Abstract
Background
Surgical drainage and antimicrobial therapy are the most accepted empirical treatments for spinal epidural abscess. However, surgery may not be indicated when patient’s general health condition is poor. Percutaneous drainage has been reported as a non-surgical treatment for children or patients with no or minor neurological deficits. Here we describe the successful treatment of an extensive spinal epidural abscess with fluoroscopy-guided percutaneous drainage in an elderly man with progressive muscle weakness who could not be operated because of a poor general health condition.
Case presentation
An 81-year-old man presented with fever, back pain, and progressive muscle weakness in bilateral legs. Magnetic resonance imaging (MRI) showed extensive fluid retention in the spinal epidural space (Th6 to L3). Paraplegia due to an epidural abscess was suspected. We considered an emergency operation; however, the patient’s general condition was poor. Therefore, fluoroscopy-guided percutaneous epidural drainage was performed. After drainage, his back pain and muscle weakness gradually resolved. After 3 weeks, MRI showed that the abscesses had completely disappeared.
Discussion
Compared with surgical drainage, fluoroscopy-guided percutaneous epidural drainage is a less invasive treatment option for patients with a poor general condition.
Keywords: Spinal epidural abscess, Percutaneous drainage, Fluoroscopy
Background
The mortality rate for epidural abscess is high [1]; therefore, early diagnosis and treatment are essential. Evidence shows that surgical drainage and antimicrobial treatment are preferred [2–5]. However, surgery is not considered when a patient’s general health condition is poor. Percutaneous puncture drainage has shown occasional success in previous reports, although the indications are unclear [6, 7]. Here we describe the successful treatment of an extensive spinal epidural abscess with percutaneous epidural puncture drainage in an elderly patient with progressive muscle weakness who could not be operated because of a poor general health condition.
Case presentation
Written informed consent was obtained from the patient and his family for publication of this case report and accompanying images.
An 81-year-old man (height, 175 cm; weight, 85 kg) visited the emergency department with bilateral leg weakness, which led to difficulty in knee flexion 3 days before. He also developed fever and experienced back pain for approximately 1 week. Earlier, he had been walking with the assistance of a walker. He reported a history of aortic valve replacement surgery, mitral valvuloplasty, and tricuspid valvuloplasty, in addition to a history of heart failure, atrial fibrillation, obstructive arteriosclerosis, diabetes, chronic obstructive pulmonary disease, spinal canal stenosis, and dementia. Therefore, his general health condition was deemed poor. He was taking aspirin, apixaban, furosemide, spironolactone, and insulin. Echocardiography showed poor wall motion with an ejection fraction of 41% and pulmonary hypertension (65/13 mmHg).
We were unable to obtain detailed information regarding neurological symptoms such as sensory disturbance and movement disorder because of the severe dementia. He could not flex his right knee, although he could briefly flex his left knee in the supine position. He also complained of severe back pain (face rating scale [FRS] = 4) at rest, which increased with body movement (FRS = 5). Except for an elevated temperature (38.0 °C), his vital signs were stable. Blood examination revealed a slight increase in C-reactive protein (3.64 mg/dl) and white blood cell count (10,300/μl).
Magnetic resonance imaging (MRI) showed extensive fluid retention in the spinal epidural space (Th6 to L3) and compression of the spinal cord (Th6/7, Th11/12, L2/3) (Fig. 1). The latter suggested paraplegia due to an epidural abscess. We performed emergency drainage using fluoroscopy-guided percutaneous puncture. The patient was placed in the prone position and received local anesthesia, following which any abscess near Th6/7, Th11/12, and L2/3 was punctured using a 14 G Tuohy needle under fluoroscopic guidance. Approximately 3 ml of purulent discharge was drained from the Th6/7 and L2/3 levels, and approximately 4 ml of a clear, light-yellow colored discharge was drained from the Th11/12 level. For involved areas near Th6/7, two needles were placed at the Th6/7 and Th8/9 levels, respectively. A 5-Fr catheter was placed under fluoroscopic guidance using a guide wire, followed by perfusion with saline until apparent removal of the corpuscles. MRI performed 1 day later showed relief from the compression due to the abscess. Three weeks later, the abscess had completely disappeared (Fig. 2).
Fig. 1.
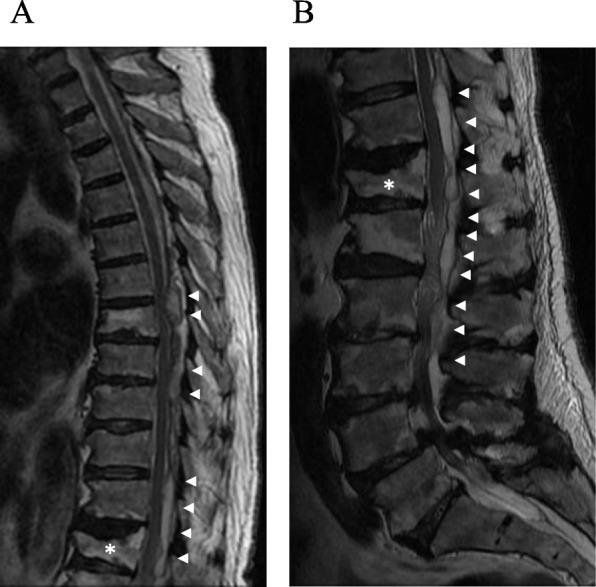
a, b Magnetic resonance imaging (T2) performed on admission. Fluid retention is observed in the epidural space behind the Th6-L3 spinal canal (arrow). Compression of the spinal cord near Th6/7, Th11/12, and L2/3 due to fluid retention is shown. Vertebral compression fractures can also be seen at Th12 (asterisk)
Fig. 2.
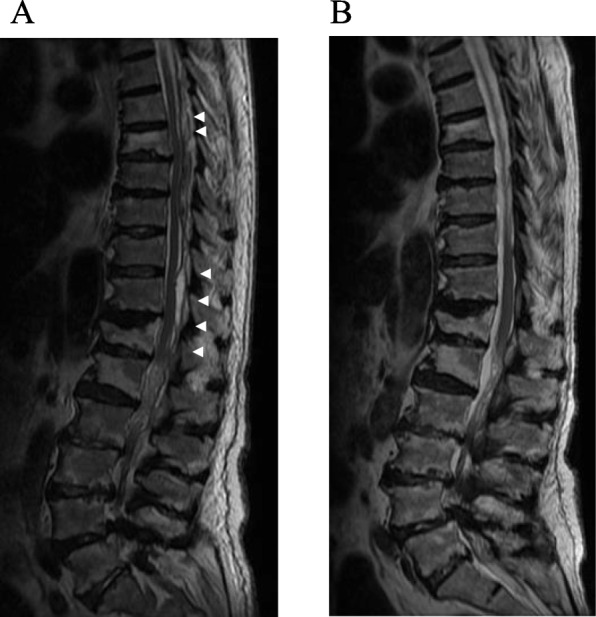
a Magnetic resonance imaging (MRI; T2) performed a day after fluoroscopy-guided percutaneous puncture. The volume of fluid in the epidural space has decreased and the spinal cord compression has been relieved (arrow). b MRI (T2) performed after 3 weeks. The epidural fluid pool has completely disappeared
At the time of admission, provisional treatment with meropenem, clindamycin, and vancomycin was initiated and continued for 3 days. The prescription was de-escalated to cefazolin and clindamycin after group G streptococcus was detected in the abscess, and the treatment was continued for 28 days. Blood cultures were negative. Pain on movement (FRS = 2) reduced after the drainage procedure, while pain at rest also improved (FRS = 1) after 3 days. The muscle weakness gradually resolved, and he could walk to a portable toilet without assistance 20 days after the procedure. He was discharged to a nursing home for the elderly on the 57th day.
Discussion
The mortality rate for spinal epidural abscess is high, reaching 16% [1]. Preoperative neurological findings are important predictors of the final neurological prognosis [2]. However, paralysis may progress rapidly, and immediate intervention is required after diagnosis [8–10]. Surgical drainage and antimicrobial therapy are the most accepted empirical treatments [2–5]. Although there are several criteria for surgical treatment [3, 11], contraindications are also reported [12, 13]. Non-surgical treatment is an alternative; however, antibiotic therapy alone is indicated only for select patients [14].
In the present case, surgical indications were determined through Baker’s criteria. The abscess was extensive and involved multiple levels, and extensive decompression was necessary. However, the patient would not be able to tolerate prolonged surgery in the prone position because of poor cardiac function. Furthermore, there were concerns about massive bleeding during and after surgery because he was taking aspirin and apixaban. The incidence of epidural hematoma after spinal surgery is 0.1 to 3% [15, 16], and extensive surgery and preoperative coagulopathy are risk factors [17]. Moreover, the risk of surgical site infection was high because of the severe diabetes. Because more than 3 days had passed since the onset of muscle weakness in his legs, we decided not to perform surgery.
To the best of our knowledge, there are no reports of percutaneous drainage in a patient with a poor general condition deemed unsuitable for surgery. Percutaneous drainage can be considered for children [18, 19], patients with no or minor neurological deficits, or patients with an abscess that is resistant to antibiotic therapy [20]. Our results have suggested that even in patients with severe neurological symptoms, drainage could facilitate neurological recovery due to immediate spinal decompression.
Increased risk of spinal epidural hematoma was also anticipated due to anticoagulant. However, the frequency of spinal epidural hematoma after epidural anesthesia in patients taking the anticoagulant heparin is 1/3,100, which is lower than that after surgery [21, 22].
In conclusion, fluoroscopy-guided percutaneous epidural drainage is a less invasive treatment option for patients with a spinal epidural abscess and a poor general health condition.
Acknowledgements
Not applicable
Abbreviations
- FRS
Face rating scale
- L
Lumbar
- MRI
Magnetic resonance imaging
- Th
Thoracic
Authors’ contributions
MF analyzed the data and wrote the paper while TS managed the patient during his admission and helped with all the procedures. NS and YK supervised the development of the work done and helped in manuscript preparation. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Ethics approval and consent to participate
Not applicable
Consent for publication
Written informed consent was obtained from the patient and his family for publication of this case report and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Masashi Fujii, Email: manutarou@yahoo.co.jp.
Tsutomu Shirakawa, Email: shira@d4.dion.ne.jp.
Nobuaki Shime, Email: shime@koto.kpu-m.ac.jp.
Yasuyo Kawabata, Email: myasuyo88@gmail.com.
References
- 1.Khanna RK, Malik GM, Rock JP, Rosenblum ML. Spinal epidural abscess: evaluation of factors influencing outcome. Neurosurg. 1996;39:958–964. doi: 10.1097/00006123-199611000-00016. [DOI] [PubMed] [Google Scholar]
- 2.McGee-Collett M, Johnston IH. Spinal epidural abscess: presentation and treatment. A report of 21 cases. Med J Aust. 1991;155:14–17. doi: 10.5694/j.1326-5377.1991.tb116369.x. [DOI] [PubMed] [Google Scholar]
- 3.Mackenzie AR, Laing RB, Smith CC, Kaar GF, Smith FW. Spinal epidural abscess: the importance of early diagnosis and treatment. J Neurol Neurosurg Psychiatry. 1998;65:209–212. doi: 10.1136/jnnp.65.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rigamonti D, Liem L, Sampath P, Knoller N, Namaguchi Y, Schreilbman DL, et al. Spinal epidural abscess: contemporary trends in etiology, evaluation, and management. Surg Neurol. 1999;52:189–196. doi: 10.1016/S0090-3019(99)00055-5. [DOI] [PubMed] [Google Scholar]
- 5.Yang SY. Spinal epidural abscess. N Z Med J. 1982;95:302–304. [PubMed] [Google Scholar]
- 6.Tabo E. Successful percutaneous drainage of epidural abscess with epidural needle and catheter. Anesthesiology. 1994;80:1393–1395. doi: 10.1097/00000542-199406000-00028. [DOI] [PubMed] [Google Scholar]
- 7.Perez-Toro MR, Burton AW, Hamid B, Koyyalagunta D. Two-Tuohy needle and catheter technique for fluoroscopically guided percutaneous drainage of spinal epidural abscess: a case report. Pain Med. 2009;10:501–505. doi: 10.1111/j.1526-4637.2008.00552.x. [DOI] [PubMed] [Google Scholar]
- 8.Darouiche RO, Hamill RJ, Greenberg SB, Weathers SW, Musher DM. Bacterial spinal epidural abscess. Review of 43 cases and literature survey. Medicine (Baltimore). 1992;71:369–385. doi: 10.1097/00005792-199211000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Akalan N, Ozgen T. Infection as a cause of spinal cord compression: a review of 36 spinal epidural abscess cases. Acta Neurochir (Wien). 2000;142:17–23. doi: 10.1007/s007010050002. [DOI] [PubMed] [Google Scholar]
- 10.Lu CH, Chang WN, Lui CC, Lee PY, Chang HW. Adult spinal epidural abscess: clinical features and prognostic factors. Clin Neurol Neurosurg. 2002;104:306–310. doi: 10.1016/S0303-8467(02)00020-3. [DOI] [PubMed] [Google Scholar]
- 11.Baker AS, OJemann RG, Baker RA. To decompress or not to decompress—spinal epidural abscess. Clin Infect Dis. 1992;15:28–29. doi: 10.1093/clinids/15.1.28. [DOI] [PubMed] [Google Scholar]
- 12.Darouiche RO. Spinal epidural abscess. N Engl J Med. 2006;355:2012–2020. doi: 10.1056/NEJMra055111. [DOI] [PubMed] [Google Scholar]
- 13.Grewal S, Hocking G, Wildsmith JA. Epidural abscesses. Br J Anaesth. 2006;96:292–302. doi: 10.1093/bja/ael006. [DOI] [PubMed] [Google Scholar]
- 14.Savage K, Holtom PD, Zalavras CG. Spinal epidural abscess: early clinical outcome in patients treated medically. Clin Orthop Relat Res. 2005;439:56–60. doi: 10.1097/01.blo.0000183089.37768.2d. [DOI] [PubMed] [Google Scholar]
- 15.Foo D, Rossier AB. Preoperative neurological status in predicting surgical outcome of spinal epidural hematomas. Surg Neurol. 1981;15:389–401. doi: 10.1016/0090-3019(81)90178-6. [DOI] [PubMed] [Google Scholar]
- 16.Lawton MT, Porter RW, Heiserman JE, Jacobowitz R, Sonntag VK, Dickman CA. Surgical management of spinal epidural hematoma: relationship between surgical timing and neurological outcome. J Neurosurg. 1995;83:1–7. doi: 10.3171/jns.1995.83.1.0001. [DOI] [PubMed] [Google Scholar]
- 17.Kou J., Fischgrund J., Biddinger A., Herkowitz H. Risk Factors for Spinal Epidural Hematoma After Spinal Surgery. Spine. 2002;27(15):1670–1673. doi: 10.1097/00007632-200208010-00016. [DOI] [PubMed] [Google Scholar]
- 18.Schweich PJ, Hurt TL. Spinal epidural abscess in children: two illustrative cases. Pediatr Emerg Care. 1992;8:84–87. doi: 10.1097/00006565-199204000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Wang JS, Fellows DG, Vakharia S, Rosenbaum AE, Thomas PS. Epidural abscess – early magnetic resonance imaging detection and conservative therapy. Anesth Analg. 1996;82:1069–1071. doi: 10.1097/00000539-199605000-00034. [DOI] [PubMed] [Google Scholar]
- 20.Lyu RK, Chen CJ, Tang LM, Chen ST. Spinal epidural abscess successfully treated with percutaneous, computed tomography - guided, needle aspiration and parenteral antibiotic therapy: case report and review of the literature. Neurosurgery. 2002;51:509–512. doi: 10.1097/00006123-200208000-00039. [DOI] [PubMed] [Google Scholar]
- 21.Tryba M. Epidural regional anesthesia and low molecular heparin. Anasthesiol Intensivemed Notfallmed Schmerzther. 1993;28:179–181. doi: 10.1055/s-2007-998902. [DOI] [PubMed] [Google Scholar]
- 22.SCHROEDER D. Statistics: Detecting a rare adverse drug reaction using spontaneous reports. Regional Anesthesia and Pain Medicine. 1998;23(6):183–189. doi: 10.1016/S1098-7339(98)90145-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.


