Abstract
Background and Aims:
Regional analgesia may play a role in pain management during breast surgery. Ultrasound approach to paravertebral block may be challenging. This study compared success rates of ultrasound-guided erector spinae plane block (ESPB) versus parasagittal in-plane thoracic paravertebral block among senior anaesthesia residents in modified radical mastectomy.
Methods:
One hundred and two female patients undergoing modified radical mastectomy were randomly categorized into PARA group receiving sagittal in-plane paravertebral block and ESPB group receiving erector spinae plane block. The block in the 1st six cases in each group was done by an experienced consultant as a demonstration for three anaesthesia residents not experienced in either block. Primary endpoint was assessing success rate of the blocks. Secondary endpoint was the haemodynamic response to skin incision and postoperative analgesia.
Results:
All patients were females undergoing modified radical mastectomy. Success rate among residents was 100% in ESPB versus 77.8% in PARA group (P = 0.002). Duration to perform the block was less in ESPB group (4.39 ± 1.2 min) than PARA group (8.18 ± 2.42 min) (P < 0.0001). Guidance frequency by consultants was significantly higher in PARA than ESPB group. Time to 1st analgesic requirement and morphine consumption postoperatively were insignificant between the groups. There was no significant difference regarding haemodynamics.
Conclusion:
ESPB may be a simple and safe alternative to parasagittal in-plane paravertebral block to provide postoperative analgesia in modified radical mastectomy especially in novice practitioners. It provides equivalent profile of postoperative analgesia with less time to perform the block.
Key words: Erector spinae, mastectomy, nerve block, paravertebral
INTRODUCTION
Breast cancer is one of the most important medical problems in the female gender, since among every eight women, one will suffer from breast cancer during her lifetime.[1] Proper pain control during and after breast surgery not only enhances patient recovery but also may prevent the development of chronic postoperative pain.[2] A variety of regional anaesthetic techniques may play a role in pain management during breast surgery from which thoracic paravertebral block may be considered the “gold standard.”[3] However, the ultrasound approach and needle manipulations to reach the paravertebral space may be challenging.[4] In addition, adverse effects like pneumothorax, epidural and intrathecal spread have been documented.[5] ESPB is a novel interfascial plane block originally described for treatment of neuropathic pain and acute pain following thoracic surgery.[6] The primary endpoint of the present study was to assess the success rates of the ESPB technique compared with the paravertebral among senior anaesthesia residents. The technique was considered successful if it had been carried out by the anaesthesia resident in 10 min or less. The technique was judged by an anaesthesia consultant as successful in the PARA group after forward displacement of the pleura by the local anaesthetic and in the ESPB group by elevation of the erector spine muscles. The time to perform the block by each resident was recorded and a learning curve for the two blocks was depicted. Secondary endpoint was to assess the two techniques regarding the haemodynamic response to skin incision and intensity of postoperative analgesia in terms of the visual analogue scale (VAS) score, 1st postoperative analgesic requirement, and the total postoperative opioid consumption. Any adverse effects related to the regional anaesthetic technique were also documented.
METHODS
This prospective randomised study was reviewed and approved by the Ethics Committee of the Alexandria Main University Hospitals (IRB # 00007555) and a written informed consent was obtained from each patient for participation in the study. The trial was conducted in the period between May 2018 and March 2019. The trial adhered to the principles of the declaration of Helsinki and was registered prior to patient enrollment at Pan-African Clinical Trial Registry (PACTR201805003353131, Principal investigator: Alabd AS, date of registration: 7th May, 2018). All eligible patients were approached for enrolment. Patients were selected from those belonging to the American Society of Anesthesiologists (ASA) class I or II, aged 40–65 years and scheduled for modified radical mastectomy at Alexandria Main University Hospitals. Patients were excluded if they had long standing diabetes mellitus (>5 years), any allergy to the study drugs, local infection at any of the puncture sites, any coagulation disorder or any neurological or psychological problem that may interfere with proper subjective interpretation of the results. Patients were optimised preoperatively. On the day of surgery, patients were admitted to the operative theatre and standard monitoring was applied. An intravenous line was inserted on the dorsum of the hand opposite to that of the operative side and premedication in the form of 2 mg midazolam and 1 μg.kg-1 fentanyl was done intravenously. Preoxygenation with 100% oxygen was done via a face mask for 3 min, then anaesthesia was induced with 2 mg.kg-1 propofol and atracurium 0.25 mg.kg-1 and a suitable sized laryngeal mask airway was inserted and secured in place. Patients were subjected to controlled mechanical ventilation technique aiming to maintain end-tidal CO2 between 35 and 40 mmHg. Then, patients were positioned lateral with the operative side above. Patients were randomly categorised into two equal groups by a third party not involved in the study using a numbered closed envelope method to be subjected to the planned regional anaesthetic block. All blocks were performed guided by a 5–13 MHz linear ultrasound probe covered in a sterile sheath attached to a Sonosite (M-Turbo; SonoSite Inc, Bothell, W, USA) portable ultrasound machine. Six successive blocks in each technique were performed by two staff anaesthesiologists who have more than 3 years' experience in ultrasound-guided regional anaesthesia and performed more than 200 blocks. These blocks were done as a demonstration to three senior anaesthesia residents. Residents were selected from those who have performed ultrasound-guided regional blocks under supervision, yet have no previous experience regarding the two studied techniques. The three residents attended and observed the 12 blocks which have been done by the two consultants. Every senior resident performed 15 successive blocks in each group under full supervision of one of the two staff anaesthesiologists. Standard disinfection was applied to the area to be blocked and the block was performed according to the following technique.
For the paravertebral block, the ultrasound transducer was applied in the parasagittal plane approximately 2.5 cm lateral to the midline till identification of the 4th thoracic vertebra. The position of the ultrasound transducer was adjusted to bring the targeted paravertebral space at the centre of the image. A 20-gauge, non-insulated, 100-mm needle (Ultraplex; B. Braun Medical, Bethlehem, Pa) was inserted at the caudal border of the transducer and advanced in a straight sagittal direction to cranial and anterior. The needle tip was observed to enter through the superior costotransverse ligament. Twenty ml of 0.25% bupivacaine was deposited just superficial to the hyperechoic pleural line. Anterior displacement of the underlying pleura confirmed proper local anaesthetic injection.[7]
For the erector spinae plane block, the ultrasound transducer was applied in the parasagittal plane lateral to the 4th thoracic spine. The transducer was slid horizontally till the tip of the transverse process became in view. Three longitudinal muscles were identified from superficial to deep: trapezius, rhomboid major, and erector spinae muscles. A 20-gauge, non-insulated, 100-mm needle (Ultraplex; B. Braun Medical, Bethlehem, Pa) was introduced in plane from caudad to cephalad till the tip reaches the plane deep to the erector spinae and 20 ml 0.25% bupivacaine was deposited deep to the muscle.[6] Upward displacement of erector spinae muscles confirmed proper local anaesthetic injection.
The duration of the technique performed by the residents was recorded, which is the time between beginning of ultrasound scanning and completion of deposition of the local anaesthetic in the plane identified. Inability of any of the residents to specify the plane correctly or to follow the needle tip during injection was guided by one of the two investigators and was recorded as a guidance intervention by a second investigator. Guidance intervention was defined as instructions that guide the resident either to modify the image of the plane by applying one of the probe manipulations or to modify the needle tip or angle in a certain direction. This was applied verbally without placing a hand with the resident. Any block taking more than 10 min to be performed or has been taken over by the staff anaesthesiologist due to technical difficulties was considered a failure and its duration was recorded as a maximum (10 min). Successful block performance was defined as completion of the block within 10 min with or without verbal guidance from the supervising consultant. The technique was considered successful in the PARA group after forward displacement of the pleura by the local anaesthetic and in the ESPB group by elevation of the erector spine muscles.
After performing the regional anaesthetic block, patients were turned to the supine position and surgery was allowed to proceed after proper positioning, disinfection, and draping. Anaesthesia was maintained in all patients with isoflurane 1% in 50% oxygen air mixture and patients were discharged to the post-anaesthesia care unit after full recovery from anaesthesia. Near the end of the surgical procedure, 1 g of paracetamol infusion was administered and was continued every 6 h postoperatively. Intraoperatively, the heart rate (HR) and mean arterial blood pressure (MABP) were recorded just after skin incision and every 5 min for 15 min. Pain was assessed postoperatively every 4 h for 24 h by a third investigator blinded to the technique of regional analgesia using a 0–10 cm VAS score. Patients experiencing pain ≥4 were managed with 2 mg morphine every 5 min till pain is <4. The time to 1st analgesic requirement postoperatively and the total dose of morphine consumption during the study period were recorded. Any adverse events related to the regional block were managed accordingly and recorded.
Using two proportions power analysis in National Council for the Social Studies and Power and sample size (NCSS and PASS) program, a sample size of 90 patients (45 blocks per group) was found to achieve 81% power to detect a difference of 30% success rate between the ESPB technique compared to the paravertebral technique at significance level of 5%.
RESULTS
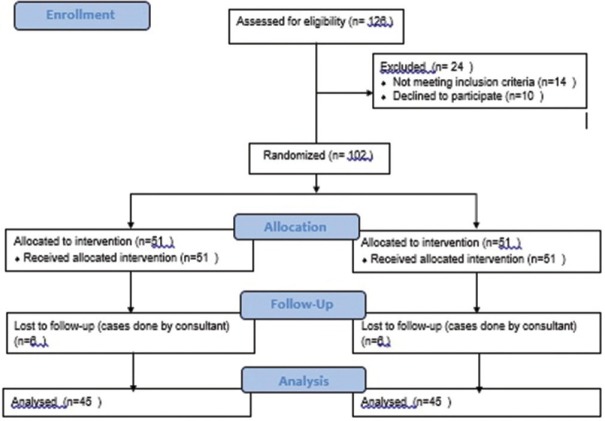
One hundred and twenty six patients were screened for recruitment. Fourteen patients did not meet the recruitment criteria and 10 patients refused to participate in the study. One hundred and two patients were included in the study. The block in the 1st six patients in each group was done by one of the two consultants as a demonstration and were not included in the statistical analysis [Figure 1]. The following 90 patients were divided equally into two groups: Group Para and group ESPB. All patients were females undergoing modified radical mastectomy with axillary clearance. There was no significant difference between the two groups regarding HR or MABP before surgical incision as well as during the studied periods after skin incision [Tables 1 and 2]. Time to 1st analgesic requirement as well as the total morphine consumption postoperatively showed no significant differences between the two studied groups [Table 3]. The success rate of the regional anaesthetic block among residents reached 100% in the ESPB while it was 77.8% in the PARA group (P = 0.002). The mean duration to perform the regional anaesthetic technique was significantly less in the ESPB group (4.39 ± 1.2 min) than the PARA group (8.18 ± 2.42 min) with a P value of < 0.0001.
Figure 1.
Consort flow diagram
Table 1.
Comparison of intraoperative heart rate variations in the two groups
| ESPB (n=45) | PARA (n=45) | Test of significance P | |
|---|---|---|---|
| Heart rate# (beats/min) | |||
| At base | 80.37±10.7 | 82.6±10.5 | (t=-0.992, P=0.324) |
| Incision | 82.11±10.33 | 85.48±12.56 | (t=-1.39, P=0.167) |
| After 5 min | 81.09±9.1 | 84.09±10.5 | (t=-1.45, P=0.151) |
| After 10 min | 77.42±9.76 | 81.28±10.47 | (t=-1.81, P=0.07) |
| After 15 min | 75.28±10.52 | 78.6±10.92 | (t=-1.5, P=0.14) |
#HR at each time was described by Mean±SD
Table 2.
Comparison of intraoperative mean arterial blood pressure variations in the two groups
| ESPB (n=45) | PARA (n=45) | Test of significance (P) | |
|---|---|---|---|
| Mean arterial blood pressure (mmHg)# | |||
| At base | 95.78±9.14 | 95.17±8.88 | (t=0.316, P=0.753) |
| Incision | 96.95±9.3 | 94.15±11.20 | (t=1.29, P=0.201) |
| After 5 min | 94.82±8.26 | 93.91±10.07 | (t=0.469, P=0.64) |
| After 10 min | 92.02±9.13 | 91.71±8.85 | (t=0.164, P=0.870) |
| After 15 min | 92.2±9.35 | 90.46±8.11 | (t=0.939, P=0.350) |
#MABP at each time was described by Mean±SD
Table 3.
Assessment of postoperative analgesia of the two regional techniques
| ESPB (n=45) | PARA (n=45) | Test of significance (P) | |
|---|---|---|---|
| Time to 1st analgesic requirement (h)Mean±SD | 11.04±1.9 | 11.22±1.95 | (t=-0.437, P=0.66) |
| Total morphine consumption (mg)Mean±SD | 6.17±2.08 | 6.22±2.09 | (t=-0.101, P=0.92) |
t; independent t-test
There were significantly more guidance interventions in the PARA group compared to the ESPB group. Residents required guidance by the consultants from 0 to 2 times with a median of 0 in the ESPB group relative to 0–3 times with a median of 2 in the PARA group. This difference between the two groups was statistically significant with a P value of ≤0.001 Table 4. The mean duration to perform the block for the three residents was calculated for every case number successively and a curve was depicted which was considered the learning curve for mastering the technique among the residents [Figure 2].
Table 4.
Assessment of technique mastering among residents
| ESPB (n=45) | PARA (n=45) | Test of significance (P) | |
|---|---|---|---|
| Duration of the technique (min) Mean±SD |
4.39±1.2 | 8.18±2.42 | (t=-9.39, P<0.0001*) |
| Frequency of guidance to interventions Median (Min-Max) |
0 (0-2) | 2 (0-3) | (U=1.637, P<0.001*) |
| Success Rate among residents (%) | 100 | 77.8 | (χ2=9.11, P=002*) |
t; independent t-test, U; Mann-Whitney test, χ2: Chi-square test, *;statistically significant
Figure 2.
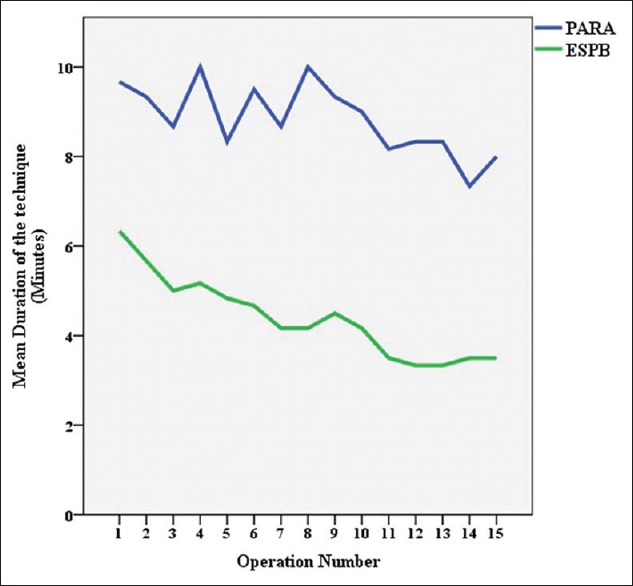
Learning curve of ESPB and Paravertebral Block among senior anaesthesia residents
DISCUSSION
The present study demonstrated that senior anaesthesia residents in Alexandria university hospitals managed the ESPB better than the parasagittal in-plane paravertebral block in cases of modified radical mastectomy. Those residents have had a previous experience in ultrasound-guided peripheral nerve and plane blocks other than the studied techniques. Such observation was evident in terms of significantly higher success rate, less requirement of guidance, and shorter duration to perform the technique in 15 successive cases under supervision of two experienced anaesthesia consultants and after observation of the technique in six cases managed by the consultants. The learning curve depicted in the present study was based on the progressive variation of the duration to perform the technique among residents [Figure 2]. It was progressively sloping downwards in the ESPB group other than the ups and downs shown in the curve of the PARA group which may reflect better mastering of the ESPB technique relative to the paravertebral technique with time. This was in conjunction with no apparent superiority of the paravertebral block over the ESPB in terms of intra- and postoperative analgesia as evident by insignificant differences between the two groups regarding the haemodynamic changes after surgical incision, the duration to 1st postoperative analgesic requirement, and the total morphine consumption postoperatively. With review of the medical literature, this may be the first study to compare the ESPB and the paravertebral block in terms of feasibility and effectiveness in cases of modified radical mastectomy.
Several previous studies have documented that ultrasound-guided paravertebral block is an advanced regional anaesthetic technique that requires special skills to manipulate the needle under ultrasonography toward the paravertebral space. Krediet et al.[7] in their illustrative review of the thoracic paravertebral space concluded that at least nine approaches are available for the thoracic paravertebral block. Each approach may have its own aspects of technical difficulty. The parasagittal in-plane view may place a challenge to the practitioner owing to the difficulty to find an acoustic window to pass the needle between the transverse processes toward the thoracic paravertebral space. When evaluating the paravertebral block versus the serratus intercostal plain blocks in breast surgery, authors documented that the paravertebral block was rather difficult in 15 out of 25 cases. This observation was in spite of selecting patients with a body mass index less than 25 which may entail less angle between the needle and the transducer and hence, expected better visualisation of the needle.[8] El-Boghdadly[9] mentioned that the thoracic paravertebral block is a highly challenging technique that requires much training rendering it impractical in the currently overloaded ultrasound training workshops. Concomitantly, complications of thoracic paravertebral block like inadvertent pleural puncture and epidural or intrathecal spread are still a concern even with ultrasound utilisation.[10]
Ultrasound-guided ESPB has been originally described for pain relief in patients with chronic neuropathic pain. However, a few recent case reports[11,12,13,14] and randomised controlled trials[15,16,17] found it effective as a postoperative analgesic technique and to reduce the postoperative opioid consumption following breast surgeries. When Forero et al.[6] performed their initial report on ESPB, they realised that when a dye is injected with guidance of ultrasonography deep to the erector spinae muscle plane, it spreads far deep and in certain levels beyond the superior costotransverse ligament. This may explain the similarity between the ESPB and the paravertebral block in the present study regarding the postoperative analgesic profile of the two techniques. Forero et al. also documented in their report the safety and simplicity of the technique. However to date, no previous studies investigated such simplicity relative to the gold standard paravertebral block.
Recently, an article published by Ivanusic et al.[18] on cadaveric models, documented that the dye injected deep to the erector spinae plane did not stain the ventral rami of the intercostal nerves suggesting a different mechanism of action of ESPB other than that due to paravertebral spread. They suggested that the mechanism of breast analgesia may be related to the marked cephalad and lateral spread of the injectate to the lateral cutaneous branches of the intercostal nerves.
Limitations to the present study include the small number of cases performed by every resident and performance of the block after induction of general anaesthesia with lack of objective determination of the spread and the onset of the block. Also, one of the limitations is the inability to blind observers who determined the number of guidance interventions.
CONCLUSION
We concluded that the ESPB may be a simple and safe alternative to the parasagittal in-plane paravertebral block to provide postoperative analgesia in cases of modified radical mastectomy especially in novice practitioners. It provides an equivalent profile of postoperative analgesia with less time consumption to perform the block.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Self-fund.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fizgerald SP. Breast-cancer screening—viewpoint of the IARC Working Group. N Engl J Med. 2015;373:1479. doi: 10.1056/NEJMc1508733. [DOI] [PubMed] [Google Scholar]
- 2.Mejdahl MK, Andersen KG, Gärtner R, Kroman N, Kehlet H. Persistent pain and sensory disturbances after treatment for breast cancer: Six year nationwide follow-up study. BMJ. 2013;346:f1865. doi: 10.1136/bmj.f1865. [DOI] [PubMed] [Google Scholar]
- 3.Simpson J, Ariyarathenam A, Dunn J, Ford P. Breast surgery using thoracic paravertebral blockade and sedation alone. Anesthesiol Res Pract. 2014;2014:127467. doi: 10.1155/2014/127467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abdallah FW, Brull R. Off side! A simple modification to the parasagittal in-plane approach for paravertebral block. Reg Anesth Pain Med. 2014;39:240–2. doi: 10.1097/AAP.0000000000000086. [DOI] [PubMed] [Google Scholar]
- 5.Gadsden JC, Lindenmuth DM, Hadzic A, Xu D, Somasundarum L, Flisinski KA. Lumbar plexus block using high-pressure injection leads to contralateral and epidural spread. Anesthesiology. 2008;109:683–8. doi: 10.1097/ALN.0b013e31818631a7. [DOI] [PubMed] [Google Scholar]
- 6.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block. A novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 7.Krediet AC, Moayeri N, van Geffen GJ, Bruhn J, Renes S, Bigeleisen PE, et al. Different approaches to ultrasound-guided thoracic paravertebral block. Anesthesiology. 2015;123:459–74. doi: 10.1097/ALN.0000000000000747. [DOI] [PubMed] [Google Scholar]
- 8.Pérez Herrero MA, López Álvarez S, Fadrique Fuentes A, Manzano Lorefice F, Bartolomé Bartolomé C, et al. Quality of postoperative recovery after breast surgery. General anaesthesia combined with paravertebral versus serratus-intercostal block. Rev Esp Anestesiol Reanim. 2016;63:564–71. doi: 10.1016/j.redar.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 9.El-Boghdadly K, Pawa A. The eretor spinae plane block: Plane and simple. Anaesthesia. 2017;72:434–8. doi: 10.1111/anae.13830. [DOI] [PubMed] [Google Scholar]
- 10.Kus A, Gurkan Y, Gul Agkul A, Solak M, Toker K. Pleural puncture and intrathoracic catheter placement during ultrasound guided paravertebralblock. J Cardiothorac Vasc Anesth. 2013;27:e11–2. doi: 10.1053/j.jvca.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 11.Singh S, Chowdhary NK. Erector spinae plane block an effective block for postoperative analgesia in modified radical mastectomy. Indian J Anaesth. 2018;62:148–50. doi: 10.4103/ija.IJA_726_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ohgoshi Y, Ikeda T, Kurahashi K. Continuous erector spinae plane block provides effective perioperative analgesia for breast reconstruction using tissue expanders: A report of two cases. J Clin Anesth. 2018;44:1–2. doi: 10.1016/j.jclinane.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 13.Bonvicini D, Tagliapietra L, Giacomazzi A, Pizzirani E. Bilateral ultrasound-guided erector spinae plane blocks in breast cancer and reconstruction surgery. J Clin Anesth. 2018;44:3–4. doi: 10.1016/j.jclinane.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 14.Nair AS, Seelam S, Naik V, Rayani BK. Opioid- free mastectomy in combination with ultrasound – Guided erector spinae block: A series of five cases. Indian J Anaesth. 2018;62:632–4. doi: 10.4103/ija.IJA_314_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gürkan Y, Aksu C, Kuş A, Yörükoǧlu UH, Kılıç CT. Ultrasound guided erector spinae plane block reduces postoperative opioid consumption following breast surgery: A randomized controlled study. J Clin Anesth. 2018;50:65–8. doi: 10.1016/j.jclinane.2018.06.033. [DOI] [PubMed] [Google Scholar]
- 16.Oksuz G, Bilgen F, Arslan M, Duman Y, Urfalıoglu A, Bilal B. Ultrasound guided bilateral erector spinae block versus tumescent anesthesia for postoperative analgesia in patients undergoing reduction mammoplasty: A randomized controlled study. Aesth Plast Surg. 2019;43:291–6. doi: 10.1007/s00266-018-1286-8. [DOI] [PubMed] [Google Scholar]
- 17.Singh S, Kumar G, Akhileshwar Ultrasound-guided erector spinae plane block for postoperative analgesia in modified radical mastectomy: A randomised control study. Indian J Anaesth. 2019;63:200–4. doi: 10.4103/ija.IJA_758_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ivanusic J, Konishi Y, Barrington MJ. A cadaveric study investigating the mechanism of action of erector spinae blockade. Reg Anesth Pain Med. 2018;43:567–71. doi: 10.1097/AAP.0000000000000789. [DOI] [PubMed] [Google Scholar]