Abstract
Background:
Anesthesia trainee may initially take longer time to intubate and unintentionally place the endotracheal tube (ETT) in the esophagus. The present study determined if ultrasound is the fastest method of confirmation of correct placement of ETT compared to capnography, and chest auscultation in trainees.
Methods:
First year anesthesia residents performed intubation in 120 patients recruited after ethical clearance and informed consent. Time to visualize flutter in trachea, double trachea sign, time to appearance of first and sixth capnography, and time to execute chest auscultation was noted.
Results:
Ultrasonography was statistically fastest method to determine endotracheal intubation (36.50 ± 15.14 seconds) vs unilateral chest auscultation (50.29 ± 15.50 seconds) vs bilateral chest auscultation (51.90 ± 15.98 seconds) vs capnography first waveform (53.57 ± 15.97 seconds) vs capnography sixth waveform (61.67 ± 15.88 seconds).
Conclusion:
When teaching endotracheal intubation to novice anesthesia residents using conventional direct laryngoscopy, ultrasonography is the fastest method to confirm correct ETT placement compared to capnograph and chest auscultation. Mentor can guide trainee to direct ETT towards trachea and can promptly detect esophageal intubation by double trachea sign.
Keywords: Endotracheal intubation, trainee anaesthetist, ultrasound
Introduction
Confirmation of endotracheal intubation is commonly done by chest auscultation and capnograph executed only after the endotracheal tube (ETT) is placed in the trachea. Endotracheal intubation is the most important technique that an anesthesia trainee learns which initially may take longer time to perform with unintentional placement of ETT in esophagus causing oxygen desaturation in the patient with morbidity.[1,2,3,4]
For teaching endotracheal intubation, simultaneous visualization of the airway by both trainee and mentor would be ideal for which a video laryngoscope is not the choice as it involves modification from the conventional laryngoscopy and thus is not the initial teaching tool for trainees.
Ultrasound has recently been used to confirm endotracheal intubation with real time images by placing a linear ultrasound probe transversely on the anterior aspect of the neck at the level of the cricothyroid membrane.
We hypothesized that as ultrasound visualization of endotracheal intubation is in real time, it would be the fastest method to confirm correct ETT placement when being performed by novice anesthesia trainees compared to conventional methods of chest auscultation and capnography, which can be performed only after endotracheal intubation is done.
The primary objective was to determine whether ultrasound is the fastest method of confirmation of correct placement of ETT compared to capnography, and chest auscultation when performed by novice anesthesia trainees. Secondary objective was to determine if ultrasound could aid to guide the endotracheal tube towards the trachea if going towards esophagus.
Methods
The present study was a prospective, single-blinded, controlled clinical trial to assess the reliability of ultrasound-guided intubation as a method for confirmation of endotracheal intubation conducted in the department of anaesthesiology, pain medicine, and critical care at All India Institute of medical Sciences in New Delhi. The institutional ethics committee approval was obtained. 120 patients, who were scheduled for elective surgery requiring general anesthesia with oro-tracheal intubation, were enrolled in the study. A written informed consent was taken from all the patients. Inclusion criteria was consenting males and female patients aged between 18-80 years with BMI <30 kg/m2 posted for elective surgeries requiring general anaesthesia with oro-tracheal intubation. Exclusion Criteria included refusal to participate in the study, patients with predictors of difficult intubation; Modified Mallampati class 3 and 4, Thyromental distance <6.5 cm, negative upper lip bite test, restricted neck movements (flexion <25 degrees, extension <85 degrees) and previous history of difficult intubation.
Novice anesthesia residents in first year of training period as postgraduate residents in the specialty of anaesthesiology were the subjects who performed endotracheal intubation. They were grouped into residents in their first six months of training and residents who were in the sixth to twelfth month of training period. Two attending anaesthesiologists who had prior experience in using ultrasound for airway assessment in their clinical practice performed all ultrasound assessments.
Patients were kept nil per oral overnight and were premedicated with tablet Alprazolam 0.25 mg and tablet Ranitidine 150 mg (per oral, at bedtime and in the coming morning of surgery with sips of water) along with any other routine medications taken by the patient. On the day of surgery, the patient was shifted to the operating room and all the standard monitors were attached and an IV access was secured. After pre-oxygenation with 100% oxygen for 3 minutes, anesthesia was induced with standard drugs.
Sonosite M-Turbo ultrasound machine (Sonosite, Inc, Bothell, WA, USA) with a HFL38 linear transducer (6-13 MHz) was placed transversely on the anterior aspect of the neck, at a level just below the cricoid cartilage by observer (one of the two attending anaesthesiologist with experience of using ultrasound for airway assessment) to visualize the trachea and esophagus in the same visual field. The first year anesthesia resident performed the intubation, and simultaneously the observer visualized the trachea in ultrasonography and noted the passage of the endotracheal tube through the trachea. In case the ETT was observed to be moving towards/hitting/passing through the esophagus, the observer immediately asked the resident to redirect the ETT towards the direction where trachea was present.
After the intubation was performed, second observer confirmed the placement of the ETT into the trachea by quantitative waveform capnography, and noted the time to appearance of the first and sixth capnography waveform. Third observer auscultated the chest for the presence of bilateral air entry and noted the time. All three observers were blinded to each other's observations and were not allowed to communicate with each other.
Observer one noted the time from removal of the facemask to the ultrasound confirmation of endotracheal intubation by passage of ETT through the trachea, seen as a brief flutter alongside an empty esophagus. Observer two noted the time for intubation from removal of the facemask till confirmation by capnography and the appearance of first waveform, and the appearance of the sixth waveform. Simultaneously, observer three performed chest auscultation and noted the time from removal of the facemask till confirmation with unilateral as well as bilateral air entry. The number of times the ETT on ultrasound was see hitting the esophagus, passing into the esophagus or hitting any other structure was also noted.
In all the patients the placement of the ETT was confirmed by all three methods, namely: Ultrasonography, waveform capnography and chest auscultation for air entry. The following parameters were noted; time to intubation confirmed via ultrasound, time to intubation confirmed via appearance of the first waveform on capnography, time to intubation confirmed via appearance of the sixth waveform on capnography, time to intubation confirmed via chest auscultation on the right side for air entry, time to intubation confirmed via chest auscultation on both sides for air entry, number of times the ETT hit the esophagus or any other structure, desaturation of SpO2 below 95%.
In any ambiguity was seen in the above observations, the mentor came to the head end of the patient and confirmed the correct placement of the ETT, by performing a repeat direct laryngoscopy. These patients were noted but were excluded from the present study. Also, in case the resident took more than three minutes for intubation or if the oxygen saturation of the patient decreased (SpO2 <95%) an experienced anaesthesiologist performed the endotracheal intubation. All these patients were also excluded from the study.
Statistical analysis
Anticipating a sensitivity of 94% (on the lower side) and prevalence of esophageal intubation of 12.5%, the estimated sample size was 103 patients, with a 95% confidence interval. Assuming a dropout rate of 15%, the final number of patients enrolled in the study was 120.
Agreement and time comparison was done between the three techniques of confirming the correct placement of endotracheal tube. The data was analyzed using IBM SPSS Statistics version 16. To validate the reliability of ultrasonography as a method for confirmation of correct placement of the ETT, as compared to capnography and chest auscultation, Pearson's correlation test and reliability analysis using interclass correlation coefficient calculation were used. Confirmation by ultrasonography was compared with confirmation with capnography by the appearance of the first waveform as well as appearance of sixth consecutive waveform. Similarly, ultrasonography was also compared with chest auscultation both unilaterally as well as bilaterally as methods of confirmation of correct placement of ETT. Comparisons of the mean time taken for confirmation of correct placement of ETT by the three methods included in this study were done using the student's paired t test. P value less than 0.05 was considered as statistically significant.
A reliability analysis using the calculation of interclass correlation coefficient (ICC) was done to assess the degree of agreement between the three methods included in the study.
Results
The demographic parameters of all the patients including age, sex, weight, height, and BMI were comparable between both groups [Tables 1 and 2].
Table 1.
Demographic data of the study population
| Variable | Mean±SD |
|---|---|
| Age (years) | 39.02±13.19 |
| Weight (kg) | 62.28±11.56 |
| Height (cm) | 157.68±9.24 |
| BMI (kg/m2) | 24.89±3.10 |
Table 2.
Sex and modified Mallampati (MMP) class of study population
| Variable | Number (%) |
|---|---|
| Sex | |
| Male | 34 (28) |
| Female | 86 (72) |
| MMP class | |
| I | 46 (41) |
| II | 74 (59) |
Ultrasonography confirmation of endotracheal intubation was at mean time of 36.50 ± 15.14 seconds (mean ± SD). Confirmation using chest auscultation for air entry showed a mean time of 50.29 ± 15.50 seconds (mean ± SD) for unilateral chest auscultation and a mean time of 51.90 ± 15.98 seconds (mean ± SD) for bilateral chest auscultation. Confirmation with capnography using appearance of first waveform was found with a mean time of 53.57 ± 15.97 seconds (mean ± SD), and a mean time of 61.67 ± 15.88 seconds (mean ± SD) was recorded for the appearance of sixth waveform on capnography [Table 3].
Table 3.
Mean time to confirm correct placement of ETT
| Variable | Total time taken for confirmation (s) mean±SD |
|---|---|
| Ultrasound | 36.50±15.14 |
| U/L chest auscultation | 50.29±15.50 |
| B/L chest auscultation | 51.90±15.18 |
| Capnography (1st waveform) | 53.57±15.97 |
| Capnography (6th waveform) | 61.67±15.88 |
The mean time differences were calculated and analyzed using Pearson's correlation test. The mean time difference between ultrasound and unilateral as well as bilateral chest auscultation was found to be statistically significant (P <0.001), 13.79 ± 4.12 seconds (mean ± SD) and 15.41 ± 4.22 seconds (mean ± SD), respectively. On comparison with capnography, the appearance of first waveform had a statistically significant meantime difference of 17.07 ± 3.56 seconds (mean ± SD) with ultrasonography (p of <0.001). The appearance of the sixth waveform on capnography showed a mean time difference of 25.17 ± 4.40 seconds (mean ± SD) with ultrasound (p of < 0.001) [Table 4].
Table 4.
Mean time difference between ultrasonography with chest auscultation and capnography
| Variable | Time difference from usg: mean±SD (s) | Pearson’s correlation value | P |
|---|---|---|---|
| U/L chest auscultation | 13.79±4.12 | 0.964 | <0.001* |
| B/L chest auscultation | 15.41±4.22 | 0.961 | <0.001* |
| Capnography (1st waveform) | 17.07±3.56 | 0.975 | <0.001* |
| Capnography (6th waveform) | 25.17±4.40 | 0.961 | <0.001* |
P<0.05, statistically significant, usg: Ultrasonography
Pearson's correlation test showed a strong positive association between ultrasonography, capnography and chest auscultation [Table 5]. Pearson's correlation test between ultrasound confirmation and chest auscultation showed a strong positive correlation (with r values of 0.964 for U/L chest auscultation and 0.961 for B/L chest auscultation) which was statistically significant, P < 0.001. Pearson's correlation coefficient ('r' value) of 0.975 was obtained between ultrasonography confirmation and the appearance of the first waveform on capnography and 'r' value between ultrasonography and appearance of the sixth waveform on capnography was 0.961, both were statistically significant with P < 0.001.
Table 5.
Pearson’s correlation of ultrasonography with chest auscultation and capnography
| Variable | Pearson’s correlation coefficient (r) | P |
|---|---|---|
| U/L chest auscultation | 0.964 | <0.001* |
| B/L chest auscultation | 0.961 | <0.001* |
| Capnography 1st waveform | 0.975 | <0.001* |
| Capnography 6th waveform | 0.961 | <0.001* |
*(P<0.05 statistically significant)
ICC value for ultrasound and U/L chest auscultation was 0.9816 (p < 0.001). ICC value of ultrasound with B/L chest auscultation was 0.9803 (P < 0.001). ICC value of ultrasound with the first waveform on capnography was 0.9867 (P < 0.001). ICC for ultrasound with appearance of the sixth waveform on capnography was 0.9795 (P < 0.001). Thus ultrasonography was found to be in strong agreement with both chest auscultation and capnography [Table 6].
Table 6.
Interclass correlation coefficient (ICC) of ultrasonography, chest auscultation and capnography
| Variable | ICC value | 95% confidence interval | P | |
|---|---|---|---|---|
| Upper limit | Lower limit | |||
| Ultrasound with U/L chest auscultation | 0.9816 | 0.9735 | 0.9872 | <0.001* |
| Ultrasound with B/L chest auscultation | 0.9803 | 0.9717 | 0.9863 | <0.001* |
| Ultrasound with capnography (1st waveform) | 0.9867 | 0.9809 | 0.9908 | <0.001* |
| Ultrasound with capnography (6th waveform) | 0.9795 | 0.9706 | 0.9858 | <0.001* |
*(P<0.05 statistically significant)
In five out of 120 patients ETT hit the esophagus as seen on ultrasound and the ETT was redirected towards the trachea. No ETT entered the trachea. All 120 endotracheal intubations were confirmed by capnography and chest auscultation. In one patient the observer was not able to visualize flicker of the trachea however there was also no visualization of double hump sign indirectly confirming the trachea to be in trachea. Sensitivity and specificity of ultrasound to correctly identify endotracheal intubation was found to be 99.17% and 100% respectively [Table 7].
Table 7.
Ultrasonography in detecting correct placement of the ETT
| Statistical test | Value (%) | 95% Confidence interval | |
|---|---|---|---|
| Lower limit | Upper limit | ||
| Specificity | 100 | 47.82 | 100 |
| Sensitivity | 99.17 | 95.44 | 99.98 |
| Positive predictive value | 100 | 96.95 | 100 |
| Negative predictive value | 83.33 | 35.88 | 99.58 |
Experience of the novice anaesthesiologist, intubating the patient divided into two groups. Group A included residents who were in their first six months of training and Group B included residents who were in the 6-12 months period of training. Out of the total 120 intubations which were performed in the study, 69 were done by residents belonging to group A, while 51 of them were performed by residents belonging to group B. All five intubation attempts, where ETT hit the esophagus was done by Group A residents.
None of the patients in the study had a desaturation of less than 97%, and there were no complications or adverse effects.
Discussion
In the present study the mean total time taken for endotracheal confirmation with ultrasound was significantly less at 36.50 ± 15.14 seconds compared to confirmation with unilateral chest auscultation (mean total time of 50.29 ± 15.50 seconds; time lag of 13.79 ± 4.12 seconds compared to ultrasound), bilateral chest auscultation for air entry (51.90 ± 15.18 seconds; time lag of 15.41 ± 4.22 seconds), capnography first wave and capnograph sixth wave. In five patients, ultrasound detected ETT hitting the esophagus. During endotracheal intubation in one patient, flutter of the ETT passing into the trachea was not detected on ultrasound however absence of a double trachea sign confirmed placement of ETT in the trachea.
Teaching the correct method of endotracheal intubation is an important part in the training of anesthesia residents. In the beginning of the training period, novice anesthesia residents may take longer time to intubate and the ETT may accidently be placed in the esophagus causing oxygen desaturation especially in patients with low functional residual capacity like obese patients.[1,2,3,4]
In the traditional method of teaching ETT, the mentor stands by the side of the resident who performs intubation. While performing direct laryngoscopy only the resident can view the progress of ETT towards larynx. Before intubation is attempted the mentor may confirm the view of larynx by coming to the head end of the patient however this does not ensure that the ETT would be placed correctly in trachea. Confirmation of correct placement of ETT is done by a repeat laryngoscopy by mentor, by capnograph or by bilateral chest auscultation.
Disadvantage of repeat laryngoscopy include hypertensive response with oral secretions obscuring airway view. Disadvantage of bilateral chest auscultation is missed esophageal intubations in many instances.[5] Disadvantages of capnography include waiting for at least 6 continuous capnographic waveforms or for 1 minute after intubation to be certain that the capnographic trace is from the trachea.[6,7] The present study demonstrated that ultrasound confirmation of correct ET intubation is statistically faster than capnography even with first waveform. Moreover capnography relies on physiological factors like ventilation, adequate pulmonary perfusion and gas exchange for its confirmation. In conditions of impaired ventilation like bronchospasm and inadequate pulmonary perfusion like cardiac arrest or pulmonary embolism, capnography may fail to correctly identify an endotracheal intubation.[8,9]
On placing a linear ultrasound probe on the anterior part of the neck at the level on cricoid, trachea is visualized in the midline as an inverted-U shaped structure, characterized by hyperechoic air-mucosal interface with a reverberation artifact posteriorly.[10,11] The esophagus is visualized deep to the trachea on its left side and can be easily identified, before induction, by the peristaltic movements seen on asking the patient to swallow.[10] When ETT, passes through the trachea, it appears as a hyperechoic bright structure, seen as a brief flutter, producing acoustic shadowing or comet-tail artifacts, which helps in visualizing it.[12,13,14,15,16,17,18,19,20,21,22,23] If the ETT accidentally enters the esophagus, it is seen as a bright hyperechoic curved line with a distal dark shadow, which is present posterior, and to the left of the trachea, giving rise to a double trachea sign [Figure 1].[15,24] This technique is independent of the patient's physiological state as it relies on the anatomical visualization of structures and also doesn't interfere with the act of performing a laryngoscopy.
Figure 1.
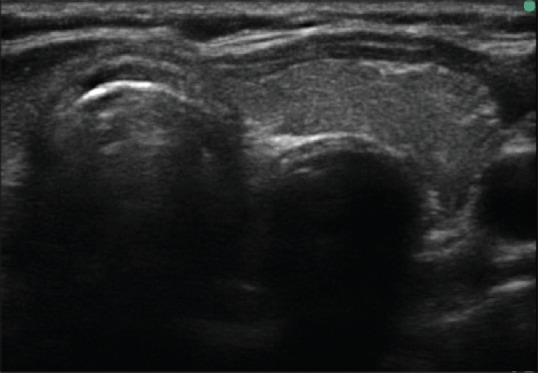
ETT inside esophagus (double trachea sign)
In a study on 25 patients posted for elective surgery, lung ultrasound (using pleural sliding sign) for verifying endotracheal intubation was compared with auscultation. Median time for verification by lung ultrasound was 40 seconds vs. 42 seconds for auscultation alone, with a mean difference of 0.88 seconds in favor of lung ultrasound.[25] As the authors performed lung ultrasound and compared auscultation with the total time consumed till bilateral pleural sliding sign was observed, not much significant time difference was observed. However in the present study auscultation with real time trans-cricoid ultrasonography for visualization of passage of endotracheal tube was done which gave a significant time lag of 14-15 seconds. Muslu et al. conducted a blinded prospective randomized study in seventy-five adult patients posted for elective surgery where anaesthesiologist randomly intubated the trachea or esophagus with direct laryngoscopy and the sonographers had to identify them with ultrasound with transducer placed transversely on the neck above the suprasternal notch. The sonographers were able to detect tracheal tube placement within 3 seconds of intubation with sensitivity and specificity of ETT to be 100% concluding, ultrasonography to be a fast and effective technique for confirming tracheal intubation.[13] In a systematic review and meta-analysis of 12 studies involving adult patients and cadaveric models, ultrasonography was found to have a high diagnostic value for identifying esophageal intubations. Detection of esophageal intubations had a pooled sensitivity of 93% and a specificity of 97%. This makes ultrasound a valuable adjunct in airway assessment, especially in situations where capnography may be unreliable.[26] A prospective study conducted in an urban teaching hospital in New York, concluded that bedside upper airway ultrasonography is a feasible method/tool to verify the placement of endotracheal tube as compared to continuous capnography.[18] Pfeifer et al. in their study compared the temporal relationship between ultrasound with chest auscultation and capnography in comparing ETT placement in emergency setting. They found that ultrasound is faster than the standard method of auscultation and capnography.[27] However their study was conducted in emergency setting. Ultrasonography is not affected by physiological factors and can be very useful in similar situations where capnography results are ambiguous.
Though video laryngoscopy and fiberoptic bronchoscopy have been found to be effective in training residents in the skill of intubation, they involve modifications of the conventional technique and are not the first method of training the trainees to perform ET intubation.[27,28,29,30] The video based methods are difficult to perform when blood or secretions are present in the airway and obscure the view. These do not affect ultrasonography as it relies on visualizing the airway and the process of intubation from outside.
In one male patient with a BMI of 29 kg/m2 ultrasonography was not able to identify endotracheal placement of the ETT possibly due to higher BMI which could have made flutter at intubation not very clear. Also the flash of acoustic shadow observed on endotracheal placement of the ETT is very rapid and can be missed. As the esophagus remained empty and collapsed in this patient with no double trachea sign, it was certain on ultrasound assessment that the ETT was not in the esophagus, which was also confirmed, by chest auscultation and capnography.
Another significant clinical finding observed in the present study was that, in all five patients in whom the ETT hit the esophagus, it was promptly detected by the ultrasound and the resident was asked to redirect the tube towards the trachea immediately. This real time, immediate detection saves valuable time and prevents morbidity and desaturation in patients. The five residents who while attempting endotracheal intubation, inadvertently ended up hitting the esophagus with the ETT were all in their first six months of training period in anesthesia. Accidental esophageal intubations is more commonly done by the residents in the initial period of their training even when performing direct laryngoscopy and passing the ETT through the vocal cords under direct vision. In the present study however, all the misplaced intubations were promptly detected and none of the patients had an arterial oxygen saturation drop below 97%. In the present study, we found ultrasound to be a reliable method for confirming endotracheal intubation when compared to capnography and consumed lesser time than both chest auscultation and capnography. Also ultrasound was able to detect the misplaced esophageal intubations promptly and redirect the ETT towards the trachea.
The limitations of the present study were that all intubations were performed on patients with MMP class I and II. Thus the results cannot be extrapolated to intubations carried out by novice anesthesia residents on patients with an anticipated difficult airway but in these situations in all probability the intubation would not be handed to the novice anesthetist. In the present study ultrasonography was used only to visualize the passage of the ETT through the trachea and was not used to determine endobronchial intubation. Also blinding was not possible in the five instances where the ETT hit the esophagus and the mentor had to guide the resident to redirect the ETT towards the trachea.
In conclusion, when teaching endotracheal intubation to novice anesthesia residents using conventional direct laryngoscopy, ultrasonography can be used as a reliable method to confirm correct placement of ETT, when compared to capnography and chest auscultation it is the fastest method. Ultrasonography can also promptly detect esophageal intubations by the appearance of double trachea sign and the resident can be guided to redirect the ETT towards the trachea.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Footnote: Presented at Canadian Anesthesia Society, Annual conference, Niagra falls.
Registration of trial: CTRI/2018/03/012820 (Clinical trials registry India).
References
- 1.Adriani J. Unrecognized esophageal placement of endotracheal tubes. South Med J. 1986;79:1591–3. doi: 10.1097/00007611-198612000-00029. [DOI] [PubMed] [Google Scholar]
- 2.Adriani J, Naraghi M, Ward M. Complications of endotracheal intubation. South Med J. 1988;8:739–44. doi: 10.1097/00007611-198806000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Clyburn P, Rosen M. Accidental oesophageal intubation. BJA. 1994;73:55–63. doi: 10.1093/bja/73.1.55. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology. 1995;82:367. doi: 10.1097/00000542-199502000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Andersen KH, Schultz-Lebahn T. Oesophageal intubation can be undetected by auscultation of the chest. Acta Anaesthesiol Scand. 1994;38:580–2. doi: 10.1111/j.1399-6576.1994.tb03955.x. [DOI] [PubMed] [Google Scholar]
- 6.Dorsch JA, Dorsch SE. “Gas Monitoring” Understanding Anesthesia Equipment. 5th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008. pp. 705–20. [Google Scholar]
- 7.Kristensen MS. Confirmation of Endotracheal Intubation Benumof and Hagberg's Airway Management: Principles and Practice. 3rd ed. New York: Elsevier Science; pp. 657–82. [Google Scholar]
- 8.Takeda T, Tanigawa K, Tanaka H, Hayashi Y, Goto E, Tanaka K. The assessment of three methods to verify tracheal tube placement in the emergency setting. Resuscitation. 2003;56:153–7. doi: 10.1016/s0300-9572(02)00345-3. [DOI] [PubMed] [Google Scholar]
- 9.Bhende MS, Thompson AE, Cook DR, Saville AL. Validity of a disposable end-tidal CO2 detector in verifying endotracheal tube placement in infants and children. Ann Emerg Med. 1992;21:142–5. doi: 10.1016/s0196-0644(05)80148-9. [DOI] [PubMed] [Google Scholar]
- 10.Singh M, Chin KJ, Chan VW, Wong DT, Prasad GA, Yu E. Use of sonography for airway assessment: An observational study. J Ultrasound Med. 2010;29:79–85. doi: 10.7863/jum.2010.29.1.79. [DOI] [PubMed] [Google Scholar]
- 11.Kundra P, Mishra SK, Ramesh A. Ultrasound of the airway. Indian J Anaesth. 2011;55:456–62. doi: 10.4103/0019-5049.89868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chou HC, Chong KM, Sim SS, Ma MH, Liu SH, Chen NC, et al. Real-time tracheal ultrasonography for confirmation of endotracheal tube placement during cardiopulmonary resuscitation. Resuscitation. 2013;84:1708–12. doi: 10.1016/j.resuscitation.2013.06.018. [DOI] [PubMed] [Google Scholar]
- 13.Muslu B, Sert H, Kaya A, Demircioglu RI, Gözdemir M, Usta B, et al. Use of sonography for rapid identification of esophageal and tracheal intubations in adult patients. J Ultrasound Med. 2011;30:671–6. doi: 10.7863/jum.2011.30.5.671. [DOI] [PubMed] [Google Scholar]
- 14.Chou HC, Tseng WP, Wang CH, Ma MH, Wang HP, Huang PC, et al. Tracheal rapid ultrasound exam (TRUE) for confirming endotracheal tube placement during emergency intubation. Resuscitation. 2011;82:1279–84. doi: 10.1016/j.resuscitation.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 15.Ma G, Davis DP, Schmitt J, Vilke GM, Chan TC, Hayden SR. The sensitivity and specificity of transcricothyroid ultrasonography to confirm endotracheal tube placement in a cadaver model. J Emerg Med. 2007;32:405–7. doi: 10.1016/j.jemermed.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 16.Hoffmann B, Gullett JP, Hill HF, Fuller D, Westergaard MC, Hosek WT, et al. Bedside ultrasound of the neck confirms endotracheal tube position in emergency intubations. Ultrasound in Med. 2014;35:451–8. doi: 10.1055/s-0034-1366014. [DOI] [PubMed] [Google Scholar]
- 17.Werner SL, Smith CE, Goldstein JR, Jones RA, Cydulka RK. Pilot study to evaluate the accuracy of ultrasonography in confirming endotracheal tube placement. Ann Emerg Med. 2007;49:75–80. doi: 10.1016/j.annemergmed.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 18.Milling TJ, Jones M, Khan T, Tad-y D, Melniker LA, Bove J, et al. Transtracheal 2-D ultrasound for identification of esophageal intubation. J Emerg Med. 2007;32:409–14. doi: 10.1016/j.jemermed.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 19.Kristensen MS, Teoh WH, Graumann O, Laursen CB. Ultrasonography for clinical decision-making and intervention in airway management: From the mouth to the lungs and pleurae. Insights Imaging. 2014;5:253–79. doi: 10.1007/s13244-014-0309-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prasad A, Yu E, Wong DT, Karkhanis R, Gullane P, Chan VW. Comparison of sonography and computed tomography as imaging tools for assessment of airway structures. J Ultrasound Med. 2011;30:965–72. doi: 10.7863/jum.2011.30.7.965. [DOI] [PubMed] [Google Scholar]
- 21.Drescher MJ, Conard FU, Schamban NE. Identification and description of esophageal intubation using ultrasound. Acad Emerg Med. 2000;7:722–5. doi: 10.1111/j.1553-2712.2000.tb02055.x. [DOI] [PubMed] [Google Scholar]
- 22.Chenkin J, McCartney CJL, Jelic T, Romano M, Heslop C, Bandiera G. Defining the learning curve of point-of-care ultrasound for confirming endotracheal tube placement by emergency physicians. Crit Ultrasound J. 2015;7:14. doi: 10.1186/s13089-015-0031-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adi O, Chuan T, Rishya M. A feasibility study on bedside upper airway ultrasonography compared to waveform capnography for verifying endotracheal tube location after intubation. Crit Ultrasound J. 2013;5:7. doi: 10.1186/2036-7902-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsung JW, Fenster D, Kessler DO, Novik J. Dynamic anatomic relationship of the esophagus and trachea on sonography: Implications for endotracheal tube confirmation in children. J Ultrasound Med. 2012;31:1365–70. doi: 10.7863/jum.2012.31.9.1365. [DOI] [PubMed] [Google Scholar]
- 25.Pfeiffer P, Rudolph S, Børglum J, Isbye D. Temporal comparison of ultrasound vs. auscultation and capnography in verification of endotracheal tube placement. Acta Anaesthesiol Scand. 2011;55:1190–5. doi: 10.1111/j.1399-6576.2011.02501.x. [DOI] [PubMed] [Google Scholar]
- 26.Weiss M, Schwarz U, Dillier CM, Gerber AC. Teaching and supervising tracheal intubation in paediatric patients using videolaryngoscopy. Paediatr Anaesth. 2001;11:343–8. doi: 10.1046/j.1460-9592.2001.00681.x. [DOI] [PubMed] [Google Scholar]
- 27.Kaplan MB, Ward DS, Berci G. A new video laryngoscope-an aid to intubation and teaching. J Clin Anesth. 2002;14:620–6. doi: 10.1016/s0952-8180(02)00457-9. [DOI] [PubMed] [Google Scholar]
- 28.Owen H, Plummer JL. Improving learning of a clinical skill: The first year's experience of teaching endotracheal intubation in a clinical simulation facility. Med Educ. 2002;36:635–42. doi: 10.1046/j.1365-2923.2002.01260.x. [DOI] [PubMed] [Google Scholar]
- 29.Wheeler M, Sullivan CL, Heffner CL, Coté CJ. Teaching residents pediatric fiberoptic intubation of the trachea. Anesthesiology. 2004;4:842–6. doi: 10.1097/00000542-200410000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Low D, Healy D, Rasburn N. The use of the BERCI DCI® video laryngoscope for teaching novices direct laryngoscopy and tracheal intubation. Anaesthesia. 2008;63:195–201. doi: 10.1111/j.1365-2044.2007.05323.x. [DOI] [PubMed] [Google Scholar]


