Abstract
Purpose
The aim of this study is to evaluate the functional results of open reduction using the Newcastle approach and internal fixation for complex intra-articular distal humeral fractures in children through the report of cases.
Material and methods
A retrospective case series of patients who underwent open reduction and internal fixation surgery because of a complex intra-articular distal humeral fracture using the Newcastle approach were reviewed. Minimum follow-up was 2 years. Demographic, clinical, and radiological data were analyzed. Also, Mayo Elbow Performance Score and four-point Likert scale were evaluated.
Results
2 children were included in the final analysis. In both fractures, the approach was sufficient for accurate reduction and the functional outcome on both elbows was satisfactory. The Mayo elbow score was 95 points (excellent results) and the five-point Likert scale, both patients were very satisfied with the outcomes. In the radiographic study, no necrosis or secondary deformities were observed.
Conclusions
Our study provides evidence that the Newcastle approach is an alternative to perform open reduction in those children supra-intercondylar fractures that cannot be reduced using a close reduction. To our knowledge, there is not previous paper that has reported the used of this approach in the treatment in this kind of fractures.
Keywords: Child, Humerus, T-condylar, Distal humerus
Introduction
Supracondylar fractures of the distal humerus are the second most common traumatic injury of the upper limb in the pediatric age. However, T-type distal humerus fractures (intercondylar) are an uncommon occurrence, representing <2% of all observed pediatric elbow fractures [1,2]. Moreover, of this fracture type in children <60 cases has been previously reported in the English literature, with only 13 of which involved children under 8 years of age [3].
In children, the distal humerus, largely composed of cartilage, is very elastic and displacement occurs mainly in the supracondylar bone area, being most elbow injuries in this age group, caused by hyperextension. For that reason, T-type distal humerus fractures in children are rare and there is usually the effect of direct forces applied to an elbow above 90° flexion [[1], [2], [3]]. The most commonly used classification system for children T-type distal humerus fractures is the adult OA/OTA classification. This classification has been questioned in this type of fracture because this classification does not take into account the ossification nuclei [2]. Toniolo and Wilkins suggested a simple classification based on the displacement degree and fragment comminution [1]. In 2006, a pediatric OA/OTA classification was developed. In this classification, this fracture can be a 13-E/4.2 [4].
Due to the low incidence of these fractures, treatment recommendations are based on publications of case reports or small case series or else adhere to the treatment principles of similar fractures of adult patients [[1], [2], [3]]. The aim of this study is to evaluate the functional results of open reduction using the Newcastle approach and internal fixation for complex intra-articular distal humeral fractures in children through the report of 2 cases. In terms of the Newcastle approach, to our knowledge there is not previous paper that have report the used of this approach in the treatment of this kind of fractures.
Materials and methods
A retrospective revision of our children patients who had undergone open reduction and internal fixation surgery because of a complex intra-articular distal humeral fracture using the Newcastle approach between 2011 and 2016 were performed. Among 76 children with supracondylar humeral fracture, only 2 patients met our inclusion and were available for analysis.
Surgical procedure: Newcastle approach [5]
A single team of trauma surgery specialists (JS, PC) performed all surgeries. Under general anesthesia and, with the patient in a lateral decubitus position the surgery was performed. The incision starts 6–7 cm (10–12 cm in adults) proximal to the tip of olecranon, following the lateral border of the olecranon itself, ending at the subcutaneous border of the ulna, 4–6 cm (8–10 cm in adults) distal to the tip of the olecranon. The size of the incision might be reduced and we should adapt it to the length of the extremity at the pediatric age. Both cutaneous skin flaps are raised and held in position using two proximal and two distal stay sutures. The ulnar nerve needs to be identified proximally and decompressed distally at the level of the two heads of the flexor carpi ulnaris without transposition. The fascia is opened following a skin incision until the border of the ulna. Afterwards the proximal aponeurosis is released from the raphe and retracted using a suture. The anconeus muscle is raised subperiosteally from the ulna and it is directed proximally until the intermuscular septum of the triceps.
The raphe is opened longitudinally at the proximal level and with a cut of 2 cm proximal to the olecranon it is retracted distally. The muscular bellies of the triceps are retracted to the medial and lateral columns of the humerus leaving the distal end of the humerus fully exposed (Fig. 3b). At this point, special attention has to be paid in order to avoid a subperiosteal dissection of the lateral belly since the vascular supply of the distal epiphysis of the humerus is posterior and lateral and its injury could result to an avascular necrosis.
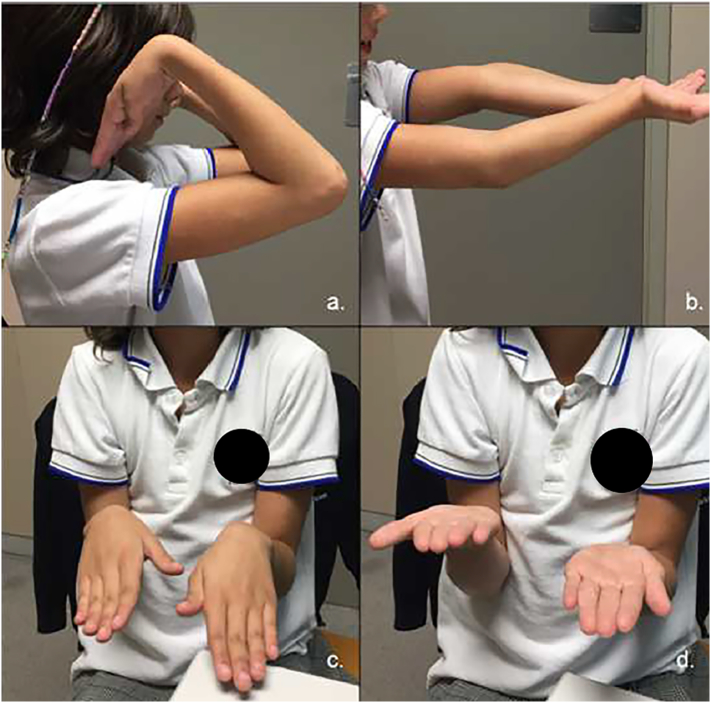
Fig. 3.
Range of motion of the patients at final follow -up. a. Flexion. b. Extension. c. Pronation. d. Supination.
Case 1
A 7-year old girl came to the emergency department referring pain and functional impairment in the right elbow after a casual fall from her stand height. She had a painful right elbow held in 80° of flexion, inability to move actively without any Neurovascular deficit. The radiological study (antero-posterior and lateral elbow view) revealed a displaced supra-intercondylar humeral fracture (Fig. 1a). In the operating room, with fluoroscopy images and under general anesthesia, this fracture pattern was confirmed. Open reduction of the fracture was performed, following the Newcastle posterior approach, and subsequently internal fixation with four 1.8 mm Kirschner wires (K-wires) (Fig. 1b). The elbow was immobilized at 90° with a brachiopalmar splint.
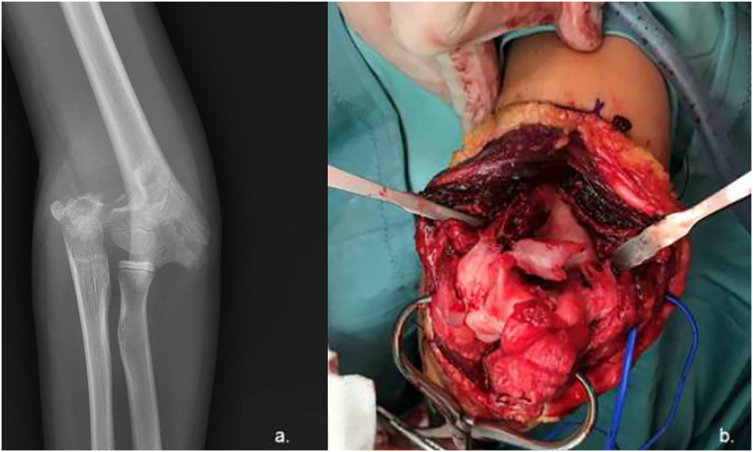
Fig. 1.
a. X-ray view in the emergency department. b. postoperative antero-posterior and lateral x-rays of the first patient.
Case 2
An 8-year-old girl, came to the emergency department reporting severe pain and functional impairment of her left elbow after a horse fall. On examination, the patient presented significant swelling and bruising in the left elbow, without a neurovascular deficit of the limb. In the radiological study (antero-posterior X-ray) a supracondylar fracture was diagnosed (Fig. 2a). In the operating room, under general anesthesia, the closed reduction of the fracture was not successful, and the surgeon opted for an open treatment. A Newcastle approach was performed, which gave evidence that apart from the supracondylar fracture, there was also a non-displaced intercondylar line (Fig. 2b). The supracondylar fracture was reduced and stabilized using internal fixation with three 1.8 mm K-wires. Since the intercondylar fracture line was stable and did not move with the surgical manipulation, no stabilization K-wires were added at that plane.
Fig. 2.
a. Antero-posterior X-ray showing a supracondylar elbow fracture. b. Intraoperative image of the supra-intercondylar elbow fracture seen through the Newcastle approach. Note the reduction clamp stabilizing the supracondylar segment and the olecranon integrity.
Results
In both patients, the same immobilization and the same rehabilitation protocol were done. Three weeks after surgery, the K-wires were removed under sedation and active flexion-extension of the elbow was initiated without restrictions. At 2 months, the patients did not have any limitation. In the X-rays controls the fractures consolidation were documented. Two years after surgery, the range of motion in case one was −5° extension and 140° flexion, and in case two was complete (Fig. 3). The patient two could practice horse riding again. In both cases, at final follow up, the Mayo elbow score was 95 points (excellent results) and the five-point Likert scale, both patients were very satisfied with the outcomes. In the radiographic study, no necrosis or secondary deformities were observed.
Discussion
T-type distal humerus fractures represent an unusual fracture pattern in the pediatric patient [[1], [2], [3]]. Because of the rarity of this fracture only few reports about treatment options and outcome measurements are published. To our knowledge, there is not previous paper that has reported the used of the Newcastle approach in the treatment of this kind of fractures. In our 2 patients, who a had a T-type distal humerus fractures treated with and open reduction and internal fixation using the Newcastle approach, after 2 years of follow-up, they had a complete range of motion, excepted for a lack of −5° extension. They had excellent scores measurement, and in their radiographic studies, fracture consolidation was achieved, and no necrosis or secondary deformities were observed.
Currently, based on literature evidence, we believe that there are two main difficulties when treating a supraintercondylar humeral pediatric fracture: a) their prompt diagnosis, b) the use of an effective classification system because the most used classification (Gartland) do not include this type of fracture. Only Toniolo and Wilkins, and Vivas y Moreno considered this fracture pattern, and c) the choice of the most appropriate surgical approach in order to attain an accurate reduction and subsequently stable osteosynthesis [1,2,6]. As in our case 2, these fractures are often difficult to diagnose, therefore, sometimes the diagnosis is made in the operating room. In a skeletally immature patient the intra-articular line of a supra-intercondylar fractures may not be visualized, either because the large cartilaginous component remaining in the young elbow, the difficult to obtain good radiographies projections or because it might not be displaced [1,2]. High quality preoperative radiographs are necessary to make a correct initial diagnosis since the malreduction or neglect of the intra-articular line can have consequences in the future articular development [6]. Based on the current literature, in addition to standard anterior- posterior and lateral projections, an oblique projection might help to identify the intercondylar fracture line. Some authors have stressed the importance of computed tomography (CT) in the proper diagnosis of this fracture pattern [2,3]. From our point of view, the use of CT for the study of this type of fractures in the pediatric age is rarely justified. Because of the radiation exposure associated with any CT, we believe that its use should be limited. CT, arthrography and magnetic resonance imaging (MRI) might help to understand the triplanar configuration of the complex physeal injuries around the elbow, however, as our other authors have commented it is important to be cautious of their use. Moreover, when may be difficult to obtain in this age group this MRI without the use of sedation [2].
Non-displaced pediatric T-type distal humerus fracture can be treated conservatively, but when displacement or rotation of fracture fragments are evident, they should be treated surgically [1,6]. In most series, in this type of fracture open reduction is recommended with the aim to restore the joint surface and stabilize the fracture, but this option might present complications, which include non-union, malunion, avascular necrosis and epiphyseal growth arrest [1,2]. Some authors suggested the use of percutaneous pinning in the treatment of intra-articular distal humerus fractures in the same way used in the surgical treatment of supracondylar fractures [7]. This minimally invasive approach tries to limit the dissection of the posterior side of the distal humerus, thus reducing the risk of damage to the condylar vascular supply and avoiding avascular necrosis, a well-documented complication of internal fixation in open reduction of condylar fractures [1,2,7]. From our point of view, it is only possible when there is no or minimal displacement of the intercondylar line.
Different surgical approaches have been described to treat this type of fractures, such as Campbell, Bryan-Morrey and Müller, which, according to the literature are the most used [1,2,6]. We suggest treating these fractures with the Newcastle approach. Although no approach has been clearly documented as superior to the surgical management of T-condylar fractures in the adolescent and pediatric population, it is important to choose one that allows to perform reduction and fixation of the fracture, avoiding damage to the still present physes [2,3]. In 1986, Papavasiliou and Beslikas published a case series of intercondylar fractures, 2 of which were approached laterally. Patients treated with a lateral approach developed a 20° flexion contracture and a 15° ulnar valgus deformity compared with the contralateral side. The authors advocated against the lateral approach in the treatment of pediatric T fractures of the distal humerus due to the difficulties in reduction of the fracture, the inability to visualize and protect the cubital nerve and the poor final range of motion [8]. An olecranon osteotomy approach allows the most extensive visualization of the articular surface. This approach is common in adults, but not in skeletally immature patients [9]. Dreyfuss and Eidelman published a series of 6 pediatric patients who underwent an olecranon osteotomy to treat a supra-intercondylar elbow fracture. There were no cases of osteotomy non-union, but all patients required a second surgery to remove osteosynthesis because it was symptomatic. More than half of the patients lost the full extension, but they had a higher satisfaction rate, according to the authors [10]. An alternative approach is the triceps splitting. In 1990, Kasser reported that the triceps splitting approach does not produce scars in the extensor mechanism, and therefore does not disturb the range of motion or diminish the strength of extension [11]. In his series, Kasser suggests that the division of the triceps is preferable to olecranon osteotomy in the treatment of intercondylar fractures in order to avoid olecranon physes. Although this is true in a growing child, in an almost skeletally mature adolescent the possible complications related to the osteotomy are those of the approach itself rather than the possible physeal injury [10,11]. Another option to avoid olecranon osteotomy is the Bryan-Morrey triceps reflection approach, which allows superior joint visualization compared to the triceps splitting approach [12]. Wolfe and Ranawat recommend that triceps release at the level of olecranon should be done with osteotomy, using a thin wafer of bone, and that the entire extensor mechanism should be reflected laterally [13]. In our cases we used the Newcastle approach, described in 2011, which is presented as an alternative in the treatment of supraintercondylar fractures in skeletally immature patients. It is an anatomical approach; it does not require an olecranon osteotomy and offers adequate visualization of the joint surface, manipulation to anatomical reduction and fracture fixation using K-wires [5]. This approach has allowed us to perform, not only arthroplasty in elbow osteoarthritis, but also osteosynthesis in supra-intercondylar fractures in adults and children [14]. We cannot conclude that this is a better approach, but it is an option, with good results, as our patients had. Also, we have to mention that in our two cases, the surgery treatment was performed by an experience surgeon in upper extremity trauma. The surgeon experience is something that has to be in count in the final outcome of our patients. Even supracondylar humeral fractures in children are common, their treatment can be challenging, especially since their management is not always performed by the most experienced surgeon [3]. The complexity of these fractures increases when there is an intercondylar extension and consequently an open approach is usually necessary for their accurate reduction [1].
To obtain good outcomes in this type of fracture, it is important to choose an approach that allows performing direct reduction and fracture fixation. Furthermore, avoiding any damage to the physes and their blood supply, which are still present is of paramount importance. For this reason, the Newcastle approach is presented as an alternative to perform open reduction in those supracondylar fractures that cannot be reduced using a close reduction, as well as for a supra-intercondylar fracture. It is an anatomical approach, does not require an olecranon osteotomy and offers enough joint surface visualization to control the joint fragments and their reduction and subsequent stabilization.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Patient's informed consent to publish this report is included in the Ethical Standards statement.
Declaration of competing interest
Jordi Salvador, Jorge H. Nuñez, Margarita Veloso, Pablo Castillón, Francesc Angles declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article. The author has no competing interest to declare.
References
- 1.Anari J.B., Neuwirth A.L., Carducci N.M., Donegan D.J., Baldwin K.D. Pediatric T-condylar humerus fractures: a systematic review. J. Pediatr. Orthop. 2015;37:36–40. doi: 10.1097/BPO.0000000000000588. [DOI] [PubMed] [Google Scholar]
- 2.Popkin C.A., Rosenwasser K.A., Ellis H.B., Jr. Pediatric and adolescent T-type distal humerus fractures. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2017;1 doi: 10.5435/JAAOSGlobal-D-17-00040. (e040) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tomori Y., Sudo Y., Iizawa N., Nanno M., Takai S. Intercondylar fracture of the distal humerus in a 7-year-old child. Medicine (Baltimore) 2017;96 doi: 10.1097/MD.0000000000006085. (e6085) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Slongo T., Audige L., Schlickewei W., Clavert J.M., Hunter J. International Association for Pediatric Traumatology, Development and validation of the AO pediatric comprehensive classification of long bone fractures by the Pediatric Expert Group of the AO Foundation in collaboration with AO Clinical Investigation and Documentation and the International Association for P. J. Pediatr. Orthop. 2006;26:43–49. doi: 10.1097/01.bpo.0000187989.64021.ml. [DOI] [PubMed] [Google Scholar]
- 5.Amirfeyz R., Clark D., Quick T., Blewitt N. Newcastle approach to the elbow, a cadaveric study. Arch. Orthop. Trauma Surg. 2011;131:747–751. doi: 10.1007/s00402-010-1206-0. [DOI] [PubMed] [Google Scholar]
- 6.Marengo L., Andreacchio A., Alberghina F., Dimeglio A., Canavese F. Functional outcome of displaced intercondylar fractures of the humerus in children and adolescents. J. Pediatr. Orthop. B. 2017;27:121–127. doi: 10.1097/BPB.0000000000000476. [DOI] [PubMed] [Google Scholar]
- 7.Kanellopoulos A.D., Yiannakopoulos C.K. Closed reduction and percutaneous stabilization of pediatric T-condylar fractures of the humerus. J. Pediatr. Orthop. 2004;24:13–16. doi: 10.1097/00004694-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Papavasiliou V.A., Beslikas T.A. T-condylar fractures of the distal humeral condyles during childhood: an analysis of six cases. J. Pediatr. Orthop. 1986;6:302–305. doi: 10.1097/01241398-198605000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Wilkinson J.M., Stanley D. Posterior surgical approaches to the elbow: a comparative anatomic study. J. Shoulder Elb. Surg. 2001;10:380–382. doi: 10.1067/mse.2001.116517. [DOI] [PubMed] [Google Scholar]
- 10.Dreyfuss D., Eidelman M. Treatment of complex intercondylar humeral fractures in adolescents by open reduction and internal fixation through the transolecranon approach. J. Pediatr. Orthop. B. 2014;23:364–368. doi: 10.1097/BPB.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 11.Kasser J.R., Richards K., Millis M. The triceps-dividing approach to open reduction of complex distal humeral fractures in adolescents: a Cybex evaluation of triceps function and motion. J. Pediatr. Orthop. 1990;10:93–96. [PubMed] [Google Scholar]
- 12.Remia L.F., Richards K., Waters P.M. The Bryan-Morrey triceps-sparing approach to open reduction of T-condylar humeral fractures in adolescents Cybex evaluation of triceps function and elbow motion. J. Pediatr. Orthop. 2004;24:615–619. [PubMed] [Google Scholar]
- 13.Wolfe S.W., Ranawat C.S. The osteo-anconeus flap. An approach for total elbow arthroplasty. J. Bone Joint Surg. Am. 1990;72:684–688. [PubMed] [Google Scholar]
- 14.Chen H., Li D., Zhang J., Xiong X. Comparison of treatments in patients with distal humerus intercondylar fracture: a systematic review and meta-analysis. Ann. Med. 2017;49:613–625. doi: 10.1080/07853890.2017.1335429. [DOI] [PubMed] [Google Scholar]