Abstract
Objective:
To investigate the effect of maxillary single and multiple rooted teeth on the success rate of buccal infiltration anesthesia.
Subjects and Methods:
This clinical study was performed by dividing the participants into three groups. Group one included 30 patients with upper anterior teeth, group two 23 patients with upper premolars teeth and group three 39 patients with upper molars for extraction. Onset time of anesthtic action was evaluted by using electronic pulp tester. Pulp testing assessments were carried out immediately before the injection and at the intervals of 2 mins following the injection until the anesthetic success obtains.
Results:
Seventy-nine patients in this study secured anesthetic success within study duration time (10 min). However, there were 13 patients with dental anesthesia failures (3 patients with single rooted teeth and 10 patients with multiple rooted teeth). There were no significant differences in the mean onset time of pulpal anesthesia between the anterior, middle and posterior teeth (P value = 0.449). Clinically, patients with single rooted teeth reported faster dental anesthesia and earlier teeth extraction than patients with multiple rooted teeth.
Conclusion:
This study showed that the single rooted teeth have faster pulpal anesthesia and early extraction than teeth with multiple roots but not statistically significant. Administration of extra local anesthetic cartridge or using intraseptal injection technique can be a solution to overcome the failure of anesthesia in the maxillary posterior teeth.
Keywords: Anesthesia, dental extraction, speed of action, tooth pattern
Introduction
Failure of dental anesthesia during treatment sessions can cause a traumatic experience for both the patient and dentist.[1] Consequently, patient will avoid intentionally forthcoming dental appointments and deterioration in the oral hygiene might occur.[2] Increase in the number of dental anesthesia failures will make the dentist feels incompetent and regretting the time, he spent since joining the dentistry.[2,3] By analyzing the causes of dental anesthetic failures and suggesting the appropriate solutions, paranoid dentists, and anxious patients will be in a good mood throughout the treatment.[3] Prilocaine is slightly less potent and considerably less toxic than lidocaine as a local anesthetic agent.[4] Prilocaine produces less tissue vasodilation than lidocaine and can be used reliably in plain solution form for short-duration procedures.[5,6] Lidocaine has a dissociation constant (pKa) of 7.7, highly protein-bound 77%, relative potency of 4 and relative toxicity of 2.[7] However, prilocaine has PKa of 7.7 and protein binding of 55%, relative potency of 4 and relative toxicity of 1.5.[6,7] In light of these facts prilocaine and lidocaine has similarity values of pKa, which are closer to physiological pH (7.4). This means equal numbers of uncharged base local anesthetic molecules are present to diffuse through the nerve sheath and as a consequently a comparable onset time of action will be achieved.[7,8,9,10,11,12] In the literature, there were a lack of the knowledge regarding the relationship between the failure of local anesthesia and the morphology of the extracted teeth.[13,14,15] No study was carried out to compare the speed of onset time of local anesthesia between single and multiple rooted teeth.[9,10] Failure of local anesthesia injections in upper and lower jaws were studied intensively.[16,17,18] The anesthetic failure can be due to pulpitis that results in hyperalgesia in enclosed pulp tissues.[19] Inflamed tissues may alter the nerves' resting membrane potentials and decrease excitability thresholds.[20] Therefore, routine local anesthetic techniques may not prevent nerve transmission adequately because of the lowered excitability thresholds.[19,20,21] Inflamed tissues may alter the nerves' resting membrane potentials and decrease excitability thresholds. Therefore, routine local anesthetic techniques may not prevent nerve transmission adequately because of the lowered excitability thresholds.[21,22] Therefore, the multiple rooted teeth with inflammation has greater volume of excitability than single rooted teeth as a consequence they need more quantity of LA to guarantee the pulpal anesthesia.[23]
The aim of this study was to investigate the effect of maxillary single and multiple rooted teeth on the speed of action and success rate of 2% lidocaine and 3% prilocaine buccal infiltrations. Null hypothesis: There is no differences in anesthesia onset time between single and multiple rooted teeth when either 2% lidocaine or 3% prilocaine used for upper dental extraction.
Subjects and Methods
This clinical trial was approved on December 11, 2016 and the ethical approval was obtained from Taibah Dental College Research Ethics Board which included 5 members and protocol approval number was issued (IRB: 00010037). Patients who attended the Oral Surgery Unit in Taibah Dental College for extraction and removal of tooth/teeth under local anesthesia were included in the study. By utilizing convenient sampling pattern, 96 patients were distributed to two groups. This study included male patient's age from 16 to 70 years old, planned for extraction of one upper tooth and have the ability to cooperate and coordinate with the requirements of the protocol. Patients with mental issues, hypersensitvity to local anesthesia, or avoidable surgical/multiple teeth extraction were excluded.
Before the study, a researcher or analyst allocated the sequence of patient identity numbers to either the lidocaine or the prilocaine group. Placard with 3% prilocaine or 2% lidocaine were placed in non-transparent envelopes, sealed, and signed by a secretary who was not associated with the study. These envelopes had been numbered consecutively outside with the patient identity number and were entered to the record of the patient's dental hospital treatment record. In the dental clinic, on dental chair, once the patient signed the consent the appended envelope was opened by the dental specialist. If the patient was in lidocaine or prilocaine group, the local anesthetic needle was inserted at the profundity of the sulcus adjacent to the apical of the tooth planned for extraction and advanced 4-7 mm until the a point that a sufficient bony contact was accomplished, 1.4 ml lidocaine 2% with epinephrine 1:100,000 or prilocaine 3% felypressin (0.03 I.U. per ml) was administered gradually over 40 s after aspiration plus a 0.4 ml mepivacaine infiltration in the hard palate 5 mm away from gingival margin for more than 20 s. No anesthetic solution was deposited as the needle is advanced to the target i.e., objective site in either routine.
The adequacy of pulp anesthesia was determined impartially by electronic pulp testing. This will be performed with an Analytic Technology Pulp Tester (Analytic Technology Redmond, Washington, USA). Testing performed at a rate of 2 min to approve the pulp tester readings, a control-unanesthetized tooth on the contra-lateral side of the upper jaw was also tested at base line i.e., benchmark and at intervals in the study.
Anesthetic success is considered when a tooth is stimulated twice by the electronic pulp tester to the maximum stimulation (64 reading) with no positive sensation. The efficacy of pulp anesthesia was assessed for maxillary upper tooth subjected for extraction or its adjacent teeth (if intended tooth for extraction was not vital), before injection (baseline or benchmark) and at intervals of 2 minutes until 10 minutes. At any point of trial (10 minutes), the anesthetized tooth becomes unresponsive for maximal pulp stimulation (64 reading), the extraction was performed. Following 10 minutes of injection of local anesthesia, if the anesthetized tooth was still positively responsive to electrical pulp tester, the second cartridge of LA was given.
BI regimen was administered. The dental surgeon gave all injections. Standard aspirating dental cartridge syringes (USA: ATI) fitted with 27-gauge, 21 mm short needles were utilized for buccal and palatal infiltrations.
Power calculation
Totally, 96 patients were recruited in this study based on a study by Gazal et al.[24] It was found that a sample size of 90 would have 90% power to spot the difference in the onset time of action of articaine and mepivacaine when used for upper teeth extractions. Data Information were entered and analyzed in statistical software package SPSS (SPSS 20, SPSS, Inc., Chicago, IL, USA).
Results
Ninety-six patients were participated in this study and four patients were excluded due to the phobia of local anesthetic injections.
Anesthetic success
In this study there were 30 patients had anterior teeth extraction, 23 had upper premolars extraction and 39 had molars extraction [Table 1]. 79 patients in this study had successful upper teeth anesthesia and extraction within the study duration time of 10 minutes. Failure of anesthesia was recorded in 13 patients (3 patients in anterior teeth group, 4 patients in middle teeth group, and 6 patients in posterior teeth group) and extra injections were administrated for completing the tooth removal procedures. Crosstabs analysis was carried out to obtain the numbers and percentages of patients in upper anterior, middle and posterior teeth extraction groups. Figure 1 and Table 2 summarizes the overall outcome of the anesthetic success for the pulp of upper teeth of the 92 patients who participated in the study. In this table, the anesthetic success represents “no response to maximal electronic pulp stimulation (64 reading)”, and the anesthetic failure represents “positive response to electronic pulp stimulation”. 10 out of 13 patients with failure anesthesia was found in middle and posterior teeth groups. Teeth with multiple roots might need more local anesthetic solution than single rooted teeth. By application Person's Chi-square test (x2), there were no significant differences in the number of the episodes of the anesthetic success for patients in anterior, middle and posterior teeth groups at time intervals (P value = 0.437).
Table 1.
Distribution of patients according to the tooth extraction morphology in both the lidocaine and prilocaine groups
| Tooth extraction group | Treatment group | Total | |
|---|---|---|---|
| Lidocaine regimen | Prilocaine regimen | ||
| Anterior teeth group | 14 | 16 | 30 |
| Middle teeth group | 15 | 8 | 23 |
| Posterior teeth group | 17 | 22 | 39 |
| Total | 46 | 46 | 92 |
Figure 1.
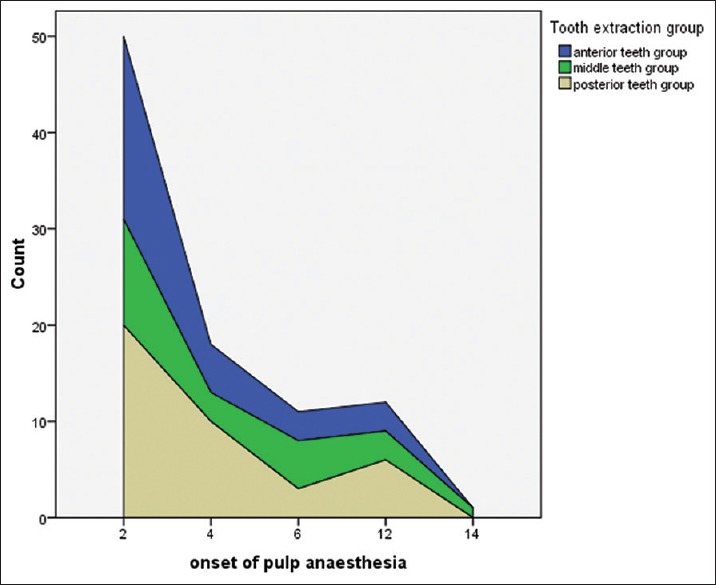
Represents the number of anterior, middle and posterior teeth along with the anesthesia onset time of action after the administration of local anesthetic agents
Table 2.
Number of the anterior, middle and posterior teeth with anesthetic successes at intervals of 2 minutes in 92 adult patients
| Anaesthetic success at time interval | 2 min | 4 min | 6 min | 8 min | 10 min | >10 min | Total 92 |
|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| anterior teeth group | 19 (63) | 5 (17) | 3 (10) | 0 (0) | 0 (0) | 3 (10) | 30 (100) |
| middle teeth group | 11 (48) | 3 (13) | 5 (22) | 0 (0) | 0 (0) | 4 (17) | 23 (100) |
| posterior teeth group | 20 (51) | 10 (26) | 3 (8) | 0 (0) | 0 (0) | 6 (15) | 39 (100) |
| Person’s Chi-square test (x2) | 7.966 | ||||||
| P | 0.437 | ||||||
Anesthesia onset time and extraction
There were no significant differences between the means of anesthesia onset time and extraction for patients in prilocaine and lidocaine groups (P-value >0.05). The range for anesthesia onset time and extraction of upper teeth in this study was from 2 to 14 minutes. Table 3 shows the mean onset time of anesthesia and extraction for patients in anterior, middle and posterior teeth extraction groups. Clinically anesthesia onset time was faster in anterior upper teeth than upper middle and posterior teeth (means: 3.73, 4.96, and 4.36 min, SD: 3.10, 3.90, and 3.52 min). The application of ANOVA T- test revealed that there were no significant differences in the mean onset time of pulpal anesthesia and extraction between the anterior, middle and posterior teeth extraction groups (P-value = 0.449) [Table 3]. However, patients in the anterior extraction group recorded faster pulpal anesthesia and earlier teeth extraction than patients in the middle and posterior extraction groups but these findings were statistically non-significant.
Table 3.
Comparisons between mean onset time of anaesthesia for patients in anterior, middle and posterior teeth groups
| Groups | Number of patients n | Mean (SD) (min) | ANOVAt-test (df=89) | P | |
|---|---|---|---|---|---|
| Anterior teeth | 30 | 3.73 (3.10) | |||
| Anesthesia onset time | Middle teeth | 23 | 4.96 (3.90) | 0.808 | 0.449 |
| Posterior teeth | 39 | 4.36 (3.52) | |||
Bold value is not statistically significant because P value > 0.05
Discussion
The findings of this study showed that the failure rate of anesthesia was higher in the patients who have posterior teeth for extraction than those with anterior ones. Single rooted teeth achieved clinically fast pulpal anesthesia and early teeth extraction compared with the teeth of multiple roots.
There are number of factors that contribute to local anesthetic failure in dental practice.[9] These factors are related to either the patient or the operator. Patient-dependent factors are anatomical, pathological and psychological.[9,10] These subjective factors were not the underlying cause for anesthetic failure in our study. Patients with pathological lesions and psychological problems were excluded from the beginning of the study. On the other hand, operator dependent factors are years of experience and the correct choice of technique and solution.[18] The dental surgeon (GG) who administrated all the infiltrative injections of LA in this study was well trained with 25 years of experience.[2] The buccal infiltration technique used for the extraction of upper maxillary teeth in this study was the appropriate one. Therefore, the operator objective factors are not the reason for the failure of dental local anesthesia amongst our participants.
In light of these facts, there are four possible accounts may explain the reasons for the failure of dental anesthesia in our study. First account might increase in the acidity at the site of injection. The subject with failure of dental anesthesia could have been diagnosed with irreversible pulpitis at the time of extraction.[20] This means the physiological pH of surrounding soft tissue around the apex of subject tooth for extraction will be decreased.[23,24,25,26,27] In the presence of tissue infection or inflammation (acidic pH), the free base (NR3) of the anesthetic hydrochloride salt of tertiary amine (NR3 - HCL) fail to liberated from its salt (HCL).[6,7] As a result of zero or few number of free bases (NR3) binds to specific receptors in the sodium channels to block the influx of sodium ions and nerve impulse generation, failure of anesthesia occurs.[6,28,29] Second account could be tooth morphology. This comprises size and number of roots for each tooth listed for extraction. Theoretically, single rooted teeth have less bulky pulpal tissue than multiple rooted teeth and therefore they should have early anesthesia and extraction.[19,20] This fact may justify the causes of dental anesthesia failure with multiple rooted teeth. Our study results are consistent with the findings of Gazalet al's study that indicated that the anesthesia onset time was faster in anterior upper teeth than middle and posterior ones.[24] Number of dental anesthesia failures was slightly higher in patients with multiple rooted teeth than those with single rooted teeth. A study by Moradi Askari et al.[10] was conducted on 100 patients suffering from irreversible pulpitis of maxillary first molars to evaluate the effectiveness of root length on the success rate of buccal infiltration anesthesia. Following the administration of buccal infiltration injections of 2% lidocaine with 1:80,000 epinephrine, root canal treatments were carried out. Pain assessment scores were recorded by using the Heft-Parker visual analog scale at different points of dent treatment. The findings of this study showed that patients with longer roots of maxillary first molars have more anesthesia failure following a single buccal infiltration injection with 2% lidocaine and 1:80000 epinephrine than those with short roots.[19] No significant difference was found between 2% lidocaine and 4% articaine in terms of anesthetic success in maxillary first molars with irreversible pulpitis.[3,19] Furthermore, another interesting results were found by Hosseini et al.[20] who studied the effect of root length of first maxillary molars with symptomatic irreversible pulpitis on the success of buccal infiltration anesthesia regardless of what the type of anesthetic agent was used. Hosseini's study findings reported that the length of the palatal root had a significant negative influence on anesthetic success.[20] Third account is the thickness of buccal cortical plate of maxillae. It was reported that the thickness of the buccal cortical plate is around 1.59 ± 0.7 mm.[30,31,32] Labial plate of upper anterior teeth is thinner than the buccal plate of posterior teeth. Although the buccal plate of maxillae is more porous and less dense than the buccal aspect of mandibular bone, the thickness of buccal plate is still performing a barrier in front of the diffusion of the local anesthesia.[31] The more the thickness of the buccal plate the slow the onset of action of LA. This fact is supported by the results of Flanagan's study[30] which reported that articaine buccal infiltration can be a substitute injection for Inferior Alveolar Nerve Block in posterior mandibular teeth on condition that the thickness of buccal cortical plate must be less than 3 mm. So, 2-3 mm is a cutoff point for successful anesthesia in mandible posterior infiltration.[31,32] Fourth account was suggested by Omar et al.[33] that the relationship between the upper multiple rooted teeth and maxillary sinus in particular the upper first molars can have an influence on the success rate of the infiltrative local anesthetic injections. In some cases, the maxillary sinus might occupy the space between the buccal and palatal roots of upper first molars.[34,35] This means that the diffusion of the local anesthetic solution might obstruct by the membrane of the maxillary sinus and therefore, the palatal root will not anesthetize.[36] Therefore, morphology of the tooth and adjacent hard tissue do play a role in the success rate of maxillary local anesthetic injections.
Conclusion
This study showed that the single rooted teeth have faster pulpal anesthesia and early extraction than teeth with multiple roots but not statistically significant. Administration of extra local anesthetic cartridge or using intraseptal injection technique can be a solution to overcome the failure of anesthesia in the maxillary posterior teeth.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Acknowledgments extend to all dental assistants and Oral and Maxillofacial surgeons in the Taibah Dental College for their participation in this study.
References
- 1.Gazal G, Tola AW, Fareed WM, Alnazzawi AA, Zafar MS. A randomized control trial comparing the visual and verbal communication methods for reducing fear and anxiety during tooth extraction. Saudi Dent J. 2016;28:80–5. doi: 10.1016/j.sdentj.2015.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gazal G, Fareed WM, Zafar MS. Role of intraseptal anaesthesia for pain-free dental treatment. Saudi J Anaesth. 2016;10:81–6. doi: 10.4103/1658-354X.169482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gazal G. Is articaine more potent than mepivacaine for use in oral surgery? J Oral Maxillofac Res. 2018;9:e5. doi: 10.5037/jomr.2018.9305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alsharif A, Omar E, Alolayan AB, Bahabri R, Gazal G. 2% lidocaine versus 3% prilocaine for oral and maxillofacial surgery. Saudi J Anaesth. 2018;12:571–7. doi: 10.4103/sja.SJA_259_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.St George G, Morgan A, Meechan J, Moles DR, Needleman I, Ng YL, et al. Injectable local anaesthetic agents for dental anaesthesia. Cochrane Database Syst Rev. 2018;7:CD006487. doi: 10.1002/14651858.CD006487.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chitre AP. Manual of Local Anesthesia in Dentistry. 3rd ed. New Delhi, India: Jaypee. Brothers Medical Publisher; 2016. pp. 63–7. [Google Scholar]
- 7.Malamed SF. Handbook of Local Anaesthesia. 3rd ed. St Louis: Mosby-Year Book; 1990. [Google Scholar]
- 8.Meechan JG. Local anaesthesia: Risks and controversies. Dent Update. 2009;36:278. doi: 10.12968/denu.2009.36.5.278. [DOI] [PubMed] [Google Scholar]
- 9.Radford A. Reasons for failed local anaesthesia in dentistry. SAAD Dig. 2007;23:24–8. [PubMed] [Google Scholar]
- 10.Meechan JG. Why does local anaesthesia not work everytime? Dent Update. 2005;32:66. doi: 10.12968/denu.2005.32.2.66. [DOI] [PubMed] [Google Scholar]
- 11.Oliver G, David DA, Bell C, Robb N. An investigation into dental local anaesthesia teaching in United Kingdom dental schools. SAAD Dig. 2016;32:7–13. [PubMed] [Google Scholar]
- 12.Hashemi SH, Ladez SR, Moghadam SA. Comparative assessment of the effects of three local anaesthetics: Lidocaine, prilocaine, and mepivacaine on blood pressure changes in patients with controlled hypertension. Glob J Health Sci. 2016;8:54157. doi: 10.5539/gjhs.v8n10p227. [DOI] [PubMed] [Google Scholar]
- 13.Moore PA. Innovations in local anesthesia are easing the pain of dentistry. Compend Contin Educ Dent. 2018;39:256–7. [PubMed] [Google Scholar]
- 14.Serrera Figallo MA, Velázquez Cayón RT, Torres Lagares D, Corcuera Flores JR, Machuca Portillo G. Use of anaesthetics associated to vasoconstrictors for dentistry in patients with cardiopathies. Review of the literature published in the last decade. J Clin Exp Dent. 2012;4:e107–11. doi: 10.4317/jced.50590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Caviedes-Bucheli J, Rojas P, Escalona M, Estrada A, Sandoval C, Rivero C, et al. The effect of different vasoconstrictors and local anaesthetic solutions on substance P expression in human dental pulp. J Endod. 2009;35:631–3. doi: 10.1016/j.joen.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 16.Ghaderi F, Ahmadbeigi M. Pain perception due to dental injection by smartject: Split mouth design study. J Dent (Shiraz) 2018;19:57–62. [PMC free article] [PubMed] [Google Scholar]
- 17.Meechan JG. The use of the mandibular infiltration anaesthetic technique in adults. J Am Dent Assoc. 2011;142:19S–24S. doi: 10.14219/jada.archive.2011.0343. [DOI] [PubMed] [Google Scholar]
- 18.Siddiqui A, Shenoi R, Sharma HU, Harankhedkar N, Shrivastava A, Vats V, et al. Causes of failure of dental local anaesthesia. Int J Contemporary Med Res. 2015;2:415–9. [Google Scholar]
- 19.Moradi Askari E, Parirokh M, Nakhaee N, Hosseini HR, Abbott PV. The effect of maxillary first molar root length on the success rate of buccal infiltration anesthesia. J Endod. 2016;42:1462–6. doi: 10.1016/j.joen.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 20.Hosseini HR, Parirokh M, Nakhaee N, V Abbott P, Samani S. Efficacy of articaine and lidocaine for buccal infiltration of first maxillary molars with symptomatic irreversible pulpitis: A randomized double-blinded clinical trial. Iran Endod J. 2016;11:79–84. doi: 10.7508/iej.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meechan JG. How to overcome failed local anaesthesia. Br Dent J. 1999;9:15–20. doi: 10.1038/sj.bdj.4800006. [DOI] [PubMed] [Google Scholar]
- 22.Abu-Mostafa N, Aldawssary A, Assari A, Alnujaidy S, Almutlaq A. A prospective randomized clinical trial compared various types of local anaesthetics cartridges. J Clin Exp Dent. 2015;7:e84–8. doi: 10.4317/jced.51534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Katz S, Drum M, Reader A, Nusstein J, Beck M. A prospective, randomized, double-blind comparison of 2% lidocaine with 1:100,000 epinephrine, 4% prilocaine with 1:200,000 epinephrine, and 4% prilocaine for maxillary infiltrations. Anesth Prog. 2010;57:45–51. doi: 10.2344/0003-3006-57.2.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gazal G, Alharbi R, Fareed WM, Omar E, Alolayan AB, Al-Zoubi H, et al. Comparison of onset anesthesia time and injection discomfort of 4% articaine and 2% mepivacaine during teeth extractions. Saudi J Anaesth. 2017;11:152–7. doi: 10.4103/1658-354X.203017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burton AJ, Backhouse O, Metcalfe TW. Prilocaine versus lignocaine for minor lid procedures. Eye (Lond) 2000;14:594–6. doi: 10.1038/eye.2000.149. [DOI] [PubMed] [Google Scholar]
- 26.Lawaty I, Drum M, Reader A, Nusstein J. A prospective, randomized, double-blind comparison of 2% mepivacaine with 1:20,000 levonordefrin versus 2% lidocaine with 1:100,000 epinephrine for maxillary infiltrations. Anesth Prog. 2010;57:139–44. doi: 10.2344/0003-3006-57.4.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kanaa MD, Whitworth JM, Corbett IP, Meechan JG. Articaine and lidocaine mandibular buccal infiltration anaesthesia: A prospective randomized double-blind cross-over study. J Endod. 2006;32:296–8. doi: 10.1016/j.joen.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 28.Ezmek B1, Arslan A, Delilbasi C, Sencift K. Comparison of hemodynamic effects of lidocaine, prilocaine and mepivacaine solutions without vasoconstrictor in hypertensive patients. J Appl Oral Sci. 2010;18:354–9. doi: 10.1590/S1678-77572010000400006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gazal, G Comparison of speed of action and injection discomfort of 4% articaine and 2% mepivacaine for pulpal anaesthesia in mandibular teeth: A randomized, double-blind cross-over trial. Eur J Dent. 2015;9:201–6. doi: 10.4103/1305-7456.156811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Flanagan DF. The effectiveness of articaine in mandibular facial infiltrations. Local Reg Anesth. 2016;9:1–6. doi: 10.2147/LRA.S94647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim C, Hwang KG, Park CJ. Local anesthesia for mandibular third molar extraction. J Dent Anesth Pain Med. 2018;18:287–94. doi: 10.17245/jdapm.2018.18.5.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gazal G. Overcoming the failure of anesthesia in the mandibular teeth. Saudi Med J. 2019;40:425. doi: 10.15537/smj.2019.5.24078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Omar EAZ, Jarab F, Fareed WM. Local Anesthesia and Extractions for Dental Students: Simple Notes and Guidelines. Bentham Science Publishers; 2018. eISBN: 978-1-68108-633-0. doi: 10.2174/97816810863301180101. [Google Scholar]
- 34.Nino-Barrera JL, Ardila E, Guaman-Pacheco F, Gamboa-Martinez L, Alzate-Mendoza D. Assessment of the relationship between the maxillary sinus floor and the upper posterior root tips: Clinical considerations. J Investig Clin Dent. 2018;9:e12307. doi: 10.1111/jicd.12307. [DOI] [PubMed] [Google Scholar]
- 35.Lovasova K, Kachlik D, Rozpravkova M, Matusevska M, Ferkova J, Kluchova D. Three-dimensional CAD/CAM imaging of the maxillary sinus in ageing process. Ann Anat. 2018;218:69–82. doi: 10.1016/j.aanat.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 36.Iwanaga J, Tubbs RS. Palatal Injection does not block the superior alveolar nerve trunks: Correcting an error regarding the innervation of the maxillary teeth. Cureus. 2018;10:e2120. doi: 10.7759/cureus.2120. [DOI] [PMC free article] [PubMed] [Google Scholar]


