Abstract
Bone healing is a complex and well-orchestrated physiological process, in which bone repairs and regenerates regaining its original biomechanical and biochemical properties. It is estimated that 5 to 10% of all fractures are complicated by delayed union or non-union. Progression to non-union is thought to be multifactorial, even though the exact biological sequence remains obscure.
Treatment should aim to addressing deficiencies in both the mechanical and biological components, along with eliminating co-factors that could negatively affect the locally induced fracture healing response.
We report a case of a 78-year-old patient who presented with a distal femoral non-union above a previously fused knee, which was successfully managed with exchange nailing and intramedullary delivery of recombinant human bone morphogenetic protein-7 (rhBMP-7).
Keywords: Femur, Non-union(s), Fused, BMP, Nail
Case report
A 78-year-old retired engineer presented to the Emergency Department, having fallen 8 ft. from a ladder. His past medical history included a left knee fusion in 1991 for osteoarthritis, hypertension, atrial fibrillation and mitral valve surgery (2007) for which he was on Warfarin, peripheral vascular disease and epilepsy. He was a non-smoker and did not drink any alcohol.
Following his arrival at the Emergency Department he was managed according to the ATLS® guidelines. His airway was patent and had good, bilateral air entry. On the left side of his chest he exhibited pain on pressure, whilst his oxygen saturation levels were 96% on air. His abdomen was soft and non-tender and exhibited no guarding or localized tenderness. Both upper extremities and the right lower extremity were not tender and remained neurovascularly intact. He complained of pain to his left thigh restricting any movement to the hip and knee joints, but with no distal neurovascular deficit. A trauma-CT performed in line with our institution's guidelines, confirmed the presence of four rib fractures and the absence of an osseous injury to the spine.
Plain radiographs of the left lower extremity revealed a distal femoral fracture, (AO classification: 33-A2) just above the fusion level (Fig. 1).
Fig. 1.
Plain radiographs of the left lower extremity showing a supracondylar distal femoral fracture (AO classification: 33-A2).
a) AP
b) Lateral.
Due to the poor skin quality surrounding the knee, a decision was taken to use an antegrade long intramedullary (IM) device for stabilization of the fracture. Intra-operatively, the patient was positioned supine on a traction table and a reamed nail (T2 Recon Nailing System — recon mode) was inserted using standard technique (Fig. 2).
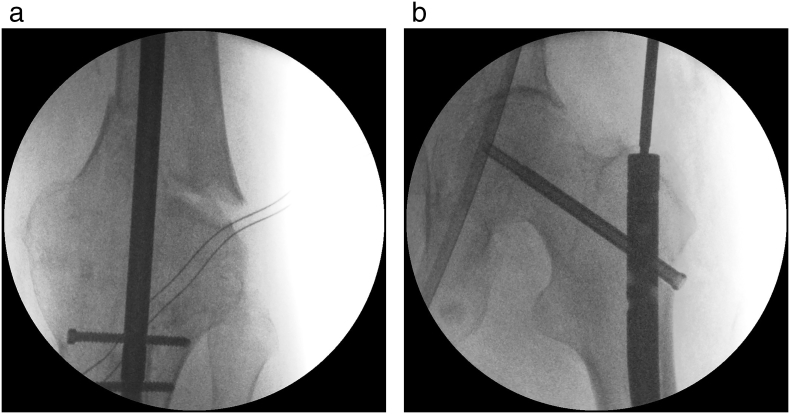
Fig. 2.
Intra-operative fluoroscopy projections (primary procedure).
a) AP view at the fracture site showing distal locking
b) AP view at the proximal femoral site (cephalomedullary screw option).
Throughout the post-operative period, the patient demonstrated no signs of superficial or deep infection. He was discharged home and was advised to mobilize partial weight bearing for the first six weeks. He was then followed-up at regular intervals at the outpatient Orthopaedic clinic. During his ten-month follow-up and because of absent clinical and radiological signs of union, a CT scan was requested, confirming the presence of an atrophic non-union (Fig. 3, Fig. 4). At the same time he was screened for possible low grade infection, but his blood parameters were within normal range. Subsequently, he was scheduled for a revision procedure including exchange nailing (antegrade nailing with further reaming of the medullary canal) and injection of recombinant human Bone Morphogenic Protein-7 (rhBMP-7) to enhance fracture healing.
Fig. 3.
Plain radiographs of non-union to left distal femur, ten months post primary procedure.
a) AP view at the fracture site
b) Lateral view at the fracture site.
Fig. 4.
CT scan of non-union to left distal femur, eleven months post primary procedure.
Confirmed the presence of an atrophic non-union with a gap of 6.5 mm at the fracture site.
a) Transverse projection
b) Sagittal projection.
He underwent the above-mentioned procedure 15 months post-injury. Due to the sclerosis of the non-union site, the operating surgeon was unable to deliver the rhBMP-7 to the fracture site without further damaging the surrounding soft tissues and local vascularity. It was therefore decided to deliver the rhBMP-7 through the plastic tube used for the exchange nailing, that was inserted through the trochanteric entry point. The marking sign on the plastic tube was placed at the non-union site under fluoroscopy guidance and accurate delivery of the rhBMP-7 was accomplished (rhBMP-7 was delivered to the non-union site by advancing the active substance within the plastic tube with the guide wire) (Fig. 5). Thereafter, the new nail (PFNA long, Depuy-Synthes) was inserted and was locked both proximally and distally. Conventional cultures from the reaming debris taken intra-operatively were negative to any microorganism growth. His post-operative course was unremarkable and was discharged home with the advice to mobilize partial weight bearing.
Fig. 5.
Intra-operative pictures and fluoroscopy views (revision procedure).
a) Picture of the plastic tube used to load and to deliver the rhBMP-7 (one vial was used)
b) Advancement and delivery of BMP-7 using the guide wiring within the plastic tube
c) Fluoroscopy projection for guidance of the rhBMP-7 at the fracture site (red arrow points the marking sign on the plastic tube).
(For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
His recovery was uneventful and was advised to mobilize full weight bearing six weeks post-operatively. The fracture progressed to clinical and radiological union six months following revision operation (Figs. 6).
Fig. 6.
Plain radiographs of non-union to left distal femur, four months post revision surgery.
a) Knee — AP
b) Knee — lateral
c) Left hip — AP.
Discussion
Management of femoral non-unions can be challenging and with often-unpredictable outcomes. Treatment modalities have been evolved over the years focusing on the optimization of both the mechanical and biological environment, tailored to each patient's individual requirements. Particularly in atrophic non-unions, the enhancement of healing with autologous iliac crest graft has been considered the gold standard due to its osteogenic, osteoinductive and osteoconductive properties [1,2].
BMP's represent powerful osteoinductive molecules that have been successfully used for the treatment of long bone non-unions, fusions and bone defects [3]. They exert their action on osteoprogenitor cells inducing mitogenesis and differentiation of the progenitor cells to osteoblasts [4].
In the presented case, the host had a number of co-morbidities, including a previously fused knee joint just distally to the fracture. The patient also exhibited several risk factors known to contribute to non-union including peripheral vascular disease, his anticoagulant drug therapy and the former soft tissue and blood supply impairment, inevitable complications of the fusion procedure [5].
At the ten-month follow-up, an established atrophic non-union was evident. Due to the state of the soft tissues around the fracture level, an open direct bone grafting approach was thought to be unsafe as it would further compromise the biological environment of the non-union. Moreover, due to his age, any attempt to harvest iliac crest bone graft from the pelvis would not have been successful due to the replacement of the cancellous graft material with fat tissue. Moreover, such a procedure has also been shown to be associated with donor site morbidity [5].
The canal was opened distally, bypassing the fused knee in order to allow adequate distal fixation by locking the intramedullary nail in the proximal tibia. Even though reaming was performed, it was felt that an additional osteogenic stimulus would further benefit the patient. Firstly, reaming generates debris which is known to contain viable osteoprogenitor cells [6]. Additionally, by delivering the rhBMP-7 at the non-union site where this debris accumulates, the contained cells would have been exposed to the inductive property of the growth factor.
Delivery of the rhBMP-7 at the non-union site through the plastic tube was found easy and with no procedure-related complications. Using the marking tip of the plastic tube under fluoroscopy guidance, it was possible to plan accurate delivery at the non-union site.
This is the first, to our knowledge, report of an intramedullary application of BMPs. We believe that this method of treatment and in particular delivering BMP's through the medullary canal to the non-union site, could be useful and could be considered in other cases where similar limitations and issues are present.
Declaration of competing interest
All authors declare no conflict of interest.
No funding was received for the completion of this project.
References
- 1.Kanakaris N.K., Paliobeis C., Nlanidakis N., Giannoudis P.V. Biological enhancement of tibial diaphyseal aseptic non-unions: the efficacy of autologous bone grafting, BMPs and reaming by-products. Injury. 2007;38(Suppl. 2):S65–S75. doi: 10.1016/s0020-1383(07)80011-8. [DOI] [PubMed] [Google Scholar]
- 2.Giannoudis P.V., Panteli M., Calori G.M. Bone healing: the diamond concept. In: Bentley G., editor. European Instructional Lectures. Springer Berlin Heidelberg; 2014. pp. 3–16. [Google Scholar]
- 3.Kanakaris N.K., Lasanianos N., Calori G.M., Verdonk R., Blokhuis T.J., Cherubino P. Application of bone morphogenetic proteins to femoral non-unions: a 4-year multicentre experience. Injury. 2009;40(Suppl. 3):S54–S61. doi: 10.1016/S0020-1383(09)70013-0. [DOI] [PubMed] [Google Scholar]
- 4.Ronga M., Fagetti A., Canton G., Paiusco E., Surace M.F., Cherubino P. Clinical applications of growth factors in bone injuries: experience with BMPs. Injury. 2013;44(Suppl. 1):S34–S39. doi: 10.1016/S0020-1383(13)70008-1. [DOI] [PubMed] [Google Scholar]
- 5.Pneumaticos S.G., Panteli M., Triantafyllopoulos G.K., Papakostidis C., Giannoudis P.V. Management and outcome of diaphyseal aseptic non-unions of the lower limb: a systematic review. The Surgeon: Journal of the Royal Colleges of Surgeons of Edinburgh and Ireland. 2014;12:166–175. doi: 10.1016/j.surge.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Giannoudis P.V., Pountos I., Morley J., Perry S., Tarkin H.I., Pape H.C. Growth factor release following femoral nailing. Bone. 2008;42:751–757. doi: 10.1016/j.bone.2007.12.219. [DOI] [PubMed] [Google Scholar]