Abstract
Background
Although arteriovenous fistula (AVF) is the preferred vascular access for hemodialysis (HD), the association between vascular access types and quality of life is not well-known. We investigated the relationships between HD vascular access types and all-cause mortality, health-related quality of life (HRQOL) and the degree of depression in a large prospective cohort.
Methods
A total of 1461 patients who newly initiated HD were included. The initial vascular access types were classified into AVF, arteriovenous graft (AVG), and central venous catheter (CVC). The primary outcomes were all-cause mortality and HRQOL and depression. The secondary outcome was all-cause hospitalization. Kidney Disease Quality of Life Short Form 36 (KDQOL-36) and Beck’s depression inventory (BDI) scores were measured to assess HRQOL and depression.
Results
Among 1461 patients, we identified 314 patients who started HD via AVF, 76 via AVG, and 1071 via CVC. In the survival analysis, patients with AVF showed significantly better survival compared with patients with other accesses (p < .001). The AVF and AVG group had higher KDQOL-36 score and lower BDI score than CVC group at 3 months and 12 months after the initiation of HD. The frequency of hospitalization was higher in patients with AVG compared to those with AVF (AVF 0.7 vs. AVG 1.1 times per year) (p = .024).
Conclusions
The patients with AVF had better survival rate and low hospitalization rate, and the patients with AVF or AVG showed both higher HRQOL and lower depression scores than those with CVC.
Keywords: Hemodialysis, vascular access, central venous catheter, mortality, quality of life, depression
Introduction
The types of vascular access were associated with survival of patients with end-stage renal disease (ESRD) undergoing hemodialysis (HD) [1–3]. Among the arteriovenous fistula (AVF), arteriovenous graft (AVG), and central venous catheter (CVC), AVF is the most preferred and recommended vascular access type because of its lower mortality and hospitalization rate. The use of CVC was associated with greater risk of infection which ultimately resulted in higher mortality [4,5]. Despite of this cumulative evidence, over half of incident HD patients inevitably start dialysis via CVC [6,7]. Therefore, we have to continue efforts to prepare permanent vascular access preemptively in impending ESRD patients. In addition, it is necessary to monitor vigilantly the characteristics of patients undergoing HD via CVC and find modifiable factors to be mended.
Besides mortality, another important aspect in choice for vascular access is the quality of life of HD patients. The health-related quality of life (HRQOL) and depression index, Beck’s depression inventory (BDI) are known to be worse in patients with ESRD, and these are probably related to the survival of ESRD patients [8,9]. The type of vascular access seems to be one of the modifiable factors for HRQOL and depression in dialysis population. However, the effects of vascular access type on HRQOL or depression in these patients have not yet been investigated thoroughly. Up to now, only a few studies dealt with the relationship between HRQOL and type of vascular access, and furthermore, the results of studies are not conclusive [10–12]. Furthermore, regarding BDI, there is only one study that showed no relationship between degree of depression and the type of vascular access [10]. These studies even had several limitations in the context of included number of patients and nature of studies. Therefore, a large-scale prospective study is required to determine the relationships between the type of vascular access and HRQOL and depression in dialysis patients.
In this study, we elucidated the characteristics, HRQOL and BDI scores and survival rate according to the initial vascular access type in incident HD patients in a large prospective Korean cohort. Also, the changes in quality of life following 3 months and 12 months after initiation of dialysis were monitored.
Methods
Study design and population
This study is a part of prospective cohort study of the Clinical Research Center for End Stage Renal Disease (CRC for ESRD) in Korea. It is a nationwide web-based multi-center prospective cohort study of patients with ESRD, designed to improve survival rate and quality of life and to create effective treatment guidelines (clinicaltrial.gov; NCT00931970). Thirty-one hospitals and clinics in Korea participated, and patients aged 18 years or more with ESRD were enrolled. All patients provided their written consent to participate in this study, which was approved by the institutional review board at each participating center. All clinical investigations were conducted in accordance with the guidelines of the 2008 Declaration of Helsinki.
Over a 7-year period (August 2008 through July 2015), a total of 2154 incident dialysis patients were enrolled in CRC for ESRD. After excluding patients under peritoneal dialysis (N = 618) or patients without the information of initial vascular access (N = 75), 1461 patients were analyzed in this study.
Measurements
The types of initial vascular access for HD were classified into AVF, AVG, and CVC. The CVCs were additionally classified as non-tunneled CVC (NTCVC) and tunneled CVC (TCVC). The type of vascular access which was monitored at 3 months or 12 months after HD was considered as a permanent vascular access for each patient.
The following demographic and clinical data were collected and analyzed; sex, time to referral to nephrology, cause of ESRD, body mass index (BMI), systolic and diastolic blood pressure, comorbidities including coronary artery disease (CAD), peripheral vascular disease (PVD), cerebrovascular disease (CVD), congestive heart failure (CHF) and malignancy, and laboratory values including hemoglobin, serum calcium, phosphorus, uric acid, and total cholesterol. In addition, the modified Charlson comorbidity index (MCCI) was calculated for each patient. The MCCI was developed to predict one-year mortality, and it has been validated in ESRD patients [13,14]. Patients were classified as early referral if their first encounter with a nephrologist occurred more than 1 year before initiation of dialysis and received education about dialysis, and all others were classified as late referral, as described previously [15].
Outcomes
The primary outcomes were all-cause mortality and HRQOL and degree of depression. The secondary outcome was all-cause hospitalization. Kidney Disease Quality of Life Short Form 36 (KDQOL-36) has been used to evaluate the HRQOL of patients with ESRD [16]. We utilized the Korean version of the KDQOL-36, which was recently translated and validated in Korean patients with ESRD [17]. Briefly, this includes 12 items that provide a generic chronic disease core as well as 24 additional kidney disease-targeted items. The 24 additional items focus on particular health-related concerns of individuals with kidney disease (symptom/problem list, 12 items; effects of kidney disease, eight items; burden of disease, four items). The item scores were aggregated without weighting and transformed linearly to a 0–100 possible range, with higher scores indicating better states, which resulted in a total of dimensions. The Korean version of BDI was used to evaluate depression in our patients. The BDI has been validated in various groups of patients and has been used in patients undergoing dialysis to evaluate depression [18]. It consists of 21 self-reported items, and each item is rated on a scale of 0–3, producing a possible score range of 0–63 [19].
Each center recorded information regarding mortality and cause of death on the CRC for ESRD web-based registry. All the medical records of patients who died in hospital registered in CRC for ESRD were checked to confirm the death and mortality date. In case of patient died in other hospitals, information of death was extracted from the Korean National Statistical Office data as of 31 December 2017. Hospitalization was defined as admission for at least 24 h, excluding diagnostic work-ups for transplantation.
Statistical analyses
Analyses of the differences in baseline characteristics according to the types of vascular access were performed using the t test or one-way ANOVA for continuous variables and the χ2 test for categorical variables. Additionally, in order to compare the quality of life and depression among three groups, univariable and multivariable linear regressions with adjustments for age, sex, type of referral, MCCI and hemoglobin levels as covariates which were selected according to the results of analyses of baseline characteristics were performed. The Kaplan–Meier method was used to compare survival curves, and differences were assessed by means of the log rank test. Statistical analysis was performed using SPSS version 21.0 (SPSS Inc., Chicago, IL). For all analyses, results were considered statistically significant if p < .05.
Results
Patients’ characteristics according to the type of initial vascular access
CVC was the most common vascular access type and 1071 patients (73.3%) started HD with CVC. AVF and AVG were 21.5% and 5.2%, respectively (Table 1). The age was older in AVG group (61.7 ± 12.5; mean ± SD) compared with AVF (57.3 ± 12.7) and CVC (58.3 ± 14.7) groups. The portion of early referral to nephrologist was higher in the order of AVF, AVG, and CVC. Regarding underlying causes of ESRD, diabetes mellitus (DM) accounted for 69.7% of AVG group, whereas the frequencies of hypertension and glomerulonephritis were relatively higher in AVF and CVC groups. The score of MCCI was significantly higher in patients with AVG which indicate more severe comorbidities than those of patients with AVF and CVC. Especially, prevalence of DM, CVD, PVD and malignancy were significantly higher in AVG group. In laboratory tests, hemoglobin and serum calcium were lower and serum phosphorus was higher in CVC group.
Table 1.
Baseline characteristics according to the types of initial vascular access.
| AVF n= 314 (21.5%) Mean ± SD or n (%) |
AVG n= 76 (5.2%) Mean ± SD or n (%) |
CVC n= 1,071 (73.3%) Mean ± SD or n (%) |
p | |
|---|---|---|---|---|
| Age (years) | 57.3 ± 12.7 | 61.7 ± 12.5 | 58.3 ± 14.7 | .051 |
| Sex, male | 207 (66.1%) | 43 (56.6%) | 652 (60.9%) | .153 |
| Time referral (months) | 58.2 ± 123.5 | 38.0 ± 47.3 | 40.4 ± 86.5 | .015 |
| Type of referral | ||||
| Early referral | 214 (72.3%) | 48 (66.7%) | 572 (56.6%) | <.001 |
| Late referral | 82 (27.7%) | 24 (33.3%) | 439 (43.4%) | |
| Cause of ESRD | ||||
| DM | 184 (58.8%) | 53 (69.7%) | 643 (60.0%) | .003 |
| Hypertension | 47 (15.0%) | 8 (10.5%) | 144 (13.4%) | |
| Glomerulonephritis | 44 (14.1%) | 6 (7.9%) | 131 (12.2%) | |
| Others | 36 (11.5%) | 5 (6.6%) | 145 (13.5%) | |
| Unknown | 24 (0.6%) | 4 (5.3%) | 8 (0.7%) | |
| Score of MCCI | 5.4 ± 2.1 | 6.6 ± 2.6 | 5.3 ± 2.3 | <.001 |
| Comorbidity | ||||
| DM | 198 (63.5%) | 61 (80.3%) | 693 (64.8%) | .018 |
| CAD | 48 (15.5%) | 11 (14.5%) | 132 (12.4%) | .342 |
| CHF | 31 (10.0%) | 12 (15.8%) | 113 (10.6%) | .331 |
| CVD | 23 (7.5%) | 15 (19.7%) | 102 (9.6%) | .005 |
| PVD | 34 (11.0%) | 17 (22.4%) | 63 (5.9%) | <.001 |
| Malignancy | 24 (7.8%) | 16 (21.1%) | 67 (6.3%) | <.001 |
| SBP (mmHg) | 142.5 ± 21.2 | 137.7 ± 20.6 | 145.7 ± 23.9 | .003 |
| DBP (mmHg) | 77.9 ± 13.3 | 72.7 ± 12.5 | 78.3 ± 14.6 | .006 |
| BMI (kg/m2) | 23.5 ± 3.7 | 23.1 ± 3.4 | 23.2 ± 3.5 | .334 |
| Hemoglobin (g/dL) | 9.1 ± 1.5 | 9.0 ± 1.4 | 8.7 ± 1.6 | <.001 |
| Calcium (mg/dL) | 7.9 ± 1.0 | 8.0 ± 0.9 | 7.7 ± 1.1 | .001 |
| Phosphorus (mg/dL) | 5.4 ± 1.7 | 4.8 ± 1.6 | 5.6 ± 2.1 | .001 |
| Uric acid (mg/dL) | 7.9 ± 2.3 | 7.6 ± 2.5 | 8.1 ± 2.7 | .107 |
| Total cholesterol (mg/dL) | 154.0 ± 45.4 | 137.1 ± 38.4 | 157.0 ± 50.1 | .004 |
| hs-CRP at 0 m | 2.4 ± 12.1 | 6.2 ± 30.1 | 5.4 ± 18.3 | .028 |
AVF: arteriovenous fistula; SD: standard deviation; AVG: arteriovenous graft; CVC: central venous catheter; ESRD: end stage renal disease; DM: diabetes mellitus; MCCI: modified Charlson comorbidity index; CAD: coronary artery disease; CHF: congestive heart failure; CVD: cerebrovascular disease; PVD: peripheral vascular disease; SBP: systolic blood pressure; DBP: diastolic blood pressure; BMI: body mass index; hs-CRP: highly sensitive C-reactive protein.
The comparisons between TCVC and NTCVC groups are depicted in Table 2. The age was younger in patients with NTCVC compared to patients with TCVC. The referral timing was similar between two groups. The score of MCCI was also similar, but prevalence of CAD, CHF, and CVD was significantly higher in NTCVC group. Laboratory tests showed lower level of hemoglobin and calcium, and higher level of phosphorus and uric acid in patients with NTCVC.
Table 2.
Comparisons of baseline characteristics between TCVC and NTCVC.
| TCVC n= 896 (83.7%) Mean ± SD or n (%) |
NTCVC n= 175 (16.3%) Mean ± SD or n (%) |
p | |
|---|---|---|---|
| Age (years) | 58.7 ± 14.7 | 56.3 ± 15.0 | .042 |
| Sex, male | 536 (59.8%) | 116 (66.3%) | .109 |
| Time referral (months) | 41.8 ± 93.2 | 33.4 ± 39.0 | .244 |
| Type of referral | |||
| Early referral | 472 (56.2%) | 100 (58.5%) | .582 |
| Late referral | 368 (43.8%) | 71 (41.5%) | |
| Cause of ESRD | |||
| DM | 534 (59.6%) | 109 (62.3%) | .005 |
| Hypertension | 122 (13.6%) | 22 (12.6%) | |
| Glomerulonephritis | 99 (11.0%) | 32 (18.3%) | |
| Others | 134 (15.0%) | 11 (6.3%) | |
| Unknown | 7 (0.8%) | 1 (0.6%) | |
| Score of MCCI | 5.3 ± 2.3 | 5.5 ± 2.4 | .312 |
| Comorbidity | |||
| DM | 580 (64.9%) | 113 (64.6%) | .938 |
| CAD | 102 (11.5%) | 30 (17.2%) | .035 |
| CHF | 68 (7.6%) | 45 (25.9%) | <.001 |
| CVD | 76 (8.5%) | 26 (14.9%) | .009 |
| PVD | 49 (5.5%) | 14 (8.0%) | .194 |
| Malignancy | 56 (6.3%) | 11 (6.3%) | .991 |
| SBP (mmHg) | 146.1 ± 23.7 | 143.6 ± 24.7 | .214 |
| DBP (mmHg) | 78.5 ± 14.8 | 76.9 ± 14.0 | .194 |
| BMI (kg/m2) | 23.2 ± 3.6 | 23.1 ± 3.4 | .952 |
| Hemoglobin (g/dL) | 8.8 ± 1.6 | 8.0 ± 1.6 | <.001 |
| Calcium (mmHg) | 7.7 ± 1.0 | 7.4 ± 1.2 | .001 |
| Phosphorus (mmHg) | 5.5 ± 2.0 | 6.4 ± 2.2 | <.001 |
| Uric acid (mmHg) | 8.1 ± 2.8 | 8.6 ± 2.6 | .010 |
| Total cholesterol (mmHg) | 157.2 ± 50.7 | 156.1 ± 46.7 | .801 |
| hs-CRP at 0 m | 5.6 ± 08.8 | 4.3 ± 15.5 | .383 |
| hs-CRP at 3 m | 2.7 ± 12.9 | 1.5 ± 5.9 | .056 |
TCVC: tunneled central venous catheter; SD: standard deviation; NTCVC: non-tunneled central venous catheter; ESRD: end stage renal disease; DM: diabetes mellitus; MCCI: modified Charlson comorbidity index; CAD: coronary artery disease; CHF: congestive heart failure; CVD: cerebrovascular disease; PVD: peripheral vascular disease; SBP: systolic blood pressure; DBP: diastolic blood pressure; BMI: body mass index; hs-CRP: highly sensitive C-reactive protein.
Patients’ characteristics according to the types of permanent vascular access
The types of permanent vascular accesses were traced in a total of 1113 patients (Table 3). There were 914 (82.1%) patients with AVF and 199 (17.9%) with AVG. Among the 1071 patients who started HD via CVC, 721 patients changed to AVF and 155 patients changed to AVG within following one year. The rest of patients were either still on the CVC or lost to follow-up or died. Those in AVF group were more likely to be younger and have lower MCCI score which indicate fewer comorbid conditions compared with AVG group. Especially, the prevalence of DM was prominently higher in AVG group compared to AVF group. The prevalence of macrovascular diseases including CVD and PVD were also higher in AVG group.
Table 3.
Baseline characteristics according to types of permanent vascular access.
| AVF n= 914 (82.1%) Mean ± SD or n (%) |
AVG n= 199 (17.9%) Mean ± SD or n (%) |
p | |
|---|---|---|---|
| Age (years) | 56.8 ± 13.5 | 61.7 ± 12.5 | <.001 |
| Sex, male | 455 (64.7%) | 87 (56.9%) | .068 |
| Time referral (months) | 48.7 ± 91.8 | 35.6 ± 45.6 | .097 |
| Type of referral | |||
| Early referral | 430 (64.7%) | 84 (59.2%) | .215 |
| Late referral | 235 (35.3%) | 58 (40.8%) | |
| Cause of ESRD | |||
| DM | 421 (59.9%) | 109 (71.2%) | .075 |
| Hypertension | 91 (12.9%) | 15 (9.8%) | |
| Glomerulonephritis | 108 (15.4%) | 15 (9.8%) | |
| Others | 75 (10.7%) | 11 (7.2%) | |
| Unknown | 8 (1.1%) | 3 (2.0%) | |
| Score of MCCI | 5.2 ± 2.2 | 6.3 ± 2.4 | <.001 |
| Comorbidity | |||
| DM | 458 (65.3%) | 118 (77.1%) | .005 |
| CAD | 90 (12.9%) | 23 (15.0%) | .492 |
| CHF | 71 (10.2%) | 23 (15.0%) | .086 |
| CVD | 57 (8.2%) | 22 (14.4%) | .018 |
| PVD | 55 (7.9%) | 20 (13.1%) | .041 |
| Malignancy | 50 (7.2%) | 18 (11.8%) | .059 |
| SBP (mmHg) | 144.4 ± 22.9 | 144.0 ± 21.3 | .839 |
| DBP (mmHg) | 78.2 ± 14.2 | 73.5 ± 12.8 | <.001 |
| BMI (kg/m2) | 23.3 ± 3.6 | 23.2 ± 3.6 | .714 |
| Hemoglobin (g/dL) | 8.8 ± 1.7 | 8.9 ± 1.5 | .704 |
| Calcium (mg/dL) | 7.7 ± 1.1 | 7.8 ± 0.91 | .343 |
| Phosphorus (mg/dL) | 5.7 ± 2.0 | 5.4 ± 1.8 | .129 |
| Uric acid (mg/dL) | 8.2 ± 2.5 | 7.9 ± 2.5 | .195 |
| Total cholesterol (mg/dL) | 156.0 ± 47.9 | 155.4 ± 53.4 | .896 |
| hs-CRP 0 m | 2.7 ± 11.8 | 3.9 ± 20.1 | .331 |
AVF: arteriovenous fistula; SD: standard deviation; AVG: arteriovenous graft; ESRD: end stage renal disease; DM: diabetes mellitus; MCCI: modified Charlson comorbidity index; CAD: coronary artery disease; CHF: congestive heart failure; CVD: cerebrovascular disease; PVD: peripheral vascular disease; SBP: systolic blood pressure; DBP: diastolic blood pressure; BMI: body mass index; hs-CRP: highly sensitive C-reactive protein.
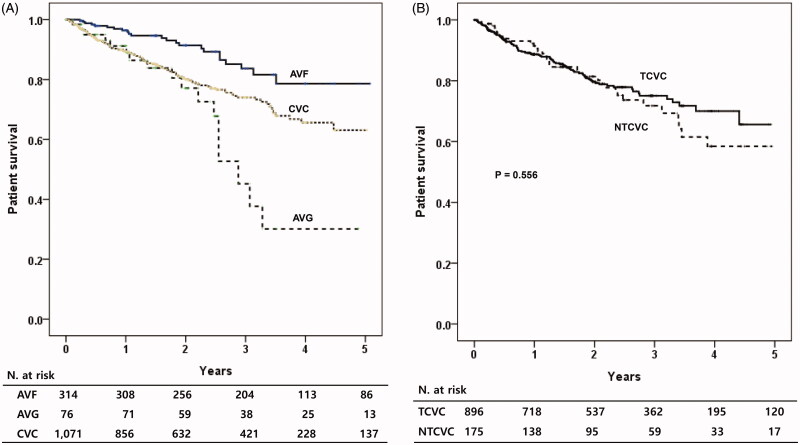
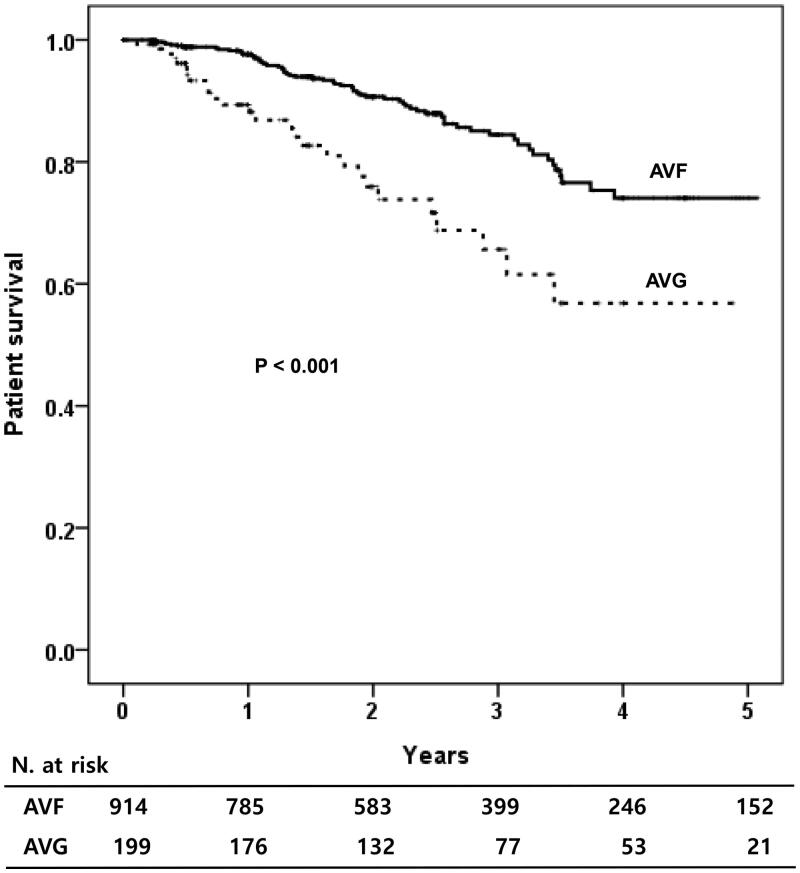
Patients’ survival according to the type of initial and permanent vascular access
During 1.9 years of mean follow-up period, 182 patients (12.5%) were died. When the patients’ survival was compared according to the types of initial vascular access, patients with AVF showed significantly better survival compared to those with other vascular accesses (p < .001) (Figure 1(A)). AVG group showed the worst patients’ survival among the three types of vascular accesses. When the TCVC and NTCVC groups were compared, the patient survival was similar between the two groups (Figure 1(B)). When the patients’ survival was analyzed according to the types of permanent vascular access, the patients having permanent AVF showed significantly better survival rate compared to those with AVG (p < .001, Figure 2).
Figure 1.
Patients’ survival according to the types of initial vascular access. (A) Comparisons among the AVF, AVG and CVC patients. (B) Comparison between NTCVC and TCVC. AVF: arteriovenous fistula; AVG: arteriovenous graft; CVC: central venous catheter; NTCVC: non-tunneled CVC; TCVC: tunneled CVC.
Figure 2.
Patients’ survival according to the types of permanent vascular access. AVF: arteriovenous fistula; AVG: arteriovenous graft.
Comparisons of HRQOL and BDI scores according to the type of initial vascular access
Table 4 shows the comparisons of HRQOL and BDI scores according to the type of initial vascular access at 3 months after beginning of HD. On comparing the KDQOL-36 according to the vascular access type, the AVF group showed significantly higher scores in seven of 10 SF-36 domains and the AVG group showed higher scores in two of 10 SF-36 domains than did the CVC group. The AVF group showed higher scores in three of 12 kidney disease targeted domains and the AVG group showed higher scores in two of 12 kidney disease targeted domains than did the CVC group. Even after adjusting for confounding variables including age, sex, type of referral, MCCI and hemoglobin level, the AVF and AVG group showed higher scores in six domains (physical composite summary, mental composite summary, physical functioning, role-physical, role-emotional, and social functioning) and two domains (mental composite summary and role-emotional) in SF-36 domains, respectively. After adjusting for confounding variables, the AVF and AVG group showed higher scores in six domains (symptoms/problems, effects of kidney disease, cognitive functioning, quality of social interaction, social support, and overall health) and two domains (symptoms/problems and patient satisfaction) in kidney disease targeted domains, respectively. BDI score was also significantly lower in AVF group which indicate less depressive mood after adjusting multiple variables (p = .024).
Table 4.
Health-related quality of life (HRQOL) and Beck’s depression inventory (BDI) scores at 3 months after dialysis beginning according to the types of initial vascular access.
| AVF (n= 215) Mean ± SD |
AVG (n= 48) Mean ± SD |
CVC (n= 608) Mean ± SD |
p† | p‡ | |
|---|---|---|---|---|---|
| HRQOL measure | |||||
| SF-36 | |||||
| PCS | 42.1 ± 9.3 | 38.7 ± 8.5 | 39.6 ± 9.5 | .021* | .024* |
| MCS | 42.6 ± 9.3 | 43.9 ± 7.6 | 39.7 ± 9.9 | .002*,** | .005*,** |
| Physical functioning | 73.6 ± 22.9 | 62.7 ± 26.9 | 65.9 ± 27.4 | .010* | .008* |
| Role-physical | 49.1 ± 41.6 | 39.1 ± 41.1 | 38.1 ± 41.0 | .022* | .015* |
| Bodily pain | 71.4 ± 23.6 | 72.9 ± 23.0 | 66.2 ± 24.9 | .047* | .108 |
| General health | 37.0 ± 19.4 | 32.2 ± 18.0 | 35.5 ± 18.0 | .370 | .114 |
| Mental health | 54.9 ± 15.6 | 55.1 ± 16.4 | 52.1 ± 18.1 | .202 | .124 |
| Role-emotional | 67.1 ± 42.8 | 74.0 ± 37.6 | 49.0 ± 44.9 | <.001*,** | <.001*,** |
| Social functioning | 68.6 ± 24.1 | 64.8 ± 26.1 | 61.7 ± 25.9 | .019* | .008* |
| Vitality | 45.5 ± 18.2 | 44.7 ± 16.6 | 42.6 ± 19.9 | .292 | .100 |
| Kidney disease targeted | |||||
| Symptoms/problems | 82.4 ± 14.1 | 83.1 ± 12.6 | 78.1 ± 16.6 | .008*,** | .016*,** |
| Effects of kidney disease | 71.5 ± 16.3 | 69.6 ± 16.5 | 67.2 ± 19.5 | .057 | .018* |
| Burden of kidney disease | 33.2 ± 21.6 | 34.6 ± 18.6 | 30.7 ± 22.6 | .376 | .413 |
| Work status | 27.1 ± 35.2 | 28.1 ± 28.2 | 23.5 ± 31.9 | .429 | .622 |
| Cognitive functioning | 87.1 ± 15.1 | 84.8 ± 14.8 | 81.1 ± 20.7 | .005* | .002* |
| Quality of social interaction | 69.5 ± 19.3 | 69.2 ± 17.7 | 63.4 ± 21.1 | .005* | .004* |
| Sexual function | 76.5 ± 25.9 | 66.7 ± 33.2 | 68.5 ± 34.3 | .381 | .145 |
| Sleep | 67.8 ± 19.8 | 71.0 ± 23.3 | 68.1 ± 19.4 | .711 | .97 |
| Social support | 57.3 ± 25.8 | 59.4 ± 23.9 | 62.0 ± 24.3 | .144 | .011* |
| Dialysis staff encouragement | 85.3 ± 19.1 | 90.6 ± 13.5 | 84.3 ± 19.1 | .187 | .618 |
| Overall health | 55.6 ± 18.7 | 54.7 ± 16.1 | 51.3 ± 19.6 | .061 | .024* |
| Patient satisfaction | 68.8 ± 23.1 | 76.6 ± 20.7 | 65.9 ± 22.6 | .024** | .014** |
| Mean | 60.6 ± 17.3 | 59.8 ± 18.2 | 56.1 ± 16.9 | ||
| BDI | 13.8 ± 9.5 | 13.7 ± 8.0 | 16.6 ± 11.0 | .020* | .024* |
AVF: arteriovenous fistula; SD: standard deviation; AVG: arteriovenous graft; CVC: central venous catheter; HRQOL: health-related quality of life; SF-36: short form 36; PCS: physical composite summary; MCS: mental composite summary; BDI: Beck’s depression inventory.
Value was obtained from unadjusted regression analysis.
Value was obtained from regression analysis adjusted for age, sex, type of referral, modified Charlson comorbidity index, and hemoglobin levels.
AVF versus CVC.
AVG versus CVC.
At 1 year after beginning of HD, almost all the KDQOL-36 scores slightly increased compared to those at 3 months after dialysis beginning (Table 5), and the average score increased from 60.6 to 62.5 in AVF group, 59.8–62.4 in AVG group and 56.1–56.6 in CVC group. The AVF and AVG group had higher mean scores in each SF-36 domain than did the CVC group, and this difference was statistically significant in five domains and one domain, respectively. After adjusting for confounding variables, physical composite summary, role-physical, bodily pain, and role-emotional domain were significantly higher in AVF group. AVG group had higher score in role-emotional domain (p = .017). In adjusted analyses of kidney disease targeted domains, AVF group showed significantly higher scores in two (symptoms/problems and patient satisfaction) and the AVG group showed significantly higher scores in two (overall health and patient satisfaction) of 12 domains than did the CVC group. Mean BDI scores were 12.9 and 17.3 in AVF and CVC groups, respectively. The difference was significant before (p = .003) and after adjustment (p = .009), and this implies that patients with AVF are also less depressive at 1 year after beginning of dialysis.
Table 5.
Health-related quality of life (HRQOL) and Beck's depression inventory (BDI) scores at 12 months after dialysis beginning according to the types of initial vascular access.
| AVF (n= 186) Mean ± SD |
AVG (n= 48) Mean ± SD |
CVC (n= 394) Mean ± SD |
p† | p‡ | |
|---|---|---|---|---|---|
| HRQOL measure | |||||
| SF-36 | |||||
| PCS | 45.2 ± 9.5 | 43.9 ± 10.1 | 41.5 ± 9.2 | .006* | .008* |
| MCS | 42.8 ± 8.7 | 42.1 ± 8.0 | 40.3 ± 9.1 | .080 | .145 |
| Physical functioning | 72.6 ± 21.9 | 70.9 ± 22.1 | 65.5 ± 25.9 | .066 | .129 |
| Role-physical | 74.4 ± 32.4 | 67.4 ± 31.9 | 57.2 ± 36.0 | <.001* | .004* |
| Bodily pain | 74.6 ± 21.0 | 73.2 ± 24.1 | 65.8 ± 22.4 | .005* | .006* |
| General health | 49.6 ± 21.6 | 48.9 ± 20.1 | 45.7 ± 21.7 | .324 | .233 |
| Mental health | 53.9 ± 16.8 | 54.6 ± 17.3 | 50.9 ± 17.1 | .302 | .567 |
| Role-emotional | 72.2 ± 40.1 | 73.9 ± 37.6 | 55.2 ± 42.1 | .002*,** | .017*,** |
| Social functioning | 67.8 ± 30.2 | 65.7 ± 31.3 | 58.0 ± 32.5 | .045* | .065 |
| Vitality | 54.8 ± 14.2 | 50.9 ± 15.1 | 50.7 ± 17.3 | .145 | .258 |
| Kidney disease targeted | |||||
| Symptoms/problems | 85.3 ± 12.1 | 86.2 ± 13.3 | 79.7 ± 16.3 | .005* | .013* |
| Effects of kidney disease | 70.0 ± 16.8 | 71.6 ± 17.8 | 69.6 ± 19.7 | .880 | .872 |
| Burden of kidney disease | 31.0 ± 20.0 | 34.0 ± 26.7 | 30.3 ± 22.9 | .757 | .78 |
| Work status | 42.0 ± 23.5 | 34.0 ± 67.7 | 31.3 ± 23.2 | .234 | .945 |
| Cognitive functioning | 69.0 ± 17.4 | 67.8 ± 11.3 | 64.8 ± 18.8 | .181 | .164 |
| Quality of social interaction | 70.0 ± 19.5 | 73.8 ± 18.5 | 64.5 ± 20.4 | .022* | .084 |
| Sexual function | 67.1 ± 25.8 | 72.9 ± 30.0 | 68.2 ± 32.7 | .914 | .866 |
| Sleep | 66.0 ± 21.1 | 65.1 ± 25.7 | 59.9 ± 22.5 | .080 | .101 |
| Social support | 73.6 ± 16.0 | 71.6 ± 20.6 | 69.0 ± 20.6 | .162 | .151 |
| Dialysis staff encouragement | 76.6 ± 15.0 | 81.7 ± 16.4 | 74.9 ± 18.6 | .185 | .375 |
| Overall health | 57.8 ± 48.8 | 60.9 ± 49.9 | 49.4 ± 45.7 | .007** | .004** |
| Patient satisfaction | 59.1 ± 17.9 | 60.9 ± 19.1 | 53.3 ± 20.1 | .025** | .031*,** |
| Mean | 62.5 ± 13.8 | 62.4 ± 14.6 | 56.6 ± 13.3 | ||
| BDI | 12.9 ± 9.4 | 14.0 ± 8.5 | 17.3 ± 10.8 | .003* | .009* |
AVF: arteriovenous fistula; SD: standard deviation; AVG: arteriovenous graft; CVC: central venous catheter; HRQOL: health-related quality of life; SF-36: short form 36; PCS: physical composite summary; MCS: mental composite summary; BDI: Beck’s depression inventory.
Value was obtained from unadjusted regression analysis.
Value was obtained from regression analysis adjusted for age, sex, type of referral, modified Charlson comorbidity index, and hemoglobin levels.
AVF versus CVC.
AVG versus CVC.
Frequency of hospitalization
The frequencies of annual hospitalization according to the type of vascular access are shown in Table 6. Regarding the four types of initial vascular access, patients with NTCVC tended to be hospitalized more frequently, but it was not statistically significant. However, the frequency of hospitalization was significantly different according to the permanent vascular access, which was higher in patients with AVG compared to those with AVF (AVF 0.7 vs. AVG 1.1 times per year) (p = .024).
Table 6.
Frequency of annual hospitalization according to the types of vascular access.
| Type of vascular access | Annual hospitalization Mean ± SD |
p |
|---|---|---|
| Initial access | ||
| AVF | 0.6 ± 1.3 | .092 |
| AVG | 0.7 ± 1.4 | |
| TCVC | 0.6 ± 1.4 | |
| NTCVC | 0.9 ± 2.0 | |
| Permanent access | ||
| AVF | 0.7 ± 1.5 | .024 |
| AVG | 1.1 ± 1.7 |
SD: standard deviation; AVF: arteriovenous fistula; AVG: arteriovenous graft; TCVC: tunneled central venous catheter; NTCVC: non-tunneled central venous catheter.
Discussion
In this multi-center prospective cohort study, we analyzed the all-cause mortality, HRQOL, and BDI scores according to the type of vascular access in incident HD patients. Similar to previous studies [20,21], the survival rate of patients with AVF was higher than those of patients with AVG or CVC. Furthermore, the HRQOL score was high and the BDI score was low in patients with AVF or AVG compared to those with CVC both 3 months and 1 year after the beginning of dialysis. These data suggest that the types of vascular access at the initiation of HD affect the physical and mental health as well as survival rate.
The patients who started dialysis with AVG were older and had more comorbidity compared to those with AVF or CVC. And also, the patients who had AVG as a permanent vascular access had higher prevalence of DM and macrovascular complications. As we expected, the survival rate was worst in patients with AVG probably due to the severe comorbidity and older age. There was no significant difference in survival rate between tunneled and NTCVC as an initial vascular access. The risk of hospitalization seemed to be higher in patients with NTCVC, but it was not statistically significant. The patients with AVG as a permanent vascular access suffered frequent hospitalization compared to AVF patients. Although we could not discriminate the exact causes of hospitalization, the patients with AVG hospitalized frequently probably due to macrovascular diseases and infectious complications led by multiple risk factors [1,21,22].
The AVF is recognized as the preferred type of vascular access for its longer patency, fewer infectious complications, and associated with lower all-cause mortality compared with AVG or CVC [1–3]. However, only a few studies have examined the relationship between the physical or mental health and vascular access type. Recently, in a small study, Domenick Sridharan et al. showed that HD patients experienced great satisfaction with AVF, but there was no significant independent association of vascular access type with HRQOL [12]. In another single center study, Afsar et al. assessed the HRQOL and depression according to the vascular access type in patients receiving HD [10]. They suggested that having a CVC influence negatively in HRQOL. Wasse et al. revealed that compared with persistent CVC use, early permanent AVF use was associated with the perception of improved health status and quality of life among patients with ESRD [11]. In this study, we used the KDQOL-36 survey, which contains kidney disease-specific questions. It showed similar results to those of previous studies in terms of HRQOL. The patients with AVF or AVG showed higher physical functioning and social functioning scores and were more likely to be satisfied with their life than patients with CVC. Moreover, this study showed that the score of HRQOL improved as the vintage of dialysis increased from 3 months to 1 year.
In the study, we also analyzed the patients’ depression score according to the type of vascular access. Weisbord et al. reported that physical and emotional symptoms were common and severe in HD patients, and were correlated directly with impaired HRQOL and depression [23]. In previous study, vascular access type was not associated with the depression [10]. However, our study showed that the degree of depression was related to the vascular access type. The patients with CVC had significantly higher BDI score compared with those with AVF or AVG. Contradictory to previous studies, this study was performed prospectively and included relatively large number of incident HD patients. It showed clearly that AVF had beneficial effect regarding patients’ mood. To the best of our knowledge, this is the only large prospective study that comprehensively elucidated the difference of BDI scores according to vascular access type. This finding might reflect the increased dialysis adequacy by AVF or AVG use which leads to greater reduction of uremic toxins and better anemia correction compared with CVC use [24,25]. Also, there is a possibility that the presence of CVC in upper body incurs disturbed body image and depression. In patients who are not candidate for the creation of AVF which is the best option in HD patients in terms of QOL and depression, every effort is needed to enhance recognition of annoying symptoms such as depression and pain and to improve the effects of intervention [26].
There were significant differences in the context of referral time according to the initial vascular access. The referral time was relatively long before the start of HD and the proportion of patients with early referral was high in patients having AVF as an initial access. However, more than half of patients referred to nephrologists ≥1 year before the initiation of dialysis started HD via temporary CVC. It implies that there is still much opportunity to increase the proportion of patients who create permanent vascular access long before the start of dialysis and avoid the use of CVC. Fortunately, the proportion of AVF as a permanent vascular access in this study was greater than 80%, which was significantly high compared to those of other countries [1,3]. South Korea is one of the highly prevalent countries in the world regarding ESRD. Therefore, early creation and regular surveillance of permanent vascular access is an important task for the care of ESRD patients [27].
Although the results of this study are informative in terms of HRQOL and depression linked to the vascular access type, this study has several limitations. First, only 871 patients at 3 months and 628 patients at 12 months after initiation of dialysis completed HRQOL and BDI surveys. Therefore, there might be a possibility of selection bias. At least, when we compared the clinical characteristics of patients according to the participation status of surveys, there were no significant differences between patients who participated and those who did not. Second, the number of patients started HD via AVG was relatively small compared with AVF or CVC, and it was difficult to make an accurate comparison. In addition, we could not follow the whole enrolled patients and the total number of patients that we could determine the permanent vascular access was less than expected nonetheless considering the censored patients due to early death. Despite of these limitations, we confirmed the importance of initial HD vascular access type in a large prospective cohort study that included only incident patients, and comprehensively elucidated the difference of HRQOL and BDI scores according to the vascular access type.
In conclusion, the survival rate of patients with AVF was higher than those of patients with AVG or CVC. Also, the HRQOL score was high and the BDI score was low in patients with AVF or AVG compared to those with CVC both 3 months and 1 year after the beginning of dialysis. These data suggest that the types of vascular access at the initiation of HD affect the physical and mental health as well as the survival rate. Therefore, it might be essential for the care of impending ESRD patients to prepare permanent vascular access preemptively and avoid the use of CVC as an initial vascular access.
Acknowledgements
This paper has been presented at the 56th ERA-EDTA congress held in Budapest (Hungary), June 13–16, 2019, and published as an abstract in Nephrol Dial Transplant 2019;34(Suppl. 1):SP598.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- 1.Astor BC, Eustace JA, Powe NR, et al. Type of vascular access and survival among incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. J Am Soc Nephrol. 2005;16(5):1449–1455. [DOI] [PubMed] [Google Scholar]
- 2.Lorenzo V, Martín M, Rufino M, et al. Predialysis nephrologic care and a functioning arteriovenous fistula at entry are associated with better survival in incident hemodialysis patients: an observational cohort study. Am J Kidney Dis. 2004;43(6):999–1007. [DOI] [PubMed] [Google Scholar]
- 3.Polkinghorne KR, McDonald SP, Atkins RC, et al. Vascular access and all-cause mortality: a propensity score analysis. J Am Soc Nephrol. 2004;15(2):477–486. [DOI] [PubMed] [Google Scholar]
- 4.Oliver MJ, Rothwell DM, Fung K, et al. Late creation of vascular access for hemodialysis and increased risk of sepsis. J Am Soc Nephrol. 2004;15(7):1936–1942. [DOI] [PubMed] [Google Scholar]
- 5.Perl J, Wald R, McFarlane P, et al. Hemodialysis vascular access modifies the association between dialysis modality and survival. J Am Soc Nephrol. 2011;22(6):1113–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saran R, Li Y, Robinson B, et al. US Renal Data System 2014 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2015;66(1 Suppl. 1):Svii, S1–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Noordzij M, Jager KJ, van der Veer SN, et al. Use of vascular access for haemodialysis in Europe: a report from the ERA-EDTA Registry. Nephrol Dial Transplant. 2014;29(10):1956–1964. [DOI] [PubMed] [Google Scholar]
- 8.Mapes DL, Lopes AA, Satayathum S, et al. Health-related quality of life as a predictor of mortality and hospitalization: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Kidney Int. 2003;64(1):339–349. [DOI] [PubMed] [Google Scholar]
- 9.Morsch CM, Goncalves LF, Barros E.. Health-related quality of life among haemodialysis patients – relationship with clinical indicators, morbidity and mortality. J Clin Nurs. 2006;15(4):498–504. [DOI] [PubMed] [Google Scholar]
- 10.Afsar B, Elsurer R, Covic A, et al. Vascular access type, health-related quality of life, and depression in hemodialysis patients: a preliminary report. J Vasc Access. 2012;13(2):215–220. [DOI] [PubMed] [Google Scholar]
- 11.Wasse H, Kutner N, Zhang R, et al. Association of initial hemodialysis vascular access with patient-reported health status and quality of life. Clin J Am Soc Nephrol. 2007;2(4):708–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Domenick Sridharan N, Fish L, Yu L, et al. The associations of hemodialysis access type and access satisfaction with health-related quality of life. J Vasc Surg. 2018;67(1):229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 14.Hemmelgarn BR, Manns BJ, Quan H, et al. Adapting the Charlson Comorbidity Index for use in patients with ESRD. Am J Kidney Dis. 2003;42(1):125–132. [DOI] [PubMed] [Google Scholar]
- 15.Park JI, Kim M, Kim H, et al. Not early referral but planned dialysis improves quality of life and depression in newly diagnosed end stage renal disease patients: a prospective cohort study in Korea. PLoS One. 2015;10(2):e0117582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rayner HC, Zepel L, Fuller DS, et al. Recovery time, quality of life, and mortality in hemodialysis patients: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2014;64(1):86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim JY, Kim B, Park KS, et al. Health-related quality of life with KDQOL-36 and its association with self-efficacy and treatment satisfaction in Korean dialysis patients. Qual Life Res. 2013;22(4):753–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hedayati SS, Yalamanchili V, Finkelstein FO.. A practical approach to the treatment of depression in patients with chronic kidney disease and end-stage renal disease. Kidney Int. 2012;81:247–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4(6):561–571. [DOI] [PubMed] [Google Scholar]
- 20.Kim HY, Bae EH, Ma SK, et al. Association between initial vascular access and survival in hemodialysis according to age. Korean J Intern Med. 2019;34(4):867–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rivara MB, Soohoo M, Streja E, et al. Association of vascular access type with mortality, hospitalization, and transfer to in-center hemodialysis in patients undergoing home hemodialysis. Clin J Am Soc Nephrol. 2016;11(2):298–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lacson E, Jr, Wang W, Lazarus JM, et al. Change in vascular access and hospitalization risk in long-term hemodialysis patients. Clin J Am Soc Nephrol. 2010;5(11):1996–2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weisbord SD, Fried LF, Arnold RM, et al. Prevalence, severity, and importance of physical and emotional symptoms in chronic hemodialysis patients. J Am Soc Nephrol. 2005;16(8):2487–2494. [DOI] [PubMed] [Google Scholar]
- 24.Tonelli M, Muirhead N.. Access type as a predictor of dialysis adequacy in chronic hemodialysis patients. ASAIO J. 2000;46(3):279–282. [DOI] [PubMed] [Google Scholar]
- 25.Chand DH, Brier M, Strife CF.. Comparison of vascular access type in pediatric hemodialysis patients with respect to urea clearance, anemia management, and serum albumin concentration. Am J Kidney Dis. 2005;45(2):303–308. [DOI] [PubMed] [Google Scholar]
- 26.Weisbord SD. Patient-centered dialysis care: depression, pain, and quality of life. Semin Dial. 2016;29(2):158–164. [DOI] [PubMed] [Google Scholar]
- 27.Jin DC, Yun SR, Lee SW, et al. Current characteristics of dialysis therapy in Korea: 2016 registry data focusing on diabetic patients. Kidney Res Clin Pract. 2018;37(1):20–29. [DOI] [PMC free article] [PubMed] [Google Scholar]