Abstract
An 80-year-old male patient presented with 2 weeks history of low back pain undergoing posterior spinal fusion with laminectomy in the prone position. The patient was induced with fentanyl, propofol, and rocuronium, and then he was positioned in the prone position. After 6 h of starting the surgery, the patient started to be hypotension and bradycardia followed by pulseless electrical activity (PEA). Code blue was activated intraoperatively with immediate initiation of cardiopulmonary resuscitation (CPR) in the prone position and multiple epinephrine boluses. Fortunately, the patient had return of spontaneous circulation. After stabilization, he was taken for computed tomography scan which showed massive pulmonary embolization and management was continued in the intensive care unit. CPR in the prone position has shown to be effective for return of spontaneous circulation after PEA.
Keywords: Cardiac arrest, cardiopulmonary resuscitation, prone position
Introduction
Cardiac arrest is a serious complication which is considered as a challenge for surgeons and anesthetists, especially during elective surgeries. Since 1960, the cornerstone of therapy for cardiopulmonary arrest is known to be cardiopulmonary resuscitation (CPR).[1] For more than 40 years, traditional CPR continued to be unchanged, despite the lack of experience in some health professionals and their performances, inadequate training, and low survival rates from outside the hospital cardiac arrests.[2] Fortunately, cardiac arrest in the prone anesthetized patient is rare. However, if it happens in such an unusual position, it is more challenging because the knowledge about how to perform CPR in the prone position is not well-understood and not so often used. On the contrary, the current technique used with prone CPR is customized from the traditional supine CPR.[3]
In 1989, prone CPR “reverse CPR” was first introduced by McNeil and reinforced by Stewart in 2002 as a new much simpler technique with many advantages and high chance to be performed by witnesses; however, little data exist beyond intraoperative case reports.[4] Standard CPR is known to be done in supine position on a firm surface (hard board or floor). Since 2005, the American Heart Association Guidelines for CPR and Emergency Cardiovascular Care recommended that CPR in the prone position might be reasonable when the patient cannot be replaced in the supine position without prejudice, particularly in hospitalized patients with an advanced airway in place.[3] This recommendation was included in the 2010 Guidelines (Class IIb, LOE C) but not reviewed in the 2015 Guidelines. This is mainly done to reduce the NO flow time (blood flow to the heart or brain), as flipping back the patient to the supine position might take a lot of time, when taking into consideration not damaging vital structures when fixed to a Mayfield Skull Clamp, for instance, or open spine surgery.[3] In addition, changing a patient's position might be difficult, time-consuming, and delays the initiation of cardiac massage.
A successful resuscitation following posterior compression, using either a one- or two-handed technique, with or without counterpressure on the sternum, has been reported regarding the performance of CPR.[5] The chest compressions are given with the hands of the rescuer in the midline between the two scapulae (i.e., at T7–T10 position) with the rest of the technique the same as for supine CPR. As a counterpressure for the missing firm surface, one hand clenched into a fist can be placed under the patient's sternum (reversed precordial compression), while the surgeon can perform the CPR from the surgical site (thoracic spine surgery) without affecting the sterility of the surgical field.[3]
One of the mainstays of the basic life support algorithms are chest compressions, with the timing of their onset considered as a major determinant of survival from cardiac arrest.[6] Many patients may suffer cardiac arrest while in the prone position and significant delays in the onset of CPR may succeed while good numbers of staff are available to return the patient safely to the supine position and commence conventional CPR.[7]
Case Presentation
The case described here is an 80-year-old male patient, a known case of hypertension, diabetes type 2, dyslipidemia, and hypothyroidism. The patient was bedridden for 1 month and needs assistance in ambulation. He was admitted with 2 weeks history of lower back pain with heaviness, numbness, and pain radiating to the right lower limb.
The patient was booked for posterior spinal fusion with laminectomy. On preoperative assessment, he had left anterior fascicular block on electrocardiogram (ECG); echocardiography showed that left ventricular function is good with ejection fraction >55% and he had no active cardiac issues. However, according to the cardiology assessment, the patient carried intermediate risk for adverse perioperative cardiac events. Chest examination showed good bilateral air entry and chest X-ray was normal.
Induction of anesthesia was done successfully with 2 μg/kg fentanyl, 1.5 mg/kg propofol, and 0.6 mg/kg rocuronium without any complications. Central line and arterial line were inserted. After that, the patient was positioned into the prone position and surgery was started at 9:55 am and the patient was doing well.
Six hours later, the patient became hypotensive and he responded to 100 μg of phenylephrine. Few minutes later, he became hypotensive again with bradycardia. About 1 mg of atropine was given, and the surgeons were informed about the patient's condition. Five minutes later, the monitor showed pulseless electrical activity (PEA) and the procedure was immediately stopped.
Code blue was activated and CPR in the prone position was initiated immediately. After two doses of epinephrine, the patient had return of spontaneous circulation with systolic pressure of 200 mmHg.
After that, the patient was flipped to the supine position. Few minutes later, he developed PEA again and CPR was resumed according to advanced cardiovascular life support (ACLS) protocols. The patient responded in many episodes to epinephrine boluses. Both norepinephrine and epinephrine were initiated at maximum doses.
Transesophageal echocardiography was done, and it showed dilated right ventricle with high pulmonary artery pressure. After that, spiral computed tomography (CT) was done and it revealed bilateral segmental massive pulmonary embolism, as shown in Picture 1a and b.
Picture 1.
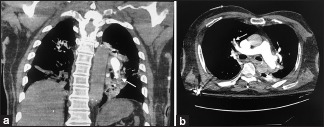
Spiral CT scan shows a massive right large pulmonary embolism, (a) Sagittal view. (b) Transverse view
The cardiologist was consulted, and according to the spiral CT findings, there was no intervention from their side.
Discussion
Many surgical operations require patients to be in the prone position; such position gives access to the surgeons to the posterior structures of the human body. Mentioning that the prone position gives better access to some structures, it also carries some risks, most of which are hypovolemia and cardiac arrest.[8] In contrast, there are some benefits to prone CPR including less risk of aspiration pneumonia and, most importantly, no delay in initiating compressions.[1]
The concept of prone CPR was first introduced by McNeil in 1989 and reinforced by Stewart in 2002.[9] According to the 2005 ACLS guidelines, one could perform CPR in the prone position only in advance hospital settings, which was the case in our patient.[1] Changing patient's position from prone to supine for the initiation of chest compressions might cause neural damage and it is time-consuming (5–6 min), as it was shown that prone CPR provides adequate cardiac and respiratory support.[5] In the case of difficulty to turn the patient into supine position, there are some actions that should be applied. First, make sure that airway is secured and make sure it is in place by checking the tube confirming it is not kinked or obstructed or displaced out of the trachea. Ensure that the ventilator is connected to the patient with 100% FIO2 concentration. In addition, check that there is no sudden unidentified loss of blood. After that, start chest compressions; it is recommended to be at the largest left ventricle cross-sectional area which is located directly below the line crossing both inferior angle of scapula as demonstrated in Figure 1. There are two techniques that prone CPR could be performed with. One of which is a two-handed technique in which the performer places two hands together at the midline at the previously mentioned level. The other technique is the one-handed technique by placing a hand at either side of the thoracic spine at the same level in the midline thoracic spine surgeries. Moreover, a sternal support should be positioned if possible.[9]
Figure 1.
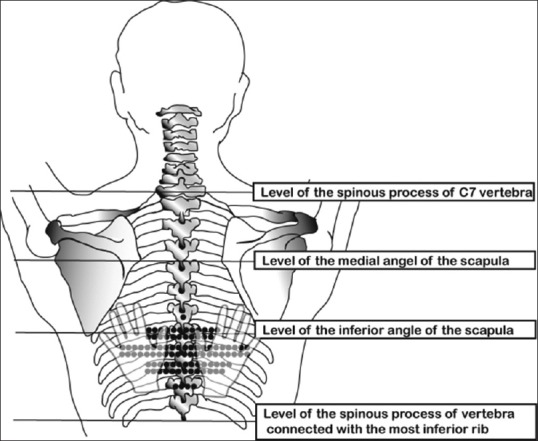
Different levels where chest compressions may be performed during prone CPR
While performing a prone CPR, it is important to ensure high-quality CPR by setting targets for rate and depth of compressions as well as minimum values provided from the monitoring machines such as capnography and continuous arterial line. During performing prone CPR, a defibrillator should be applied using maximum energy discharge. A patient should be shocked at the end of expiration with the lowest positive end expiratory pressure to minimize the chest impedance. There are few techniques that the defibrillator's pads should be placed in. One of which is the one electrode technique placed to the left lower sternal border and the other posteriorly below the scapula. While the two electrode gel pads placed on the back of the chest on either side of the thoracic spine one low down on the left side just posterior to the mid axillary line and the other inferior to the right scapula. Successful electrical defibrillation has been reported in patients having spinal surgery in the prone position.[10]
Although prone CPR has shown to be convenient, the gold standard is to have the patient positioned supine as much as possible to perform effective CPR.[9]
There were some reported cases of cardiac arrest while in the prone position that underwent prone CPR which showed to be successful. The method of which prone CPR was preformed varied from one case to another; however, the outcomes were similar in all.[4] In neurological surgery setting, a case was reported of a 77-year-old female who underwent prone CPR due to hemorrhagic shock; after return of spontaneous circulation, the patient was transferred to the intensive care unit, where norepinephrine was administered in small doses; in our case, the patient received epinephrine while performing compression which helped in recovering his blood pressure.[2] Another case reported in neurological surgery setting was of a 6-month-old baby girl; she underwent prone CPR due to compression of the cervical spine leading to hypotension and hemorrhage; air was entrained into the venous circulation. Prone CPR was commenced and the patient received intermittent positive airway pressure ventilation for 4 days postoperatively. This study defers from our case in that the patient has history of respiratory distress requiring mouth-to-mouth resuscitation, indicating previous respiratory insufficiency.[11] Moreover, a 60-year-old female case was reported; she underwent prone CPR due to an air embolism that lead to cardiac arrest. This patient also suffered some broad complex tachycardia. Afterward, the patient showed complete recovery postoperatively.[12] In an orthopedic setting, a 12-year-old male underwent spinal fusion to treat his scoliosis. His procedure was complicated by severe sudden bradycardia, ECG changes, and decrease in the mean arterial pressure that did not respond to norepinephrine. Due to inability to turn the patient to supine position, prone CPR was started which eventually showed no complications and good postoperative recovery.[7] Prone CPR has repeatedly showed good outcomes with no delay in initiating compressions.
Conclusion
Orthopedic surgeries, in specific spine surgeries, mandate their patients to be positioned prone on the operation table. Being in the prone position upsurges the risk of cardiac arrest during surgery due to air embolism and hemodynamic instability. Due to recent studies and case reports that were done all over the world, prone CPR has shown high rates of survival and return of spontaneous circulation with good postoperative recovery and no complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors thanks Mr. Abdulaziz Alsudairi; Medical Trainee, King Saud bin Abdulaziz University for Health Sciences and Dr. Samer Arab; Consultant, Anesthesia Department, King Abdulaziz Medical City, Riyadh, Saudi Arabia, for their valuable input and case progress summarization.
References
- 1.Yien HW. Is the upside-down position better in cardiopulmonary resuscitation? J Chin Med Assoc. 2006;69:199–201. doi: 10.1016/S1726-4901(09)70218-7. [DOI] [PubMed] [Google Scholar]
- 2.de Souza Gomes D, Bersot CD. Cardiopulmonary resuscitation in the prone position. Open J Anesthesiol. 2012;2:199–201. [Google Scholar]
- 3.Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, et al. Part 1: Executive summary.2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:315–67. doi: 10.1161/CIR.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 4.Stewart JA. Resuscitating an idea: Prone CPR. Resuscitation. 2002;54:231–6. doi: 10.1016/s0300-9572(02)00145-4. [DOI] [PubMed] [Google Scholar]
- 5.Wei J, Tung D, Sue SH, Wu SV, Chuang YC, Chang CY. Cardiopulmonary resuscitation in prone position: A simplified method for outpatients. J Chin Med Assoc. 2006;69:202–6. doi: 10.1016/S1726-4901(09)70219-9. [DOI] [PubMed] [Google Scholar]
- 6.Haffner E, Sostarich AM, Fosel T. Successful cardiopulmonary resuscitation in prone position. Anaesthesist. 2010;59:1099–101. doi: 10.1007/s00101-010-1785-8. [DOI] [PubMed] [Google Scholar]
- 7.Tobias JD, Mencio GA, Atwood R, Gurwitz GS. Intraoperative cardiopulmonary resuscitation in the prone position. J Pediatr Surg. 1994;29:1537–8. doi: 10.1016/0022-3468(94)90208-9. [DOI] [PubMed] [Google Scholar]
- 8.Kwee MM. The prone position during surgery and its complications: A systematic review and evidence-based guidelines. Int Surg. 2015;100:292–303. doi: 10.9738/INTSURG-D-13-00256.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clinical guideline for positioning patient under general anesthesia. Department of Anesthesia, King Abdulaziz Medical City, Riyadh, Saudi Arabia; DPP-7810-03-00-03, 2018. [Google Scholar]
- 10.Walsh SJ, Bedi A. Successful defibrillation in the prone position. Br J Anaesth. 2002;89:799. doi: 10.1093/bja/aef565. [DOI] [PubMed] [Google Scholar]
- 11.Kelleher A, Mackersie A. Cardiac arrest and resuscitation of a 6-month old achondroplastic baby undergoing neurosurgery in the prone position. Anaesthesia. 1995;50:348–50. doi: 10.1111/j.1365-2044.1995.tb04615.x. [DOI] [PubMed] [Google Scholar]
- 12.Brown J, Rogers J, Soar J. Cardiac arrest during surgery and ventilation in the prone position: A case report and systematic review. Resuscitation. 2001;50:233–8. doi: 10.1016/s0300-9572(01)00362-8. [DOI] [PubMed] [Google Scholar]


