ABSTRACT
Background: Adolescents are at high risk of sexual assault compared to any other age group. The pattern of post-traumatic stress symptoms plus life-impairing disturbances in self-organization (emotion dysregulation, negative self-concept and interpersonal problems) is termed Complex Post-Traumatic Stress Disorder (CPTSD). Research about CPTSD after sexual assault in adolescents is limited owing to the challenges associated with assessing this group. This study aims to determine the frequency and structure of CPTSD, and the relationship of emotion dysregulation with impairment and additional trauma exposure among adolescents who have been sexually assaulted.
Method: Prospective cohort study of adolescents attending the Sexual Assault Referral Centres serving London over a 2-year period. We conducted cross-sectional analyses (n = 99) on data collected 4–5 months after sexual assault, and Confirmatory Factor Analyses (CFA) and Latent Class Analyses (LCA) to determine the CPTSD profile. CTPSD was defined according to the ICD-11, selecting symptom indicators from the following measures: Strengths and Difficulties Questionnaire (SDQ), Children’s Revised Impact of Event Scale (CRIES-13), Short version of the Mood and Feelings Questionnaire (S-MFQ), The Development and Well-Being Assessment (DAWBA). We analysed the association of CPTSD symptom domains with impairment (measured with the SDQ, and the Children’s Global Assessment Scale; C-GAS) and with additional trauma exposure.
Results: The frequency of ICD-11 PTSD was 59%, and of ICD-11 CPTSD was 40%. CPTSD symptoms showed a strong fit for a correlated 4-factor model, and LCA distinguished a class of participants with high levels of CPTSD symptoms. Emotion dysregulation was associated with impairment in functioning and exposure to trauma beyond other self-organization disturbances and core PTSD symptoms.
Conclusions: Disturbances in self-organization are frequent in sexually assaulted adolescents, and emotion dysregulation is associated with impairment and further exposure to trauma. Emotion dysregulation should be considered in preventive and treatment strategies for these vulnerable youth.
KEYWORDS: Complex PTSD, emotion dysregulation, adolescents, LCA, CFA
HIGHLIGHTS: • CPTSD is common in early stages after sexual assault in adolescents. • Emotion dysregulation is associated with further exposure to trauma and impairment. • Clinicians should systematically assess for CPTSD and plan prevention and treatment strategies accordingly.
Antecedentes: Las adolescentes presentan mayor riesgo de abuso sexual comparadas con cualquier otro grupo de edad. El patrón de síntomas de estrés postraumáticos sumados a las perturbaciones incapacitantes en la autoorganización (desregulación emocional, autoconcepto negativo, y problemas interpersonales) recibe el nombre de trastorno de estrés postraumático complejo (TEPT-C). Las investigaciones en TEPT-C luego de un abuso sexual en adolescentes es limitado dados los desafíos asociados a la evaluación de este grupo. El presente estudio busca determinar la frecuencia y estructura del TEPT-C, y la relación entre la desregulación emocional con deterioro y con exposición a traumas adicionales en mujeres adolescentes en quienes se haya cometido abuso sexual.
Métodos: Se realizó un estudio prospectivo de cohortes en adolescentes que acudían a los Centros de Referencia por Abuso Sexual que operan en Londres, durante un periodo de dos años. Condujimos análisis transversales (n = 99) en la información recolectada cuatro a cinco meses después del abuso sexual, además de Análisis Factoriales de Confirmación (AFC) y Análisis de Clases Latentes (ACL) para determinar el perfil del TEPT-C. Se definió al TEPT-C según la CIE-11, seleccionando indicadores de los síntomas a partir de las mediciones siguientes: Cuestionario de Fortalezas y Debilidades (SDQ, por sus siglas en inglés), Escala de Impacto del Evento Revisado para Niños (CRIES-13, por sus siglas en inglés), la Versión Abreviada del Cuestionario de Ánimo y Emociones (S-MFQ, por sus siglas en inglés), la Evaluación del Desarrollo y Bienestar (DAWBA, por sus siglas en inglés). Analizamos la asociación de los dominios de síntomas del TEPT-C con deterioro (medido en la SDQ, y con la Escala de Evaluación Global Infantil; C-GAS, por sus siglas en inglés), y con exposición a traumas adicionales.
Resultados: La frecuencia del Trastorno de Estrés Postraumático (TEPT) según la CIE-11 fue de 59%, y de TEPT-C según la CIE-11 fue de 40%. Los síntomas de TEPT-C mostraron un ajuste alto con un modelo correlacionado de cuatro factores, y el ACL distinguió una clase de participantes con alto niveles de síntomas del TEPT-C. El deterioro en el funcionamiento y la exposición a traumas posteriores asociados con la desregulación emocional fueron más allá de las perturbaciones en la autorregulación y en los síntomas nucleares del TEPT.
Conclusiones: Las perturbaciones en la autoorganización son frecuentes en adolescentes en quienes se ha cometido un abuso sexual, y la desregulación emocional está asociada con deterioro y con exposición posterior a trauma. La desregulación emocional debería ser considerada en estrategias de prevención y tratamiento para estas jóvenes vulnerables.
PALABRAS CLAVE: TEPT, TEPT-C, abuso sexual, desregulación emocional, adolescentes, AFC, ACL
背景:与其他年龄段相比,青少遭遇性侵犯风险较高。创伤后应激障碍加上影响生活的自我组织障碍(即情绪失调,负面的自我概念和人际关系问题)的模式被称为复杂型创伤后应激障碍(CPTSD)。由于对该人群进行评估存在一定挑战,关于青少年在性侵犯后引发CPTSD的研究非常有限。本研究旨在确定CPTSD的发病频率和结构,以及性侵犯后青少年的情绪失调与功能障碍和附加创伤暴露的关系。
方法:这项前瞻性队列研究对在伦敦性侵犯转诊中心的青少年进行了为期两年的研究。我们对性侵犯后4–5个月收集的数据进行了横断分析(n = 99),并通过验证性因子分析(CFA)和潜在类别分析(LCA)来确定CPTSD剖面分类。 CTPSD是根据ICD-11定义的,并从以下指标中选择症状指标:优势和困难问卷(SDQ),儿童事件影响量表修订版(CRIES-13),情绪和感受问卷简版(S-MFQ) ),发展与幸福感评估工具(DAWBA)。我们分析了CPTSD症状领域与功能损伤(通过SDQ和儿童整体评估量表( C-GAS)进行测量)和附加创伤暴露之间的关联。
结果:ICD-11 PTSD的发生率为59%,ICD-11 CPTSD的发生率为40%。 CPTSD症状显示出和一个相互关联的四因素模型非常高的拟合性,并且LCA区分出一类具有高CPTSD症状的被试。和其它自我组织障碍和PTSD核心症状相比,情绪失调与功能损伤和附加创伤暴露的关联性更强。
结论:性侵犯后,青少年中经常出现自我组织障碍,尤其是情绪失调与功能损伤和附加创伤暴露相关。在这些高易感性青少年的预防和治疗措施中,应考虑情绪失调的影响。
关键字: PTSD, 复杂型PTSD, 性侵犯, 情绪失调, 青少年, LCA, CFA
1. Background
It has long been recognized that severe interpersonal trauma may disrupt capacities in self-organization as well as triggering core post-traumatic symptoms (i.e. re-experiencing traumatic memories, cognitive and behavioural avoidance of traumatic reminders, and a persistent sense of threat). Disturbances in self-organization can be present in the absence of trauma-related cues, and include three symptom domains: (1) emotion dysregulation (i.e. heightened emotional reactivity, under controlled anger, irritability, temper outbursts), (2) negative self-concept (i.e. beliefs about oneself as diminished, defeated or worthless), and (3) interpersonal problems (i.e. persistent preoccupation or avoidance of social engagement, difficulties in sustaining relationships). This symptom profile, including core PTSD symptoms and disturbances in self-organization, has been codified as a new construct named Complex Post-Traumatic Stress Disorder (CPTSD) in the recently published 11th version of the International Classification of Diseases (ICD-11).
Describing new diagnostic categories has a direct impact on clinical practice, as it implies recognizing the existence of distinct aetiological pathways, course, treatment response and prognosis. It is therefore clinically important to validate new diagnostic categories empirically. For this, an effective tool to operationalize diagnostic constructs is of major importance, and only very recently a disorder-specific measure for PTSD and CPTSD has been developed and validated in adult survivours (Cloitre et al., 2018; Karatzias et al., 2017). In the last two decades, many investigations of trauma-related sequalae have used Confirmatory Factor Analyses (CFA) and Latent Class Analysis (LCA), and several possible CPTSD models have received empirical support (Cloitre, Garvert, Brewin, Bryant, & Maercker, 2013; Hyland et al., 2016; Knefel, Garvert, Cloitre, & Lueger-Schuster, 2015), with preliminary evidence suggesting that PTSD and CPTSD constructs could be distinguished (Hyland et al., 2017). However, data on adolescents are limited (Perkonigg et al., 2016; Sachser, Keller, & Goldbeck, 2017).
The degree to which disturbances in self-organization may affect survivors’ lives to a greater extent than core PTSD features is of clinical relevance. Empirical data suggests that patients with CPTSD symptoms have greater functional impairment than those with PTSD alone (Brewin et al., 2017; Cloitre et al., 2013; Karatzias et al., 2017; Zerach, Shevlin, Cloitre, & Solomon, 2019), and emotion dysregulation has been highlighted as the most significant contributor to survivors’ impairment (Cloitre et al., 2011; Cloitre, Miranda, Stovall-McClough, & Han, 2005). However, the impact attributable to each dimension of self-organization symptoms, over and above core PTSD symptoms, needs to be determined.
Last but not least, survivors of sexual trauma are at risk for further exposure to sexual assault (Walsh et al., 2012), and understanding the possible mechanisms underlying this cycle is a priority. It is crucial for treatment and preventive strategies to better understand post-assault factors that may impair, not only the daily functioning of survivors of sexual assault but also their ability to respond self-protectively in potentially threatening new situations. Cross-sectional data suggest that the use of unhelpful emotional regulation strategies could be one mediating factor between childhood sexual abuse and adult exposure to sexual trauma (Messman-Moore, Walsh, & DiLillo, 2010). Also, longitudinal studies on undergraduate survivors of rape have highlighted emotional dysregulation as a prospective predictor of further exposure to sexual trauma within the first 2–8 months of the trauma aftermath (Messman-Moore, Brown, & Koelsch, 2005; Messman-Moore, Ward, & Zerubavel, 2013). However, these studies included university student only, and results cannot be generalized to traumatized youth that are treated in clinical services. For these patients, the relationship of emotional dysregulation and further exposure to trauma in the first months of a sexual trauma is still unclear.
Undertaking investigations in the acute aftermath of a sexual trauma poses practical and ethical challenges (e.g. the need to give young people adequate time to consent; recruitment of young people who wish to participate without their parents’ knowledge; participants’ disclosure of previous or ongoing abusive situations; the potential requirement to activate safeguarding procedures; and the potential impact on judicial processes). Studies focusing on these early stages are therefore very limited, with no available data on emotion dysregulation or CPTSD in these young survivors. Here we report on a hard-to-ascertain sample of adolescents who sought help soon after a sexual assault. We examine difficulties in self-organization and core PTSD symptoms, with the following aims:
First, we wanted to determine the frequency of CPTSD and each of its symptom domains during the first months after adolescent sexual trauma. In keeping with previous results we expected to find high rates of CPTSD, and in particular of emotion dysregulation.
Second, we aimed to determine empirically the multivariate structure of CPTSD symptoms in our sample of sexually assaulted adolescents. For this, we used CFA to compare competing CPTSD models of symptom structure. We also aimed to determine if there was empirical evidence showing that certain symptoms aggregate in individuals at above-chance levels to form distinct post-traumatic syndromal patterns of PTSD and CPTSD. For this, we used latent class analysis (LCA), which posits that a heterogeneous group of patients can be reduced to several homogeneous subgroups with similar patterns of symptom endorsement. Informed by previous data, we predicted that there would be a distinct group of survivors likely to report difficulties in both self-organization and core PTSD symptoms (i.e. CPTSD).
Finally, we aimed to determine the association of self-organization disturbances, and particularly of emotion dysregulation, with impairment in adolescents’ functioning and with the extent of further exposure to trauma after experiencing a sexual assault.
2. Method
2.1. Participants
The sample is from a prospective observational cohort study (Khadr et al., 2018) of adolescents who sought help, after a sexual assault, from any of the three Sexual Assault Referral Centres (SARCs) serving London. Adolescents aged 13–17 years attending during April 2013–2015 were invited to participate. Non-English speakers and adolescents with learning disabilities were eligible. Sexual assault was defined as any reported sexual act without consent, or where the young person was not deemed competent to give consent, or where the young person was not sure about what happened due to the effects of drugs. Participants received a baseline assessment within the first 6 weeks post-assault (T0) and a follow-up assessment at 4–5 months post-assault (T1). For the purposes of this study, we used cross-sectional data collected at T1.
During the recruitment period, 491 adolescents were eligible. Of these, 141 (29%) consented to participate and completed the T0 assessment, and 106 (75%) completed the T1 follow-up assessment. In view of the small number of males recruited, we selected female participants only, leaving a final sample of 134 at T0 and 99 at T1. The mean age at sexual assault was 15.6 years (SD = 1.3) and just over half of the sample was of white ethnicity (51%). Sixty-nine participants (51%) had received mental health help in the year before the assault, and almost a third (32%) reported past sexual abuse or assault. Most assaults involved vaginal, oral and/or anal rape (92%) and the assailant was a stranger in 37% of cases. More detailed information about the characteristics of the sample and ethical approval are reported elsewhere (Khadr et al., 2018).
2.2. Measures
2.2.1. Complex PTSD diagnosis
As defined in the ICD-11, meeting diagnostic criteria for CPTSD required at least one symptom of re-experiencing, avoidance and over-arousal, in addition to at least one symptom of emotion dysregulation, negative self-concept and interpersonal problems. Unfortunately, the newly developed instrument to measure this construct, called the International Trauma Questionnaire (ITQ) (Cloitre et al., 2018), was not available at the time of our study design. Therefore, we followed previous literature to select the set of symptom indicators that were deemed to best represent the ICD-11 definition of CPTSD (Maercker et al., 2013), focused on a limited but central group of symptoms. To determine a probable CPTSD diagnosis, a total of 18 items from four different measures collected at T1 were used (Table 1): Strengths and Difficulties Questionnaire (SDQ) (Goodman, Ford, Simmons, Gatward, & Meltzer, 2003), Children’s Revised Impact of Event Scale (CRIES-13) (Perrin, Meiser-Stedman, & Smith, 2005), Short version of the Mood and Feelings Questionnaire (S-MFQ) (Angold, Costello, Messer, & Pickles, 1995), The Development and Well-Being Assessment (DAWBA) (Goodman, Ford, Richards, Gatward, & Meltzer, 2000).
Table 1.
Items used to represent the symptoms of Post-Traumatic Stress Disorder (PTSD) and Complex Post-Traumatic Stress Disorder (CPTSD) according to ICD-11: proposed symptom indicators for CPTSD.
| Factors | Test items | Measures |
|---|---|---|
| Core PTSD symptoms | Intrusion: | |
| (x1) Since the incident that brought you to the sexual assault referral centre, have you experienced flashbacks? | Proforma | |
| (x2) Have you had a lot of upsetting dreams of the event? | DAWBA | |
| Avoidance: | ||
| (x3) Do you try not to think about it? | CRIES-13 | |
| (x4) Do you stay away from reminders (i.e. places or situations)? | CRIES-13 | |
| Sense of threat: | ||
| (x5) Are you alert and watchful even when there is no obvious need to be? | CRIES-13 | |
| (x6) Do you startle more easily or feel more nervous? | CRIES-13 | |
| Emotion dysregulation | (x7) Do you get easily irritable? | CRIES-13 |
| (x8) I get very angry and often lose my temper | SDQ | |
| (x9) Do you have marked or rapid mood changes? | DAWBA | |
| negative self-concept | (x10) I felt I was no good any more | S-MFQ |
| (x11) I hated myself | S-MFQ | |
| (x12) I was a bad person | S-MFQ | |
| (x13) I thought nobody really loved me | S-MFQ | |
| Interpersonal problems | (x14) I have one good friend or more | SDQ |
| (x15) Other people my age generally like me | SDQ | |
| (x16) Are you really proud of being good with friends? | DAWBA | |
| (x17) I am usually on my own. I generally play alone or keep to myself | SDQ | |
| (x18) Overall, do you particularly fear or avoid social situations that involve a lot of people, meeting new people or doing things in front of other people? | DAWBA |
Abbreviations: ICD = International Classification of Diseases; SDQ = Strengths and Difficulties Questionnaire; CRIES-13 = Children’s Revised Impact of Event Scale; S-MFQ = Short version of the Mood and Feelings Questionnaire; DAWBA = The Development and Well-Being Assessment.
2.2.2. Further exposure to trauma
At T1 participants were asked two questions (from a proforma) to determine if they had been exposed to any further trauma since the incident for which they sought help. They were asked to answer dichotomously (yes, no) and to provide details about (1) any abuse or assault, and (2) whether they had experienced any sexual contact without their consent.
2.2.3. Impairment
Self-reported impairment was measured at T1 using the impact score of the SDQ (Goodman, 1999). Clinician-rated impairment was assessed at T1 using the Children’s Global Assessment Scale (C-GAS) (Shaffer et al., 1983). Clinicians, who were blind to the nature of the assault, rated the CGAS based on symptoms reported at T1 by the participants in a structured diagnostic interview of DSM-IV Psychiatric Disorders (DAWBA).
2.3. Statistical analyses
2.3.1. Descriptive and frequency estimations
We used STATA (version 13.0) to estimate the frequency of CPTSD along with the proportion of individuals meeting criteria for each diagnostic criterion. For this, we needed to determine if patients endorsed each CPTSD item (yes/no). For items with more than two response options, we imposed a simple dichotomy (presence/absence of impairment) using a cut-off score determined by their SDQ and CGAS scores. For instance, for a CPTSD item with five response options, we used one-way ANOVA to compare the five CPTSD groups in terms of their SDQ scores. This is followed by post-hoc comparisons (with bonferroni correction) to help determine an optimal way to regroup the five CPTSD groups of individuals into just two (i.e. impaired or not).
These descriptive data correspond to a subsample of 63 participants with full T1 data for all CPTSD diagnostic criterion.
2.3.2. Confirmatory factor and regression analyses
We aimed to clarify the CPTSD multidimensional structure and examine the internal and external validity of the construct. CFA was conducted in Mplus 7.0 (Muthén & Muthén, 2012) using weighted least-squares means and variances adjusted (WLSMV) estimator with delta parameterization because of categorical indicators. We compared three nested models (Figure 1): a unidimensional 1-factor model for CPTSD and two multidimensional models; a first-order model with four factors (i.e. core PTSD, emotion dysregulation, negative self-concept, interpersonal problems) and a second-order model for CPTSD as an overriding construct subtended by four factors (factors as per first-order model). We compared the most parsimonious models (i.e. first-order model) with increasingly complex models, which would represent the existence of an overriding construct (i.e. second-order model). This sequence of model comparison helps to guard against overfitting to the sample data, which would undermine the generalizability of our model results. We did not expect a unidimensional model to fit our data (Wolf et al., 2015) (model a of Figure 1). We expected to find a good fit for both multidimensional models (Cloitre et al., 2013; Knefel et al., 2015), representing either the co-occurrence of self-organization disturbances with core PTSD symptoms (first order, model b of Figure 1) or the existence of a unitary higher-order CPTSD construct (second order, model c of Figure 1). We further examined a bifactor model (see Online Resource, Figure S1), which similarly to a second-order model recognizes the existence of an overriding general factor (i.e. CPTSD), alongside the co-occurrence of specific sub-constructs (i.e. self-organization disturbances and core PTSD). We report technical details of model fit evaluation in the supplementary material.
Figure 1.
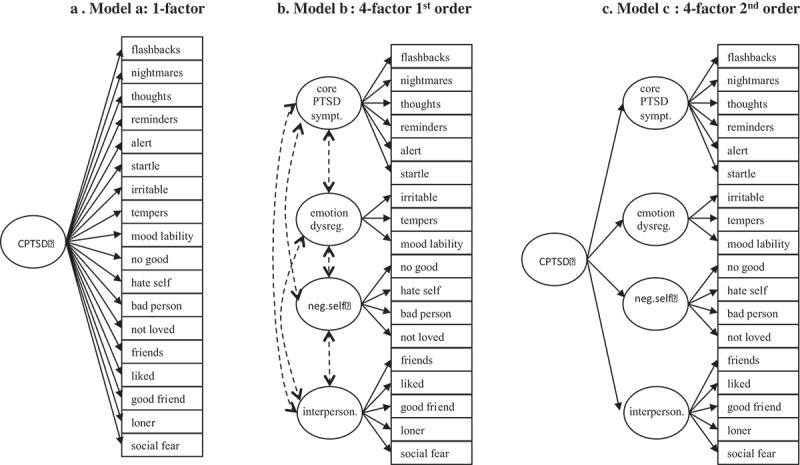
Alternative models of the symptom structure of Complex Post-Traumatic Stress Disorder (CPTSD) and symptoms of emotion dysregulation, negative self-concept and interpersonal problems.
In order to analyse the association of each of the CPTSD domains from the CFA model results (i.e. post-traumatic stress symptoms, emotion dysregulation, negative self-concept and interpersonal problems) with impairment, we entered into the model external observed variables as outcomes (SDQ and C-GAS impairment scores) and computed a regression path with the four factors as predictor variables. Further exposure to trauma was also introduced as an outcome variable.
1.3.3. Latent class analyses
Latent Class Analyses (LCA) was used to identify groups of participants with different symptom patterns in relation to self-organization disturbances and core PTSD symptoms. LCA analyses were conducted in Mplus 7.0 (Muthén & Muthén, 2012). The 18 items used in the CFA were also used in the LCA, but coded dichotomously as present or not. The LCA models were estimated using robust maximum likelihood method with 500 initial stage random starts and 80 final stage optimizations to determine if the best log-likelihood value was obtained and replicated. LCA models with one-class solution were first estimated assuming the presence of only one type of symptom profile. An increasing number of classes were estimated to see if they improve model predictions of the observed data. Improvement in model fit was evaluated based on multiple criteria outlined by Wang and Wang (2012). Smaller values of Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), sample size-adjusted BIC (aBIC) indicate better fit. Bootstrapping was conducted to see if improvement in model fit were statistically significant. This would be indicated by p-values smaller than 0.05 for the Lo-Mendell-Rueben Likelihood Ratio Test (LMR LR), adjusted for model degrees of freedom and sample size (aLMR LR), as well as the Bootstrap Likelihood Ratio Test (BLRT). Besides model fit, good classification would be indicated by entropy values that are 0.8 or higher (Clark, 2010) and probability of correct class assignment should be 0.7 or higher (Nagin, 2005). We also examined the interpretability of latent classes, especially when they included only less than 5% of all respondents.
3. Results
3.1. Frequency estimates of CPTSD
According to ICD-11 definitions, N = 37 (59%) met criteria for PTSD, and N = 25 (40%) met criteria for CPTSD. N = 38 (60%) reported at least one symptom of self-organization in each of the three domains [N = 55 (87%) emotion dysregulation, N = 47 (75%) negative self-concept and N = 47 (75%) interpersonal problems]. (see Online Resource, Figure S2).
3.2. Confirmatory factor analyses
As shown in Table 2, the uni-dimensional model did not have an acceptable fit to the data. The results of the bifactor model CFA showed that out of the 18 items, six did not load significantly to the general factor, nor another three into their specific sub-constructs.
Table 2.
Fit indices and model comparison of Complex Post-Traumatic Stress Disorder (CPTSD) competing models.
| CPTSD models | X2 | df | p | CFI | TLI | RMSEA | nested models | ΔX2 | Δdf | p |
|---|---|---|---|---|---|---|---|---|---|---|
| (a) 1-factor 1st order | 266.318 | 135 | 0 | .845 | .824 | .097 | ||||
| (b) 4-factor 1st order | 164.293 | 129 | .0195 | .958 | .951 | .052 | ||||
| (c) 4-factor 2nd order | 172.649 | 131 | .009 | .951 | .943 | .056 | b) vs c) | 7.07 | 2 | .029 |
Abbreviations: CFI = comparative fit index; TLI = Tucker–Lewis index; RMSEA = root-mean-square error of approximation.
The 4-factor first- and second-order models both had an excellent fit (CFI = .958, .951/TLI = .951, .943/RMSEA = .052, .056, respectively). When comparing these first- and second-order models, the former showed significantly better fit (Δx2 = 7.07, Δdf = 2, p = .0029). This model represents self-organization disturbances as being correlated with core PTSD symptoms at the same level, as it would be the case of many co-morbid disorders (i.e. tic disorders co-occurring with ADHD and OCD) (Huisman-van Dijk, Van de Schoot, Rijkeboer, Mathews, & Cath, 2016).
In the 4-factor first-order model, which showed the optimal balance between model fit and interpretability, all 18 items loaded significantly (standardized factor loadings ranging between .39-.96) on their target factor (see Online Resource, Table S1) and all 4-factors showed moderate-strong correlations with one another (see Online Resource, Table S2).
3.3. Latent class analyses
LCA analyses revealed that the survivors could be differentiated into two classes according to the presence of core PTSD symptoms, emotion dysregulation, negative self-concept and interpersonal problems (see Online Resource, Table S3). As shown in Figure 2, participants from Class 1 (43%) presented high levels of PTSD symptoms, emotion dysregulation, negative self-concept and interpersonal problems (i.e. CPTSD symptom profile). Participants from Class 2 (57%) presented lower levels of core PTSD and emotion dysregulation symptoms, and similar levels of interpersonal problems, but did not present difficulties in negative self-concept. There was not a healthy group with low levels in all symptom domains.
Figure 2.
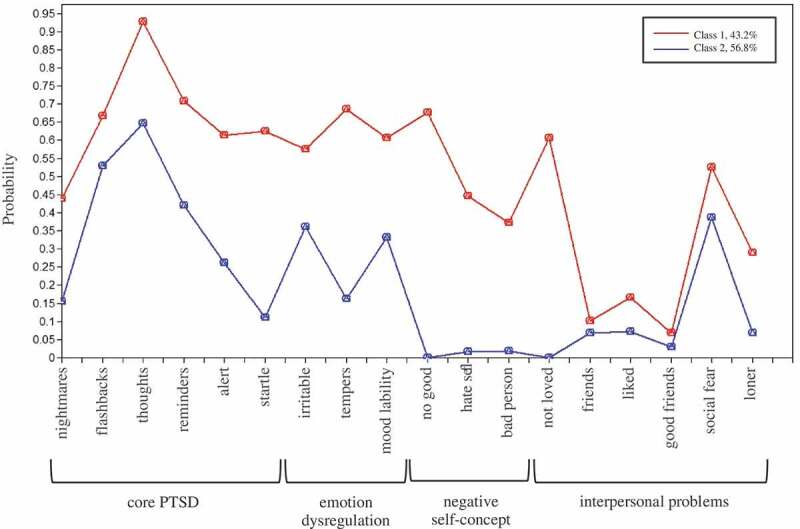
Symptom endorsement of complex PTSD (Post-Traumatic Stress Disorder) by class.
3.4. Association of emotion dysregulation with impairment and further trauma exposure
The 4-factor first-order model showed the best fit and therefore was used for cross-sectional regression analyses at 4–5 months after sexual assault (T1).
As shown in Table 3, emotion dysregulation was significantly associated with impairment rated by clinicians (C-GAS score) and rated by the participants (SDQ impairment score), over and above core PTSD symptoms, and the other self-organization disturbances.
Table 3.
Regression analyses where the 4 CPTSD (Complex Post-Traumatic Stress Disorder) factors are used as independent variables predicting impairment rated by the victims (SDQ), impairment rated by clinicians (CGAS), and further trauma exposure during the 4–5 months post-sexual assault.
| SDQ impairment |
CGAS impairment |
any further trauma exposure |
further sexual trauma exposure |
|||||
|---|---|---|---|---|---|---|---|---|
| predictor variables | β (SE) | p [95% CI] | B (SE) | p [95% CI] | B (SE) | p [95% CI] | B (SE) | p [95% CI] |
| Core PTSD symptoms | .12 (.15) | .438 [−0.56, 1.28] | .08 (.15) | .606 [−4.91, 2.86] | −.57(.28) | .040* | −.56(.32) | .078 |
| Emotion dsyregulation | .49 (.16) | .002 [0.49, 2.52]** | .54 (.14) | <.001 [−11.14, −3]** | .84(.28) | .002** | .70(.32) | .030* |
| Negative self-concept | .03 (.14) | .832 [−0.73, 0.91] | .18 (.14) | .203 [−6.09, 1.3] | −.16(.24) | .491 | −.13(.30) | .681 |
| Interpersonal problems | .20 (.12) | .083 [−1.38, 0.12] | .08 (.13) | .511 [−2.16, −4.36] | −.34(.22) | .119 | .58(.30) | .054 |
Abbreviations: β = standardized coefficients; SE = standard error; CI = confidence interval; SDQ = Strengths and Difficulties Questionnaire; CGAS = Children’s Global Assessment Scale.
*p < .05, **p < .005
At first follow up (T1), 29 out of 99 participants reported suffering any type of physical, sexual or psychological abuse between T0 and T1 (any further trauma exposure), and 9 out of the 99 (9%) reported suffering a new sexual trauma between T0 and T1 (further sexual trauma exposure). Emotion dysregulation was significantly associated with further exposure to general and to sexual trauma above and beyond core PTSD symptoms, negative self-concept and interpersonal problems (Table 3).
4. Discussion
Previous research on adult survivors of interpersonal trauma has provided compelling evidence of the relevance of a meaningful triad of symptoms characterized by emotion dysregulation, negative self-concept and interpersonal problems. In this study we aimed to: determine if adolescents also commonly reported these symptoms during the aftermath of a sexual trauma; clarify the symptom structure of disturbances in self-organization in relation to core PTSD symptoms; and examine the association of self-organization disturbances with impairment in functioning and further exposure to trauma. Firstly, in keeping with previous empirical data in adults and youth (Cloitre et al., 2011; Perkonigg et al., 2016; Wolf et al., 2015) we found high rates of all self-organization disturbances, probably suggesting an overlap between the three domains. Overall, 40% met criteria for CPTSD in our adolescent sample. These results are in keeping with the high CPTSD rates (32.8% to 42.8%) found in adults assessed in trauma clinics (Hyland et al., 2016; Karatzias et al., 2017; Nickerson et al., 2016), and are consistent with the theoretical basis that severe interpersonal trauma in young people increases likelihood of self-organizational disturbances. Also, the frequency of probable ICD-11 PTSD that we found in our sample (59%) was similar to the rates reported during the acute aftermath in sexually traumatized youth (Darves-Bornoz et al., 1998; Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992). In our study, PTSD rates were above CPTSD rates, while the latest evidence suggests that CPTSD is a more commonly observed condition than PTSD in clinical samples (Karatzias et al., 2017). One possible explanation for these results could be that our data was collected during the acute phase after the sexual trauma, when core PTSD symptoms are expected to be particularly salient, while most data in the literature are collected time after trauma exposure. Also, Our ICD-11 estimation of PTSD was slightly higher than the one found using DSM-IV criteria in the same study sample (48.2%) (Khadr et al., 2018). This is in keeping with recent findings in adolescent samples (Sachser et al., 2017) and is not surprising given the narrow definition used by the ICD approach, which directs clinicians’ attention to a simplified PTSD diagnosis.
Secondly, we aimed to test a number of plausible structural models of the latent structure of self-organization difficulties in young people after a sexual trauma. The question was whether CPTSD was a unidimensional construct (i.e. 1-factor model), whether it was formed by correlated symptom dimensions of core PTSD, emotion dysregulation, negative self-concept and interpersonal problems (i.e. first-order model) or whether these four dimensions were part of a unitary underlying CPTSD liability (i.e. second-order model). Our findings convincingly support a multidimensional nature, as the 4-factors were well represented in the first-order model (model b of Figure 1) and also in the second-order model (model c of Figure 1), with all symptoms significantly loading and with a good fit of the data in both cases. However, when statistically comparing both models, the first-order model was a better fit. These results suggest that emotion dysregulation, negative self-concept, interpersonal problems and core PTSD symptoms represent moderately correlated dimensions in traumatized adolescents, and an underlying CPTSD construct would not better explain their co-occurrence during the first months after a sexual traumatic event. This is the first study that assesses the dimensional structure of self-organization disturbances and core PTSD using bifactor modelling. Several relational items did not load significantly into the general factor (CPTSD). The use of bifactor models in future studies may support researchers in examining to what extent measured difficulties in self-organization are explained by the post-traumatic reaction.
Once the co-occurrence of self-organization disturbances and core PTSD symptoms was confirmed in a variable-centred approach (CFA), we wanted to describe in a person-centred approach (LCA) whether this clinical presentation was endorsed by a subgroup of adolescents. Results showed that soon after sexual assault there were two distinct classes of participants with those from Class 1 being more likely to present symptoms of core PTSD and self-organization disturbances (i.e. CPTSD). Participants from Class 2 presented lower levels of core PTSD and emotion dysregulation symptoms, and similar levels of interpersonal problems, but did not present difficulties in negative self-concept. These results are consistent with past literature (Cloitre et al., 2013; Perkonigg et al., 2016) describing a subgroup of young individuals likely to endorse the CPTSD symptom profile, with a high probability of core PTSD symptoms and disturbances in the three self-organization domains (Class 1). However, instead of differentiating a second distinct group of survivors with only core PTSD symptoms, results showed a subgroup of adolescents likely to report emotion dysregulation difficulties alongside core PTSD. These results should be interpreted in view of the particularities of our study sample, as emotion regulation difficulties are expected to be present in normative developing adolescents to some degree, and impairing symptoms can be particularly frequent in adolescent females (Stringaris & Goodman, 2009). Also, given the acuteness and severity of the trauma in this particular help-seeking sample, and the lack of similar previous studies, we speculate that some degree of difficulties in regulating the emotions would be expected in an acute period. Indeed, in contrast to findings from trauma-exposed adolescents in the community (Perkonigg et al., 2016), there was no group with a low probability of symptoms. Consistent with our results, studies that evaluate clinical participants have found two or three classes, with no resilient group being present in many cases.
Finally, as hypothesized, emotion dysregulation was cross-sectionally associated with impairment beyond other self-organization and core PTSD symptoms. These results are in keeping with epidemiological studies that highlighted the particular role of emotion dysregulation (as defined as in our study) in explaining young people’s impairment (Stringaris & Goodman, 2009). Also, consistent with past literature, difficulties in emotion dysregulation were independently associated with further exposure to trauma during the first 4–5months after a sexual trauma. As both variables were measured cross-sectionally at T1 one cannot infer whether difficulties in emotion regulation were present before traumatic experiences, are a consequence of these repeated events or both. The association between emotion dysregulation and further exposure to trauma is consistent with previous findings that repeated exposure to trauma leads to emotion dysregulation, and with the hypothesis that emotion dysregulation may lead to further exposure. Our study design does not allow us to determine the direction of causality. Indeed, it is plausible that this relationship is bidirectional.
The results of this study should be interpreted in view of several limitations. First of all, we did not carry out diagnostic interviews to determine diagnosis. A clinician-administered diagnostic interview for PTSD and CPTSD is currently under development (Karatzias et al., 2017), and once available, it will be a critical element for the assessment of the validity of these ICD – 11 diagnoses. Also, there was no validated measure for CPTSD symptoms at the time of the study design, and we used items of different validated measures that appeared to be valid representations of the ICD-11 proposed CPTSD symptoms. This method could affect the validity and reliability of the results, as one cannot ascertain if the tool employed actually measures the intended construct or if it provides stable or consistent responses, limiting its reproducibility. Thus, it is hard to know to which extent the results of this study are restricted to the performance of the items used, or they are more broadly representations of the CPTSD construct. However, psychometric assessments of disturbances in self-organization have showed that several potential symptom indicators of the ICD-11 CPTSD can be used interchangeably (Shevlin et al., 2018).
Secondly, results should be interpreted with caution given that we did not have a large sample size. It is of note that a minimum sample size acceptable for structural analysis has not been determined. Simulation studies support that sample size requirements in LCA depends on many factors (Park & Yu, 2018), and having more (rather than fewer) high-quality indicators can compensate for small sample size (Wurpts & Geiser, 2014). It is also of note that this is a very unique sample, partially due to ethical complexities when undertaking studies with such severely and acutely traumatized young people. Longitudinal studies involving adults exposed to sexual assault report recruitment rates that are usually below 45% (Campbell, Sprague, Cottrill, & Sullivan, 2011). Our recruitment (29%) and retention (75%) rates were within the expected range. Thirdly, the results refer to those female adolescents that seek clinical help after being sexually assaulted and therefore cannot be generalized to other traumatized populations. Finally, we used data collected cross-sectionally at T1, and so causality inferences cannot be drawn.
5. Conclusion
Traumatized young people with disturbances in self-organization, and particularly with emotion dysregulation, deserve researchers’ and clinicians’ attention. These problems are very common in sexually assaulted adolescents soon after the trauma, and are accompanied with impairment and risk of chronic exposure to trauma. They should be considered by attending clinicians who encounter these young individuals in the early stages after trauma, in order to systematically assess for disturbances in self-organization, and plan prevention and treatment plans accordingly. Clinicians might face a lack of guidance in regard to the best approach to tackle these relevant symptoms in youth. While some data suggest an improvement of CPTSD symptoms with first-line treatments for PTSD (i.e. Trauma-focused Cognitive Behavioural Therapy) (Betancourt et al., 2014) (Sachser et al., 2017) it is notable that these patients still report significant symptoms at the end of the therapy (Sachser et al., 2017), and it is still unclear if sequentially designed interventions with an initial stabilization phase (Ford, Steinberg, Hawke, Levine, & Zhang, 2012) would enhance treatment outcomes. Further studies should determine if traumatized adolescents with disturbances in self-organization might require different forms of intervention than those with only core PTSD symptoms, and if interventions targeting emotion dysregulation in the first months after trauma would improve victims’ lives and reduce the risk for further traumatization.
Acknowledgments
L. Villalta was financially supported by the Alicia Koplowitz Foundation while working on this manuscript. We thank Prof. E. Garralda for her comments and suggestions throughout the project.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data of this article can be accessed here.
References
- Angold, A., Costello E., Messer, S. C., & Pickles, A. (1995). Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research, 5, 237–11. [Google Scholar]
- Betancourt, T. S., McBain, R., Newnham, E. A., Akinsulure-Smith, A. M., Brennan, R. T., Weisz, J. R., & Hansen, N. B. (2014, December 01). A behavioral intervention for war-affected youth in Sierra Leone: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 53(12), 1288–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin, C. R., Cloitre, M., Hyland, P., Shevlin, M., Maercker, A., Bryant, R. A., … Reed, G. M. (2017). A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clinical Psychology Review, 58, 1–15. [DOI] [PubMed] [Google Scholar]
- Campbell, R., Sprague, H. B., Cottrill, S., & Sullivan, C. M. (2011). Longitudinal research with sexual assault survivors: A methodological review. Journal of Interpersonal Violence, 26(3), 433–461. [DOI] [PubMed] [Google Scholar]
- Clark, S. L. (2010). Mixture modeling with behavioral data. Los Angeles, CA: University of California. [Google Scholar]
- Cloitre, M., Courtois, C. A., Charuvastra, A., Carapezza, R., Stolbach, B. C., & Green, B. L. (2011). Treatment of complex PTSD: Results of the ISTSS expert clinician survey on best practices. Journal of Traumatic Stress, 24(6), 615–627. [DOI] [PubMed] [Google Scholar]
- Cloitre, M., Garvert, D. W., Brewin, C. R., Bryant, R. A., & Maercker, A. (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. European Journal of Psychotraumatology, 4, 20706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre, M., Miranda, R., Stovall-McClough, K. C., & Han, H. (2005). Beyond PTSD: Emotion regulation and interpersonal problems as predictors of functional impairment in survivors of childhood abuse. Behavior Therapy, 36(2), 119–124. [Google Scholar]
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. [DOI] [PubMed] [Google Scholar]
- Darves-Bornoz, J. M., Lepine, J. P., Choquet, M., Berger, C., Degiovanni, A., & Gaillard, P. (1998). Predictive factors of chronic post-traumatic stress disorder in rape victims. European Psychiatry: The Journal of the Association of European Psychiatrists, 13(6), 281–287. [DOI] [PubMed] [Google Scholar]
- Ford, J. D., Steinberg, K. L., Hawke, J., Levine, J., & Zhang, W. (2012, January). Randomized trial comparison of emotion regulation and relational psychotherapies for PTSD with girls involved in delinquency. Journal of Clinical Child and Adolescent Psychology, 41(1), 27–37. [DOI] [PubMed] [Google Scholar]
- Goodman, R. (1999). The extended version of the strengths and difficulties questionnaire as a guide to child psychiatric caseness and consequent burden. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 40(5), 791–799. [PubMed] [Google Scholar]
- Goodman, R., Ford, T., Richards, H., Gatward, R., & Meltzer, H. (2000). The development and well-being assessment: Description and initial validation of an integrated assessment of child and adolescent psychopathology. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 41, 645–655. [PubMed] [Google Scholar]
- Goodman, R., Ford, T., Simmons, H., Gatward, R., & Meltzer, H. (2003). Using the strengths and difficulties questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. International Review of Psychiatry, 15(1–2), 166–172. [DOI] [PubMed] [Google Scholar]
- Huisman-van Dijk, H. M., Van de Schoot, R., Rijkeboer, M. M., Mathews, C. A., & Cath, D. C. (2016). The relationship between tics, OC, ADHD and autism symptoms: A cross- disorder symptom analysis in Gilles de la Tourette syndrome patients and family-members. Psychiatry Research, 237, 138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland, P., Murphy, J., Shevlin, M., Vallieres, F., McElroy, E., Elklit, A., … Cloitre, M. (2017). Variation in post-traumatic response: The role of trauma type in predicting ICD-11 PTSD and CPTSD symptoms. Social Psychiatry and Psychiatric Epidemiology, 52(6), 727–736. [DOI] [PubMed] [Google Scholar]
- Hyland, P., Shevlin, M., Elklit, A., Murphy, J., Vallières, F., Garvert, D. W., & Cloitre, M. (2016). An assessment of the construct validity of the ICD- 11 proposal for complex posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy. doi: 10.1037/tra0000114 [DOI] [PubMed] [Google Scholar]
- Wang, J, & Wang, X. (2012). Structural equation modeling: Applications using Mplus. Wiley Series in Probability and Statistics. [Google Scholar]
- Karatzias, T., Cloitre, M., Maercker, A., Kazlauskas, E., Shevlin, M., Hyland, P., … Brewin, C. R. (2017). PTSD and complex PTSD: ICD-11 updates on concept and measurement in the UK, USA, Germany and Lithuania. European Journal of Psychotraumatology, 8(sup7), 1418103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khadr, S., Clarke, V., Wellings, K., Villalta, L., Goddard, A., Welch, J., … Viner, R. (2018). Mental and sexual health outcomes following sexual assault in adolescents: A prospective cohort study. The Lancet Child & Adolescent Health, 2(9), 654–665. [DOI] [PubMed] [Google Scholar]
- Knefel, M., Garvert, D. W., Cloitre, M., & Lueger-Schuster, B. (2015). Update to an evaluation of ICD-11 PTSD and complex PTSD criteria in a sample of adult survivors of childhood institutional abuse by Knefel & Lueger-Schuster (2013): A latent profile analysis. European Journal of Psychotraumatology, 6, 25290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., Reed, G. M., van Ommeren, M., … Saxena, S. (2013). Proposals for mental disorders specifically associated with stress in the international classification of diseases-11. Lancet, 381(9878), 1683–1685. [DOI] [PubMed] [Google Scholar]
- Messman-Moore, T. L., Brown, A. L., & Koelsch, L. E. (2005). Posttraumatic symptoms and self-dysfunction as consequences and predictors of sexual revictimization. Journal of Traumatic Stress, 18(3), 253–261. [DOI] [PubMed] [Google Scholar]
- Messman-Moore, T. L., Walsh, K. L., & DiLillo, D. (2010). Emotion dysregulation and risky sexual behavior in revictimization. Child Abuse & Neglect, 34(12), 967–976. [DOI] [PubMed] [Google Scholar]
- Messman-Moore, T. L., Ward, R. M., & Zerubavel, N. (2013). The role of substance use and emotion dysregulation in predicting risk for incapacitated sexual revictimization in women: Results of a prospective investigation. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors, 27(1), 125–132. [DOI] [PubMed] [Google Scholar]
- Muthén, L. K., & Muthén, B. (2012). Mplus user’s guide (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nagin, D. (2005). Group-based modeling of development. Cambridge, MA: Harvard University Press. [Google Scholar]
- Nickerson, A., Cloitre, M., Bryant, R. A., Schnyder, U., Morina, N., & Schick, M. (2016). The factor structure of complex posttraumatic stress disorder in traumatized refugees. European Journal of Psychotraumatology, 7, 33253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, J., & Yu, H.-T. (2018). Recommendations on the sample sizes for multilevel latent class models. Educational and Psychological Measurement, 78(5), 737–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkonigg, A., Hofler, M., Cloitre, M., Wittchen, H. U., Trautmann, S., & Maercker, A. (2016). Evidence for two different ICD-11 posttraumatic stress disorders in a community sample of adolescents and young adults. European Archives of Psychiatry and Clinical Neuroscience, 266(4), 317–328. [DOI] [PubMed] [Google Scholar]
- Perrin, S., Meiser-Stedman, R., & Smith, P. (2005). The children’s revised impact of event scale (CRIES): Validity as a screening instrument for PTSD. Behavioural and Cognitive Psychotherapy, 33, 487–498. [Google Scholar]
- Rothbaum, B. O., Foa, E. B., Riggs, D. S., Murdock, T., & Walsh, W. (1992). A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress, 5(3), 455–475. [Google Scholar]
- Sachser, C., Keller, F., & Goldbeck, L. (2017). Complex PTSD as proposed for ICD-11: Validation of a new disorder in children and adolescents and their response to trauma-focused cognitive behavioral therapy. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 58(2), 160–168. [DOI] [PubMed] [Google Scholar]
- Shaffer, D., Gould, M. S., Brasic, J., Ambrosini, P., Fisher, P., Bird, H., & Aluwahlia S. (1983). A children’s global assessment scale (CGAS). Archives of General Psychiatry, 40(11), 1228–1231. [DOI] [PubMed] [Google Scholar]
- Shevlin, M., Hyland, P., Roberts, N. P., Bisson, J. I., Brewin, C. R., & Cloitre, M. (2018). A psychometric assessment of disturbances in self-organization symptom indicators for ICD-11 complex PTSD using the International Trauma Questionnaire. European Journal of Psychotraumatology, 9(1), 1419749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris, A., & Goodman, R. (2009). Mood lability and psychopathology in youth. Psychological Medicine, 39(8), 1237–1245. [DOI] [PubMed] [Google Scholar]
- Walsh, K., Danielson, C. K., McCauley, J. L., Saunders, B. E., Kilpatrick, D. G., & Resnick, H. S. (2012). National prevalence of posttraumatic stress disorder among sexually revictimized adolescent, college, and adult household-residing women. Archives of General Psychiatry, 69(9), 935–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf, E. J., Miller, M. W., Kilpatrick, D., Resnick, H. S., Badour, C. L., Marx, B. P., … Friedman, M. J. (2015). ICD-11 complex PTSD in US national and veteran samples: Prevalence and structural associations with PTSD. Clinical Psychological Science: A Journal of the Association for Psychological Science, 3(2), 215–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurpts, I. C., & Geiser, C. (2014). Is adding more indicators to a latent class analysis beneficial or detrimental? Results of a Monte-Carlo study. Frontiers in Psychology, 5(920). doi: 10.3389/fpsyg.2014.00920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zerach, G., Shevlin, M., Cloitre, M., & Solomon, Z. (2019). Complex posttraumatic stress disorder (CPTSD) following captivity: A 24-year longitudinal study. European Journal of Psychotraumatology, 10(1), 1616488. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


