Abstract
Objective:
Gender-based serologic differences for nonstructural protein 1(NS1) antigen (Ag) and IgM antibody (Ab) detection have been reported among cases of dengue in few studies. However, to understand its distribution with patient's gender and their demographic profile, this study is designed to fill the gaps in the available gender based data, and is the first from this region.
Materials and Methods:
A total of 4252 blood samples were collected aseptically during the outbreaks of 2016–17. Serum was separated and processed for dengue ELISA (NS1Ag and IgM Ab). All the relevant clinical data and variables such as gender and their demographic profile were recorded and statistically analyzed.
Results:
A total of 978 (23%) patients were found seropositive either by NS1 Ag or IgM Ab ELISA. The proportion of male was higher than female among all seropositive cases, with the ratio of (M:F) 1.54:1 (P < 0.0001). The males were predominately more affected compared to females among rural (P = 0.001) and semi-urban (P = 0.016) areas. The positive NS1 (P = 0.004) and IgM (P = 0.0001) both results were significantly associated with male gender.
Conclusion:
Every case of dengue must be screened for NS1Ag and IgMAb to increase the diagnostic precision, despite the males being more affected as compared to females due to sociocultural differences.
Keywords: Gender-specific dengue, IgM ELISA, non structural protein 1
Introduction
Globally, dengue fever has shown a significant increase in the past few decades.[1] Worldwide 3.9 billion population are at risk of dengue fever in more than 100 countries.[2] The reports from various National Surveillance Agencies suggest that dengue fever outbreaks from different parts of India have rapidly increased, thus contributing to global burden.[1] The outbreaks frequency in some states of North India, including Uttar Pradesh and Delhi, have become more susceptible to dengue fever.[3]
Aedes aegypti is the main vector for dengue virus infection. It mainly flourishes in particular settings such as areas where storage or waterlogging is common, like unfurnished/semi-furnished drainage systems in rural and semi-urban municipal areas and wherever waste disposal services are poor.[4,5] The hyper incidence of dengue fever in such settings might be related to specific demographic area and factors such as rural/semi-urban and gender, there is the inadequacy of gender-specific data because such studies are not routinely conducted and data reported or analyzed by most of the surveillance systems.[5]
A few international studies that have examined male and female dengue incidence have reported a significant association with male gender.[5,6] A contrasting result of an Indian study suggested that seropositivity and hemorrhagic findings were reported with greater propensity in females.[7] Hence, this study aims to understand the gender-based prevalence of dengue infection in rural population of Western Uttar Pradesh in North India.
Materials and Methods
This cross-sectional observational study, approved by University Ethics Committee “408 UPUMS/Dean/2018–2019 E. C. No.2017/82,” was conducted at this Tertiary Care Hospital in the Western part of Uttar Pradesh, India. The samples were received from clinically suspected cases with the presence of any or all of the signs and symptoms of dengue, such as fever/headache/myalgia/retro-orbital pain/rashes/hemorrhagic manifestations in the acute phase of their illness (1–6 days). A total of 4252 blood samples were aseptically collected and properly transported to the Viral Research and Diagnostic Laboratory at the Department of Microbiology during the outbreaks of 2016 and 2017. Serum was separated aseptically from the clotted blood, and one half was immediately processed for Non Structural Protein 1 (NS1) antigen and IgM Antibody Capture (MAC) ELISA, and the other half was stored at −80°C for further processing.
The diagnosis of cases was made by either/or both positive by NS1 antigen (NS1 Ag) and IgM antibody (IgM Ab) MAC ELISA. All the sera were subjected to ELISAs same day as per the manufacturer's instructions QUALISA Dengue NS1 (Qualpro diagnostics Pvt. Ltd., Goa, India) and MICROLISA IgM (J. Mitra and Co, New Delhi) as described below in brief.
For NS1 ELISA, a total of 50 μL sample diluent was added to each well and 100 μL of negative, positive controls were also added followed by serum samples in the corresponding wells. The plate was incubated for 30 min at 37°C. It was then washed to remove any unwanted and unbound antigens and blot dried. Further, 100 μL of conjugate was added to each well and plate again incubated for 60 min at 37°C followed by washing and drying. Further, 100 μL of substrate was added, and plate again incubated for 15 min in dark at room temperature. Finally, 100 μL of stop solution was added, and absorbance was read at 450 nm.
For IgM ELISA, a total of 100 μL of negative and positive controls, calibrator and 100 μL diluted serum samples (1:100) were added to corresponding wells and incubated at 37°C for 60 min. The plate was washed 5 times and dried. Further, 100 μL of conjugate was then added, and plate incubated for 60 min at 37°C. After incubation, washing was done, and then 100 μL of substrate was added and incubated in dark for 30 min at 37°C. Finally, 100 μL of stop solution was added, and absorbance was read at 450 nm.
The data entry and results analysis were done with the Statistical Package for Social Sciences (SPSS) version 22.0 (IBM Corp., Armonk, New York, USA). All the relevant variables were analyzed by descriptive statistics. P < 0.05 was considered statistical significant.
Results
Of the total samples, 978 (23%) patients were found seropositive for dengue either by NS1 or IgM ELISA [Table 1]. Of the total seropositive patients (978), the proportion of male was higher over female with the ratio of (M:F) being 1.54:1 [Table 1]. This difference between male and female preponderance among all seropositive cases was statistically significant (P < 0.0001). The observed mean age ± standard deviation of all patients was 27.16 ± 14.82 years. Among all the seropositive cases, 527 (12.39%) patients belonged to rural, 209 (4.91%) were from semi-urban areas, and 242 (5.69%) were from urban areas. The male cases were predominately significant from rural (P = 0.001) and semi-urban (P = 0.016) areas as compared to females except urban (P > 0.05) area [Table 1].
Table 1.
Gender and locality wise distribution of suspected dengue cases (n=4252)
| Gender | Total samples, n (%) | Positive samples, n (%) | NS1 Ag positive, n (%) | IgM Ab positive, n (%) | NS1 and IgM both positive, n (%) | Locality | ||
|---|---|---|---|---|---|---|---|---|
| Rural, n (%) | Semi urban, n (%) | Urban, n (%) | ||||||
| Male | 2284 (53.71) | 594 (26) | 449 (19.65) | 326 (14.27) | 181 (7.92) | 321 (14.05) | 130 (5.69) | 143 (6.26) |
| Female | 1968 (46.28) | 384 (19.51) | 307 (15.59) | 208 (10.56) | 131 (6.65) | 206 (10.46) | 79 (4.01) | 99 (5.03) |
| Level of (P<0.05) considered to be statistically significant | <0.0001 | 0.004 | 0.001 | >0.05 | 0.001 | 0.016 | >0.05 | |
NS1 Ag: Non structural protein 1 antigen; IgM Ab: IgM Antibody
A total of 756 cases were detected positive for dengue by NS1 alone, 534 by IgM and 312 cases were detected by both NS1 and IgM ELISA [Table 2]. It was also observed that 444 cases were detected positive by NS1 ELISA where IgM ELISA was negative. It might be due to the fact that the sample may have been collected within a week of the illness when IgM antibodies against the virus were not formed. IgM antibodies were detected in 222 cases only, and these cases might have reported after 1 week of illness [Table 2].
Table 2.
Cross table between NS1 and IgM ELISA among total seropositive dengue fever cases (n=978)
| Tests name (ELISA) | IgM (MAC) | Total (%) | ||
|---|---|---|---|---|
| Positive (%) | Negative (%) | |||
| NS1 | Positive | 312 (31.9) | 444 (45.4) | 756 (77.3) |
| Negative | 222 (22.7) | 00 (00) | 222 (22.7) | |
| Total | 534 (54.6) | 444 (45.4) | 978 (100) | |
NS1: Non structural protein 1; IgM (MAC): IgM antibody capture; ELISA: Enzyme-linked immunosorbent assay
A marked rise in the number of dengue positive cases was observed between August and December in both epidemics of 2016 and 2017. In both epidemics, the males were more commonly affected than females [Figure 1]. In the epidemic of 2016, the seropositive cases were observed from August 2016 onward, and 22 cases were reported this month and rose steeply to 164 in September 2016. In October 2016, maximum number of cases detected were 228. In epidemic of 2017, the first case was reported positive in July 2017 as single case in this month but followed by steep rose with 35 cases being positive in August 2017. Two hundred and thirty cases were reported positive in September 2017, with maximum of 426 cases being detected in October 2017 [Figure 1]. A total of 525 (324 males and 201 females) cases were detected in the year 2016 and 453 (270 males and 183 females) cases were detected in 2017. Hence, the overall seroprevalence of dengue in both the years in the present study is 978/4252 (594 males and 384 females).
Figure 1.
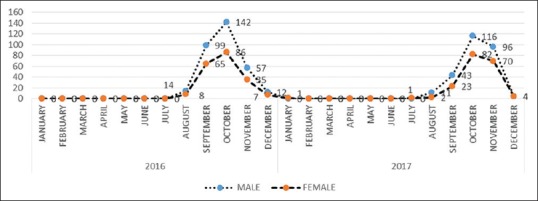
Gender wise monthly distribution of dengue cases (epidemic season 2016–2017)
Discussion
Dengue fever has become a major public health problem in India, especially north India, including Delhi and its adjoining states. Currently, to scale the severity and monitor the epidemics of dengue, several strategies have been operating at National and State level under various National and State Sentinel Surveillance System in our country. The National Vector Borne Disease Control Programme and Integrated Disease Surveillance Programme (IDSP) are mutually functioning for passive sentinel surveillance program for prevention and control of dengue.[8]
In the present study, 23% of the suspected cases were found seropositive for dengue during outbreaks of 2016–2017. Although the prevalence of gender-wise distribution of dengue cases is not well defined, only few studies have characterized the gender-based prevalence.[7,9] The exposure of the persons to disease-prone environment and conditions might be associated with demographic factors such as habitat, age, and gender. One recent Indian study found that the association of gender-based serological findings among 700 patients suspected to be of dengue. Of these, 40% of suspected cases were found serologically positive, it shows dengue is significantly associated with the female gender.[7] This study was hospital based, and due to the small sample size, it did not reflect the actual gender-based prevalence of the infected population.
In the present study, the sample size is 6-fold more compared to the previous study, and it was found that males being affected significantly more compared to females. Similarly, many other Indian studies independently done by Agarwal et al., Ray et al., and Wali et al., found a higher number of male patients infected with dengue compared to females, sex ratio (M:F) being 1.9:1, 1:0.57, and 2.5:1, respectively.[10,11,12]
A seroanalysis based large sample size study demonstrated that males were more prominently affected than females in preceding 3 years' epidemic data.[13] The studies from several other Asian countries have shown a consistent pattern of males being more commonly affected.[9] It might be due to differences in sociocultural environment where male are more exposed to outdoor activities and their bodies less covered as compared to females.[14,15]
The results in our study are supported by above studies, where males are more affected compared to females. Similar results have also been obtained in various other studies across the world. Goswami et al. have found a statistically significant association between the presence of NS1 antigens and IgM antibodies among male gender.[16] Brown et al. have reported a significantly higher sensitivity of IgM antibody ELISA in male gender.[9]
The NS1 ELISA being the most potent tool, it was able to detect 444 cases more where IgM was negative. Although the IgM was detected in 222 cases more, where NS1 was negative. The NS1 protein is highly sensitive; it becomes detectable from the onset of dengue fever among both primary and secondary infection. At the onset of infection, it is presented in higher concentration in the patient's blood samples.[17] It a reliable viral marker for diagnosis initially (from day 1) fever, but the sensitivity declines after 4–5 days of onset and finally antigen titer becoming undetectable.[18] The present study has been carried out at this tertiary care hospital, and some cases might have reported later in the illness. Thus, to maintain the diagnostic accuracy and efficacy, we used NS1 and IgM ELISA simultaneously in each sample.
The NS1 ELISA is able to detect up to 50% of cases more when used alone, and it is a highly sensitive and specific test. The inclusion of NS1 ELISA in the test panel minimizes the chance of missing any case.[2,19]
Thus, the combined results of both assays (NS1 and IgM ELISA) show that the overall accuracy and diagnostic ability to identify dengue fever may help increase the overall diagnostic sensitivity.
Conclusion
To the best of our knowledge, it is first study with a large sample size to know the gender-based prevalence in this region of our country. We report each of the single positive case to IDSP and the National Institute of Epidemiology on the day of reporting.; hence, we assume genuineness of the submitted data. Thus, we conclude here that despite the male preponderance, every single case must be investigated for dengue serologically for NS1 Ag and IgM Ab, irrespective of the gender.
Financial support and sponsorship
This study was supported by VRDL-ICMR (DHR), Ministry of Family and Health Welfare, Government of India.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mutheneni SR, Morse AP, Caminade C, Upadhyayula SM. Dengue burden in India: Recent trends and importance of climatic parameters. Emerg Microbes Infect. 2017;6:e70. doi: 10.1038/emi.2017.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Debnath F, Ponnaiah M, Acharya P. Dengue fever in a municipality of West Bengal, India, 2015: An outbreak investigation. Indian J Public Health. 2017;61:239–42. doi: 10.4103/ijph.IJPH_309_16. [DOI] [PubMed] [Google Scholar]
- 3.Jain S, Mittal A, Sharma SK, Upadhyay AD, Pandey RM, Sinha S, et al. Predictors of dengue-related mortality and disease severity in a tertiary care center in North India. Open Forum Infect Dis. 2017;4:ofx056. doi: 10.1093/ofid/ofx056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Getachew D, Tekie H, Gebre-Michael T, Balkew M, Mesfin A. Breeding sites of Aedes aegypti: Potential dengue vectors in dire dawa, East Ethiopia. Interdiscip Perspect Infect Dis. 2015;706276:1–8. doi: 10.1155/2015/706276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anker M, Arima Y. Male-female differences in the number of reported incident dengue fever cases in six Asian countries. Western Pac Surveill Response J. 2011;2:17–23. doi: 10.5365/WPSAR.2011.2.1.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ooi EE. Changing pattern of dengue transmission in Singapore. WHO Regional Office for South-East Asia (Dengue Bulletin) 2001;25:40–5. [Google Scholar]
- 7.Chakravarti A, Arora R, Luxemburger C. Fifty years of dengue in India. Trans R Soc Trop Med Hyg. 2012;106:273–82. doi: 10.1016/j.trstmh.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 8.Chakravarti A, Roy P, Malik S, Siddiqui O, Thakur P. A study on gender-related differences in laboratory characteristics of dengue fever. Indian J Med Microbiol. 2016;34:82–4. doi: 10.4103/0255-0857.174106. [DOI] [PubMed] [Google Scholar]
- 9.Brown MG, Vickers IE, Salas RA, Smikle MF. Seroprevalence of dengue virus antibodies in healthy Jamaicans. Hum Antibodies. 2009;18:123–6. doi: 10.3233/HAB-2009-0207. [DOI] [PubMed] [Google Scholar]
- 10.Agarwal R, Kapoor S, Nagar R, Misra A, Tandon R, Mathur A, et al. A clinical study of the patients with dengue hemorrhagic fever during the epidemic of 1996 at Lucknow, India. Southeast Asian J Trop Med Public Health. 1999;30:735–40. [PubMed] [Google Scholar]
- 11.Ray G, Kumar V, Kapoor AK, Dutta AK, Batra S. Status of antioxidants and other biochemical abnormalities in children with dengue fever. J Trop Pediatr. 1999;45:4–7. doi: 10.1093/tropej/45.1.4. [DOI] [PubMed] [Google Scholar]
- 12.Wali JP, Biswas A, Handa R, Aggarwal P, Wig N, Dwivedi SN. Dengue haemorrhagic fever in adults: A prospective study of 110 cases. Trop Doct. 1999;29:27–30. doi: 10.1177/004947559902900110. [DOI] [PubMed] [Google Scholar]
- 13.Prakash O, Singh DD, Mishra G, Prakash S, Singh A, Gupta S, et al. Observation on dengue cases from a virus diagnostic laboratory of a tertiary care hospital in North India. Indian J Med Res. 2015;142(Suppl):S7–S11. doi: 10.4103/0971-5916.176596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prasith N, Keosavanh O, Phengxay M, Stone S, Lewis HC, Tsuyuoka R, et al. Assessment of gender distribution in dengue surveillance data, the Lao people's democratic republic. Western Pac Surveill Response J. 2013;4:17–24. doi: 10.5365/WPSAR.2012.3.4.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaplan JE, Eliason DA, Moore M, Sather GE, Schonberger LB, Cabrera-Coello L, et al. Epidemiologic investigations of dengue infection in Mexico, 1980. Am J Epidemiol. 1983;117:335–43. doi: 10.1093/oxfordjournals.aje.a113546. [DOI] [PubMed] [Google Scholar]
- 16.Goswami L, Runumi C, Rasul ES. Seroprevalence of dengue infection in a tertiary care hospital in Assam. Int J Med Dent Sci. 2018;7:1582–5. [Google Scholar]
- 17.Anand AM, Sistla S, Dhodapkar R, Hamide A, Biswal N, Srinivasan B. Evaluation of NS1 antigen detection for early diagnosis of dengue in a tertiary hospital in Southern India. J Clin Diagn Res. 2016;10:DC01–4. doi: 10.7860/JCDR/2016/15758.7562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gowri Sankar S, Dhananjeyan KJ, Paramasivan R, Thenmozhi V, Tyagi BK, John Vennison S. Evaluation and use of NS1 igM antibody detection for acute dengue virus diagnosis: Report from an outbreak investigation. Clin Microbiol Infect. 2012;18:E8–10. doi: 10.1111/j.1469-0691.2011.03694.x. [DOI] [PubMed] [Google Scholar]
- 19.Tricou V, Vu HT, Quynh NV, Nguyen CV, Tran HT, Farrar J, et al. Comparison of two dengue NS1 rapid tests for sensitivity, specificity and relationship to viraemia and antibody responses. BMC Infect Dis. 2010;10:142. doi: 10.1186/1471-2334-10-142. [DOI] [PMC free article] [PubMed] [Google Scholar]


