Abstract
Background:
Spinal cord injury (SCI) carries debilitating lifelong consequences and, therefore, requires careful review of different treatment strategies.
Methods:
An extensive review of the English literature (PubMed 1990 and 2019) was performed regarding recent advances in the treatment of SCI; this included 46 articles written over 28 years.
Results:
Results of this search were divided into five major modalities; neuroprotective and neuroregenerative pharmaceuticals, neuromodulation, stem cell-based therapies, and various external prosthetic devices. Lately, therapeutic strategies were mainly focused on two major areas: neuroregeneration and neuroprotection.
Conclusion:
Despite recent advancements, more clinical trials on a larger scale and further research are needed to provide better treatment modalities of this devastating neurological disease.
Keywords: Exoskeleton, Neuromodulation, Spinal cord injury, Spine, Stem cells, Trauma

INTRODUCTION
Spinal cord injury (SCI) is a devastating illness resulting in neurological deficits and poor quality of life. It has an annual incidence of 15–40 cases per million and a prevalence of more than 1 million cases in North America.[12] The incidence and prevalence of traumatic SCI is expected to increase as the population ages, particularly secondary to traumatic falls in the elderly.[45] The annual cost of SCI exceeds 7 billion dollars.[12]
This literature review focuses on the advances in pharmacology, stem cell technologies, neuromodulation, and external prosthetics. Several pharmacological therapies have already been tested in the past and are currently being investigated. Further, both neuroprotective and neuroregenerative drugs are being implemented in clinical trials.[45] Stem cell therapy trials are also ongoing, but more data are needed from Phase II clinical trials to document efficacy.
MATERIALS AND METHODS
Peer-reviewed articles were searched through PubMed using search terms “acute SCI,” “SCI treatment,” “neuromodulation,” “stem cell therapy for SCI,” “SCI pharmaceuticals,” and “SCI exoskeleton from 1990 to 2019 (English journals). Using appropriate inclusion and exclusion criteria, 46 peer-reviewed articles were used. All studies focused on current advancements in the management of SCI, including stem cell therapies, neuromodulation, and external prosthetics.
RESULTS AND DISCUSSION
Neuroprotective and neuroregenerative pharmaceuticals [Tables 1 and 2]
Table 1:
Neuroprotective pharmaceuticals.
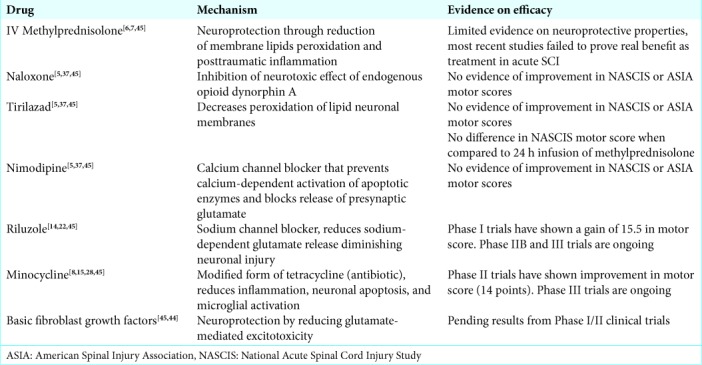
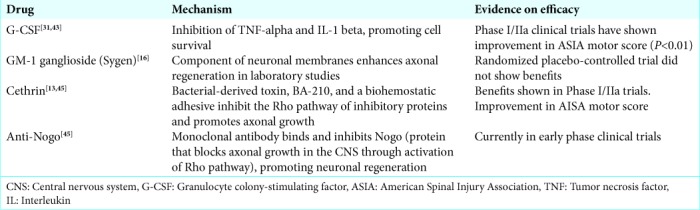
Table 2:
Neuroregenerative pharmaceuticals.
Methylprednisolone
Several neuroprotective and neuroregenerative pharmaceutical drugs have been investigated for SCI management. A well-known neuroprotective agent, methylprednisolone, has been associated with improved neurological outcomes. It decreases the peroxidation of membrane lipids and posttraumatic inflammation.[45] Despite its effects in preclinical settings, it does still remain controversial in the clinical setting. A Cochrane review found no significant effect for a high-dose 24 h infusion of methylprednisolone in terms of motor recovery at 6 months.[7,45] However, when started within 8 h after injury, an additional 4-point improvement in National Acute SCI Study (NASCIS) motor score was seen.[7,45] Its association with increased rates of gastrointestinal hemorrhage and wound infections also adds to its controversy.[7,45] A randomized controlled trial evaluating high-dose 48 h infusion showed no difference in NASCIS motor score recovery versus 24 h infusion.[6,45] The guidelines now suggest that methylprednisolone infusion within 8 h of injury should be performed only in certain situations, taking into consideration the associated complications.[27,45]
Naloxone, tirilazad, and nimodipine
Three drugs, naloxone, tirilazad, and nimodipine, were studied for their neuroprotective abilities. They all have Phase III randomized controlled trials which have not shown any difference in NASCIS motor score recovery or the American Spinal Injury Association (ASIA) motor score between treatment and placebo groups.[5,6,27,37,45] Tirilazad is a nonglucocorticoid 21-aminosteroid that attenuates peroxidation of neuronal lipid membranes. Tirilazad had no difference in NASCIS motor score between tirilazad and 24 h infusion of methylprednisolone.[6,45] The neuroprotective value of naloxone is believed to be due to blockage of the neurotoxic effects of the endogenous opioid dynorphin A. Nimodipine is a calcium channel blocker that inhibits calcium-dependent activation of lytic cellular enzymes as well as presynaptic glutamate release.[5,37,45]
Riluzole
Riluzole, a sodium channel blocker approved for the treatment of amyotrophic lateral sclerosis, has been studied in preclinical models of SCI. It diminishes secondary injury by blocking activation of sodium channels and reducing release of neuronal glutamate.[41,45] Phase I/II trials evaluating the safety and pharmacokinetics of riluzole began in humans in 2010 and were completed in 2012.[14,22,45] In the Phase I trial, a gain of 15.5 points in motor score for patients with cervical injuries was found for the riluzole group of 24 patients over the comparison registry group of 26 patients.[22] At 180 days, there was a gain of 31.2 points for patients with cervical injuries for 24 riluzole patients and of 15.7 points for 26 registry patients.[22] There was a gain of 9 points in pinprick scores in riluzole patients with complete or incomplete cervical injuries versus registry patients.[22] A Phase IIB/III double-blinded randomized controlled trial was started in 2014 looking at the safety and neuroprotective efficacy of riluzole in patients with acute cervical SCI. These results will provide Class I evidence regarding the use of riluzole.
Minocycline
Minocycline, a modified form of tetracycline, is another neuroprotective agent that has shown some promise in animal models.[15,45] In animal models of SCI, it has been shown that minocycline decreases neuronal and oligodendrocytes apoptosis, microglial activation in addition to anti-inflammatory effects.[15] In randomized controlled Phase II clinical trials, minocycline was associated with 14-point gain in motor score over placebo in patients with cervical SCI.[8,22,45] Pinprick scores in these motor-incomplete patients were 14 points higher than placebo.[22,28,45] Phase III clinical trials will be able to provide further evidence regarding its use.
Fibroblast growth factor
Basic fibroblast growth factor has shown to provide neuroprotection by improving functional and respiratory parameters in animal models by reducing glutamate-mediated excitotoxicity.[44,45] There are current Phase I/II trials that are further investigating this therapy. Furthermore, cytokine granulocyte colony-stimulating factor which inhibits tumor necrosis factor-alpha and interleukin-1 beta, promoting cell survival has shown benefits in two nonrandomized studies.[31,43]
GM-1 ganglioside (Sygen)
A neuroregenerative agent, GM-1 ganglioside (Sygen) has been shown to enhance axonal regeneration in laboratory studies.[45] Gangliosides are important glycolipid molecules that are components of neuronal membranes. Randomized placebo-controlled trial using this agent did not show any difference in neurological recovery in patients at 6 months.[16,45]
Cethrin
Cethrin is a permeable paste that can be applied to spinal cord dura postinjury that is a combination of a bacterial-derived toxin, BA-210, and a biohemostatic adhesive. It inhibits the Rho pathway of inhibitory proteins and promotes axonal growth in vitro.[45] Phase I/IIa trials were done where it was applied to dura in patients with complete injuries, and no complications were seen at 1-year follow-up.[13,45] In fact, in patients with cervical injuries receiving cethrin, there was an improvement in ASIA motor score.[45]
Anti-Nogo
Another neuroregenerative drug, anti-Nogo, is a monoclonal antibody made to bind to Nogo-A, and has been shown to promote neural regeneration.[45] Nogo-A is a protein that blocks axonal growth in the central nervous system.[45] This anti-Nogo agent is still under investigation. Many of these neuroprotective and neuroregenerative agents have shown promising results and future studies will be helpful in establishing their efficacy.
Neuromodulation [Table 3]
Table 3:
Other modalities; neuromodulation, stem-cell transplant, and prosthetic devices.
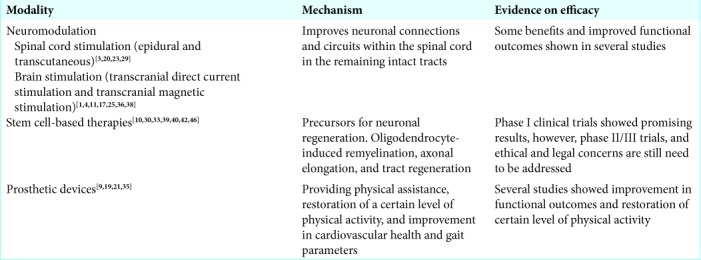
It is well known that neuromodulation, the use of electrical stimulation to alter neuronal circuitry, has been tried in various neurological disorders including SCI. Neuroplasticity-mediated functional recruitment of axons (particularly spared axons) to potentiate sprouting, regeneration, and formation of new interconnections between neurons forms the basis of modern neuromodulation techniques. This is complemented with the presence of some intact ascending and descending circuits in patients with SCI, making neuromodulation a feasible option.[29] Spinal cord stimulation, one of the forms of neuromodulation, is a rapidly growing method for SCI. For spinal cord stimulation, epidural or transcutaneous method may be used, and clinical studies have already demonstrated some improvement in motor function with these methods. [3,20,23] Besides, spinal cord stimulation techniques, brain stimulation, and peripheral nerve stimulation are other approaches to neuromodulation in SCI.[29] Several studies have demonstrated functional improvement in volitional movements of lower limbs and hand dexterity in patients with SCI.[3,17] However, whether neuromodulation is affordable and accessible to all patients remains a major challenge.[29]
Activity-dependent plasticity
Moreover, the concept of activity-dependent plasticity has been recently employed to achieve substantial improvements in motor function, based on the recent finding that neurorehabilitation is the only treatment option which can be offered to SCI patients for long-term improvement in motor function.[26] In this model, high-intensity training combined with electrical neuromodulation has shown to improve neuronal connections and circuits within the spinal cord by working synergistically at least in a subpopulation of patients.[26] This holds great promise for recovery of motor function after SCI.
Spinal cord stimulation
With respect to spinal cord stimulation, epidural spinal stimulation has well been tested in patients with chronic pain and most recently in patients with SCI. This method involves surgical placement of electrodes onto the dorsal surface of the spinal cord.[29] Several studies utilizing neuromodulation in patients with SCI ASIA A and B demonstrated an improved ability to make lower extremity voluntary movements following epidural stimulation of their spinal cord.[3,20,23] Moreover, with respect to the effects on upper body, one case study demonstrated improvements in handgrip strength and motor strength of the upper extremities in patients following epidural spinal stimulation once a day.[34] Unlike the epidural method, transcutaneous stimulation is another method and is a noninvasive approach to spinal cord stimulation. It involves placement of electrodes onto the skin surface of a patient. Aside from experimental studies on animals, more clinical trials and studies are needed to fully ascertain the advantages as well as long-term side effects of spinal cord stimulation for SCI.[29]
Brain stimulation for SCI
Brain stimulation for SCI is also currently being employed. Transcranial direct current stimulation and transcranial magnetic stimulation are two main approaches that are being used to augment the neuronal plasticity between the spinal cord and the brain in individuals with SCI.[29] Several studies have already demonstrated to improve functional outcomes from using transcranial direct current stimulation in patients with motor complete SCI.[17,36,38] Transcranial direct current stimulation is a noninvasive method to deliver direct current with the use of scalp electrodes.[17] Transcranial magnetic stimulation is another noninvasive approach that delivers magnetic waves to the brain and has shown improvements in hand function in studies on patients with tetraplegia. Fine motor tasks and handgrip strength improved with the use of transcranial magnetic stimulation.[2,18] Transcranial magnetic stimulation can also have a positive impact on patient’s walking speed as evidenced by one of the trials.[32] Larger scale trials are needed to assess these promising results. In addition, although deep brain stimulation has already been tested in experimental studies on animals, its potential in treating patients with SCI still needs to be elucidated with clinical trials and further research.[24]
Brain–machine interfaces
Brain–machine interfaces are another modern tool for patients with SCI. These devices, which can be used to control various prosthetic devices such as the exoskeleton as well as directly stimulate paralyzed muscles, have already demonstrated improved outcomes in patients with SCI through several recent studies.[1,4,11,25] Clinical trials for the use of brain–machine interfaces and their computer algorithms are ever increasing as further research into advances in technology, feasibility and accessibility of these devices are still needed. In conclusion, due to increasing promising results, neuromodulation for SCI will remain a rapidly growing field in the upcoming years.
Stem cell-based therapies [Table 3]
Stem cell-based therapies and cellular scaffolds have yielded promising progress with respect to neuronal repair.[10] Phase I clinical trials have demonstrated that transplantation of olfactory ensheathing cells can be a safe, promising option to aid in neuronal repair in patients with SCI, but more Phase II clinical trials are still needed.[33,42] Several trials have also demonstrated the safe use of transplanted neuroprotective Schwann cells for nerve repair in patients with SCI, but clinical trials assessing the actual efficacy of this method are still ongoing.[39,40,46] In addition, several clinical trials have also demonstrated safety in using stem cells from various sources for SCI, but there are many more that are in the process of recruiting patients for transplantation of various stem cells.[10] Ethical and tumorigenesis concerns with stem cell-based therapies, however, will certainly need to be addressed as their research evolves.[10]
In vitro manipulation of the embryonic stem cells (ESCs)
Recently, in vitro manipulation of the ESCs differentiation to neuronal and glial lineages under controlled conditions has shown promising results after transplantation in animal models of acute SCI.[30] These included oligodendrocyte- induced remyelination, axonal elongation, and tract regeneration. However, legal and ethical drawbacks have limited the employment of ESC in the treatment of SCI patients. This might be largely attributed to the destruction of the blastocyst on isolation of the cells.[30] Moreover, development of teratomas after ESCs transplantation in numerous animal models has raised significant concerns about the functionality of these cells as a potential therapeutic avenue in SCI management.[30]
Various cell-based therapies
Despite extensive research exploring various cell-based therapies such as transplantation of oligodendrocyte precursors, induced pluripotent stem cells, bone marrow-derived (BM-MSCs), adipose-derived (AD-MSCs), and umbilical cord (U-MSCs),[30] there have been a lack of large Phase III clinical trials investigating the therapeutic efficacy of stem cell therapy.
Prosthetic devices [Table 3]
Robotic exoskeletons or powered exoskeletons have emerged as an advantageous rehabilitation tool for certain disabled individuals with SCI. The studies provided preliminary evidence on efficacy of exoskeletons on cardiovascular health, energy expenditure, body composition, gait parameters, level of physical activity, neuropathic pain level, and quality of life. They can be used to restore a certain level of physical activity years after injury.[9,19,35] Body weight supported treadmill training and locomotion training with driven gait orthosis are now considered essential component in the rehabilitation of SCI patients. According to the meta-analysis of powered exoskeletons, <5% of SCI patients have the ability to ambulate without any physical assistance.[35] However, following an exoskeleton training program, 67% of patients were able to walk with exoskeleton-assisted ambulation without physical assistance.[35] This meta-analysis included exoskeletons such as ReWalkTM, EksoTM, and IndegoTM. In addition, even in complex training situations, there were no adverse events, falls, or fractures.[35] Furthermore, the neurologically controlled exoskeleton HALTM has recently been Food and Drug Administration approved for use in the United States. This system has been proven to be beneficial in the rehabilitation of patients with chronic spinal cord injuries.[21] This technology is constantly being evolved, and it is important to strive for an interdisciplinary team approach to provide greater accessibility to this technology. This might help patients to preserve the physical capacity before restoration becomes necessary. The future of prosthetic devices is bright for SCI patients and will continue to be investigated.
CONCLUSION
We investigated the advancements in neuroprotective pharmacology, stem cell technologies, neuromodulation, and various external prosthetics for the treatment of SCI. However, more clinical trials and research will continue to establish their efficacy.
Footnotes
How to cite this article: Shah M, Peterson C, Yilmaz E, Halalmeh DR, Moisi M. Current advancements in the management of spinal cord injury: A comprehensive review of literature. Surg Neurol Int 2020;11:2.
Contributor Information
Manan Shah, Email: manan.shah3@wayne.edu.
Catherine Peterson, Email: catherine.peterson@wayne.edu.
Emre Yilmaz, Email: emre.yilmaz@gmx.de.
Dia Radi Halalmeh, Email: deaa_h1@yahoo.com.
Marc Moisi, Email: moisimd@aol.com.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ajiboye AB, Willett FR, Young DR, Memberg WD, Murphy BA, Miller JP, et al. Restoration of reaching and grasping movements through brain-controlled muscle stimulation in a person with tetraplegia: A proof-of-concept demonstration. Lancet. 2017;389:1821–30. doi: 10.1016/S0140-6736(17)30601-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alexeeva N, Calancie B. Efficacy of quadropulse rTMS for improving motor function after spinal cord injury: Three case studies. J Spinal Cord Med. 2016;39:50–7. doi: 10.1179/2045772314Y.0000000279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Angeli CA, Edgerton VR, Gerasimenko YP, Harkema SJ. Altering spinal cord excitability enables voluntary movements after chronic complete paralysis in humans. Brain. 2014;137:1394–409. doi: 10.1093/brain/awu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bouton CE, Shaikhouni A, Annetta NV, Bockbrader MA, Friedenberg DA, Nielson DM, et al. Restoring cortical control of functional movement in a human with quadriplegia. Nature. 2016;533:247–50. doi: 10.1038/nature17435. [DOI] [PubMed] [Google Scholar]
- 5.Bracken MB, Shepard MJ, Collins WF, Holford TR, Young W, Baskin DS, et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the second national acute spinal cord injury study. N Engl J Med. 1990;322:1405–11. doi: 10.1056/NEJM199005173222001. [DOI] [PubMed] [Google Scholar]
- 6.Bracken MB, Shepard MJ, Holford TR, Leo-Summers L, Aldrich EF, Fazl M, et al. Administration of methylprednisolone for 24 or 48 hours or tirilazad mesylate for 48 hours in the treatment of acute spinal cord injury. Results of the third national acute spinal cord injury randomized controlled trial. National Acute Spinal Cord Injury Study. JAMA. 1997;277:1597–604. [PubMed] [Google Scholar]
- 7.Bracken MB. Steroids for acute spinal cord injury. Cochrane Database Syst Rev. 2002;3:CD001046. doi: 10.1002/14651858.CD001046. [DOI] [PubMed] [Google Scholar]
- 8.Casha S, Zygun D, McGowan MD, Bains I, Yong VW, Hurlbert RJ. Results of a phase II placebo-controlled randomized trial of minocycline in acute spinal cord injury. Brain. 2012;135:1224–36. doi: 10.1093/brain/aws072. [DOI] [PubMed] [Google Scholar]
- 9.Cruciger O, Schildhauer TA, Meindl RC, Tegenthoff M, Schwenkreis P, Citak M, et al. Impact of locomotion training with a neurologic controlled hybrid assistive limb (HAL) exoskeleton on neuropathic pain and health related quality of life (HRQoL) in chronic SCI: A case study. Disabil Rehabil Assist Technol. 2016;11:529–34. doi: 10.3109/17483107.2014.981875. [DOI] [PubMed] [Google Scholar]
- 10.Dalamagkas K, Tsintou M, Seifalian AM. Stem cells for spinal cord injuries bearing translational potential. Neural Regen Res. 2018;13:35–42. doi: 10.4103/1673-5374.224360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donati AR, Shokur S, Morya E, Campos DS, Moioli RC, Gitti CM, et al. Long-term training with a brain-machine interface-based gait protocol induces partial neurological recovery in paraplegic patients. Sci Rep. 2016;6:30383. doi: 10.1038/srep30383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fehlings MG, Nakashima H, Nagoshi N, Chow DS, Grossman RG, Kopjar B. Rationale, design and critical end points for the Riluzole in Acute Spinal Cord Injury Study (RISCIS): A randomized, double-blinded, placebo-controlled parallel multi-center trial. Spinal Cord. 2016;54:8–15. doi: 10.1038/sc.2015.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fehlings MG, Theodore N, Harrop J, Maurais G, Kuntz C, Shaffrey CI, et al. A phase I/IIa clinical trial of a recombinant Rho protein antagonist in acute spinal cord injury. J Neurotrauma. 2011;28:787–96. doi: 10.1089/neu.2011.1765. [DOI] [PubMed] [Google Scholar]
- 14.Fehlings MG, Wilson JR, Frankowski RF, Toups EG, Aarabi B, Harrop JS, et al. Riluzole for the treatment of acute traumatic spinal cord injury: Rationale for and design of the NACTN Phase I clinical trial. J Neurosurg Spine. 2012;17:151–6. doi: 10.3171/2012.4.AOSPINE1259. [DOI] [PubMed] [Google Scholar]
- 15.Festoff BW, Ameenuddin S, Arnold PM, Wong A, Santacruz KS, Citron BA. Minocycline neuroprotects, reduces microgliosis, and inhibits caspase protease expression early after spinal cord injury. J Neurochem. 2006;97:1314–26. doi: 10.1111/j.1471-4159.2006.03799.x. [DOI] [PubMed] [Google Scholar]
- 16.Geisler FH, Coleman WP, Grieco G, Poonian D, Sygen Study Group. The Sygen multicenter acute spinal cord injury study. Spine (Phila Pa 1976) 2001;26:S87–98. doi: 10.1097/00007632-200112151-00015. [DOI] [PubMed] [Google Scholar]
- 17.Gomes-Osman J, Field-Fote EC. Cortical vs. afferent stimulation as an adjunct to functional task practice training: A randomized. comparative pilot study in people with cervical spinal cord injury. Clin Rehabil. 2015;29:771–82. doi: 10.1177/0269215514556087. [DOI] [PubMed] [Google Scholar]
- 18.Gomes-Osman J, Field-Fote EC. Improvements in hand function in adults with chronic tetraplegia following a multi-day 10Hz rTMS intervention combined with repetitive task practice. J Neurol Phys Ther. 2015;39:23. doi: 10.1097/NPT.0000000000000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gorgey AS. Robotic exoskeletons: The current pros and cons. World J Orthop. 2018;9:112–9. doi: 10.5312/wjo.v9.i9.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grahn PJ, Lavrov IA, Sayenko DG, Van Straaten MG, Gill ML, Strommen JA, et al. Enabling task-specific volitional motor functions via spinal cord neuromodulation in a human with paraplegia. Mayo Clin Proc. 2017;92:544–54. doi: 10.1016/j.mayocp.2017.02.014. [DOI] [PubMed] [Google Scholar]
- 21.Grasmücke D, Zieriacks A, Jansen O, Fisahn C, Sczesny-Kaiser M, Wessling M, et al. Against the odds: What to expect in rehabilitation of chronic spinal cord injury with a neurologically controlled Hybrid Assistive Limb exoskeleton. A subgroup analysis of 55 patients according to age and lesion level. Neurosurg Focus. 2017;42:E15. doi: 10.3171/2017.2.FOCUS171. [DOI] [PubMed] [Google Scholar]
- 22.Grossman RG, Fehlings MG, Frankowski RF, Burau KD, Chow DS, Tator C, et al. A prospective, multicenter, phase I matched-comparison group trial of safety, pharmacokinetics, and preliminary efficacy of riluzole in patients with traumatic spinal cord injury. J Neurotrauma. 2014;31:239–55. doi: 10.1089/neu.2013.2969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harkema S, Gerasimenko Y, Hodes J, Burdick J, Angeli C, Chen Y, et al. Effect of epidural stimulation of the lumbosacral spinal cord on voluntary movement, standing, and assisted stepping after motor complete paraplegia: A case study. Lancet. 2011;377:1938–47. doi: 10.1016/S0140-6736(11)60547-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hentall ID, Gonzalez MM. Promotion of recovery from thoracic spinal cord contusion in rats by stimulation of medullary raphe or its midbrain input. Neurorehabil Neural Repair. 2012;26:374–84. doi: 10.1177/1545968311425178. [DOI] [PubMed] [Google Scholar]
- 25.Hochberg LR, Bacher D, Jarosiewicz B, Masse NY, Simeral JD, Vogel J, et al. Reach and grasp by people with tetraplegia using a neurally controlled robotic arm. Nature. 2012;485:372–5. doi: 10.1038/nature11076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hofer AS, Schwab ME. Enhancing rehabilitation and functional recovery after brain and spinal cord trauma with electrical neuromodulation. Curr Opin Neurol. 2019;32:828–35. doi: 10.1097/WCO.0000000000000750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hugenholtz H, Cass DE, Dvorak MF, Fewer DH, Fox RJ, Izukawa DM, et al. High-dose methylprednisolone for acute closed spinal cord injury only a treatment option. Can J Neurol Sci. 2002;29:227–35. doi: 10.1017/s0317167100001992. [DOI] [PubMed] [Google Scholar]
- 28.Hurlbert RJ. Methylprednisolone for acute spinal cord injury: An inappropriate standard of care. J Neurosurg. 2000;93:1–7. doi: 10.3171/spi.2000.93.1.0001. [DOI] [PubMed] [Google Scholar]
- 29.James ND, McMahon SB, Field-Fote EC, Bradbury EJ. Neuromodulation in the restoration of function after spinal cord injury. Lancet Neurol. 2018;17:905–17. doi: 10.1016/S1474-4422(18)30287-4. [DOI] [PubMed] [Google Scholar]
- 30.Jin MC, Medress ZA, Azad TD, Doulames VM, Veeravagu A. Stem cell therapies for acute spinal cord injury in humans: A review. Neurosurg Focus. 2019;46:E10. doi: 10.3171/2018.12.FOCUS18602. [DOI] [PubMed] [Google Scholar]
- 31.Kamiya K, Koda M, Furuya T, Kato K, Takahashi H, Sakuma T, et al. Neuroprotective therapy with granulocyte colony-stimulating factor in acute spinal cord injury: A comparison with high-dose methylprednisolone as a historical control. Eur Spine J. 2015;24:963–7. doi: 10.1007/s00586-014-3373-0. [DOI] [PubMed] [Google Scholar]
- 32.Kumru H, Benito-Penalva J, Valls-Sole J, Murillo N, Tormos JM, Flores C, et al. Placebo-controlled study of rTMS combined with Lokomat® gait training for treatment in subjects with motor incomplete spinal cord injury. Exp Brain Res. 2016;234:3447–55. doi: 10.1007/s00221-016-4739-9. [DOI] [PubMed] [Google Scholar]
- 33.Li L, Adnan H, Xu B, Wang J, Wang C, Li F, et al. Effects of transplantation of olfactory ensheathing cells in chronic spinal cord injury: A systematic review and meta-analysis. Eur Spine J. 2015;24:919–30. doi: 10.1007/s00586-014-3416-6. [DOI] [PubMed] [Google Scholar]
- 34.Lu DC, Edgerton VR, Modaber M, AuYong N, Morikawa E, Zdunowski S, et al. Engaging cervical spinal cord networks to reenable volitional control of hand function in tetraplegic patients. Neurorehabil Neural Repair. 2016;30:951–62. doi: 10.1177/1545968316644344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miller LE, Zimmermann AK, Herbert WG. Clinical effectiveness and safety of powered exoskeleton-assisted walking in patients with spinal cord injury: Systematic review with meta-analysis. Med Devices (Auckl) 2016;9:455–66. doi: 10.2147/MDER.S103102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murray LM, Edwards DJ, Ruffini G, Labar D, Stampas A, Pascual-Leone A, et al. Intensity dependent effects of transcranial direct current stimulation on corticospinal excitability in chronic spinal cord injury. Arch Phys Med Rehabil. 2015;96:S114–21. doi: 10.1016/j.apmr.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pointillart V, Petitjean ME, Wiart L, Vital JM, Lassié P, Thicoipé M, et al. Pharmacological therapy of spinal cord injury during the acute phase. Spinal Cord. 2000;38:71–6. doi: 10.1038/sj.sc.3100962. [DOI] [PubMed] [Google Scholar]
- 38.Raithatha R, Carrico C, Powell ES, Westgate PM, Chelette Ii KC, Lee K, et al. Non-invasive brain stimulation and robot-assisted gait training after incomplete spinal cord injury: A randomized pilot study. Neuro Rehabil. 2016;38:15–25. doi: 10.3233/NRE-151291. [DOI] [PubMed] [Google Scholar]
- 39.Saberi H, Firouzi M, Habibi Z, Moshayedi P, Aghayan HR, Arjmand B, et al. Safety of intramedullary Schwann cell transplantation for postrehabilitation spinal cord injuries: 2-year follow-up of 33 cases. J Neurosurg Spine. 2011;15:515–25. doi: 10.3171/2011.6.SPINE10917. [DOI] [PubMed] [Google Scholar]
- 40.Saberi H, Moshayedi P, Aghayan HR, Arjmand B, Hosseini SK, Emami-Razavi SH, et al. Treatment of chronic thoracic spinal cord injury patients with autologous Schwann cell transplantation: An interim report on safety considerations and possible outcomes. Neurosci Lett. 2008;443:46–50. doi: 10.1016/j.neulet.2008.07.041. [DOI] [PubMed] [Google Scholar]
- 41.Schwartz G, Fehlings MG. Secondary injury mechanisms of spinal cord trauma: A novel therapeutic approach for the management of secondary pathophysiology with the sodium channel blocker riluzole. Prog Brain Res. 2002;137:177–90. doi: 10.1016/s0079-6123(02)37016-x. [DOI] [PubMed] [Google Scholar]
- 42.Tabakow P, Raisman G, Fortuna W, Czyz M, Huber J, Li D, et al. Functional regeneration of supraspinal connections in a patient with transected spinal cord following transplantation of bulbar olfactory ensheathing cells with peripheral nerve bridging. Cell Transplant. 2014;23:1631–55. doi: 10.3727/096368914X685131. [DOI] [PubMed] [Google Scholar]
- 43.Takahashi H, Yamazaki M, Okawa A, Sakuma T, Kato K, Hashimoto M, et al. Neuroprotective therapy using granulocyte colony-stimulating factor for acute spinal cord injury: A phase I/IIa clinical trial. Eur Spine J. 2012;21:2580–7. doi: 10.1007/s00586-012-2213-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Teng YD, Mocchetti I, Taveira-DaSilva AM, Gillis RA, Wrathall JR. Basic fibroblast growth factor increases long-term survival of spinal motor neurons and improves respiratory function after experimental spinal cord injury. J Neurosci. 1999;19:7037–47. doi: 10.1523/JNEUROSCI.19-16-07037.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wilson JR, Forgione N, Fehlings MG. Emerging therapies for acute traumatic spinal cord injury. CMAJ. 2013;185:485–92. doi: 10.1503/cmaj.121206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhou XH, Ning GZ, Feng SQ, Kong XH, Chen JT, Zheng YF, et al. Transplantation of autologous activated Schwann cells in the treatment of spinal cord injury: Six cases, more than five years of follow-up. Cell Transplant. 2012;21(Suppl 1):S39–47. doi: 10.3727/096368912X633752. [DOI] [PubMed] [Google Scholar]


