Abstract
Neoteric studies have called attention to the prominence of management in healthcare sectors. Positive relationship have been noticed between performance management, clinical performance, and clinical outcome. However, there is still debate related to which managers have to lead healthcare organizations, and what kind of management should be followed, we are now about to analyze. Systematic review of the literature is a starting point to present and discuss the current of information concerning with how management can affect the quality and perpetuity of health systems. Through in-depth analysis of 27 studies, we concluded that the performance of healthcare systems and organizations positively consistent with leadership, management practices, manager characteristics, and cultural features that are related to values and administrative approaches. There was also testimony that doctors who lead healthcare organizations show excellence in performance better than others. Finally, this review acting as roadmap which indicating how do the relationship between the management and performance of healthcare systems, and organizations can be furtherly investigated.
Keywords: Healthcare system, leadership, management, performance
Introduction
For the last decade, sustainability and quality maintenance at affordable cost were the main targets of all healthcare systems against which they compete to achieve.[1] The last few years has witnessed era of technological upgrades and spurts in diagnostic science, which lead to increase in life expectancy, patients' concerns and expectations. This in turn resulted in rising in healthcare costs.[2] And this was proved, in the recent economic slump.[3] It was a surpassing defiance to all healthcare systems to maintain their funding levels and make it as mortgage for innovation, customer expectations and epidemiology.[4]
The Value of Management and the Management of Value
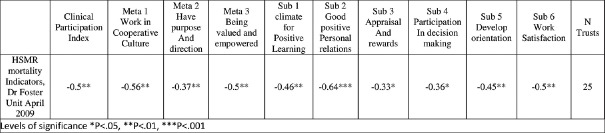
Equity and accessibility issues emerge when these costs ought to be covered by the patient himself.[5] Quality and costs, double edged weapon and two ends of string which pulled by societies who strive to reduce costs. And the other end pulled by stakeholders seeking quality improvements and accessibility. The increased awareness of the patient being the center of the healthcare system, intensified the existing needs about the quality of services.[6] The cost crisis and the increased efforts of containment in the western region since 1960 was due to technological upgrades and spurts in diagnostic science,[7] pushed many healthcare organizations accordingly, to overlook the efficiency of care due to tremendous increase in costs and funds, and this in turn negatively affected sustainability. This problem in sustainability together with lack of efficiency will be solved by pumping money along with public resources allocated to increased insurance costs.[8] The response of the physicians and all staff was to press to refund for the healthcare system, this was happening when the care delivery system was itself the technical system (plagued tax-based systems vicious circle) Figure 1. Physicians always pay attention to patient, effectiveness, and evidence-based practices, with little attention to efficiency and cost control.[9,10,11] Strategic vision which is oriented toward efficiency, cost control and entire population is needed to solve managerial and sustainability snags.
Figure 1.
Vicious resource Circle before 1990
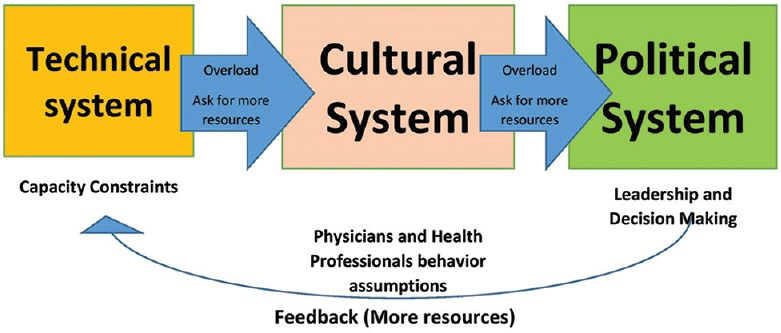
Clinical processes, professional and cultural independence of the physicians was considered historically as red line, the managers do not dare to infringe.[12,13] Some control has been exercised in market-based systems mostly through some contractual obligations. However, trials of control have been attempted thorough input-output assessments in tax-based systems[14] [Figure 2]. Deep planning and extensive allocation of inputs were the main methods to control and manage healthcare disbursement, especially in 1980s. Input control might be restriction of bed numbers, purchasing and staffing. The same thing to output control which was introduced in 1990s through control of diagnostic investigations, prescriptions and medical visits. At the end of 1990s, control of outcome measures was applied via coverage of requirements of health care, morbidity and mortality measures.
Figure 2.
Focus of control change, in diagnosis related groups
The healthcare systems addressed only the crust of problems related to methods and contents of care delivery processes. Early in 1990s, the implementation of tools, approaches and techniques related to clinical pathways, process reengineering and lean management, seemed to be inconsistent and restricted.[15,16] Moreover, in the late 1990s, methods and tools related to clinical governance and auditing began to prosper and thrive.[17] The effect of managers, either business or general managers, on clinical processes was completely restricted for many years.
Through the regenerated concentration on controlling inputs, the managers and decision makers try to scavenge hegemony over the price of health systems, because of the neoteric financial crisis.[18,19] Restrictions are being decreed on health systems by limitation of buying policies, testing new technology and staffing or replacement of workers. Thrusting and rates for clinical services are being re-deliberated and decreased. Nearly with no exemption, prevailing disbursement means in the short-term, prevailing inputs. The repeated concentration on input and resource thoroughness has sundry prejudice and bad sequel. First of all, policies of cost reduction do not frankly favors constitutional interference in the industrious styles embraced by persons engaged and managerial staff at health care organizations. One more, policies of input control and cost reduction, might evenly affect good and bad performing institutes in the same healthcare framework. Furthermore, insomuch as cuts are executed horizontally, internationality is ultimately deteriorated. Unless we try to change manner of supply of healthcare services, cuts can mostly influence accessibility, quality and equity.
In the early seventies, defy of sustainability with medical care systems were handled by using the idea of allowing each person to have only a fixed amount of (a particular commodity), as one of the best solutions to give the patients accessibility, and equity to care with high quality within an economically reasonable structure. Allowing each person to have only a fixed amount of (a particular commodity), integrated a chain of different points of view that were prepared to boost 1) Priority regulation in making decisions[20] 2) Remodeled care delivery process out of a better comprehension of and more suitable work on the “black box” of medical practice.[21] It is no longer tolerable, to use inappropriate drugs, therapies, diagnostics, vindicatory medicine, spurious variability, herbal treatments, and wasting of resources. Critical decisions such as those related to use of costly bio drugs, medical devices, prostheses for patients with bad prognosis, predicted bad outcomes and restricted life expectancy are focus of attention of social and public insurance. However, allowing each person to have only a fixed amount of (a particular commodity), accomplished relatively little considerable lowering in total supplies, as there was a lack of assent about services to be neglected and modicum political volition to face challenging decisions.
Allowing each person to have only a fixed amount of (a particular commodity), must be encouraged with concentration on professional framework to ameliorate the participation of physicians in management of these challenges.[22] Leadership models may be beneficial in this situation. Actually, according to neoteric studies and discussions, leadership can reinforce the value created by health systems, strategies and professionals.[23,24,25] Nearly, all health systems are actively keep track of dispensation and stewardship of their health institutes.[18] What kind of leadership, and which leaders, however, should be applied? How can leadership conciliated with ethics in critical decisions? Since 5 years, motivating, but restricted, testimony has increasingly expounded that leadership does matter.[19] The next section demonstrates some of the most neoteric studies and influx of researches that handle leadership and performance of health organization, which yet affects the continuity and internationality of health systems. Nevertheless, we also debate that we are improbable to proceed research in this area until we manage the validity of our data and methods and scrutinize the barriers to cooperative multidisciplinary researches with a shared converge. In the last section, we offered, developed and discussed a roadmap for such future researches.
Review of Literature
Does management and leadership affect health systems?
In recent decades, both researchers and physicians have regenerated their solicitude in the influence of leadership and management on health system and organizational performance. We used PubMed, Emerald, and Science Direct as English references to do this systematic review. Management pursuit, health care services, health care organizations, leadership effect, quality, and health care performance, were all key words which were extracted to coincide with survey items. With no time limitations, the review included both notional and experimental researches. Furthermore, we also incorporated the pertinent reports by global research organizations as London School of Economics. We summed up a scientific working research that comprises the methods, conclusion and results.[26] We chose 27 papers and researches on the principle of the research guidelines and their relation to the subject.
In the late nineties, some trends of research began to improve, and that was demonstrated by review results. However, more neoteric experimental reports show increase in the attention to assess the effect of leadership on clinical performance and other aspects of healthcare system. Perhaps, this change is related to the fact that the leaders in healthcare confront maladjusted or discordant external expectations of the stakeholders, most of them result from relatively powerful but broken organizational forces and from growing powerful market strength. Whenever the situation is complicated, the organizations will struggle more towards the “leadership and management” to puzzle out a solution.[23]
Does leadership and management matter? What style and what kind of leadership should be recommended? How does it matter? All these questions have now become a source of concern. Though, assessment of performance is still dialectical: some writers[20] have proposed that management of performance depending on targets could lead to a range of non-planned and maladjusted outcomes, remarkably the deformation of the clinical priorities, betting, threatening and bullying of the employees, and absence of confidence among people and staff.
In spite of the fact that we are obliged to improve the way of setting performance targets for systems of healthcare, we also must decide if good leadership pursuits can have a favorable effect on performance. We can divide the studies of the effect of leadership on performance in healthcare into four groups, broadly: 1) researches that study the effect of leadership activities on performance, that is, the effect of planning, regulation, coordination, management, and commanding; 2) studies that concentrate on the effect of leaders' merits on performance, comprising their backgrounds, professional history, and exploitation in training; 3) projects that describe the effect of the incorporation of staff in management process on production; and 4) researches that dissect the effect of organizational culture and leadership styles on production.
The effect of leadership activities on performance
Previously, in the ancient researches, no relations had been found between performance and management[21]: yet, in the same research,[21] there were some rebuttals of a quadruple relationships between operating superfluous created, leadership and performance. They used waiting time criterion for inpatient admission given in patient's file, during 3 months duration. In spite of the fact that, neoteric studies have called attention to relations between leadership and performance,[26,27,28] Bloom conducted a research on 1100 hospitals and found that leadership in cardiology and orthopedic surgery departments showed a strong interconnection with performance.
Improved leadership activities has shown a significant impact on decrease of morbidity and mortality rates, as demonstrated by proof. Also good leadership has shown good fiscal actions through increase of income per bed. Operational management also included in the same study flow, as it is practically used in healthcare organizations.[22]
The concept of efficiency together with quality and productivity, in terms of what's called lean management, has been introduced from 1998-2008. Review of these practices in different institutes, has been defined in more than 33 studies that identified cases of lean transformation and record positive results. Moreover, there was a significant positive relation reported by different studies entailed the linkage between leadership and organizational performance. Nevertheless, leadership is not amounting to management: some studies reported that management include; designing, budgeting, regulation, staffing, and commanding, and separated them from solving problems, and leadership practices that find directions, motivating people and align them. Furthermore, leaders can participate in a range of different managerial practices that impact performance of individuals and teams.[23] A survey was conducted, specified 60 experimental articles in which the statement of leadership in healthcare is correlated with satisfaction of individuals and teams. Also, an article that identified the association between leadership and employee retention as well as performance[24] was carried out using quantitative methods to investigate the relationship between organizational performance and leadership behaviors, it was longitudinal experimental study. Leadership which allows engagement of individuals with each other's is considered as a significant indicator of organizational performance. Furthermore, the neoteric King's Fund report, stems from assessment of the testimony on the theme, indicates that the NHS demands strong management and leadership “from the hospital ward to the hospital board”.[25] And specified that the most important point of weakness and threat of the NHS over a long period of time has been the absence of participation of physicians in management, particularly, when the decisions were related to “how will we spend the budget?”
The effect of leadership characteristics on organizational performance
The second classification of articles handled the association between the features of managers (for instance; training history, background and career), and organizational performance. These articles seeks to defend the progressively peppy role for clinicians being managers and leaders. Researchers have found that the best management practices is exhibited by managers who are clinically qualified.[27] The best hospitals in the United States are led by doctors, who occupy chief executive officers position. World Report league tables and United States news stated that 16 out of 21 best ranked hospitals were drove by clinicians.[29] In the Italian NHS, high levels of managerial achievement could be achieved by leaders who have clinical background, and have heaped up experience in huge number of healthcare organizations.[30]
The effect of the participation of staff in leadership on performance
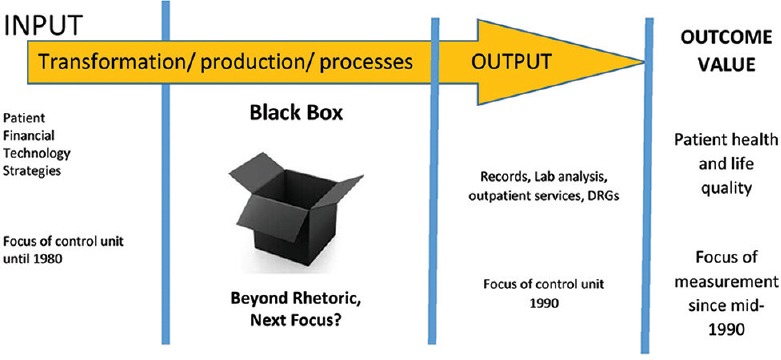
The third group of researches stem from the concept of participation of clinicians in the leadership process, and its benefit. Some researchers focus on methods to measure and develop this participation to improve organizational performance. This group includes researches that focus on how “clinical-leaders” are able to inspire their colleagues more efficiently than non-medical leaders, particularly in clinical practices. However, they strive to win over their colleagues to assure the value of leadership in performance improvement.[31] Many researches have also considered the risks of this mixing process and the resistance that may result from it, in which the clinician become the manager of the hospital.[26] Others, nevertheless, debate that the participation of doctors in management is important and makes a positive effect on performance.[11,13] More precisely, some articles entail the relation between leader physicians and high performance in best practice hospitals.[32] Furthermore, neoteric proof proposes a clear relation between medical participation and measures of improved performance in England.[33] Based on the concept of medical participation “as energetic and favorable engagement of clinicians within their ordinary working activities to preserve, and boost the organizational performance which itself acknowledge this pledge in reinforcing and heartening best quality of care”.[34] This definition developed a credible sincere indicator of medical participation (Medical Engagement Scale). The scholars gathered data from approximately 4000 clinicians across 40 secondary care funds and found that mortality rates has been improved significantly with high levels of doctors participation. Also they found, lowering in adverse events, conservation of service economy, fiscal status, quality of care, and the accomplishment of goals in all services. [Figure 3] presents the liaison between clinical participation and standardized hospital mortality rates.
Figure 3.
Effect of Medical Participation on Hospital Standardized Mortality Rates
A rapprochement of the ten funds that expound the highest levels of clinical participation and those that elucidate the lowest grades of performance, based on ratings of Care Quality Commission. This comparison demonstrated pure and considerable differences in total quality, fiscal management, national priorities, essence standards, and implementation of commitments, Figure 4. This outcome suggests that there is a serene and harmonious link between clinical participation and performance, supporting that if clinicians become more engaged in service renewal and change, outputs and outcomes will get better. Based on these significant consistent correlations among these results, although we could not implicate any eventual causal relationship between those two variables. It is intractable, however, to understand how revolutionary positive changes in service distribution could be achieved successfully by non-participated, non-cooperative and indignant medical staff. Moreover, striving around concepts of; focused care, clinical management, and service lines in health organizations, push the leaders with good management skills to run the new models of organizational performance improvement efficiently, as suggested by several studies. Substantially, this will contribute to maximal clinical and fiscal performance.[35] Finally, some studies affirm that loss of proficient managers due to cut cost can endanger the performance.
Figure 4.
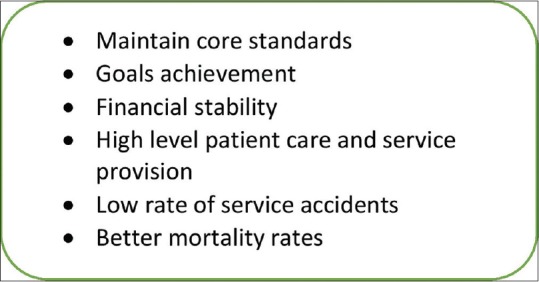
Effect of Clinical Participation in Management
The effect of leadership styles and organizational culture on performance
The fourth group of researches demonstrated that an entrusted relationship subsists between organizational culture and performance together with leadership styles. Leadership styles and organizational culture varied across healthcare organizations and can be linked with indicators of performance and organizational merits. An assessment of cultural quality or features of hospitals with high and low performance demonstrates that the best hospitals differ from other low performing hospitals, in terms of their engagement in leadership, which is not charismatic, - but transactional - and their concept of management, which is based on multidisciplinary management of performance, clear vision, and using of managerial practices and tools, such as financing, business and strategic planning.[28] The scholars, however, notify against the hazard of dysfunction related to cultural changes towards the features of hospitals with high performance, such as excessive affirmation on goals and tunnel vision.
The difference between hospitals with high performance and those with low performance regarding mortality rates associated with acute myocardial infarctions, was demonstrated by neoteric study, which revealed that they differ ultimately in the scope of organizational goals and values, senior leadership engagement, frequent presence of staff, presence of experts in cardiac care, assortment and communication among teams. Medication reconciliation, rapid response teams, and clinical practice guidelines; were all protocols for myocardial infarction care. They were used in all organizations, however these traits could not consistently differentiate hospitals with high performance form others with low performance.[36]
Finally, those researches are correlated with the study that designed to show that the absolute presence of leadership practices does not emphasize better performance if it is not combined with educational and training efforts that reinforce clinician participation in the process of management.[10,29] The main goal of those four data sources of our literature is that leadership does have effects on organizational performance, but this effect in most of cases is mediated by statement and context.
Limitations of literature and obstacles faced by extra research
This research demonstrates the relationship between leadership and organizational performance. It uncover the existence of a testimony supporting a favorable effect of leadership on performance. Several restrictions of this literature, yet, should be considered. First, the testimony is increasing but remains non decisive. More precisely, some restrictions of this research are; qualitative descriptive rather than experimental.[10,25,29] Misleading methods used to score leadership practices, particularly in quantitative researches.[37] Lack of demonstration of causal relations among dimensions of management and performance.[38]
Furthermore, many researches have shown some of the hazards that future experimental researches will face. First, indicators used to assess leadership practices may be caused by the authenticated presence of formal practices, tools and roles of management. This process may be deceptive because physicians may foster formal administrative roles as part of “tutelary” strategy. In addition, physician choose to be appointed in an administrative roles as a head of department in a trial to preserve their professional autonomy, position and power. But they do not practice the administrative tasks anticipated from this role.[39] However, the indicators used to assess leadership practices should be based on knowledge of genuine engagement in, and adherence to leadership responsibilities. Also, causal relationship could not be addressed in this literature. For example, hospitals face intense external threats that can alter the financial performance of the organization, especially, the consensus building with politically designed performance.
Conclusion
As referred to in the introduction, cut cost without consideration of the outcomes accomplished can be risky and self-destroying, leading to spurious “savings” and restricted care with limited accessibility. Therefore, the future internationality and continuity of healthcare organizations will depend on improvement of the concept of value, which is known to be outcome in respect to cost.[40] The induction of value is significantly related to the ability of controlling of the “black box” of the process of healthcare. Thus, more concern to outcome indicators is needed, particularly when we look to its special multidimensional condition. Furthermore, costs should be assessed and controlled with reference to care-cycle-total-costs, interrelated with patient clinical situation. It is inadequate to think only about cost of single service. Obviously, the management of value will push us to solve the problem of artificial variation among staff in handling and use of therapies, guidelines, pathways, timing, resources, and diagnostics[41] also dealing with vindicatory medicine[42] and decisions serving concepts of cost-benefit. The quality of micromanagement should be considered strictly in hospitals and wards, as well as the building design, and administration.
For the last twenty years, nearly all health organizations have constantly rearranged their governance as well as their structure, but all these efforts will be in vain unless they are associated with evolution of leadership capabilities.[43] We are required to know how to increase exploitation in the development of leadership capabilities in health organizations. All collected proofs till now, in spite of being non decisive and restricted in some aspects, pointed to leadership. Leadership does matter from different aspects, performance is interrelated with leadership practices, leadership styles, and cultural traits that are associated with strategies and values. Moreover, there are many evidences that shows that medical organizations managed my clinicians have high performance and excellence over those managed by non-clinicians.[44] That means that clinicians as managers lead better than other managers who have non-medical backgrounds. This difference occur because clinicians have different perspectives other than anyone else. Such order may be more effective because doctors have more knowledge and sensitivity particularly in decision making.[28,43]
According to this research and shown limitations, future researches should be considered, regarding strength of association, trial to push the research to be experimental to understand the relationships between leadership roles, practices and performance, clear definition of methods and indicators, the real proportional value of particular aspects of leadership, the real motivator of professional towards leadership practices, appropriate role of clinical mangers, specific medical background that dominate, transitional leadership, and which clinical background promotes and facilitates this change to improve the performance.
Also, our research still incomplete because it is deprived of contextual analysis. Cooperative multidimensional researches that concerned with the context in the analysis is important to determine whether leadership issues can be separated from the organizational preferences made by health institutes. Furthermore, particularly within global comparative researches, authors require to foster a common frame for investigation and analysis of performance drivers. Specifically, this stream of studies should answer those research questions. Is the espousal of leadership practices specified by which of these corresponding factors? Compulsory isomorphism resulting from political impacts, coerce exerted by undependable organizations upon dependable ones, mimicry and isomorphism that force organization to change themselves to compete with other organizations. Is there a detaching phenomenon officially for which institutes foster leadership models but not really implement? Is it enhanced by financial or non-financial inducement? For example, how necessary are, system management, rehabilitation and theoretical models, relationships among stakeholders? The future research should determine to what extent the experience is specific to its individual context? How it can be issued? For example; the United Kingdom, France, Germany, Italy, Switzerland, and Spain have different cultural features, even inside each country there are diversity in cultures. Thus, authors have to delineate the evolution of clinical participation in leadership in reference to the recent cultural context.
At last, we should reconcile the researches on the effects of management, culture and leadership. According to this scope, there is a considerable chance to combine theory with practice. At least, scholars who focuses on this topic and staff need to design more efficiently on each other's work, even if this cooperation is a big challenge, because each group could benefit from each other. Such mutual efforts could lead to regenerated contributions by significant research to health systems confronting a big challenge.
Coming researches in this topic could be very beneficial to understand “if” and “how” leadership could be the cornerstone for following the continuity of healthcare systems that strive to preserve and improve the real global health coverage.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Special thanks of gratitude to my colleague Dr. Ahmed Elmalky who gave help in review process.
References
- 1.Arisha A, Rashwan W. Modeling of healthcare systems: Past, current and future trends. 2016 Winter Simulation Conference (WSC) 2016;76:911–22. doi: 10.1109/wsc. 2016.7822203. [Google Scholar]
- 2.Alimo-Metcalfe B, Alban-Metcalfe J, Bradley M, Mariathasan J, Samele C. The impact of engaging leadership on performance, attitudes to work and wellbeing at work. J Health Organization Manage. 2008;22:586–98. doi: 10.1108/14777260810916560. [DOI] [PubMed] [Google Scholar]
- 3.Bode I. Social citizenship in post-liberal Britain and post-corporatist Germany: Curtailed, fragmented, streamlined, but still on the agenda Social Policy Review 20. Analysis and Debate in Social Policy. 2008:191–209. doi: 101332/policy press/97818474207630030011. [Google Scholar]
- 4.Boyes S. A strategy for engaging primary and secondary care doctors in medical leadership. Medical Leadership. 2008:86–94. doi: 104324/9781315440880-11. [Google Scholar]
- 5.Brown L. Innovation in public sector services: Entrepreneurship, creativity and management. Public Manage Rev. 2009;11:393–4. [Google Scholar]
- 6.Cabral A, Oram C, Allum S. Developing nursing leadership talent-views from the NHS nursing leadership for South-East England. J Nurs Manage. 2018;27:75–83. doi: 10.1111/jonm.12650. [DOI] [PubMed] [Google Scholar]
- 7.Chen BK. Defensive medicine under enterprise insurance: Do physicians practice defensive medicine, and can enterprise insurance mitigate its effect. SSRN Electronic J. 2010 doi: 102139/ssrn 1640955. [Google Scholar]
- 8.Clark J. Clinical leadership and engagement: No longer an optional extra Management and Leadership –. A Guide for Clinical Professionals. 2015:19–32. doi: 101007/978-3-319-11526-9_2. [Google Scholar]
- 9.Cohen A. The dark triad and leadership Counterproductive Work Behav. 2018:156–84. doi: 104324/9781315454818-8. [Google Scholar]
- 10.Correia T, Dussault G, Pontes C. The impact of the financial crisis on human resources for health policies in three Southern-Europe countries. Health Policy. 2015;119:1600–5. doi: 10.1016/j.healthpol.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 11.Lega F, Calciolari S. Coevolution of patients and hospitals: How changing epidemiology and technological advances create challenges and drive organizational innovation. J Healthc Manag. 2012;57:17–34. [PubMed] [Google Scholar]
- 12.Coutts J. Engaging physicians to improve quality. Healthc Q. 2010;13:23–5. doi: 10.12927/hcq.2010.21809. [DOI] [PubMed] [Google Scholar]
- 13.Craighead P, Anderson R, Sargent R. Developing leadership within an academic medical department in Canada: A road map for increasing leadership span. Healthc Q. 2011;14:80–4. doi: 10.12927/hcq.2011.22494. [DOI] [PubMed] [Google Scholar]
- 14.Ferrè F, Cuccurullo C, Lega F. The challenge and the future of health care turnaround plans: Evidence from the Italian experience. Health Policy. 2012;106:3–9. doi: 10.1016/j.healthpol.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 15.Fleming H. Improving quality and lowering cost through community care teams. J Healthc Manag. 2018;63:242–50. doi: 10.1097/JHM-D-18-00078. [DOI] [PubMed] [Google Scholar]
- 16.Fox DM. Designing Care: Aligning the nature and management of health care. JAMA. 2010;303:885. [Google Scholar]
- 17.Garpenby P, Nedlund A. Political strategies in difficult times – The “Backstage” experience of Swedish politicians on formal priority setting in healthcare. Soc Sci Med. 2016;163:63–70. doi: 10.1016/j.socscimed.2016.06.046. [DOI] [PubMed] [Google Scholar]
- 18.Goodall AH. Physician-leaders and hospital performance: Is there an association? Soc Sci Med. 2011;73:535–9. doi: 10.1016/j.socscimed.2011.06.025. [DOI] [PubMed] [Google Scholar]
- 19.Goodman JC. Priceless: Curing the Healthcare Crisis. Oakland, CA: Independent Institute; 2012. [Google Scholar]
- 20.Groves KS. Examining the impact of succession management practices on organizational performance. Health Care Manage Rev. 2017:1. doi: 10.1097/HMR.0000000000000176. doi: 101097/Hmr 0000000000000176. [DOI] [PubMed] [Google Scholar]
- 21.Gunderman RB. Why leadership matters Leadership in Healthcare. 2008:1–24. doi: 101007/978-1-84800-943-1_1. [Google Scholar]
- 22.Herrman H, Freidin J, Brownie S. Leadership and professionalism Professionalism in Mental Healthcare. 2013 Doi: 101017/Cbo 9780511910074017. [Google Scholar]
- 23.Kane L. Understanding health systems: From Sierra Leone To WONCA. London J Primary Care. 2016;8:35–6. doi: 10.1080/17571472.2016.1173428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kezar A. Change Implementation How Colleges Change. 2018:193–211. doi: 104324/9781315121178-12. [Google Scholar]
- 25.Kirkpatrick I, Jespersen PK, Dent M, Neogy I. Medicine and management in a comparative perspective: The case of Denmark and England. Sociol Health Illn. 2009;31:642–58. doi: 10.1111/j.1467-9566.2009.01157.x. [DOI] [PubMed] [Google Scholar]
- 26.Moreno E, Girón F, Vázquez-Polo F, Negrín M. Optimal healthcare decisions: The importance of the covariates in cost–effectiveness analysis. Eur J Oper Res. 2012;218:512–22. [Google Scholar]
- 27.Kutzin J. Health Financing For Universal Coverage and Health System Performance: Concepts and Implications for Policy. 2013. Retrieved From https://www Ncbi Nlm Nih Gov/Pmc/Articles/PMC3738310/ [DOI] [PMC free article] [PubMed]
- 28.Schnurr S. The 'Other' side of leadership discourse: Humour and the performance of relational leadership activities Leadership. Discourse Work. 2009:42–60. doi: 101057/9780230594692_3. [Google Scholar]
- 29.Lega F. Lights and shades in the managerialization of the Italian National Health Service. Health Serv Manage Res. 2008;21:248–61. doi: 10.1258/hsmr.2008.008007. [DOI] [PubMed] [Google Scholar]
- 30.Mascia D, Piconi I. Career histories and managerial performance of health care chief executive officers. Health Care Manage Rev. 2013;38:71–80. doi: 10.1097/HMR.0b013e31823dc85b. [DOI] [PubMed] [Google Scholar]
- 31.Mauck S. What distinguishes top-performing hospitals in acute myocardial infarction mortality rates? A qualitative study. J Emerg Med. 2011;41:109. doi: 10.7326/0003-4819-154-6-201103150-00003. doi: 10.1016/J. Jemermed. 2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nicol A. Improving clinical leadership and management in the NHS. J Healthc Leadership. 2012:59. doi: 102147/JhlS28298. [Google Scholar]
- 33.Opp K. Collective identity, rationality and collective political action. Rationality Society. 2012;24:73–105. [Google Scholar]
- 34.Papanicolas I, Smith PC. Assessing health systems Health Services Research Health Care Systems and Policies. 2018:1–13. doi: 101007/978-1-4614-6419-8_2-1. [Google Scholar]
- 35.Schimmel N. Presidential Healthcare Reform Rhetoric. 2016 doi: 101007/978-3-319-32960-4. [Google Scholar]
- 36.Spurgeon P, Mazelan PM, Barwell F. Medical engagement: A Crucial Underpinning to Organizational Performance. Health Services Manage Res. 2011;24:114–20. doi: 10.1258/hsmr.2011.011006. [DOI] [PubMed] [Google Scholar]
- 37.Strech D, Persad G, Marckmann G, Danis M. Are physicians willing to ration health care. Conflicting findings in a systematic review of survey research? Health Policy. 2009;90:113–24. doi: 10.1016/j.healthpol.2008.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Szykula SA, Jackson DF. Managed mental health care in large jails: Empirical outcomes on cost and quality. J Correct Health Care. 2005;11:223–40. [Google Scholar]
- 39.Vlastarakos PV, Nikolopoulos TP. The interdisciplinary model of hospital administration: Do health professionals and managers look at it in the same way? Eur J Public Health. 2007;18:71–6. doi: 10.1093/eurpub/ckm042. [DOI] [PubMed] [Google Scholar]
- 40.Wattis J. Practical Management and Leadership for Doctors. 2018 doi: 101201/9781351017398. [Google Scholar]
- 41.Whittington JL, Meskelis S, Asare E, Beldona S. Enhancing engagement through effective performance management Enhancing Employee Engagement. 2017:81–90. doi: 101007/978-3-319-54732-9_8. [Google Scholar]
- 42.Wickramasinghe N. Lean principles for healthcare Lean Thinking for Healthcare. 2013:3–11. doi: 101007/978-1-4614-8036-5_1. [Google Scholar]
- 43.Witman Y, Smid GA, Meurs PL, Willems DL. Doctor in the lead: Balancing between two worlds. Organization. 2010;18:477–95. [Google Scholar]
- 44.Yeh I, Chang C, Ueng J, Ramaswamy V. Reducing risk through governance Operations Serv Manage. 2018:1769–80. Doi: 104018/978-1-5225-3909-4 Ch082. [Google Scholar]