Abstract
Background:
Bone–patellar tendon–bone (BPB) autografts and hamstring tendon (HT) autografts are 2 popular choices for anterior cruciate ligament reconstruction (ACLR). Although existing meta-analyses have explored the clinical outcomes between BPB and HT autografts, none have based their analysis on studies with just femoral suspensory fixation methods.
Purpose:
To evaluate and compare clinical outcomes, particularly graft failure and knee stability, of ACLR with BPB or HT autografts with suspensory femoral fixation.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A literature search was conducted of studies reporting single-bundle ACLR with BPB autografts and HT autografts with suspensory fixation with a minimum 24-month follow-up. Graft failure rate, knee stability, and clinical outcomes were compared for BPB versus HT autografts. Knee stability was measured with the Lachman test, pivot-shift test, and KT-1000/2000 arthrometer side-to-side difference (SSD). Clinical outcomes were measured with Lysholm scores and the Tegner activity scale, as well as rate of return to preinjury sports. Donor site morbidity among included studies was reviewed. A random-effects model was used for calculations of summary estimates. Subgroup, sensitivity, and trial sequential analyses were conducted.
Results:
Five studies were included. Graft failure was seen more often in the HT group than the BPB group, and this was statistically significant (P = .03). However, the trial sequential analysis outcome indicated that the included sample size was not large enough to support a solid positive finding. The analysis showed no significant difference in SSD, Lachman test, pivot-shift test, rate of return to sports, Lysholm score, or Tegner score between groups. Subgroup analyses found no significant difference between groups.
Conclusion:
This meta-analysis demonstrated no significant differences in knee stability and knee functional outcomes between BPB and HT autografts with suspensory fixation. More evidence is needed to prove the lower risk of failure with use of BTB autograft with suspensory fixation.
Keywords: anterior cruciate ligament, bone–patellar tendon–bone, hamstring, autograft, fixation, suspensory
Bone–patellar tendon–bone (BPB) autografts and 4-strand hamstring tendon (HT) autografts are two popular graft choices for anterior cruciate ligament reconstruction (ACLR).20,41 Because there is controversy on the specific advantages and disadvantages of these 2 grafts, a number of meta-analyses have compared these 2 choices over the past years.3,4,21,29,30,32,44 Li et al21 and Xie et al44 reported that there was no statistical difference of postoperative graft failure between BPB grafts and HT grafts. However, Samuelsen et al32 reported that HT autografts failed at a higher rate than BPB autografts. Of note however, these meta-analyses included studies with both suspensory fixations (eg, EndoButton) and aperture fixations (eg, interference screw), which introduced a significant confounding factor to the results of the comparisons.
Although the interference screw is the most common type of femoral fixation for ACLR with BPB,12,42 screws present several disadvantages, which include the risk of blowout of the bone tunnel as well as damage to the bone blocks and tendons.24 Conversely, suspensory femoral fixations such as EndoButton (Smith & Nephew) or Tightrope (Arthrex) show the advantages of precise position of the tunnel and high tensile strength.11,13,37–39 However, there are 2 concerns regarding BPB grafts with suspensory fixation.7,15,24 First, the graft-bone motion of BPB grafts with suspensory fixation is higher than that of BPB grafts with interference screw fixation, which might influence BPB bone graft healing with the host bone tunnel.7,15 Moreover, it has been observed that BPB grafts with suspensory button fixations fail as a result of the sutures cutting through the bone during biomechanical testing.24 Hence, whether suspensory fixation is a beneficial complement to BPB autografts is still in dispute.
The purpose of this study was to systematically review and compare the clinical outcomes of BPB and HT autografts with femoral suspensory fixation in ACLR and to evaluate the feasibility of concomitant utilization of suspensory fixation and BTB autografts.
Methods
Search Strategy
In June 2018, 2 independent reviewers (W.C. and H.L.) performed a literature search in the PubMed, Embase, and Cochrane Library databases in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines and reviewed the search results, with a senior author (Y.W.) arbitrating on any disagreement.22 The detailed search strategy was as follows: (anterior cruciate ligament OR ACL) AND (bone–patellar tendon–bone OR BPB OR bone tendon bone OR BTB OR patellar tendon OR PT) AND (hamstring OR semitendinosus OR gracilis).
The titles and abstracts were reviewed for all search results, and potentially eligible studies received a full-text review. Finally, the reference lists of the included studies and literature reviews found in the initial search were manually screened for additional articles meeting the inclusion criteria. When a series of published articles reported on the same population, they were regarded as a single study.
Inclusion Criteria
The inclusion criteria for clinical articles were as follows: (1) clinical studies reporting graft failure or graft retear after anatomic ACLR with BPB autografts and HT autografts, including prospective cohort studies, retrospective cohort studies, and randomized controlled trials; (2) mean follow-up time longer than 24 months; (3) single-bundle reconstruction; (4) suspensory femoral fixation; and (5) full-text availability.
Exclusion Criteria
The exclusion criteria were (1) case series; (2) failure to report postoperative clinical or functional outcomes; (3) use of other grafts (eg, allografts); and (4) nonclinical studies, including reviews, cadaveric studies, biomechanical studies, surgical technique articles, and case reports.
Evaluation of the Study Quality
The Jadad Scale was used to evaluate the methodological quality of the randomized studies,19 and the Newcastle-Ottawa Scale was used to evaluate the methodological quality of nonrandomized studies.17 The Jadad Scale is a 5-point scale, with ≥3 points indicating a relatively high-quality study, and the Newcastle-Ottawa Scale is a 9-point scale, with ≥7 points rating a study as relatively high quality.44 Each study was independently assessed by 2 authors (W.C., H.L.), and disagreements were resolved by discussion.
Data Extraction
Two blinded reviewers (Y.C., F.J.) conducted data extraction and analysis using a predetermined data sheet. The relevant information included the following: study design, population size, population age, graft failure, postoperative functional outcome measures, return-to-sports rate, and follow-up time points. The functional outcomes focused on Tegner score, Lysholm score, Lachman test, pivot-shift test, and KT-1000/2000 arthrometer results. Given the heterogeneity of description among studies, we reviewed the incidence of donor site morbidity discretely—specifically, anterior knee pain and kneeling pain—instead of pooling the inconsistent results together. The detailed information of graft failure was also summarized. Failure rate was selected as the primary outcome. As 2 of the articles reported on the same population,13,43 when the outcome was not available in the article published in 2016,43 data were borrowed from the 200313 article.
Statistical Analysis
All statistical analyses were performed with Review Manager 5.3 software (The Cochrane Collaboration). A random-effects model was applied in consideration of the varied follow-up time and study designs across trials.34,35 Means were calculated for age and follow-up time. When the range was given instead of a standard deviation, the standard deviation was calculated with a method by Hozo et al.16 For data unable to be merged owing to inconsistent or absent data, a descriptive analysis was performed. A P value of <.05 was considered statistically significant.
Sensitivity and trial sequential analyses (TSAs) were conducted as described in our previous study.36 The heterogeneity was quantified with the I 2 statistic.14 When I 2 > 75%, which indicated high heterogeneity across studies, sensitivity analysis was used to reveal the potential source of heterogeneity. TSA was performed for the primary outcome to avoid an early false-positive conclusion drawn by traditional meta-analysis techniques. Based on the study design (randomized controlled trial [RCT] or non-RCT), subgroup analysis was conducted.
Results
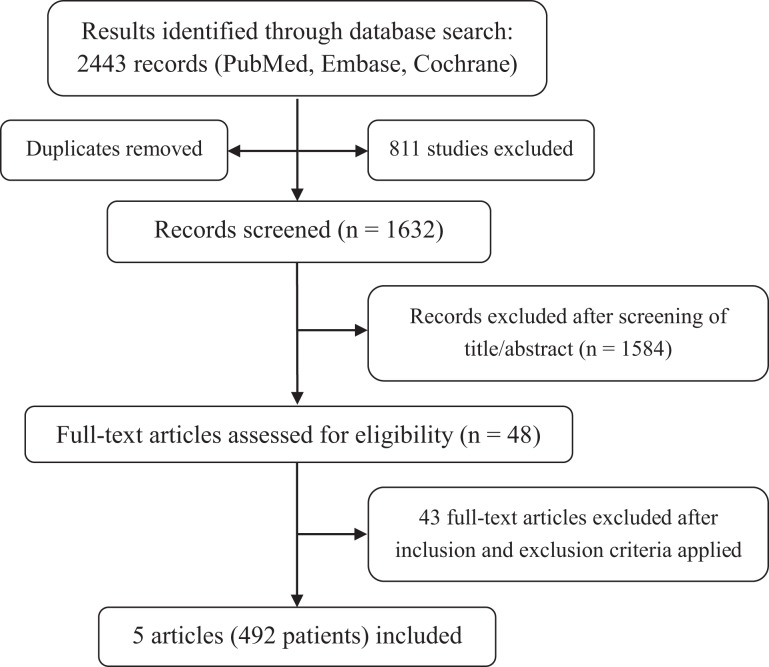
The initial literature search resulted in 2443 articles. After removal of duplicates, the articles were screened according to inclusion and exclusion criteria, and 48 unique articles were evaluated and full texts assessed for eligibility. Ultimately, 6 articles2,13,18,25,40,43 were included in this review, but as 2 of the articles13,43 reported on the same cohort, they were considered a single study for the purposes of this review (Figure 1). The characteristics of the studies are summarized in Table 1. There were 492 patients in total, however 11 patients were lost to follow-up, leaving 481 patients for analysis. Of these 481 patients, 233 had BPB autografts (BPB group) and 248 had HT autografts (HT group).
Figure 1.
Flowchart of the literature search process.
TABLE 1.
Study Characteristicsa
| Study: Design | Patients, n | Mean Age, y | Male:Female, n | Follow-up, mo | Jadad or NOS Score |
|---|---|---|---|---|---|
| Barrett et al (2002)2: CS | 7 | ||||
| BPB | 37 | 25.2 | 0:37 | 52 | |
| HT | 39 | 23.2 | 0:39 | 40.9 | |
| Ibrahim et al (2005)18: PCS | 22.3 | 81 | 9 | ||
| BPB | 40 | 40:0 | |||
| HT | 45 | 45:0 | |||
| Taylor et al (2009)40: RCT | 36 | 3 | |||
| BPB | 32 | 21.7 | 25:7 | ||
| HT | 32b | 22.1 | 28:4 | ||
| Mohtadi et al (2016)25: RCT | 5 | ||||
| BPB | 110 | 28.7 | 63:47 | 24 | |
| HT | 110 | 28.5 | 59:51 | 24 | |
| Webster et al (2016)43,c: RCT | 5 | ||||
| BPB | 22 | 26.6 | 16:6 | 184 | |
| HT | 25 | 26.1 | 20:5 | 182 | |
| Feller and Webster (2003)13,c: RCT | 5 | ||||
| BPB | 31 | 25.8 | 23:8 | 36 | |
| HT | 34 | 26.3 | 24:10 | 36 |
aBPB, bone–patellar tendon–bone; CS, case series; HT, hamstring tendon; NOS, Newcastle-Ottawa Scale; PCS, prospective cohort study; RCT, randomized controlled trial.
bThere were 8 patients in the BPB group and 3 in the HT group lost to follow-up.
cThese studies reported on the same cohort and were considered 1 study.
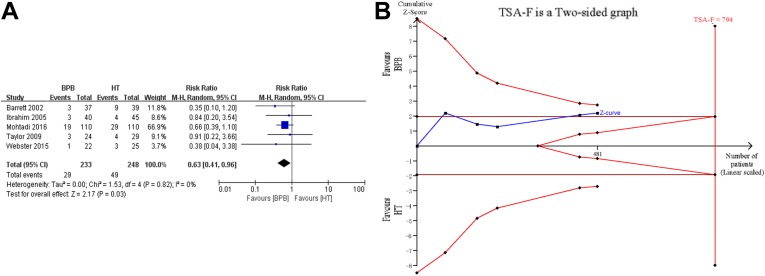
Graft Failure
Graft failure was reported in all 5 studies. Overall, 29 of 233 patients in the BPB group and 49 of 248 patients in the HT group experienced graft failure. The analysis showed that the BPB group (12.4%) was less likely to experience graft failure than the HT group (19.8%) (risk ratio, 0.63; 95% CI, 0.41-0.96; P = .03) (Figure 2A). However, the TSA indicated that there was not enough evidence proving a lower failure rate when BPB was used compared with HT (Figure 2B). The detailed information regarding graft failure is summarized in Table 2.
Figure 2.
(A) Traditional analysis of graft failure rate. Risk ratio for graft failure was in favor of BPB (95% CI, 0.41-0.96; P = .03). (B) Trial sequential analysis of graft failure rate. The Z curve crossed the conventional boundary (horizontal brown lines), suggesting the superiority of BPB, but failed to cross the 2-sided significance testing boundaries, futility boundaries, and trial sequential monitoring boundaries (red curves). The sample size of included studies also did not reach the required number (vertical red line). BPB, bone–patellar tendon–bone; HT, hamstring tendon; M-H, Mantel-Haenszel; TSA-F, trial sequential analysis–.
TABLE 2.
Graft Failure Informationa
| Study: Group | Information |
|---|---|
| Barrett (2002)2 | |
| BPB | Clinical failure occurred in 3 patients: 2 had a 1+ pivot shift and 1+ Lachman, and 1 had a 2+ Lachman and 2+ pivot shift. |
| HT | Failure of the graft occurred in 9 cases at final follow-up, as determined by the presence of a 1+ pivot shift in 5 cases, a KT-1000 arthrometer difference >5 mm in 1 case, and a 2+ Lachman and 1+ or 2+ pivot shift in 4 cases. |
| Ibrahim (2005)18 | Occasional giving way was reported by 2 patients in the BPB group and 3 in the HT group. Two patients reported giving way during physical activity (1 BPB and 1 HT). |
| Taylor (2009)40 | There were 3 BPB and 4 HT graft ruptures: 75% of the HT ruptures occurred before or at 1 y, while all the BTB ruptures occurred after 1 y; 6 graft ruptures occurred because of a noncontact injury mechanism and 1 in a contact injury. |
| Mohtadi (2016)25 | |
| BPB | 3 patients with complete traumatic tear and 16 with atraumatic graft failure |
| HT | 12 patients with complete traumatic tear and 17 with atraumatic graft failure |
| Webster (2016)43 | |
| BPB | 1 rupture occurred at 6 mo owing to a significant trauma. |
| HT | Between 3 and 15 y, 3 patients experienced rerupture. |
aBPB, bone–patellar tendon–bone; HT, hamstring tendon.
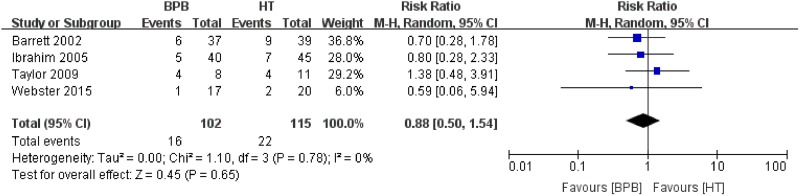
KT-1000/2000 Arthrometer Side-to-Side Difference
All 5 studies used instrumented laxity measurements as an outcome measure. Barrett et al2 reported that 6 BPB cases and 9 HT cases had a side-to-side difference (SSD) >3 mm. Ibrahim et al18 demonstrated that the KT-1000 arthrometer revealed 5 BPB cases and 7 HT cases that had an SSD >3 mm. Taylor et al40 evaluated SSD using the KT-2000 arthrometer (134 N) in only 8 patients with BPB and 11 with HT grafts and found that 4 each had an SSD >3 mm. Webster et al43 reported that 1 BPB case and 2 HT cases had an SSD ≥3 mm at 15-year follow-up. Mohtadi et al25 assessed anterior knee stability using a KT arthrometer and found that the SSD (mean ± SD) was 4.9 ± 2.3 mm for the BPB group and 5.0 ± 2.1 mm for the HT group. Four studies2,18,40,43 reporting patients with an SSD >3 mm were used for the meta-analysis. The analysis showed no significant difference between the groups, and the risk ratio for a KT-1000/2000 SSD >3 mm was 0.88 in favor of BPB (95% CI, 0.50-1.54; P = .65) (Figure 3).
Figure 3.
Analysis of instrumented laxity measurement of side-to-side difference >3 mm. BPB, bone–patellar tendon–bone; HT, hamstring tendon; M-H, Mantel-Haenszel.
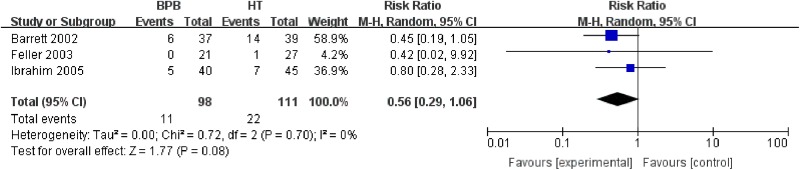
Lachman Test
Three studies2,13,18 including 209 patients reported data regarding the postoperative Lachman test. The analysis showed no significant difference between the groups, and the risk ratio for positive Lachman test result was 0.56 in favor of BPB (95% CI, 0.29-1.06; P = .08) (Figure 4).
Figure 4.
Comparison of positive Lachman test result between BPB and HT groups after anterior cruciate ligament reconstruction. BPB, bone–patellar tendon–bone; HT, hamstring tendon; M-H, Mantel-Haenszel.
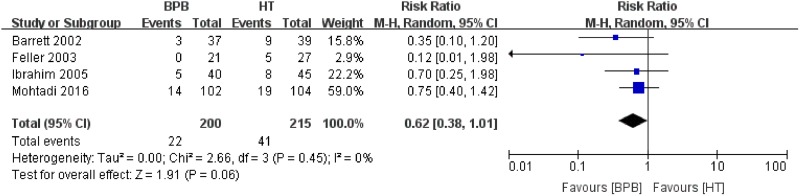
Pivot-Shift Test
The pivot-shift test was performed in 4 studies2,13,18,25 including 415 patients. The analysis showed no significant difference between the groups, and the risk ratio for positive pivot-shift test was 0.62 in favor of BPB (95% CI, 0.38-1.01; P = .06) (Figure 5).
Figure 5.
Comparison of positive pivot-shift test result between BPB and HT groups after anterior cruciate ligament reconstruction. BPB, bone–patellar tendon–bone; HT, hamstring tendon; M-H, Mantel-Haenszel.
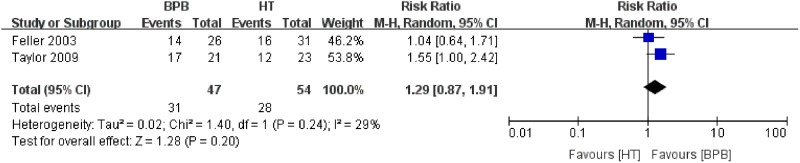
Return to Sports
Two studies reported the outcome of return to sports after surgery. Taylor et al40 reported that 81% of the patients with BPB and 52% with HT grafts were able to return to their preinjury activity levels. In 2016, Webster et al43 reported that 82% and 68% of patients with BPB and HT grafts returned to sports, respectively, but the level of activity was unknown. Nevertheless, in their report, which focused on the same cohort dating back to the 2003 study,13 the authors indicated that 53.8% of patients in the BPB group and 51.6% in the HT group returned to their preinjury level of sports participation 3 years after surgery. The analysis showed that the difference between groups in the rate of return to preinjury sports was nonsignificant (risk ratio, 1.29; 95% CI, 0.87-1.91; P = .20) (Figure 6).
Figure 6.
Analysis of return to preinjury sports rate. BPB, bone–patellar tendon–bone; HT, hamstring tendon; M-H, Mantel-Haenszel.
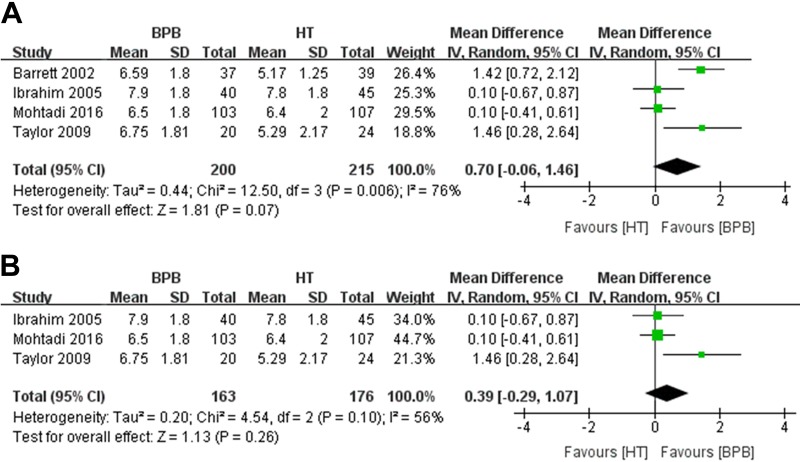
Tegner Score
Tegner scores were reported in 4 studies2,18,25,40 comprising 200 patients with BPB autografts and 215 with HT autografts. There was no significant difference between the groups (mean difference [MD], 0.70; 95% CI, –0.06 to 1.46; P = .07) (Figure 7A). The I 2 of 76% indicated significant heterogeneity among the studies. Hence, a sensitivity analysis was conducted, and we found that the study by Barrett et al2 contributed to most of the heterogeneity. Yet, excluding this study did not make much difference to the result (MD, 0.39; 95% CI, –0.29 to 1.07; P = .26) (Figure 7B).
Figure 7.
Analysis of Tegner scores (A) before and (B) after sensitivity analysis. BPB, bone–patellar tendon–bone; HT, hamstring tendon; IV, inverse variance.
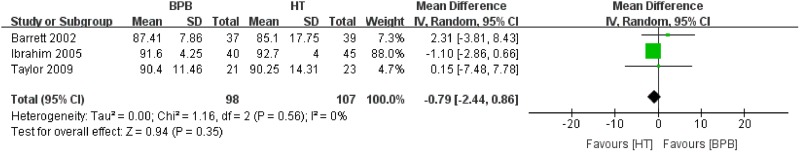
Lysholm Score
Lysholm scores were reported in 3 studies2,18,40 comprising 98 patients with BPB autografts and 107 with HT autografts. There was no significant difference between the groups (MD, –0.79; 95% CI, –2.44 to 0.86; P = .35) (Figure 8).
Figure 8.
Analysis of Lysholm scores. BPB, bone–patellar tendon–bone; HT, hamstring tendon; IV, inverse variance.
Subgroup Analysis
The subgroup analyses to eliminate the influence of study design found no significant difference with regard to graft failure, SSD, Lachman test, pivot-shift test, Tegner score, or Lysholm score between groups (Table 3). All studies presenting the rate of return to sports were RCTs; thus, the subgroup analysis was unnecessary.
TABLE 3.
Subgroup Analysis Outcomea
| Outcome: Study Design | Studies, n | Patients (BTB:HT), n | I 2, % | Risk Ratio (95% CI) | P Value |
|---|---|---|---|---|---|
| Graft failure | |||||
| RCT | 3 | 156:164 | 0 | 0.66 (0.41 to 1.06) | .09 |
| Non-RCT | 2 | 77:84 | 0 | 0.51 (0.20 to 1.29) | .16 |
| Side-to-side difference | |||||
| RCT | 2 | 25:31 | 0 | 1.19 (0.46 to 3.08) | .72 |
| Non-RCT | 2 | 77:84 | 0 | 0.74 (0.37 to 1.50) | .41 |
| Lachman test | |||||
| RCT | 1 | 21:27 | NA | 0.42 (0.02 to 9.92) | .59 |
| Non-RCT | 2 | 77:84 | 0 | 0.56 (0.29 to 1.09) | .09 |
| Pivot-shift test | |||||
| RCT | 2 | 123:131 | 41 | 0.49 (0.10 to 2.40) | .38 |
| Non-RCT | 2 | 77:84 | 0 | 0.53 (0.24 to 1.16) | .11 |
| Tegner score | |||||
| RCT | 2 | 123:131 | 77 | 0.67 (–0.64 to 1.99) | .32 |
| Non-RCT | 2 | 77:84 | 84 | 0.77 (–0.52 to 2.06) | .24 |
| Lysholm score | |||||
| RCT | 1 | 21:23 | NA | 0.15 (–7.48 to 7.78) | .97 |
| Non-RCT | 2 | 77:84 | 9 | –0.71 (–2.84 to 1.43) | .52 |
aBPB, bone–patellar tendon–bone; HT, hamstring tendon; NA, not applicable; RCT, randomized controlled trial.
Donor Site Morbidity
Donor site morbidity was described differently among studies. Feller and Webster13 reported that there were significantly fewer patients with anterior knee pain in the HT group at 8 months and 2 years postoperatively. In addition, the incidence of kneeling pain was significantly greater in the BTB group at all follow-up times. Webster et al43 presented results in a 15-year follow-up of the same population, at which point the incidences of anterior knee pain and kneeling pain were similar between groups. According to Ibrahim et al,18 patients with anterior knee pain were significantly more represented in the BTB group (10 of 40) versus the HT group (3 of 40) at a mean follow-up of 81 months. Taylor et al40 reported no significant difference between groups in terms of pain associated with kneeling at 5 years postoperatively.
Discussion
The purpose of this study was to evaluate clinical outcomes, particularly graft failure and knee stability, of ACLR with BPB or HT autografts with suspensory femoral fixations only. We found that the BPB group (12.4%) had a lower graft failure rate than the HT group (19.8%) (risk ratio, 0.63; P < .03). But this finding was opposed by the TSA, which indicated that a larger sample size must be acquired by conducting more well-designed clinical trials before the cessation of this debate. Furthermore, there were no significant differences in knee stability or knee function outcomes between BPB and HT autografts with suspensory fixation.
It is universally acknowledged that graft failure is the first thing to avoid after ACLR.23 The time required for bone-to-bone incorporation of the BPB graft is shorter than that for bone-tendon incorporation of HT, which may contribute to the difference of failure rate between these choices.10 Recently published meta-analyses comparing ACLR with BPB autografts and HT autografts, regardless of fixation methods, resulted in 2 divergent conclusions concerning failure rate. Most found no significant difference between these types of graft,9,10,44,45 while 2 studies with much larger sample sizes, including 47,613 patients32 and 15,557 patients,27 revealed a significantly lower secondary rupture rate after the BPB procedure. Although the difference was statistically significant in the study that included 47,613 patients, rerupture rates were low: 2.80% in the BPB and 2.84% in the HT group.32 Whether such a narrow difference is of any clinical importance should be deliberated.
SSD measured by KT-1000/2000 arthrometer, Lachman test, and pivot-shift test are indicators to determine knee stability after ACLR. A number of meta-analyses published in recent years have reported better stability in knees reconstructed with BPB autografts. Xie et al44 in 2015, Mohtadi et al26 in 2011, and Li et al21 in 2011 found significantly higher risk ratios for positive pivot-shift test result in the HT autograft group. Li et al and Mohtadi et al also observed significantly decreased SSD (as measured by KT-1000) in the BPB group. A significantly higher risk ratio of positive Lachman test result was reported by Mohtadi et al in 2011. The conclusions are quite plausible, as all 3 of these studies were highly appraised according to the Quality of Reporting of Meta-analyses (QUOROM) score system, which was designed to evaluate the quality of meta-analyses.33 In the current review, all of these joint stability outcomes were comparable between the BPB and HT groups. This divergence may be explained by a meta-analysis conducted in 2017 that compared suspensory and aperture fixation in HT autografts.8 The analysis showed a significantly higher incidence of SSD >3 mm in the patients with aperture fixation, which confirms our findings of similar joint stability outcomes between BPB and HT grafts when aperture fixation was not included.
The primary purpose of ACLR is to help patients return to their preinjury activity levels.1 Most previous meta-analyses reported no difference between BPB and HT grafts in terms of activity level and knee function, including rate of return to preinjury sports, Tegner score, and Lysholm score, which tallied with our outcomes.26,32 Given the donor site morbidity with the use of BTB autograft, including anterior knee pain and patellofemoral problems, as reported in most of our included studies with a follow-up period <5 years,13,18 HT autograft may be the preferred option.
Nevertheless, the reliability of bone-to-bone healing once made BPB autograft the “gold standard” graft choice of ACLR.28 Unlike reconstructing with HT autograft, the suspensory fixation method was utilized less often than interference screws, merely in about 10% of cases as reported,42 when fixing BPB autograft. However, drilling the screws increases the risk of bone block damage, and the block sometimes slips in the tunnel when the fixation is not rigid enough.24 Moreover, with the popularization of anatomic ACLR, the femoral tunnel is placed lower on the lateral wall of the intercondylar notch, which can lead to issues with graft passage and the likelihood of graft-tunnel mismatch.6 Employing suspensory fixation can solve these problems,24 especially when it is difficult to preserve sufficient bone stock in the bone tunnel or when it is at risk of posterior wall blowout. Moreover, suspensory fixation can be a solution when an interference screw is inapplicable in revision cases with tunnel enlargement.11 Taketomi et al37 confirmed that that EndoButton is a reliable method for BTB by evaluating patients with 3-dimensional computed tomography 1 year after surgery. In a biomechanical study, Mickelson et al24 found that adjustable-loop cortical buttons had similar failure loads as compared with interference screws. The results of our review also indicated that the clinical outcome of BPB autografts with suspensory fixation is comparable with that of HT autografts.
A well-designed RCT with long-term follow-up is one of the best ways to evaluate a surgical technique.26 The rerupture rates of BTB autografts with traditional interference fixation in 2 recently published RCTs comparing BTB and HT autografts were 6.6% (4 of 61 patients) at 16-year follow-up5 and 9.4% (3 of 32 patients) at 17-year follow-up.31 In addition, in one of our included RCTs, Webster et al43 reported a rerupture rate of 4.5% for BTB autograft by suspensory fixation at 15-year follow-up. However, their sample size was small, suggesting that more studies comparing BTB via different fixation methods should be conducted in the future.
This meta-analysis comparing BPB and HT autografts, both with suspensory fixation, eliminated the bias caused by multiple fixation methods in previous studies. The low heterogeneity across most outcomes, as well as the consistent conclusions drawn by the subgroup analyses and the regular analyses in most cases, strengthens the credibility of the results. In addition, the selected outcomes are all clinically relevant and may offer practical advice for surgeons when choosing an optimal graft. Moreover, TSA was applied to ensure that a reliable positive conclusion was drawn with a sufficient sample size and power of a test.
Limitations
There are several limitations in this study that need to be specified. First, not all the studies included were well-designed RCTs with the highest evidence level, which may introduce biases to the results. Second, the KT-1000/2000 arthrometer measurements were performed with varying forces, which made comparison of SSD less accurate. Finally, follow-up time varied greatly, from 2 to 15 years among the studies, which may undermine the credibility of the outcomes.
Conclusion
This meta-analysis demonstrated that there were no significant differences in knee stability and knee functional outcomes between BPB and HT autografts using suspensory fixation methods. More evidence is in need to confirm there is a lower risk of failure with the use of BTB autograft with suspensory fixation.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was supported by the Initial Foundation for Scientific Research of Huashan Hospital (2017QD080). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. [DOI] [PubMed] [Google Scholar]
- 2. Barrett GR, Noojin FK, Hartzog CW, Nash CR. Reconstruction of the anterior cruciate ligament in females: a comparison of hamstring versus patellar tendon autograft. Arthroscopy. 2002;18(1):46–54. [DOI] [PubMed] [Google Scholar]
- 3. Biau DJ, Katsahian S, Kartus J, et al. Patellar tendon versus hamstring tendon autografts for reconstructing the anterior cruciate ligament: a meta-analysis based on individual patient data. Am J Sports Med. 2009;37(12):2470–2478. [DOI] [PubMed] [Google Scholar]
- 4. Biau DJ, Tournoux C, Katsahian S, Schranz PJ, Nizard RS. Bone–patellar tendon–bone autografts versus hamstring autografts for reconstruction of anterior cruciate ligament: meta-analysis. BMJ. 2006;332(7548):995–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bjornsson H, Samuelsson K, Sundemo D, et al. A randomized controlled trial with mean 16-year follow-up comparing hamstring and patellar tendon autografts in anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(9):2304–2313. [DOI] [PubMed] [Google Scholar]
- 6. Boddu CK, Arif SK, Hussain MM, et al. Prevention of graft-tunnel mismatch during anatomical anterior cruciate ligament reconstruction using a bone–patellar tendon–bone graft. Bone Joint J. 2015;97(3):324–328. [DOI] [PubMed] [Google Scholar]
- 7. Brown CJ, Wilson DR, Hecker AT, Ferragamo M. Graft-bone motion and tensile properties of hamstring and patellar tendon anterior cruciate ligament femoral graft fixation under cyclic loading. Arthroscopy. 2004;20(9):922–935. [DOI] [PubMed] [Google Scholar]
- 8. Browning WR, Kluczynski MA, Curatolo C, Marzo JM. Suspensory versus aperture fixation of a quadrupled hamstring tendon autograft in anterior cruciate ligament reconstruction: a meta-analysis. Am J Sports Med. 2017;45(10):2418–2427. [DOI] [PubMed] [Google Scholar]
- 9. Chee MY, Chen Y, Pearce CJ, et al. Outcome of patellar tendon versus 4-strand hamstring tendon autografts for anterior cruciate ligament reconstruction: a systematic review and meta-analysis of prospective randomized trials. Arthroscopy. 2017;33(2):450–463. [DOI] [PubMed] [Google Scholar]
- 10. Ciccotti MC, Secrist E, Tjoumakaris F, Ciccotti MG, Freedman KB. Anatomic anterior cruciate ligament reconstruction via independent tunnel drilling: a systematic review of randomized controlled trials comparing patellar tendon and hamstring autografts. Arthroscopy. 2017;33(5):1062–1071. [DOI] [PubMed] [Google Scholar]
- 11. Colombet P, Bouguennec N. Suspensory fixation device for use with bone–patellar tendon–bone grafts. Arthrosc Tech. 2017;6(3):e833–e838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Eysturoy NH, Nissen KA, Nielsen T, Lind M. The influence of graft fixation methods on revision rates after primary anterior cruciate ligament reconstruction. Am J Sports Med. 2018;46(3):524–530. [DOI] [PubMed] [Google Scholar]
- 13. Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(4):564–573. [DOI] [PubMed] [Google Scholar]
- 14. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Honl M, Carrero V, Hille E, Schneider E, Morlock MM. Bone–patellar tendon–bone grafts for anterior cruciate ligament reconstruction: an in vitro comparison of mechanical behavior under failure tensile loading and cyclic submaximal tensile loading. Am J Sports Med. 2002;30(4):549–557. [DOI] [PubMed] [Google Scholar]
- 16. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. Bmc Med Res Methodol. 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hurley ET, Lim FD, Farrington SK, Mullett H. Open versus arthroscopic latarjet procedure for anterior shoulder instability: a systematic review and meta-analysis. Am J Sports Med. 2019;47(5):1248–1253. [DOI] [PubMed] [Google Scholar]
- 18. Ibrahim SA, Al-Kussary IM, Al-Misfer AR, et al. Clinical evaluation of arthroscopically assisted anterior cruciate ligament reconstruction: patellar tendon versus gracilis and semitendinosus autograft. Arthroscopy. 2005;21(4):412–417. [DOI] [PubMed] [Google Scholar]
- 19. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. [DOI] [PubMed] [Google Scholar]
- 20. Leys T, Salmon L, Waller A, Linklater J, Pinczewski L. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012;40(3):595–605. [DOI] [PubMed] [Google Scholar]
- 21. Li S, Su W, Zhao J, et al. A meta-analysis of hamstring autografts versus bone–patellar tendon–bone autografts for reconstruction of the anterior cruciate ligament. Knee. 2011;18(5):287–293. [DOI] [PubMed] [Google Scholar]
- 22. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:B2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Maletis GB, Chen J, Inacio MC, Funahashi TT. Age-related risk factors for revision anterior cruciate ligament reconstruction: a cohort study of 21,304 patients from the Kaiser Permanente anterior cruciate ligament registry. Am J Sports Med. 2016;44(2):331–336. [DOI] [PubMed] [Google Scholar]
- 24. Mickelson DT, Lefebvre T, Gall K, Riboh JC. Adjustable-loop femoral cortical suspensory fixation for patellar tendon anterior cruciate ligament reconstruction: a time zero biomechanical comparison with interference screw fixation. Am J Sports Med. 2018;46(8):1857–1862. [DOI] [PubMed] [Google Scholar]
- 25. Mohtadi N, Chan D, Barber R, Paolucci EO. Reruptures, reinjuries, and revisions at a minimum 2-year follow-up: a randomized clinical trial comparing 3 graft types for ACL reconstruction. Clin J Sport Med. 2016;26(2):96–107. [DOI] [PubMed] [Google Scholar]
- 26. Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011;9:CD005960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nawasreh Z, Adams G, Pryzbylkowski O, Logerstedt D. Influence of patient demographics and graft types on ACL second injury rates in ipsilateral versus contralateral knees: a systematic review and meta-analysis. Int J Sports Phys Ther. 2018;13(4):561–574. [PMC free article] [PubMed] [Google Scholar]
- 28. Panni AS, Milano G, Lucania L, Fabbriciani C. Graft healing after anterior cruciate ligament reconstruction in rabbits. Clin Orthop Relat Res. 1997;343:203–212. [PubMed] [Google Scholar]
- 29. Poehling-Monaghan KL, Salem H, Ross KE, et al. Long-term outcomes in anterior cruciate ligament reconstruction: a systematic review of patellar tendon versus hamstring autografts. Orthop J Sports Med. 2017;5(6):2325967117709735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Poolman RW, Farrokhyar F, Bhandari M. Hamstring tendon autograft better than bone patellar-tendon bone autograft in ACL reconstruction: a cumulative meta-analysis and clinically relevant sensitivity analysis applied to a previously published analysis. Acta Orthop. 2007;78(3):350–354. [DOI] [PubMed] [Google Scholar]
- 31. Sajovic M, Stropnik D, Skaza K. Long-term comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: a 17-year follow-up of a randomized controlled trial. Am J Sports Med. 2018;46(8):1800–1808. [DOI] [PubMed] [Google Scholar]
- 32. Samuelsen BT, Webster KE, Johnson NR, Hewett TE, Krych AJ. Hamstring autograft versus patellar tendon autograft for ACL reconstruction: is there a difference in graft failure rate? A meta-analysis of 47,613 patients. Clin Orthop Relat Res. 2017;475(10):2459–2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schuette HB, Kraeutler MJ, Houck DA, McCarty EC. Bone–patellar tendon–bone versus hamstring tendon autografts for primary anterior cruciate ligament reconstruction: a systematic review of overlapping meta-analyses. Orthop J Sports Med. 2017;5(11):2325967117736484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sun Y, Chen J, Li H, Jiang J, Chen S. Steroid injection and nonsteroidal anti-inflammatory agents for shoulder pain: a PRISMA systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2015;94(50):e2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sun Y, Lu S, Zhang P, Wang Z, Chen J. Steroid injection versus physiotherapy for patients with adhesive capsulitis of the shoulder: a PRIMSA systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2016;95(20):e3469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sun Y, Zhang P, Liu S, et al. Intra-articular steroid injection for frozen shoulder: a systematic review and meta-analysis of randomized controlled trials with trial sequential analysis. Am J Sports Med. 2017;45(9):2171–2179. [DOI] [PubMed] [Google Scholar]
- 37. Taketomi S, Inui H, Nakamura K, et al. Secure fixation of femoral bone plug with a suspensory button in anatomical anterior cruciate ligament reconstruction with bone–patellar tendon–bone graft. Joints. 2015;3(3):102–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Taketomi S, Inui H, Yamagami R, et al. Bone–patellar tendon–bone autograft versus hamstring tendon autograft for anatomical anterior cruciate ligament reconstruction with three-dimensional validation of femoral and tibial tunnel positions. J Knee Surg. 2018;31(9):866–874. [DOI] [PubMed] [Google Scholar]
- 39. Tashiro Y, Okazaki K, Murakami K, et al. Anterolateral rotatory instability in vivo correlates tunnel position after anterior cruciate ligament reconstruction using bone–patellar tendon–bone graft. World J Orthop. 2017;8(12):913–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Taylor DC, DeBerardino TM, Nelson BJ, et al. Patellar tendon versus hamstring tendon autografts for anterior cruciate ligament reconstruction: a randomized controlled trial using similar femoral and tibial fixation methods. Am J Sports Med. 2009;37(10):1946–1957. [DOI] [PubMed] [Google Scholar]
- 41. Thompson SM, Salmon LJ, Waller A, et al. Twenty-year outcome of a longitudinal prospective evaluation of isolated endoscopic anterior cruciate ligament reconstruction with patellar tendon or hamstring autograft. Am J Sports Med. 2016;44(12):3083–3094. [DOI] [PubMed] [Google Scholar]
- 42. Tibor L, Chan PH, Funahashi TT, et al. Surgical technique trends in primary ACL reconstruction from 2007 to 2014. J Bone Joint Surg Am. 2016;98(13):1079–1089. [DOI] [PubMed] [Google Scholar]
- 43. Webster KE, Feller JA, Hartnett N, Leigh WB, Richmond AK. Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: a 15-year follow-up of a randomized controlled trial. Am J Sports Med. 2016;44(1):83–90. [DOI] [PubMed] [Google Scholar]
- 44. Xie X, Liu X, Chen Z, et al. A meta-analysis of bone–patellar tendon–bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015;22(2):100–110. [DOI] [PubMed] [Google Scholar]
- 45. Xie X, Xiao Z, Li Q, et al. Increased incidence of osteoarthritis of knee joint after ACL reconstruction with bone–patellar tendon–bone autografts than hamstring autografts: a meta-analysis of 1,443 patients at a minimum of 5 years. Eur J Orthop Surg Traumatol. 2015;25(1):149–159. [DOI] [PubMed] [Google Scholar]