Abstract
Objective:
Postoperative nausea and vomiting (PONV) is a daily phenomenon, to which less attention has been paid in a variety of surgeries. Despite the individual studies, there is no comprehensive study on the prevalence of PONV. The aim of this study was to determine the global prevalence of PONV.
Materials and Methods:
In this systematic and meta-analysis study, descriptive studies of four databases (PubMed, Web of Science, Scopus, and Google Scholar) were searched for relevant texts from the time they were created until 31 December 2018. The random effects model was used for meta-analysis of studies included. All the steps were carried out by two individuals. Hoy et al.'s tool was used to evaluate its risk bias.
Results:
A total of 23 studies that were performed on 22,683 people from 11 countries were entered into the final phase. The prevalence of PONV, nausea, and vomiting was 27.7%, 31.4%, and 16.8%, respectively. The prevalence of PONV was higher during the first 24 h in European countries.
Conclusion:
Considering the high prevalence of PONV and our goal to better control it, it is necessary to use high cost-effective approaches and recommendations and to educate health caregivers and patients.
Keywords: Meta-analysis, postoperative nausea and vomiting, prevalence, surgery complications
Introduction
Nowadays, attention to postoperative time is as important as the intraoperative time. PONV is an unpleasant and commonly occurring phenomenon after surgical procedures.[1] Nausea refers to a feeling of a tendency to vomiting and vomiting refers to reflux of the gastric contents.[2] Nausea and vomiting are a multidimensional phenomenon and are affected by various risk factors. The most important factors affecting the incidence of postoperative nausea and vomiting (PONV) include female gender, nonsmoker, and high age.[3] Although there is no accurate information on the prevalence of PONV worldwide, individual studies indicate a prevalence of 20%–30% in normal populations[1,4] and 70%–80% in high-risk populations (tonsillectomy, strabismus, and laparoscopy).[5] PONV imposes a lot of impacts on patients, which leads to decreased quality of life and overall satisfaction, dehydration, electrolyte imbalance, aspiration of gastric secretions, esophageal rupture, bleeding, increased morbidity, increased hospitalization time, delayed discharge from hospital, delayed return to work, and, more importantly, increased rehospitalization.[6,7,8,9,10,11]
On the contrary, PONV imposes billions of dollars to the healthcare system annually due to increased surgical complications, unpredictable hospitalizations, long-term nursing care, and increased care required in postoperative recovery.[12,13,14] Despite the plenty of texts available, PONV has been studied in terms of the various definitions, risk factors, complications, and management, but there are only individual studies on PONV prevalence, and despite the vast searches carried out by researchers, as well as its great importance, there has still been no comprehensive study in this regard. Determining the precise prevalence of PONV can help better manage it by surgeons, nurses, and patients. It also helps policymakers in determining effective operational programs to deal with it. The aim of this study was to determine the prevalence of PONV after surgery.
Materials and Methods
Registration and eligibility criteria
The protocol has been registered (PROSPERO: CRD42019130265). The methods adopted for this systematic review were developed in accordance with the Cochrane book and PRISMA checklist.[15] Institutional Review Board approval and informed patients' consent were not needed for this type of studies. Cross-sectional, case–control, and cohort studies were included, and case series, letter to editors, case reports, clinical trials, study protocols, systematic reviews, and narrative reviews were excluded from this study. Participants: All studies conducted on patients with breast cancer were included. Outcome: The main objective was quality of life. The outcome was collected as reported. Sampling methods and sample size: All observational studies with any sampling and census designs were included in the systematic review. The minimum required sample size was ≥25 patients.
Search strategy
Searches were conducted by two independent researchers in four international databases, PubMed, Web of Science, Scopus, and Google Scholar, for related studies from the inception of the databases to 31 December 2018 in English language. To ensure literature saturation, the reference lists of included studies or relevant reviews identified through the search were scanned. The specific search strategies were created by a Health Sciences Librarian with expertise in systematic review search using the MESH terms and free terms according to the PRESS standard.[16] After the MEDLINE strategy was finalized, it was adapted to search in other databases. Accordingly, PROSPERO was searched for ongoing or recently related completed systematic reviews. The key words used in the search strategy were “prevalence,” “incidence,” “epidemiology,” “nausea,” “vomiting,” “Postoperative nausea and vomiting,” and “PONV” combined with Boolean operators including AND, OR, and NOT.
Selection of studies and data extraction
Two researchers independently screened the titles and abstracts considering the eligibility criteria. After removing duplicated studies, full texts of the studies were screened depending on the eligibility criteria, and the required information were extracted. To resolve questions about eligibility, additional information were obtained from the authors of the study where necessary. The consensus method was used to solve controversies between the two researchers. Extracted data items were first author, year, country, sampling method, design, year of data collection, type of surgery, participants, gender (male/female), age, setting, sample size and risk of bias, and prevalence of nausea, vomiting, and PONV.
Quality assessment
To assess the methodological quality and risk of bias of each included observational study, Hoy et al.'s tool was used.[17] This 10-item tool was used to evaluate the quality of studies in two dimensions including external validity (items 1–4 assessed the target population, sampling frame, sampling method, and nonresponse bias minimal) and internal validity (items 5–9 assessed the data collection method, case definition, study instrument, and mode of data collection, while item 10 assessed bias related to data analysis). The risk of bias was independently evaluated by two researchers. Disagreements were resolved through consensus method.
Data synthesis
All the eligible studies were included in the synthesis after a systematic review. Data were combined with the forest plot. The prevalence of PONV was evaluated by the random effects model. The heterogeneity of the preliminary studies was evaluated with I2 tests. Subgroup analysis was conducted to determine the heterogeneity based on the age, type of surgery, and gender. Meta-analysis was performed using STAT 14 statistical software.
Results
Overall results
Study selection
A total of 403 articles from initial searches were retrieved in various databases. Of 361 nonduplicated studies in the title and abstract screening process, 311 studies were excluded due to inappropriate titles. Out of 50 studies, 23 had eligibility criteria. Out of 27 excluded studies, 10 studies were review, 1 study was letter to the editor, 4 studies had no full text, 10 studies were published in non-English language, and 2 studies did not meet the minimum quality requirements for inclusion in the study [Figure 1].
Figure 1.
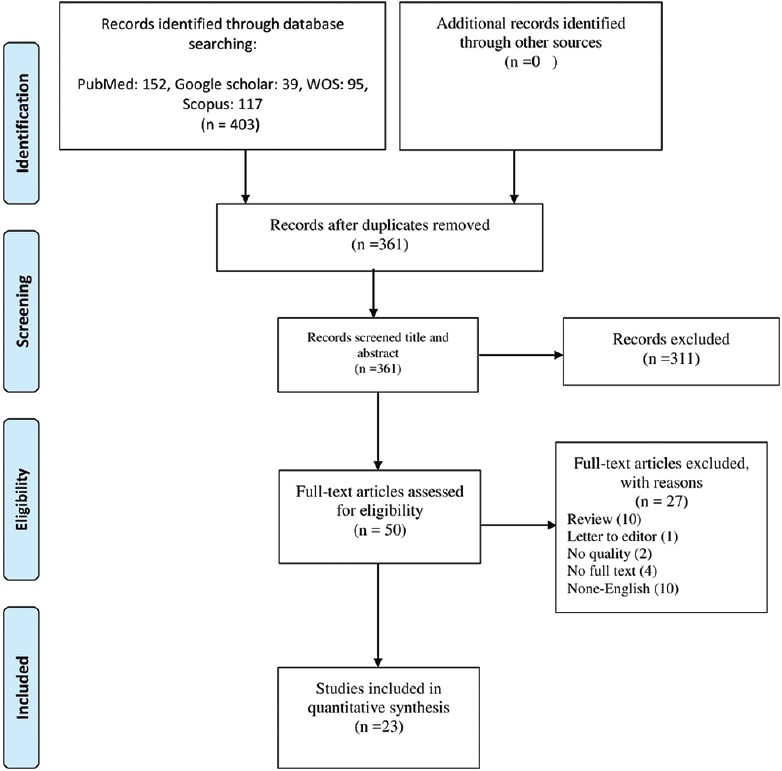
Flow diagram of study selection
Study characteristics
Twenty-three studies were conducted on 22,683 participants from 11 countries from 2002 to 2018. The age range of the participants was between 5 and 73 years. Of the 23 included, more studies were carried out in the United States (n = 7), South Korea (n = 5), and Czech Republic and Japan (n = 2) for each country. The most common sampling method was census (n = 19), and the design of included studies was prospective cross-sectional (n = 14), respectively. Data were collected in most studies (n = 21) between 2000 and 2015. The time of data collection was not mentioned in two studies. PONV was recorded and reported based on standard forms after the surgery. PONV was recorded and reported in most studies (n = 17) within 24 h of surgery. It was also reported in the recovery room (RR) in six studies and 48 h postoperatively in three studies. Regarding the type of surgery, patients with any type of surgery were included in the study in most studies (n = 11). Regarding the consequences examined, PONV was specifically reported in most studies (n = 19). Nausea and vomiting were reported separately in 11 and 12 studies, respectively. Most studies (n = 22) had low bias risk [Table 1].
Table 1.
Demographic characteristics of included studies
| First author (year) | Year | Country | Sampling method | Design | Year of data collection | Type of surgery | Participants | Age (years) | Time of assessment | Outcomes | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Adamek,S.[23] | 2013 | Czech Republic | Census | Prospective cross-sectional | 2011-2012 | Abdominal | 109 | 65 | 24 h | PONV | Low |
| Bradshaw,W. A.[24] | 2002 | USA | Census | Prospective cross-sectional | 2000 | Abdominal | 104 | 48 | 24 h | PONV, nausea | Low |
| Choi,J. B.[25] | 2014 | South Korea | Census | Retrospective cross-sectional | 2011 | All surgeries | 1878 | 51 | 48 h | PONV | Low |
| Conti,D.[26] | 2014 | Italy | Census | Retrospective cross-sectional | 2011-2012 | All surgeries | 1347 | 73 | RR | PONV | Low |
| Doubravska,L.[27] | 2010 | Czech Republic | Census | Prospective cross-sectional | 2008 | All surgeries | 1942 | 51.3 | 24 h | PONV, nausea, vomiting | Low |
| East,J. M.[28] | 2010 | Jamaica | Census | Retrospective cohort | 2007 | Abdominal | 266 | 36.6 | RR/24 h | PONV | Low |
| Habib,Ashraf S[29] | 2006 | USA | Census | Retrospective cross-sectional | 2004 | All surgeries | 3641 | 52 | 24 h/RR | PONV, nausea, vomiting | Low |
| Hara,R.[30] | 2013 | Japan | Census | Retrospective cross-sectional | 2007-2009 | All surgeries | 1200 | 50.0 | 24 h | PONV, vomiting | Low |
| Hijazi,E. M.[31] | 2018 | Jordan | Census | Prospective cross-sectional | 2013-2015 | Heart surgery | 300 | 57.7 | 48 h | Nausea, vomiting | Low |
| Latz,B.[32] | 2011 | Germany | Census | Prospective cross-sectional | 2011 | Craniotomy | 229 | 54 | RR/24 h | PONV, nausea, vomiting | Low |
| Lee,J.[33] | 2016 | USA | Census | Retrospective cross-sectional | 2012-2015 | Heart surgery | 160 | 5.6 | 24 h | Vomiting | Low |
| Maddali,M. M.[34] | 2003 | Oman | Census | Prospective cross-sectional | 2003 | All surgeries | 491 | UK | 24 h | PONV | Low |
| Moreno,C.[35] | 2013 | Portugal | Census | Prospective cross-sectional | 2011 | All surgeries | 157 | 57 | RR/24 H | PONV | Low |
| Morino,R.[36] | 2013 | Japan | Census | Prospective cross-sectional | 2010 | All surgeries | 1645 | 59 | 24 H/48 H | PONV, nausea, vomiting | Low |
| Odom-Forren,J.[37] | 2013 | USA | Census | Prospective cross-sectional | 2013 | All surgeries | 248 | 52 | RR | Nausea, vomiting | Moderate |
| Oh,AY[38] | 2010 | South Korea | Random | Prospective cross-sectional | 2010 | Eye surgery | 78 | 7.5 | 24 H | PONV | Low |
| Phillips,C[39] | 2015 | USA | Consecutive | Prospective cross-sectional | 2008-2012 | Orthognathic surgery | 204 | 19 | 24 h | Nausea, vomiting | Low |
| Silva,Alessandro[40] | 2006 | USA | Census | Retrospective cross-sectional | 2006 | Orthognathic surgery | 514 | 31.34 | 24 h | PONV | Low |
| Villeret,I[41] | 2002 | France | Census | Prospective cross-sectional | 2001 | All surgeries | 407 | 5 | 24 h | PONV, nausea, vomiting | Low |
| Wilson,S[42] | 2009 | USA | Census | Retrospective cross-sectional | UK | Breast surgery | 148 | 52.2 | 24 h | PONV | Low |
| Won,Young Ju[43] | 2011 | South Korea | Consecutive | Prospective cross-sectional | 2009-2010 | Thyroidectomy | 177 | 44.1 | 24 h | PONV, nausea, vomiting | Low |
| Yi,M[44] | 2018 | South Korea | Census | Retrospective cross-sectional | 2010-2015 | All surgeries | 6773 | 50.21 | 24 h | PONV | Low |
| Yoo,J. Y[45] | 2013 | South Korea | Consecutive | Prospective cross-sectional | UK | Thyroidectomy | 170 | 41.5 | 24 h | PONV, nausea, vomiting | Low |
PONV: Postoperative nausea and vomiting; RR: Recovery room, UK: Unknown
Meta-analysis of PONV prevalence
Overall, 23 studies were included to the meta-analysis. Of all included studies, 19 studies reported PONV index and the 4 remaining studies reported only nausea and/or vomiting, separately. PONV prevalence in the overall (occurring during the RR or first 24 or 48 h after surgery) 19 studies was reported to be between 6.7% and 73.4% worldwide. Based on the results of random effect method, the overall prevalence of PONV in 21,276 patients was 27.7% [95% confidence interval (CI): 23.3, 32.1; I2= 98.4%].
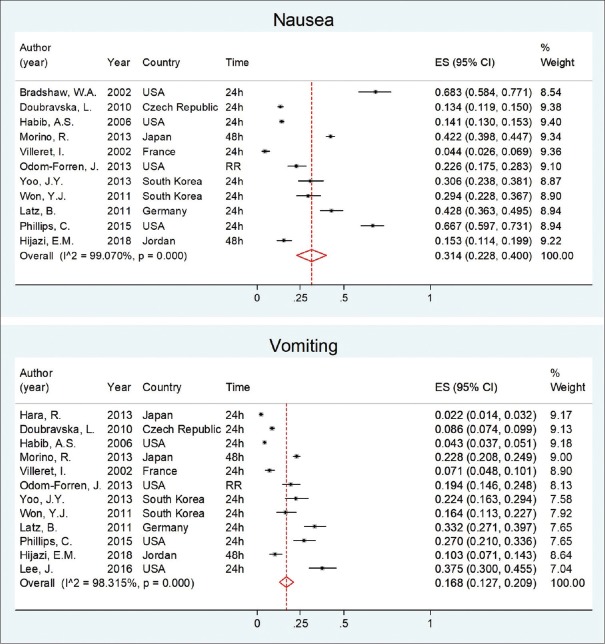
The prevalence of nausea in the overall 11 studies was reported to be between 6.7% and 73.4%, and the prevalence of vomiting in 12 studies was reported to be between 2.2% and 37.5%. Pooled prevalence based on random effect method of nausea and vomiting in 9067 and 10,323 patients was 31.4% (95% CI: 22.8, 40.0; I2 = 99.0%) and 16.8% (95% CI: 12.7, 20.9; I2 = 98.3%), respectively [Figure 2].
Figure 2.
Forest plot and pooled analyses of nausea and vomiting prevalence after surgery worldwide
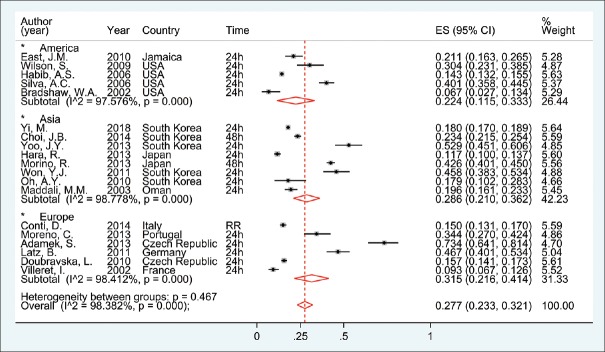
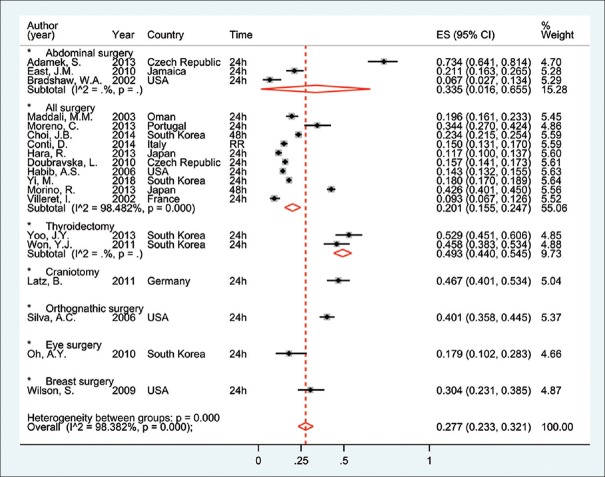
Subgroup analysis was done based on continents, type of surgery, and time of PONV. The prevalence of PONV in Europe is higher than in other continents; and therefore the pool estimated (in random model) prevalence in Europe and America was 31.5% (95% CI: 21.6, 41.4; I2 = 98.4%) and 22.4% (95% CI: 16.3, 26.5; I2 = 97.6%), respectively [Figure 3]. In all of 19 study witches reported PONV, 10 study conducted in all type of surgery and other 9 study conducted in specific surgery wards. Subgroup analysis based on the type of surgery showed pooled prevalence of PONV for 10 studies with all surgery participants to be 20.1% (95% CI: 15.5, 24.7; I2 = 98.5%) [Figures 4 and 5]. The pooled prevalence of PONV in the first 24 h was 1.7 times as high as in RR. Also, the pooled prevalence of nausea and vomiting in RR was lower than first 24 h after surgery [Table 2].
Figure 3.
Forest plot, pooled analyses, and subgroup analyses by continents for estimation of PONV prevalence after surgery worldwide
Figure 4.
Forest plot, pooled analyses, and subgroup analyses by type of surgery for estimation of PONV prevalence after surgery worldwide
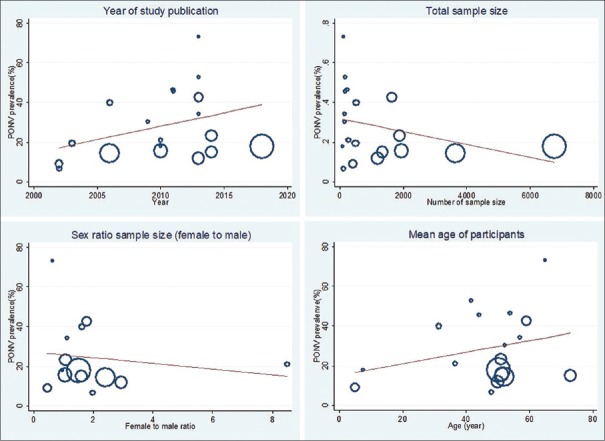
Figure 5.
Meta-regression between prevalence of PONV and year of study publication, total and sex ratio sample size, and mean age of participants worldwide
Table 2.
Result of meta-analysis for estimation the PONV prevalence by time of surgery worldwide
| First author (year) | Country | Nausea; ES (95% CI) | Vomiting; ES (95% CI) | PONV; ES (95% CI) | |||
|---|---|---|---|---|---|---|---|
| First 24 h | Recovery room | First 24 h | Recovery room | First 24 h | Recovery room | ||
| Yi, M. (2018)[44] | South Korea | 18 (17.0, 18.9) | |||||
| Lee, J. (2016)[33] | USA | 37.5 (30.0, 45.5) | |||||
| Phillips, C. (2015)[39] | USA | 66.7 (59.7, 73.1) | 27.0 (21.0, 33.6) | ||||
| Conti, D. (2014)[26] | Italy | 15.0 (13.1, 17.0) | |||||
| Adamek, S. (2013)[23] | Czech Republic | 73.4 (64.1, 81.4) | |||||
| Hara, R. (2013)[30] | Japan | 2.2 (1.4, 3.2) | 11.7 (10.0, 13.7) | ||||
| Moreno, C. (2013)[35] | Portugal | 34.4 (27.0, 42.4) | 24.8 (18.3, 32.4) | ||||
| Morino, R. (2013)[36] | Japan | 40.0 (37.6, 42.4) | 21.9 (20.0, 24.0) | 40.6 (38.2, 43.0) | |||
| Odom-Forren, J. (2013)[37] | USA | 22.6 (17.5, 28.3) | 19.4 (14.6, 24.8) | ||||
| Yoo, J.Y. (2013)[45] | South Korea | 30.6 (23.8, 38.1) | 22.4 (16.3, 29.4) | 52.9 (45.1, 60.6) | |||
| Latz, B. (2011)[32] | Germany | 42.8 (36.3, 49.5) | 28.4 (22.6, 34.7) | 33.2 (27.1, 39.7) | 15.7 (11.3, 21.1) | 46.7 (40.1, 53.4) | 28.8 (23.0, 35.2) |
| Won, Y.J. (2011)[43] | South Korea | 29.4 (22.8, 36.7) | 16.4 (11.3, 22.7) | 45.8 (38.3, 53.4) | |||
| Doubravska, L. (2010)[27] | Czech Republic | 13.4 (11.9, 15.0) | 8.6 (7.4, 9.9) | 15.7 (14.1, 17.3) | |||
| East, J.M. (2010)[28] | Jamaica | 21.1 (16.3, 26.5) | 3.4 (1.6, 6.3) | ||||
| Oh, A.Y. (2010)[38] | USA | 17.9 (10.2, 28.3) | |||||
| Wilson, S. (2009)[42] | USA | 30.4 (23.1, 38.5) | |||||
| Habib, A.S. (2006)[29] | USA | 14.1 (13.0, 15.3) | 14.3 (13.1, 15.4) | 4.3 (3.7, 5.1) | 2.8 (2.3, 3.4) | 14.3 (13.2, 15.5) | 15.0 (13.8, 16.2) |
| Silva, A.C. (2006)[40] | USA | 40.1 (35.8, 44.5) | |||||
| Maddali, M.M. (2003)[34] | Oman | 19.6 (16.1, 23.3) | |||||
| Bradshaw, W.A. (2002)[24] | USA | 68.3 (58.4, 77.1) | 6.7 (2.7, 13.4) | ||||
| Villeret, I. (2002)[41] | France | 4.4 (2.6, 6.9) | 7.1 (4.8, 10.1) | 9.3 (6.7, 12.6) | |||
| Overall random pooled ES | 33.9 (2.6, 6.9) | 21.4 (12.4, 30.4) | 17.1 (12.6, 21.5) | 12.4 (0.6, 24.3) | 28.7 (23.8, 33.6) | 16.7 (10.7, 22.7) | |
PONV: Postoperative nausea and vomiting; ES: Effect size; CI: Confidence interval
Meta-regression analysis
We used meta-regression analysis based on the year of study publication, total and sex ratio sample size, the mean age of participants, and variables to identify source of heterogeneity of PONV prevalence. In the univariable model, there was no significant association between included variables and PONV prevalence (P > 0.05) [Figure 5].
Discussion
Although PONV is one of the most common complications after a variety of surgeries, there are many texts on definitions, causes, and therapeutic recommendations; there are fewer studies on the exact incidence and severity of this disorder in the world. According to researchers' best knowledge, this is the first meta-analysis study in the field. This systematic review and meta-analysis was conducted to determine the prevalence of PONV worldwide. In this study, 23 studies that were conducted on 22,683 participants from 2002 to 2018 in different countries were entered into the final analysis phase. The results of the study showed that the overall prevalence of PONV was 27.7% worldwide. There was no previous study that merely examined the incidence of PONV using meta-analysis method, but a review nonsystematic study that was performed in previous years indicated PONV prevalence to be 25%,[18] indicating an increase in PONV prevalence considering increasing frequency and types of surgical procedures, complex surgical procedures, therapeutic methods, and recommendations for controlling PONV. Previous studies that specifically examined nausea and vomiting reported the prevalence to be 31.4% and 16.8%, respectively. Although nausea is a primary cause of vomiting in most cases, and these two factors are interrelated, they should be considered as a single complication.[19] The prevalence of PONV was higher in Europe. The difference in the prevalence of PONV in different continents can be attributed to the demographic characteristics of the populations under study, the type of surgeries, different PONV management procedures used in countries, and methods used to record and measure it in these countries. The results of this study showed that the prevalence of PONV in surgery of breast and abdominal cancers is more than other surgeries, which is consistent with some previous evidence.[20] Although the effect of the type of surgery on the prevalence of PONV is still discussed as one of the controversial issues due to the effect of the patients' characteristics and the factors associated with anesthesia, many evidences, especially the large trials, showed no relationship between the type of surgery and prevalence of PONV.[3,6,21] There was no significant relationship between PONV frequency with gender and age. Contrary to previous evidence which showed the effect of woman's age and gender on PONV prevalence,[20,22] as younger individuals and women suffer from a higher prevalence of PONV, this can be due to differences in the methodology used to conduct previous studies and the present study.
Limitation
(1) All studies were descriptive studies that have cross-sectional methodology limitations. (2) Considering data collection tools, there was no consistent method in various studies that resulted in diversity of data extracted, and thus only shared data were extracted for the purpose of data consistency. (3) In many studies, there was no complete information in the text, and thus attempts were made to contact with the corresponding authors. (4) Only English-language studies were introduced; as a result, studies published in other languages were excluded.
Strengths
(1) A systematic review and meta-analysis approach was used to collect and analyze data. (2) According to researchers' best knowledge, this is the first study in this area. (3) In addition to the overall prevalence of PONV, nausea and vomiting were also extracted and analyzed in separate studies. The prevalence of PONV was also extracted based on reported periods (RR, 24 h, and 48 h).
Conclusion
The aim of this present systematic review study and meta-analysis was to evaluate the global prevalence of PONV after surgery. The results of the study indicate a high prevalence of PONV. Considering the lower attention in the clinic and the ability to prevent it, attention to its precise prevalence and the use of guidelines, proper training of patients before surgery, and the provision of the necessary infrastructure seem necessary.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Dolin S, Cashman J, Bland J. Effectiveness of acute postoperative pain management: I. Evidence from published data. Br J Anaesth. 2002;89:409–23. [PubMed] [Google Scholar]
- 2.Becker DE. Nausea, vomiting, and hiccups: A review of mechanisms and treatment. Anesth Prog. 2010;57:150–7. doi: 10.2344/0003-3006-57.4.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Apfel C, Heidrich F, Jukar-Rao S, Jalota L, Hornuss C, Whelan RP, et al. Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br J Anaesth. 2012;109:742–53. doi: 10.1093/bja/aes276. [DOI] [PubMed] [Google Scholar]
- 4.Gan TJ, Meyer TA, Apfel CC, Chung F, Davis PJ, Habib AS, et al. Society for ambulatory anesthesia guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2007;105:1615–28. doi: 10.1213/01.ane.0000295230.55439.f4. [DOI] [PubMed] [Google Scholar]
- 5.Kovac AL. Update on the management of postoperative nausea and vomiting. Drugs. 2013;73:1525–47. doi: 10.1007/s40265-013-0110-7. [DOI] [PubMed] [Google Scholar]
- 6.Apfel CC, Läärä E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting conclusions from cross-validations between two centers. Anesthesiology. 1999;91:693–700. doi: 10.1097/00000542-199909000-00022. [DOI] [PubMed] [Google Scholar]
- 7.Eberhart L, Högel J, Seeling W, Staack A, Geldner G, Georgieff M. Evaluation of three risk scores to predict postoperative nausea and vomiting. Acta Anaesthesiol Scand. 2000;44:480–8. doi: 10.1034/j.1399-6576.2000.440422.x. [DOI] [PubMed] [Google Scholar]
- 8.Scuderi PE, Conlay LA. Postoperative nausea and vomiting and outcome. Int Anesthesiol Clin. 2003;41:165–74. doi: 10.1097/00004311-200341040-00012. [DOI] [PubMed] [Google Scholar]
- 9.Stadler M, Bardiau F, Seidel L, Albert A, Boogaerts JG. Difference in risk factors for postoperative nausea and vomiting. Anesthesiology. 2003;98:46–52. doi: 10.1097/00000542-200301000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Toprak V, Keles G, Kaygisiz Z, Tok D. Subcutaneous emphysema following severe vomiting after emerging from general anesthesia. Acta Anaesthesiol Scand. 2004;48:917–8. doi: 10.1111/j.0001-5172.2004.00456.x. [DOI] [PubMed] [Google Scholar]
- 11.Wu CL, Naqibuddin M, Rowlingson AJ, Lietman SA, Jermyn RM, Fleisher LA. The effect of pain on health-related quality of life in the immediate postoperative period. Anesth Analg. 2003;97:1078–85. doi: 10.1213/01.ANE.0000081722.09164.D5. [DOI] [PubMed] [Google Scholar]
- 12.Le TP, Gan TJ. Update on the management of postoperative nausea and vomiting and postdischarge nausea and vomiting in ambulatory surgery. Anesthesiol Clin. 2010;28:225–49. doi: 10.1016/j.anclin.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 13.Odom-Forren J, Fetzer SJ, Moser DK. Evidence-based interventions for post discharge nausea and vomiting: A review of the literature. J Perianesth Nurs. 2006;21:411–30. doi: 10.1016/j.jopan.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Watcha MF. The cost-effective management of postoperative nausea and vomiting. Anesthesiology. 2000;92:931–3. doi: 10.1097/00000542-200004000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6. doi: 10.1016/j.jclinepi.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 17.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: Modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65:934–9. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 18.Kovac AL. Prevention and treatment of postoperative nausea and vomiting. Drugs. 2000;59:213–43. doi: 10.2165/00003495-200059020-00005. [DOI] [PubMed] [Google Scholar]
- 19.Gan TJ. Risk factors for postoperative nausea and vomiting. Anesth Analg. 2006;102:1884–98. doi: 10.1213/01.ANE.0000219597.16143.4D. [DOI] [PubMed] [Google Scholar]
- 20.Öbrink E, Jildenstål P, Oddby E, Jakobsson JG. Post-operative nausea and vomiting: Update on predicting the probability and ways to minimize its occurrence, with focus on ambulatory surgery. Int J Surg. 2015;15:100–6. doi: 10.1016/j.ijsu.2015.01.024. [DOI] [PubMed] [Google Scholar]
- 21.Apfel CC, Philip BK, Cakmakkaya OS, Shilling A, Shi YY, Leslie JB, et al. Who is at risk for postdischarge nausea and vomiting after ambulatory surgery? Anesthesiology. 2012;117:475–86. doi: 10.1097/ALN.0b013e318267ef31. [DOI] [PubMed] [Google Scholar]
- 22.Horn CC, Wallisch WJ, Homanics GE, Williams JP. Pathophysiological and neurochemical mechanisms of postoperative nausea and vomiting. Eur J Pharmacol. 2014;722:55–66. doi: 10.1016/j.ejphar.2013.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adamek S, Matouskova O, Polanecky O, Svetlik S, Skorepa J, Snajdauf M. The effect of postoperative pain treatment on the incidence of anastomotic insufficiency after rectal and rectosigmoideal surgery. Prague Med Rep. 2013;114:214–21. doi: 10.14712/23362936.2014.10. [DOI] [PubMed] [Google Scholar]
- 24.Bradshaw WA, Gregory BC, Finley CR, Ross A, Wilds T, Still M, et al. Frequency of postoperative nausea and vomiting in patients undergoing laparoscopic foregut surgery. Surg Endosc. 2002;16:777–80. doi: 10.1007/s00464-001-8342-0. [DOI] [PubMed] [Google Scholar]
- 25.Choi JB, Shim YH, Lee YW, Lee JS, Choi JR, Chang CH. Incidence and risk factors of postoperative nausea and vomiting in patients with fentanyl-based intravenous patient-controlled analgesia and single antiemetic prophylaxis. Yonsei Med J. 2014;55:1430–5. doi: 10.3349/ymj.2014.55.5.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Conti D, Ballo P, Boccalini R, Boccherini A, Cantini S, Venni A, et al. The effect of patient sex on the incidence of early adverse effects in a population of elderly patients. Anaesth Intensive Care. 2014;42:455–9. doi: 10.1177/0310057X1404200405. [DOI] [PubMed] [Google Scholar]
- 27.Doubravska L, Dostalova K, Fritscherova S, Zapletalova J, Adamus M. Incidence of postoperative nausea and vomiting in patients at a university hospital. Where are we today? Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2010;154:69–76. doi: 10.5507/bp.2010.012. [DOI] [PubMed] [Google Scholar]
- 28.East JM, Mitchell DI. Emergency open cholecystectomy is associated with markedly lower incidence of postoperative nausea and vomiting (PONV) than elective open cholecystectomy: A retrospective cohort study. BMC Surg. 2010;10:6. doi: 10.1186/1471-2482-10-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Habib AS, Chen YT, Taguchi A, Henry Hu X, Gan TJ. Postoperative nausea and vomiting following inpatient surgeries in a teaching hospital: A retrospective database analysis. Curr Med Res Opin. 2006;22:1093–9. doi: 10.1185/030079906X104830. [DOI] [PubMed] [Google Scholar]
- 30.Hara R, Hirota K, Sato M, Tanabe H, Yazawa T, Habara T, et al. The impact of remifentanil on incidence and severity of postoperative nausea and vomiting in a university hospital-based ambulatory surgery center: A retrospective observation study. Korean J Anesthesiol. 2013;65:142–6. doi: 10.4097/kjae.2013.65.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hijazi EM, Edwan H, Al-Zoubi N, Radaideh H. Incidence of Nausea and Vomiting After Fast-Track Anaesthesia for Heart Surgery. Braz J Cardiovasc Surg. 2018;33:371–5. doi: 10.21470/1678-9741-2018-0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Latz B, Mordhorst C, Kerz T, Schmidt A, Schneider A, Wisser G, et al. Postoperative nausea and vomiting in patients after craniotomy: Incidence and risk factors. J Neurosurg. 2011;114:491–6. doi: 10.3171/2010.9.JNS10151. [DOI] [PubMed] [Google Scholar]
- 33.Lee J, Faraoni D, Lee S, Brown M, Odegard K, Randolph A, et al. Incidence and risk factors for postoperative vomiting following atrial septal defect repair in children. Paediatr Anaesth. 2016;26:644–8. doi: 10.1111/pan.12908. [DOI] [PubMed] [Google Scholar]
- 34.Maddali MM, Mathew J, Fahr J, Zarroug AW. A prospective study of incidence of postoperative nausea and vomiting in a tertiary care hospital in Oman. Middle East J Anaesthesiol. 2003;17:131–41. [PubMed] [Google Scholar]
- 35.Moreno C, Veiga D, Pereira H, Martinho C, Abelha F. Postoperative nausea and vomiting: Incidence, characteristics and risk factors – A prospective cohort study. Rev Esp Anestesiol Reanim. 2013;60:249–56. doi: 10.1016/j.redar.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 36.Morino R, Ozaki M, Nagata O, Yokota M. Incidence of and risk factors for postoperative nausea and vomiting at a Japanese Cancer Center: First large-scale study in Japan. J Anesth. 2013;27:18–24. doi: 10.1007/s00540-012-1468-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Odom-Forren J, Jalota L, Moser DK, Lennie TA, Hall LA, Holtman J, et al. Incidence and predictors of postdischarge nausea and vomiting in a 7-day population. J Clin Anesth. 2013;25:551–9. doi: 10.1016/j.jclinane.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 38.Oh A, Kim J, Hwang J, Do S, Jeon Y. Incidence of postoperative nausea and vomiting after paediatric strabismus surgery with sevoflurane or remifentanil–sevoflurane. Br J Anaesth. 2010;104:756–60. doi: 10.1093/bja/aeq091. [DOI] [PubMed] [Google Scholar]
- 39.Phillips C, Brookes CD, Rich J, Arbon J, Turvey T. Postoperative nausea and vomiting following orthognathic surgery. Int J Oral Maxillofac Surg. 2015;44:745–51. doi: 10.1016/j.ijom.2015.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Silva AC, O'Ryan F, Poor DB. Postoperative nausea and vomiting (PONV) after orthognathic surgery: A retrospective study and literature review. J Oral Maxillofac Surg. 2006;64:1385–97. doi: 10.1016/j.joms.2006.05.024. [DOI] [PubMed] [Google Scholar]
- 41.Villeret I, Laffon M, Duchalais A, Blond M, Lecuyer A, Mercier C. Incidence of postoperative nausea and vomitingin paediatric ambulatory surgery. Pediatr Anesth. 2002;12:712–7. doi: 10.1046/j.1460-9592.2002.00952.x. [DOI] [PubMed] [Google Scholar]
- 42.Wilson S, Meyer H, Fecho K. Postoperative nausea and vomiting after inpatient and outpatient breast surgery: Incidence and effects of midazolam. Ambul Surg. 2009;15:1–19. [Google Scholar]
- 43.Won YJ, Yoo JY, Chae YJ, Kim DH, Park SK, Cho HB, et al. The incidence of postoperative nausea and vomiting after thyroidectomy using three anaesthetic techniques. J Int Med Res. 2011;39:1834–42. doi: 10.1177/147323001103900526. [DOI] [PubMed] [Google Scholar]
- 44.Yi MS, Kang H, Kim MK, Choi GJ, Park YH, Baek CW, et al. Relationship between the incidence and risk factors of postoperative nausea and vomiting in patients with intravenous patient-controlled analgesia. Asian J Surg. 2018;41:301–6. doi: 10.1016/j.asjsur.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 45.Yoo JY, Chae YJ, Cho HB, Park KH, Kim JS, Lee SY. Comparison of the incidence of postoperative nausea and vomiting between women undergoing open or robot-assisted thyroidectomy. Surg Endosc. 2013;27:1321–5. doi: 10.1007/s00464-012-2607-7. [DOI] [PubMed] [Google Scholar]