Abstract
Skin cancer, including melanoma, basal cell carcinoma and cutaneous squamous cell carcinoma, has one of the highest global incidences of any form of cancer. In 2016 more than 16,000 people were diagnosed with melanoma in the UK. Over the last decade the incidence of melanoma has increased by 50% in the UK, and about one in ten melanomas are diagnosed at a late stage. Among the keratinocyte carcinomas (previously known as non-melanoma skin cancers), basal cell carcinoma is the most common cancer amongst Caucasian populations. The main risk factor for all skin cancer is exposure to ultraviolet radiation—more than 80% are considered preventable. Primary care clinicians have a vital role to play in detecting and managing patients with skin lesions suspected to be skin cancer, as timely diagnosis and treatment can improve patient outcomes, particularly for melanoma. However, detecting skin cancer can be challenging, as common non-malignant skin lesions such as seborrhoeic keratoses share features with less common skin cancers. Given that more than 80% of skin cancers are attributed to ultraviolet (UV) exposure, primary care clinicians can also play an important role in skin cancer prevention. This article is one of a series discussing cancer prevention and detection in primary care. Here we focus on the most common types of skin cancer: melanoma, squamous cell carcinoma and basal cell carcinoma. We describe the main risk factors and prevention advice. We summarise key guidance on the symptoms and signs of skin cancers and their management, including their initial assessment and referral. In addition, we review emerging technologies and diagnostic aids which may become available for use in primary care in the near future, to aid the triage of suspicious skin lesions.
Keywords: Basal cell carcinoma, Early diagnosis, Melanoma, Primary care, Skin cancer, Squamous cell carcinoma
Key Summary Points
| Skin cancer, including melanoma and keratinocyte carcinomas (basal cell carcinoma and cutaneous squamous cell carcinoma), has one of the highest global incidences of any form of cancer. Incidence rates of these types of skin cancer are increasing. |
| Primary care clinicians have a vital role to play in detecting and managing patients with skin lesions suspected to be cancer; timely diagnosis and treatment can improve patient outcomes, particularly for melanoma. However, detecting skin cancers can be challenging. |
| 80% of skin cancers are considered preventable, primarily through reduction in exposure to the main risk factor, UV radiation. Primary care clinicians can play an important role in skin cancer prevention through tailored advice about the risks of UV exposure. |
| This article focusses on the most common types of skin cancer: melanoma, squamous cell carcinoma and basal cell carcinoma. We describe the main risk factors and prevention advice. We summarise key guidance on the symptoms and signs of skin cancers and their management, including their initial assessment and referral. |
| In addition, we review emerging technologies and diagnostic aids, which at present require more evidence for their safety and efficacy, but may become available for use in primary care in the near future, to aid the triage of suspicious skin lesions. |
Background
Skin cancer, including melanoma, basal cell carcinoma (BCC) and cutaneous squamous cell carcinoma (SCC), has one of the highest global incidences of any form of cancer [1]. Melanoma is the fifth most common cancer in the UK, with around 16,000 patients diagnosed in 2016. If melanoma is diagnosed at an early stage, 5-year survival can be up to 95%, making early detection and treatment key to improving survival. However, melanoma is prone to metastasise, making it responsible for up to 90% of skin cancer deaths (2285 deaths in 2016 in the UK) [2, 3]. Furthermore, among Caucasian populations in the UK, the incidence of melanoma has quadrupled over the last 30 years, and is expected to be among the cancers with the fastest increasing incidence over the next 20 years, rising by a further 7% [4].
The ‘non-melanoma skin cancers’ (NMSC) include SCC and BCC, although they arise from keratinocyte cells and are increasingly known as keratinocyte carcinomas (KCs) [5]. They are very common. In the UK in 2015, more than 142,000 new cases were diagnosed, including about 80% BCC and 20% SCC [6, 7]. Similar to melanoma, the incidence of KCs has risen over recent decades, with an increase of 61% over the past 10 years alone [6].
In the UK, most patients with skin cancer first present in primary care [8], where clinicians then face the challenge of distinguishing a rare possible skin cancer from common benign skin lesions [9]. The National Cancer Diagnosis Audit in England recently reported that the median primary care interval (time from first presentation to referral) for melanoma was 0 days, the joint lowest of the 21 cancers reported [10]. Prolonged intervals of 60 and 90 days were experienced by 6% and 4.8% cases respectively [10], suggesting that primary care clinicians are generally accurate at recognising suspicious skin lesions. However, among patients referred with suspicious skin lesions via an urgent suspected cancer ‘2-week-wait’ (2WW) system in England, only around 3% are diagnosed with melanoma [11], suggesting that improved primary care triage could reduce burden on both patients and specialist care. Although this article principally aims to support primary care clinicians in the UK to recognise and manage patients with possible skin cancer in a timely way, it will also be of relevance to clinicians in other healthcare systems. We focused on the National Institute for Health and Care Excellence (NICE) guidelines, developed for use in England and Wales, to direct the discussion. We present melanoma and the keratinocyte carcinomas separately, except when their assessment and management can be considered together.
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Risk Factors
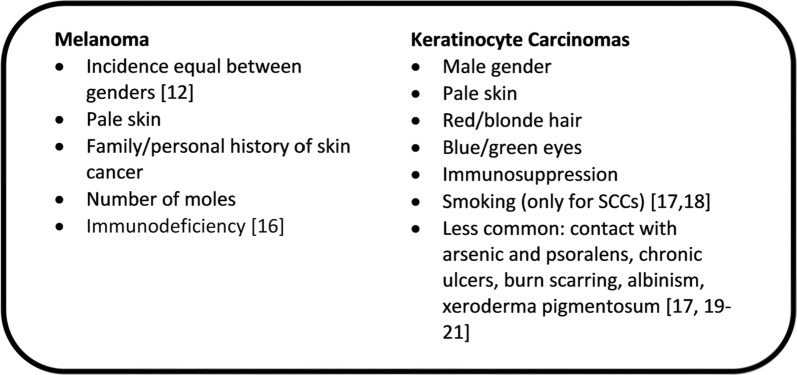
Skin cancer incidence relates strongly to age, with age-specific incidence rates rising sharply from 50 years to peak in those over 75 years of age. In contrast to most other cancers, 25% of melanomas are diagnosed in those aged 50 and under [12]. The main risk factor for all skin cancers is preventable, namely exposure to ultraviolet (UV) radiation, with more than 80% of melanomas attributed to UV exposure [13, 14]. This includes not only long-term exposure but also short periods of intense sun exposure or burning, especially in childhood or with sunbed use. For SCCs, cumulative UV exposure appears to be the main risk factor, whereas intermittent UV exposure is the leading risk factor for BCCs [15]. Other risk factors for melanoma and KCs are listed in Fig. 1 [12, 16–21].
Fig. 1.
Risk factors for melanoma and KCs
Prevention
Prevention of skin cancer focuses on patient education about the risks and benefits of sun exposure, and tailoring advice to the individual patient risk [22, 23]. Figure 2 provides a summary of advice on avoiding sun exposure [22–25]. A systematic review exploring complex risk communication, undertaken to support NICE guidelines on sunlight exposure [22], found that only tailored messages (i.e. personalised to individual circumstances) had strong evidence as a potentially effective strategy for improving health behaviour outcomes. Relative risk reduction (i.e. the relative decrease in the risk of an adverse event in the group adhering to preventative advice compared to the group not following preventative advice) was thought to be more persuasive in getting people to adopt certain behaviours than other statistical presentations. There is evidence that interventions based on the appearance-damaging effects of UV exposure, and the positive effects of sun protection, may be effective in altering behaviour [26]. Cancer Research UK have produced numerous patient information resources as part of their Sun Smart campaign [27], which can be used by clinicians to aid communication with patients.
Fig. 2.
Advice to give patients aiming to reduce sun exposure and risk of skin cancer [22–25]
Screening
There is no evidence worldwide to support the use of screening programs at a population level [28, 29], although there is recent research interest in using risk assessment models to identify people at higher risk of melanoma, for personalised approaches to surveillance [30–32]. Guidelines in the USA recommend screening for patients at high risk of melanoma due to a strong family or personal history of skin cancer [33], and the Royal Australian College of General Practitioners’ guidance suggests a 6-monthly full-skin examination for patients at high risk of melanoma and annually for those at high risk of KC [25]. Interestingly, a recent systematic review assessing BCC screening against the World Health Organisation screening criteria [34] concluded that it may be beneficial for lesions on the face.
Detecting Skin Cancer in Primary Care
Melanoma
Symptoms and Signs
The commonest subtype of melanoma is known as superficial spreading melanoma: this classically presents as a pigmented skin lesion (‘mole’) that has changed in size, shape or colour [35] (Fig. 3). It most commonly presents on the trunk in men and on the legs in women [12]. Other melanoma subtypes include nodular melanoma (5%), lentigo maligna (melanoma in situ, 4–15%), and acral lentiginous melanoma (5%) [36, 37] and these may present in different ways.
Fig. 3.
Clinical images of types of melanoma. a Superficial spreading melanoma. b Nodular melanoma. c Amelanotic melanoma. d Lentigo maligna. e Acral lentiginous melanoma.
The images are reproduced with the kind permission of the Primary Care Dermatology Society and are available on their website: http://www.pcds.org.uk/
Nodular melanomas tend to occur on the head and neck of older people: they grow quickly, and are usually firm, symmetrical and evenly pigmented papules or nodules, which may ulcerate and bleed.
Lentigo maligna (also known as Hutchinson’s freckle) develop as a slow-growing precursor pigmented macule which may remain in situ for many years. Once it becomes invasive it is known as lentigo maligna melanoma and may progress rapidly, often being poorly defined and variably pigmented; they are much more common in people aged 60 and over.
Acral lentiginous melanomas occur exclusively on the palms and soles and under nails, and are thought to be unrelated to sun exposure. Although uncommon among Caucasians, they are commoner in people with pigmented or Asian skin. They typically appear as a large pigmented macule, but can mimic warts with a verrucous, non-pigmented appearance [38–40].
An estimated 2–20% of melanomas are amelanotic—these can appear as a non-pigmented mimic of any subtype, with nodular melanomas the most likely to be amelanotic [38]. They are more common in older age groups over 70 years of age and in the head and neck region, and tend to have worse outcomes than pigmented melanomas [38].
Management
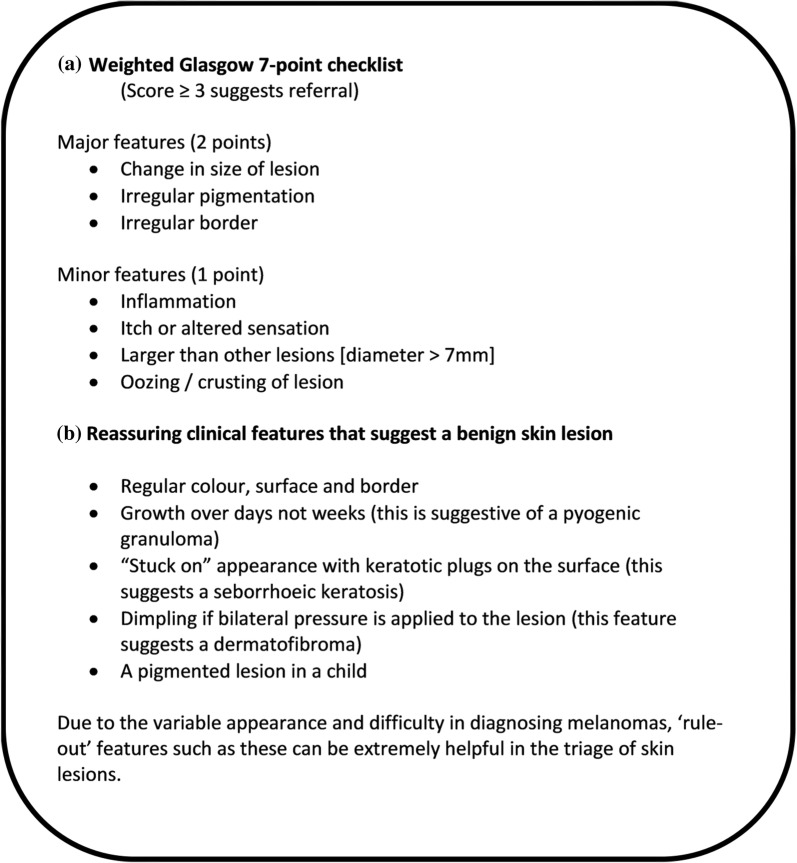
NICE guidance (2015) recommends using naked eye examination and the weighted Glasgow 7-point checklist to assess suspicious skin lesions (see Fig. 4; [24, 41, 42]). If a lesion scores 3 or more, then referral via an urgent suspected cancer pathway is recommended [41]. There are a number of other checklists available, such as the “ABCDE” mnemonic, most commonly used in North America, which refers to Asymmetry, Border irregularity, Colour variation, Diameter larger than 6 mm, Evolution/changing [43, 44]. NICE recommends that a suspected melanoma should not be excised in primary care [45], although a recent study suggests that no harm came to patients undergoing primary care excision in the rural Scottish setting [46]. To avoid missing atypical melanomas, the NICE clinical knowledge summary also recommends referring the following lesions via an urgent suspected cancer pathway: new nodules which are pigmented or vascular in appearance; nail change such as a new pigmented line or pigmentation under the nail; or any skin lesion that is persistent or slowly evolving and unresponsive, with an uncertain diagnosis [24].
Fig. 4.
a Weighted Glasgow 7-point checklist for assessing suspicious pigmented skin lesions, as recommend by NICE guidance (2015) [41, 42]. b Reassuring clinical features that do not require referral to secondary care (unless there are other concerning symptoms) as they suggest a benign lesion [24]
A routine referral for risk estimation, education and possible surveillance should be considered for anyone who is potentially at high risk for developing melanoma. This includes those who have giant congenital pigmented naevi (benign melanocytic naevi originating in utero measuring greater than 20 cm in diameter [47]), a family history of three or more melanoma cases, more than 100 normal moles, or any atypical moles (particularly if multiple) [24].
Squamous Cell Carcinoma (SCC)
Symptoms and Signs
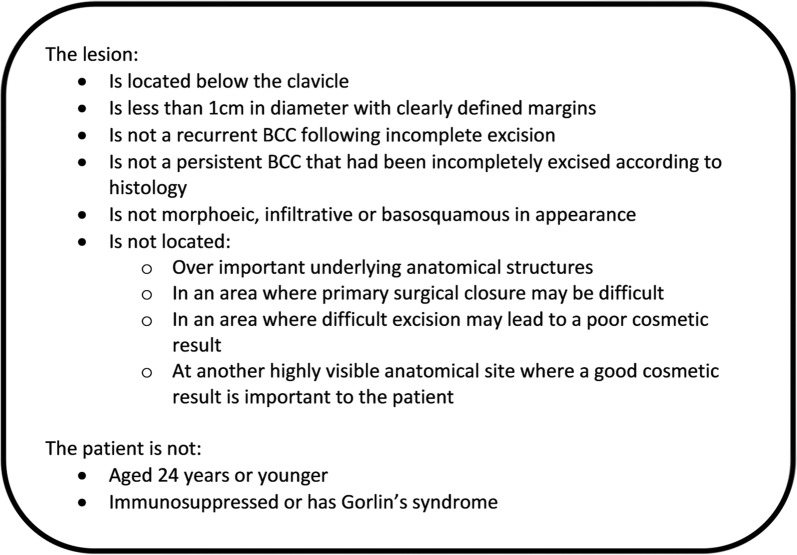
SCCs tend to arise in areas that are frequently exposed to the sun: face, scalp, ears, neck, and upper limbs [48] (Fig. 5). Typically, they appear either as an indurated (firm), nodular, crusted lesion, or as an ulcer with no crusting [49, 50]. However, their appearance is variable and they should be suspected in any lesion that is larger than 1 cm, is non-healing, keratinized or crusted, and has a documented expansion over the past 8 weeks [51]. In situ SCC (Bowen’s disease) typically appear as erythematous, scaly plaques with clearly defined margins, but can sometimes be pigmented and flat with poorly defined margins [19]. A variant of SCC is keratoacanthoma; these are domed, fast-growing, nodules with a central hyperkeratotic region [52]. High-risk SCCs include those on the lips, ears, non-sun-exposed sites, in areas of previous injury, those that are larger than 2 cm in diameter, are in immunocompromised patients, or are a recurrence of a previously treated lesion. These have a higher probability of metastasis and recurrence after treatment [45].
Fig. 5.
Clinical images of types of SCCs. a Well-differentiated SCC. b SCC on scalp. c Poorly differentiated SCC. d Keratoacanthoma. The images are reproduced with the kind permission of the Primary Care Dermatology Society and are available on their website: http://www.pcds.org.uk/
Management
As for melanoma, confirmation of an SCC relies on excision and histopathological examination; therefore all patients with a suspicious lesion should be referred on an urgent suspected cancer pathway to secondary care [41].
Basal Cell Carcinoma (BCC)
Symptoms and Signs
BCCs commonly arise in the head, neck, trunk and limbs [20], but can be variable in their clinical presentations (Fig. 6). There are several histological subtypes [53] which may present differently. Nodular and micro-nodular BCCs are commonly found on the face and present as pearly pink or white cystic papules or nodules that have telangiectasia on their surface and may be ulcerated. Superficial BCCs are usually on the upper trunk and shoulders, and present as erythematous, well-demarked, scaly plaques with pearly white borders. They are often large (> 20 mm), multiple and slow growing, and can be confused with Bowen’s disease. Another important mimic is amelanotic melanoma, which can present as a red lesion and be confused with a BCC [54]. Morphoeic BCCs (also known as sclerosing or infiltrative) usually occur on the face and present as skin-coloured, waxy, scar-like lesions; they tend to recur and can infiltrate cutaneous nerves. Pigmented BCCs are brown, blue or greyish lesions that can resemble melanomas. Baso squamous BCCs have mixed BCC and SCC characteristics and can be more aggressive than other forms of BCC [53, 55, 56].
Fig. 6.
Clinical images of types of BCC. a BCC. b Superficial BCC. c Morphoeic BCC. d Pigmented BCC. e Basosquamous BCC. The images are reproduced with the kind permission of the Primary Care Dermatology Society and are available on their website: http://www.pcds.org.uk/
Management
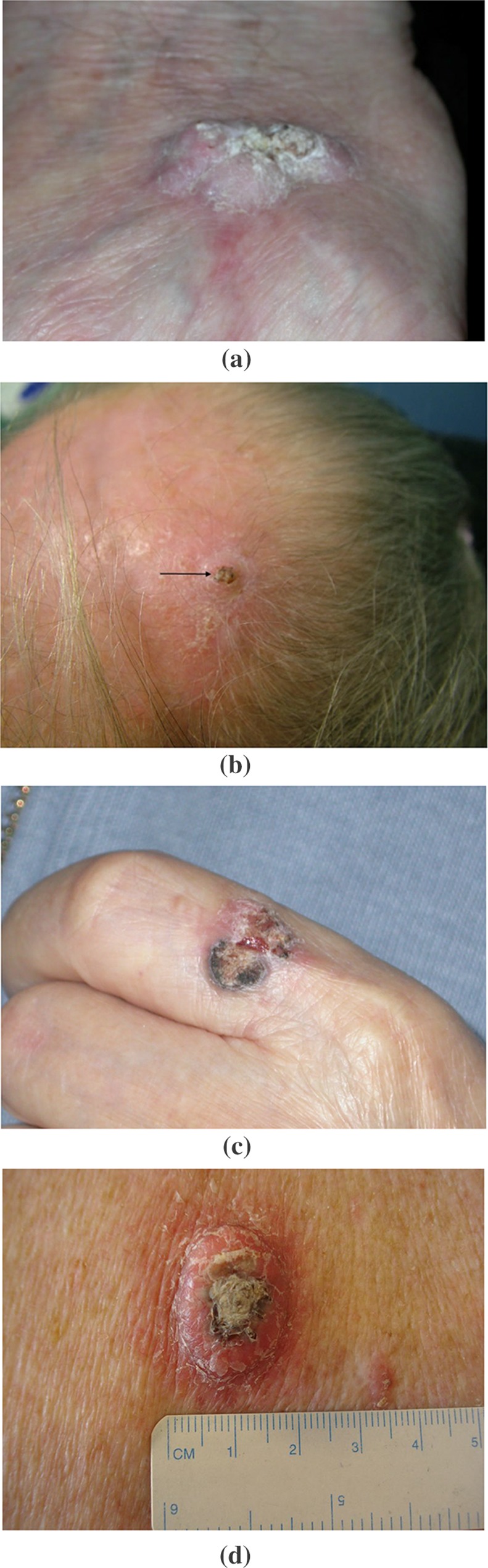
The 2010 NICE guidance recommends that low-risk BCCs (see Fig. 7) may be excised by primary care clinicians with appropriate training [53, 57]. This guidance may vary by local agreement, depending on the clinicians’ role, competencies and local policy. For all other patients with a suspected BCC, routine referral to specialist care is recommended, although, if there is concern that a delay in referral will make a “significant impact” because of factors such as lesion site or size, then referral via an urgent cancer pathway should be considered [41].
Fig. 7.
Features of low-risk BCCs [53]
Tools for Evaluating Suspicious Skin Lesions in Primary Care
Dermoscopy
A dermatoscope is a handheld magnification tool and light source which eliminates skin surface reflection, and can help assessment of skin lesions with visualisation of deeper subsurface structures [58]. Dermoscopy performed by trained specialists is both more sensitive and specific in classifying skin lesions than clinical examination with the naked eye alone [59, 60]. There have been two recent Cochrane reviews of the evidence for dermoscopy to diagnose keratinocyte carcinomas [61] and melanoma [62]. Both found that most evidence was derived from secondary care populations; hence, there was insufficient evidence to support routine use of dermoscopy by primary care clinicians. Our group’s recent systematic review of dermoscopy use in primary care also found the literature to be scanty; however, there was some evidence that dermoscopy has the potential to help primary care clinicians triage suspicious lesions [63]. It also highlighted that further evidence is needed on patient acceptability and minimum training requirements for primary care clinicians to reach competence, as well as the cost-effectiveness of implementing dermoscopy in primary care.
Teledermatology
This term describes the use of information technology to facilitate skin management, most commonly by sharing digital images of lesions with dermatology specialists. Teledermatology referral systems are already well established in some areas of the UK. A recent Cochrane review assessing the diagnostic accuracy of teledermatology for detecting melanomas, BCCs and SCCs in adults compared to face-to-face diagnosis by a specialist concluded that teledermatology is accurate for identifying the majority of malignant lesions [64]. However, it also suggested that further research is needed to fully determine its diagnostic accuracy, feasibility and cost-effectiveness as a triaging tool for referring suspicious skin lesions from primary to secondary care.
SIAscopy/MoleMate System
Spectrophotometric intracutaneous analysis (SIAscopy) is a non-invasive scanning technology, incorporated into the MoleMate system, and evaluated in a randomised controlled trial set in UK general practice. The MoleMate system was not found to improve appropriateness of referral, and its use led to a higher proportion of lesions being referred [65]. However, there was some evidence that a higher referral rate from general practice may actually be cost-effective owing to improved outcomes associated with earlier diagnosis of melanomas [66].
Artificial Intelligence (AI)-Supported Systems
The use of AI/machine learning to evaluate skin lesions has received a huge amount of recent attention in both the lay and medical press. Experimental studies using images of lesions from specialist clinics have shown that AI algorithms can classify images of skin cancer with an accuracy that matches or even exceeds dermatologists [67, 68]. This suggests that AI has the potential to assist primary care clinicians to triage suspicious skin lesions; research is now needed on real-world primary care populations to establish the accuracy and safety of using these AI technologies in primary care.
Other Diagnostic Tools
Many other non-invasive tests and diagnostic technologies have been developed to aid skin cancer diagnosis, including high frequency ultrasonography, optical coherence tomography, reflectance confocal microscopy, and computer-assisted diagnosis. They have been evaluated in several recent Cochrane reviews, all of which found a paucity of evidence for their accuracy in either primary or specialist care settings. Therefore, at present, there is insufficient evidence to recommend their use [64, 69–73].
Conclusions
Advice on limiting sun exposure remains an important task for primary care clinicians, especially among high-risk patient groups. Any suspected melanomas or SCCs should be referred via urgent cancer pathways to specialist care for histological diagnosis and management. Suspected BCCs should be referred routinely to specialist care unless they are of concern because of their size or location, when they may warrant urgent referral.
A number of diagnostic technologies are in development, some of which may have a significant impact on clinical practice. We may therefore be on the verge of significant changes in the detection of possible skin cancers in primary care. However, the evidence for the safe and effective use of most of these technologies by primary care clinicians is currently lacking. There is weak evidence for use of dermoscopy and teledermatology in primary care, but even these approaches require further evaluation before they can be recommended for widespread implementation in primary care.
Acknowledgements
Permissions
All images in this article are reused with the kind permission of the Primary Care Dermatology Society (PCDS) who holds the copyright for these images. All images were downloaded from the PCDS website: http://www.pcds.org.uk/. Accessed on 30 Aug 2019.
Funding
No funding was obtained to specifically support this research or publish this article. Authors Owain T. Jones and Garth Funston are Clinical Research Fellows and author Fiona M. Walter is Director of the multi-institutional CanTest Collaborative, which is funded by Cancer Research UK (C8640/A23385).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Disclosures
Authors Owain T. Jones, Charindu K. I. Ranmuthu, Per N. Hall, Garth Funston and Fiona M. Walter have no conflicts of interest to disclose. However, author Garth Funston is a member of the journal’s Editorial Board.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Footnotes
Enhanced Digital Features
To view enhanced digital features for this article go to 10.6084/m9.figshare.9976475.
References
- 1.Ferlay J, Colombet M, Soerjomataram I, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer. 2018;103:356–387. doi: 10.1016/j.ejca.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Cancer Research UK About melanoma. https://www.cancerresearchuk.org/about-cancer/melanoma/about. Accessed 30 Aug 2019.
- 3.Garbe C, Peris K, Hauschild A, et al. Diagnosis and treatment of melanoma. European consensus-based interdisciplinary guideline—update 2016. Eur J Cancer. 2016;63:201–217. doi: 10.1016/j.ejca.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 4.Mistry M, Parkin DM, Ahmad AS, Sasieni P. Cancer incidence in the United Kingdom: projections to the year 2030. Br J Cancer. 2011;105(11):1795–1803. doi: 10.1038/bjc.2011.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karimkhani C, Boyers LN, Dellavalle RP, Weinstock MA. It’s time for “keratinocyte carcinoma” to replace the term “nonmelanoma skin cancer”. J Am Acad Dermatol. 2015;72(1):186–187. doi: 10.1016/j.jaad.2014.09.036. [DOI] [PubMed] [Google Scholar]
- 6.Cancer Research UK. Non-melanoma skin cancer statistics. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/non-melanoma-skin-cancer#heading-Zero. Accessed 30 Aug 2019.
- 7.Karia PS. Epidemiology and outcomes of cutaneous squamous cell carcinoma. In: Schmults CD, editor. High-risk cutaneous squamous cell carcinoma: a practical guide for patient management. Berlin: Springer; 2016. pp. 3–28. [Google Scholar]
- 8.Hiom SC. Diagnosing cancer earlier: reviewing the evidence for improving cancer survival. Br J Cancer. 2015;112(s1):S1–S5. doi: 10.1038/bjc.2015.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hamilton W, Stapley S, Campbell C, Lyratzopoulos G, Rubin G, Neal RD. For which cancers might patients benefit most from expedited symptomatic diagnosis? Construction of a ranking order by a modified Delphi technique. BMC Cancer. 2015;15(1):820. doi: 10.1186/s12885-015-1865-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Swann R, McPhail S, Witt J, et al. Diagnosing cancer in primary care: results from the national cancer diagnosis audit. Br J Gen Pract. 2018;68(666):e63–e72. doi: 10.3399/bjgp17X694169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Public Health England. National Cancer Intelligence Network Be Clear on Cancer: skin cancer awareness local pilot campaign. Interim evaluation results. 2016. London: Public Health England.
- 12.Cancer Research UK. Melanoma skin cancer incidence statistics. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/melanoma-skin-cancer/incidence. Accessed 30 Aug 2019.
- 13.Brown KF, Rumgay H, Dunlop C, et al. The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br J Cancer. 2018;118(8):1130–1141. doi: 10.1038/s41416-018-0029-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cancer Research UK. Melanoma skin cancer risk. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/melanoma-skin-cancer/risk-factors#heading-Two. Accessed 30 Aug 2019.
- 15.Cameron MC, Lee E, Hibler BP, et al. Basal cell carcinoma: epidemiology; pathophysiology; clinical and histological subtypes; and disease associations. J Am Acad Dermatol. 2019;80(2):303–317. doi: 10.1016/j.jaad.2018.03.060. [DOI] [PubMed] [Google Scholar]
- 16.Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: I. Common and atypical naevi. Eur J Cancer. 2005;41(1):28–44. doi: 10.1016/j.ejca.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 17.Diepgen TL, Mahler V. The epidemiology of skin cancer. Br J Dermatol. 2002;146(s61):1–6. doi: 10.1046/j.1365-2133.146.s61.2.x. [DOI] [PubMed] [Google Scholar]
- 18.Zak-Prelich M, Narbutt J, Sysa-Jedrzejowska A. Environmental risk factors predisposing to the development of basal cell carcinoma. Dermatol Surg. 2004;30(s2):248–252. doi: 10.1111/j.1524-4725.2004.30089.x. [DOI] [PubMed] [Google Scholar]
- 19.Kallini JR, Hamed N, Khachemoune A. Squamous cell carcinoma of the skin: epidemiology, classification, management, and novel trends. Int J Dermatol. 2015;54(2):130–140. doi: 10.1111/ijd.12553. [DOI] [PubMed] [Google Scholar]
- 20.Rubin AI, Chen EH, Ratner D. Basal-cell carcinoma. N Engl J Med. 2005;353(21):2262–2269. doi: 10.1056/NEJMra044151. [DOI] [PubMed] [Google Scholar]
- 21.Nikolaou V, Stratigos AJ, Tsao H. Hereditary nonmelanoma skin cancer. Semin Cutan Med Surg. 2012;31(4):204–210. doi: 10.1016/j.sder.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Institute for Health and Care Excellence. Sunlight exposure: risks and benefits. NG34. London: NICE; 2016.
- 23.Behavioral Counseling to Prevent Skin Cancer US preventive services task force recommendation statement. JAMA. 2018;319(11):1134–1142. doi: 10.1001/jama.2018.1623. [DOI] [PubMed] [Google Scholar]
- 24.National Institute for Health and Care Excellence. Melanoma and pigmented lesions—clinical knowledge summary. https://cks.nice.org.uk/melanoma-and-pigmented-lesions#!scenario. Accessed 30 Aug 2019.
- 25.The Royal Australian College of General Practitioners ‘Red Book’ Taskforce. Guidelines for preventive activities in general practice (“The Red Book”). 9th ed. South Melbourne: RACGP; 2018.
- 26.Williams AL, Grogan S, Clark-Carter D, Buckley E. Appearance-based interventions to reduce ultraviolet exposure and/or increase sun protection intentions and behaviours: a systematic review and meta-analyses. Br J Health Psychol. 2013;18(1):182–217. doi: 10.1111/j.2044-8287.2012.02089.x. [DOI] [PubMed] [Google Scholar]
- 27.Cancer Research UK. Sun, UV and cancer. https://www.cancerresearchuk.org/about-cancer/causes-of-cancer/sun-uv-and-cancer. Accessed 30 Aug 2019.
- 28.Wolff T, Tai E, Miller T. Screening for skin cancer : an update of the evidence for the US. Preventive services task force. Ann Intern Med. 2009;150:194–198. doi: 10.7326/0003-4819-150-3-200902030-00009. [DOI] [PubMed] [Google Scholar]
- 29.Johansson M, Brodersen J, Gotzsche PC, Jorgensen KJ. Screening for reducing morbidity and mortality in malignant melanoma. Cochrane Database Syst Rev. 2019;(6):CD012352. [DOI] [PMC free article] [PubMed]
- 30.Williams LH, Shors AR, Barlow WE, Solomon C, White E. Identifying persons at highest risk of melanoma using self-assessed risk factors. J Clin Exp Dermatol Res. 2011;2(6):1000129. [DOI] [PMC free article] [PubMed]
- 31.Usher-Smith JA, Emery J, Kassianos AP, Walter FM. Risk prediction models for melanoma: a systematic review. Cancer Epidemiol Biomarkers Prev. 2014;23(8):1450–1463. doi: 10.1158/1055-9965.EPI-14-0295. [DOI] [PubMed] [Google Scholar]
- 32.Usher-Smith JA, Kassianos AP, Emery JD, et al. Identifying people at higher risk of melanoma across the UK: a primary-care-based electronic survey. Br J Dermatol. 2017;176(4):939–948. doi: 10.1111/bjd.15181. [DOI] [PubMed] [Google Scholar]
- 33.Hill L, Ferrini RL. Skin cancer prevention and screening: summary of the American College of Preventive Medicine’s practice policy statements. CA Cancer J Clin. 2008;48(4):232–235. doi: 10.3322/canjclin.48.4.232. [DOI] [PubMed] [Google Scholar]
- 34.Hoorens I, Vossaert K, Ongenae K, Brochez L. Is early detection of basal cell carcinoma worthwhile? Systematic review based on the WHO criteria for screening. Br J Dermatol. 2016;174(6):1258–1265. doi: 10.1111/bjd.14477. [DOI] [PubMed] [Google Scholar]
- 35.Walter FM, Birt L, Cavers D, et al. “This isn’t what mine looked like”: a qualitative study of symptom appraisal and help seeking in people recently diagnosed with melanoma. BMJ Open. 2014;4(7):1–12. doi: 10.1136/bmjopen-2014-005566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Markovic S, Erickson L, Rao R, et al. Malignant melanoma in the 21st century, part 1: epidemiology, risk factors, screening, prevention, and diagnosis. Mayo Clin Proc. 2007;82(3):364–380. doi: 10.4065/82.3.364. [DOI] [PubMed] [Google Scholar]
- 37.Chamberlain A, Ng J. Cutaneous melanoma–atypical variants and presentations. Aust Fam Physician. 2009;38(7):476–482. [PubMed] [Google Scholar]
- 38.Thomas NE, Kricker A, Waxweiler WT, et al. Comparison of clinicopathologic features and survival of histopathologically amelanotic and pigmented melanomas: a population-based study. JAMA Dermatol. 2014;150(12):1306–1314. doi: 10.1001/jamadermatol.2014.1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Muinonen-Martin AJ, O’Shea SJ, Newton-Bishop J. Amelanotic melanoma. BMJ. 2018;360:k826. doi: 10.1136/bmj.k826. [DOI] [PubMed] [Google Scholar]
- 40.Newton-Bishop J, Bataille V, Gavin, et al. The prevention, diagnosis, referral and management of melanoma of the skin: concise guidelines. Royal College of Physicians & British Association of Dermatologists. Concise guidance to good practice series, no. 7. London: RCP; 2007. [DOI] [PMC free article] [PubMed]
- 41.National Institute for Health and Care Excellence. Suspected cancer: recognition and referral. NG12. London: NICE; 2015. [PubMed]
- 42.Walter FM, Prevost AT, Vasconcelos J, et al. Using the 7-point checklist as a diagnostic aid for pigmented skin lesions in general practice: a diagnostic validation study. Br J Gen Pract. 2013;63(610):e345–e353. doi: 10.3399/bjgp13X667213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ward WH, Lambreton F, Goel N, Yu JQ, Farma JM. Clinical presentation and staging of melanoma. Cutaneous melanoma: etiology and therapy. Brisbane: Codon; 2017. [PubMed] [Google Scholar]
- 44.Friedman RJ, Rigel DS, Kopf AW. Early detection of malignant melanoma: the role of physician examination and self-examination of the skin. CA Cancer J Clin. 1985;35(3):130–151. doi: 10.3322/canjclin.35.3.130. [DOI] [PubMed] [Google Scholar]
- 45.National Institute for Health and Care Excellence. Cancer services guideline: improving outcomes for people with skin tumours including melanoma. CSG8. London: NICE; 2006. [PubMed]
- 46.Murchie P, Adam R, Khor WL, et al. Impact of rurality on processes and outcomes in melanoma care: results from a whole-Scotland melanoma cohort in primary and secondary care. Br J Gen Pract. 2018;68(673):e566–e575. doi: 10.3399/bjgp18X697901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Krengel S, Scope A, Dusza SW, Vonthein R, Marghoob AA. New recommendations for the categorization of cutaneous features of congenital melanocytic nevi. J Am Acad Dermatol. 2013;68(3):441–451. doi: 10.1016/j.jaad.2012.05.043. [DOI] [PubMed] [Google Scholar]
- 48.Rowe DE, Carroll RJ, Day CL. Prognostic factors for local recurrence, metastasis, and survival rates in squamous cell carcinoma of the skin, ear, and lip: implications for treatment modality selection. J Am Acad Dermatol. 1992;26(6):976–990. doi: 10.1016/0190-9622(92)70144-5. [DOI] [PubMed] [Google Scholar]
- 49.Motley RJ, Preston PW, Lawrence CM. Multi-professional guidelines for the management of the patient with primary cutaneous squamous cell carcinoma. London: British Association of Dermatologists; 2009.
- 50.Primary Care Dermatology Society. Squamous cell carcinoma. http://www.pcds.org.uk/clinical-guidance/squamous-cell-carcinoma. Accessed 30 Aug 2019.
- 51.New Zealand Guidelines Group . Suspected cancer in primary care. Wellington: Ministry of Health; 2009. [Google Scholar]
- 52.Kwiek B, Schwartz RA. Keratoacanthoma (KA): an update and review. J Am Acad Dermatol. 2016;74(6):1220–1233. doi: 10.1016/j.jaad.2015.11.033. [DOI] [PubMed] [Google Scholar]
- 53.National Institute for Health and Care Excellence. Improving outcomes for people with skin tumours including melanoma: evidence update October 2011. London: NICE; 2011. [PubMed]
- 54.Mcclain SE, Mayo KB, Shada AL, Smolkin ME, Patterson JW, Slingluff CL. Amelanotic melanomas presenting as red skin lesions: a diagnostic challenge with potentially lethal consequences. Int J Dermatol. 2012;51(4):420–426. doi: 10.1111/j.1365-4632.2011.05066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Maloney ME, Jones DB, Mack Sexton F. Pigmented basal cell carcinoma: investigation of 70 cases. J Am Acad Dermatol. 1992;27(1):74–78. doi: 10.1016/0190-9622(92)70160-h. [DOI] [PubMed] [Google Scholar]
- 56.Salasche SJ, Amonette RA. Morpheaform basal-cell epitheliomas. J Dermatol Surg Oncol. 1981;7(5):387–394. doi: 10.1111/j.1524-4725.1981.tb00662.x. [DOI] [PubMed] [Google Scholar]
- 57.Royal College of General Practitioners. Guidance and competences to support the accreditation of GPs with Extended Roles (GPwERs) in dermatology and skin surgery. London: RCP; 2018.
- 58.Rosendahl C, Cameron A, McColl I, Wilkinson D. Dermatoscopy in routine practice—“chaos and clues”. Aust Fam Physician. 2012;41(7):482–487. [PubMed] [Google Scholar]
- 59.National Institute for Health and Care Excellence. Melanoma: assessment and management. NG14. London: NICE; 2015. [PubMed]
- 60.Argenziano G, Cerroni L, Zalaudek I, et al. Accuracy in melanoma detection: a 10-year multicenter survey. J Am Acad Dermatol. 2012;67(1):54–59. doi: 10.1016/j.jaad.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 61.Dinnes J, Deeks JJ, Chuchu N, et al. Visual inspection and dermoscopy, alone or in combination, for diagnosing keratinocyte skin cancers in adults. Cochrane Database Syst Rev. 2018;(12):CD011901. 10.1002/14651858.cd011901.pub2. [DOI] [PMC free article] [PubMed]
- 62.Dinnes J, Deeks JJ, Chuchu N, et al. Dermoscopy, with and without visual inspection, for diagnosing melanoma in adults. Cochrane Database Syst Rev. 2018;(12):CD011902. 10.1002/14651858.cd011902.pub2. [DOI] [PMC free article] [PubMed]
- 63.Jones O, Jurascheck L, van Melle M, et al. Dermoscopy for melanoma detection and triage in primary care: a systematic review. BMJ Open. 2019;9(8):e027529. doi: 10.1136/bmjopen-2018-027529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chuchu N, Dinnes J, Takwoingi Y, et al. Teledermatology for diagnosing skin cancer in adults. Cochrane Database Syst Rev. 2018;(12):CD013193. 10.1002/14651858.cd013193. [DOI] [PMC free article] [PubMed]
- 65.Walter FM, Morris HC, Humphrys E, et al. Effect of adding a diagnostic aid to best practice to manage suspicious pigmented lesions in primary care: randomised controlled trial. BMJ. 2012;345(7866):e4110. doi: 10.1136/bmj.e4110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wilson ECF, Emery JD, Kinmonth AL, et al. The cost-effectiveness of a novel SIAscopic diagnostic aid for the management of pigmented skin lesions in primary care: a decision-analytic model. Value Health. 2013;16(2):356–366. doi: 10.1016/j.jval.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 67.Fujisawa Y, Otomo Y, Ogata Y, et al. Deep-learning-based, computer-aided classifier developed with a small dataset of clinical images surpasses board-certified dermatologists in skin tumour diagnosis. Br J Dermatol. 2019;180(2):373–381. doi: 10.1111/bjd.16924. [DOI] [PubMed] [Google Scholar]
- 68.Tschandl Philipp, Codella Noel, Akay Bengü Nisa, Argenziano Giuseppe, Braun Ralph P, Cabo Horacio, Gutman David, Halpern Allan, Helba Brian, Hofmann-Wellenhof Rainer, Lallas Aimilios, Lapins Jan, Longo Caterina, Malvehy Josep, Marchetti Michael A, Marghoob Ashfaq, Menzies Scott, Oakley Amanda, Paoli John, Puig Susana, Rinner Christoph, Rosendahl Cliff, Scope Alon, Sinz Christoph, Soyer H Peter, Thomas Luc, Zalaudek Iris, Kittler Harald. Comparison of the accuracy of human readers versus machine-learning algorithms for pigmented skin lesion classification: an open, web-based, international, diagnostic study. The Lancet Oncology. 2019;20(7):938–947. doi: 10.1016/S1470-2045(19)30333-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dinnes J, Bamber J, Chuchu N, et al. High frequency ultrasound for the diagnosis of skin cancer in adults. Cochrane Database Syst Rev. 2018;(12):CD013188. 10.1002/14651858.cd013188. [DOI] [PMC free article] [PubMed]
- 70.Ferrante di Ruffano L, Dinnes J, Deeks JJ, et al. Optical coherence tomography for the diagnosis of skin cancer in adults. Cochrane Database Syst Rev. 2018;(12):CD013189. 10.1002/14651858.cd013189. [DOI] [PMC free article] [PubMed]
- 71.Dinnes J, Deeks JJ, Chuchu N, et al. Reflectance confocal microscopy for the diagnosis of cutaneous melanoma in adults. Cochrane Database Syst Rev. 2018;(12):CD013190. 10.1002/14651858.cd013190. [DOI] [PMC free article] [PubMed]
- 72.Ferrante di Ruffano L, Takwoingi Y, Dinnes J, et al. Computer-assisted diagnosis techniques (dermoscopy and spectroscopy-based) for diagnosing skin cancer in adults. Cochrane Database Syst Rev. 2018;(12):CD013186. 10.1002/14651858.cd013186. [DOI] [PMC free article] [PubMed]
- 73.Mogensen M, Jemec GBE. Diagnosis of nonmelanoma skin cancer/keratinocyte carcinoma: a review of diagnostic accuracy of nonmelanoma skin cancer diagnostic tests and technologies. Dermatol Surg. 2007;33(10):1158–1174. doi: 10.1111/j.1524-4725.2007.33251.x. [DOI] [PubMed] [Google Scholar]