuracy of d = 0.06, the sample size was estimated as 267 individuals based on using Cochran formula.
Nonrandom convenience sampling method was used. Patients willing to participate in the study completed the questionnaire. The questionnaire developed by Ghiasvand et al. was used to calculate the amount of exposure to catastrophic expenditures.[12] The validity of the questionnaire was approved by five professors and experts in the area of health economics. The test–retest method was also employed as a questionnaire to examine the reliability of the questionnaire, for which 25 questionnaires were distributed among 25 patients who were part of the research population at a 10-day interval, and the Cronbach's alpha coefficient was obtained 85% between the answers.
To gather data about the direct costs of treatment, the patients who had the inclusion criteria were offered with the questionnaires. The study objectives were explained to patients/patient accompaniment with adequate physical/mental conditions to take part in the study and complete the questionnaire, and individuals were guaranteed that the data would stay secret. Patient billing costs were also obtained from the hospital income unit.
To find the rate of exposure to the catastrophic expenditures of health care services, the portion of the cost of health care to the households’ ability to pay was used. The ability to pay is also received from the household's total expenditure over a specified period of time, minus the cost of food during the same stop. If the portion is higher than 0.4, and/or in other words, if the expenditures on health care costs is higher than 40% of household capacity, it is alleged that the family is being exposed to catastrophic expenditures. Because access to household expenditure over a given point was difficult due to the conditions of the patient and his/her accompaniments, researchers used average annual earnings as substitute variables.[13] The catastrophic expenditures of households were estimated based on the WHO formula. Data were analyzed using SPSS software version 16 [SPSS Inc.: Chicago, IL, USA]. Descriptive statistics (including frequency, mean and standard devation), Chi-square analysis tests, and logistic regression were used to evaluate the relationship between independent variables and dependent variables.
Results
Descriptive findings
Tables 1 and 2 indicates the distribution of respondents’ demographic variables. Roughly 88% of the family heads were male and the rest were women. The greatest number of households ranged between two to four, and most of them resided in the village (85.7%). Most of the insured patients had Universal Health Insurance Fund (UHIF) and employee insurance. Patients with supplementary insurance accounted for 51.5% of the individuals, and roughly 55% of the patients were exposed to catastrophic expenditures of treatment.
Table 1.
Demographic characteristics of the study samples
| Demographic factors | Frequency (%) | Demographic factors | Frequency (%) |
|---|---|---|---|
| The patient’s gender | Having supplementary insurance | ||
| Male | 121 (45.5) | Have it | 137 (51.5) |
| Female | 145 (54.5) | Do not have it | 129 (48.5) |
| Family supervisor gender | Residential house ownership | ||
| Male | 233 (87.9) | Private | 236 (88.7) |
| Female | 32 (12.1) | Leased | 30 (11.3) |
| Place of residence | Private car ownership | ||
| Village | 38 (85.7) | Have it | 139 (52.3) |
| City | 228 (14.3) | Do not have it | 127 (47.7) |
| Patient education | Level of education of the patient’s family head | ||
| Illiterate | 78 (29.3) | Illiterate | 55 (20.7) |
| Under the diploma | 110 (41.4) | Under the diploma | 108 (40.6) |
| Diploma | 38 (14.3) | Diploma | 43 (16.2) |
| Associate Degree | 8 (3) | Associate degree | 15 (5.6) |
| Bachelor’s | 28 (10.5) | Bachelor’s | 34 (12.8) |
| Master’s | 4 (1.5) | Master’s | 9 (3.4) |
| PhD | 2 (0.8) | ||
| The job of household head | Earnings | ||
| Unemployed | 42 (15.8) | <8000000 rials | 68 (25.7) |
| Retired | 48 (18) | 8000000 rials and 13000000 rials | 71 (26.8) |
| Employee | 27 (10.2) | ||
| Worker | 12 (4.5) | 13000000 rials and 20000000 rials | 72 (27.2) |
| Self-employed | 113 (42.5) | ||
| Manager | 2 (0.8) | ||
| University professor | 4 (1.5) | >20000000 rials | 54 (20.4) |
| Unable to work | 5 (1.9) | ||
| Veteran | 13 (4.9) | ||
| Insurance funds | Exposure to catastrophic costs | ||
| Employee | 91 (34.2) | Yes | 144 (54.8) |
| Other classes | 60 (22.6) | ||
| Rural | 22 (8.3) | No | 119 (45.2) |
| Universal health | 88 (33.1) | ||
| Iranians | 5 (1.9) | Total | 263 (100) |
| Total | 266 (100) |
Table 2.
Descriptive Statistics of the research variables
| Variable name | mean | The standard deviation |
|---|---|---|
| Age | 59.05 | 15.31 |
| Length of hospitalization (days) | 5.44 | 9.14 |
| Length of hospitalization in the last year (days) | 4.73 | 15.49 |
| Outpatient costs (Rials) | 2,300,000 | - |
| Number of family members | 3.13 | 1.42 |
| The number of family members with the disease | 1.11 | 0.315 |
| Premium (Rials) | 227,000 | - |
| Costs paid in hospital | 11,500,000 | - |
As shown in Table 3, the mean cost of hospitalization and outpatient costs among people facing catastrophic expenditures is much more than other people.
Table 3.
The average hospitalization costs and outpatient costs separated by individuals exposed to the catastrophic expenditures and other people
| Variable name | Hospitalization costs | Outpatient costs | ||
|---|---|---|---|---|
| does not have catastrophic expenditures | Has catastrophic expenditures | does not have catastrophic expenditures | Has catastrophic expenditures | |
| Mean (Rials) | 1,260,000 | 19,800,000 | 673,000 | 3,690,000 |
Based on Table 4, people with rural insurance, on average, paid the highest cost of treatment in the hospital. The lowest cost, on average, is also paid by people of other funds. ICU and ICU-OH wards, followed by ICUs, internal medicine, general surgery, neurology, CCU, Internal Cardiac and Angiography wards, respectively, accounted for the highest average cost of hospital payment. Furthermore, the results showed that General Surgery and CCU accounted for the highest proportion of patients with catastrophic expenditures.
Table 4.
The mean of costs paid in hospitals separated by the hospitalization wards and fund
| Hospitalization ward | The mean cost of payments in the hospital (rials) | Insurance fund | The mean cost of payments in the hospital (rials) |
|---|---|---|---|
| Internal Cardiac | 4,900,000 | Employees | 6,000,000 |
| CCU | 5,140,000 | Other classes | 3,000,000 |
| ICU OH | 37,500,000 | rural | 27,000,000 |
| angiography | 3,690,000 | UHIF | 18,000,000 |
| General surgery | 11,300,000 | Iranians | 26,000,000 |
| ICU | 22,000,000 | ||
| Internal | 16,600,000 | ||
| Internal Neurotics | 6,700,000 |
Bivariate relationships
The results of Table 5 show that with regard to the relationship between the patient's income and the cost of treatment, as expected, patients exposed to the catastrophic expenditures were those with lower income.
Table 5.
Investigating the status of exposure to catastrophic costs in terms of income groups and separated by different funds
| Variable name | Catastrophic costs | ||
|---|---|---|---|
| Do not have (%) | Has it (%) | Total (%) | |
| Income | |||
| <8000000 rials | 8 (11.8) | 60 (88.2) | 68 (100) |
| 8000000 rials and 13000000 rials | 36 (50.7) | 35 (49.3) | 71 (100) |
| 13000000 rials and 20000000 rials | 36 (50.7) | 35 (49.3) | 71 (100) |
| >20000000 rials | 39 (73.6) | 14 (26.4) | 53 (100) |
| Total | 119 (45.2) | 144 (54.8) | 263 (100) |
| Insurance fund | |||
| Employees | 59 (49.6) | 29 (20.1) | 88 (33.5) |
| Other classes | 50 (42.0) | 10 (6.9) | 60 (22.8) |
| Rural | 0 (0.0) | 22 (15.3) | 22 (8.4) |
| Universal health | 9 (7.6) | 79 (54.9) | 88 (33.5) |
| Iranians | 1 (8) | 4 (2.8) | 5 (1.9) |
| Total | 119 (100) | 144 (100) | 263 (100) |
| Chi-square test statistic, significance level | 115, 0.00 | ||
| Job of the household head | |||
| Unemployed | 20 (16.8) | 22 (15.3) | 42 (16) |
| Retired | 33 (27.7) | 14 (9.7) | 47 (17.9) |
| Employee | 19 (16) | 7 (4.9) | 26 (9.9) |
| Worker | 1 (8) | 11 (7.6) | 12 (4.6) |
| Self-employed | 28 (23.5) | 84 (58.3) | 112 (42.6) |
| Manager | 2 (1.7) | 0 (0.0) | 2 (0.8) |
| University professor | 2 (1.7) | 2 (1.4) | 4 (1.5) |
| Unable to work | 2 (1.7) | 3 (2.1) | 5 (1.9) |
| Veteran | 12 (10.1) | 3 (2.1) | 13 (4.9) |
| Total | 119 (100) | 144 (100) | 263 (100) |
| Chi-square test statistic, significance level | 59.3, 0.00 | ||
As viewed in Table 5, most of the patients presenting to the hospital were self-employed, and most of them were exposed to catastrophic expenditures. The unemployed also accounted for 16% of the total number of people that their number of vulnerable people to those not exposed to catastrophic expenditures is more eminent. Of course, retirees also account for a substantial share of clients, with the difference that most of them were not exposed to catastrophic expenditures. The Chi-square test was applied to investigate the relationship between family head and vulnerability of people. The results suggest the significance of the relationship which is shown in the above table. As envisioned, the type of insurance fund is linked to the catastrophic expenditures. People who are exposed to the catastrophic expenditures are often covered by UHIF, and high percentage of people with employees and other classes insurance (except the covered people of the welfare organization) are not vulnerable compared to other funds.
Table 6 indicates the results of bivariate relationships between independent variables and treatment costs of patients. The results of Table 6 show that there is a significant relationship between the residency origin, length of hospitalization, education of the head of household, the occupation of the head of household, having supplementary insurance, and the type of insurance fund, with the variable of the patient's treatment costs (being catastrophic or not). In other words, the treatment costs were higher for patients living in rural areas who had longer hospitalization, household head with lower education, household head with self-employed job, used UHIF, and lacked a supplementary insurance. This group of people is more exposed to the catastrophic expenditures.
Table 6.
Investigating the relationship between the research variables and the occurrence of catastrophic expenditures
| Variable | Occurrence or non-occurrence of catastrophic expenditures | |||
|---|---|---|---|---|
| Chi-square | P | phi coefficient | V Kramer coefficient | |
| Gender | 0.211 | 0.646 | 0.028- | - |
| Residency origin | 7.61 | 0.006 | 0.17 | - |
| Level of Education | 11.1 | 0.049 | - | 0.205 |
| hospitalization cause | 7.07 | 0.31 | - | 0.16 |
| Hospitalization ward | 9.13 | 0.24 | - | 0.19 |
| Transfer from another hospital | 1.33 | 0.25 | 0.071 | - |
| Undergoing surgical operation | 1.41 | 0.24 | 0.073 | - |
| length of hospitalization | 17.6 | 0.001 | - | 0.26 |
| The gender of the head of household | 1.72 | 0.19 | 0.081- | - |
| The education of head of household | 22.1 | 0.001 | - | 0.29 |
| Suffering with a disease by family members | 1.25 | 0.26 | 0.07 | - |
| Acute and chronic disease of family members | 1.85 | 0.17 | 0.16- | - |
| The job of household head | 59.31 | 0.00 | 0.47 | - |
| The ownership of residential house | 0.05 | 0.82 | - | 0.014 |
| private car | 0.99 | 0.32 | 0.06 | - |
| Supplementary insurance | 159.3 | 0.00 | 0.778 | - |
| Type of insurance fund | 115.01 | 0.00 | - | 0.66 |
Multivariate relations
Table 7 indicates the logistic regression results in examining the likelihood of the catastrophic expenditures of treatment for patients due to independent variables of the research. The results of this model indicate that among all independent research variables, three variables of length of hospitalization, having supplementary insurance and type of insurance fund have a significant effect on the likelihood of catastrophic expenditures of treatment. The value of odds ratio shows that having supplementary insurance reduces the likelihood of exposure to catastrophic expenditures by up to 80 times. The probability of being exposed to catastrophic expenditures for patients whose basic insurance is in other classes is about 70% lower than those covered by other funds. The length of hospitalization is one of the operational variables that the results of logistic regression model show, where increasing the length of hospitalization may increase the likelihood of catastrophic expenditures of treatment.
Table 7.
Logistic Regression Results in investigating the effects of independent variables on the status of patients’ treatment costs
| Variable name | Estimation coefficient | P | Odds ratio | Wald statistics | The standard error | ||
|---|---|---|---|---|---|---|---|
| Supplementary insurance | 4.321 | 0.000 | 75.270 | 80.029 | 0.483 | ||
| Type of insurance fund | -1.166 | 0.037 | 0.312 | 4.354 | 0.559 | ||
| length of hospitalization | 0.134 | 0.001 | 1.143 | 10.464 | 0.041 | ||
| Constant value of a | -1.941 | 0.000 | 0.144 | 32.521 | 0.340 | ||
| Chi-square test | statistics quantity | 202.9 | |||||
| Significance level. | 0.000 | ||||||
| Nigel Kirk’s quasi-coefficient | 71.9 | ||||||
The significance of the Chi-square test in investigating goodness of fit of the model indicates the effectiveness of the logistic regression model in examining the effect of independent variables on the dependent variable. The Nigel Kirk's quasicoefficient also shows that approximately 72% of the variations of the function variable in the regression model were explained based on the independent variables of the model.
Discussion
Approximately 55% of patients were exposed to catastrophic expenditures. This number was 42.6% in the study conducted by Anbari et al. in patients hospitalized in Markazi province.[14] The study conducted by Hatam et al. in a semi-private general hospital in Shiraz in 2013 indicated that the rate of exposure to catastrophic expenditures in hospitalized patients was 47.5%. Hatam et al. revealed that among the various insureds of the various basic insurances, the insured of the Iran health insurance organization experienced the highest catastrophic expenditures (48.4%).[15] Ghiasvand et al. in their study showed that in general hospitals in Tehran, 15.05% of patients were exposed to healthcare catastrophic expenditures.[16] Based on household income and expenditure data, Ghiasvand et al. has shown that Qom province with 4.9% accounts for the highest exposure to catastrophic expenditures in urban areas.[17] In the studies of Kavosiet al.,[18] Ghiasvand et al.[16] and Panahi 20 67.9%, 15.5% and 30% of patients were exposed to catastrophic expenditures, respectively. Furthermore, the overall proportion of exposure to the CHE in hospitals was 35.9% in iran.[19]
In the present study, regarding the relationship between patient income and the status of medical expenses, as expected, those patients with lower incomes were exposed to catastrophic expenditures. Hatam et al. showed that households living in the first income decile (the poorest households) had the most exposure to catastrophic expenditures.[15]
Among the 30 studied subjects entitled to discount by the hospital's Social working department, 70% of them received a discount of <5,000,000 rials (119 USD), and 30% received a discount of over 5,000,000 rials (119 USD). People who received the highest discount from the hospital, all were vulnerable in financial terms and exposed to the catastrophic expenditures.
There was a significant relationship between the residency origin, the length of hospitalization, the education of the household head, the job of the household head, having the supplementary insurance and the type of insurance fund with the variable of the catastrophic expenditures of treatment. Patients living in rural areas who had longer hospitalization, household head with lower education, household head with self-employed job, UHIF coverage, and lacked a supplementary insurance were more exposed to the catastrophic expenditures. In the study of Kavosi et al., there was significant relationship among the use of outpatient services, the type of treatment used, and the refusal of other family members to use health services.[18] In the study of Ghiasvand et al., the gender and education level of the household head, the number of hospitalization days, informal payments, and household income levels increased the likelihood of being exposed to catastrophic expenditures.[16] Panahi's research also showed that the existence of a member aged more than 60 in the household, female patient, and increase in the age of the patient have a positive relationship with the high levels of catastrophic expenditures. Furthermore, the presence of a member aged <12, a member with chronic disease, and admission to a private hospital are the main causes increasing the likelihood of being exposed to catastrophic expenditures, and that increase in the wealth index was one of the main factors reducing the likelihood of being exposed to catastrophic expenditures.[20]
In his study, Ekman stated that higher distance of the households to health care services, leads to the higher likelihood of increased catastrophic expenditures.[21] This is true for the villagers in the present study, since these people have to bear the transportation and accommodation costs in the city. Moreover, rural patients, if straightly present to the level two-family physician without a referral from level one family physician, then they should pay the entire billing fee out of pocket, which will be heavy for villagers who are often among the low-income class of the society. Furthermore, villagers are less likely to receive supplementary insurance compared to urban residents.[22] The Rural Insurance Fund aims to extend financial protection for uncovered families, increase fair financial participation, reduce out-of-pocket payment, and reduce the number of households being exposed to healthcare catastrophic expenditures below 1%;[23] however, in his study, Tofighi showed that 70.6% of those who were covered by rural insurance were exposed to catastrophic expenditures. He concluded that rural insurance does not adequately cover and failed to reduce the health catastrophic expenditures, and people covered by rural insurance have faced catastrophic expenditures due to problems such as lack of support at the second level.[24] Another point is that some studies have shown that the role of the basic insurance coverage is ineffective on the prevention of exposure to catastrophic expenditures.[13,15]
Regarding the other significant variables and comparison with other studies, Hatam et al. in their study showed that there was a significant relationship between the average length of hospitalization and the risk of exposure to catastrophic expenditures of health. The likelihood of exposure to healthcare catastrophic expenditures for patients whose household head is not covered by supplementary insurance is 3.2 times higher.[15] In his study, Ghiasvand et al. also indicated that the supplementary insurance coverage indicated a statistically significant relationship with the avoidance of heavy health care costs.[12]
The results of logistic regression showed that all independent variables of the study, three variables of hospitalization length, having supplementary insurance and type of insurance fund had a significant effect on the likelihood of catastrophic expenditures of treatment. Having supplementary insurance reduces the likelihood of being exposed to catastrophic expenditures by 80 times. The likelihood of being exposed to catastrophic expenditures in patients who are insured by other classes in relation to other insured people is approximately 70% lower. The length of hospitalization is one of the operational variables, where the results of the logistic regression model show that increasing the length of hospitalization may increase the likelihood of being exposed to catastrophic expenditures. Ghiasvand et al. also suggests that an increase in hospitalization length leads to a higher likelihood of catastrophic expenditures.[16]
The higher tariffs of the studied private hospital can be a significant factor in the rate of exposure to catastrophic expenditures. As Panahi et al. showed in their study, admission to private hospitals is one of the main factors in increasing the likelihood of exposure to catastrophic expenditures.[20] Private hospitals play a crucial role in providing services and as the National Accounts of 2008 showed private sector with a capacity of 27.2% of the capacity of public hospitals beds accounts for 42.3% of total hospitalization care costs. This means that if the government seeks to reduce its health costs, it is essential that its monitoring system, i.e., its supervisory role on private providers become more specific and transparent.[25]
The status of coverage by health insurance, as well as the coverage level of is one causes of the exposure to catastrophic expenditures. Low coverage of services and high levels of co-payment mean that households experience higher risk of catastrophic expenditures and economic hardship.[26] Other studies show the deficient function of insurance in Iran in which the cost coverage and service coverage are limited; and copayment is high. It has even reduced the protective effect of insurance.[27]
Conclusion
The emergence of health care catastrophic expenditures, especially at the hospital level, is of particular importance, as most studies focused on the catastrophic expenditures of health care services at the household level, and so far little research has been conducted at the hospital level. The importance of this is that most hospitalized patients are those who have somehow got to the service center to take advantage of the service, and factors such as poverty or the lack of geographical access has not prevented using health services, self-medication or presenting to traditional therapists. According to the above, the incidence of catastrophic expenditures due to the use of health services shows that even among citizens with relative ability to refere and use health services, there is a far more serious warning about the distribution of financial burden of health services compared to what is at the household level. This can be a relative deterioration of benefiting from health services in the country. The exposure of most of the insureds of the UHIF in this study will be a significant point for future policy making of this fund, as the results of this study showed the socioeconomic status of the insured people in this newly established fund, as well as the rural insurance fund which are worse than other funds and benefiting and exposure to healthcare catastrophic expenditures was higher, and this requires a specific policy to reduce the exposure of these people to catastrophic expenditures to ensure the government that there is no household which ignores its health issues due to poverty and that no family suffers health poverty due to the use of health services. Adoption of specific targeted policies for these vulnerable people in respect with reducing out-of-pocket payments through mechanism such as stepwise copayments as a step-by-step reduction in the price the consumer encounters, maximum out-of-pocket limit, fee exemptions or waiver and providing supplementary insurance to reduce the exposure to catastrophic expenditures was suggested for support them.
Financial support and sponsorship
This study was supported by Iran Health insurance organization
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank the participants of this study.
References
- 1.O’Donnell OA, Wagstaff A. Washington, D.C: World Bank Publications; 2008. Analyzing Health Equity using Household Survey Data: A Guide to Techniques and their Implementation. [Google Scholar]
- 2.Wagstaff A, Doorslaer EV. Catastrophe and impoverishment in paying for health care: With applications to Vietnam 1993–1998. Health Econ. 2003;12(11):921–33. doi: 10.1002/hec.776. [DOI] [PubMed] [Google Scholar]
- 3.Evans DB, Edejer TT, Lauer J, Frenk J, Murray CJ. Measuring quality: From the system to the provider. Int J Qual Health Care. 2001;13(6):439–46. doi: 10.1093/intqhc/13.6.439. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. The World Health Report 2000: Health Systems: Improving Performance. Geneva: World Health Organization; 2000. [Google Scholar]
- 5.Knaul FM, Arreola-Ornelas H, Méndez-Carniado O, Bryson-Cahn C, Barofsky J, Maguire R, et al. Evidence is good for your health system: Policy reform to remedy catastrophic and impoverishing health spending in Mexico. Lancet. 2006;368(9549):1828–41. doi: 10.1016/S0140-6736(06)69565-2. [DOI] [PubMed] [Google Scholar]
- 6.Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ, et al. Household catastrophic health expenditure: A multicountry analysis. Lancet. 2003;362(9378):111–7. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 7.Kavosi Z, Rashidian A, Pourmalek F, Majdzadeh R, Pourreza A, Mohammad K, et al. Measuring household exposure to catastrophic health care expenditures: A longitudinal study in Zone 17 of Tehran. Hakim Res J. 2009;12(2):38–47. [Google Scholar]
- 8.Jowett M. Theoretical Insights into the Development of Health Insurance in Low-Income Countries. Working Papers 188chedp, Centre for Health Economics, University of York. 2004 [Google Scholar]
- 9.Kavosi Z, Rashidian A, Pourreza A, Majdzadeh R, Pourmalek F, Hosseinpour AR, et al. Inequality in household catastrophic health care expenditure in a low-income society of Iran. Health Policy Plan. 2012;27(7):613–23. doi: 10.1093/heapol/czs001. [DOI] [PubMed] [Google Scholar]
- 10.Health Sector Revolution plan. Tehran: Ministry of Health and Medical Education; 2014. [Google Scholar]
- 11.Yazdi-Feyzabadi V, Mehrolhassani MH, Darvishi A. Measuring catastrophic health expenditures and its inequality: Evidence from Iran's health transformation program. Health Policy Plan. 2019;34(4):316–25. doi: 10.1093/heapol/czz031. [DOI] [PubMed] [Google Scholar]
- 12.Ghiasvand H, Hadian M, Maleki M. Relationship between health insurance and catastrophic medical payment in hospitals affiliated to Iran university of medical science 2009. J Econ Res. 2011;46(94):207–24. [Google Scholar]
- 13.Ghiasvand H, Hadian M, Maleki M, Shabaninejad H. Determinants of catastrophic medical payments in hospitals affiliated to Iran university of medical sciences 2009. Hakim Res J. 2010;13(3):145–54. [Google Scholar]
- 14.Anbari Z, Mohammadbeigi A, Mohammadsalehi N, Ebrazeh A. Health expenditure and catastrophic costs for inpatient- and out-patient care in Iran. Int J Prev Med. 2014;5(8):1023–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Hatam N, Orejlu PH, Jafari A, Kavosi Z. Catastrophic healthcare expenditures of hospitalized patients in the hospitals of Shiraz in 2013. Shiraz E Med. 2015;16(5):3–7. [Google Scholar]
- 16.Ghiasvand H, Sha’baninejad H, Arab M, Rashidian A. Hospitalization and catastrophic medical payment: Evidence from hospitals located in Tehran. Arch Iran Med. 2014;17(7):507–13. [PubMed] [Google Scholar]
- 17.Ghiasvand H, Gorji HA, Maleki M, Hadian M. Catastrophic health expenditure among Iranian rural and urban households, 2013-2014. Iran Red Crescent Med J. 2015;17(9):e30974. doi: 10.5812/ircmj.30974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kavosi Z, Delavari H, Keshtkaran A, Setoudehzadeh F. Catastrophic health expenditures and coping strategies in households with cancer patients in Shiraz Namazi hospital. Middle East J Cancer. 2014;5(1):13–22. [Google Scholar]
- 19.Aryankhesal A, Etemadi M, Mohseni M, Azami-Aghdash S, Nakhaei M. Catastrophic health expenditure in Iran: A review article. Iran J Public Health. 2018;47(2):166–77. [PMC free article] [PubMed] [Google Scholar]
- 20.Panahi H, Janati A, Narimani M, Assadzadeh A, Mohammadzadeh P, Naderi A. Catastrophic expenditures for hospitalized patients in Tabriz, Iran. Payesh. 2014;13(6):655–63. [Google Scholar]
- 21.Ekman B. Catastrophic health payments and health insurance: Some counterintuitive evidence from one low-income country. Health Policy. 2007;83(2):304–13. e27868. doi: 10.1016/j.healthpol.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Lankarani KB, Ghahramani S, Zakeri M, Joulaei H. Lessons learned from national health accounts in Iran: Highlighted evidence for policymakers. Shiraz E Med J. 2015;16(4):1–3. [Google Scholar]
- 23.Ibrahimipour H, Maleki MR, Brown R, Gohari M, Karimi I, Dehnavieh R. A qualitative study of the difficulties in reaching sustainable Universal Health Insurance Coverage in Iran. Health Policy Plan. 2011;26(6):485–95. doi: 10.1093/heapol/czq084. [DOI] [PubMed] [Google Scholar]
- 24.Tofighi S, Asefzadeh S, Mamikhani J, Sadeghifar J. The impact of rural health insurance on reduction of catastrophic health expenditure (CHE) J Appl Environ Biol Sci. 2014;4(5):154–60. [Google Scholar]
- 25.Universal Health Coverage in Iran. Tehran: Islamic Republic of Iran's National Institute of Health Research; 2014. [Google Scholar]
- 26.Wagstaff A, Lindelow M. Can insurance increase financial risk? The curious case of health insurance in China. J Health Econ. 2008;27(4):990–1005. doi: 10.1016/j.jhealeco.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 27.Ghorbanian A, Rashidian A, Lankarani KB, Kavosi Z. The prevalence and determinants of catastrophic health expenditures in Iran: A systematic review and meta-analysis. Health Scope. 2017;8(1):e63210. [Google Scholar]


