ABSTRACT
Background: Results on the association between posttraumatic stress symptoms (PTSS) and posttraumatic growth (PTG) are inconsistent, and there may be unknown factors mediating or moderating this relationship. Identifying these factors could help in developing an intervention strategy for promoting PTG. However, few studies have examined relationships among PTSS, resilience, and PTG concurrently, and no study has investigated the effect of childhood trauma on these relationships in adulthood.
Objective: The aim of this study was to examine the moderated mediating effect of childhood trauma on resilience and its associations with PTSS and PTG in adult victims of traumatic accidents or crimes. We hypothesized that resilience would mediate relationships between PTSS and PTG and that its mediating effects would differ depending on childhood trauma.
Methods: We included adult victims of accidents or crimes referred to a university hospital or specialized support centre (n = 143). PTSS, resilience, childhood trauma, and PTG were measured with the following questionnaires: PTSD Checklist for DSM-5, Connor-Davidson Resilience Scale, Adverse Childhood Experiences Questionnaire, and the Short Form of the Posttraumatic Growth Inventory, respectively.
Results: The effect of PTSS on PTG was found to be fully mediated by resilience, and this mediating effect was moderated according to childhood trauma: the more childhood traumatic experiences, the greater the mediating effect of resilience was between PTSS and PTG. The effect of resilience on PTG was highest in the high childhood trauma group.
Conclusion: Therapists treating individuals with psychological trauma should attempt to identify a history of childhood trauma and to evaluate resilience. Therapeutic approaches tailored according thereto may improve PTG among individuals with PTSS symptoms, especially those with high levels of childhood trauma.
KEYWORDS: Posttraumatic stress, resilience, posttraumatic growth, childhood trauma
HIGHLIGHTS: • The effect of PTSS on PTG was fully mediated by resilience, and this mediating effect was moderated according to childhood trauma in adult accident or crime victims. • The more childhood trauma, the greater the mediating effect of resilience was between PTSS and PTG.
Antecedentes: Los resultados en la asociación entre síntomas de estrés postraumático (PTSS por sus siglas en inglés) y crecimiento postraumático (PTG por sus siglas en inglés) son inconsistentes, y pueden haber factores desconocidos mediando o moderando esta relación. Identificar estos factores pudiese ayudar en desarrollar una estrategia de intervención para promover el PTG. Sin embargo, pocos estudios han examinado las relaciones entre PTSS, resiliencia y PTG simultáneamente, y ningún estudio ha investigado el efecto del trauma infantil sobre estas relaciones en la adultez.
Objetivo: el objetivo de este estudio fue examinar los efectos moderados mediadores del trauma infantil en la resiliencia y su asociación con PTSS y PTG en víctimas adultas de crimen o de accidentes traumáticos. Hipotetizamos que la resiliencia mediaría las relaciones entre PTSS y PTG y que sus efectos mediadores serían diferentes dependiendo del trauma infantil.
Métodos: Incluimos en este estudio a víctimas adultas de accidentes o crímenes que fueron referidas a un hospital universitario o a un centro de apoyo especializado (n=143). PTSS, resiliencia, trauma infantil y PTG fueron medidos con los siguientes cuestionarios: lista de chequeo de TEPT para DSM-5, Escala de resiliencia Connor-Davidson, Cuestionario de Experiencias Adversas en la Infancia y la Forma Abreviada del Inventario de Crecimiento Postraumático, respectivamente.
Resultados: Se encontró que los efectos de los PTSS en el PTG fueron completamente mediados por la resiliencia, y que este efecto mediador fue moderado de acuerdo al trauma infantil: a mayor cantidad de experiencias traumáticas en la infancia, mayor fue el efecto mediador de la resiliencia entre los PTSS y el PTG. El efecto de la resiliencia en el PTG fue mayor en el grupo con más trauma infantil.
Conclusión: Los terapeutas que tratan a individuos con trauma psicológico deberían tratar de identificar antecedentes de trauma infantil y evaluar la resiliencia. Los enfoques terapéuticos diseñados para ello podrían mejorar el PTG entre individuos con PTSS, especialmente aquellos con alto nivel de trauma infantil.
PALABRAS CLAVE: Estrés Postraumático, Resiliencia, Crecimiento postraumático, Trauma infantil
背景:创伤后应激症状 (PTSS) 和创伤后生长 (PTG) 之间的关联结果不一致, 可能存在未知因素中介或调节这种关系。识别这些因素可能有助于制定促进对PTG的干预策略。但是, 很少有研究同时检查PTSS, 韧性和PTG之间的关系, 没有研究调查儿童期创伤对成年后这些关系的影响。
目的:本研究的目的是探讨童年创伤对韧性的带调节的中介作用, 及其和成年事故或犯罪受害者的PTSS和PTG的关系。我们假设, 复原力会中介PTSS和PTG之间的关系, 其中介效果会因童年创伤而有所不同。
方法:在这项研究中, 我们纳入了转诊到大学医院或专业支持中心的事故或犯罪的成年受害者 (n = 143) 。 PTSS, 韧性, 童年创伤和PTG分别通过以下问卷进行了测量:DSM-5 PTSD症状清单, Connor-Davidson韧性量表, 负性童年经历问卷和创伤后成长量表简版。
结果:PTSS对PTG的作用完全由韧性中介, 而这种中介作用是由童年创伤来调节的:童年创伤经历越多, PTSS和PTG之间的韧性中介作用越大。在高童年创伤暴露组中, 韧性对PTG的影响最高。
结论:治疗心理创伤患者的治疗师应尝试确定儿童创伤史, 并评估其韧性程度。根据其量身定制的治疗方法可以促进具有PTS症状的个体 (尤其是童年创伤暴露水平高的个体) 的PTG。
关键词: 创伤后应激, 韧性, 创伤后成长, 童年创伤
1. Introduction
Over 70% of people worldwide experience a traumatic event in their lifetime (Benjet et al., 2016). Post-traumatic stress disorder (PTSD) is a problem most closely associated with exposure to traumatic events. The prevalence of PTSD ranges from 1.3% to 12.2% depending on the study methods and features of the population (Karam et al., 2014). The symptoms of PTSD are recalls of traumatic memories, negative alterations in mood and cognition, avoidance, and hyperarousal (American Psychiatric Association, 2013). PTSD results in poor quality of life and increased use of health services. For instance, PTSD is associated with chronic physical conditions, such as back and neck pain, arthritis, headaches, asthma, heart disease, and stroke (Atwoli, Stein, Koenen, & McLaughlin, 2015). Furthermore, among the many trauma survivors who do not develop PTSD, trauma exposure or subsyndromal PTSD is still associated with functional impairment, suicidality, and physical health problems (Marshall et al., 2001).
While the negative consequences of trauma have garnered the greatest amount of attention, researchers have recently begun to assess positive changes in a person in the aftermath of trauma and have proposed the concept of post-traumatic growth (PTG) (Zoellner & Maercker, 2006). PTG is defined as a tendency for people to show a better functional level after experiencing traumatic events (Tedeschi & Calhoun, 2004). PTG is reflected in a greater appreciation for life, improved relationships with others, a better sense of personal strength, recognition of new possibilities, and spiritual development (Tedeschi & Calhoun, 1996). Positive associations between PTSD symptoms and PTG have been reported. One study indicated that trauma survivors with PTSD show more PTG than those without PTSD (Schubert, Schmidt, & Rosner, 2016). Researchers have also reported that PTSS positively predicts PTG (Strasshofer, Peterson, Beagley, & Galovski, 2018). A meta-analysis of PTSS and PTG, however, found positive associations to be small (Shand, Cowlishaw, Brooker, Burney, & Ricciardelli, 2015). Further research revealed a quadratic relationship between PTSD symptom severity and PTG, with the two constructs exhibiting curvilinearity in an inverse U relationship (Shakespeare-Finch & Lurie-Beck, 2014; Tsai, El-Gabalawy, Sledge, Southwick, & Pietrzak, 2015), indicating that there may be an optimal intermediate level of posttraumatic stress that strengthens PTG. Notwithstanding, other studies have reported a negative correlation between PTSD symptoms and PTG (Ai, Cascio, Santangelo, & Evans-Campbell, 2005). As such, the relationship between posttraumatic stress symptoms (PTSS) and PTG remains unclear and more research is needed to clarify factors affecting the relationship.
Whereas PTG is defined as a stress-induced increase in psychological benefits beyond the pre-traumatic state of psychological functioning, resilience reflects the maintenance of healthy or adaptive functioning over the passage of time in the aftermath of adversity (Southwick, Bonanno, Masten, Panter-Brick, & Yehuda, 2014). While there is no single, coherent, conceptual framework for resilience, it may reflect protective factors (e.g. personality characteristics, social factors, etc.) or a process of adaptation (e.g. positive cognitive appraisals, coping style, etc.) (Dutton & Greene, 2010). Experts in the field of resilience propose that all plans for research and intervention should clearly define resilience as a modifiable factor (Lutha & Cicchetti, 2000). Indeed, the Connor-Davidson Resilience Scale (CD-RISC), a measure of resilience used worldwide, considers resilience as modifiable and as improving with treatment (Connor & Davidson, 2003). Thus, it may be appropriate to consider resilience as a factor worth targeting in psychological intervention for successful adjustment after adversity.
Interestingly, in the National Comorbidity Survey, exposure rates to traumatic events exceeded 50%, whereas the lifetime prevalence for PTSD was estimated at 7.8% (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). The fact that the vast majority of individuals exposed to violent or life-threatening events do not go on to develop PTSD has not received adequate attention. The evidence that does exist suggests that resilience to violent and life-threatening events is quite common (Bonanno, Wortman, & Nesse, 2004) and that more than three-fourths of individuals exposed to trauma are resilient (Shalev, Liberzon, & Marmar, 2017). A 6-year follow-up study of the trajectory of posttraumatic stress after traumatic injury in 1084 patients reported that 73% were resilient (Bryant et al., 2015). Also, a negative correlation between resilience and PTSD symptoms has been reported (Connor & Davidson, 2003). Meanwhile, resilience has been shown to be positively correlated with PTG (Connor & Davidson, 2003), and factors, such as personal strength, relating to others, and new possibilities of PTG, have been found to be positively associated with resilience (Nishi, Matsuoka, & Kim, 2010). Therefore, in the process of adapting in the aftermath of adversity, resilience may play a mediating role between PTSS and PTG.
Given the inconsistent results on the association between PTSS and PTG, we presumed that there may be factors moderating their relationship. A large body of research has indicated that adverse childhood experiences are associated with multiple physical and mental health problems, with maladjustment, and with unhealthy lifestyles in adulthood (Felitti et al., 1998; Hughes et al., 2017). Moreover, exposure to cumulative trauma in one’s childhood has been found to result in a complex of PTSD symptoms in adults (Cloitre et al., 2009). In PTSD patients among African American women, childhood maltreatment (e.g. physical and sexual abuse) was shown to increase the risk for suicide attempts (Thompson, Kaslow, Lane, & Kingree, 2000). Research has further indicated that childhood trauma negatively influences an individual’s internal representation of self, consisting of affective, defensive, and cognitive components and that the internalized representation of self affects resilience and psychological adjustment in adulthood (Browne & Winkelman, 2007). As such, an adult’s coping and adaptation after trauma may depend on traumatic experiences in their childhood.
Traumatic stress reactions and PTG can co-exist. PTG does not imply the absence of emotional distress and difficulties in living, and PTG is not necessarily reflected in a reduction in psychological pain (Meichenbaum, 2012). While previous studies have examined associations between PTSS and resilience, between PTSS and PTG, or between resilience and PTG separately, few studies have examined relationships among PTSS, resilience, and PTG concurrently. Moreover, to our knowledge, there is no study of the effect of childhood trauma on these relationships in adults. Therefore, we aimed to examine the moderated mediating effects of childhood trauma on resilience and its associations with PTSS and PTG in adult victims of traumatic accidents or crimes. We hypothesized that resilience would mediate relationships between PTSS and PTG and that its mediating effects would differ depending on childhood trauma.
2. Methods
2.1. Procedures
To recruit patients, we advertised our study on the bulletin boards of two recruiting sites: one was a university medical centre, and the other was a Smile Centre. At the former, victims of accidents were targeted in the emergency centre. In the latter, victims of crimes were targeted for recruitment. Smile Centres, founded by the Korean Ministry of Justice, serve as a one-stop support centre offering integrated psychological services for victims of various crimes. There are thirteen Smile Centres throughout the country, one of which participated in the current study.
2.2. Participants
Data were collected from 143 participants in Korea (82 females, 61 males) who were older than 18 years and who were victims of various kinds of accidents or crimes. More specifically, accidents included car accidents, falling accidents, and workplace accidents. Crimes included sexual violence, general violence, domestic violence, and other violent crimes. The Life Events Checklist of the Diagnostic and Statistical Manual of Mental Disorder-Fifth Edition was utilized to document trauma (Weathers et al., 2013). Their psychiatric diagnoses were made by psychiatrists and clinical psychologists. Participants did not have any of the following conditions: a primary psychotic diagnosis, a serious medical condition, intellectual disabilities, or neuro-cognitive impairment. The mean age of the participants was 37.69 years (SD = 12.03). Further demographic characteristics are presented in Table 1. This study was approved by the Institutional Review Board of an affiliated National Centre (116271-2018-13).
Table 1.
Demographic and psychosocial characteristics of the participants (n = 143).
| Variables | M ± SD or n (%) | Median (range) |
|---|---|---|
| Age (years) | 37.7 ± 12.0 | 36 (19 ~ 65) |
| Gender | ||
| Male | 61 (42.7) | |
| Female | 82 (57.3) | |
| Education | ||
| ≤ Middle school | 5 (3.5) | |
| High school | 70 (49.0) | |
| College/University | 33 (23.1) | |
| Post-graduate | 29 (20.3) | |
| No response | 6 (4.2) | |
| Marital status | ||
| Single | 61 (42.7) | |
| Married/Cohabiting | 66 (46.2) | |
| Divorced/Widowed | 16 (11.2) | |
| Type of trauma | ||
| Traffic accident | 60 (42.0) | |
| Falling/Slipping | 6 (4.2) | |
| Injuries with machine | 5 (3.5) | |
| Sexual violence | 24 (16.8) | |
| Violent assault | 24 (16.8) | |
| Domestic violence | 7 (4.9) | |
| Robbery/Attempted murder | 8 (5.6) | |
| Others | 9 (6.3) | |
| Time since exposure to adult trauma (T) | ||
| T < 3 months | 90 (62.9) | |
| 3 months ≤ T < 1 years | 28 (19.6) | |
| 1 year ≤ T < 5 years | 18 (12.6) | |
| T ≥ 5 years | 7 (4.9) | |
| Study variables | ||
| PCL-5 | 40.8 ± 19.9 | 44 (0 ~ 80) |
| CD-RISC | 53.3 ± 17.5 | 52 (5 ~ 98) |
| ACE | 2.1 ± 2.1 | 1 (0 ~ 8) |
| PTGI-SF | 19.2 ± 12.3 | 16 (0 ~ 48) |
M = mean; SD = standard deviation; PCL-5 = PTSD Checklist-5; ACE = Adverse Childhood Experiences Questionnaire; CD-RISC = Connor-Davidson Resilience Scale; PTGI-SF = Short Form of the Posttraumatic Growth Inventory.
2.3. Measures
2.3.1. PTSS
To assess PTSD symptoms among the participants, 20 items from the PTSD Checklist for DSM-5 (PCL-5) were used in the current study (Blevins, Weathers, Davis, Witte, & Domino, 2015). On a 5-point Likert scale, respondents were asked to rate their experiences of being bothered over the past month by repeated, disturbing, unwanted memories of stressful experiences. In the current study, the internal consistency of the measure was high (Cronbach’s α = 0.95).
2.3.2. Resilience
Resilience in the participants was measured using the 25-item Connor-Davidson Resilience Scale (CD-RISC) (Connor & Davidson, 2003). Total scores for CD-RISC range from 0 to 100, with items rated on a 5-point Likert scale (from 0, ‘rarely true’, to 4, ‘true nearly all of the time’). The CD-RISC has a 5-factor structure: Factor 1 corresponds to the notion of personal competence, high standards, and tenacity. Factor 2 relates to trust in one’s instincts, tolerance of negative affect, and the strengthening effects of stress. Factor 3 reflects positive acceptance of change and secure relationships. Factors 4 and 5 relate to control and spiritual influences, respectively. Higher scores correspond with greater resilience. The Cronbach’s alpha for this measure in the present study was 0.94.
2.3.3. Childhood trauma
The Adverse Childhood Experiences (ACE) questionnaire was adopted to measure experiences of childhood trauma in the participants (Felitti et al., 1998). Items in the questionnaire addressed physical, emotional, and sexual abuse, as well as violence and neglect. With responses of yes or no to the 10 items, total scores ranged from 0 to 10, with higher scores suggesting more severe experiences of childhood trauma. The internal consistency of this measure in the current study was high (Cronbach’s α = 0.80)
2.3.4. PTG
A short form of the Posttraumatic Growth Inventory (PTGI-SF) was adopted in the current study (Cann et al., 2010), using 10 items to assess degrees of relating to others, new possibilities, personal strength, spiritual change, and appreciation of life, without losing the validity of the original scale. Sample items included ‘I developed new interests,’ ‘I accept needing others,’ and ‘I discovered that I am stronger than I thought I was.’ The internal consistency was high (Cronbach’s α = 0.89).
2.4. Statistical analysis
Descriptive statistics were used to summarize the demographic characteristics of participants. There was acceptable multicollinearity, with variance inflation factor values less than 10 among independent, mediate, and moderate variables. To estimate mediating effects, we used PROCESS for SPSS Macro (Hayes, 2012). In order to reduce multicollinearity and to facilitate interpretation of the results, we ran mean centralization first for independent, mediator, and moderating variables. Bootstrapping was applied with 5,000 resamples, and bias-corrected 95% confidence intervals (CI) were used to investigate mediation effects and moderated mediation effects.
3. Results
3.1. Moderated mediation effects of childhood trauma
To examine our proposed model, we utilized PROCESS Model 14 (see Figure 1). Table 2 presents the estimated regression coefficients. As can be seen, individuals with relatively less PTSS expressed more resilience (ß = −.398, 95% CI = −.530 to −.266, p < .001). Furthermore, holding PTSS, resilience as a mediator significantly affected PTG (ß = .286, 95% CI = .163 to .409, p < .001). The interactive effect of resilience and childhood trauma on PTG was significant (ß = .042, 95% CI = .0002 to .0831, p = .049). The indirect effect of PTSS on PTG through resilience depended on childhood trauma (ω = −.398[.286 + .042v], v = childhood trauma) (see Figure 1 and Table 3).
Figure 1.
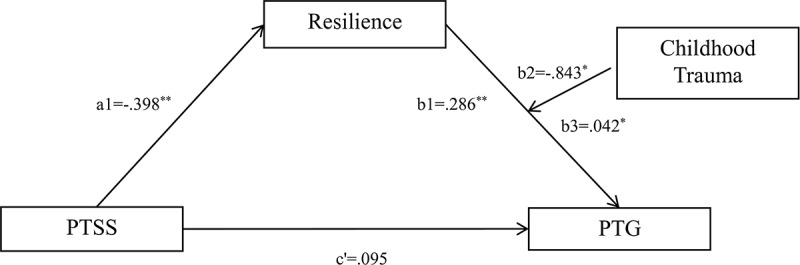
Moderated-mediation effect model among PTSS, resilience, PTG, and childhood trauma. PTSS = posttraumatic stress symptoms; PTG = posttraumatic growth; * p < 0.05; *** p < 0.001.
Table 2.
Moderated mediation effect outcomes.
| Unstandardized Coefficients |
||||||
|---|---|---|---|---|---|---|
| Coeff (ß) | SE | t | p | LLCI | ULCI | |
| Outcome: Resilience | ||||||
| (Constant) | −.141 | 1.341 | −.105 | .916 | −2.793 | 2.512 |
| PTSS (a1) | −.398 | .067 | −5.945*** | .000 | −.530 | −.266 |
| Outcome: PTG | ||||||
| (Constant) | .491 | .973 | .504 | .618 | −1.434 | 2.416 |
| PTSS (c’) | .095 | .054 | 1.745 | .0833 | −.013 | .202 |
| Resilience (b1) | .286 | .062 | 4.592*** | .0000 | .163 | .409 |
| Childhood trauma (b2) | −.843 | .385 | −2.192* | .0302 | −1.604 | −.082 |
| Resilience*Childhood trauma (b3) | .042 | .021 | 1.987* | .0490 | .0002 | .083 |
PTSS = posttraumatic stress symptoms; PTG = posttraumatic growth; LLCI = lower level of the 95% confidence interval; ULCI = upper level of the 95% confidence interval; *p < .05; ***p < .001.
Table 3.
Significance test of moderated mediation effect by bootstrapping.
| Childhood trauma | Indirect effect |
Boot SE | Boot LLCI | Boot ULCI |
|---|---|---|---|---|
| Moderated mediation effect | ||||
| Mean-1SD | −.0753 | .0405 | −.1600 | −.0008 |
| Mean | −.1138 | .0326 | −.1821 | −.0564 |
| Mean+1SD | −.1574 | .0392 | −.2409 | −.0914 |
| Index of moderated mediation | ||||
| Childhood trauma | Index | Boot SE | Boot LLCI | Boot ULCI |
| −.0166 | .0093 | −.0378 | −.0016 |
SD = standard deviation, LLCI = lower level of the 95% confidence interval, ULCI = upper level of the 95% confidence interval.
3.2. Significance of moderated mediation effects upon bootstrapping
We used bootstrapping to test the moderated mediation effects of childhood trauma. Estimates are presented with bootstrapped standard errors and 95% bootstrapped CIs (see Table 3). The indices of indirect effects and of moderated mediating effects were deemed statistically significant if the 95% CI was not zero (Hayes, 2015): a bootstrap CI that does not include a zero provides more direct and definitive evidence of moderation of indirect effects of posttraumatic stress by childhood trauma than does a test of moderation of a single path. Herein, the effects of moderated mediation of childhood trauma were statistically significant at all levels. The test revealed that higher levels of childhood trauma were accompanied by greater moderated mediation effects (−1SD = −.0753, mean = −.1138, +1SD = −.1574) (see Figure 2).
Figure 2.
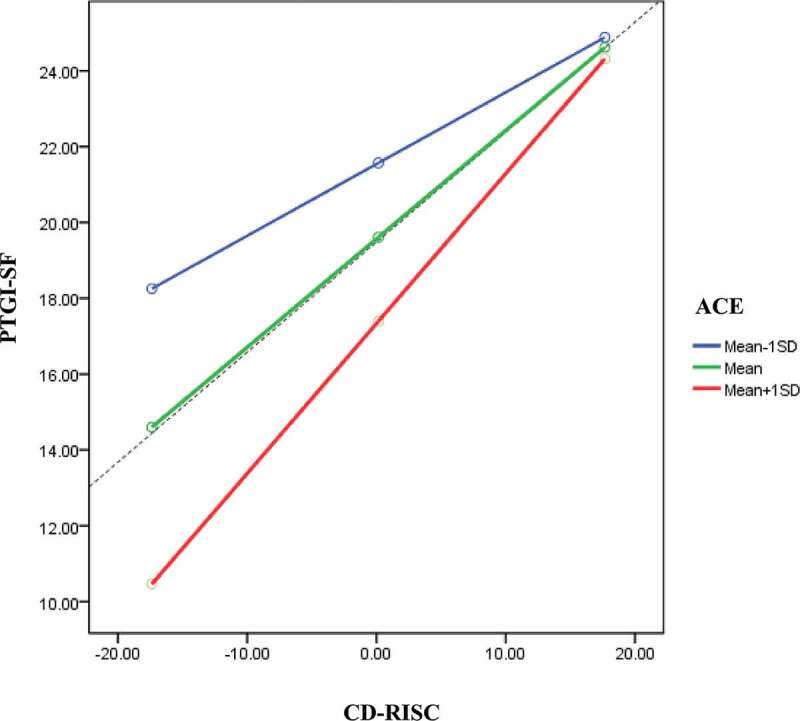
The moderating effect of childhood trauma on resilience and posttraumatic growth. PTGI-SF = Shosrt Form of the Posttraumatic Growth Inventory; CD-RISC = Connor-Davidson Resilience Scale; ACE = Adverse Childhood Experiences Questionnaire.
4. Discussion
This study aimed to examine the moderated mediating effect of childhood trauma on resilience and its association between PTSS and PTG in adult victims of accidents or crimes. Our findings indicated that the effect of PTSS on PTG is fully mediated by resilience and that the mediating effect of resilience on the relationship between PTSS and PTG is moderated by childhood trauma levels. The greater the childhood traumatic experiences, the greater the mediating effect of resilience was between PTSS and PTG. The effect of resilience on PTG was greatest in the high childhood trauma group, and high levels of resilience were associated with high levels of PTG regardless of childhood trauma. With lower resilience, however, higher levels of childhood trauma were accompanied by lower levels of PTG, compared to lower levels of childhood trauma.
Although there are several studies on PTSS, PTG, resilience, and childhood trauma, rarely have the relationships among these four variables been investigated together as in our research. One study suggested that greater resilience is associated with lower PTSD severity and more PTG in adolescent survivors of a severe natural disaster (Yuan, Xu, Liu, & An, 2018). Another study reported that different factors of PTG were correlated with resilience and PTSD symptoms in motor vehicle accident survivors (Nishi et al., 2010). However, these studies regarded PTSD and PTG as distinct outcomes and did not investigate the interactions among their relationships. Moreover, few studies have considered childhood trauma distinct from adulthood trauma.
The model of this study holds clinical implications for intervention after trauma. Our study results indicate that the mediating effect of resilience can be taken into account in the pathway from PTSS to PTG. Beyond simple reduction of PTSD symptoms, resilience-based psychotherapeutic interventions of individuals who have experienced PTSS after trauma may help promote PTG. For example, enhancing emotional regulation, cognitive flexibility and reappraisal, positive emotions, meaning making, purpose in life, and the ability to harness social support may help reinforce resilient functioning and promote PTG (Horn & Feder, 2018). Nowadays, various evidence-based psychotherapeutic interventions for traumatized patients integrate these components to enhance therapeutic effects (Schnyder & Cloitre, 2015). Our results emphasize the importance of enhancing resilience aspects in therapy for patients with psychological trauma.
In this study, individuals with more childhood trauma showed a greater mediating effect for resilience between PTSS and PTG. However, in individuals with very little traumatic experiences in their childhood, the effect of resilience on PTG was small. Therefore, patients with psychological trauma who also experienced high levels of childhood trauma may benefit more from resilience enhancing interventions to help with overcoming adversity and with bolstering PTG than patients with lower levels of childhood trauma. Integrative therapeutic approaches for complex PTSD may prove more effective with addressing the development and enhancement of self-soothing skills, healthy adult self-care functioning, and internal and external resources. However, as this was not a focus of our study, further studies applying our model are needed.
The present results should be interpreted along with consideration of a few study limitations. First, while the results from this conditional process model for analysing a hypothesized moderated mediation pathway imply a relationship between variables and the possibility of causality, the cross-sectional design prevents us from drawing any developmental causal relationships between variables. Second, the subjects of the present study only included accidents or crime victims who visited specialized centres for each trauma, and they had been exposed to quite severe trauma. A comparison between other psychological trauma survivors and other clinical populations would have been valuable to determine if the associations found in our study are specific to individuals with severe psychological trauma or not. More research that includes a longitudinal study design, a larger sample size, and comparison study with other clinical populations is needed to expand our understanding of how resilience and childhood trauma may interact with trauma-related processes and their influence on PTG. In addition, other resilience-related factors, such as sense of coherence in the salutogenesis framework, need to be investigated as potential or alternative contributors to PTG (Schafer, Becker, King, Horsch, & Michael, 2019).
In conclusion, our study suggests that resilience fully mediates and may help explain the relationships between PTSS and PTG. We found that childhood trauma moderates the mediation effect of resilience between PTSS and PTG in adult accident or crime victims. Therapists treating individuals with psychological trauma should seek to identify a history of childhood trauma and to evaluate resilience. Tailored therapeutic approaches seeking to develop resilience may improve PTG among individuals with PTSS, especially those who have experienced high levels of childhood trauma.
Funding Statement
This study was supported by a clinical research grant (2018-3) from the National Center for Mental Health, Republic of Korea. The funding source had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Acknowledgments
We would like to thank the patients for participating in the study, and So Yeon Hyun for her assistance with data collection and management.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed here.
References
- Ai, A. L., Cascio, T., Santangelo, L. K., & Evans-Campbell, T. (2005). Hope, meaning, and growth following the September 11, 2001, terrorist attacks. Journal of Interpersonal Violence, 20, 523–8. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statisical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Atwoli, L., Stein, D. J., Koenen, K. C., & McLaughlin, K. A. (2015). Epidemiology of posttraumatic stress disorder: Prevalence, correlates and consequences. Current Opinion in Psychiatry, 28, 307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjet, C., Bromet, E., Karam, E., Kessler, R., McLaughlin, K., Ruscio, A., … Hill, E. (2016). The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychological Medicine, 46, 327–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28, 489–498. [DOI] [PubMed] [Google Scholar]
- Bonanno, G. A., Wortman, C. B., & Nesse, R. M. (2004). Prospective patterns of resilience and maladjustment during widowhood. Psychology and Aging, 19, 260. [DOI] [PubMed] [Google Scholar]
- Browne, C., & Winkelman, C. (2007). The effect of childhood trauma on later psychological adjustment. Journal of Interpersonal Violence, 22, 684–697. [DOI] [PubMed] [Google Scholar]
- Bryant, R. A., Nickerson, A., Creamer, M., O’Donnell, M., Forbes, D., Galatzer-Levy, I., … Silove, D. (2015). Trajectory of post-traumatic stress following traumatic injury: 6-year follow-up. British Journal of Psychiatry, 206, 417–423. [DOI] [PubMed] [Google Scholar]
- Cann, A., Calhoun, L. G., Tedeschi, R. G., Taku, K., Vishnevsky, T., Triplett, K. N., & Danhauer, S. C. (2010). A short form of the Posttraumatic Growth Inventory. Anxiety, Stress, and Coping, 23, 127–137. [DOI] [PubMed] [Google Scholar]
- Cloitre, M., Stolbach, B. C., Herman, J. L., Kolk, B. V. D., Pynoos, R., Wang, J., & Petkova, E. (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress, 22, 399–408. [DOI] [PubMed] [Google Scholar]
- Connor, K. M., & Davidson, J. R. (2003). Development of a new resilience scale: The Connor‐Davidson resilience scale (CD‐RISC). Journal of Depression and Anxiety, 18, 76–82. [DOI] [PubMed] [Google Scholar]
- Dutton, M. A., & Greene, R. (2010). Resilience and crime victimization. Journal of Traumatic Stress, 23, 215–222. [DOI] [PubMed] [Google Scholar]
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., … Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14, 245–258. [DOI] [PubMed] [Google Scholar]
- Hayes, A. F. (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling (White paper). Retrieved from http://www.afhayes.com/public/process2012.pdf [Google Scholar]
- Hayes, A. F. (2015). An index and test of linear moderated mediation. Multivariate Behavioral Research, 50, 1–22. [DOI] [PubMed] [Google Scholar]
- Horn, S. R., & Feder, A. (2018). Understanding Resilience and Preventing and Treating PTSD. Harvard Review of Psychiatry, 26, 158–174. [DOI] [PubMed] [Google Scholar]
- Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C., … Dunne, M. P. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. The Lancet Public Health, 2, e356–e366. [DOI] [PubMed] [Google Scholar]
- Karam, E. G., Friedman, M. J., Hill, E. D., Kessler, R. C., McLaughlin, K. A., Petukhova, M., … Bromet, E. J. (2014). Cumulative traumas and risk thresholds: 12‐month PTSD in the World Mental Health (WMH) surveys. Journal of Depression and Anxiety, 31, 130–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060. [DOI] [PubMed] [Google Scholar]
- Lutha, S. S., & Cicchetti, D. (2000). The construct of resilience: Implications for interventions and social policies. Development and Psychopathology, 12, 857–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall, R. D., Olfson, M., Hellman, F., Blanco, C., Guardino, M., & Struening, E. L. (2001). Comorbidity, impairment, and suicidality in subthreshold PTSD. American Journal of Psychiatry, 158, 1467–1473. [DOI] [PubMed] [Google Scholar]
- Meichenbaum, D. (2012). Roadmap to resilience: A guide for military, trauma victims and their families. Belleair, FL: Institute Press. [Google Scholar]
- Nishi, D., Matsuoka, Y., & Kim, Y. (2010). Posttraumatic growth, posttraumatic stress disorder and resilience of motor vehicle accident survivors. BioPsychoSocial Medicine, 4, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer, S. K., Becker, N., King, L., Horsch, A., & Michael, T. (2019). The relationship between sense of coherence and post-traumatic stress: A meta-analysis. European Journal of Psychotraumatology, 10, 1562839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnyder, U., & Cloitre, M. (2015). Evidence based treatments for trauma-related psychological disorders: A practical guide for clinicians. Switzerland: Springer International Publishing. [DOI] [PubMed] [Google Scholar]
- Schubert, C. F., Schmidt, U., & Rosner, R. (2016). Posttraumatic growth in populations with posttraumatic stress disorder—A systematic review on growth‐related psychological constructs and biological variables. Clinical Psychology & Psychotherapy, 23, 469–486. [DOI] [PubMed] [Google Scholar]
- Shakespeare-Finch, J., & Lurie-Beck, J. (2014). A meta-analytic clarification of the relationship between posttraumatic growth and symptoms of posttraumatic distress disorder. Journal of Anxiety Disorders, 28, 223–229. [DOI] [PubMed] [Google Scholar]
- Shalev, A., Liberzon, I., & Marmar, C. (2017). Post-traumatic stress disorder. The New England Journal of Medicine, 376, 2459–2469. [DOI] [PubMed] [Google Scholar]
- Shand, L. K., Cowlishaw, S., Brooker, J. E., Burney, S., & Ricciardelli, L. A. (2015). Correlates of post-traumatic stress symptoms and growth in cancer patients: A systematic review and meta-analysis. Psychooncology, 24, 624–634. [DOI] [PubMed] [Google Scholar]
- Southwick, S. M., Bonanno, G. A., Masten, A. S., Panter-Brick, C., & Yehuda, R. (2014). Resilience definitions, theory, and challenges: Interdisciplinary perspectives. European Journal of Psychotraumatology, 5, 25338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strasshofer, D. R., Peterson, Z. D., Beagley, M. C., & Galovski, T. E. (2018). Investigating the relationship between posttraumatic stress symptoms and posttraumatic growth following community violence: The role of anger. Psychological Trauma, 10, 515–522. [DOI] [PubMed] [Google Scholar]
- Tedeschi, R. G., & Calhoun, L. G. (1996). The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9, 455–471. [DOI] [PubMed] [Google Scholar]
- Tedeschi, R. G., & Calhoun, L. G. (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Journal of Psychological Inquiry, 15, 1–18. [Google Scholar]
- Thompson, M. P., Kaslow, N. J., Lane, D. B., & Kingree, J. (2000). Childhood maltreatment, PTSD, and suicidal behavior among African American females. Journal of Interpersonal Violence, 15, 3–15. [Google Scholar]
- Tsai, J., El-Gabalawy, R., Sledge, W. H., Southwick, S. M., & Pietrzak, R. H. (2015). Post-traumatic growth among veterans in the USA: Results from the National Health and Resilience in Veterans Study. Psychological Medicine, 45, 165–179. [DOI] [PubMed] [Google Scholar]
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The life events checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD at www.ptsd.va.gov.
- Yuan, G., Xu, W., Liu, Z., & An, Y. (2018). Resilience, posttraumatic stress symptoms, and posttraumatic growth in Chinese Adolescents After a Tornado: The role of mediation through perceived social support. Journal of Nervous and Mental Disease, 206, 130–135. [DOI] [PubMed] [Google Scholar]
- Zoellner, T., & Maercker, A. (2006). Posttraumatic growth in clinical psychology—A critical review and introduction of a two component model. Clinical Psychology Review, 26, 626–653. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The life events checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD at www.ptsd.va.gov.


