Abstract
Post-operative knee pain management has become a challenge to provide early relief and pain-free postoperative care to the patient. The major objectives of post-operative analgesic treatment are to reduce opioid requirements, post-operative pain, and adverse events related to opioid intake. This narrative review aimed to document post-operative analgesia techniques after total knee arthroplasty (TKA). The traditional approach involved high-dose opioid-based regimen, though opioid is considered strong analgesic, but are associated with a number of unwanted side effects to seek for alternative techniques. The role of sciatic nerve block in TKA pain is doubtful. Femoral Nerve Block (FNB) is still considered as the gold standard; however, FNB is associated with quadriceps weakness and risk of fall and sciatic block with foot drop. To overcome these drawback more distal nerve block techniques has evolved, namely saphenous nerve block in adductor canal, selective tibial which are claimed to provide comparable analgesia to that of femoral and sciatic nerve block. The combination of pre-emptive and multi-modal analgesia and technically well-delivered regional nerve blocks and postoperative physical therapy are an essential component which not only minimize the side effects of traditional opioid-based analgesia but also speed up functional recovery, increases patient satisfaction, and reduces the overall length of hospitalization and cost.
Keywords: Multi-modal analgesia, postoperative analgesia, regional blocks, total knee arthroplasty
Introduction
Joint replacement surgeries are considered as one of the most painful orthopaedic procedures. This painful procedure is the result of inadequate and poorly treated postoperative pain after major joint replacement surgery. This pain episode must be timely addressed because not only does this significantly prolong the rehabilitation process, but also causes the increased risk of other complications. If not addressed within time or without proper approach, these postoperative painful episodes can progress into chronic pain, which eventually prolongs the overall length of hospitalization and cost.[1] The journey to achieve the complete and long-term pain relief begins before the surgery is performed. An important basis to achieve long-term pain relief and functional recovery after the joint surgery involves sufficient peri-operative analgesia.[2] One of the important aspects to achieve successful outcome after joint surgery is the early joint mobilization with the initiation of physical therapy.[3] Several new drugs and novel techniques to ameliorate the post-operative pain post-surgery are being introduced every year, but most of the patients still end up suffering from extreme pain immediately after surgery which often progresses into chronic pain.[4]
Arthroscopic knee surgery has become increasingly popular in modern orthopaedics.[5,6] Still, the post-operative knee pain management involving early relief and pain-free postoperative care to the patient remains a challenge to several clinicians.[7,8] In some cases, pain management in itself has become a priority for management as a daycare procedure. Persistent pain after knee arthoplasty remains an unresolved issue for many patients.[9,10] Pain is considered as a very subjective event because everyone has a different perception and threshold of pain.[11] And therefore, it becomes very difficult to standardize any pain regime for a particular surgery. Several factors that cause knee pain, which include irritation of free nerve endings of the joint capsule, synovial tissue, anterior fat pad.[12,13] Following factors influence the post-arthroplasty pain such as the;
Anesthetic technique,
Patient pain threshold,
Residual effects of perioperative analgesia,
The use and duration of tourniquet exsanguinations,
Pre-operative pain level,
Volume of drug injected,
Surgical trauma involved,
The sex of the patient,
The experience of the surgeons, and finally,
The postoperative activity level of the patients.[14]
Adding to these, the post-operative pain levels are also influenced by the preoperative pain levels of the patient.[15] It is important to remember that adequate analgesia affects the overall hospital stay and early rehabilitation of the patient after surgery.[16,17] The conventional techniques of pain alleviation after total joint replacement included a heavy reliance on the opioid, oral or intravenous (IV), patient-controlled analgesia (PCA) with IV opioid or epidural infusion.[18] Opioid is considered as a strong analgesic, but they are linked with several unwanted side effects like vomiting, nausea, delay ambulation, constipation, sedation, respiratory depression, and pruritus.[19,20] Continuous epidural and PCA limits patient ambulation requires close monitoring and frequent dose adjustment and may not be appropriate for all patients.[21,22] Studies have found out that a single dose regime might be unsuitable for every patient in PCA. All these conditions often lead to under dosing or overdosing with troublesome side effects.[23,24] The increased understanding of pain patho-physiology, pharmacology of analgesics and their limitations have led the researchers to find alternative approaches for pain management. These novel approaches to target the pain management at different levels that support each other with minimal side effects. The aim of the current review article is to provide concisely and up to date information on the available analgesics modalities after total knee arthoplasty, which is important for both safety and effectiveness for most patients. Optimal postoperative analgesia after total knee arthroplasty is the key for earlier recovery and functional outcomes.
Analgesics Options after TKR
The following list includes the available modalities for the management of postoperative analgesia after total knee arthoplasty (TKA):
Pre-emptive analgesia
Local infiltration
Systemic analgesics- opioid, non-opioid, patient-controlled analgesia (PCA)
Neuraxial analgesia
Regional nerve blocks- single shot or continuous
Combinations – multi-modal analgesia
1. Pre-emptive analgesia
Preemptive analgesia, an antinociceptive treatment, is the treatment which is initiated prior to the surgery so that the pain sensitization evoked by the incision-related and inflammatory injuries occurring during surgery can be prevented. Along with conducting before the surgery, Pre-Emptive analgesia can be utilized in the early postoperative period.[25,26] This protective effect is provided by pre-emptive analgesia on the nociceptive system. In order to block the pain sensation, literature has recorded several approaches including drugs and routes:
1a. Parenteral and oral nonsteroidal anti-inflammatory drugs (NSAIDs): Nonsteroidal anti-inflammatory drugs (NSAIDs) involve a category of drugs that have chiefly the analgesic and antipyretic actions.[27] Majority of NSAIDs serve as non-selective inhibitors of the enzyme cyclooxygenase (COX). Further, they also reversibly inhibit both the isoenzymes (COX-1 and COX-2).[28] COX enzyme catalyzes the formation of thromboxane and prostaglandins from arachidonic acid. These released prostaglandins then serve as the messenger molecules in the inflammation pathway.[29]
1b. Sublingual and intravenous (IV) opioids: Opioids are known to produce profound and prolong analgesia. This positive role in pre-emptive analgesia is due to the interaction of opioids with various opioid receptors that ultimately produce analgesia.[30,31] The study carried out by Campiglia et al., report that in patients who underwent elective abdominal surgery, the pre-medication with sublingual morphine sulfate resulted in superior control of postoperative pain, when compared to pre-medication with sublingual midazolam.[32]
1c. Local anesthetics (LA): Local anesthetics are the membrane-stabilizing drugs. They act primarily by hampering sodium influx through voltage-gated sodium channels. This hamper mechanism thereby inhibits the generation of the action potential.[33,34,35]
1d. Systemic antiepileptics (GABA (gamma-amino butyric acid) analogues): The gamma-amino-butyric acid (GABA) analogues like the pregabalin and gabapentin were conventionally employed as therapeutic adjunct towards the management of partial seizures.[36] These both pregabalin and gabapentin are effective in reducing the perioperative pain intensity, opioid consumption and opioid-related side effects, producing very few adverse effects.[37,38,39,40]
II. Local infiltration analgesia (LIA)
This is a simple and effective analgesic technique that involves the permeation of adjuvants throughout the wound at the time of surgery [Figure 1]. The duration of effect of analgesia can be prolonged by the precise placement of a catheter to the surgical site for postoperative administration of further local anesthetic.[41] The most used drugs for both intra-articular and extra-articular injection are morphine, steroid, clonidine, ephenephrine, keterolac, ropivacine, and bupivacaine.
Figure 1.
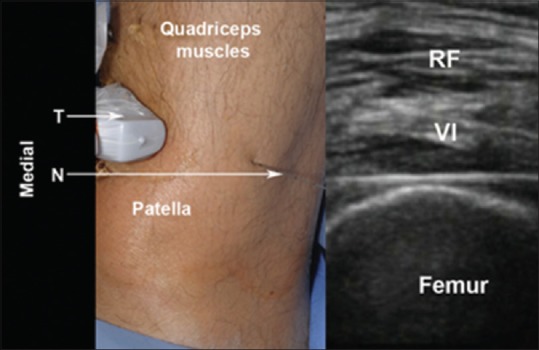
Ultrasound-guided local infiltration. N: Needle; RF: Rectus femoris muscle; T: Transducer (linear, high frequency); VI: Vastus intermedius muscle (Source: R. O'Donnell and J. Dolan* Anaesthesia and analgesia for knee joint arthroplasty. BJA Education, 18(1): 8e15, 2018)
III. Intrathecal morphine with local anesthesia
Local anesthesia supplemented with intrathecal (IT) morphine to alleviate post-operative pain provides good postoperative analgesia. This combination also causes the parenteral opioid-sparing effect for the first 24 hours.[42,43] But, despite several advantages, this approach is linked with increased frequency of urinary retention, nausea-vomiting and pruritus. We suggest that the low dose intrathecal morphine (at around 100 microgram) is very effective and might be safer than single-shot femoral nerve block.[44]
IV. Epidural analgesia
Epidural analgesia has been documented to be extremely beneficial for postoperative pain relief after knee replacement surgeries. This technique is the proven and most successful technique for postoperative analgesia TKA. Without doubt, therefore, epidural analgesia has turned out to be the most widely used procedure in routine clinical practice involving knee replacement surgeries. Very few side-effects of epidural analgesia include some unintended motor blockade, dysfunction in bowel and bladder activity, and hemodynamic instability.[45]
V. Regional nerve block techniques
Regional analgesia Block Techniques in the total knee arthoplasty (TKA) is attaining wide recognition in comparison to epidural analgesia. This approach is involved in fewer side effects and most importantly, is associated with the improved analgesic profile. Regional nerve block proceeds by blocking important nerves in the femoral region, sciatic nerve and common peroneal branches. However, by blocking these major nerves, there might be severe complications causing weakness of the muscles, motor blockade, and even paralysis. All these factors may affect the early functional recovery of the patient.[46]
Femoral nerve block
Femoral nerve is the central nerve supply to the maximum portion of the knee joint.[47] Femoral nerve block (FNB) can be recommended as the technique of choice since it causes better analgesia and less adverse effects. FNB's are one of the oldest blocks employed for TKA analgesia. They have been used because they provide excellent analgesia and are relatively easy to perform. However, the biggest disadvantage of FNB is the risk of fall and its associated quadriceps weakness.[48]
Adductor canal block (ACB)
Adductor canal block (ACB), an ultrasound-guided technique, is one the most important and most simple sensory nerve block for postoperative analgesia following knee surgery. ACB provides quality pain relief when compared to femoral nerve catheter and facilitate discharge of patients after total knee arthroplasty.[49] Adductor canal block causes a good analgesic profile by maintaining quadriceps muscle strength, thereby causing earlier mobility and complete recovery.[50,51,52] [Figure 2].
Figure 2.
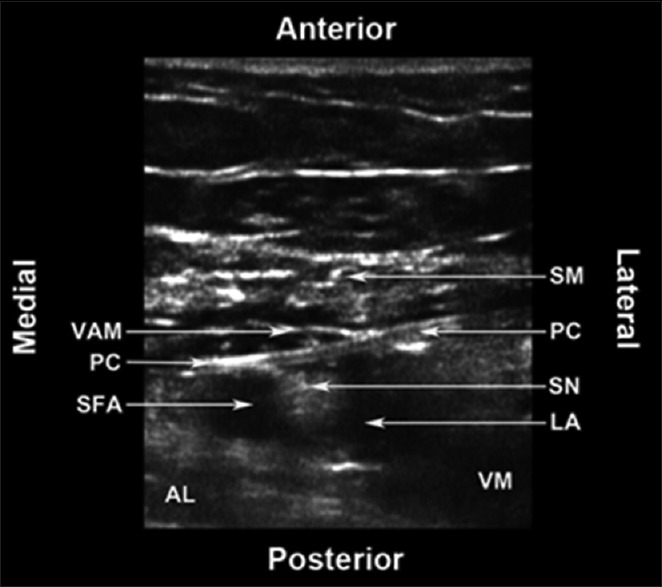
The adductor canal block: AL: Adductor longus muscle; LA: Local anaesthetic; PC: Perineural catheter; SFA: Superficial femoral artery; SM: Sartorius muscle; SN: Saphenous nerve; VAM: Vastoadductor membrane; VM: Vastus medialis muscle. (Source: R. O'Donnell and J. Dolan* Anaesthesia and analgesia for knee joint arthroplasty. BJA Education, 18(1): 8e15, 2018)
Sciatic and selective tibial nerve block
Sciatic nerve provides superior analgesia after TKA.[53] Sciatic nerve blocks the posterior knee pain by blocking at a proximal position in the perigluteal region. The performance of Block within the immediate postoperative period can be quite challenging for the patient. The factors affecting the performance of the sciatic nerve block include the position difficulty in a narcotized patient, the nature of post-operative pain, and the availability of personnel and equipment.[54]
Other potential blocks
Multimodal analgesia after TKA
Multimodal analgesia post-TKA involves the mixture of multiple analgesic drugs with or without techniques which act via distinct mechanism thereby causing synergistic analgesia. Multimodal analgesia post-TKA is a comprehensive approach for postoperative knee pain with an objective to amplify the analgesic effect and reduce the side effects of medications. The most commonly involved drugs in this multimodal analgesia regimen are opioid and their derivatives acetaminophen, gabapentinoid, dexamethasone and ketamine and non-steroidal anti-inflammatory drugs.[55]
I-Pack block
It stands for the Interspace between the Popliteal Artery and the Capsule of the posterior Knee [Figure 3]. This is a comparatively recent block with not many studies worked on this block, but one study suggested that it added as an analgesic advantage when combined with adductor canal block.[56] It is an ultrasound-guided approach which targets to serve analgesia of the posterior knee capsule. It helps by blocking the terminal articular branches of tibial and peroneal nerves sparing the main nerves.
Figure 3.
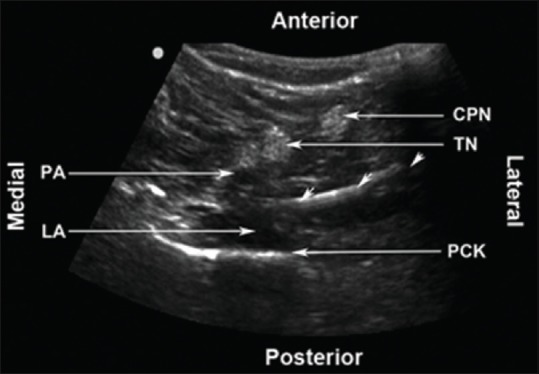
I-PACK Block. CPN: Common peroneal nerve; LA: Local anaesthetic; PA: Popliteal artery; PCK: Posterior capsule of the knee; TN: Tibial nerve. (Source: R. O'Donnell and J. Dolan* Anaesthesia and analgesia for knee joint arthroplasty. BJA Education, 18(1): 8e15, 2018)
Sub-sartorial compartment block
This is an ultrasound-guided injection of local anaesthetic (LA) below the sartorius muscle distal to the adductor hiatus proximal to the knee. This approach aims at depositing LA around saphenous nerve. This nerve is adjacent to the saphenous branch of the genicular artery. In this approach, the block serves as a sensory block and does not cause any motor paralysis.[57]
Obturator nerve block
The relative contribution of the obturator nerve in TKA pain is under dispute. This approach primarily impacts the skin and the adductor muscle over the medial aspect of thigh.[58] The posterior branches follow the popliteal vessels and join with popliteal plexus and may play a part in the posterior knee pain TKA patients.[59,60]
Conclusion
Early rehabilitation and quality analgesia are primary requirements for initial functional recovery post-TKA. Both these requirements are considered essential by both the interventional surgeon and the patient. The correct amalgamation of multimodal and pre-emptive analgesia, technically superior delivery model of regional nerve blocks, and post-operative physical therapy are fundamental components. This approach both speeds up functional recovery and minimizes the side effects of traditional opioid-based analgesia. In summary, it increases patient satisfaction and reduces the overall length of hospitalization and its associated cost.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Vertesich K, Puchner SE, Staats K, Schreiner M, Hipfl C, Kubista B, et al. Distal femoral reconstruction following failed total knee arthroplasty is accompanied with risk for complication and reduced joint function. BMC Musculoskelet Disord. 2019;20:47. doi: 10.1186/s12891-019-2432-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abstracts from the 37th Annual Meeting of the Society of General Internal Medicine. J Gen Int Med. 2014;29:1–545. doi: 10.1007/s11606-014-2834-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feng JE, Novikov D, Anoushiravani AA, Schwarzkopf R. Total knee arthroplasty: Improving outcomes with a multidisciplinary approach. J Multidiscip Healthc. 2018;11:63–73. doi: 10.2147/JMDH.S140550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gan TJ. Poorly controlled postoperative pain: Prevalence, consequences, and prevention. J Pain Res. 2017;10:2287. doi: 10.2147/JPR.S144066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katz JN, Brownlee SA, Jones MH. The role of arthroscopy in the management of knee osteoarthritis. Best Pract Res Clin Rheumatol. 2014;28:143–56. doi: 10.1016/j.berh.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doral MN, Bilge O, Huri G, Turhan E, Verdonk R. Modern treatment of meniscal tears. EFORT Open Rev. 2018;3:260–8. doi: 10.1302/2058-5241.3.170067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wylde V, Beswick A, Bruce J, Blom A, Howells N, Gooberman-Hill R. Chronic pain after total knee arthroplasty. EFORT Open Rev. 2018;3:461–70. doi: 10.1302/2058-5241.3.180004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Society KK. Guidelines for the management of postoperative pain after total knee arthroplasty. Knee Surg Relat Res. 2012;24:201–7. doi: 10.5792/ksrr.2012.24.4.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grosu I, Lavand'homme P, Thienpont E. Pain after knee arthroplasty: An unresolved issue. Knee Surg Sports Traumatol Arthrosc. 2014;22:1744–58. doi: 10.1007/s00167-013-2750-2. [DOI] [PubMed] [Google Scholar]
- 10.Kornilov N, Lindberg MF, Gay C, Saraev A, Kuliaba T, Rosseland LA, et al. Factors related to postoperative pain trajectories following total knee arthroplasty: A longitudinal study of patients admitted to a Russian orthopaedic clinic. Pain Res Treatment. 2016;2016:3710312. doi: 10.1155/2016/3710312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coghill RC. Individual differences in the subjective experience of pain: New insights into mechanisms and models. Headache. 2010;50:1531–5. doi: 10.1111/j.1526-4610.2010.01763.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Draghi F, Ferrozzi G, Urciuoli L, Bortolotto C, Bianchi S. Hoffa's fat pad abnormalities, knee pain and magnetic resonance imaging in daily practice. Insights Imaging. 2016;7:373–83. doi: 10.1007/s13244-016-0483-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McDougall JJ. Arthritis and pain. Neurogenic origin of joint pain. Arthritis Res Ther. 2006;8:220. doi: 10.1186/ar2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bradshaw P, Hariharan S, Chen D. Does preoperative psychological status of patients affect postoperative pain. A prospective study from the Caribbean? Br J Pain. 2016;10:108–15. doi: 10.1177/2049463716635680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lindberg MF, Miaskowski C, Rustøen T, Rosseland LA, Paul SM, Lerdal A. Preoperative pain, symptoms, and psychological factors related to higher acute pain trajectories during hospitalization for total knee arthroplasty. PLoS One. 2016;11:e0161681. doi: 10.1371/journal.pone.0161681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sahoo MR, Gowda MS, Kumar AT. Early rehabilitation after surgery program versus conventional care during perioperative period in patients undergoing laparoscopic assisted total gastrectomy. J Minim Access Surg. 2014;10:132–8. doi: 10.4103/0972-9941.134876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharma V, Morgan PM, Cheng EY. Factors influencing early rehabilitation after THA: A systematic review. Clin Orthop RelatRes. 2009;467:1400–11. doi: 10.1007/s11999-009-0750-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garimella V, Cellini C. Postoperative pain control. Clin Colon Rectal Surg. 2013;26:191–6. doi: 10.1055/s-0033-1351138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rogers E, Mehta S, Shengelia R, Reid MC. Four strategies for managing opioid-induced side effects in older adults. Clin Geriatr. 2013:21. [PMC free article] [PubMed] [Google Scholar]
- 20.WHO Guidelines on the Pharmacological Treatment of Persisting Pain in Children with Medical Illnesses. Geneva: World Health Organization; 2012. [PubMed] [Google Scholar]
- 21.Nada EM, Alabdulkareem A. Morphine versus fentanyl patient-controlled analgesia for postoperative pain control in major hepatic resection surgeries including living liver donors: A retrospective study. Saudi J Anaesth. 2018;12:250. doi: 10.4103/sja.SJA_625_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maddox RR, Oglesby H, Williams CK, Fields M, Danello S. Continuous respiratory monitoring and a “smart” infusion system improve safety of patientcontrolled analgesia in the postoperative period. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 4: Technology and Medication Safety) Rockville (MD): Agency for Healthcare Research and Quality (US); 2008. [PubMed] [Google Scholar]
- 23.Patak LS, Tait AR, Mirafzali L, Morris M, Dasgupta S, Brummett CM. Patient perspectives of patient-controlled analgesia (PCA) and methods for improving pain control and patient satisfaction. Reg Anesth Pain Med. 2013;38:326–33. doi: 10.1097/AAP.0b013e318295fd50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Woodhouse A, Mather LE. The effect of duration of dose delivery with patient-controlled analgesia on the incidence of nausea and vomiting after hysterectomy. Br J Clin Pharmacol. 1998;45:57–62. doi: 10.1046/j.1365-2125.1998.00635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vadivelu N, Mitra S, Schermer E, Kodumudi V, Kaye AD, Urman RD. Preventive analgesia for postoperative pain control: A broader concept. Local Reg Anesth. 2014;7:17–22. doi: 10.2147/LRA.S62160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shah P, Bhosale UA, Gupta A, Yegnanarayan R, Sardesai S. A randomized double-blind placebo-controlled study to compare preemptive analgesic efficacy of novel antiepileptic agent lamotrigine in patients undergoing major surgeries. N Am J Med Sci. 2016;8:93–9. doi: 10.4103/1947-2714.177315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steinmeyer J. Pharmacological basis for the therapy of pain and inflammation with nonsteroidal anti-inflammatory drugs. Arthritis Res. 2000;2:379–85. doi: 10.1186/ar116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meek IL, Van de Laar MA, E Vonkeman H. Non-steroidal anti-inflammatory drugs: An overview of cardiovascular risks. Pharmaceuticals (Basel, Switzerland) 2010;3:2146–2162. doi: 10.3390/ph3072146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brune K, and Patrignani P. New insights into the use of currently available non-steroidal anti-inflammatory drugs. J Pain Res. 2015;8:105–18. doi: 10.2147/JPR.S75160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Hasani R, Bruchas MR. Molecular mechanisms of opioid receptor-dependent signaling and behavior. Anesthesiology. 2011;115:1363–81. doi: 10.1097/ALN.0b013e318238bba6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dumas EO, Pollack GM. Opioid tolerance development: A pharmacokinetic/pharmacodynamic perspective. AAPS J. 2008;10:537–51. doi: 10.1208/s12248-008-9056-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Campiglia L, Cappellini I, Consales G. Premedication with sublingual morphine sulphate in abdominal surgery. Clin Drug Investig. 2009;29:25–30. doi: 10.2165/0044011-200929001-00004. [DOI] [PubMed] [Google Scholar]
- 33.Theile JW, Cummins TR. Recent developments regarding voltage-gated sodium channel blockers for the treatment of inherited and acquired neuropathic pain syndromes. Front Pharmacol. 2011;2:54. doi: 10.3389/fphar.2011.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Swain A, Nag DS, Sahu S, Samaddar DP. Adjuvants to local anesthetics: Current understanding and future trends. World J Clin Cases. 2017;5:307–23. doi: 10.12998/wjcc.v5.i8.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bujedo BM. Current evidence for spinal opioid selection in postoperative pain. Korean J Pain. 2014;27:200–9. doi: 10.3344/kjp.2014.27.3.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zareba G. New treatment options in the management of fibromyalgia: Role of pregabalin. Neuropsychiatr Dis Treat. 2008;4:1193–201. doi: 10.2147/ndt.s3257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Woolf CJ. Central sensitization: Implications for the diagnosis and treatment of pain. Pain. 2011;152:S2–15. doi: 10.1016/j.pain.2010.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Verma V, Singh N, Singh Jaggi A. Pregabalin in neuropathic pain: Evidences and possible mechanisms. Curr Neuropharmacol. 2014;12:44–56. doi: 10.2174/1570159X1201140117162802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bannister K, Sikandar S, Bauer CS, Dolphin AC, Porreca F, Dickenson AH. Pregabalin suppresses spinal neuronal hyperexcitability and visceral hypersensitivity in the absence of peripheral pathophysiology. Anesthesiology. 2011;115:144–52. doi: 10.1097/ALN.0b013e31821f6545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patel R, Dickenson AH. Mechanisms of the gabapentinoids and α 2 δ-1 calcium channel subunit in neuropathic pain. Pharmacol Res Perspect. 2016;4:e00205. doi: 10.1002/prp2.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McCarthy D, Iohom G. Local infiltration analgesia for postoperative pain control following total hip arthroplasty: A systematic review. Anesthesiol Res Pract. 2012;2012:709531. doi: 10.1155/2012/709531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Savjani KT, Gajjar AK, Savjani JK. Drug solubility: Importance and enhancement techniques. ISRN Pharm. 2012;2012:195727. doi: 10.5402/2012/195727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mugabure Bujedo B. A clinical approach to neuraxial morphine for the treatment of postoperative pain. Pain Res Treat. 2012;2012:612145. doi: 10.1155/2012/612145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Álvarez N, Ledesma R, Hamaji A, Hamaji M, Vieira JE. Continuous femoral nerve blockade and single-shot sciatic nerve block promotes better analgesia and lower bleeding for total knee arthroplasty compared to intrathecal morphine: A randomized trial. BMC Anaesthesiol. 2017;17:64. doi: 10.1186/s12871-017-0355-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Turnbull ZA, Sastow D, Giambrone GP, Tedore T. Anesthesia for the patient undergoing total knee replacement: Current status and future prospects. Local Reg Anesth. 2017;10:1–7. doi: 10.2147/LRA.S101373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jiménez-Almonte JH, Wyles CC, Wyles SP, Norambuena-Morales GA, Báez PJ, Murad MH, et al. Is local infiltration analgesia superior to peripheral nerve blockade for pain management after THA: A network meta-analysis. Clin Orthop Relat Res. 2016;474:495–516. doi: 10.1007/s11999-015-4619-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu Q, Chelly JE, Williams JP, Gold MS. Impact of peripheral nerve block with low dose local anesthetics on analgesia and functional outcomes following total knee arthroplasty: A retrospective study. Pain Med (Malden, Mass) 2015;16:998–1006. doi: 10.1111/pme.12652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thacher RR, Hickernell TR, Grosso MJ, Shah R, Cooper HJ, Maniker R, et al. Decreased risk of knee buckling with adductor canal block versus femoral nerve block in total knee arthroplasty: A retrospective cohort study. Arthroplast Today. 2017;3:281–5. doi: 10.1016/j.artd.2017.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rasouli MR, Viscusi ER. Adductor canal block for knee surgeries: An emerging analgesic technique. Arch Bone Jt Surg. 2017;5:131–2. [PMC free article] [PubMed] [Google Scholar]
- 50.Berninger MT, Friederichs J, Leidinger W, Augat P, Bühren V, Fulghum C, et al. Effect of local infiltration analgesia, peripheral nerve blocks, general and spinal anesthesia on early functional recovery and pain control in unicompartmental knee arthroplasty. BMC Musculoskelet Disord. 2018;19:249. doi: 10.1186/s12891-018-2165-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Anastase DM, Cionac Florescu S, Munteanu AM, Ursu T, Stoica CI. Analgesic techniques in hip and knee arthroplasty: From the daily practice to evidence-based medicine. Anesthesiol Res Pract. 2014;2014:569319. doi: 10.1155/2014/569319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gudmundsdottir S, Franklin JL. Continuous adductor canal block added to local infiltration analgesia (LIA) after total knee arthroplasty has no additional benefits on pain and ambulation on postoperative day 1 and 2 compared with LIA alone. Acta Orthop. 2017;88:537–42. doi: 10.1080/17453674.2017.1342184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rodziewicz TL, Tunnell DJ. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2019. [Last updated on 2018 Oct 27]. Sciatic nerve block. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470391/ [PubMed] [Google Scholar]
- 54.Luo J, Min S. Postoperative pain management in the postanesthesia care unit: An update. J Pain Res. 2017;10:2687–98. doi: 10.2147/JPR.S142889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Maheshwari AV, Blum YC, Shekhar L, Ranawat AS, Ranawat CS. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthopaedics Relat Res. 2009;467:1418–23. doi: 10.1007/s11999-009-0728-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thobhani S, Scalercio L, Elliott CE, Nossaman BD, Thomas LC, Yuratich D, et al. Novel regional techniques for total knee arthroplasty promote reduced hospital length of stay: An analysis of 106 patients. Ochsner J. 2017;17:233–8. [PMC free article] [PubMed] [Google Scholar]
- 57.Lee DH, Lee MY, Kwack KS, Yoon SH. Effect of adductor canal block on medial compartment knee pain in patients with knee osteoarthritis: Retrospective comparative study. Medicine. 2017;96:e6374. doi: 10.1097/MD.0000000000006374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bergeron SG, Kardash KJ, Huk OL, Zukor DJ, Antoniou J. Functional outcome of femoral versus obturator nerve block after total knee arthroplasty. Clin Orthop Relat Res. 2009;467:1458–62. doi: 10.1007/s11999-009-0732-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sato K, Sai S, Shirai N, Adachi T. Ultrasound guided obturator versus sciatic nerve block in addition to continuous femoral nerve block for analgesia after total knee arthroplasty. Jpn Clin Med. 2011;2:29–34. doi: 10.4137/JCM.S7399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Runge C, Børglum J, Jensen JM. The analgesic effect of obturator nerve block added to a femoral triangle block after total knee arthroplasty: A randomized controlled trial. Reg Anesth Pain Med. 2016;41:445–51. doi: 10.1097/AAP.0000000000000406. [DOI] [PubMed] [Google Scholar]


