Abstract
Introduction
Trigger finger is ten times less common than trigger thumb in infants and children and, unlike trigger thumb, may arise from a variety of underlying causes. To our knowledge, we describe the first case of pediatric trigger finger secondary to an extraskeletal chondroma.
Case Presentation
We report the case of an 11-year-old girl presenting with a typical history of triggering of the fourth finger, in whom a nodule attached to the flexor digitorum superficialis was found; clinical, ultrasound, and operative findings are described. Histological analysis was diagnostic of extraskeletal chondroma, also known as chondroma of soft tissues.
Conclusion
This is a very uncommon benign cartilaginous tumor, mostly reported in patients aged 30 to 60 years (just one pediatric extraskeletal chondroma of the hand has been described), and presentation with trigger finger has been reported just once, in a 76-year-old man. This condition should be considered in the differential diagnosis of pediatric trigger finger.
1. Introduction
Trigger finger is ten times less common than trigger thumb in infants and children [1].
Unlike trigger thumb, pediatric trigger finger may arise from a variety of underlying anatomic causes, including nodularity or thickening of the flexor digitorum superficialis (FDS) or flexor digitorum profundus (FDP) tendons, abnormal relationships between the FDS and FDP tendons, proximal FDS decussation, and constriction of the A1, A2, or A3 pulleys. More uncommon causes include intratendinous calcification, granulation tissue, cysts, and the association with mucopolysaccharide storage disorders (Hurler syndrome and Hunter syndrome) [1].
To our knowledge, trigger finger secondary to an extraskeletal chondroma (EC) has never been reported in children.
The aim of this work was to describe our experience of a trigger finger in an 11-year-old girl, which was found to be secondary to EC.
2. Case Report
An 11-year-old girl presented with a typical history of triggering of the fourth finger of her left hand which started six months before. The girl could move completely her finger, but in the position of flexion, locking of the digit occurred and passive unlocking caused discomfort.
At physical examination, a nodule of about 5 mm was palpable at the site of triggering, just distally to the distal palmar crease in line with the fourth finger.
Ultrasound examination (Figure 1) showed an avascular mass of about 6 × 2 mm, attached to the flexor tendons, anechogenic with an echogenic core.
Figure 1.
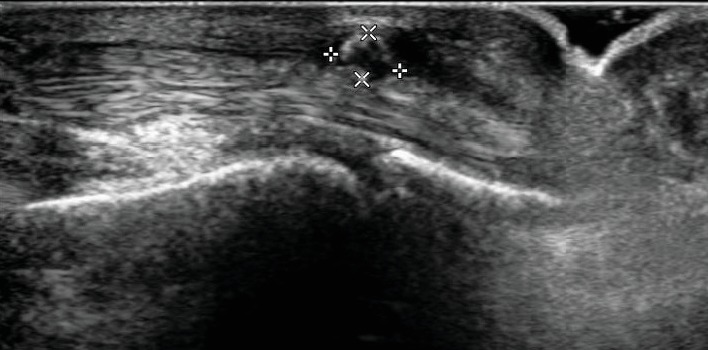
Ultrasound examination of the fourth finger of her left hand shows an avascular mass of about 6 × 2 mm, attached to the flexor tendons, anechogenic with an echogenic core.
Surgery for excisional biopsy and release of the triggering was performed under general anesthesia. A 1.5 cm transverse skin incision was performed at the distal palmar crease, just proximally to the A1 pulley area. Longitudinal incision of the A1 pulley revealed the nodule with a diameter of about 6 mm, attached to the tendon of the FDS. The nodule moved out of the A1 pulley as the digit was flexed and entered the pulley with difficulty as the digit was extended, causing catching and sudden release of the tendon. No relationship with the FDP or with the underlying metacarpal bone was found. The mass was excised from the tendon using a scalpel and referred for histopathological examination. The histological analysis (Figures 2 and 3) was diagnostic of chondroma.
Figure 2.
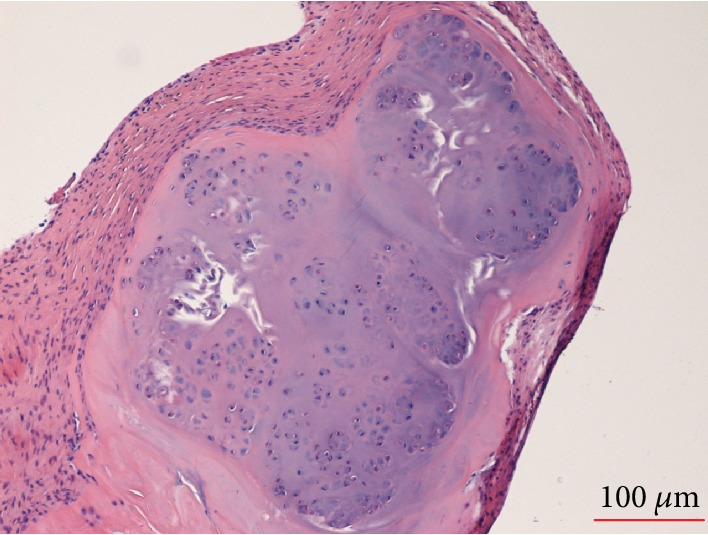
Histopathology. The resected specimen was an unorientable fragment of about 5 mm of diameter. It was routinely formalin fixed and paraffin embedded for the histological study. Microscopic examination revealed that the lesion consisted of three components: fibroblastic spindle cells, cartilage without significant cellular atypia, and small marginal irregular bony trabeculae. These features were diagnostic of chondroma.
Figure 3.
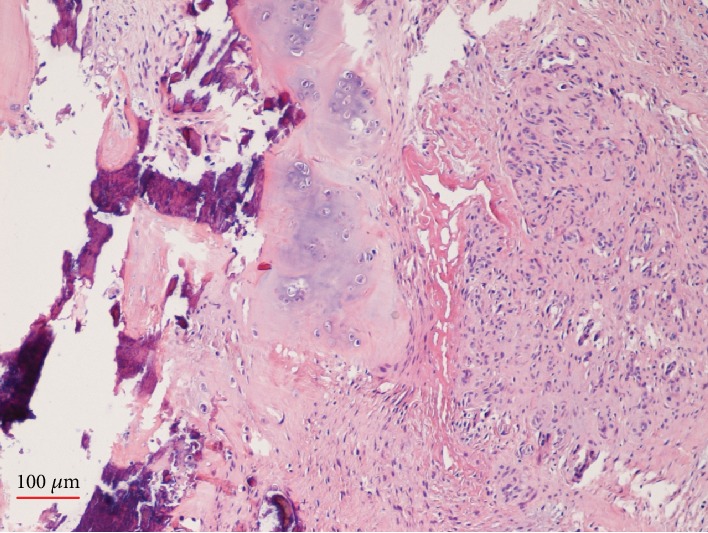
Histopathology.
The postoperative course was uneventful with rapid recovery of the complete range of motion. At the last follow-up, 27 months after surgery, magnetic resonance did not show recurrence and the patient did not report any episode of triggering after the operation.
3. Discussion
EC (or soft tissue chondroma) is a rare benign (1.5% of all benign soft tissue tumors) cartilaginous tumor with uncertain aetiology [2] arising from soft tissues such as tendons, tendon sheath synovia, and joint capsules with no continuity to the bone or periosteum and with tendency to occur in the hands and feet. It affects both sexes equally and mainly occurs in patients aged 30 to 60 years [3].
First described by Baumuller in 1883 [2], EC is a distinct histopathological diagnosis in contrast to other cartilage-containing lesions and characterized by cellular atypism. Areas of ossification and calcification may be found within the hyaline cartilage that composes most of the lesion [2].
Our literature analysis of EC affecting the hand and upper extremity (Table 1) revealed 25 cases reported [2, 4–16], located in digits (eight cases), within the carpal tunnel (three), or in other sites in the hand (ten); in four cases, information about the exact location was missing. The average size ranged from 0.5 to 12 cm in an estimated diameter. There was clear male predominance. The average patient age was 46 years, but age was not reported in all instances. Just one pediatric case was reported, a 12-year-old male patient presenting with a history of enlarging mass over the hypothenar eminence of the hand [5].
Table 1.
Review of the published cases of EC affecting the hand and upper extremity.
| Author | Year of publication | Number of cases | Exact site of origin | Therapy | Patient age (y) | Gender | Size of chondroma (cm) |
|---|---|---|---|---|---|---|---|
| Wenny et al. [16] | 2018 | 1 | Left hand | Surgical excision | 54 | M | 4 × 7 |
| Saito et al. [4] | 2017 | 1 | Index finger | Surgical excision | 63 | M | 4 × 3.8 |
| Schwaiger et al. [2] | 2017 | 1 | Ring finger | Surgical excision | 76 | M | 3 × 1 × 1 |
| Khandeparkar et al. [6] | 2014 | 1 | Radial aspect of the wrist | Surgical excision | 52 | M | 5 × 4 × 3 |
| Ikeda and Osamura [7] | 2013 | 1 | Carpal tunnel | Surgical excision | 82 | F | 12 × 4.5 × 4.2 |
| Suganuma et al. [3] | 2011 | 1 | Index finger | Surgical excision | 62 | M | 5 × 4.5 × 5 |
| Ishii et al. [8] | 2010 | 1 | Index finger, subungual | Surgical excision | 39 | M | — |
| Le Corroller et al. [9] | 2008 | 1 | Palmar side of the distal forearm | Surgical excision | 40 | M | Diameter 4.5 |
| Singh et al. [5] | 2005 | 1 | Hypothenar eminence | Surgical excision | 12 | M | 4 × 4 |
| Cumming et al. [10] | 2005 | 1 | Carpal tunnel | Surgical excision | 47 | M | — |
| De Smet 11 | 2005 | 1 | Elbow/proximal forearm | Surgical excision | 50 | M | Diameter 3-4 |
| Cho and Kim 12 | 2003 | 1 | Ring finger, subungual | Surgical excision | 21 | M | Diameter 0.5 |
| Boudart et al. [13] | 2003 | 1 | Carpal tunnel | Surgical excision | 18 | F | — |
| Thool et al. [14] | 2001 | 1 | Forearm | Surgical excision | 54 | M | 6 × 5 |
| De Poulpiquet et al. [15] | 1999 | 1 | Little finger | Surgical excision | 26 | M | — |
| Nakamura et al. [2] | 1997 | — | — | — | — | — | — |
| Yamada et al. [2] | 1995 | 1 | Ring finger | Surgical excision | 51 | M | 4 × 2.2 × 1.5 |
| Isayama et al. [2] | 1991 | 1 | Thumb | Surgical excision | 44 | M | — |
| DelSignore et al. [2] | 1990 | 1 | Palmar side of the hand | Surgical excision | — | — | — |
| Van Demark et al. [2] | 1990 | — | — | — | — | — | — |
| Marcial-Seoane et al. [2] | 1990 | 1 | Upper arm | Surgical excision | — | — | — |
| Catalano et al. [2] | 1988 | — | — | — | — | — | — |
| Sowa et al. [2] | 1987 | 2 | Palmar and dorsal sides of the hand | Surgical excision | — | — | — |
| Perri and Tripi [2] | 1986 | 1 | Wrist | Surgical excision | — | — | — |
Clinical appearance was typically characterized by swelling due to a palpable subcutaneous mass; the three cases within the carpal tunnel were associated with symptoms of carpal tunnel syndrome. Trigger finger secondary to EC, similar to what we have reported in an 11-year-old girl, was described only in a 76-year-old man [2]. All cases underwent surgical excision with a recurrence rate reported to be 15% to 25% [2].
4. Conclusion
Extraskeletal chondroma is a rare benign tumor in the hand. Depending on where the EC is located, it can cause symptoms and mimic other conditions as described in our case [2]. This condition should be considered in the differential diagnosis of pediatric trigger finger.
Additional Points
This study was conducted at the Anna Meyer Children's University Hospital, Florence, Italy.
Consent
Informed consent was obtained from the parents of the patient included in the study, including the use of clinical photographs.
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors' Contributions
All authors analyzed and interpreted the patient date and are contributors to writing the manuscript. All authors read and approved the final manuscript.
References
- 1.Shah A. S., Bae D. S. Management of pediatric trigger thumb and trigger finger. Journal of the American Academy of Orthopaedic Surgeons. 2012;20(4):206–213. doi: 10.5435/JAAOS-20-04-206. [DOI] [PubMed] [Google Scholar]
- 2.Schwaiger K., Ensat K., Neureiter D., Wechselberg G., Hladik M. Trigger finger caused by extraskeletal chondroma. The Journal of Hand Surgery. 2017;42(1):e51–e55. doi: 10.1016/j.jhsa.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Suganuma S., Tada K., Tsuchiya H. Giant extraskeletal chondroma of the index finger: a case report. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2011;64(10):1377–1379. doi: 10.1016/j.bjps.2011.02.024. [DOI] [PubMed] [Google Scholar]
- 4.Saito M., Nishimoto K., Nakayama R., et al. Extraskeletal chondroma of the index finger: a case report. Case Reports in Oncology. 2017;10(2):479–484. doi: 10.1159/000477237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh P., Mathur S. K., Kundu Z. S., Singh S., Marwah N., Arora B. Extraskeletal chondroma of the hand—a case report. Indian Journal of Pathology & Microbiology. 2005;48(2):206–208. [PubMed] [Google Scholar]
- 6.Khandeparkar S. G., Joshi A., Khande T., Kesari M. A rare case of giant soft tissue chondroma of the wrist: a cytopathological study with review of the literature. Journal of Cytology. 2014;31(1):40–43. doi: 10.4103/0970-9371.130695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ikeda K., Osamura N. Trigger finger at the A2 pulley in children - two case reports. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2010;63(8):e635–e636. doi: 10.1016/j.bjps.2010.02.014. [DOI] [PubMed] [Google Scholar]
- 8.Ishii T., Ikeda M., Oka Y. Subungual extraskeletal chondroma with finger nail deformity: case report. The Journal of Hand Surgery. 2010;35(2):296–299. doi: 10.1016/j.jhsa.2009.10.026. [DOI] [PubMed] [Google Scholar]
- 9.Le Corroller T., Bouvier-Labit C., Champsaur P. Diffuse mineralization of forearm extraskeletal chondroma. Joint Bone Spine. 2008;75(4):479–481. doi: 10.1016/j.jbspin.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 10.Cumming D., Massraf A., Jones J. W. Extraskeletal chondroma as a cause of carpal tunnel syndrome: a case report. Hand Surgery. 2005;10(02n03):327–330. doi: 10.1142/S0218810405002954. [DOI] [PubMed] [Google Scholar]
- 11.De Smet L. Posterior interosseous neuropathy due to compression by a soft tissue chondroma of the elbow. Acta Neurologica Belgica. 2005;105(2):86–88. [PubMed] [Google Scholar]
- 12.Cho S. B., Kim S. C. Subungual extraskeletal chondroma mimicking glomus tumor. The Journal of Dermatology. 2003;30(6):492–494. doi: 10.1111/j.1346-8138.2003.tb00422.x. [DOI] [PubMed] [Google Scholar]
- 13.Boudart D., Vancabeke M., Penders W., Putz P. Carpal tunnel syndrome due to an extraskeletal chondroma case report. Chirurgie de la Main. 2003;22(1):51–53. doi: 10.1016/s1297-3203(02)00007-0. [DOI] [PubMed] [Google Scholar]
- 14.Thool A. A., Raut W. K., Lele V. R., Bobhate S. K. Fine needle aspiration cytology of soft tissue chondroma. A case report. Acta Cytologica. 2001;45(1):86–88. doi: 10.1159/000327193. [DOI] [PubMed] [Google Scholar]
- 15.De Poulpiquet P., Segonds J. M., Balaire P., Gros P., Grippari J. L. Chondroma of the soft tissues of the hand. Report of a recurrent case. Revue d'orthopédie et de chirurgie de l'appareil moteur. 1999;85(8):861–864. [PubMed] [Google Scholar]
- 16.Wenny R., Pollhammer M. S., Duscher D., et al. Giant extraskeletal chondroma of the hand: a rare case. Archives of Plastic Surgery. 2018;45(4):388–389. doi: 10.5999/aps.2017.01053. [DOI] [PMC free article] [PubMed] [Google Scholar]


