Abstract
Background and Aims:
The multimodal analgesia strategies to minimise opioid-related side effects are highly desirable in bariatric surgical procedures. We evaluated the efficacy of ultrasound-guided transversus abdominis plane (USG-TAP) block and intravenous lidocaine for postoperative analgesia in obese patients undergoing laparoscopic bariatric surgery.
Methods:
We studied 56 patients with body mass index >35 kg/m2. They were randomly allocated to Lidocaine group (Group A) and USG-TAP group (Group B). Group A patients were given intravenous Lidocaine (1.5 mg/kg) bolus followed by (1.5 mg/kg/h) infusion. Group B patients were given ultrasound-guided bilateral TAP block using 20 cc of 0.375% ropivacaine each side. Postoperative numeric rating pain scale score (NRS) hours were compared. Other parameters compared were total fentanyl requirement, sedation score, postoperative nausea vomiting (PONV) score and patient satisfaction score. A P value < 0.05 was considered statistically significant.
Results:
The patient in the Group A had lower resting NRS score (P < 0.05) postoperatively and less fentanyl consumption (P < 0.001) than in Group B. The difference in the sedation scores (P = 0.161) and PONV (P = 0.293) score was found to be statistically insignificant between Group A and B. The difference between the two groups was statistically significant with respect to patient satisfaction score with majority of patients having an excellent patient satisfaction score in Group A as compared to Group B.
Conclusion:
Intravenous Lidocaine as part of multimodal analgesic technique in obese patients undergoing laparoscopic bariatric surgery improves pain score and reduces opioid requirement as compared to USG-TAP Block.
Key words: Bariatric, morbid obesity, postoperative analgesia, systemic lidocaine, ultrasound-guided transversus abdominis plane
INTRODUCTION
Pain produces a physiological stress response seen as a cascade of endocrine-metabolic and inflammatory events leading to organ dysfunction, morbidity, mortality with increased hospital stay and cost.[1]
The global prevalence of obesity is increasing with the World Health Organization estimating that 11% of adults are obese worldwide.[2] Bariatric surgeries like Laparoscopic sleeve gastrectomy and Laparoscopic Roux en Y gastric bypass surgery (RYGB) offers an alternative method of maintaining long-term weight reduction and improving OSA outcomes while at the same time improving glycemic control and reducing cardiovascular and cancer risk.[3]
Traditionally opioid analgesics represent the mainstay for pain management, but their use may be associated with adverse effects like opioid-induced respiratory depression and postoperative respiratory failure in morbidly obese patients.[3] The use of multimodal strategies that minimise opioid-related side effects are highly desirable in morbidly obese patients undergoing surgical procedures.
Intravenous lidocaine has been used as a part of multimodal approach for postoperative analgesia in various surgeries including laparoscopic procedure.[4] It has analgesic, anti-inflammatory, and anti-hyperalgesic properties. This occurs by the inhibition of Na+ channels, NMDA, and G-protein-coupled receptors. The concerns for LA toxicity has been raised with continuous intravenous lidocaine infusion.
The locoregional blocks have now become the integral part of multimodal analgesia regimes. The transversus abdominis plane (TAP) block[5] is one such technique that has been reintroduced for procedures that involve the abdominal wall. The TAP block provides effective analgesia with opioid-sparing effects. Disadvantages include the absence of effectiveness for visceral pain and the effect of the block is dependent on the technique used and patient anatomy.[6]
The level of evidence comparing efficacy of intravenous lidocaine versus TAP block in bariatric surgery remains scarce in literature. We assume that both TAP block and intravenous lidocaine have comparable efficacy for postoperative analgesia after bariatric surgery. The primary objective of our study is to compare the efficacy of these two techniques in terms of postoperative NRS score in bariatric surgery patients.
METHODS
The present study was carried out after approval from the Institutional Ethics Committee (IEC/BLK/AARCE/ANAESTHESIOLOGY/JULY/2017/13, dated 12/07/2017). The study was registered with CTRI (CTRI/2017/12/010999) and was conducted during December 2017 to May 2018. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study included 56 ASA Physical Status II and III obese patients aged 18–60 years with a BMI >35 kg/m2 scheduled for laparoscopic bariatric surgery under general anaesthesia. Patients with refractory haemodynamic instability, including systolic blood pressure (BP) <90 mmHg or a mean BP <60 mmHg, HR <55 beats/min not induced by beta-blocking agents, high grade atrioventricular block and patients with liver/renal dysfunction, neurovascular patients with a history of CVA/TIA, pregnant patient or breast feeding mother and patient allergic to local anaesthetic drugs were excluded from the study. After obtaining informed written consent, patients who met the inclusion criteria were randomly allotted into two groups: Lidocaine group (Group A) and USG-TAP group (Group B) comprising of 28 patients in each. Randomisation was done using computer generated sequence of random numbers in a 1:1 ratio. Allocation concealment was done using sequentially numbered opaque sealed envelopes (SNOSE technique). The study undertaken was a prospective, randomised, comparative study.
Routine preoperative preparation included fasting for 6 h prior to surgery and patients were premedicated with intravenous metoclopramide 10 mg, intravenous ranitidine 50 mg, and intravenous glycopyrrolate 0.2 mg preoperatively in the preoperative holding area.
All the medications in the study protocol was given on dosing body weight[7] (DBW = IBW + 0.25x [ACTUAL BODY WEIGHT - IBW]
IBW = Ideal Body Weight (kg) = height (cm) – X
Where X = 100 in males and 105 in females
On arrival in the operation room, standard monitoring equipments were attached and intravenous access secured. Baseline vital signs were recorded using multiparameter monitor (Datex Ohmeda FCU-8 monitor), which included ECG (lead II and V5), oxygen saturation (SpO2), noninvasive blood pressure (NIBP), end-tidal carbon dioxide (EtCO2), gas monitoring of desflurane (Et desflurane %), and temperature using nasopharyngeal probe. Induction was started with administration of intravenous fentanyl (1 μg/kg), intravenous propofol (1–2 mg/kg), and tracheal intubation was facilitated with intravenous succinylcholine (1.5 mg/kg). Neuromuscular blockade was continued with initial bolus of intravenous cisatracurium (0.1 mg/kg) and maintenance with intravenous cisatracurium (0.05 mg/kg) every 20–40 min. Anaesthesia was maintained with O2 and N2O in a 50:50 ratio and desflurane at a flow rate of 2 L/min to achieve minimum alveolar concentration values between 0.8 and 1.0. Around 90 s before the estimated time of tracheal intubation, Group A patients were given intravenous lidocaine (1.5 mg/kg) bolus over 10 min followed by 1.5 mg/kg/h infusion. The infusion was discontinued at the time of removal of laparoscopic ports at the end of surgery. Group B patients were given ultrasound-guided bilateral transversus abdominis plane block by subcostal approach using 20 cc of 0.375% ropivacaine on each side using sonosite S nerve machine (Soma Technology Inc. Bloomfield CT06002 USA), with linear array probe HFL-38 (13-6 MHz) just after induction of anaesthesia.
Intraoperatively, the patients with increase in blood pressure or heart rate beyond 20% from the baseline value were given intravenous fentanyl 0.5 μg/kg. All patients received intravenous paracetamol 1 g over 10 min and intravenous ondansetron 4 mg approximately 30 min before anticipated extubation time and normothermia was maintained during surgery. Patients were extubated alert, warm, awake, and comfortable after adequate reversal of neuromuscular block by intravenous neostigmine 0.05 mg/kg and intravenous glycopyrrolate 0.01 mg/kg. Time to recovery was noted from removal of laparoscopic ports till time to extubation.
The following parameters were recorded postoperatively at 1st, 2nd, 4th, 8th, and 24th h by the acute pain service team at the hospital which includes resting NRS pain score, blood pressure, heart rate, respiratory rate, Spo2, postoperative nausea vomiting (PONV) scores, and sedation scores.[6] The NRS scale: 11-point numeric scale ranges from “0” representing one pain extreme (e.g., “no pain”) to “10” representing the other pain extreme (e.g., “pain as bad as you can imagine” or “worst pain imaginable”) [0: no pain, 1–4: mild pain, 5–6: moderate pain, and 7–10: severe pain]. Patient controlled analgesia [CADD Legacy infusion model 6400 by Smiths Medical] pump was attached in PACU. Fentanyl 20 μg with a lockout interval of 15 min (max dose 60 μg in 1 h). Time required for first rescue analgesia and total intraoperative and postoperative fentanyl requirement was compared between both the groups and at the end of 24 h, patients were asked to rank the quality of pain relief on a four-point pain satisfaction scale, in both the groups, viz., 1 is excellent, 2 is very good, 3 is satisfactory, and 4 is poor. Side effects like confusion, dizziness, headache, hypotension, bradycardia, hypertension, dysrhythmias, and Local site: swelling and redness of skin at the site of injection were noted.
Researchers have reported the VAS at 6 h in the Lidocaine group as 5 ± 7.42[8] and TAP group as 1 ± 1.48.[6] Based on these previous studies, the minimum required sample size at 5% level of significance and 80% power is obtained as at least 28 patients in each group. The tests used are unpaired t-test, Mann–Whitney test, Paired t-test, Wilcoxon test, Chi-square test, Fisher's exact test. The quantitative variables in both groups was expressed as mean ± SD and compared using unpaired t-test between groups and paired t-test within each group at various follow-ups. Pain scores in both groups were expressed as median and IQR and compared between groups using Mann–Whitney test, while within groups across follow-ups comparison was done using Wilcoxon test. The qualitative variables were expressed as frequencies/percentages and compared using Chi-square test. A P value < 0.05 were considered statistically significant. Statistical Package for Social sciences (SPSS) version 16.0 was used for statistical analysis.
RESULTS
The demographic profile and the duration of surgery in the two groups was comparable [Table 1]. Figure 1 shows the consort flow diagram of the patient selection and dropouts. The difference between the type of bariatric surgery performed (Laparoscopic RYGB or Laparoscopic Sleeve Gastrectomy) in both the groups was found to be statistically insignificant (P = 0.091) and the laparoscopic port site insertion was similar in both the groups.
Table 1.
Demographic profile and mean duration of surgery compared in both the groups
| Mean±SD | P | ||
|---|---|---|---|
| LIDOCAINE | TAP | ||
| Age (years) | 40.89±12.73 | 42.82±11.2 | 0.275 |
| Weight (kg) | 121.48±26.53 | 115.01±17.64 | 0.144 |
| Height (cms) | 161.61±9.2 | 159.11±8.88 | 0.155 |
| BMI (kg/m2) | 46.48±9.34 | 45.05±5.67 | 0.245 |
| Mean duration of surgery (mins) | 142.50±38.96 | 148.39±44.66 | 0.300 |
Figure 1.
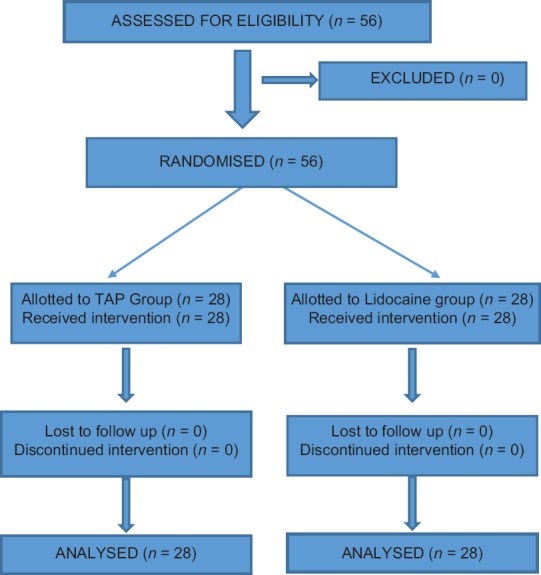
CONSORT flow diagram
The patient in the lidocaine group had lower resting NRS score measured at 1 h, 2 h, 4 h, and 8 h (P < 0.05) postoperatively than in TAP group [Table 2]. The average fentanyl used intraoperatively in lidocaine group was lower as compared to TAP group (P < 0.001). The mean time required for the first dose of rescue analgesia post-extubation was more in lidocaine group than in TAP Group (P < 0.001). The total 24 h requirement of fentanyl was lower in Lidocaine group than TAP group. The difference was found to be highly statistically significant at 1 h, 2 h, 4 h, 8 h, and 24 h postoperatively (P < 0.001) [Tables 3 and 4].
Table 2.
NRS score comparison at various time points
| NRS Score | Median/IQR (Range) | P | |
|---|---|---|---|
| LIDOCAINE | TAP | ||
| 1 h | 2.00/1.00 (1, 6) | 2.00/1.00 (1, 9) | 0.002 |
| 2 h | 2.00/1.00 (1, 6) | 2.00 1.00 (1, 6) | 0.001 |
| 4 h | 1.00/1.00 (1, 3) | 2.00/1.25 (1, 6) | 0.003 |
| 8 h | 1.00/1.00 (1, 3) | 2.00/1.00 (1, 4) | 0.065 |
| 24 h | 1.00/0.25 (1, 2) | 1.00/1.00 (1, 3) | 0.205 |
Table 3.
Comparison of Fentanyl consumption at various time points
| Fentanyl Dose (µg) | Mean±SD | P (Lidocaine vs Tap) | |
|---|---|---|---|
| Lidocaine | TAP | ||
| 1 h | 30.71±25.81 | 56.43±10.96 | <0.001 |
| 2 h | 76.43±31.29 | 115.71±67.74 | <0.001 |
| 4 h | 145.71±67.74 | 212.86±42.59 | <0.001 |
| 8 h | 197.14±109.37 | 325.71±126.45 | <0.001 |
| 24 h | 214.29±130.85 | 388.93±190.46 | <0.001 |
Table 4.
Comparison Of Time To Post-Extubation Rescue Analgesia (RA)/Intraoperative Fentanyl Used/Postoperative Fentany Used 24 H (µg)
| Mean±SD | P | ||
|---|---|---|---|
| Lidocaine | TAP | ||
| Time to rescue analgesia post Extubation (min) | 35.89±33.83 | 4.11±11.87 | <0.001 |
| Intraoprative fentanyl used (µg) | 141.79±29.32 | 187.86±36.95 | <0.001 |
| Total fentanyl post op in 24 h (µg) | 218.93±138.04 | 138.04±198.28 | <0.001 |
The difference in the PONV score was found to be statistically insignificant (P = 0.293) between the Lidocaine and TAP block group. The difference in the sedation scores was statistically insignificant for the two groups (P = 0.161). We found that the difference between the two groups was found to be statistically significant with respect to patient satisfaction score. The majority of patients (n = 24) had an excellent patient satisfaction score in Lidocaine group compared to 11 patients in TAP group [Table 5]. We did not observe any side effects attributable to either of the two techniques.
Table 5.
Comparison of patient pain satisfaction score
| Patient Pain Satisfaction Score | Lidocaine | TAP | P | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Excellent | 24 | 85.71% | 11 | 39.29% | <0.001 |
| Very Good | 0 | 0.00% | 5 | 17.86% | 0.010 |
| Satisfactory | 4 | 14.29% | 9 | 32.14% | 0.057 |
| Poor | 0 | 0.00% | 3 | 10.71% | 0.038 |
| TOTAL | 28 | 100% | 28 | 100% | |
DISCUSSION
With increasing use of USG in current anaesthesia practice, TAP block has made its resurgence as a part of MMA. There are studies reporting benefits of intravenous lidocaine infusion in bariatric surgery in terms of reduced opioid use perioperatively, early ambulation, early return of bowel function, and overall better patient satisfaction. But we could not find any study to decide which of the two techniques is better. This study was formulated to have an objective assessment and analysis to find out the best suitable technique in these subset of patients.
Despite the comparable duration of surgery, the lidocaine group required significantly less fentanyl intraoperatively as compared to the TAP group. We found that the TAP block group patients had lower resting mean NRS scores (NRS < 4) at 1, 2, 4, 8, and 24 h. The postoperative NRS score (at 1, 2, 4, and 8 h) and the total 24 h requirement of fentanyl was lower in Lidocaine group than in TAP group. These results were in agreement with the results of Sinha et al.[6] and Wassef M, et al.[9] who reported lower resting postoperative median VAS pain score of the TAP block compared to control group. De Oliveira GS et al.[7] and Emily N et al.[8] also reported lower pain score in lidocaine group than control group in their study. Sinha A et al.[6] also found decreased requirement of opioid in TAP group than in control group in their study and Wassef M et al.[9] reported no significant difference between the TAP and control group in terms of opioid consumption. De Oliveira GS et al.[7] and Emily N et al.[8] reported lower opioid requirements in lidocaine group than control group in their study. In our study, there was no difference in sedation score between both the groups. None of our patients had sedation score more than 2, this could be due to the fact that the narcotic consumption was less in our study as we administered PCA regulated drug. Sinha A et al.[6] in their comparative study found higher sedation score in control group than in TAP group. This was likely due to the higher opioid consumption in the control group patients. There was no difference in the PONV score between both groups in our study. We found higher level of patient satisfaction in Lidocaine group than TAP group in our study. Sinha et al.[6] assessed patient satisfaction scores at the end of first postoperative day which was significantly more in the TAP group compared to control group.
Our study has some limitations. First, the TAP block is technically difficult in morbidly obese patients due to excessive subcutaneous fat and increased depth of transversus abdominis plane. In the supine position, the subcutaneous fat hangs over the flank and leads to difficulty in probe handling and poor visualisation of the needle during the procedure. Needle-beam angle is one of the most important factors influencing the visualisation of the needle during the in-plane approach of an USG procedure [Figures 2 and 3][10] It is difficult to attain a desired (>55 degrees) needle-beam angle with the increasing depth of the target during USG procedures. Sinha A et al.[6] also reported in their study that in obese patients there is an increase in the number of reflective interfaces not only leading to more echoes but also decreasing the incident sound available to penetrate deeper tissues, such as nerves, vessels, or other targeted structures. They used the modified technique in which the visibility of the muscle layers could be improved by the 15° tilt away from the side in which block had to be performed and an assistant pulled the abdomen toward opposite side. We experienced difficulty in giving TAP block due to aforementioned reasons and in 8 of our patients in TAP group we needed the help of an assistant to pull the abdomen toward opposite side so that the handling of the ultrasound probe is easier and needle visualisation is improved due to better needle-to-probe alignment. On the contrary, giving lidocaine infusion requires only an infusion pump and no technical expertise to handle equipment like USG machine. Second limitation is that because of the different type of procedure involved (USG TAP and Lidocaine infusion), patient could not be blinded to group allocation. Third, the effects of lidocaine was not monitored on the second postoperative day in our study and according to previous literature it has been noted that most of the beneficial effects of lidocaine on the sympathoadrenal response occurred on the second postoperative day, that is, after the lidocaine infusion was stopped.
Figure 2.
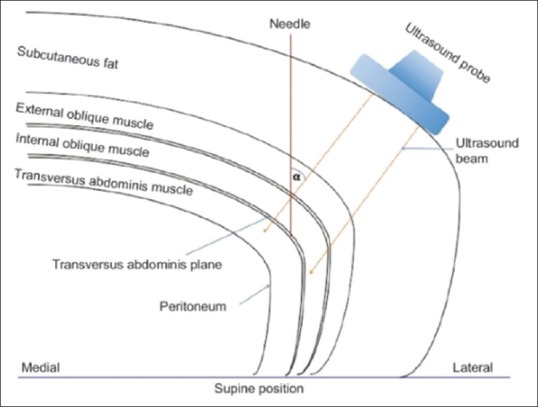
Line diagram depicting the ultrasound-guided transversus abdominis plane block in the supine position in obese patients. α;=needle-beam angle. The needle-beam angle in the supine position is acute and, therefore, needle visualisation is difficult. Also, the handling of the probe is difficult in view of the overhanging subcutaneous fat tissue in the flank region[10]
Figure 3.
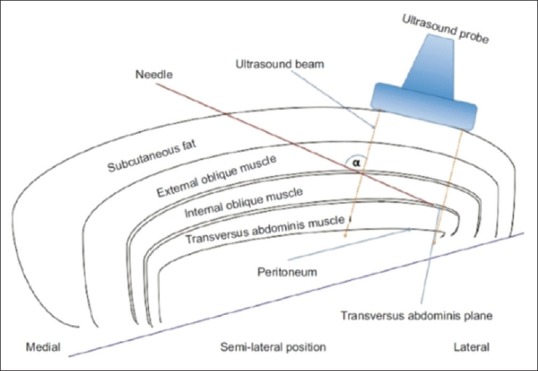
Line diagram depicting the ultrasound-guided transversus abdominis plane block in the semilateral position in obese patients. α;=needle-beam angle. The subcutaneous fat is pushed medially and, hence, probe handling is easier. In the semilateral position, we are able to achieve better alignment between needle and ultrasound probe and the needle-beam angle is obtuse. Hence, we have better needle visualisation in the semilateral position[10]
In our study we also aimed to observe for any side effects associated with use of either technique. During the course of our study, we did not observe any untoward event attributable to either of the two techniques. Based on the findings of our study, we suggest that both TAP block and intravenous lidocaine infusion are safe and effective techniques to reduce perioperative narcotic use. However, intravenous lidocaine infusion provide better NRS score and patient satisfaction score with reduced opioid consumption postoperatively as compared to TAP block in bariatric surgical patients.
CONCLUSION
Intravenous Lidocaine is a more efficacious component of multimodal analgesia as compared to USG-guided TAP block for postoperative analgesia in obese patients undergoing laparoscopic bariatric surgery.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
This article does not contain any procedure with animals performed by any of the authors.
Declaration of patient consent
Informed consent was obtained from all individual participants included in the study.
The study was registered with CTRI (CTRI/2017/12/010999). http://ctri.nic.in/Clinicaltrials/login.php.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Alvarez A, Singh PM, Sinha AC. Postoperative analgesia in morbid obesity. Obes Surg. 2014;24:652–9. doi: 10.1007/s11695-014-1185-2. [DOI] [PubMed] [Google Scholar]
- 2.World_Health_Organization. Obesity and overweight, WHO Factsheet N°311. [Last cited on 2014 Nov 05]. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/
- 3.P Mandal, Murshed Anaesthetic management for laparoscopic gastric bypass procedure in morbid obesity. Indian J Anaesth. 2008;52:412. [Google Scholar]
- 4.McCarthy GC, Megalla SA, Habib AS. Impact of intravenous lidocaine infusion on postoperative analgesia and recovery from surgery a systematic review of randomized controlled trials. Drugs. 2010;70:1149–63. doi: 10.2165/10898560-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 5.McDonnell JG, Laffey JG. Transversus abdominis plane block. Anesth Analg. 2007;105:883. doi: 10.1213/01.ane.0000268542.45107.79. [DOI] [PubMed] [Google Scholar]
- 6.Sinha A, Jayaraman L, Punhani D. Efficacy of ultrasound-guided transversus abdominis plane block after laparoscopic bariatric surgery: A double blind, randomized, controlled study. Obes Surg. 2013;23:548–53. doi: 10.1007/s11695-012-0819-5. [DOI] [PubMed] [Google Scholar]
- 7.De Oliveira GS, Duncan K, Fitzgerald P, Nader A, Gould RW, McCarthy RJ. Systemic lidocaine to improve quality of recovery after laparoscopic bariatric surgery: A randomized double-blinded placebo-controlled trial. Obes Surg. 2014;24:212–8. doi: 10.1007/s11695-013-1077-x. [DOI] [PubMed] [Google Scholar]
- 8.Alvey EN, Ching YH, Karlnoski RA, Dalvi PH. Systemic intraoperative lidocaine infusion for postoperative pain management in obese patients: A randomized, placebo controlled pilot study. Case Studies in Surgery. 2016;2:10–16. [Google Scholar]
- 9.Wassef M, Lee DY, Levine JL, Ross RE, Guend H, Vandepitte C, et al. Feasibility and analgesic efficacy of the transversus abdominis plane block after single-port laparoscopy in patients having bariatric surgery. J Pain Res. 2013;6:837–41. doi: 10.2147/JPR.S50561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Toshniwal G, Soskin V. Ultrasound-guided transversus abdominis plane block in obese patients. Indian J Anaesth. 2012;56:104–5. doi: 10.4103/0019-5049.93368. [DOI] [PMC free article] [PubMed] [Google Scholar]


