Abstract
Aim
This review study aimed to determine the effectiveness and factors affecting the success of DSME programs in T2DM patients living in ME countries.
Methods
An extensive manual literature search was conducted using PubMed and Google Scholar for clinical trials assessing the effect of diabetes self-management education (DSME) for type 2 diabetes mellitus patients in Middle East countries. Information from the included studies was summarized in relation to study population, sample size, duration of follow-up, characteristics of DSME program, and follow-up time, besides in addition to parameters used in assessment, results, and conclusions. The risk of bias in the included studies was assessed using the Cochrane risk of bias tool. The effect of DSME on clinical and patient-reported outcomes was measured by calculation of the percentage of DSME studies that produce a significant improvement in these outcomes for patients in intervention group as compared to those in control group. Additionally, the effect of DSME on each clinical outcome was assessed by calculating the mean for the absolute effect of DSME on that outcome.
Results
Twelve studies were included in this review. Heterogeneity was found among included studies in terms of DSME program characteristics, the enrolled patients, duration of follow-up, assessment methods, and obtained outcomes. All clinical glycemic outcomes (glycosylated hemoglobin, fasting, and non-fasting blood glucose), lipid profile (total cholesterol and triglycerides), and body mass index were significantly improved for patients in intervention group as compared to those in control group in at least 60% of the included studies. All patients' reported outcomes (medication adherence, self-management behavior, knowledge, self-efficacy, health belief and quality of life) were significantly improved by the DSME program.
Conclusion
DSME programs are highly effective in improving glycemic control, lipid profile and BMI, and modestly effective in improving BP. Thus, they can reduce the risks of developing diabetes complications. Patient diabetes knowledge, DSM behaviors, adherence to medications, self-efficacy, and quality of life can also be significantly improved by DSME.
Keywords: diabetes self-management education, type 2 diabetes mellitus, Middle East countries
Introduction
Diabetes mellitus (DM) is a globally epidemic metabolic disorder with a global prevalence of 8.4%, with the highest levels (9.2%) reported in the Middle East region. This high prevalence is expected to continue rising in the future.1,2 Despite the availability of many DM types, type 2 DM (T2DM) is the commonest type as it accounts for 90% cases.3 T2DM is characterized by hyperglycemia due to insulin resistance and defective insulin secretion.4 Inadequate glycemic control can increase the risk of DM complications4 and lower patient quality of life.5 Therefore, poorly controlled DM can pose a considerable economic burden not only to patients but also to the society.6 This economic burden is prominent in the Middle East (ME) countries reaching 1.3% of the regional gross domestic product.6 Successful reduction of DM related health costs can be achieved through maintaining effective glycemic control.7,8 Accordingly, better glycemic control is an important target of DM management. Unfortunately, poor glycemic control is a common problem among patients living in the ME region.9 According to the last report of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD), hyperglycemia cannot be well controlled by anti-diabetic medications alone, instead treatment of hyperglycemia can be accomplished through patient-centered DM care.10 Unfortunately, there are many barriers to optimal diabetes care for patients in ME countries including patients’ lifestyles and lack of patient education.11 DM self-management education (DSME) and support is a crucial part of establishing and implementing the principles of diabetes care.10
Many reviews were conducted to evaluate the benefits of DSME programs for T2DM patients in developed12,13 and developing countries;14 however, only one review study was conducted specifically to assess the benefits of such programs for patients living in ME countries and was focusing on T1DM patients15 while no review study was conducted on T2DM patients. Therefore, this study aimed to review the effectiveness and factors affecting the success of DSME programs in T2DM patients living in ME countries.
Methods
Search Strategy
An extended literature review using the electronic databases of Google Scholar and PubMed was conducted for 2 months starting from the end days of August 2017 based on the following sets of keywords: “diabetes self-management education”, “diabetes self-management educational program evaluation”, “diabetes self-care education”, “pharmacist-led diabetes self-management education” and “nurse-led diabetes self-management education”.
Inclusion Criteria and Study Selection
Articles published in English during the last 10 years between 1st January 2007 and 1st September 2017, which focus on the effect of DM self-management education among adult (18–99 years) patients with type 2 DM who live in any Middle East country, were included in this review study. Only interventional controlled clinical trials (randomized and non-randomized) were included, while reviews and qualitative and observational studies were excluded.
Review Method
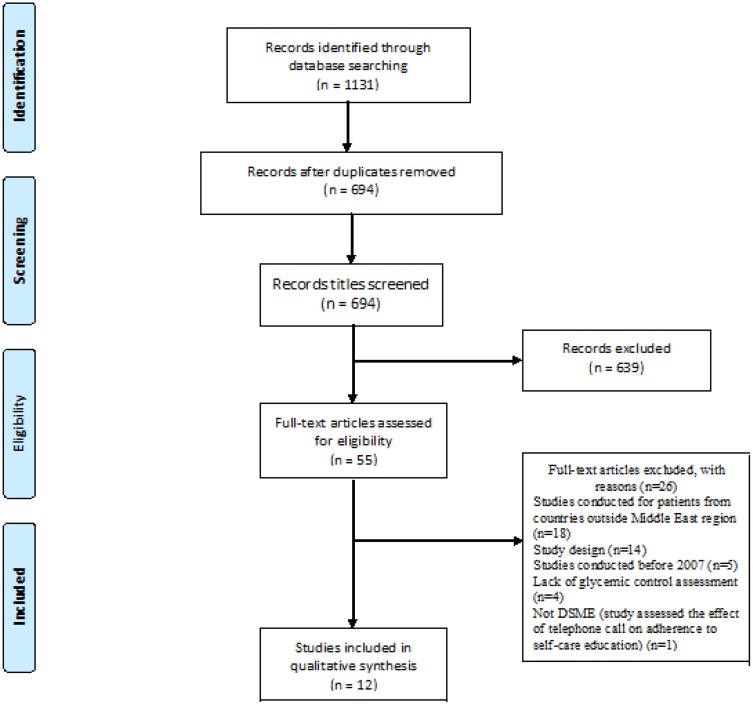
The main author of this study did a manual review for all titles during the database search. Relevant articles in which their titles imply the presence of DSMEthrough their inclusion of certain words such as education, care, support, and management were retrieved and reviewed. On the other hand, articles were not reviewed if their titles indicate that they had been conducted in a non–Middle East country (Figure 1).
Figure 1.
The PRISMA flow chart of included and excluded studies.
Extraction and Summarizing Methods
Information from the included studies was summarized in relation to the country where study was conducted, description of study population, sample size, duration of follow-up, details about DSME program (mode of delivery, education provider, theoretical bases, frequency and duration of the educational sessions), and the follow-up time, besides the parameters used during assessment, results, and conclusions. For this review, all data about the clinical outcome were presented as mean±standard deviation. Some studies present their results using a mean and confidence interval; for these studies, the standard deviation was calculated from the confidence interval based on the Cochrane method.16
Risk of Bias Assessment
All the included studies were assessed for the presence of any risk of bias using the Cochrane Risk of Bias tool.16
Sample Size
The DSME studies were categorized according to the number of enrolled patients into small sample size studies (with a sample of less than 100), intermediate (100–200) and large (greater than 200).
Characteristics of the DSME Program
The Provider of DSME
DSME was provided by various healthcare professionals including pharmacists, physicians, dietitians, nurses, and DM educators and in some cases by a non-healthcare professional (eg, interested DM patients). To achieve the aim of this study and to know which DSME provider is the best, DSME was classified as being delivered by a team (ie, two or more individuals were involved with the provision of DSME to the study participants), a pharmacist or another single provider (a nurse or trained DM educator).
Mode of Delivering DSME
During face-to-face contact, delivery of DSME was categorized into 3 distinct types: (1) education for a group of patients, (2) education to each patient individually, and (3) a combined education which consists of group education followed by individual education.
Additionally, the DSME programs were also categorized as supported (eg, phone contact and/or written material) and non-supported programs.
Contents and Duration of the DSME Program
The duration of the DSME program was measured based on the number (frequency) of the provided educational sessions and the contact time of each educational session. For this review, the number of educational sessions was categorized into DSME with many sessions (more than 5 educational sessions) and DSME with few sessions (less than 5 educational sessions).17 The total contact time was calculated by multiplying the frequency of educational sessions with the contact time of each educational session. DSME was categorized based on total contact time as short (less than 4 hrs) or long (more than 4 hrs).18
Regarding the covered self-management topics, the AADE7 self-care behaviors (diet, medication consumption, exercise, healthy coping with stress, self-monitoring of blood glucose (SMBG)), resolving problems (such as hypoglycemia and sick days management), and reducing diabetes risks were covered either completely or partially by the included studies; the studies were categorized based on the percent of covered topics into either poor with coverage of less than 50% of AADE7 self-care topics (ie, 3 topics or less) or good with coverage of at least 50% of AADE7 self-care topics (ie, 4 topics or more).19
Follow-Up Period
DSME programs had a wide range of follow-up periods; for this review, DSME studies were categorized according to follow-up period as short (3 months or less), intermediate (>3– 6 months) and long (>6 months).20 Some studies had more than 1 follow-up assessment; however, in this review, the effect of the DSME program will be based on the assessments of the last follow-up period.
Retention rate was categorized based on Cochrane Collaboration criteria into good (retention rate ≥80%) and poor (retention rate <80%).16
Effect of DSME on the Clinical Outcomes
The included studies expressed the changes in clinical outcomes (those that can be measured clinically such as glycosylated hemoglobin (HbA1c), blood glucose level, lipid profile, blood pressure (BP), and body weight) by different ways, including the change between pre- and post-intervention in each study arm, compare post-intervention values between an intervention group (IG) and control group (CG) (after taking into account non-significantly different baseline level), or compare the mean difference between IG and CG. In this review, we evaluated the changes in the clinical outcomes by 2 methods. First, we calculated the percentage of DSME studies that produce a significant improvement in the clinical outcome by including only studies that directly compare follow-up results between IG and CG. Second, we examined the absolute effect (absolute improvement) in clinical outcomes for all the included studies; the absolute change was calculated by measuring the difference in the change (post-study value – baseline value) between the IG and CG.21 Furthermore, we examined the influence of different factors such as the enrolled sample, characteristics of the DSME, and the follow-up period on the absolute effect of DSME on glycemic control.
Effect of DSME on the Patient-Reported Outcomes
The included studies expressed the changes in the patient-reported outcomes (directly reported by the patient who experienced it such as quality of life (QOL), medication adherence, health beliefs, self-efficacy, self-management behavior, knowledge and attitude towards diabetes) by different ways, including the difference between pre and post-intervention in each study arm, comparison of post-intervention (absolute value or proportion of participants achieving the outcome) values between IG and CG, or comparison of the mean difference between IG and CG. Additionally, patient-reported outcomes are usually assessed by a wide variety of questionnaires; therefore, we evaluated the changes in patient-reported outcomes by just calculating the percentage of DSME programs that produce a significant improvement in a patient-reported outcome.
Results
Twelve studies22–33 were found to be eligible and thus included in this review. The included studies were conducted in five ME countries, 7 in Iran,24,26,27,29–32 2 in Turkey,22,33 1 in UAE,23 1 in Jordan25 and 1 in Qatar.28 Heterogeneity was found among the included studies in terms of DSME program characteristics, the enrolled patients, duration of follow-up, assessment methods, and obtained outcomes (Table 1). Because of this heterogeneity, it was not possible to conduct a meta-analysis.
Table 1.
Characteristics of the Included Studies
| Study Details | Study Design | Enrolled Patients | Demographic Characteristics | Enrolled Patients (IG/CG) | Patients That Completed The Study (IG/CG) | ORR(%) | Follow Up Period (months) | DSME characteristics | Assessed Clinical Parameters (N) | Assessed Patient-Reported Parameters (N) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Educational Sessions, N (duration) | Covered Self-Care Topics (N) | DSME Provider | Mode Of Delivering DSME | Supporting Strategy | Theory-Based | ||||||||||
| Mollaoğlu et al 2007, Turkey22 | RCT | T2DM aged 18–65 years who are able to read | Non-significant difference between patients in IG and CG regarding age, gender, marital status, and educational level | 50 (25/25)* | 50 (25/25) | 100 | 2 | 3 sessions (30-40 min each session) | Diet, exercise, medication, and SMBG(4) | Nurse | Individually | Educational brochure | None | HbA1c, PPBG, FBG, T-Chol, LDL-C, HDL-C, TG(7) | None (0) |
| Al Mazroui et al 2009, UAE23 | RCT | T2DM patients on oral anti-diabetic agents | Non-significant difference between patients in IG and CG regarding age, gender, duration of DM and family history of DM | 240 (120/120)* | 234(117/117) | 97.5 | 12 | 1 session (unknown period) | Medications, exercise, SMBG, and reducing risk (smoking cessation)(4) | Pharmacist | Individually | Printed leaflet | None | HbA1c, FBG, SBP, DBP, T-chol, LDL-c, HDL-C, TG, BMI, and CHD risk(10) | Medication adherence, knowledge, quality of life(3) |
| Faresi et al 2011, Iran24 | RCT | T2DM patients with uncontrolled hyperglycemia (HbA1c > 7%) and the ability to read and write | Non-significant differences between patients in IG and CG regarding age, gender, duration of DM, type of DM treatment, educational level, and in presence of co-morbid diseases | 174 (87/87)* | 174 (87/87) | 100 | 3 | 2 sessions (unknown period) | Diet, exercise, and medications(3) | Pharmacist | Individually | Phone call | None | HbA1c and FBG(2) | None (0) |
| Jarab et al 2012, Jordan25 | RCT | T2DM patients already on treatment but with uncontrolled hyperglycemia (HbA1c >7.5%) | Non-significant differences between patients in IG and CG regarding age, gender, duration of DM, marital status, monthly income, and educational level | 171 (85/86)* | 156 (77/79) | 91.23 | 6 | 1 session (unknown period) | Diet, medication, exercise, SMBG and reducing risk (smoking cessation)(5) | Pharmacist | Individually | A phone call and educational booklet (combined) | Motivational interviewing | HbA1c, FBG, SBP, DBP, T-chol, LDL-c, HDL-C, TG, and BMI(9) | Medication adherence, DSM activity, and behavior(2) |
| Jaleh et al 2013, Iran26 | RCT | T2DM patients | Non-significant differences between patients in IG and CG regarding age, gender, marital status, and educational level. A significant difference was found between IG and CG regarding Job-status | 62 (31/31)* | 62 (31/31) | 100 | 3 | 2 sessions (60 mins each) | Diet, medication, exercise, and SMBG(4) | Nurse | Groups of patients | A phone call and educational booklet (combined) | None | HbA1c, FBG, PPBG(3) | Medication adherence(1) |
| Zareban et al 2013, Iran27 | QET(QRT) | T2DM females 30–60 years with uncontrolled hyperglycemia (Hba1c ≥ 7%) | Non-significant difference between patients in IG and CG regarding marital status, smoking, educational level, type of treatment and employment status | 138 (69/69)* | 132 (65/67) | 95.65 | 3 | 5 sessions (unknown period) | Diet, exercise, medication, SMBG, and reducing risks (smoking cessation and foot care)(5) | Team | Groups of patients | Pamphlet and training video CD | Health belief model | HbA1c(1) | DSM behavior, self-efficacy, health beliefs and attitudes towards diabetes(4) |
| Mohamed et al 2013, Qatar28 | RCT | Arabic-speaking adult patients with T2DM | Non-significant difference between patients in IG and CG regarding age at diagnosis, duration of DM, educational level and monthly income. A significant difference was found for age between patients in IG and CG | 430(215/215) | 290 (109/181) | 67.44 | 12 | 4 sessions (unknown period) | Diet, exercise, and SMBG(3) | Trained health educator | Groups of(10–20) patients | Educational booklet | Empowerment | HbA1c, FBG, DBP, SBP, T-Chol, LDL-C, HDL-C, TG, ACR, and BMI(10) | Knowledge, DSM behavior, and attitude towards diabetes(3) |
| Jahangard-Rafsanjani et al 2015, Iran29 | RCT | T2DM patients who are using oral hypoglycemic medications and had uncontrolled hyperglycemia (A1C >7%) | Non-significant differences between patients in IG and CG regarding age, gender, educational level, duration of DM and number of medications used | 101 (51/50)* | 85 (45/40) | 84.16 | 5 | 5 sessions (each one 30 mins) | Diet, exercise, and SMBG(3) | Pharmacist | Individually | Combined (pamphlet plus phone call) | None | HbA1c, SBP, DBP, and BMI(4) | Medication adherence and DSM behavior(2) |
| Shakibazadeh et al 2015, Iran30 | Prospective controlled trial | Newly diagnosed people with T2DM | Non-significant differences between patients in IG and CG regarding age, gender, marital status, duration of DM, educational level, and the mainly used treatment. | 280 (140/140) | 276(138/138) | 98.57 | 21 | 8 educational session (2.5 hrs each one) | All AADE7 self-care behaviors(7) | Team | Groups of patients | Pamphlets and brochures | Motivational interviewing | HbA1c(1) | Diabetes knowledge, DSM behavior, self-efficacy, health belief, and attitude towards diabetes(5) |
| Ebrahimi et al 2016, Iran31 | RDBCT | Adult patients with T2DM | Non-significant differences between patients in IG and CG regarding age, gender, marital status, occupation, duration of DM and educational level | 106(53/53)* | 103 (50/53) | 97.17 | 3 | 5–7 educational sessions (60–90 mins each) | Diet, exercise, medication, and reducing risks (foot care)(4) | Team | Groups (10 in each group) of patients | None | Empowerment | HbA1c, FBG, PPBG, T-Chol, LDL-C, HDL-C, and TG(7) | None (0) |
| Reisi et al 2017, Iran32 | RCT | Adults aged 25 years or more with T2DM without severe complications | Non-significant differences between patients in IG and CG regarding age, gender, marital status, duration of DM, and educational level | 80 (40/40)* | 71 (35/36) | 88.75 | 6 | 6 sessions (50–60 mins each session) | Diet, exercise, Medications, SMBG, resolving problems (treatment of hypoglycemia), and reducing risk (foot care)(6) | The provider is not declared | Groups of patients (10–15 patient in each group) then individualized | Phone call | Self-efficacy | HbA1c(1) | DSM behavior, self-efficacy, and outcome expectation(3) |
| Surucu et al 2017, Turkey33 | RDBCT | T2DM adults (older than 18 years) with at least 6 months history of DM and no physical disability | Non-significant differences between patients in IG and CG regarding age, gender, marital status, employment, duration of DM, and educational level | 139 (70/69)* | 78 (38/40) | 56.12 | 6 | 3 sessions (each one 1 hr) | Not clear | Nurse | Groups5–10 of patients | None | Orem’s Self-care Deficit Nursing | HbA1c(1) | DSM behavior(1) |
| Total | 1971 (986/985) | 1711 (817/894) | 82 | 46 | 48 | 56 | 24 | ||||||||
| Average ± SD | 164.25±108.39 (82.17±54.15/82.08±54.23) | 142.58±84.43 (68.08±37.53/74.5±48.69) | 89.72±14.16 | 6.83±5.57 | 3.83±2.21 | 4.36±1.29$1 | 4.67±3.7 | 2.67±1.32$2 | |||||||
Notes: *Based on sample size calculation. $1The average for only studies that declared their DSME contents. $2The average for only studies that assessed patient-reported outcomes.
Abbreviations: T2DM, type 2 diabetes mellitus; RCT, randomized controlled clinical trial; RDBCL, randomized double-blind controlled clinical trial; QET, quasi-experimental trial; QRT, quasi-randomized trial; HbA1c, glycosylated hemoglobin; T-chol, total cholesterol; LDL-c, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; SBP, systolic blood pressure; DBP, diastolic blood pressure; ACR, albumin to creatinine ratio; DSM, diabetes self-management; ORR, overall retention rate.
Characteristics of the DSME Program
The frequency of educational sessions varied among the included studies and ranged from 1 to 8 sessions. Seven studies (58.83%) provided the enrolled patients with DSME through a few educational sessions,22–26,28,33 while DSME through many educational sessions was found in 5 (41.17%) studies.27,29–32 Meanwhile, the duration of each educational session was mentioned only in 7 (58.83%) studies,22,26,29–33 in which the average of one educational session was 66.4 ±39.97 with a range of 30–150 mins. Accordingly, the total contact time of the DSME was short in four (33.33%) studies,22,26,29,33 intermediate in two (16.67%) studies,31,32 and long in 1 (8.33%) study.30 The covered topics by the DSME was good in 8 (66.67%) studies,22,23,25–27,30–32 poor in 3 (25%) studies24,28,29 and not declared in 1 (8.33%) study.33 The main provider of DMSE was a pharmacist in 4 (33.33%) studies,23–25,29 a nurse in 3 (25%) studies,22,26,33 a trained DM educator in 1 (8.33%) study,28 and a team in 3 (25%) studies,27,30,31 while the DSME provider was not declared in 1 (8.33%) study32 (Table 1).
DSME was delivered by a face-to-face method in all the included studies. DSME was delivered to groups of 5–20 T2DM patients in 6 (50%) studies,26–28,30,31,33 to each patient individually in 5 (41.67%) studies22–25,29 and in the last (8.33%) study32 the education was initially group-based then individualized. This face-to-face DSME was supported in 10 (83.33%) studies.22–30,32 DSME was supported by phone contact in 2 (16.67%) studies,24,32 by written material in 5 (41.67%) studies22,23,27,28,30 and by a combined support method in 3 (25%) studies25,26,29 (Table 1).
Finally, DSME was theory-based only in 7 (58.33%) studies.25,27,28,30–33 DSME-based theory was motivational interviewing in 2 (16.67%) studies,25,30 empowerment in 2 (16.67%) studies,28,31 health belief model in one (8.33%) study,27 self-efficacy in one (8.33%) study32 and Orem’s self-care deficit nursing in one (8.33%) study33 (Table 1).
Follow-Up Period of the DSME Program
The follow-up period after a DSME program ranged from 8 weeks to 21 months with an average of 6.83±5.57 months. The follow-up period was short (≤3months) in 5 (41.67%) studies;22,24,26,27,31 intermediate (>3 ≤ 6months) in 4 (33.33%) studies;25,29,32,33 and long (>6months) in 3 (25%) studies.23,28,30
The Enrolled T2DM Patients
Five (41.67%) studies24,25,27,29,30 assessed the benefits of DSME on T2DM patients with uncontrolled hyperglycemia, and 4 of these studies24,25,27,29 already enrolled patients with HbA1c ≥6.5% while the last one enrolled only newly diagnosed T2DM patients.30 On the other hand, 7 (58.33%) studies enrolled patients without regard to their glycemic control; meanwhile, 2 (16.67%) of these 7 studies32,33 enrolled patients without DM complications or disabilities, and other 2 (16.67%) studies were designed for patients on oral antidiabetic agents.23,29
A total of 1971 [986 in the IGvs.985 in the CG] with a range of 50–430 (25–215 in both IG and CG) and an average of 164.25±108.39 T2DM patients (83±54.03 in IG vs.82.92± 54.09 in CG) were enrolled in the included studies; however, the number of enrolled patients was based on sample size calculation in only 9 studies.23–27,29,31–33 A total of 1711 (817 in IG vs.894 in CG) with a range of 50–290 (IG: 25–138; CG: 25–181) and an average of 142.58±84.43 (68.08±37.53 in IG vs.74.5±48.69 in CG) T2DM patients had completed the clinical trials. This leads to a retention rate of about 89.72% (87.98% in IG vs.91.43% in CG), in which 10 (83.3%) of the included studies had a good retention rate (Table 1).
Risk of Bias
Seven (58.33%) of the included studies had poor quality in which most of these studies had a high risk of bias because of the non-blinding of participants and personnel. Details are given in Table 2.
Table 2.
Assessment of Bias Risk in the Included Studies
| Study Reference Number | Random Sequence Generation | Allocation Concealment | Blinding Of Participants And Personnel | Blinding Of Outcome Assessment | Incomplete Outcome Data | Selective Reporting | Other Bias | Study Quality |
|---|---|---|---|---|---|---|---|---|
| 22 | Unclear | Unclear | low | low | low | Low | Low | Fair |
| 23 | low | Low | high | low | low | Low | Low | Fair |
| 24 | Unclear | Unclear | high | unclear | Low | Low | High (not compare the statistical difference in the effect between IG and CG) | Poor |
| 25 | Low | Unclear | High | Unclear | Low | Low | Low | Poor |
| 26 | Unclear | Unclear | High | Unclear | Low | Low | Low | Poor |
| 27 | High | Unclear | High | Low | Low | Low | Low | Poor |
| 28 | Low | Unclear | Unclear | Unclear | High | Low | High (significant difference in the baseline level of lipid profile and BMI between IG and CG). | Poor |
| 29 | Low | Low | High | Low | Low | Low | Low | Fair |
| 30 | High | Low | Low | Unclear | Low | Low | Low | Poor |
| 31 | Low | Low | Unclear | Low | Low | Low | Low | Fair |
| 32 | Low | Low | High | Unclear | Low | Low | Low | Poor |
| 33 | Low | High | Low | Low | Low | Low | Low | Fair |
Effect of DSME Programs on the Clinical Outcomes
All of the included studies assessed the effect of DSME on at least one clinical outcome. They assessed a wide variety of clinical outcomes with an average of 4.67±3.7 and a range of 1–10 clinical outcomes. Four (33.33%) studies27,30,32,33 assessed a single clinical outcome, three (25%) studies24,26,29 assessed 2–5 clinical outcomes, while 5 (41.67%) studies22,23,25,28,31 assessed more than 5 clinical outcomes (Table 1).
The Effect of DSME on HbA1c
Twelve (100%) studies assessed the effect of DSME on HbA1c.22–33 Eight (66.67%) of these studies22,24,26,27,29,30,32,33 performed a statistical comparison between pre- and post-study HbA1c value in each study arm, in which a statistically significant improvement was evident in the IG of all (100%) of these 8 studies, while it was evident in CG in 1 (12.5%) study only.29 On the other hand, 10 studies (83.33%)22,23,25,26,28–33 assessed the effect of DSME on HbA1c by doing a statistical comparison between IG and CG, in which 8 (80%) of these studies22,23,25,26,28,30–32 showed a statistically significant improvement in HbA1c in IG compared to CG. The mean change of HbA1c after the DSME program in IG was −1.15%±0.55 with a range of (−0.33 to −2%), while the mean change in the CG was −0.08%±0.18 with a range of (+0.1 to −0.52%) (Table 3). The absolute effect of DSME on HbA1c was −1.05%±0.58 with a range of (−0.18 to −1.9%); this effect will be higher if we exclude data from studies with non-significant results (Table 4).
Table 3.
The Effect of DSME on Glycosylated Hemoglobin
| Parameter/Study Reference Number | Baseline | Post-Intervention | Change | Absolute Effect | |||
|---|---|---|---|---|---|---|---|
| IG | CG | IG | CG | IG | CG | ||
| 22 | 9.5±1.7 | 9.7±1.6 | 7.5±1.3* | 9.6±1.6*# | −2** | −0.1 | −1.9 |
| 23 | 8.5±1.06 | 8.4±1.06 | 6.9±1.05$ | 8.3±1.05$ | −1.6** | −0.1 | −1.5 |
| 24 | 9.3±1.7 | 8.9±1.1 | 7.5±1.6* | 9±1.2*# | −1.8$ | +0.1$ | −1.9 |
| 25 | 8.5±7.22 | 8.4±7.75 | – | – | −0.8** | 0.1 | −0.9 |
| 26 | 9.7+1.4 | 9.7+1.5 | 8.3±1.3* | 9.6±1.4*# | −1.4** | −0.1 | −1.3 |
| 27 | 9.71±1.81 | 9.04±1.54 | 8.3 ±1.17* | 9.06±1.52*# | −1.41$ | +0.02$ | −1.43 |
| 28 | 8.67±1.5 | 8.61±2.9 | 7.87±1.38$ | 8.42±1.99$ | −0.8** | −0.19 | −0.61 |
| 29 | 7.63±1.6 | 7.52±1.9 | 6.6±1.5* | 7±1.7* | −1.03**# | −0.52 | −0.51 |
| 30 | 9.2±2.5 | 8.8+2.2 | 8.1±1.6* | 8.9±2.2*# | −1.1** | +0.1 | −1.2 |
| 31 | 7.75 ± 1.29 | 8.61± 1.55 | – | – | –** | – | −0.86±0.28** |
| 32 | 8.4±1.06 | 8.46±1.08 | 8.07±1.16* | 8.49±1.03*# | −0.33**# | +0.03 | −0.36 |
| 33 | 7.85±1.73 | 7.68±1.64 | 7.47±1.51* | 7.48±1.42*# | −0.38**# | −0.2 | −0.18 |
| Mean±SD | −1.15±0.55^ | −0.08±0.18^ | −1.05±0.58 | ||||
Notes: *Significant difference between pre- and post-intervention in the same group. *# Non-significant difference between pre- and post-intervention in the same group. **Significantly different effect between IG and CG. **#Non-significantly different effect between IG and CG. $No statistical comparison or no data about significance. ^Mean for 11 studies only (studies with data about the change in HbA1c value).
Table 4.
The Absolute Effect of DSME Program on Different Clinical Parameters
| Lab data | No. Of Included Studies | Absolute Effect For All Included Studies (range) | Number Of Studies That did A Statistical Comparison Between IG And CG | Number Of Studies With A Statistically Significant Difference Between IG And CG (Percent) | Absolute Effect For Studies That Show A Statistically Significant Difference Between IG And CG (range) |
|---|---|---|---|---|---|
| HbA1c | 12 | −1.05±0.58 (−0.18 to −1.9) | 10 | 8 (80%) | −1.08±0.50 (−0.36 to −1.9) |
| FBG | 7 | −26.99±16.73 (−10.1 to −57.6) | 6 | 6 (100%) | −27.11±18.33 (−10.1 to −57.6) |
| Non- FBG | 3 | −44.44±10.52 (−32.41 to −51.9) | 2 | 2 (100%) | −42.16±13.78 (−32.41 to −51.9) |
| T-Chol | 5 | −23.31±8.83 (−13.3 to −32.48) | 5 | 4 (80%) | −25.37±8.71 (−13.3 to −32.48) |
| LDL-C | 5 | −17.74±14.67 (+3.5 to −34.21) | 5 | 2 (40%) | −23.98±1.10 (−23.2 to −24.75) |
| HDL-C | 5 | 2.78±4.94 (−5.8 to +6.92) | 5 | 3 (60%) | 5.27±1.44 (+4.26 to 6.92) |
| TG | 5 | −38.16±19.24 (−11.65 to −62) | 5 | 4 (80%) | −44.79±14.17 (−27 to −62) |
| SBP | 4 | −2.05±4.24 (3 to −6.9) | 4 | 1 (25%) | −6.9 |
| DBP | 4 | −4.5±5.4 (+1.8 to -9.1) | 4 | 2 (50%) | −9±0.14 (−8.9 to −9.1) |
| BMI | 4 | −0.62±0.22 (−0.4 to −0.9) | 3 | 2 (66.67%) | −0.45±0.07 (−0.4 to −0.5) |
Abbreviations: HbA1c, glycosylated hemoglobin; FBG, fasting blood glucose; NFBG, non-fasting blood glucose; T-Chol, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; SBP, systolic blood pressure; DBP, diastolic blood pressure; BMI, body mass index; ACR, albumin to creatinine ratio; IGm, intervention group; CG, control group.
Effect of DSME on Fasting Blood Glucose
Seven (58.33%) studies22–26,28,31 assessed the effect of DSME on FBG. Only 2 (28.57%) studies24,26 performed a statistical comparison between pre- and post-study FBG values in each study arm. A statistically significant improvement was evident in the IG of all (100%) of these studies, while it was evident only in 1 (50%) study26 in the CG. On the other hand, 6 studies (85.71%)22,23,25,26,28,31 assessed the effect of DSME on FBG by doing a statistical comparison between IG and CG, where all (100%) of these studies showed a statistically significant improvement in IG compared to CG. Collectively, the mean change (improvement) in the FBG after DSME within IG was −38.49 ±10.35mg/dL with a range of (−24.66 to −54.9mg/dL) which was higher than that in the CG −10.64±16.44 mg/dL with a range of (+16.2 to −31.1mg/dL) (Table 5). The absolute effect of DSME on FBG is −26.99±16.73 mg/dL with a range of (−10.1 to −57.6mg/dl) (Table 4).
Table 5.
The Effect of DSME on Fasting and Nonfasting Blood Glucose Level
| Parameter | FBG | Non-FBG (PPBG Or RBG) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Post-Intervention | Change | Absolute Effect | Baseline | Post-Intervention | Change | Absolute Effect | |||||||
| Study Reference Number | IG | CG | IG | CG | IG | CG | IG | CG | IG | CG | IG | CG | ||
| 22 | 178.3 ± 81.7 | 199.2 ± 77.6 | 137.1±41.8$ | 168.1±62.9$ | −41.2** | −31.1 | −10.1 | 263.6±67.8 | 266.1±71 | 181±40.3$ | 235.4±62.7 | −82.6** | −30.7 | −51.9 |
| 23 | 194.94±52.54 | 184.68±42.03 | 140.04±26.41$ | 170.64±41.03$ | −54.9** | −14.04 | −40.86 | – | – | – | – | – | – | – |
| 24 | 176.6±57.5 | 170.4±60.6 | 145.8±50* | 165.9±54.8*# | −30.8$ | −4.5$ | −26.3 | – | – | – | – | – | – | – |
| 25 | 225±195.14 | 210.6±372.06 | – | – | −41.4** | +16.2 | −57.6 | – | – | – | – | – | – | – |
| 26 | 182±51.9 | 212±63.9 | 144±40* | 189±48* | −38** | −23 | −15 | 288±85.4 | 273±90.1 | 222±73* | 256±100 | −66** | −17 | −49 |
| 28 | 170.82±59.4 | 170.1±75.6 | 146.16±49.86$ | 162.72±64.08$ | −24.66** | −7.38 | −17.28 | – | – | – | – | – | – | – |
| 31 | 175.68 ± 31.67 | 197.47 ± 42.13 | – | – | –** | – | −21.79±7.38** | 279.7± 52.63 | 312± 54.98 | – | – | –** | – | −32.41 |
| Mean±SD | −38.49±10.35 | −10.64±16.44 | −26.99±16.73 | −74.3±11.74 | −23.85±9.69 | −44.44±10.52 | ||||||||
Notes: *Significant difference between pre- and post-intervention in the same group. *#Nonsignificant difference between pre- and post-intervention in the same group. **Significantly different effect between IG and CG. $No statistical comparison.
Effect of DSME on Non-Fasting Blood Glucose
The effect of DSME on non-FBG (NFBG) was assessed in 3 (25%) studies;22,26,31 one study assessed random blood glucose (RBG)31 and 2 studies22,26 assessed postprandial blood glucose (PPBG). All the 3 studies (100%) assessed the effect of DSME on NFBG by doing a statistical comparison between IG and CG; they reported a statistically significant improvement in IG compared to CG. On the other hand, only one (33.33%) study26 did a statistical comparison between pre- and post-study NFBG values in each study arm, and a statistically significant improvement was evident only the IG. The mean improvement of NFBG after DSME in IG was −74.3 ± 11.74 mg/dL with a range of (−66 to −82.6mg/dL), while the mean improvement in the CG was −23.85±9.69mg/dL with a range of (−17 to −24.7mg/dL) (Table 5). The absolute effect of DSME on NFBG was −44.44±10.52mg/dL (Table 4).
The Effect of DSME on the Lipid Profile
The effect of DSME on the lipid profile [total cholesterol (T-Chol), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triglyceride (TG)] was assessed in 5 (41.67%) studies.22,23,25,28,31 All of these 5 (100%) studies assessed the effect of DSME on lipid profile by statistical comparison between IG and CG. Four (80%) of these studies22,23,25,31 showed a statistically significant improvement in T-Choland TG of patients in IG compared to CG after DSME program; meanwhile, only 3 (60%)24,28,31 and 2 (40%)23,25 of these studies showed a statistically significant improvement in HDL-C and LDL-C, respectively.
The mean improvement in lipid profile after DSME was higher in patients in IG compared to CG [T-Chol: −24.58±7.5mg/dL (−13.6 to −30.55) vs. −1.68±7.15mg/dL (+3.8 to −12.11)], [LDL-C: −16.93±6.99mg/dL (−7 to −23.2) vs. −3.3±7.11mg/dL (+5.03 to −10.5)], [HDL-C: 2.82±6.0 mg/dL (−5.8 to +8.12) vs.1.07±1.63 mg/dL (0 to +3.49)], and [TG: −24.77±17.28 mg/dL (−3.4 to −44.29) vs. +12.47±14.56 mg/dL (24.5 to −8.7)] (Table 6). The absolute effect of DSME on T-Chol was −26.65±12.06 mg/dL, LDL-C was −17.74±14.67mg/dL, HDL-C was 2.78±4.94 mg/dL and TG was −38.16±19.24 mg/dL (Table 4).
Table 6.
The Effect of DSME Program on Lipid Profile
| Parameter/Study Reference Number | 22 | 23 | 25 | 28 | 31 | Mean±SD | ||
|---|---|---|---|---|---|---|---|---|
| T-Chol | Baseline | IG | 180.6±38.7 | 203.4±40.02 | 181.75±172.62 | 207.7±37.51! | – | |
| CG | 190±52 | 203.79±41.05 | 181.75±149.87 | 186.8±39.01! | – | |||
| Post-intervention | IG | 167±31.9$ | 172.85±29.38$ | – | 180.59±37.9$ | 159.38±56.43$ | ||
| CG | 189.7±43.1$ | 205.72±40.53$ | – | 174.79±35.58$ | 184.13±59.61$ | |||
| Change | IG | −13.6** | −30.55** | −27.07** | −27.11**# | – | −24.58±7.5& | |
| CG | −0.3 | 1.93 | 3.87 | −12.01 | – | −1.63±7.13& | ||
| Absolute effect | −13.3 | −32.48 | −30.94 | −15.1 | −41.42+11.87** | −26.65±12.06 | ||
| LDL-C | Baseline | IG | 114.6±41.8 | 137.28±37.97 | 81.21±172.62 | 134.96±24.36! | – | |
| CG | 97.9±29.3 | 134.57±33.86 | 85.07±183.17 | 121.42±2.32! | – | |||
| Post-intervention | IG | 107.6±36.6$ | 117.56±24.32$ | – | 117.17±24.36$ | 142.32 ± 47.71$ | ||
| CG | 87.4±24.7$ | 139.6±34.45$ | – | 113.69±23.2$ | 166.53± 52.84$ | |||
| Change | IG | −7 | −19.72** | −23.2** | −17.79**# | – | −16.93±6.99 & | |
| CG | −10.5** | 5.03 | 0.00 | −7.73 | – | −3.3±7.11& | ||
| Absolute effect | +3.5 | −24.75 | −23.2 | −10.06 | −34.21+9.94**# | −17.74±14.67 | ||
| HDL-C | Baseline | IG | 44.1±12.8 | 46.4±9.24 | 50.27±123.3 | 52.2±10.82 | – | |
| CG | 45±11.9 | 46.02±11.29 | 50.27±58.28 | 50.65±10.44 | – | |||
| Post-intervention | IG | 48.4±10.4$ | 51.04±11.15$ | – | 60.32±10.83$ | 49.9 ± 9.35$ | ||
| CG | 45.4±13.1$ | 46.4±11.15$ | – | 54.14±11.12$ | 42.98± 9.76$ | |||
| Change | IG | 4.3**# | 4.64** | −5.8**# | 8.12** | – | 2.82±6.0& | |
| CG | 0.4 | 0.38 | 0.00 | 3.49 | – | 1.07±1.63& | ||
| Absolute effect | 3.9 | 4.26 | −5.8 | 4.63 | 6.92±1.88** | 2.78±4.94 | ||
| TG | Baseline | IG | 149±69.8 | 141.72±65.81 | 168.29±508.34 | 156.78±28.34! | – | |
| CG | 147.4±49.9 | 137.29±56.41 | 177.15±476.75 | 140.71±29.23! | – | |||
| Post-intervention | IG | 145.6 ±40.5$ | 110.72±37.13$ | – | 136.4±28.34$ | 166.5±52.01$ | ||
| CG | 171.9±47.6 | 154.12±37.13$ | – | 131.98±26.57$ | 207.92±66.99$ | |||
| Change | IG | −3.4** | −31** | −44.29** | −20.38**# | – | −24.77±17.28& | |
| CG | +24.5 | 16.83 | 17.71 | −8.73 | – | 12.58±14.61& | ||
| Absolute effect | −27.9 | −47.83 | −62 | −11.65 | −41.42±11.87** | −38.16±19.24 | ||
Notes: **Significantly different effect between IG and CG. **#Nonsignificantly different effect between IG and CG. $No statistical comparison or no data about significance. !A significant difference between IG and CG at baseline level. &The mean for 4 values only.
The Effect of DSME on Blood Pressure
Four (33.33%) studies23,25,28,29 assessed the effect of DSME on blood pressure (BP). All of these (100%) studies assessed the effect of DSME on BP by a statistical comparison between IG and CG; where 1 (25%)25 and 2 (50%)23,25 of these studies showed a statistically significant improvement in systolic BP (SBP) and diastolic BP (DBP), respectively, for patients in IG compared to those in CG. The mean change in SBP and DBP of the IG was −2.6±2.96 mmHg (+0.8 to −5.8) and −4.55±4.26 mmHg (+0.5 to −8.9), respectively; meanwhile, the mean change in the CG for SBP and DBP was −0.55±1.35mmHg (+1.1 to −2.2), and −0.05±1.39 mmHg (+1.8 to −1.3), respectively (Table 7). The absolute effect of DSME on SBP was −2.05±4.24 mmHg and on DBP was −4.5±5.4 mmHg (Table 4).
Table 7.
Effect of DSME Program on Blood Pressure and Body Mass Index
| Parameter/Study Reference Number | 23 | 25 | 28 | 29 | Mean ±SD | ||
|---|---|---|---|---|---|---|---|
| SBP | Baseline | IG | 131.4±17.51 | 132±44.64 | 137.3±12.86 | 132±17.6 | |
| CG | 132.6±19.11 | 134±40.91 | 136.0±12.72 | 136.4±19.7 | |||
| Post-intervention | IG | 127.2±14.94$ | – | 136.1±12.53$ | 132.8±17.6*# | ||
| CG | 132.1±11.27$ | – | 135.4±12.3$ | 134.2±18.7*# | |||
| Change | IG | −4.2** | −5.8** | −1.2**# | +0.8**# | −2.6±2.96 | |
| CG | −0.5 | +1.1 | −0.6 | −2.2 | −0.55±1.35 | ||
| Absolute effect | −3.7 | −6.9 | −0.6 | +3.0 | −2.05±4.24 | ||
| DBP | Baseline | IG | 85.2±8.76 | 85±46.77 | 85.2±13.34 | 81.7±9.9 | |
| CG | 83.9±10.08 | 85±17.22 | 82.1±13.48 | 83.3±11.6 | |||
| Post-intervention | IG | 76.3±7.34$ | – | 82.5±12.96$ | 82.2±9.7*# | ||
| CG | 84.1±8.91$ | – | 81.2±13.5$ | 82±11.8*# | |||
| Change | IG | −8.9** | −7.1** | −2.7**# | +0.5**# | −4.55±4.26 | |
| CG | +0.2 | +1.8 | −0.9 | −1.3 | −0.05±1.39 | ||
| Absolute effect | −9.1 | −8.9 | −1.8 | +1.8 | −4.5±5.4 | ||
| BMI | Baseline | IG | 28.34±4.19 | 32.4±39.11 | 34.8±5.41! | 29.3±4.8 | |
| CG | 27.98±4.7 | 32.8±1.51 | 32.7±3.05! | 29.4±4 | |||
| Post-intervention | IG | 27.69±3.8* | – | 34.4±5.27$ | 29.1±4.8* | ||
| CG | 27.99±4.4*# | – | 32.7±3.33$ | 29.7±4.2*# | |||
| Change | IG | −0.65 | −0.5**# | −0.4** | −0.2** | −0.44±0.19 | |
| CG | +0.01 | +0.4 | 0 | +0.3 | +0.18±0.2 | ||
| Absolute effect | −0.66 | −0.9 | −0.4 | −0.5 | −0.62±0.22 | ||
Notes: *Significant difference between pre- and post-intervention in the same group. *#Nonsignificant difference between pre- and post-intervention in the same group. **Significantly different effect between IG and CG. **#Nonsignificantly different effect between IG and CG. $No statistical comparison or no data about significance. !Significant difference between IG and CG at the baseline level.
The Effect of DSME on Body Mass Index
Four (33.33%) studies23,25,28,29 assessed the effect of DSME on body mass index (BMI); three (75%) of these studies25,28,29 assessed the effect of DSME on BMI by doing a statistical comparison between IG and CG, in which 2 (66.67%) studies28,29 showed a statistically significant improvement in BMI for patients in the IG compared to those in CG. On the other hand, only one study23 performed a direct comparison between pre- and post-BMI values in each study arm, in which only patients in the IG showed a significant improvement post-DSME. The mean improvement of BMI in the IG was −0.44±0.19kg/m2 (−0.2 to −0.65), while the mean change in the CG for BMI was +0.18±0.2kg/m2 (0 to +0.4) (Table 7). The absolute effect of DSME on BMI was −0.62±0.22kg/m2 (Table 4).
The Effect of DSME on Other Clinical Parameters
The effect of DSME on albumin/creatinine ratio was assessed in one study,28 which showed a statistically significant difference between IG and CG. The change in IG was −2.45 and −0.24 in CG leading to an absolute effect of −2.21. Meanwhile, the effect of DSME on the CHD risk factor was assessed using Framingham and BNF risk score in one study (24 only) which showed a statistically significant reduction in patients with moderate risk in IG compared to those in CG.
Factors Influencing the Effect of DSME on Glycemic Control
Although all laboratory data of HbA1c, FBG, and NFBG are important parameters to detect glycemic control, we based the assessment of factors influencing the effect of DSME on the glycemic control mainly on 2 parameters, HbA1c and FBG, because of the heterogeneity and the limited number of studies that assessed the effect of DSME on NFBG in which 2 of these studies22,26 assessed PPBG and one assessed RBG.31
DSME can achieve a statistically significant effect on the glycemic control of patients in the IG compared to CG (Tables 4 and 6). The overall improvement effect on glycemic control (FBG and HbA1c) is greatest in studies that enrolled DM patients with uncontrolled hyperglycemia [HbA1c: −1.19±0.53% vs. −0.96±0.63%; FBG: −33.58±10.3mg/dL vs. −24.35±19.06mg/dL] than those enrolled patients without regard to their glycemic control (Table 8). Meanwhile, the improvement in HbA1c was more prominent in studies performed with small sample size than those with intermediate or large sample size [−1.19±0.78% vs. −0.96±0.62% vs. −1.1±0.45%], but the improvement of FBG was greatest with intermediate sample size studies and the least with small sample size studies [−12.55±3.46mg/dL vs. −35.23±19.5mg/dL vs. −29.07±16.67mg/dL].
Table 8.
Factors Influencing the Effect of the DSME Program on Glycemic Control
| Factor | Glycosylated Hemoglobin (HbA1c) | Percent Of Studies That Showed A Significant Difference in HbA1c Between IG And CG | Fasting Blood Glucose (FBG) | Percent Of Studies That Showed A Significant Difference in FBG Between IG And CG | |||
|---|---|---|---|---|---|---|---|
| No. Of Included Studies | Absolute Effect For All Included Studies In Percent (Range) | No. Of Included Studies | Absolute Effect For All Included Studies In mg/dL (Range) | ||||
| All enrolled patients | 12 | −1.05±0.58(−0.18 to −1.9) | 8/10(80%) | 7 | −26.99±16.73(−10.1 to −57.6) | 6/6(100%) | |
| Enrolled patients | Uncontrolled hyperglycemia | 5 | −1.19±0.53(−0.51 to −1.9) | 2/3(66.67%) | 2 | −33.58±10.3(−26.3 to −40.86) | 1/1(100%) |
| Without regard to glycemic control | 7 | −0.96±0.63(−0.18 to −1.9) | 6/7(85.2%) | 5 | −24.35±19.06(−10.1 to −57.6) | 5/5(100%) | |
| Sample size | Small | 3 | −1.19±0.78(−0.36 to −1.9) | 3(100%) | 2 | −12.55±3.46(−10.1 to −15) | 2(100%) |
| Intermediate | 6 | −0.96±0.62(−0.18 to 1.9) | 2/4(50%) | 3 | −35.23±19.5(−21.79 to −57.6) | 2(100%) | |
| Large | 3 | −1.1±0.45 (−0.61 to −1.5) | 3/3 (100%) | 2 | −29.07±16.67 (−17.28 to −40.86) | 2 (100%) | |
| Frequency of DSME sessions | Few (less than 5 sessions) | 7 | −1.18±0.65 (−0.18 to −1.9) | 5/6 (83.33%) | 6 | −27.86±18.16 (−10.1 to −57.6) | 5/5 (100%) |
| Many | 5 | −0.88±0.45(−0.36 to −1.43) | 3/4(75%) | 1 | −21.79±7.38 | 1/1(100%) | |
| Contact time | Short (less than 4 hrs) | 4 | −0.97±0.78(−0.18 to −1.9) | 2/4(50%) | 2 | −12.55±3.46(−10.1 to −15) | 2/2(100%) |
| Long (more than 4 hrs) | 3 | −0.81±0.42(−0.36 to −1.2) | 3(100%) | 1 | −21.79±7.38 | 1/1(100%) | |
| Covered self-care topics | Poor (less than 4 topics) | 3 | −1.01±0.78(−0.51 to −1.9) | 1/2(50%) | 2 | −21.79±6.38(−17.28 to −26.3) | 1/1(100%) |
| Good (4 topics or more) | 8 | −1.18±0.47(−0.36 to −1.9) | 7/7(100%) | 5 | −29.07±19.77(−10.1 to −57.6) | 5/5(100%) | |
| DSME provider | Pharmacist | 4 | −1.2±0.62(−0.51 to −1.9) | 2/3(66.67%) | 3 | −41.59±15.66(−26.3 to −57.6) | 2/2(100%) |
| A single provider (non-pharmacist) | 4 | −1±0.76(−0.18 to −1.9) | 3/4(75%) | 3 | −14.13±3.67(−10.1 to −17.28) | 3/3(100%) | |
| Team | 3 | −1.16±0.29(−0.86 to −1.43) | 2/2(100%) | 1 | −21.79±7.38 | 1/1(100%) | |
| Mode of delivering DSME | Individualized | 5 | −1.34±0.62(−0.51 to −1.9) | 3/4(75%) | 4 | −33.72±20.28(−10.1 to −57.6) | 3/3(100%) |
| Group | 6 | −0.93±0.48(−0.18 to −1.43) | 4/5(80%) | 3 | −18.02±3.46(−15 to −21.79) | 3/3(100%) | |
| Combined | 1 | −0.36 | 1/1(100%) | - | - | - | |
| Support | Supported DSME | 10 | −1.16±0.55(−0.36 to −1.9) | 7/8(87.5%) | 6 | −27.86±18.16(−10.1 to −57.6) | 5/5(100%) |
| Not supported DSME | 2 | −0.52±0.48(−0.18 to −0.86) | 1/2(50%) | 1 | −21.79±7.38 | 1/1(100%) | |
| Theory-based | Theory-based | 7 | −0.79±0.44(−0.18 to −1.43) | 5/6(83.33%) | 3 | −32.22±22.09(−17.28 to −57.6) | 3/3(100%) |
| Non-theory-based | 5 | −1.42±0.57(−0.51 to −1.9) | 3/4(75%) | 4 | −23.07±13.67(−10.1 to −40.86) | 3/3(100%) | |
| Follow up period | Short | 5 | −1.48±0.44(−0.86 to −1.9) | 3/3(100%) | 4 | −18.3±7.17(−10.1 to −26.3) | 3/3(100%) |
| Intermediate | 4 | −0.49±0.31(−0.18 to −0.9) | 2/4(50%) | 1 | −57.6 | 1/1(100%) | |
| Long | 3 | −1.1±0.45(−0.61 to −1.5) | 3/3(100%) | 2 | −29.07±16.67(−17.28 to −40.86) | 2/2(100%) | |
| Risk of bias | Studies with fair quality (low risk of bias) | 5 | −0.99±0.71(−0.18 to −1.9) | 3/5(60%) | 3 | −24.25±15.53(−10.1 to −40.86) | 3/3(100%) |
| Studies with poor quality (high risk of bias) | 7 | −1.1±0.52 | 5/5(100%) | 4 | −29.05±19.65(−15 to −57.6) | 3/3(100%) | |
Note: Range is not stated in case if only one study was included in the analysis.
According to the characteristics of the DSME program, the greatest improvement in glycemic control was reported in studies with few DSME sessions [HbA1c: −1.18±0.65% vs. −0.88±0.45%; FBG: −27.86±18.16mg/dL vs. −21.79±7.38mg/dL], in studies with good coverage of self-care topics [HbA1c: −1.18±0.47% vs. −1.01±0.78%; FBG: −29.07±19.77mg/dL vs. −21.79±6.38mg/dL], in studies that depend on a pharmacist for delivering DSME [HbA1c: −1.2±0.62% vs −1±0.76% vs −1.16±0.29%; FBG: −41.59±15.66mg/dL vs −14.13±3.67mg/dL vs −21.79±7.38mg/dl], in studies that deliver DSME in an individual basis [HbA1c −1.34±0.62% vs −0.93±0.48% vs. −0.36%; FBG: −33.72±20.28mg/dL vs −18.02±3.46mg/dL], and in studies that adopt face to face DSME supported by a written material and/or phone calls [HbA1c: −1.16±0.55% vs −0.52±0.48%; FBG: −27.86±18.16mg/dL vs. −21.79±7.38mg/dL]. On the other hand, DSME studies with short contact time were more effective to lower HbA1c [−0.97±0.78% vs −0.81±0.42%], but less effective to lower FBG than those with long contact time [−12.55±3.46mg/dL vs −21.79±7.38mg/dL]. Additionally, theory-based studies were more effective to improve FBG but less effective to improve HbA1c compared to non-theory-based DSME studies [HbA1c: −0.79±0.44% vs −1.42±0.57%; FBG: −32.22±22.09mg/dL vs −23.07±13.67mg/dL].
Based on the follow-up period as a variable, the effect to improve HbA1c was greatest by studies with short follow-up period, intermediate for studies with longer follow-up period and the least with intermediate follow-up period [−1.48±0.44% vs −0.49±0.31% vs −1.1±0.45%]. However, the improvement of FBG was highest with intermediate follow-up period studies and the least by those with short follow-up period [−18.3±7.17mg/dL vs −57.6mg/dL vs −29.07±16.67mg/dL].
Effect of DSME on Patients’ Reported Outcomes
Nine (75%) of the included studies23,25–30,32,33 assessed the effect of DSME on at least one patient-reported outcome. The included studies assessed a wide variety of patient-reported outcomes with an average of 2.67 ±1.32 and a range of 1–5 outcomes (Table 1). Four (33.33%) studies25,26,29,33 assessed less than 3 outcomes and 5 (41.67%) studies23,27,28,30,32 assessed at least 3 patient-reported outcomes.
The effects of DSME on diabetes self-management (DSM) behavior and activities were assessed in 7 (58.33%) studies25,27–30,32,33 utilizing various questionnaires such as the summary of diabetes self-care activities (SDSCA),25,29,30,32,33 knowledge attitude and practice (KAP) questionnaire, 28 and an author developed questionnaire.27 However, only 6 of these studies directly compare the effect of DSME on DSM behavior between patients in IG and CG in which five (83.33%) of them25,28–30,33 showed a significant improvement of DSM behavior among patients in IG compared to those in CG. Meanwhile, 2 (33.33%) studies28,32 showed a significant improvement in overall DSM behavior score while the other 3 (50%) studies25,29,30 showed only significant improvement in some of the DSM behaviors (eg, diet, medication consumption and self-monitoring of blood glucose). Only one study27 assessed the effect of DSME on the DSM behavior by comparing pre–post-intervention values. In that study, only patients in IG showed a significant improvement in DSME.
The other commonly assessed patient-reported outcomes include medication adherence which was assessed in 4 (33.33%) studies,23,25,26,29 knowledge in 3 (25%) studies,23,28,30 self-efficacy in 3 (25%) studies,27,30,32 attitudes towards diabetes in 3 (25%) studies,27,28,30 health beliefs in 2 (16.67%) studies,27,30 quality of life in 1 (8.33%) study,23 and outcome expectations in 1 (8.33%) study.32 All of these reported outcomes were significantly improved in IG after the DSME program. Anyhow, the exact effect of DSME on the patient-reported outcomes is difficult to be counted because of the small number of studies that assessed these outcomes, in addition to the heterogeneous nature of the assessment tools and methods of presenting the results. Details are given in Table 9.
Table 9.
The Effect of DSME on Different Patients’ Reported Outcomes
| Parameter (Patient-Reported Outcome) | Study Reference Number | Assessment Tool | Outcome (Result) |
|---|---|---|---|
| Diabetes self-care behavior | 25 | SDSCA | Diet, physical activity, SMBG but not foot care or smoking cessation were significantly improved after the DSME program in IG as compared to CG |
| 29 | SDSCA | Diet and SMBG but not physical activity, foot care or smoking cessation were significantly improved after the DSME program in IG as compared to CG | |
| 30 | SDSCA | Diet, physical activity, foot care, and SMBG but not smoking cessation were significantly improved after the DSME program in IG as compared to CG | |
| 32 | SDSCA | Overall self-care activities were significantly improved after the DSME program in IG as compared to CG | |
| 33 | SDSCA | Overall self-care activities were improved in IG but the difference is not statistically significance by comparison between IG and CG | |
| 27 | The author developed new questionnaire | Overall self-care practices were significantly improved after the DSME program in IG and not in CG | |
| 28 | Knowledge, attitude, and practice (KAP) questionnaire | Overall self-care practices were significantly improved after the DSME program in IG as compared to CG | |
| Medication adherence | 23 | Author developed questionnaire | Overall medication adherence was significantly improved after the DSME program in IG as compared to CG |
| 26 | Previously developed questionnaire (Cheri Ann Hernandez) | The proportion of patients with favorable medication adherence was increased significantly after DSME in IG as compared to CG | |
| 25 | Morisky medication adherence questionnaire (4 items) | The proportion of patients who reported medication non-adherence was decreased significantly after DSME in IG as compared to CG | |
| 29 | Morisky medication adherence questionnaire (8 items) | The proportion of patients who reported medication non-adherence was decreased significantly after DSME in IG as compared to CG | |
| Knowledge | 23 | Author-developed questionnaire | The proportion of patients who had poor knowledge was decreased only in IG |
| 28 | KAP questionnaire | Overall knowledge score was significantly improved after DSME in IG as compared to CG | |
| 30 | A brief diabetes knowledge test | Only patients using oral anti-diabetic showed a significantly greater improvement in total knowledge score for patients in IG as compared to those in CG | |
| Self-efficacy | 27 | Author-developed questionnaire | Self-efficacy was significantly improved after DSME in IG but not in CG |
| 30 | Diabetes empowerment scale | Perceived self-efficacy was significantly improved after DSME in IG as compared to CG | |
| 32 | Diabetes management self-efficacy scale | Self-efficacy was significantly improved after DSME in IG as compared to CG | |
| Attitude towards diabetes | 27 | Author-developed questionnaire | The overall attitude score was only significantly improved in IG |
| 28 | KAP | Overall attitude score was significantly improved after DSME in IG as compared to CG | |
| 30 | Diabetes care profile | Both positive and negative attitudes were significantly improved after DSME in IG as compared to CG | |
| Health belief | 27 | Author-developed questionnaire | All domains of health belief (perceived susceptibility, severity, benefits and barriers) were significantly improved only in IG (not in CG) after DSME |
| 30 | Browns health beliefs instrument | Overall health belief score was significantly improved after DSME in IG as compared to CG | |
| Quality of life | 23 | Short-form-26 | All domains of quality of life (pain, general and mental health, physical and social functioning, emotion and vitality) significantly improved after DSME in IG as compared to CG |
| Outcome expectation | 32 | Outcome expectancies questionnaire | An overall score was significantly improved after DSME in IG as compared to CG |
Abbreviations: SDSCA, summary of diabetes self-care activities; IC, intervention group; CG, control group.
Discussion
The current systematic review showed that DSME can significantly improve glycemic control in at least 80% of the studies enrolled in T2DM patients who live in Middle East countries. Many other international review studies showed that HbA1c,34,35 FBG17 and NFBG36 were also significantly improved by DSME in most of the included studies.
This review showed that the absolute effect to improve HbA1c was 1.05%, which was higher than that reported in other systematic review studies (0.50–0.57%),36,37 while it was lower than that reported by a review for DSME studies among Chinese T2DM patients (1.19%).38 To confirm the current finding of high effectiveness of DSME program to improve glycemic control inT2DM patients in ME countries, we excluded all studies with poor quality and high risk of bias and the obtained results were also excellent, where 60% of the studies achieved a significant glycemic improvement in IG compared to CG; moreover, their absolute effect to reduce HbA1c is still high (0.99%). This improvement is consistent with the statement of the American Diabetes Association (ADA), which declared that DSME can improve HbA1c for T2DM patients by about 1%.39 So, it can be concluded that the effectiveness of DSME programs in improving glycemic control may be highly affected by the culture and characteristics of the enrolled patients. On the other hand, this review found that the absolute effect of DSME to improve NFBG is 44mg/dL; although no other review study showed an exact absolute effect of DSME on NFBG, this is somewhat a reasonable result since NFBG level can be reduced more than FBG level,40 which was reduced (as shown by the current review) by about 27mg/dL. This improvement in FBG is very close (−22.68mg/dL) to what has been shown in another review study of the DSME programs conducted in developed countries.17
Regarding the factors influencing the effect of DSME on glycemic control, this review showed that the effect of DSME to improve glycemic control is greater for studies enrolling patients with uncontrolled hyperglycemia; this finding was similar to many other reviews.41,42 On the other hand, this review showed that small sample sized studies achieved the greatest improvement in HbA1c compared to large sample size studies. The current finding was inconsistent with that of Gary et al43 which found a greater improvement in HbA1c by larger sized studies. However, the current review agreed with Gary et al in that the least improvement in FBG can be achieved by small sample size studies. This controversy may result from the small number of included studies in the current review. Anyhow, whatever the difference is, it is obvious that DSME studies without regard to their sample size can still achieve significant improvement in glycemic control.43
The characteristics of the DSME program can significantly influence its effect on glycemic control. In this regard, the greatest improvement of glycemic control was achieved by studies with good coverage of DSM topics. Similarly, Fan et al found that when the number of diabetes-related topics covered during DSME sessions was increased, the effect on the knowledge and metabolic control outcomes will be increased.20
Regarding the DSME sessions, the greatest effect to improve glycemic control was achieved by studies with few DSME sessions and short contact time. This finding was not in tune with many other reviews and meta-analyses;20,44 however, Ricci-Cabello and colleagues showed no statistically significant differences for the total duration of the intervention, the number of sessions included the duration of each session, the total number of hours of intervention or its intensity (number of hours per month).45 Meanwhile, a study conducted in 2017 to explore T2DM patients’ preference for DSME showed that patients prefer to be educated through fewer sessions and short periods of time.46 This collectively indicates that the content of the educational sessions and how they are delivered to patients' need appear to be more important than the number and duration of the educational sessions.47
For DSME providers, the greatest improvement in glycemic control was achieved when the pharmacist is the provider; this was consistent with a meta-analysis study which showed that the individual-based DSME can achieve greater glycemic improvement than team-based one.42 Furthermore, pharmacist-led DSME was better than other DSME single providers such as dietitian, nurse or diabetes educator, because of the role of the pharmacist to solve medication-related errors and enhance medication adherence.48
This review also showed that the DSME studies delivered to T2DM patients on an individual basis were more effective to improve glycemic control than group-based DSME. However, the literature showed some controversy about this subject where one review found a greater benefit by the group-based DSME;49 meanwhile, other reviews found that individual-based DSME is the best.37,45 The greater effectiveness of the individual-based over group-based DSME to T2DM patients who live in ME countries may be somewhat reasonable since many limitations accompanied the group-based DSME in developing countries such as being delivered in a familiar local language and must be sensitive to the cultural issues of the population.17
Supported DSME programs were shown to be more effective than non-supported DSME in improving glycemic control. Pillay and colleagues found that supporting the DSME program can result in a greater benefit, especially for programs with less than 10 hrs of contact time.50 Another study showed that supporting DSME with a phone call or written material can increase patient satisfaction and understanding which ultimately can result in better glycemic control.44
One of the findings of the current review is that theory-based DSME was less effective to improve glycemic control than non-theory-based studies. This was in contrast to the already known that DSME should be theory-based to become more effective.51 However, there was no evidence about which theory-based intervention is the most effective.52 This means that choosing a non-suitable theory for DSME can result in a paradoxical lower benefit. Anyhow, the current review showed that the highest effect in theory-based DSME was achieved by studies adopting health-belief theory.
Regarding the effect of DSME on lipid profile, the present study showed that most DSME studies (60–80%) can significantly improve T-Chol, HDL-C, and TG of patients in IG compared to those in CG. Similarly, 75% of the studies included in a recent systematic review showed a significant improvement in lipid profile.34 On the other hand, this review showed that the absolute effect of DSME on T-Chol, LDL-C, HDL-C, and TG was −23.31mg/dL, −17.74mg/dL, +2.78mg/dL, and −38.16mg/dL, respectively. Another review study showed a slightly lower absolute effect of DSME on T-Chol, LDL-C, HDL-C, and TG (−5.81mg/dL, −2.96mg/dL, 5.99mg/dL, and −37.73mg/dL).53 This difference may be acceptable since there is some evidence that the effect of DSME on lipid profiles can vary in different regions of the world.54
The current review showed that only a few studies (25% and 50%) can significantly improve SBP and DBP, respectively. Meanwhile, the effect of DSME to lower SBP was less than that of DBP (−2 vs −4.5mmHg). Similarly, a meta-analysis for DSME studies conducted in developed countries between 1990 and 2006 found that the effect of DSME on DBP is greater than that produced on SBP.20
The results of this review showed that DSME can effectively reduce BMI (−0.62 kg/m2), this effect was significant in 66.67% of the included studies. Meanwhile, patients of only one study showed non-significant benefit of DSME on BMI were found not educated about doing physical activity. Other studies found a great link between physical activity and weight loss.55,56 The current findings are consistent with that of a recent systematic review showing that nearly half of the included studies reported a significant BMI improvement with an effect of up to −0.7kg/m2.57
Although most of the included studies in this review had a short period of follow-up, some studies examined the effect of DSME to reduce the risk of diabetes complications such as nephropathy and cardiac diseases and reported a significant effect to reduce these risks. Similar findings were obtained by other studies.54,58
For DSM behaviors and activity, this review showed that DSME can effectively and significantly improve most DSM behaviors in 83.33% of the included studies; similarly, 90% of theory-based DSME studies showed improvement in overall or some DSM behaviors.52 Anyhow, the current review found that DSME programs have limited benefits to improve some behaviors especially smoking cessation and foot care. A similar finding was obtained by other reviews regarding the non-significant effect of DSME to improve foot care59 and smoking cessation.14,42 This finding may be acceptable since smoking is highly addictive practice and guidelines usually recommend a combination of behavioral therapy with medications to aid smoking cessation.60
Although few studies assessed other patients’ reported outcomes such as medication adherence, knowledge, self-efficacy, attitude toward diabetes, health belief, quality of life and outcome expectations, the results of the current study showed a significant improvement in all of these outcomes. Similarly, a systematic review related to pharmacist-led DSME studies also showed a significant improvement in medication adherence, quality of life, and diabetes knowledge after DSME.42 On the other hand, other reviews showed a significant effect of theory-based DSME to improve self-efficacy.52
There are many limitations to this review that should be mentioned. Firstly, it includes a small number of studies with the majority of them conducted in Iran. So, it may be inaccurate to generalize the results of this review to patients living in other Middle East countries. Secondly, most of the included studies have poor quality and a high risk of bias. However, these limitations are acceptable since few studies were conducted in the ME region. Therefore, performing other future reviews is highly recommended to support the findings of the current study.
Conclusion
DSME programs are highly effective to improve glycemic control, lipid profile and BMI, while modestly effective to improve BP. Thus, they can reduce the risks of developing diabetes complications. Patient diabetes knowledge, DSM behaviors, adherence to medications, self-efficacy, and quality of life also can be significantly improved by DSME. DSME delivered by the pharmacist to each patient individually through no more than 4 educational sessions supported by written material and/or phone calls can result in the greatest improvement in glycemic control.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Cho NH, Shaw JE, Karuranga S, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi: 10.1016/j.diabres.2018.02.023 [DOI] [PubMed] [Google Scholar]
- 2.NCD Risk Factor Collaboration (NCD-RISC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zheng Y, Ley SH, Hu FB. Global etiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14(2):88–98. doi: 10.1038/nrendo.2017.151 [DOI] [PubMed] [Google Scholar]
- 4.DeFronzo RA, Ferrannini E, Groop L, et al. Type 2 diabetes mellitus. Nat Rev Dis Primers. 2015;1:15019. [DOI] [PubMed] [Google Scholar]
- 5.Lau CY, Qureshi AK, Scott SG. Association between glycaemic control and quality of life in diabetes mellitus. J Postgrad Med. 2004;50(3):189–193, discussion 194. [PubMed] [Google Scholar]
- 6.Bommer C, Sagalova V, Heesemann E, et al. Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care. 2018;41(5):963–970. doi: 10.2337/dc17-1962 [DOI] [PubMed] [Google Scholar]
- 7.Gagliardino JJ, Atanasov PK, Chan JCN, et al. Resource use associated with type 2 diabetes in Africa, the Middle East, South Asia, Eurasia, and Turkey: results from the International Diabetes Management Practice Study (IDMPS). BMJ Open Diabetes Res Care. 2017;5(1):e000297. doi: 10.1136/bmjdrc-2016-000297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esposti LD, Saragoni S, Buda S, et al. Glycemic control and diabetes-related health care costs in type 2 diabetes; retrospective analysis based on clinical and administrative databases. Clinicoecon Outcomes Res. 2013;5:193–201. doi: 10.2147/CEOR.S41846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zabetian A, Keli HM, Echouffo-Tcheugui JB, et al. Diabetes in the Middle East and North Africa. Diabetes Res Clin Pract. 2013;101(2):106–122. doi: 10.1016/j.diabres.2013.03.010 [DOI] [PubMed] [Google Scholar]
- 10.Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–2701. doi: 10.2337/dci18-0033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Assaad-Khalil SH, Al Arouj M, Almaatouq M, et al. Barriers to the delivery of diabetes care in the Middle East and South Africa: a survey of 1082 practicing physicians in five countries. Int J Clin Pract. 2013;67(11):1144–1150. doi: 10.1111/ijcp.12205 [DOI] [PubMed] [Google Scholar]
- 12.Gucciardi E, Chan VW, Manuel L, Sidani S. A systematic literature review of diabetes self-management education features to improve diabetes education in women of Black African/Caribbean and Hispanic/Latin American ethnicity. Patient Educ Couns. 2013;92(2):235–245. doi: 10.1016/j.pec.2013.03.007 [DOI] [PubMed] [Google Scholar]
- 13.Norris SL, Lau J, Smith SJ, et al. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25(7):1159–1171. doi: 10.2337/diacare.25.7.1159 [DOI] [PubMed] [Google Scholar]
- 14.Dube L, Van den Broucke S, Housiaux M, et al. Type 2 diabetes self-management education programs in high and low mortality developing countries: a systematic review. Diabetes Educ. 2015;41(1):69–85. doi: 10.1177/0145721714558305 [DOI] [PubMed] [Google Scholar]
- 15.Gagliardino JJ, Chantelot JM, Domenger C. Impact of diabetes education and self-management on the quality of care for people with type 1 diabetes mellitus in the Middle East (the International Diabetes Mellitus Practices Study, IDMPS). Diabetes Res Clin Pract. 2019;147:29–36. doi: 10.1016/j.diabres.2018.09.008 [DOI] [PubMed] [Google Scholar]
- 16.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011. [Google Scholar]
- 17.Steinsbekk A, Rygg L, Lisulo M, Rise MB, Fretheim A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res. 2012;12(1):213. doi: 10.1186/1472-6963-12-213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson TM, Richards J, Churilla JR. Care utilization patterns and diabetes self-management education duration. Diabetes Spectr. 2015;28(3):193–200. doi: 10.2337/diaspect.28.3.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Farrar JT, Dworkin RH, Max MB. Use of the cumulative proportion of responders analysis graph to present pain data over a range of cut-off points: making clinical trial data more understandable. J Pain Symptom Manage. 2006;31(4):369–377. doi: 10.1016/j.jpainsymman.2005.08.018 [DOI] [PubMed] [Google Scholar]
- 20.Fan L, Sidani S. Effectiveness of diabetes self-management education intervention elements: a meta-analysis. Can J Diabetes. 2009;33(1):18–26. doi: 10.1016/S1499-2671(09)31005-9 [DOI] [Google Scholar]
- 21.Tripepi G, Jager KJ, Dekker FW. Measures of effect: relative risks, odds ratios, risk difference, and ‘number needed to treat’. Kidney Int. 2007;72(7):789–791. doi: 10.1038/sj.ki.5002432 [DOI] [PubMed] [Google Scholar]
- 22.Mollaoğlu M, Beyazıt E. Influence of diabetic education on patient metabolic control. App Nurs Res. 2009;22:183–190. doi: 10.1016/j.apnr.2007.12.003 [DOI] [PubMed] [Google Scholar]
- 23.Al Mazroui NR, Kamal MM, Ghabash NM, et al. Influence of pharmaceutical care on health outcomes in patients with type 2 diabetes mellitus. Br J Clin Pharmacol. 2009;67(5):547–557. doi: 10.1111/bcp.2009.67.issue-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Faresi S, Sabzghabaee AM, Zargarzadeh AH, Amini M. Effect of pharmacist-led patient education on glycemic control of type 2 diabetics: a randomized controlled trial. J Res Med Sci. 2011;16(1):43–49. [PMC free article] [PubMed] [Google Scholar]
- 25.Jarab AS, Alqudah SG, Mukattash TL, Shattat G, al-Qirim T. Randomized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in Jordan. J Manag Care Pharm. 2012;18(7):516–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aliha JM, Asgari M, Khayeri F, et al. Group education and nurse-telephone follow-up effects on blood glucose control and adherence to treatment in type 2 diabetes patients. Int J Prev Med. 2013;4(7):797–802. [PMC free article] [PubMed] [Google Scholar]
- 27.Zareban I, Niknami S, Hidarnia A, et al. The effect of education based on the health belief model on reduction of HbA1c level in diabetes type 2. J Res Health. 2013;3(2):370–378. [Google Scholar]
- 28.Mohamed H, Al-Lenjawi B, Amuna P, et al. Culturally sensitive patient-centered educational program for self-management of type 2 diabetes: a randomized controlled trial. Prim Care Diabetes. 2013;7:199–206. doi: 10.1016/j.pcd.2013.05.002 [DOI] [PubMed] [Google Scholar]
- 29.Jahangard-Rafsanjani Z, Sarayani A, Nosrati M, et al. Effect of a community pharmacist-delivered diabetes support program for patients receiving specialty medical care: a randomized controlled trial. Diabetes Educ. 2015;41(1):127–135. doi: 10.1177/0145721714559132 [DOI] [PubMed] [Google Scholar]
- 30.Shakibazadeh E, Bartholomew LK, Rashidian A, Larijani B. Persian diabetes self-management education (PDSME) program: evaluation of effectiveness in Iran. Health Promot Int. 2016;31(3):623–634. doi: 10.1093/heapro/dav006 [DOI] [PubMed] [Google Scholar]
- 31.Ebrahimi H, Sadeghi M, Amanpour F, Vahedi H. Evaluation of empowerment model on indicators of metabolic control in patients with type 2 diabetes, a randomized clinical trial study. Prim Care Diabetes. 2016;10:129–135. doi: 10.1016/j.pcd.2015.09.003 [DOI] [PubMed] [Google Scholar]
- 32.Reisi M, Javadzade H, Sharifirad G, et al. Effects of an educational intervention on self-care and metabolic control in patients with type II diabetes. Client-Centered Nursing Care. 2017;3(3):205–214. doi: 10.32598/jccnc.3.3.205 [DOI] [Google Scholar]
- 33.Surucu HA, Kizilci S, Ergor G. The impacts of diabetes education on self care agency, self-care activities and HbA1c levels of patients with type 2 diabetes: a randomized controlled study. Int J Caring Sci. 2017;10(1):479. [Google Scholar]
- 34.Vas A, Devi ES, Vidyasagar S, et al. Effectiveness of self-management programs in diabetes management: a systematic review. Int J Nurs Pract. 2017;23(5):xx–xx. [DOI] [PubMed] [Google Scholar]
- 35.Krishna S, Boren SA. Diabetes self-management care via cell phone: a systematic review. J Diabetes Sci Technol. 2008;2(3):509–517. doi: 10.1177/193229680800200324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carpenter R, DiChiacchio T, Barker K. Interventions for self-management of type 2 diabetes: an integrative review. Int J Nurs Sci. 2018;6(1):70–91. doi: 10.1016/j.ijnss.2018.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ Couns. 2016;99(6):926–943. doi: 10.1016/j.pec.2015.11.003 [DOI] [PubMed] [Google Scholar]
- 38.Choi TS, Davidson ZE, Walker KZ, et al. Diabetes education for Chinese adults with type 2 diabetes: a systematic review and metaanalysis of the effect on glycemic control. Diabetes Res Clin Pract. 2016;116:218–229. doi: 10.1016/j.diabres.2016.04.001 [DOI] [PubMed] [Google Scholar]
- 39.Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: A joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Clin Diabetes. 2016;34(2):70–80. doi: 10.2337/diaclin.34.2.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Woerle HJ, Neumann C, Zschau S, et al. Impact of fasting and postprandial glycemia on overall glycemic control in type 2 diabetes importance of postprandial glycemia to achieve target HbA1c levels. Diabetes Res Clin Pract. 2007;77(2):280–285. doi: 10.1016/j.diabres.2006.11.011 [DOI] [PubMed] [Google Scholar]
- 41.Minet L, Møller S, Vach W, et al. Mediating the effect of self-care management intervention in type 2 diabetes: a meta-analysis of 47 randomized controlled trials. Patient Educ Couns. 2010;80(1):29–41. doi: 10.1016/j.pec.2009.09.033 [DOI] [PubMed] [Google Scholar]
- 42.van Eikenhorst L, Taxis K, van Dijk L, de Gier H. Pharmacist-led self-management interventions to improve diabetes outcomes. A systematic literature review and meta-analysis. Front Pharmacol. 2017;8:891. doi: 10.3389/fphar.2017.00891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gary TL, Genkinger JM, Guallar E, Peyrot M, Brancati FL. A meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educator. 2003;29(3):488–501. doi: 10.1177/014572170302900313 [DOI] [PubMed] [Google Scholar]
- 44.Dehkordi LM, Abdoli S. Diabetes self-management education; experience of people with diabetes. J Caring Sci. 2017;6(2):111–118. doi: 10.15171/jcs.2017.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ricci-Cabello I, Ruiz-Pérez I, Rojas-García A, et al. Characteristics and effectiveness of diabetes self-management educational programs targeted to racial/ethnic minority groups: a systematic review, meta-analysis, and meta-regression. BMC Endocr Disord. 2014;14:60. doi: 10.1186/1472-6823-14-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fan F, Sidani S. Preferences of persons with type 2 diabetes for diabetes self-management education interventions: an exploration. Health. 2017;9:1567–1588. doi: 10.4236/health.2017.911115 [DOI] [Google Scholar]
- 47.Beck J, Greenwood DA, Blanton L, et al. 2017 National standards for diabetes self-management education and support. Diabetes Educ. 2017;43(5):449–464. doi: 10.1177/0145721717722968 [DOI] [PubMed] [Google Scholar]
- 48.Greer N, Bolduc J, Geurkink E, et al. Pharmacist-led chronic disease management: a systematic review of effectiveness and harms compared with usual care. Ann Intern Med. 2016. doi: 10.7326/M15-3058 [DOI] [PubMed] [Google Scholar]
- 49.Odgers-Jewell K, Ball LE, Kelly JT, et al. Effectiveness of group-based self-management education for individuals with type 2 diabetes: a systematic review with meta-analyses and meta-regression. Diabet Med. 2017;34(8):1027–1039. doi: 10.1111/dme.13340 [DOI] [PubMed] [Google Scholar]
- 50.Pillay J, Armstrong MJ, Butalia S, et al. Behavioral programs for type 2 diabetes mellitus: A systematic review and network meta-analysis. Ann Intern Med. 2015;163:848–860. doi: 10.7326/M15-1400 [DOI] [PubMed] [Google Scholar]
- 51.Williams GC, Zeldman A. Patient-centered diabetes self-management education. Curr Diab Rep. 2002;2(2):145–152. doi: 10.1007/s11892-002-0074-6 [DOI] [PubMed] [Google Scholar]
- 52.Zhao FF, Suhonen R, Koskinen S, Leino-Kilpi H. Theory-based self-management educational interventions on patients with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. J Adv Nurs. 2017;73(4):812–833. doi: 10.1111/jan.13163 [DOI] [PubMed] [Google Scholar]
- 53.Sherifali D, Bai JW, Kenny M, Warren R, Ali MU. Diabetes self-management programs in older adults: a systematic review and meta-analysis. Diabet Med. 2015;32(11):1404–1414. doi: 10.1111/dme.12780 [DOI] [PubMed] [Google Scholar]
- 54.Tshiananga JK, Kocher S, Weber C, et al. The effect of nurse-led diabetes self-management education on glycosylated hemoglobin and cardiovascular risk factors: a meta-analysis. Diabetes Educ. 2012;38(1):108–123. doi: 10.1177/0145721711423978 [DOI] [PubMed] [Google Scholar]
- 55.Sigal RJ, Kenny GP, Boulé NG, et al. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes. Ann Intern Med. 2007;147:357–369. doi: 10.7326/0003-4819-147-6-200709180-00005 [DOI] [PubMed] [Google Scholar]
- 56.Donnelly JE, Honas JJ, Smith BK, et al. Aerobic exercise alone results in clinically significant weight loss for men and women: midwest exercise trial 2. Obesity. 2013;21:E219–E228. doi: 10.1002/oby.20145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kumah E, Sciolli G, Toraldo ML, Murante AM. The diabetes self-management education programs and their integration in the usual care: a systematic literature review. Health Policy. 2018;122(8):866–877. doi: 10.1016/j.healthpol.2018.06.003 [DOI] [PubMed] [Google Scholar]
- 58.Brunisholz KD, Briot P, Hamilton S, et al. Diabetes self-management education improves quality of care and clinical outcomes determined by a diabetes bundle measure. J Multidiscip Health. 2014;7:533–542. doi: 10.2147/JMDH.S69000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Heinrich E, Schaper NC, de Vries NK. Self-management interventions for type 2 diabetes: a systematic review. Eur Diabetes Nurs. 2010;7:71–76. doi: 10.1002/edn.160 [DOI] [Google Scholar]
- 60.Supporting smoking cessation: a guide for health professionals. Melbourne: The Royal Australian College of General Practitioners; 2011. [updated July 2014] Available from: https://www.racgp.org.au/download/documents/Guidelines/smoking-cessation.pdf. Accessed November16, 2019. [Google Scholar]