ABSTRACT
Background: Adverse childhood experiences (ACEs) have been identified as an important public health problem with serious implications. Less well understood is how distinct configurations of childhood adversities carry differential risks for mental health, emotional, and social outcomes later in life.
Objective: To determine if distinct profiles of childhood adversities exist for males and females and to examine if unique associations exist between the resultant latent profiles of childhood adversities and multiple indicators of mental health and social and emotional wellbeing in adulthood.
Method: Participants (N = 1,839) were a nationally representative household sample of adults currently residing in the USA and the data were collected via online self-report questionnaires. Latent class analysis was used to identify the optimal number of classes to explain ACE co-occurrence among males and females, separately. ANOVAs, chi-square tests, and t-tests were used to compare male and female classes across multiple mental health, emotional, and social wellbeing variables in adulthood.
Results: Females were significantly more likely than males to report a range of ACEs and mental health, social, and emotional difficulties in adulthood. Two- and four-class models were identified as the best fit for males and females, respectively, indicating more complexity and variation in ACE exposures among females. For males and female, ACEs were strongly associated with poorer mental health, emotional, and social outcomes in adulthood. Among females, growing up in a dysfunctional home environment was a significant risk factor for adverse social outcomes in adulthood.
Conclusions: Males and females have distinct patterns of childhood adversities, with females experiencing more complex and varied patterns of childhood adversity. These patterns of ACEs were associated with numerous negative mental, emotional, and social outcomes among both sexes.
KEYWORDS: Childhood trauma, PTSD, ACE, latent class analysis, childhood adversity, mental health
HIGHLIGHTS: • 21% of males and 39% of females in the US population have been exposed to multiple ACEs in their first 18 years of life.• Females reported a more complex history of childhood adversities than males.• Exposure to ACEs is strongly associated with poorer mental health, social, and emotional outcomes in adulthood.• Exposure to particular ACEs such as growing up in a dysfunctional home was a significant risk factor for negative social outcomes among adult females.
Antecedentes: Las experiencias adversas infantiles (ACEs en su sigla en inglés) se han identificado como un problema de salud pública importante, con serias implicaciones. Menos comprendido es el cómo distintas configuraciones de adversidades infantiles acarrean riesgos diferenciales para los resultados de salud mental, emocional y social.
Objetivo: Determinar si existen distintos perfiles de adversidades infantiles para hombres y para mujeres y examinar si existen asociaciones únicas entre los perfiles latentes resultantes de adversidad infantil y múltiples indicadores de salud mental y bienestar social y emocional en la adultez.
Método: Los participantes (N = 1,839) fueron una muestra representativa de hogares de adultos actualmente residiendo en los Estados Unidos y los datos se recolectaron en cuestionarios de auto-reporte vía online. El análisis de clases latentes se utilizó para identificar el número óptimo de clases que explican la co-ocurrencia de ACEs entre hombres y mujeres, separadamente. Se empleó pruebas de ANOVA, chi-cuadrado y t para comparar clases de hombres y mujeres a través de múltiples variables de salud mental y bienestar social y emocional en la adultez.
Resultados: Las mujeres fueron significativamente más propensas que los hombres a reportar un rango de ACEs y dificultades de salud mental y dificultades sociales y emocionales en la adultez. Modelos de dos y cuatro clases se identificaron como los de mejor ajuste para hombres y mujeres, respectivamente, indicando mayor complejidad y variación de exposición a ACEs en las mujeres. Para hombres y mujeres, las ACEs se asociaron fuertemente a resultados más pobres en salud mental, emocionales y sociales en la adultez. En las mujeres, crecer en un ambiente de hogar disfuncional fue un factor de riesgo significativo para resultados sociales adversos en la adultez.
Conclusiones: Los hombres y mujeres tienen distintos patrones de adversidad infantil, en tanto las mujeres experimentan más complejos y variados patrones de adversidad infantil. Estos patrones de ACEs se asociaron con numerosos resultados negativos mentales, emocionales y sociales entre ambos sexos.
PALABRAS CLAVE: trauma infantil, TEPT, ACE, Análisis de clases latentes, Adversidad infantil, Salud mental
背景:童年期逆境经历 (ACEs) 已被确定为一个重要, 有严重影响的公共卫生问题。人们对童年期逆境的独特结构如何对以后生活中心理健康, 情绪和社会结果带来不同风险的了解还很少。
目标:确定男性和女性是否存在不同的童年期逆境剖面, 并考查由此产生的童年期逆境潜在剖面与成年后心理健康及社会和情绪健康的多个指标是否存在独特关联。
方法:1839名参与者是目前居住在美国的全国性家庭成人代表样本, 数据通过线上自评量表收集。潜在类别分析用于确定男性和女性各自最佳类别数目, 以解释其ACE并发。方差分析, 卡方检验和t检验用于比较男性和女性各类别中在多种成年后心理健康, 情绪和社会健康变量间的差异。
结果:女性比男性更有可能报告一系列ACEs, 以及成年后的心理健康, 社会和情绪障碍。男性和女性的最佳模型分别为两类和四类, 这表明女性中ACE暴露的复杂性和差异性更大。对于男性和女性, ACEs与成年期更差的心理健康, 情绪和社会结果密切相关。在女性中, 在功能失调的家庭环境中成长是成年后不良社会结果的重要风险因素。
结论:男性和女性的童年期逆境模式截然不同, 女性的童年期逆境模式更为复杂和多样。 ACEs的这些模式与男女之间许多负面的心理, 情绪和社会结果均有相关
关键词: 童年期创伤, PTSD, ACE, 潜在类别分析, 童年期逆境, 心理健康
Evidence of the occurrence of adverse childhood experiences (ACE) such as sexual abuse, domestic violence, and parental incarceration, and their impact across the lifespan, is recognized as a landmark of epidemiological research. In the USA (US), approximately 50% of children under 18 years of age have been exposed to at least one ACE event, and approximately 33% have been exposed to multiple ACEs (Sacks & Murphey, 2018). ACE exposure increases risk of cognitive, social, and emotional impairments in childhood (Hughes et al., 2017) and is associated with a range of deleterious mental health outcomes in adulthood such as depression (Poole, Dobson, & Pusch, 2017), anxiety (Green et al., 2010), posttraumatic stress disorder (PTSD) (Lu, Mueser, Rosenberg, & Jankowski, 2008); and increases risk of low socioeconomic status in later life (Metzler, Merrick, Klevens, Ports, & Ford, 2017).
Numerous studies indicate a dose–response relationship between the number of ACEs and poor mental health and social difficulties later in life (e.g. substance abuse, interpersonal and self-directed violence, sexual risk taking, poor self-rated health) (Anda et al., 2002; Chapman et al., 2004; Hughes et al., 2017; Kalmakis & Chandler, 2015). There is also evidence of sex differences in exposure to different types of ACEs, particularly sexual abuse with females substantially more likely than males to report this event (Cavanaugh, Petras, & Martins, 2015; McAnee, Shevlin, Murphy, & Houston, 2019; Roxburgh & MacArthur, 2014; Schilling, Aseltine, & Gore, 2007; Strine et al., 2012). Research also shows that females are more likely than males to being diagnosed with PTSD and affective disorders (Altemus, Sarvaiya, & Neill Epperson, 2014; Olff, 2017); findings that call for further sex-specific investigations of traumatic exposures and associated problems.
A growing literature suggests that distinct profiles of childhood adversity are identifiable among trauma-exposed populations (Debowska, Willmott, Boduszek, & Jones, 2017; Rivera, Fincham, & Bray, 2018), and certain patterns of childhood adversities may be particularly harmful (Lanier, Maguire-Jack, Lombardi, Frey, & Rose, 2018). Specifically, qualitatively different constellations of ACEs, rather than summative and cumulative aspects of exposure, may be more useful in terms of explaining the mental health and social outcomes of individuals exposed to ACEs (Curran, Adamson, Stringer, Rosato, & Leavey, 2016). Put another way, distinct profiles of childhood adversity may be uniquely associated with mental and social health outcomes in adulthood. The identification of such profiles could, therefore, be applied to better inform treatment and allow for the tailoring of intervention practices for groups with different needs (Shevlin, Murphy, Elklit, Murphy, & Hyland, 2018).
The objectives of the present study were to (1) identify distinct profiles of childhood adversities for males and females in a nationally representative sample of US adults, and (2) determine their associations with multiple indicators of mental health (i.e. symptoms of PTSD, Complex PTSD (CPTSD), depression, and anxiety), and emotional and social wellbeing (i.e. relationship status, educational achievement, employment status, income level, psychological wellbeing, and loneliness) in adulthood. Based on existing findings that the frequency and patterns of exposure to ACEs differs by sex (Debowska, Boduszek, Sherretts, Willmott, & Jones, 2018; McAnee et al., 2019), we hypothesized that distinct profiles of ACEs would be identified for males and females. Additionally, based on an extensive literature showing that polyvictimization, or exposure to multiple different types of victimizations during childhood (Finkelhor, Ormrod, & Turner, 2007), increases risk for psychosocial problems in later life (Charak et al., 2016; Hovens, Giltay, Spinhoven, van Hemert, & Penninx, 2015), we hypothesized that profiles characterized by multiple different ACE events would be associated with poorer mental health and social and emotional wellbeing outcomes in adulthood.
1. Methods
1.1. Participants and procedures
The present study used a nationally representative household sample of non-institutionalized adults currently residing in the US. Data were collected in March 2017 from an online research panel that is representative of the adult US population and participants were selected using random probability-based sampling methods. Inclusion criteria were that respondents were aged between 18 and 70 years at the time of the survey and had reported at least one traumatic event in their lifetime, as measured by a modified version of the Life Events Checklist for DSM-5 (LEC-5) (Weathers et al., 2013) and selected items from Adverse Childhood Experiences Questionnaire (Felitti et al., 1998). In total, 3,953 panel members were contacted to participate in the survey and 1,839 volunteered and met the includion criteria (participation rate = 46.5%). The survey design oversampled among females and minority populations (i.e. African American and Hispanic), each at a 2:1 ratio given their increased likelihood of trauma-related distress (Koenen et al., 2017). To adjust for this oversampling, the data were weighted in order to be representative of the entire US adult population aged 18–70 years according to the following benchmarks: sex, age, race/ethnicity, education, census region, household income, home ownership status and metropolitan area. Questionnaires were completed on-line (median time of completion = 18 min), and no payment for participation was offered, however, individuals were incentivized to participate through entry into a raffle for prizes by the survey panel company. Ethical approval for this study was provided by the research ethics committee at the National College of Ireland.
The mean age of the weighted sample was 44.55 years (range = 18–70, SD = 14.89) and included similar numbers of males (48.0%, n = 883) and females (52.0%, n = 956). The majority of the sample were ‘In a committed relationship’ (63.4%, n = 1165) with the remainder ‘Single’ (23.3%, n = 428), ‘Divorced’ (10.9%, n = 202), or ‘Widowed’ (2.4%, n = 44). The majority of the sample were ‘White, Non-Hispanic’ (63.8%, n = 1173), followed by ‘Hispanic’ (16.9%, n = 310), ‘Black, Non-Hispanic’ (11.8%, n = 217), ‘Other, Non-Hispanic’ (6.3%, n = 115), and ‘2+ Races, Non-Hispanic’ (1.3%, n = 24). Approximately one-third of the sample reported that their highest level of educational achievement was a ‘Bachelor’s degree or higher’ (31.8%, n = 585), and similar amounts indicated ‘Some college’ (i.e. had attended college but did not graduate) (30.3%, n = 558) and ‘Finished high school’ (28.7%, n = 528); 9.1% (n = 168) indicated that they ‘Did not finish high school’. Nearly half of the sample earned ‘US$75,000 or more per year’ (48.5%, n = 891), 29.8% (n = 547) earned between ‘US$35,000-US$74,999ʹ, 11.0% (n = 202) earned between ‘US$20,000-US$34,999ʹ, and 10.8% (n = 199) earned between ‘US$0-US$19,999ʹ.
1.2. Measures
1.2.1. Childhood adversity
ACEs were measured using the Adverse Childhood Experiences Questionnaire (Felitti et al., 1998), a 10-item self-report questionnaire measuring different domains of childhood abuse and neglect, and household dysfunction (see Table 1 for each event). Respondents indicated if each event occurred during their first 18 years of life using a binary response format (‘Yes’ = 1, ‘No’ = 0). The psychometric properties of this measure have been well-demonstrated (Wingenfeld et al., 2011).
Table 1.
Differences in endorsement rates for each ACE variable among males and females (N = 1,839).
| Overall |
Females |
Males |
||||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | χ2 | OR (95% CI) | |
| ACE 1: Sexual abuse | 321 | 17.5 | 231 | 24.3 | 90 | 10.2 | 63.19*** | 2.83 (2.18–3.69) |
| ACE 2: Physical abuse | 289 | 15.7 | 152 | 15.9 | 136 | 15.4 | .09 | 1.04 (0.81–1.34) |
| ACE 3: Physical neglect | 98 | 5.4 | 66 | 6.9 | 32 | 3.6 | 9.85** | 1.98 (1.28–3.05) |
| ACE 4: Emotional abuse | 388 | 21.3 | 216 | 22.7 | 172 | 19.7 | 2.46 | 1.20 (0.96–1.50) |
| ACE 5: Emotional neglect | 312 | 17.0 | 198 | 20.8 | 113 | 12.9 | 20.54*** | 1.78 (1.39–2.29) |
| ACE 6: Domestic violence | 213 | 11.5 | 113 | 11.8 | 99 | 11.2 | .17 | 1.06 (0.80–1.41) |
| ACE 7: Parental separation/divorce | 613 | 33.5 | 333 | 34.9 | 280 | 31.9 | 1.91 | 1.15 (0.94–1.39) |
| ACE 8: Household alcohol/drug abuse | 450 | 24.5 | 273 | 28.6 | 177 | 20.0 | 18.33*** | 1.60 (1.29–1.99) |
| ACE 9: Household mental illness/suicide attempt | 284 | 15.5 | 182 | 19.1 | 102 | 11.6 | 19.96*** | 1.81 (1.39–2.35) |
| ACE 10: Member of household went to prison | 146 | 8.0 | 86 | 9.1 | 60 | 6.8 | 3.16 | 1.36 (0.97–1.92) |
χ2 = chi-square test; OR (95% CI) = odds ratio with 95% confidence intervals; statistical significance = *p ≤ .05; **p ≤ .01; ***p ≤ .001.
1.2.2. Indicators of mental health
Symptoms of Major Depressive Disorder and Generalized Anxiety Disorder were measured using the eight-item Patient Health Questionnaire Depression Scale (Kroenke et al., 2009) and the Generalized Anxiety Disorder 7-item Scale (Spitzer, Kroenke, Williams, & Lowe, 2006), respectively. For both measures, respondents indicate how often they have been bothered by each symptom over the last 2 weeks using a 4-point Likert-scale ranging from ‘Not at all’ (0) to ‘Nearly every day’ (3). Scores on the PHQ-8 range from 0 to 24 and on the GAD-7 from 0 to 21. In both cases, higher scores reflect greater symptomatology. The PHQ-8 (Manea, Gilbody, & McMillan, 2015) and GAD-7 (Kertz, Bigda-Peyton, & Bjorgvinsson, 2013) have previously demonstrated excellent psychometric properties. The internal reliability of the PHQ-8 (α = .93) and the GAD-7 (α = .94) were excellent within the current sample.
The International Trauma Questionnaire (ITQ) (Cloitre et al., 2018) is a self-report scale measuring the ICD-11 symptoms of PTSD and CPTSD (scale is freely available at https://www.traumameasuresglobal.com/itq). The ITQ includes six items measuring each PTSD symptom and six items measuring each ‘Disturbance in Self Organization’ (DSO) symptom (ICD-11 CPTSD is a combination of PTSD and DSO symptoms). The ITQ identifies a respondent’s most distressing traumatic experience, and how much the respondent has been bothered by each symptom in the past month. All items are answered in relation to this traumatic event. Participants answer the PTSD items in relation to how much each symptom has bothered them over the last month, and the DSO items are completed in terms of how the respondent typically feels, thinks about oneself, and relates to others. All items are answered on a 5-point Likert-type scale ranging from 0 (‘Not at all’) to 4 (‘Extremely’). PTSD symptoms range from 0 to 24, and CPTSD symptoms range from 0 to 48, with higher scores reflecting more symptoms. The psychometric properties of the ITQ have been supported in multiple general population samples (Ben‐Ezra et al., 2018; Cloitre et al., 2018) and the internal reliability of the PTSD (α = .90), DSO (α = .93), and total (α = .92) scores were excellent among the current sample.
1.2.3. Indicators of emotional wellbeing
Psychological wellbeing was assessed using the five-item World Health Organization Wellbeing Index (WHO-5). The WHO-5 is an internationally validated measure of positive psychological health and a review of 213 studies provided support for the reliability and validity of the scale scores (Topp, Ostergaard, Sondergaard, & Bech, 2015). Respondents indicate how they have been feeling over the past 2 weeks to each positively phrased statement using a 6-point Likert-type scale (0 = ‘At no time’ to 5 = ‘All of the time’). Scores range from 0 to 25 with higher scores reflecting greater psychological wellbeing. The reliability of the WHO-5 within the current sample was excellent (α = .93).
The six-item De Jong Gierveld Loneliness Scale was used to measure feelings of social and emotional loneliness (De Jong Gierveld & Van Tilburg, 2006). All items are answered using a 3-point Likert-type scale of ‘Very much agree’ (1), ‘Somewhat agree’ (2), and ‘Do not agree’ (3). Following the scoring guidelines provided by the scale authors, all items were dichotomized to reflect the ‘Presence’ (1) or ‘Absence’ (0) of each indicator of loneliness. Loneliness scores therefore range from 0 to 6 with higher scores reflecting more feelings of loneliness. This scale has been shown to be reliable and valid in large-scale general population surveys (De Jong Gierveld & Van Tilburg, 2010), and the internal reliability was good within the current sample (α= .81).
1.2.4. Indicators of social wellbeing
The following variables were also used as indicators of social wellbeing: relationship status (0 = ‘In a committed relationship’, 1 = ‘Not in a committed relationship’), educational status (0 = ‘Finished college/university’, 1 = ‘Did not finish college/university’), employment status (0 = ‘Employed/retired’, 1 = ‘Unemployed’), and annual income (0 = ‘At or above the median’, 1 = ‘Below the median’).
1.3. Data analysis
Frequencies and sex differences in exposure to each ACE event were compared using chi-square tests. Sex differences for each mental health and social and emotional wellbeing variable were assessed using independent samples t-tests and chi-square tests.
LCA was used to identify the optimal number of latent classes to explain the co-occurrence of the 10 ACE events among males and females, separately. LCA is a type of mixture modelling that facilitates identification of distinct classes in a population based on similar patterns of responses to categorical data (Nylund, Asparouhov, & Muthén, 2007). The fit of six models (1–6 classes) were evaluated using Mplus version 8.2 (Muthén & Muthén, 2013) and the models were estimated using the robust maximum likelihood estimator (Yuan & Bentler, 2000). To avoid solutions based on local maxima, 200 random sets of starting values and 20 final stage optimizations were used. The relative fit of the competing models was compared using the Akaike Information Criterion (AIC) (Akaike, 1987), the Bayesian Information Criterion (BIC) (Schwarz, 1978), and the sample-size adjusted BIC (Sclove, 1987). In all cases, the model with the lowest value is considered the best fitting. The BIC has demonstrated superior performance in detecting the correct number of classes in simulation studies (Nylund et al., 2007), therefore this index was given precedence in the class enumeration process. In addition, the Lo-Mendell-Rubin adjusted likelihood ratio test (Rubin, Mendell, & Lo, 2001) was used to compare models with increasing numbers of latent classes. When a non-significant value occurs, the model with one less class should be selected. Finally, entropy values (range 0–1) were evaluated to appraise the accuracy of the classifications, with higher values preferred.
Following the selection of the appropriate LCA solutions for males and females, the classes were compared on all mental health and social and emotional wellbeing variables. As each mental health and emotional wellbeing variable was measured on a continuous scale, mean differences were assessed using analysis of variance (ANOVA) tests. As the social wellbeing variables were measured categorically, chi-square tests were used.
All analyses were performed with the weighting variable applied to ensure that the findings were representative of the adult general population of the US. At the variable level, missing data were low, ranging from 0.1% to 3.5%. The missing data were handled using maximum likelihood imputation in Mplus.
2. Results
2.1. Sex differences
Frequencies and sex differences in exposure to the 10 ACEs are reported in Table 1. The most frequently reported event in the full sample was ‘parental separation or divorce’ (33.5%) and the least frequently reported event was ‘physical neglect’ (5.4%). There were significant sex differences on five ACEs, with females being more likely than males to report exposure to ‘sexual abuse’, ‘physical neglect’, ‘emotional neglect’, ‘alcohol and drug abuse in the household’, and ‘household member had a serious mental illness’.
Sex differences across all mental health and social and emotional wellbeing variables are reported in Table 2. Females had significantly higher levels of PTSD, CPTSD, depression, generalized anxiety, and loneliness; and lower levels of psychological wellbeing. All effect sizes were small. Females were significantly more likely than males to be unemployed (OR = 1.8) and to have an annual income below the median (OR = 1.2).
Table 2.
Differences between males and females on all mental health and social and emotional wellbeing variables (N = 1,839).
| Overall |
Females |
Males |
||||||
|---|---|---|---|---|---|---|---|---|
| Mental Health | Mean | SD | Mean | SD | Mean | SD | t | Cohen’s d |
| Posttraumatic stress disorder | 3.74 | 4.95 | 4.34 | 5.33 | 3.11 | 4.41 | −5.27*** | .25 |
| Complex PTSD | 8.36 | 8.92 | 9.54 | 9.53 | 7.10 | 8.05 | −5.73*** | .28 |
| Major depressive disorder | 4.08 | 5.40 | 4.86 | 5.72 | 3.25 | 4.91 | −6.37*** | .30 |
| Generalized anxiety disorder | 3.62 | 4.85 | 4.45 | 5.26 | 2.72 | 4.17 | −7.71*** | .36 |
| Social and Emotional Wellbeing | ||||||||
| Psychological well-being | 14.99 | 6.35 | 14.25 | 6.57 | 15.78 | 6.02 | 5.16*** | .24 |
| Loneliness |
1.76 |
1.77 |
1.87 |
1.81 |
1.64 |
1.72 |
−2.76** |
.13 |
| |
N |
% |
N |
% |
N |
% |
χ2 |
OR (95% CI) |
| Divorced, separated or never married | 630 | 34.3 | 318 | 33.3 | 312 | 35.3 | .87 | 0.91 (0.75–1.11) |
| Did not finish college | 1254 | 68.2 | 639 | 66.8 | 615 | 69.6 | 1.58 | 0.88 (0.72–1.07) |
| Income below the median | 777 | 42.3 | 425 | 44.5 | 352 | 39.9 | 4.05* | 1.21 (1.01–1.46) |
| Unemployed | 312 | 17.0 | 200 | 20.9 | 112 | 12.7 | 22.11*** | 1.82 (1.42–2.34) |
t = independent samples t-test; χ2 = chi-square test; OR (95% CI) = odds ratio with 95% confidence intervals Statistical significance: *p ≤ .05; **p ≤ .01; ***p ≤ .001.
2.2. LCA results
The LCA results for males and females are presented in Table 3. The best-fitting model for males included two classes (see Figure 1) as this solution had the lowest BIC value, and the LMR-A test became non-significant at three classes. The entropy value of .89 indicated that the data was well represented by this model. Class 1 (‘Low Adversity’) included 78.6% (n = 694) of males and was characterized by very low probabilities of endorsing all ACE events. Class 2 (‘Mixed Adversity’) included the remaining 21.4% (n = 189) of males, and was characterized by a high probability of experiencing emotional abuse, and moderate probabilities of endorsing physical abuse, parental separation/divorce, household alcohol/drug abuse, emotional neglect, and domestic violence.
Table 3.
LCA fit statistics based on responses to the ACE for males (n = 883) and females (n = 956).
| Classes | Log-Likelihood | AIC | BIC | ssaBIC | LMR-A (p) | Entropy |
|---|---|---|---|---|---|---|
| Males | ||||||
| 1 | −2410 | 4841 | 4886 | 4854 | – | – |
| 2 | −2023 | 4088 | 4181 | 4115 | 764 (< .001) | .89 |
| 3 | −1994 | 4053 | 4195 | 4094 | 56 (.392) | .73 |
| 4 | −1974 | 4034 | 4225 | 4088 | 40 (1.00) | .78 |
| 5 | −1954 | 4017 | 4257 | 4085 | 38 (.474) | .83 |
| 6 | −1940 | 4011 | 4299 | 4093 | 27 (.768) | .84 |
| Females | ||||||
| 1 | −5689 | 11,399 | 11,450 | 11,418 | – | – |
| 2 | −4899 | 9841 | 9948 | 9881 | 1560 (< .001) | .88 |
| 3 | −4814 | 9692 | 9855 | 9754 | 168 (.223) | .81 |
| 4 | −4755 | 9597 | 9816 | 9680 | 115 (.376) | .76 |
| 5 | −4735 | 9578 | 9853 | 9682 | 40 (.762) | .77 |
| 6 | −4714 | 9559 | 9891 | 9685 | 39 (.763) | .76 |
Best-fitting models in bold. AIC = Akaike information criterion; BIC = Bayesian information criterion; ssaBIC = sample-size adjusted BIC; LMR-A = Lo-Mendell-Rubin adjusted likelihood ratio test
Figure 1.
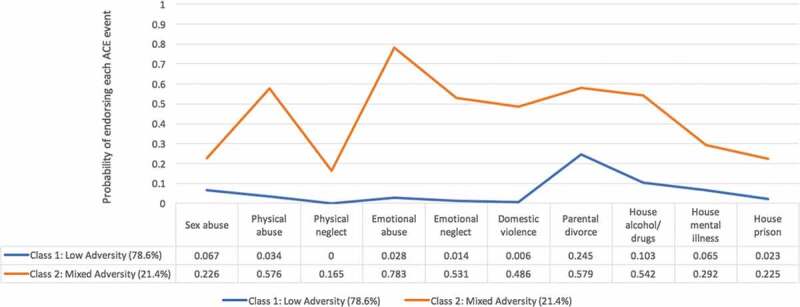
LCA profile plot for childhood adversities among males (n = 883).
Among females, a four-class solution was deemed the best representation of the data (see Figure 2). This solution produced lower AIC and ssaBIC values than the more parsimonious models. Although the LMR-A test was non-significant at two-classes and entropy levels declined with increasing classes, the four-class solution possessed the lowest BIC value. Since the BIC has been shown to be the optimal information criterion test for determining model fit, this result was given precedence and the four class solution was selected. Class 1 (‘High Adversity’) included 7.5% (n = 72) of females and was characterized by high probabilities of experiencing all ACEs, with the exception of household mental illness and parental imprisonment which were moderate and low. Class 2 (‘Child Abuse and Neglect’) included 15.1% (n = 144) of females and was characterized by a high probability of experiencing emotional abuse, and moderate probabilities of experiencing sexual abuse, physical abuse, and emotional neglect. Class 3 (‘Dysfunctional Home’) included 16.4% (n = 156) of females and was characterized by a high probability of experiencing parental separation and divorce and moderate probabilities of household alcohol/drug use, household mental illness/suicide attempt, and sexual abuse. Finally, Class 4 (‘Low Adversity’) included 61.1% (n = 584) of females, and was characterized by very low probabilities of endorsing all ACEs.
Figure 2.
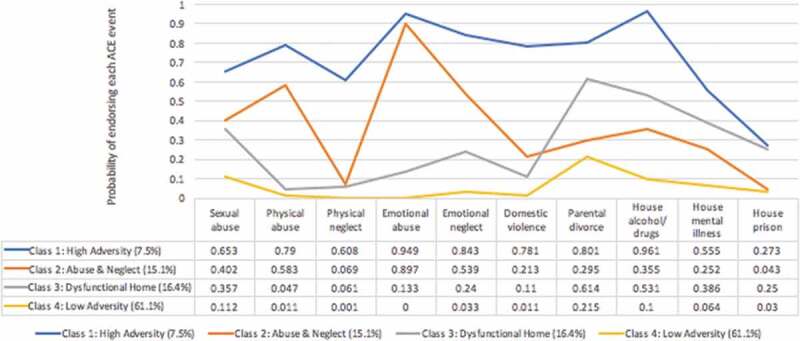
LCA profile plot for childhood adversities among females (n = 956).
2.3. Class membership and associated mental health and social and emotional wellbeing
For males, results from the independent samples t-tests showed that the ‘Mixed Adversity’ class had significantly higher levels of PTSD, CPTSD, depression, generalized anxiety, and loneliness, and, significantly lower levels of psychological wellbeing compared to the ‘Low Adversity’ class (ps < .001). These differences were all moderate-to-large, with the biggest effect for psychological wellbeing (d = 1.19). Membership of the ‘Mixed Adversity’ class was associated with a significantly higher likelihood of not attending university, and having an annual income below the median (see Table 4).
Table 4.
Differences between the male LCA classes on all mental health and social and emotional wellbeing variables (n = 883).
| Mental Health | LCA Classes | Mean | SD | t | df | Cohen’s d |
|---|---|---|---|---|---|---|
| Post-traumatic stress disorder | Mixed adversity | 6.02 | 5.91 | −8.22*** | 221 | .77 |
| Low adversity | 2.29 | 3.47 | ||||
| Complex PTSD | Mixed adversity | 13.72 | 10.53 | −10.21*** | 209 | .98 |
| Low adversity | 5.30 | 6.09 | ||||
| Major depressive disorder | Mixed adversity | 6.69 | 6.33 | −8.98*** | 858 | .83 |
| Low adversity | 2.30 | 3.96 | ||||
| Generalized anxiety disorder | Mixed adversity | 5.61 | 5.48 | −8.79*** | 224 | .82 |
| Low Adversity | 1.91 | 3.30 | ||||
| Social and Emotional Wellbeing | ||||||
| Psychological well-being | Mixed adversity | 5.45 | 6.41 | 9.73*** | 265 | 1.19 |
| Low adversity | 16.84 | 11.87 | ||||
| Loneliness | Mixed adversity | 2.57 | 1.95 | −7.68*** | 255 | .70 |
| |
Low adversity |
1.39 |
1.55 |
|
|
|
| |
|
% (n) |
|
χ2 |
|
OR (95% CI) |
| Not in a committed relationship | Mixed adversity | 37.0% (70) | .31 | 1 | 1.10 (0.79–1.53) | |
| Low adversity | 34.9% (242) | |||||
| Did not attend college | Mixed adversity | 77.8% (147) | 7.71* | 1 | 1.70 (1.17–2.48) | |
| Low adversity | 67.3% (467) | |||||
| Income below the median | Mixed adversity | 51.9% (98) | 14.59*** | 1 | 1.87 (1.35–2.59) | |
| Low adversity | 36.5% (253) | |||||
| Unemployed | Mixed adversity | 13.2% (25) | .06 | 1 | 1.06 (0.66–1.71) | |
| Low adversity | 12.5% (87) | |||||
t = independent samples t-test; df = degrees of freedom; χ2 = chi-square test; OR (95% CI) = odds ratio with 95% confidence intervals Statistical significance: *p ≤ .05; **p ≤ .01; ***p ≤ .001.
For females, results from the one-way between groups ANOVA tests showed that the four classes significantly differed on all mental health and emotional wellbeing variables, with effects ranging from moderate-to-large (see Table 5). For each mental health and emotional wellbeing variable, the ‘High Adversity’ class had significantly higher symptom scores than all other classes. The ‘Dysfunctional Home’ and ‘Child Abuse and Neglect’ classes exhibited significantly higher symptom scores on all mental health and emotional wellbeing variables compared to the ‘Low Adversity’ class. The ‘Dysfunctional Home’ and ‘Child Abuse and Neglect’ classes did not differ from each other on any of the mental health or the emotional wellbeing variables.
Table 5.
Differences between the female LCA classes on all mental health and social and emotional wellbeing variables (n = 956).
| Mental Health | Classes | Mean | SD | F | Eta-squared |
|---|---|---|---|---|---|
| Post-traumatic stress disorder | Class 1: High adversity | 10.372,3,4 | 6.89 | 58.52*** | .17 |
| Class 2: Abuse and neglect | 5.871,4 | 5.58 | |||
| Class 3: Dysfunctional home | 5.431,4 | 5.53 | |||
| Class 4: Low adversity | 2.901,2,3 | 4.17 | |||
| Complex PTSD | Class 1: High adversity | 20.532,3,4 | 11.90 | 77.06*** | .23 |
| Class 2: Abuse and neglect | 13.681,4 | 9.08 | |||
| Class 3: Dysfunctional home | 12.141,4 | 10.06 | |||
| Class 4: Low adversity | 6.431,2,3 | 7.8 | |||
| Major depressive disorder | Class 1: High adversity | 9.932,3,4 | 7.45 | 52.73*** | .15 |
| Class 2: Abuse and neglect | 7.191,4 | 5.90 | |||
| Class 3: Dysfunctional home | 6.401,4 | 6.42 | |||
| Class 4: Low adversity | 3.211,2,3 | 4.37 | |||
| Generalized anxiety disorder | Class 1: High adversity | 9.162,3,4 | 6.65 | 44.26*** | .13 |
| Class 2: Abuse and neglect | 6.401,4 | 5.61 | |||
| Class 3: Dysfunctional home | 5.391,4 | 5.77 | |||
| Class 4: Low adversity | 3.111,2,3 | 4.18 | |||
| Social and Emotional Wellbeing | |||||
| Psychological wellbeing | Class 1: High adversity | 9.513,4 | 6.61 | 40.29*** | .12 |
| Class 2: Abuse and neglect | 11.374 | 6.07 | |||
| Class 3: Dysfunctional home | 12.831,4 | 6.51 | |||
| Class 4: Low adversity | 15.911,2,3 | 6.08 | |||
| Loneliness | Class 1: High adversity | 3.193,4 | 1.96 | 38.87*** | .13 |
| Class 2: Abuse and neglect | 2.594 | 1.94 | |||
| Class 3: Dysfunctional home | 2.341,4 | 1.92 | |||
| |
Class 4: Low adversity |
1.411,2,3 |
1.56 |
|
|
| |
|
% (n) |
|
χ2 |
Phi coefficient |
| Not in a committed relationship | Class 1: High adversity | 27.8% (20) | 7.93* | .09 | |
| Class 2: Abuse and neglect | 34.0% (49) | ||||
| Class 3: Dysfunctional home | 42.3% (66)* | ||||
| Class 4: Low adversity | 31.2% (182) | ||||
| Did not finish college | Class 1: High adversity | 70.4% (50) | 6.35 | .00 | |
| Class 2: Abuse and neglect | 70.1% (101) | ||||
| Class 3: Dysfunctional home | 73.2% (115) | ||||
| Class 4: Low adversity | 63.9% (373)* | ||||
| Income below the median | Class 1: High adversity | 61.1% (44)* | 23.54*** | .16 | |
| Class 2: Abuse and neglect | 47.2% (68) | ||||
| Class 3: Dysfunctional home | 55.4% (87)* | ||||
| Class 4: Low adversity | 38.9% (227)* | ||||
| Unemployed | Class 1: High adversity | 33.3% (24)* | 8.34* | .09 | |
| Class 2: Abuse and neglect | 22.1% (32) | ||||
| Class 3: Dysfunctional home | 17.3% (27) | ||||
| Class 4: Low adversity | 20.0% (117) |
Superscript numbers indicate significant differences between classes; F = ANOVA test; Statistical significance: *p ≤ .05; **p ≤ .01; ***p ≤ .001.
Significant differences were present across the four classes for each social wellbeing variable with the exception of academic status. Significantly more people than expected in the ‘High Adversity’ class had an annual income below the median and were unemployed. Significantly more respondents than expected in the ‘Dysfunctional Home’ class were not currently in a relationship and had an annual income below the median.
3. Discussion
The present study found that females in the US are more likely than males to report experiences of childhood sexual abuse, physical neglect, emotional neglect, household drug/alcohol abuse, and household mental illness. The sex differences in rates of ACEs, particularly relating to sexual abuse, are consistent with existing evidence (Giarratano, Ford, & Nochajski, 2017; Stoltenborgh, van Ijzendoorn, Euser, & Bakermans-Kranenburg, 2011). Previous findings have indicated that approximately 20% of females in the US have been exposed to serious sexual violence in their lifetime, with the majority of these women (79%) reporting their first sexual assault in childhood or young adulthood (Breiding et al., 2014)
The LCA results indicated that males and females have distinct profiles of childhood adversity, with females characterized by more complex and varied histories of childhood adversities (four classes) compared to males (two classes). This is in line with existing research showing that females who have been exposed to child sexual abuse are more likely to report additional traumatic events in childhood (Banyard, Hamby, & Grych, 2017; Cavanaugh et al., 2015). These findings revealed that for females child sexual abuse tends to co-occur with other types of adversities. All three of the female adversity profiles were characterized by at least a moderate probability of sexual abuse. This may partially explain the complexity of childhood adversity among females; however, it does not explain why females were more likely than males to have a profile of childhood adversity characterized primarily by a disturbed home life. Previous research has suggested that females may be more willing to report some types of ACEs (Strine et al., 2012) and that variation in responses on trauma-related topics may occur due to the sensitive nature of questions (Curran et al., 2016). Specifically, estimates of male sexual abuse may be affected by under-reporting due to unwillingness to disclose abuse (Finkelhor, 2019; Negriff, Schneiderman, Smith, Schreyer, & Trickett, 2014), with reluctance to disclose potentially extending to other types of traumatic exposures (Vaswani, 2018). Whatever the reasons for the greater complexity of childhood adversities reported among females, future research should investigate whether this complex history of childhood adversity accounts, even in part, for the twofold increased risk of multiple internalizing disorders among females (Caspi et al., 2014; Kessler et al., 2005, 1994)
The classes characterized by the most severe history of childhood adversities (i.e. the female ‘High Adversity’ class and the male ‘Mixed Adversity’ class) had the poorest mental health, and emotional and social wellbeing outcomes in adulthood. These results confirm our initial hypothesis and align with the existing literature that individuals exposed to polyvictimization in childhood are at elevated risk for a range of psychosocial difficulties in later life (Andersen, Hughes, Zou, & Wilsnack, 2014).
Among females, the two classes that differed qualitatively rather than quantitatively (the ‘Dysfunctional Home’ and ‘Child Abuse and Neglect’ classes) differed across two social outcomes, whereby females with a history of childhood adversity, characterized by a disrupted and unstable home life, were at particular risk of having low-income levels and not being in a committed relationship in adulthood. This is consistent with previous findings within the ACE literature which found that household dysfunction is associated with negative social outcomes in adulthood (Levenson, Willis, & Prescott, 2016). Household dysfunction in the forms of co-occurring parental drug or alcohol abuse, mental illness, conflict, and incarceration could be confounded with socioeconomic status which is a strong predictor of a range of mental health and physical problems as well as overall life opportunities (Metzler et al., 2017). Further investigation of ACEs integrated within a social disadvantage framework is, therefore, warranted (Nurius, Logan-Greene, & Green, 2012).
Research has shown that females are twice as likely as males to be diagnosed with PTSD, despite the fact that males report higher exposure of traumatic events across the lifespan (Benjet et al., 2016; Breslau, 2002). The sex difference in risk of PTSD appears not to be due to the nature of the traumatic event (i.e. greater likelihood of reporting sexual-based traumas among females) or various methods of assessing trauma exposure and/or PTSD (Tolin & Foa, 2006) but may be associated with sex differences in known risk factors associated with PTSD (Christiansen & Hansen, 2015). However, the present study suggests that the developmental timing of exposure to adversities and trauma may be an important factor. Indeed, it is interesting to note that although males are more likely than females to be trauma-exposed across the lifespan, the present study found the opposite pattern in the first 18 years of life with respect to ACEs. In this case, females were twice as likely as males to report multiple ACEs. Thus, the risk of PTSD (and other internalizing psychiatric disorders) may not only be predicted by the quantity and quality of traumatic exposure(s), but also by when in the developmental period these events occurred. The experience of trauma in childhood, in particular, can influence the development of negative schemas about the self, others, and the world (Beck, 2008; Jacobs, Reinecke, Gollan, & Kane, 2008), which ultimately increase vulnerability to disorders such as depression, anxiety, and PTSD (Ostefjells et al., 2017). Explaining sex differences in risk of developing certain psychiatric disorders are, however, a complex and sensitive issue, and almost certainly encompass many interacting evolutionary, biological, psychological, social, and methodological factors (Olff, 2017). Nonetheless, our findings offer the possibility that at least some of this effect may be attributable to the different profiles of adversity and trauma endorsed by males and females in the early stages of life.
The identification of different profiles of ACE co-occurrence among males and females has several implications. For clinical purposes, knowledge of sex differences in ACEs can facilitate a more nuanced understanding of subgroups with differential risk for social, emotional, and mental health difficulties and this can help to guide improvements in intervention and treatment programmes. By simultaneously investigating mental health and social outcomes, this study provides a broad understanding of individual life conditions (e.g. opportunities, social factors) and contributes novel evidence into a field that has predominately focussed on investigating the links between ACEs and health (Metzler et al., 2017).
The findings of the present study are not without limitations. The use of self-reported and retrospective data on childhood adversities may introduce response and recall bias (Debowska & Boduszek, 2017), however, retrospectively collected data regarding early adversities has been shown to be reliable via test-re-test reliability analysis (Dong et al., 2004). In the present study, it was not possible to account for the exact timing of exposure to ACEs, their chronicity, severity, or intensity; all of which are important elements of such experiences and may have biased the results (Ports, Ford, & Merrick, 2016; Riem & Karreman, 2018). Furthermore, the use of cross-sectional data hinders inferences about causality. Other unaccounted factors could also be contributing to the relations between ACE profiles and mental health and emotional and social wellbeing outcomes such as parental income and parental education status (Davis-Kean, 2005; Wade et al., 2016). A four-class solution was selected as the best representation of the data among females as the BIC was lower for this solution than the more parsimonious models. This solution also produced lower AIC and ssaBIC values. The LCA for the females was, however, characterized by inconsistencies among the statistical indicators for assessing model fit, the entropy value and the LMR-A test indicated that a two-class solution represented the data well. Replication with other populations is therefore needed before definitely concluding that females have more complex patterns of ACE exposures.
Finally, the present study has focused on investigating the negative outcomes associated with childhood adversity, but less is known about the role of resilience and protective factors for mental health despite ACEs (Banyard et al., 2017; Poole et al., 2017).
To conclude, five important findings from this study are worth highlighting: (1) 21% of males and 39% of females in the US population have been exposed to multiple ACEs in their first 18 years of life; (2) females reported a more complex and varied history of childhood adversities than males; (3) exposure to ACEs is strongly associated with poorer mental health and emotional and social wellbeing in adulthood; (4) exposure to particular ACEs such as growing up in a dysfunctional home environment appear to be a significant risk factor for negative social outcomes among females in adulthood; and (5) recognition of sex differences in patterns of childhood adversity may offer unique insights into why females are more likely to develop multiple internalizing psychiatric disorders than males during adulthood. Overall, the results of the present study are consistent with a wide body of research indicating that a history of childhood adversity, whether for males or for females, is associated with negative outcomes in the domains of mental health and emotional and social wellbeing later in life. The present study adds to existing research by demonstrating the importance of considering specific combinations of childhood adversities when investigating the links between ACEs and adverse outcomes across the lifespan (Lanier et al., 2018; McLafferty et al., 2015).
Funding Statement
This work was supported by the COllaborative Network for Training and EXcellence in psychoTraumatology (CONTEXT) programme from the European Union's Horizon 2020, under the Marie Sklodowska-Curie [722523]; the National Institutes of Mental Health [R01 MH08661]; the Irish Research Council [GOIPG/2018/319].
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Akaike, H. (1987). Factor analysis and AIC. Psychometrika, 52(3), 317–12. [Google Scholar]
- Altemus, M., Sarvaiya, N., & Neill Epperson, C. (2014). Sex differences in anxiety and depression clinical perspectives. Frontiers in Neuroendocrinology, 35(3), 320–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anda, R. F., Whitfield, C. L., Felitti, V. J., Chapman, D., Edwards, V. J., Dube, S. R., & Williamson, D. F. (2002). Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatric Services, 53(8), 1001–1009. [DOI] [PubMed] [Google Scholar]
- Andersen, J. P., Hughes, T. L., Zou, C., & Wilsnack, S. C. (2014). Lifetime victimization and physical health outcomes among lesbian and heterosexual women. PloS One, 9(7), e101939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banyard, V., Hamby, S., & Grych, J. (2017). Health effects of adverse childhood events: Identifying promising protective factors at the intersection of mental and physical well-being. Child Abuse & Neglect, 65, 88–98. [DOI] [PubMed] [Google Scholar]
- Beck, A. T. (2008). The evolution of the cognitive model of depression and its neurobiological correlates. American Journal of Psychiatry, 165(8), 969–977. [DOI] [PubMed] [Google Scholar]
- Ben‐Ezra, M., Karatzias, T., Hyland, P., Brewin, C. R., Cloitre, M., Bisson, J. I., … Shevlin, M. (2018). Posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD) as per ICD‐11 proposals: A population study in Israel. Depression and Anxiety, 35(3), 264–274. [DOI] [PubMed] [Google Scholar]
- Benjet, C., Bromet, E., Karam, E. G., Kessler, R. C., McLaughlin, K. A., Ruscio, A. M., … Koenen, K. C. (2016). The epidemiology of traumatic event exposure worldwide: Results from the world mental health survey consortium. Psychological Medicine, 46(2), 327–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breiding, M. J., Smith, S. G., Basile, K. C., Walters, M. L., Chen, J., & Merrick, M. T. (2014). Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization–National intimate partner and sexual violence survey, USA, 2011. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, D.C.: 2002), 63(8), 1–18. [PMC free article] [PubMed] [Google Scholar]
- Breslau, N. (2002). Epidemiologic studies of trauma, posttraumatic stress disorder, and other psychiatric disorders. Canadian Journal of Psychiatry. Revue Canadienne De Psychiatrie, 47(10), 923–929. [DOI] [PubMed] [Google Scholar]
- Caspi, A., Houts, R. M., Belsky, D. W., Goldman-Mellor, S. J., Harrington, H., Israel, S., … Poulton, R. (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2(2), 119–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh, C. E., Petras, H., & Martins, S. S. (2015). Gender-specific profiles of adverse childhood experiences, past year mental and substance use disorders, and their associations among a national sample of adults in the USA. Social Psychiatry and Psychiatric Epidemiology, 50(8), 1257–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman, D. P., Whitfield, C. L., Felitti, V. J., Dube, S. R., Edwards, V. J., & Anda, R. F. (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82(2), 217–225. [DOI] [PubMed] [Google Scholar]
- Charak, R., Byllesby, B. M., Roley, M. E., Claycomb, M. A., Durham, T. A., Ross, J., … Elhai, J. D. (2016). Latent classes of childhood poly-victimization and associations with suicidal behavior among adult trauma victims: Moderating role of anger. Child Abuse & Neglect, 62, 19–28. [DOI] [PubMed] [Google Scholar]
- Christiansen, D. M., & Hansen, M. (2015). Accounting for sex differences in PTSD: A multi-variable mediation model. European Journal of Psychotraumatology, 6, 26068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre, M., Shevlin, M., Brewin, C., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The International Trauma Questionnaire: Development of a self‐report measure of ICD‐11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. [DOI] [PubMed] [Google Scholar]
- Curran, E., Adamson, G., Stringer, M., Rosato, M., & Leavey, G. (2016). Severity of mental illness as a result of multiple childhood adversities: US National Epidemiologic Survey. Social Psychiatry and Psychiatric Epidemiology, 51(5), 647–657. [DOI] [PubMed] [Google Scholar]
- Davis-Kean, P. (2005). The influence of parent education and family income on child achievement: The indirect role of parental expectations and the home environment. Journal of Family Psychology, 19, 294. [DOI] [PubMed] [Google Scholar]
- De Jong Gierveld, J., & Van Tilburg, T. (2006). A 6-item scale for overall, emotional, and social loneliness: Confirmatory tests on survey data. Research on Aging, 28(5), 582–598. [Google Scholar]
- De Jong Gierveld, J., & Van Tilburg, T. (2010). The De Jong Gierveld short scales for emotional and social loneliness: Tested on data from 7 countries in the UN generations and gender surveys. European Journal of Ageing, 7(2), 121–130. doi: 10.1007/s10433-010-0144-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debowska, A., & Boduszek, D. (2017). Child abuse and neglect profiles and their psychosocial consequences in a large sample of incarcerated males. Child Abuse & Neglect, 65, 266–277. [DOI] [PubMed] [Google Scholar]
- Debowska, A., Boduszek, D., Sherretts, N., Willmott, D., & Jones, A. D. (2018). Profiles and behavioral consequences of child abuse among adolescent girls and boys from Barbados and Grenada. Child Abuse & Neglect, 79, 245–258. [DOI] [PubMed] [Google Scholar]
- Debowska, A., Willmott, D., Boduszek, D., & Jones, A. D. (2017). What do we know about child abuse and neglect patterns of co-occurrence? A systematic review of profiling studies and recommendations for future research. Child Abuse & Neglect, 70, 100–111. [DOI] [PubMed] [Google Scholar]
- Dong, M., Anda, R. F., Felitti, V. J., Dube, S. R., Williamson, D. F., Thompson, T. J., … Giles, W. H. (2004). The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect, 28(7), 771–784. [DOI] [PubMed] [Google Scholar]
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., … Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- Finkelhor, D. (2019). Child sexual abuse: Challenges facing child protection and mental health professionals. Childhood and Trauma, 101–116. [Google Scholar]
- Finkelhor, D., Ormrod, R. K., & Turner, H. A. (2007). Polyvictimization and trauma in a national longitudinal cohort. Development and Psychopathology, 19(1), 149–166. [DOI] [PubMed] [Google Scholar]
- Giarratano, P., Ford, J. D., & Nochajski, T. H. (2017). Gender differences in complex posttraumatic stress symptoms, and their relationship to mental health and substance abuse outcomes in incarcerated adults. Journal of Interpersonal Violence, 886260517692995. doi: 10.1177/0886260517692995 [DOI] [PubMed] [Google Scholar]
- Green, J. G., McLaughlin, K. A., Berglund, P. A., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C. (2010). Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: Associations with first onset of DSM-IV disordersnational comorbidity survey replication I. Archives of General Psychiatry, 67(2), 113–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovens, J. G., Giltay, E. J., Spinhoven, P., van Hemert, A. M., & Penninx, B. W. (2015). Impact of childhood life events and childhood trauma on the onset and recurrence of depressive and anxiety disorders. The Journal of Clinical Psychiatry, 76(7), 931–938. [DOI] [PubMed] [Google Scholar]
- Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C., … Dunne, M. P. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health, 2(8), e356–e366. [DOI] [PubMed] [Google Scholar]
- Jacobs, R. H., Reinecke, M. A., Gollan, J. K., & Kane, P. (2008). Empirical evidence of cognitive vulnerability for depression among children and adolescents: A cognitive science and developmental perspective. Clinical Psychology Review, 28(5), 759–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmakis, K. A., & Chandler, G. E. (2015). Health consequences of adverse childhood experiences: A systematic review. Journal of the American Association of Nurse Practitioners, 27(8), 457–465. [DOI] [PubMed] [Google Scholar]
- Kertz, S., Bigda-Peyton, J., & Bjorgvinsson, T. (2013). Validity of the generalized anxiety disorder-7 scale in an acute psychiatric sample. Clinical Psychology & Psychotherapy, 20(5), 456–464. [DOI] [PubMed] [Google Scholar]
- Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. [DOI] [PubMed] [Google Scholar]
- Kessler, R. C., McGonagle, K. A., Zhao, S., Nelson, C. B., Hughes, M., Eshleman, S., & Kendler, K. S. (1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the USA: Results from the National Comorbidity Survey. Archives of General Psychiatry, 51(1), 8–19. [DOI] [PubMed] [Google Scholar]
- Koenen, K. C., Ratanatharathorn, A., Ng, L., McLaughlin, K. A., Bromet, E. J., Stein, D. J., … Kessler, R. C. (2017). Posttraumatic stress disorder in the World Mental Health Surveys. Psychological Medicine, 47(13), 2260–2274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K., Strine, T. W., Spitzer, R. L., Williams, J. B., Berry, J. T., & Mokdad, A. H. (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1–3), 163–173. [DOI] [PubMed] [Google Scholar]
- Lanier, P., Maguire-Jack, K., Lombardi, B., Frey, J., & Rose, R. A. (2018). Adverse childhood experiences and child health outcomes: Comparing cumulative risk and latent class approaches. Maternal and Child Health Journal, 22(3), 288–297. [DOI] [PubMed] [Google Scholar]
- Levenson, J. S., Willis, G. M., & Prescott, D. S. (2016). Adverse childhood experiences in the lives of male sex offenders: Implications for trauma-informed care. Sexual Abuse, 28(4), 340–359. [DOI] [PubMed] [Google Scholar]
- Lu, W., Mueser, K. T., Rosenberg, S. D., & Jankowski, M. K. (2008). Correlates of adverse childhood experiences among adults with severe mood disorders. Psychiatric Services, 59(9), 1018–1026. [DOI] [PubMed] [Google Scholar]
- Manea, L., Gilbody, S., & McMillan, D. (2015). A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. General Hospital Psychiatry, 37(1), 67–75. [DOI] [PubMed] [Google Scholar]
- McAnee, G., Shevlin, M., Murphy, J., & Houston, J. (2019). Where are all the males? Gender-specific typologies of childhood adversity based on a large community sample. Child Abuse & Neglect, 90, 149–159. [DOI] [PubMed] [Google Scholar]
- McLafferty, M., Armour, C., McKenna, A., O’Neill, S., Murphy, S., & Bunting, B. (2015). Childhood adversity profiles and adult psychopathology in a representative Northern Ireland study. Journal of Anxiety Disorders, 35, 42–48. [DOI] [PubMed] [Google Scholar]
- Metzler, M., Merrick, M. T., Klevens, J., Ports, K. A., & Ford, D. C. (2017). Adverse childhood experiences and life opportunities: Shifting the narrative. Children and Youth Services Review, 72, 141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (2013). Mplus user’s guide (7th ed.). Los Angeles: Muthén & Muthén. [Google Scholar]
- Negriff, S., Schneiderman, J. U., Smith, C., Schreyer, J. K., & Trickett, P. K. (2014). Characterizing the sexual abuse experiences of young adolescents. Child Abuse & Neglect, 38(2), 261–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurius, P. S., Logan-Greene, P., & Green, S. (2012). Adverse childhood experiences (ACE) within a social disadvantage framework: Distinguishing unique, cumulative, and moderated contributions to adult mental health. Journal of Prevention & Intervention in the Community, 40(4), 278–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund, K. L., Asparouhov, T., & Muthén, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo Simulation Study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4), 535–569. [Google Scholar]
- Olff, M. (2017). Sex and gender differences in post-traumatic stress disorder: An update. European Journal of Psychotraumatology, 8(sup4), 1351204. [Google Scholar]
- Ostefjells, T., Lystad, J. U., Berg, A. O., Hagen, R., Loewy, R., Sandvik, L., … Rossberg, J. I. (2017). Metacognitive beliefs mediate the effect of emotional abuse on depressive and psychotic symptoms in severe mental disorders. Psychological Medicine, 47(13), 2323–2333. [DOI] [PubMed] [Google Scholar]
- Poole, J. C., Dobson, K. S., & Pusch, D. (2017). Childhood adversity and adult depression: The protective role of psychological resilience. Child Abuse & Neglect, 64, 89–100. [DOI] [PubMed] [Google Scholar]
- Ports, K. A., Ford, D. C., & Merrick, M. T. (2016). Adverse childhood experiences and sexual victimization in adulthood. Child Abuse & Neglect, 51, 313–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riem, M. M. E., & Karreman, A. (2018). Childhood adversity and adult health: The role of developmental timing and associations with accelerated aging. Child Maltreatment, 24(1), 17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera, P. M., Fincham, F. D., & Bray, B. C. (2018). Latent classes of maltreatment: A systematic review and critique. Child Maltreatment, 23(1), 3–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roxburgh, S., & MacArthur, K. R. (2014). Childhood adversity and adult depression among the incarcerated: Differential exposure and vulnerability by race/ethnicity and gender. Child Abuse & Neglect, 38(8), 1409–1420. [DOI] [PubMed] [Google Scholar]
- Rubin, D. B., Mendell, N. R., & Lo, Y. (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. [Google Scholar]
- Sacks, V., & Murphey, D. (2018). The prevalence of adverse childhood experiences, nationally, by state, and by race/ethnicity. Retrieved from https://www.childtrends.org/wp-content/uploads/2018/02/ACESBriefUpdatedFinal_ChildTrends_February2018.pdf
- Schilling, E. A., Aseltine, R. H., & Gore, S. (2007). Adverse childhood experiences and mental health in young adults: A longitudinal survey. BMC Public Health, 7(1), 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz, G. (1978). Estimating the dimension of a model. Annals of Statistics, 6, 461–464. [Google Scholar]
- Sclove, S. L. (1987). Application of model-selection criteria to some problems in multivariate analysis. Psychometrika, 52(3), 333–343. [Google Scholar]
- Shevlin, M., Murphy, S., Elklit, A., Murphy, J., & Hyland, P. (2018). Typologies of child sexual abuse: An analysis of multiple abuse acts among a large sample of Danish treatment-seeking survivors of childhood sexual abuse. Psychological Trauma: Theory, Research, Practice and Policy, 10(3), 263–269. [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., Williams, J. B., & Lowe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. [DOI] [PubMed] [Google Scholar]
- Stoltenborgh, M., van Ijzendoorn, M. H., Euser, E. M., & Bakermans-Kranenburg, M. J. (2011). A global perspective on child sexual abuse: Meta-analysis of prevalence around the world. Child Maltreatment, 16(2), 79–101. [DOI] [PubMed] [Google Scholar]
- Strine, T. W., Dube, S. R., Edwards, V. J., Prehn, A. W., Rasmussen, S., Wagenfeld, M., … Croft, J. B. (2012). Associations between adverse childhood experiences, psychological distress, and adult alcohol problems. American Journal of Health Behavior, 36(3), 408–423. [DOI] [PubMed] [Google Scholar]
- Tolin, D. F., & Foa, E. B. (2006). Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin, 132(6), 959–992. [DOI] [PubMed] [Google Scholar]
- Topp, C. W., Ostergaard, S. D., Sondergaard, S., & Bech, P. (2015). The WHO-5 well-being index: A systematic review of the literature. Psychotherapy and Psychosomatics, 84(3), 167–176. [DOI] [PubMed] [Google Scholar]
- Vaswani, N. (2018). Adverse childhood experiences in children at high risk of harm to others: A gendered perspective. Glasgow: Centre for Youth and Criminal Justice.
- Wade, R., Jr., Cronholm, P. F., Fein, J. A., Forke, C. M., Davis, M. B., Harkins-Schwarz, M., … Bair-Merritt, M. H. (2016). Household and community-level adverse childhood experiences and adult health outcomes in a diverse urban population. Child Abuse & Neglect, 52, 135–145. [DOI] [PubMed] [Google Scholar]
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The Life Events Checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD. Retrieved from www.ptsd.va.gov
- Wingenfeld, K., Schafer, I., Terfehr, K., Grabski, H., Driessen, M., Grabe, H., … Spitzer, C. (2011). The reliable, valid and economic assessment of early traumatization: First psychometric characteristics of the German version of the Adverse Childhood Experiences Questionnaire (ACE). Psychotherapie, Psychosomatik, Medizinische Psychologie, 61(1), e10–14. [DOI] [PubMed] [Google Scholar]
- Yuan, K.-H., & Bentler, P. M. (2000). Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociological Methodology, 30(1), 165–200. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Sacks, V., & Murphey, D. (2018). The prevalence of adverse childhood experiences, nationally, by state, and by race/ethnicity. Retrieved from https://www.childtrends.org/wp-content/uploads/2018/02/ACESBriefUpdatedFinal_ChildTrends_February2018.pdf
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The Life Events Checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD. Retrieved from www.ptsd.va.gov


