Abstract
Background
This study aims to investigate the coronary microcirculatory resistance and prognosis of patients with acute myocardial infarction (AMI) concomitant with hyperhomocysteinemia (HHcy) after an elective percutaneous coronary intervention (PCI).
Methods
A total of 101 patients that underwent elective PCI between May 2015 and July 2018 due to AMI were consecutively enrolled in this study. Patients were divided into a HHcy group (53) and a normal Hcy group (control; 48) based on their plasma homocysteine concentration. The characteristics of coronary angiography, the index of microcirculatory resistance (IMR) of infarct-related vessels (IRV), changes in left ventricular end diastolic diameter (LVEDd) and left ventricular ejection fraction (LVEF) before and after PCI, and the incidence of major adverse cardiovascular events (MACE) three months after PCI were compared between these groups.
Results
Compared to the results from the Hcy group, the HHcy group had a higher IMR. The HHcy group had significantly higher LVEDd and a lower LVEF than the Hcy group 3 months after PCI. Additionally, the incidence of MACE at three months after PCI was higher in the HHcy group than in the Hcy group. Pearson correlation analysis revealed a positive correlation with IMR in the HHcy group. Furthermore, there was a difference in the LVEDd measured at one day after PCI and at three months after PCI in the HHcy group.
Conclusion
AMI patients concomitant with HHcy that undergo elective PCI are prone to coronary microcirculatory dysfunction and have a poor cardiac function and poor prognosis at three months after PCI.
1. Introduction
Acute myocardial infarction (AMI) is one of the most common cardiac diseases worldwide and has three clinical forms: acute non-ST-segment elevation myocardial infarction (NSTEMI), ST-segment elevation myocardial infarction (STEMI), and unstable angina [1]. While it has been well recognized that AMI is caused by a blockade of the coronary arteries, coronary microcirculation, which is essential for the survival of the local myocardium and myocardial recovery after AMI [2], also plays an important role in disease development, progression, and prognosis. Indeed, several studies have revealed that impaired microcirculation predicts the poor outcomes of AMI patients [3, 4]. Currently, the mainstay of treatment for patients with AMI is percutaneous coronary intervention (PCI). However, PCI may also cause microcirculatory dysfunction, thus, leading to a poor prognosis [5]. Hence, an accurate determination of the functional status of the microcirculation offers a valuable assessment of the outcomes of patients with AMI after PCI. Among these measures, the index of microcirculatory resistance (IMR) is a relatively simple quantitative measure of coronary microcirculatory function and is considered to be a reliable indicator of the extent of coronary vascular bed expansion. For instance, Fearon et al. found that the IMR obtained immediately after emergency PCI in STEMI patients was significantly negatively correlated with the postoperative echocardiographic wall motion scores obtained three months after PCI, as evidenced by the observation that the group with an IMR >32 had a significantly lower wall motion score than that of the group with an IMR <32 [6]. Additionally, they proposed that an IMR >40 is a predictor of death or hospitalization due to heart failure [7], and an elevated IMR after AMI has been shown to be an important indicator of a lowered myocardial survival rate [8]. Therefore, IMR is an appropriate index for the evaluation of microcirculatory function in AMI patients.
Homocysteine (Hcy) is an amino acid that is generated through protein breakdown. A high plasma Hcy level, hyperhomocysteinemia (HHcy), plays an important role in arterial damage and thrombosis [9]. Recent studies have shown that HHcy contributes to a high IMR and circulating hs-CRP in patients with coronary atherosclerotic stenosis [10]. Furthermore, HHcy is an independent predictor of increased coronary microcirculation resistance [10]. Additionally, HHcy is closely associated with an increased risk of long-term adverse events in patients with coronary artery diseases [11]. Moreover, the long-term risk of all-cause mortality of patients that have undergone PCI is significantly higher when plasma Hcy levels exceed 13.5 μmol/L [12]. Together, these findings suggest that there is a prognostic value of HHcy in patients with cardiac diseases. However, whether HHcy may be used to predict the outcomes of patients with AMI that have undergone elective PCI has not been well explored. This study aimed to investigate whether the coronary microcirculatory resistance, as reflected by IMR, could be used to assess the short-term prognosis of patients with AMI complicated by HHcy.
2. Materials and Methods
2.1. Ethics Statement
This study protocol was approved by the Ethics Committee of the Second Affiliated Hospital of Wenzhou Medical University. Written informed consent was obtained from all participants.
2.2. Subject Selection
A total of 101 patients that were undergoing elective PCI due to acute NSTEMI or STEMI in the Second Hospital affiliated to Wenzhou Medical University between May 2017 and May 2019 were consecutively selected for this study. Patients who had acute occlusion of at least one major epicardial coronary artery were included in this study. None of the patients had accepted the thrombolytic therapy. Patients who had one or more of the following traits were excluded from our study: (1) uncontrolled severe heart failure (ejection fraction < 35%), (2) inability to tolerate dual antiplatelet therapy, (3) extremely slow arrhythmia (hearty rate < 50/min), (4) hemorrhagic disease, (5) asthma or severe pulmonary dysfunction, (6) a history of coronary artery bypass surgery, (7) severe liver and kidney dysfunction, and (8) acute and chronic infectious diseases. Based on a cut-off plasma Hcy level of 10 μmol/L defined by the American Heart Association (AHA) [13] before PCI, these patients were divided into two groups: a HHcy group (Hcy > 10 μmol/L; n = 53) and a normal Hcy group (control; Hcy < 10 μmol/L; n = 48).
The diagnostic criteria for hypercholesterolemia were based on the following recommendations for the prevention and treatment of dyslipidemia that were formulated in 1997 in China: total cholesterol (TC) > 5.2 mmol/L, low-density lipoprotein cholesterol > 3.4 mmol/L, or plasma TC concentration after adequate lipid-lowering therapy was controlled. Diabetes mellitus was diagnosed based on the following criteria, defined by the American Diabetes Association: fasting blood glucose >7.0 mmol/L or insulin injection and/or the requirement of hypoglycemic drugs to maintain blood glucose within the normal range. Hypertension was diagnosed based on the Joint National Committee VII (JNC VII) guidelines: systolic blood pressure (SBP) > 140 mmHg and/or diastolic blood pressure (DBP) > 90 mmHg, or the patient had a history of chronic hypertension and needed oral antihypertensive drugs to control the blood pressure. Smoking was referred to as a continuous period of smoking that lasted more than six months. A high BMI was defined as a BMI >24 kg/m2. Chronic kidney disease was defined as a glomerular filtration rate lower than 60 ml/min/1.73 m2 or a positive marker of renal injury without a decrease in glomerular filtration rate.
2.3. Elective PCI
All patients underwent coronary angiography and balloon dilatation and stenting for infarct-related vessels (IRV). A successful stent was defined as having all of the following features: significant relief or disappearance of chest pain, a fully expanded and adherent stent as revealed by angiography, less than 20% of the residual stenosis of the target vessel, no intimal tear or dissection, and a thrombolysis in myocardial infarction (TIMI) grade III flow.
2.4. Determination of IMR
IMR was obtained using pressure and temperature sensitive guidewire (St. Jude Medical Company, Sweden) after stent implantation of all IRVs. The procedure is briefly described as follows: (1) aortic pressure was set to zero and the guidewire was calibrated outside of the body; (2) the guidewire was sent to the guide catheter port to calibrate the pressure and temperature, and the pressure of the ostium of the guidewire was equalized to the pressure of the ostium of the guide catheter, which was similar to the mean aortic pressure (Pa) and was used as a pressure reference. Additionally, the corrected temperature was used as a reference for subsequent temperature changes; (3) the guidewire was further pushed through the lesion segment and exceeded two-thirds of the total length; (4) intracoronary nitroglycerin (200 μg) was injected to minimize the coronary arterial tone; (5) three milliliters of room temperature normal saline was quickly injected using the thermal dilution technique. When the liquid entered the ostium of the coronary artery, the pressure guide shaft recorded the first temperature curve. When the liquid passed through the sensor of the head of the guidewire, the second temperature curve was recorded. The time difference between the recording of the first and the second temperature curve was defined as the mean transit time (Tmn). The mean transit time of the baseline (bTmn) was obtained from three continuous measurements; (6) ATP (140 μg/kg/min, over 3–6 min) was pumped through the elbow vein to maximize hyperemia of the coronary artery, followed by rapid injection of 3 ml of normal saline after 90 seconds three times in a row to obtain the mean transit time under hyperemia (hTmn); (7) the Pa values at the resting and hyperemic state and the mean distal coronary pressure (Pd) at the stenotic lesion were recorded, and the IMR was calculated by the machine based on the following formula: IMR = Pd × Tmn.
2.5. Plasma Hcy Measurement
Two days before angiography, a 5 ml blood sample was collected from an elbow vein of each patient. This sample was placed in a test tube containing ethylenediaminetetraacetic acid and centrifuged at 2,500 rpm/min for 20 minutes. The supernatant was collected and stored at −20°C. The plasma Hcy concentration was measured using an ELISA kit (DADE Behring, USA) and a Biochemical Automated Analyzer (DADE Behring, USA).
2.6. Follow-Up
Echocardiography was performed for all patients using an ultrasound system (IE33, Philips) at one day and three months after PCI. The examination conditions were as follows: the probe frequency was 2.0 MHz∼4.0 MHz and the Doppler velocity range was −30 cm/s∼30 cm/s. Several important cardiac functional parameters, including left ventricular end diastolic diameter (LVEDd) and left ventricular ejection fraction (LVEF), were recorded. The LVEF was measured using the Simpson biplane method. At three months after PCI, major adverse cardiovascular events (MACE) were defined as the occurrence of cardiac death, recurrent myocardial infarction and angina pectoris, severe heart failure, malignant arrhythmia, and retargeted revascularization, as previously reported [14].
2.7. Statistical Analysis
All statistical analyses were performed using SPSS 20.0 software (USA). Measurement data are expressed as mean ± standard deviation (SD). After the Kolmogorov–Smirnov test for normality, comparisons were calculated using t-tests and analysis of variance (ANOVA) between groups, while the X2 test was used to compare the count data. Linear regression analysis was used to examine the correlation between the Hcy concentration and IMR and the changes in LVEDd and LVEF of each patient between one day and three months after PCI. Pearson correlation analysis and multivariate logistic regression analysis were used to evaluate the relationship between total MACE and the related risk factors at 3 months after PCI. Statistical significance was defined as a P value less than 0.05.
3. Results
3.1. Comparison of the Demographic and Basal Clinical Characteristics of Patients between the Two Groups
As shown in Table 1, there were no significant differences in the age, smoking habits, BMI, hypertension, hyperlipidemia, diabetes, chronic kidney disease, PCI, or common biochemical test results and medications between the HHcy and control groups (P > 0.05). As expected, the plasma Hcy concentration was significantly higher in the HHcy group than in the control group (14.15 ± 3.30 mmol/L vs. 6.67 ± 1.66 mmol/L, P < 0.01). Additionally, the hs-CRP level was higher in the HHcy group than in the control group (10.9 ± 1.3 mg/L vs. 9.7 ± 1.6 mg/L, P < 0.01).
Table 1.
Comparison of the demographic and basal clinical characteristics of patients between the two groups.
| Characteristics | HHcy group (n = 53) | Control group (n = 48) | P | X 2 (t) |
|---|---|---|---|---|
| Age (years) | 57.3 ± 10.9 | 55.9 ± 8.8 | 0.500 | 0.677 |
| Gender, male (%) | 30 (56.6%) | 25 (47.2%) | 0.649 | 0.208 |
| BMI (kg/m2) | 27.3 ± 3.2 | 27.0 ± 4.0 | 0.696 | 0.391 |
| CKD | 7 (13.2%) | 4 (7.5%) | 0.432 | 0.617 |
| Smoker | 23 (43.4%) | 16 (30.2%) | 0.300 | 1.076 |
| Hypertension | 21 (39.6%) | 18 (34.0%) | 0.827 | 0.048 |
| Diabetes mellitus | 19 (35.8%) | 16 (30.2%) | 0.791 | 0.070 |
| Dyslipidemia | 24 (45.3%) | 22 (45.8%) | 0.956 | 0.003 |
| Previous PCI | 17 (32.1%) | 18 (37.5%) | 0.567 | 0.327 |
| STEMI | 48 (90.6%) | 45 (93.8%) | 0.554 | 0.350 |
| FBG (mmol/L) | 6.0 ± 1.2 | 5.8 ± 9.3 | 0.479 | 0.711 |
| Cre (μmoI/L) | 74.8 ± 15.3 | 74.6 ± 13.9 | 0.286 | 1.072 |
| LDL-C (mmol/L) | 3.1 ± 0.5 | 3.0 ± 0.6 | 0.228 | 1.213 |
| HDL-C (mmol/L) | 1.4 ± 0.4 | 1.6 ± 0.5 | 0.249 | −1.161 |
| CTnI (ng/ml) | 0.86 ± 0.69 | 0.71 ± 0.35 | 0.191 | 1.316 |
| BNP (pg/ml) | 453.6 ± 124.6 | 393.3 ± 204.9 | 0.074 | 1.806 |
| Hs-CRP (mg/L) | 10.9 ± 1.3 | 9.7 ± 1.6 | 0.000 | 4.116 |
| Medications: | ||||
| Beta-blocker | 38 (71.7%) | 35 (72.9%) | 0.891 | 0.019 |
| Calcium-blocker | 24 (45.3%) | 20 (41.7%) | 0.714 | 0.134 |
| Aspirin | 53 (100%) | 48 (100%) | 1.000 | |
| Clopidogrel | 53 (100%) | 48 (100%) | 1.000 | |
| Atorvastatin | 51 (96.2%) | 47 (97.9%) | 0.617 | 0.250 |
| Nitrates | 32 (60.4%) | 30 (62.5%) | 0.827 | 0.048 |
| ACEI/ARB | 31 (58.5%) | 30 (62.5%) | 0.681 | 0.169 |
| Homocysteine (μmol/L) | 14.15 ± 3.30 | 6.67 ± 1.66 | 0.000 | 14.152 |
HHcy: high homocysteine; BMI: body mass index; CKD: chronic kidney diseases; PCI: percutaneous coronary intervention; FBG: fasting blood glucose; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density lipoprotein cholesterol; CTnI: cardiac troponin I; Hs-CRP: high-sensitivity C-reactive protein; ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker.
3.2. Comparison of Coronary Angiographic Characteristics and IMR between the Two Groups
We next evaluated the differences in the coronary angiographic characteristics and IMR between the HHcy group and the control group. As shown in Table 2, there were no statistically significant differences in the number of diseased coronary arteries, the TIMI flow grades, the morphological characteristics of the atherosclerotic lesions, or the intracoronary distribution between the two groups (P > 0.05). Additionally, no difference was observed in the vascular sites between the two groups, as evaluated by pressure guidewire (P > 0.05). However, the IMR was significantly higher in the HHcy group than in the control group (P < 0.01).
Table 2.
Comparison of coronary angiographic characteristics and IMR between the two groups.
| HHcy (n = 53) | Control (n = 48) | P | X 2 (t) | ||
|---|---|---|---|---|---|
| Culprit vessel number | 1 | 31 (58.5%) | 23 (47.9%) | 0.287 | 1.132 |
| 2 | 18 (34.0%) | 21 (43.8%) | 0.313 | 1.018 | |
| 3 | 4 (7.5%) | 4 (8.3%) | 0.884 | 0.021 | |
| TIMI flow grade | 0 | 0 | 0 | 1 | |
| 1 | 0 | 0 | 1 | ||
| 2 | 3 (5.7%) | 2 (4.2%) | 0.730 | 0.119 | |
| 3 | 50 (94.3%) | 46 (95.8%) | 0.730 | 0. 119 | |
| Culprit vessel | LMCA | 1 (1.9%) | 0 (0%) | 0.339 | 0.915 |
| LAD | 37 (67.9%) | 32 (64.6%) | 0.734 | 0.115 | |
| Circumflex | 6 (11.3%) | 5 (10.4%) | 0.884 | 0.021 | |
| RCA | 9 (17.0%) | 11 (22.9%) | 0.455 | 0.559 | |
| Side branch | 25 (47.2%) | 29 (60.4%) | 0.183 | 1.777 | |
| IMR | 38.28 ± 8.05 | 27.13 ± 4.83 | 0.000 | 8.336 | |
HHcy: high homocysteine; TIMI: thrombolysis in myocardial infarction; LMCA: left main coronary artery; LAD: left anterior descending artery; RCA: right coronary artery; IMR: index of microvascular resistance.
3.3. Comparison of Cardiac Function and the Incidence of MACE after PCI between the Two Groups
The differences in LVEDd and LVEF were not statistically significant between the HHcy group and the control group at one day after PCI (P > 0.05). However, the LVEDd was significantly higher in the HHcy group than in the control group (52.3 ± 4.2 mm vs. 48.4 ± 4.6 mm, P < 0.01) 3 months after PCI. Furthermore, the difference in the LVEDd between one day and three months after PCI was significantly higher in the HHcy group than in the control group (4.2 ± 2.0 mm vs. 1.1 ± 2.5 mm, P < 0.01). At three months after PCI, the LVEF was significantly lower in the HHcy group than in the control group (47.8 ± 6.4% vs. 54.7 ± 6.1%, P < 0.01). Additionally, the difference in the LVEF between one day and three months after PCI was significantly lower in the HHcy group than in the control group (−2.2 ± 2.8% vs. 2.6 ± 2.9%, P < 0.01). We also found that the incidence of MACE was significantly higher in the HHcy group than in the control group 3 months after PCI (24.5% vs. 6.3%, P=0.019; Table 3).
Table 3.
Comparison of cardiac function and the incidence of MACE after PCI between the two groups.
| HHcy (n = 53) | Control (n = 48) | P | X 2 (t) | ||
|---|---|---|---|---|---|
| LVEDd (mm) | 1st day after PCI | 48.2 ± 3.7 | 47.3 ± 4.6 | 0.325 | 0.989 |
| 3 months after PCI | 52.3 ± 4.2 | 48.4 ± 4.6 | 0.000 | 4.410 | |
| Difference | 4.2 ± 2.0 | 1.1 ± 2.5 | 0.000 | 6.780 | |
| EF (%) | 1st day after PCI | 50.0 ± 7.4 | 52.1 ± 6.8 | 0.142 | −1.479 |
| 3 months after PCI | 47.8 ± 6.4 | 54.7 ± 6.1 | 0.000 | −5.535 | |
| Difference | −2.2 ± 2.8 | 2.6 ± 2.9 | 0.000 | −8.573 | |
| Total number of MACE | 13 (24.5%) | 3 (6.3%) | 0.019 | 5.503 | |
HHcy: high homocysteine; LVEDd: left ventricular end diastolic dimension; EF: ejection fraction; MACE: major adverse cardiovascular events.
3.4. Determination of Risk Factors for MACE Three Months after PCI
Univariate linear regression and logistic regression analysis showed that Hcy, LVEF, and age were independent risk factors for MACE three months after PCI in patients with AMI, with correlation coefficients (r) of 0.324, 0.389, and 0.304 and odds ratios of 3.741, 4.986, and 2.652, respectively. Among these risk factors, LVEF had the strongest correlation with MACE, followed by Hcy (Table 4).
Table 4.
Determination of risk factors for MACE at three months after PCI.
| Univariate regression analysis | Logistic regression analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| MACE (n = 16) | None-MACE (n = 95) | X 2 (t) | P | B | r | OR | P | |
| Age | 57.5 ± 9.6 | 52.0 ± 10.8 | 0.996 | 0.041 | 0.769 | 0.297 | 2.652 | 0.031 |
| Male | 10 (62.5%) | 48 (50.5%) | 0.787 | 0.375 | ||||
| Smoker | 7 (43.8%) | 34 (35.8%) | 0.373 | 0.542 | ||||
| Hypertension | 8 (50.0%) | 32 (33.7%) | 1.314 | 0.252 | ||||
| Diabetes mellitus | 5 (31.3%) | 30 (31.6%) | 0.001 | 0.979 | ||||
| Dyslipidemia | 7 (43.8%) | 39 (41.1%) | 0.041 | 0.839 | ||||
| BMI ≥24 kg/m2 | 9 (56.3%) | 51 (53.7%) | 0.036 | 0.849 | ||||
| CKD | 1 (6.3%) | 10 (10.5%) | 0.280 | 0.596 | ||||
| Previous PCI | 8 (50.0%) | 27 (28.4%) | 2.954 | 0.086 | ||||
| Calcium-blocker | 8 (50.0%) | 36 (37.9%) | 0.839 | 0.360 | ||||
| Beta-blocker | 10 (62.5%) | 63 (66.3%) | 0.089 | 0.766 | ||||
| ACEI/ARB | 10 (62.5%) | 51 (53.7%) | 0.430 | 0.512 | ||||
| Nitrates | 11 (68.8%) | 51 (53.7%) | 1.261 | 0.262 | ||||
| Statins | 15 (93.8%) | 94 (98.9%) | 2.091 | 0.148 | ||||
| EF | 42.9 ± 5.0 | 52.5 ± 6.5 | 5.63 | <0.01 | 0.986 | 0.389 | 4.986 | 0.022 |
| Hcy | 15.32 ± 4.93 | 9.70 ± 3.96 | −5.004 | <0.01 | 0.805 | 0.324 | 3.741 | 0.029 |
MACE: major adverse cardiovascular events. BMI: body mass index; CKD: chronic kidney diseases; PCI: percutaneous coronary intervention; ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; EF: ejection fraction; Hcy: homocysteine.
3.5. Correlation between Hcy and IMR and Changes in LVEDd and LVEF
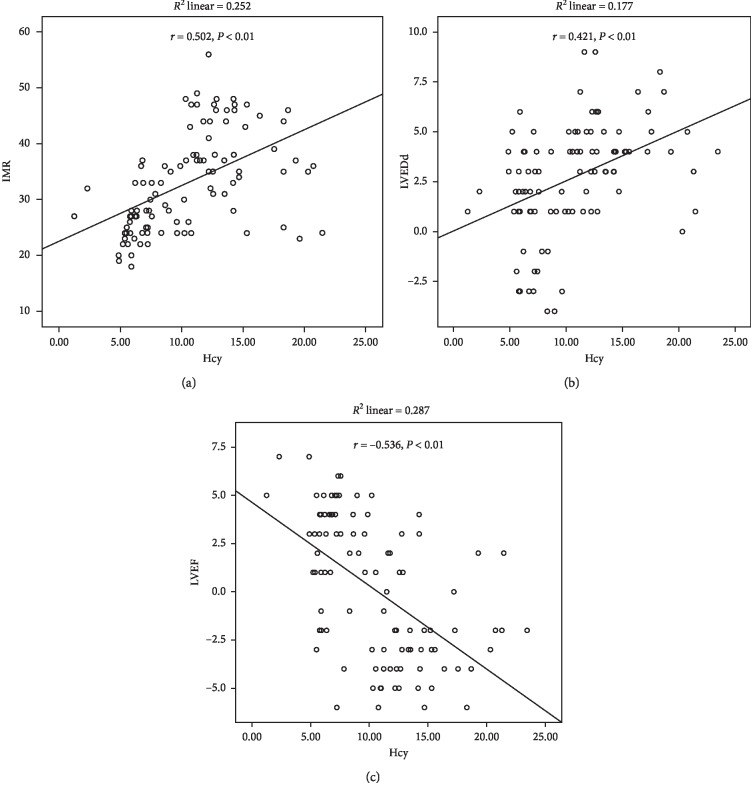
The correlations between the level of Hcy with IMR and the changes in LVEDd and LVEF between one day and three months after PCI were determined using Pearson correlation analysis and multivariate logistic regression analysis. The Hcy level was positively correlated with the IMR (r = 0.502, P < 0.01) and the LVEDd change between one day and three months after PCI (r = 0.421, P < 0.01). However, the Hcy level was negatively correlated with the LVEF change (r = –0.536, P < 0.01; Figure 1 and Table 5).
Figure 1.
Correlation between the homocysteine levels and index of microcirculatory resistance (IMR) (a), the differences in the left ventricular ejection fraction (LVEDd) (b), and the left ventricular ejection fraction (LVEF) (c) between one day and three months after selective PCI of patients.
Table 5.
Correlation between Hcy and IMR and changes in LVEDd and EF.
| r | P | |
|---|---|---|
| IMR | 0.502 | <0.01 |
| LVEDd difference (mm) | 0.421 | <0.01 |
| EF difference (%) | –0.536 | <0.01 |
IMR: index of microvascular resistance; LVEDd: left ventricular end diastolic dimension; EF: ejection fraction.
4. Discussion
In the present study, we evaluated the coronary microcirculatory resistance and short-term prognosis of patients with AMI complicated by HHcy. We found that (1) there was a positive correlation between HHcy and the IMR and LVEDd changes between one day and three months after PCI, (2) there was a negative correlation between HHcy and LVEF changes between one day and three months after PCI, and (3) HHcy was an independent factor for MACEs in patients with AMI after selective PCI. Our study provides a strong rationale for effectively controlling the plasma Hcy levels of patients with AMI before performing the PCI procedure. There are also views that high Hcy was only a concomitant factor of coronary heart disease, and intervention of Hcy did not reduce the risk of cardiovascular and cerebrovascular diseases [15, 16]. The reasons accounting for some findings that treatment of HHcy did improve the prognosis may be attributed to many factors, including a multifactorial disease, age, gender, hypertension, hyperlipidemia, elevated serum creatinine, coffee and alcohol intake, and folic acid and vitamin B12 intake, which may all affect Hcy levels. Therefore, these interfering factors may have effects on the above findings to some degree.
Previous studies have shown that there is a link between the plasma Hcy level and cardiovascular diseases and that this is considered to be an independent predictor of the outcome in patients with AMI. For instance, elevated circulating Hcy levels are associated with increased mortality and overall adverse outcomes of patients with AMI even after successful coronary angioplasty [17]. Additionally, the inclusion of plasma Hcy levels in the Framingham Coronary Heart Disease Risk Score System substantially increases the predictive value of the risk of coronary heart disease and risk of cardiovascular events [18]. Therefore, it has been proposed that Hcy serves as a modifiable cardiovascular risk factor and holds a predictive value for the severity of cardiovascular diseases [19–21]. In line with the above findings, in the present study, we also found a positive correlation between HHcy and MACEs in patients with AMI after PCI. Together, these findings point to the importance of lowering the plasma Hcy in patients with AMI.
In the present study, we found that the IMR was significantly higher in the HHcy group than in the control group. Additionally, we found that the level of Hcy was positively correlated with the IMR, suggesting that patients with AMI with HHcy were prone to more severe coronary microcirculatory dysfunction. No significant differences in LVEDd and LVEF were observed between the two groups on the first day after PCI. This suggests that the patients in both groups had comparable cardiac function prior to PCI. However, three months after PCI, the LVEDd and LVEDd differences were significantly higher and the LVEF changes between one day and three months after PCI were significantly lower in the HHcy group than in the group with normal plasma Hcy levels. These observations indicate that the cardiac function is more severely impaired following selective PCI in AMI patients with HHcy, as evidenced by the observation of elevated circulating hs-CRP levels in AMI patients with HHcy. Although HHcy and elevated hs-CRP were independent risk factors of cardiovascular diseases [22] and the combination of these two features improved the predictive value of the outcome of cerebrovascular diseases [23], it was not clear whether there was any correlation between HHcy and elevated hs-CRP levels. Because hs-CRP is an indicator of an inflammatory response, our findings suggest that HHcy potentially exacerbates AMI-induced inflammation in the heart. Collectively, these findings suggest that the recovery of cardiac function in AMI patients with HHcy three months after PCI was not as good as that observed in control patients. Therefore, we believe that AMI patients with HHcy that miss emergency PCI have a poorer prognosis than those without HHcy, even if they undergo elective PCI at a later date.
Traditional and nontraditional risk factors for coronary heart disease can damage the endothelial function of epicardial vessels and distal microvessels, which may cause endothelial cell-dependent dysfunction, especially in patients with AMI [24]. While PCI has been shown to efficiently restore the blood flow to the infarcted region of the heart, it also increases the epicardial vascular endothelial dysfunction and promotes thrombus detachment, subsequently leading to an increased risk of distal microcirculatory embolization, which in turn results in decreased myocardial perfusion and compromised postoperative rehabilitation in patients with AMI [25]. Several studies have demonstrated that an elevated Hcy level is an independent risk factor for coronary endothelial cell dysfunction [26, 27]. Indeed, the level of plasma Hcy affects the body's coagulation function by injuring vascular endothelial cells, causing inflammatory responses of arterial blood vessels [28]. The present study also revealed that the level of hs-CRP was significantly elevated in the HHcy group. A previous study [29] found that HHcy inhibits the repair of myocardial cells after MI. The main mechanisms through which this occurs are the suppression of stem cell factor-induced repair and increased myocardial interstitial fibrosis, leading to thickening, hardening, and hyaline degeneration of the arteriolar wall. However, several prospective clinical trials have reported no significant correlation between HHcy and atherothrombotic vascular disease [30]. Whether there is a close correlation between HHcy and cardiovascular diseases and whether the lowering of plasma Hcy levels would be clinically helpful remain to be clarified in future studies.
This study had some limitations. For example, this was a single-center retrospective study with a small sample size. Thus, the findings of this study should be further corroborated in large cohort studies in the future. Additionally, this study did not include any investigations into the effect of preangiography medications on the IMR.
In conclusion, we report that HHcy is positively correlated with the IMR and the severity of cardiac dysfunction, and also serves as a prognostic factor for MACEs in patients with AMI after selective PCI.
Data Availability
The data sets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Anderson J. L., Morrow D. A. Acute myocardial infarction. New England Journal of Medicine. 2017;376(21):2053–2064. doi: 10.1056/nejmra1606915. [DOI] [PubMed] [Google Scholar]
- 2.Chen Z. J., Gao R. L. Coronary Heat Disease. Beijing, China: People’s Medical Publishing House; 2002. [Google Scholar]
- 3.den Uil C. A., Lagrand W. K., van der Ent M., et al. Impaired microcirculation predicts poor outcome of patients with acute myocardial infarction complicated by cardiogenic shock. European Heart Journal. 2010;31(24):3032–3039. doi: 10.1093/eurheartj/ehq324. [DOI] [PubMed] [Google Scholar]
- 4.Gutterman D. D., Chabowski D. S., Kadlec A. O., et al. The human microcirculation: regulation of flow and beyond. Circulation Research. 2016;118(1):157–172. doi: 10.1161/circresaha.115.305364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Niccoli G., Burzotta F., Galiuto L., Crea F. Myocardial no-reflow in humans. Journal of the American College of Cardiology. 2009;54(4):281–292. doi: 10.1016/j.jacc.2009.03.054. [DOI] [PubMed] [Google Scholar]
- 6.Fearon W. F., Shah M., Ng M., et al. Predictive value of the index of microcirculatory resistance in patients with ST-segment elevation myocardial infarction. Journal of the American College of Cardiology. 2008;51(5):560–565. doi: 10.1016/j.jacc.2007.08.062. [DOI] [PubMed] [Google Scholar]
- 7.Fearon W. F., Low A. F., Yong A. S., et al. Prognostic value of the index of microcirculatory resistance measured after primary percutaneous coronary intervention. Circulation. 2013;127(24):2436–2441. doi: 10.1161/circulationaha.112.000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim H.-S., Yoon M.-H., Tahk S.-J., et al. Usefulness of the index of microcirculatory resistance for invasively assessing myocardial viability immediately after primary angioplasty for anterior myocardial infarction. European Heart Journal. 2009;30(23):2854–2860. doi: 10.1093/eurheartj/ehp313. [DOI] [PubMed] [Google Scholar]
- 9.Eldibany M. M., Caprini J. A. Hyperhomocysteinemia and thrombosis: an overview. Archives of Pathology & Laboratory Medicine. 2007;131(131):872–884. doi: 10.5858/2007-131-872-HATAO. [DOI] [PubMed] [Google Scholar]
- 10.Lin C., Zhang P., Xue Y., Huang Y., Cui L. Impact of hyperhomocysteinemia on coronary microcirculation in patients referred for elective coronary angiography. International Journal of Clinical and Experimental Medicine. 2017;10:10625–10633. [Google Scholar]
- 11.Kwon S. W., Kim J.-Y., Suh Y. J., et al. Prognostic value of elevated homocysteine levels in Korean patients with coronary artery disease: a propensity score matched analysis. Korean Circulation Journal. 2016;46(2):154–160. doi: 10.4070/kcj.2016.46.2.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hassan A., Dohi T., Miyauchi K., et al. Prognostic impact of homocysteine levels and homocysteine thiolactonase activity on long-term clinical outcomes in patients undergoing percutaneous coronary intervention. Journal of Cardiology. 2017;69(6):830–835. doi: 10.1016/j.jjcc.2016.08.013. [DOI] [PubMed] [Google Scholar]
- 13.Sacco R. L., Adams R., Albers G., et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Stroke. 2006;37(2):577–617. doi: 10.1161/01.str.0000199147.30016.74. [DOI] [PubMed] [Google Scholar]
- 14.Keeley E. C., Velez C. A., O’Neill W. W., Safian R. D. Long-term clinical outcome and predictors of major adverse cardiac events after percutaneous interventions on saphenous vein grafts. Journal of the American College of Cardiology. 2001;38(3):659–665. doi: 10.1016/s0735-1097(01)01420-6. [DOI] [PubMed] [Google Scholar]
- 15.Marti-Carvajal A. J., Sola I., Lathyris D. Homocysteine-lowering interventions for preventing cardiovascular events. The Cochrane Database of Systematic Reviews. 2015;8:p. CD006612. doi: 10.1002/14651858.CD006612.pub4. [DOI] [PubMed] [Google Scholar]
- 16.Qin X., Fan F., Cui Y., et al. Folic acid supplementation with and without vitamin B6 and revascularization risk: a meta-analysis of randomized controlled trials. Clinical Nutrition. 2014;33(4):603–612. doi: 10.1016/j.clnu.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 17.Schnyder G., Flammer Y., Roffi M., Pin R., Hess O. M. Plasma homocysteine levels and late outcome after coronary angioplasty. Journal of the American College of Cardiology. 2002;40(10):1769–1776. doi: 10.1016/s0735-1097(02)02481-6. [DOI] [PubMed] [Google Scholar]
- 18.Veeranna V., Zalawadiya S. K., Niraj A., et al. Homocysteine and reclassification of cardiovascular disease risk. Journal of the American College of Cardiology. 2011;58(10):1025–1033. doi: 10.1016/j.jacc.2011.05.028. [DOI] [PubMed] [Google Scholar]
- 19.Seshadri N., Robinson K. Homocysteine, B vitamins, and coronary artery disease. Medical Clinics of North America. 2000;84(1):215–237. doi: 10.1016/s0025-7125(05)70215-7. [DOI] [PubMed] [Google Scholar]
- 20.Schnyder G., Pin R., Roffi M., Flammer Y., Hess O. M. Association of plasma homocysteine with the number of major coronary arteries severely narrowed. The American Journal of Cardiology. 2001;88(9):1027–1030. doi: 10.1016/s0002-9149(01)01983-x. [DOI] [PubMed] [Google Scholar]
- 21.Ciccarone E., Di Castelnuovo A., Assanelli D., et al. Homocysteine levels are associated with the severity of peripheral arterial disease in type 2 diabetic patients. Journal of Thrombosis and Haemostasis. 2003;1(12):2540–2547. doi: 10.1111/j.1538-7836.2003.00500.x. [DOI] [PubMed] [Google Scholar]
- 22.Saleh N., Samir N., Megahed H., Farid E. Homocysteine and other cardiovascular risk factors in patients with lichen planus. Journal of the European Academy of Dermatology and Venereology. 2014;28(11):1507–1513. doi: 10.1111/jdv.12329. [DOI] [PubMed] [Google Scholar]
- 23.Yan J., Liao J. K., Wang D. Elevated homocysteine and C-reactive protein levels independently predict worsening prognosis after stroke in Chinese patients. Journal of Huazhong University of Science and Technology [Medical Sciences] 2010;30(5):643–647. doi: 10.1007/s11596-010-0557-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Niccoli G., Scalone G., Lerman A., Crea F. Coronary microvascular obstruction in acute myocardial infarction. European Heart Journal. 2016;37(13):1024–1033. doi: 10.1093/eurheartj/ehv484. [DOI] [PubMed] [Google Scholar]
- 25.Valgimigli M., Biondi-Zoccai G., Tebaldi M., et al. Tirofiban as adjunctive therapy for acute coronary syndromes and percutaneous coronary intervention: a meta-analysis of randomized trials. European Heart Journal. 2010;31(1):35–49. doi: 10.1093/eurheartj/ehp376. [DOI] [PubMed] [Google Scholar]
- 26.Woo K. S., Chook P., Lolin Y. I., et al. Hyperhomocyst(e)inemia is a risk factor for arterial endothelial dysfunction in humans. Circulation. 1997;96(8):2542–2544. doi: 10.1161/01.cir.96.8.2542. [DOI] [PubMed] [Google Scholar]
- 27.Salehzadeh H., Mokhtari B., Nematollahi D. Selective electrochemical determination of homocysteine in the presence of cysteine and glutathione. Electrochimica Acta. 2014;123:353–361. doi: 10.1016/j.electacta.2014.01.072. [DOI] [Google Scholar]
- 28.Wang Y., Wang X., Liang X., et al. Inhibition of hydrogen sulfide on the proliferation of vascular smooth muscle cells involved in the modulation of calcium sensing receptor in high homocysteine. Experimental Cell Research. 2016;347(1):184–191. doi: 10.1016/j.yexcr.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Wan J., Deng Y., Guo J., et al. Hyperhomocysteinemia inhibited cardiac stem cell homing into the peri-infarcted area post myocardial infarction in rats. Experimental and Molecular Pathology. 2011;91(1):411–418. doi: 10.1016/j.yexmp.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 30.Kaul S., Zadeh A. A., Shah P. K. Homocysteine hypothesis for atherothrombotic cardiovascular disease. Journal of the American College of Cardiology. 2006;48(5):914–923. doi: 10.1016/j.jacc.2006.04.086. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets generated and analyzed during the current study are available from the corresponding author upon reasonable request.