Abstract
Objectives
We assessed differences in trends, prevalence, and sociodemographic correlates of current smoking among several predominant Hispanic/Latino heritage groups (Puerto Ricans, Dominicans, Central and South Americans, and other Hispanic/Latinos) in New York City (NYC). We additionally compared current smoking prevalence between heritage groups and non-Hispanic/Latino Whites.
Design and Methods
Data from the Community Health Survey, a representative, dual-frame landline/cellphone survey, were analyzed to assess age-adjusted prevalence of current smoking, separately among heritage groups from 2003-2016. Logistic regression was used to estimate odds ratios and 95% CIs for current smoking by Hispanic/Latino heritage group relative to non-Hispanic/Latino Whites in combined 2012-2016 data. Logistic regression was also used to examine correlates of smoking among each heritage group, separately.
Results
Between 2003-2016, current smoking prevalence decreased among all Hispanic/Latinos heritage groups except Puerto Ricans, who had the highest smoking prevalence among all groups examined. Sex-stratified trend analyses showed decreases among all groups except Puerto Rican and other Hispanic/Latino males. In multivariable-adjusted models, relative to non-Hispanic/Latino Whites, there was no association with current smoking among Puerto Ricans, but odds of smoking were lower among all other heritage groups. Female sex was inversely associated with current smoking among all heritage groups, and acculturation was positively associated with smoking among all groups except Central/South Americans. Lower educational attainment was strongly associated with smoking among Puerto Ricans.
Conclusions
Lack of progress in reducing smoking among Puerto Ricans in NYC is concerning. Opportunities for cultural, sex-specific, and other targeted outreach to this community should be explored.
Keywords: Latino Health, Tobacco Use, New York City, Health Disparities, Cigarette Smoking
Introduction
According to recent estimates, the United States Hispanic/Latino population exceeds 58 million, and comprises individuals from at least 21 national origin groups recognized by the US Census Bureau.1 Despite this geographic and cultural diversity, health risk factor and disease prevalence estimates are frequently presented for Hispanic/Latinos as a single category, possibly obscuring within-ethnic health differences by country of origin or heritage group. Evidence of heterogeneity by heritage group has been previously observed for numerous health outcomes among Hispanic/Latinos living in the United States, including mortality from cancer2 and cardiovascular disease,3 and prevalence of chronic conditions like diabetes and hypertension.4-6 Analysis of National Health Interview Survey (NHIS) data found that while self-reported prevalence of multiple chronic health conditions was lower among Hispanic/Latinos overall compared with non-Hispanic/Latino Whites (21% vs 25%, respectively), prevalence among Puerto Ricans (27%) was significantly higher.7
Disparities in health outcomes across Hispanic/Latino subgroups may reflect heterogeneity in the prevalence of risk factors for these conditions, including smoking.8 Overall, Hispanic/Latinos living in the United States have a smoking prevalence that is lower than that of non-Hispanic/Latino Whites; however, significant variation has been observed by heritage group, with the highest prevalence generally observed among Puerto Ricans.9,10 Additionally, while US Hispanic/Latino males have higher smoking prevalence relative to females,9-12 a positive relationship between acculturation and smoking has more consistently been observed for females.13,14 The mechanisms through which acculturation affects smoking behaviors have not been fully elucidated, and may vary by Hispanic/Latino heritage due to each group’s distinct cultural norms (eg, acceptability of smoking among women), patterns of migration, experience of structural racism and targeted tobacco marketing to immigrant communities in the United States.15-17 Relative to females of other Hispanic/Latino heritage groups, stronger associations between acculturation and smoking have generally been observed among those of Mexican heritage,13 though more data are needed on groups that comprise smaller proportions of the US Hispanic/Latino population, including Dominicans.
In New York City (NYC), Hispanic/Latinos are the largest racial/ethnic minority group and account for approximately 29% of the citywide population compared with 18% nationally.18 Since 2002, the city has enacted comprehensive tobacco legislation that has led to overall declines in smoking19; however, recent data suggest that differences in smoking prevalence by Hispanic/Latino heritage group persist.20
Our analysis used data from the NYC Community Health Survey (CHS) to examine the following: 1) trends in smoking prevalence between 2003 and 2016, stratified by Hispanic/Latino heritage group; 2) current smoking prevalence among Hispanic/Latino heritage groups relative to non-Hispanic/Latino Whites; and 3) sociodemographic factors associated with current smoking among predominant Hispanic/Latino heritage groups.
Methods
The NYC CHS is a cross-sectional, dual-frame landline/cellphone survey conducted annually since 2002 by the NYC Department of Health and Mental Hygiene. CHS survey items primarily assessed self-reported health risk factors, behaviors, and outcomes (eg, diabetes, hypertension, and depression). A stratified random sample of approximately 9,000 non-institutionalized, adult NYC residents was used to produce representative citywide estimates and 42 neighborhood estimates. Each neighborhood comprised several adjoining zip codes; these designations were created to approximate NYC Community Planning Districts by the United Hospital Fund, a NYC-based health care non-profit organization.21 From 2002-2008, only households with a landline were included in the survey; a sample of cellphone-only households was added beginning in 2009. Post-stratification weights were constructed to weight each response to the population of the respondents’ neighborhood, based on the respondent’s age, sex, and race/ethnicity (five categories, including Hispanic/Latino overall). Surveys were administered using a computer-assisted telephone interviewing system and were conducted in English, Spanish, Chinese, or Russian. CHS procedures were approved by NYC Department of Health’s Institutional Review Board.
The outcome of interest was current cigarette smoking. Respondents were defined as currently smoking if they reported smoking 100 or more cigarettes in their lifetime, and if they reported that they currently smoked on some or all days. All respondents were asked: “Are you Hispanic or Latino?” Beginning in 2003, respondents who identified as Hispanic/Latino were asked to report which single group best described their Hispanic/Latino origin or ancestry: Puerto Rican; Dominican/Dominican American; Central and South American; Cuban/Cuban American; Mexican/Mexican American; other Latin American; or other Hispanic/Latino. We examined Puerto Rican, Dominican, and Central or South American heritage groups; the weighted sample size corresponding to each group was approximately 420,000, 538,000, and 425,000 NYC residents, respectively. Due to small sample sizes, other heritage groups were combined in a single category termed “other Hispanic/Latino”; respondents of Mexican heritage comprised approximately 60% of this group (weighted sample size: 240,000 NYC residents), and those of Cuban heritage comprised approximately 15% (weighted sample size: 32,000 NYC residents).
Sociodemographic variables of interest included age (18-24, 25-44, 45-64, ≥65 years), sex (male, female), educational attainment (less than high school, high school graduate, some college/technical school, college graduate), household income relative to federal poverty level (FPL) (<200% FPL, ≥200% FPL), and health insurance status (insured, uninsured). Using a proxy measure of acculturation recently employed by Rodriquez et al (2019),22 we cross-classified respondents’ self-reported place of birth (born in the 50 US states or DC, born outside the 50 US states or DC) and survey language (English, language other than English). Respondents born in the 50 US states or DC who answered the survey in English were considered more acculturated, while those born elsewhere who answered in another language were considered less acculturated. A middle category, for respondents who were considered bicultural, was created by combining: 1) respondents born outside the 50 US states or DC and who answered in English; and 2) respondents born in the 50 US states or DC who answered in a language other than English, as the latter group had too few respondents to analyze as its own category. Among Hispanic/Latinos, we excluded three respondents who answered in languages other than English or Spanish.
Statistics
From 2003-2016, we separately estimated age-adjusted prevalence of current smoking among each Hispanic/Latino heritage group for each year and tested for linear trends in prevalence over this period using the POLY statement in SUDAAN’s DESCRIPT procedure. Trend analyses stratified by heritage group and sex were also conducted. Using combined 2012-2016 data to increase statistical power, we separately estimated age-adjusted prevalence of sociodemographic variables among Hispanic/Latino heritage groups and non-Hispanic/Latino Whites.
Odds ratios (ORs) and 95% CIs for current smoking by Hispanic/Latino heritage group relative to non-Hispanic/Latino Whites were estimated using logistic regression using pooled 2012-2016 data. We estimated unadjusted associations, and two multivariable models adjusted for the following covariates selected a priori based on their associations with smoking in the general population: Model 1 included age, sex, household poverty, education, and health insurance status; Model 2 additionally adjusted for the proxy measure of acculturation. Models included all Hispanic/Latino and non-Hispanic/Latino White respondents; dummy variables were created for each Hispanic/Latino heritage group, with non-Hispanic/Latino Whites as the referent.
We used logistic regression models, stratified by heritage group, to examine correlates of current smoking among each group. Unadjusted and multivariable ORs and 95% CIs were estimated for each sociodemographic variable of interest.
Models were restricted to respondents with complete data on included variables. Between 2013-2016, missing values for household income (~11%) were singly imputed using selected demographic and health-related variables; we excluded from multivariable models ~10% of respondents from the 2012 survey (<2% of combined 2012-2016 respondents). Missingness for all other variables was <2%. Of 13,305 Hispanic/Latino respondents from the 2012-2016 cycles, 12,691 (95%) had complete data on all variables and were included in multivariable models (3,668 Puerto Ricans, 4,191 Dominicans, 2,665 Central/South Americans, 2,032 other Hispanic/Latinos; 135 respondents without heritage information were only included in analyses of all Hispanic/Latinos).
Analyses used survey weights to adjust for complex survey design and non-response. Prevalence estimates were age-adjusted based on the 2000 US Census standard population. Analyses were conducted using SAS v.9.4 and SAS-callable SUDAAN v.11.0.1.
All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants included in the study.
Results
Trend Analyses, 2003-2016
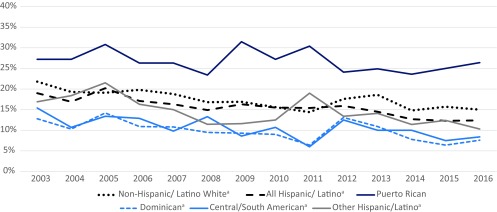
Between 2003 and 2016, prevalence of current smoking among all Hispanic/Latino adults in NYC decreased from 19% to 12% (P for linear trend <.001), compared with 22% to 15% among non-Hispanic/Latino Whites (P <.001) (Figure 1). Prevalence among Dominicans and Central and South Americans in 2003 was 13% and 15%, respectively; in 2016, smoking prevalence among each group was 8% (P<.001 for both). In contrast, Puerto Ricans had smoking prevalence that was higher than other Hispanic/Latino heritage groups and non-Hispanic/Latino Whites, with no significant reductions in prevalence during this period (27% to 25%, P=.10). When stratified by sex, decreases in smoking were observed among Dominican males (16% to 10%, P=.02) and Central and South American males (20% to 10%, P=.03), but not Puerto Rican males (32% to 33%, P=.89) or other Hispanic/Latino males (21% to 18%, P=.08) (data not shown). Among females, decreases in prevalence were observed among all heritage groups, including Puerto Rican females (25% to 20%, P=.002).
Figure 1. Current smoking trends among adult non-Hispanic/Latino Whites and Hispanic/Latinos, by heritage group, in the NYC CHS, 2003-2016.
a. Indicates significant P for test of linear trend.
Due to a high proportion of unreliable estimates, trends for other Hispanic/Latino females are not shown.
Source: NYC Community Health Survey, 2003-2016. Prevalence estimates are age-adjusted to the 2000 US Census Population.
Demographic Characteristics of Hispanic/Latinos in NYC, 2012-2016 Combined
Demographic characteristics of Hispanic/Latinos, overall and by heritage group, and of non-Hispanic/Latino Whites in NYC in 2012-2016 are shown in Table 1. Hispanic/Latinos were generally younger than non-Hispanic/Latino Whites and had a higher proportion of females. Among the heritage groups, Puerto Ricans had the highest proportion aged ≥65 years, while other Hispanic/Latinos had the lowest. Distribution of socioeconomic variables varied across Hispanic/Latino heritage groups, as well as comparing Hispanic/Latinos to non-Hispanic/Latino Whites. For example, Hispanic/Latinos were approximately 10 times more likely than non-Hispanic/Latino Whites to have less than high school education, though variation was observed by heritage group. Among Hispanic/Latinos, Puerto Ricans had the highest proportion classified as more acculturated (born in the 50 states or DC and answered the survey in English), while Central and South Americans had the lowest acculturation rates.
Table 1. Prevalence of demographic and socioeconomic variables by race/ethnicity and Hispanic/Latino heritage group from the NYC CHS, 2012-2016.
| non-Hispanic/Latino White | All Hispanic/Latino | Hispanic/Latino heritage groups | ||||||
| Pa | Puerto Rican | Dominican | Central and South American | Other | Pb | |||
| N, respondents | 16,302 | 13,305 | 3,827 | 4,345 | 2,812 | 2,148 | ||
| Age group | ||||||||
| 18-24 yrs | 8% | 16% | <.001 | 17% | 18% | 13% | 18% | <.001 |
| 25-44 yrs | 37% | 43% | 34% | 37% | 45% | 57% | ||
| 45-64 yrs | 33% | 30% | 32% | 33% | 31% | 20% | ||
| ≥65 yrs | 22% | 11% | 16% | 13% | 11% | 5% | ||
| Sex | ||||||||
| Male | 48% | 45% | .02 | 44% | 41% | 48% | 49% | <.001 |
| Female | 52% | 55% | 56% | 59% | 52% | 51% | ||
| Educational attainment | ||||||||
| Less than high school | 4% | 41% | <.001 | 33% | 42% | 40% | 46% | <.001 |
| High school graduate | 17% | 26% | 28% | 26% | 24% | 26% | ||
| Some college/technical school | 22% | 21% | 27% | 21% | 20% | 15% | ||
| College graduate | 56% | 13% | 13% | 12% | 16% | 13% | ||
| Health insurance status | ||||||||
| Insured | 92% | 75% | <.001 | 88% | 86% | 66% | 57% | <.001 |
| Uninsured | 8% | 25% | 12% | 14% | 34% | 43% | ||
| Household poverty | ||||||||
| <200% federal poverty level | 26% | 72% | <.001 | 63% | 79% | 70% | 75% | <.001 |
| ≥200% federal poverty level | 74% | 28% | 37% | 21% | 30% | 25% | ||
| Acculturationc | ||||||||
| More acculturated | 71% | 26% | <.001 | 63% | 16% | 13% | 18% | <.001 |
| Bicultural | 23% | 18% | 19% | 15% | 20% | 18% | ||
| Less acculturated | 7% | 56% | 18% | 69% | 67% | 64% | ||
Data are age-adjusted to the US 2000 standard population and weighted to NYC adult residential population. Due to rounding, percentages may not sum to 100%.
a. P-values from chi-square tests comparing demographic characteristics among non-Hispanic/Latino White to all Hispanic/Latinos.
b. P values from chi-square test comparing demographic characteristics across Hispanic/Latino heritage groups.
c. More acculturated refers to respondents born in the 50 US states or DC who answered survey in English; bicultural refers to those born in the 50 US states or DC who answered in a language other than English or who were born outside the 50 US states and DC and answered in English; less acculturated refers to those born outside the 50 US states or DC who responded in a language other than English. For Hispanic/Latino respondents, excluded 3 respondents who answered in languages other than Spanish.
Smoking Prevalence Among Hispanic/Latino Heritage Groups Relative to Non-Hispanic/Latino Whites, 2012-2016 Combined
Table 2 shows associations of Hispanic/Latino heritage groups with current smoking. In unadjusted models, odds of current smoking relative to non-Hispanic/Latino Whites were higher among Puerto Ricans, but lower among Dominicans and Central and South Americans. After adjustment for age, sex, health insurance status, household poverty, and educational attainment (Model 1), no significant association with smoking was observed for Puerto Rican heritage relative to non-Hispanic/Latino Whites; however, magnitude of inverse associations increased for all other Hispanic/Latino heritage groups. With further adjustment for place of birth/survey language (Model 2), associations with smoking were unchanged for Puerto Rican heritage, as were the inverse associations with other heritage groups.
Table 2. Odds ratios (OR) and 95%CI for current smoking by Hispanic/Latino heritage group in the NYC CHS, 2012-2016.
| Unadjusted | Model 1 | Model 2 | |||||
| N | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| Non-Hispanic/Latino White | 15,478 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | |||
| Hispanic/Latino | |||||||
| Puerto Rican | 3,668 | 1.63 (1.43, 1.84) | <.001 | 1.11 (.95, 1.28) | .18 | 1.11 (.96, 1.28) | .17 |
| Dominican | 4,191 | .51 (.43, 61) | <.001 | .32 (.26, .39) | <.001 | .47 (.37, .59) | <.001 |
| Central and South American | 2,665 | .63 (.52, .76) | <.001 | .35 (.28, .44) | <.001 | .51 (.40, .65) | <.001 |
| Other | 2,032 | .84 (.70, 1.01) | .07 | .38 (.30, .49) | <.001 | .56 (.43, .72) | <.001 |
Model 1, adjusted for age, sex, health insurance status, household poverty, educational attainment.
Model 2, adjusted for age, sex, health insurance status, household poverty, educational attainment, acculturation.
N reflects number of respondents with complete data who were included in fully adjusted models.
Sociodemographic Correlates of Smoking Among Hispanic/Latino Heritage Groups, 2012-2016 Combined
Table 3 and Table 4 present unadjusted and multivariable-adjusted associations of demographic and socioeconomic variables with smoking, shown separately for Hispanic/Latino heritage groups, and for Hispanic/Latinos overall.
Table 3. Odds ratios (OR) and 95% CI for demographic and socioeconomic variables among all Hispanic/Latinos, Puerto Ricans, and Dominicans in the NYC CHS, 2012-2016.
| All Hispanic/Latino, N=12,691 | Puerto Rican, N=3,668 | Dominican, N=4,191 | ||||||||||
| Unadjusted | Multivariable-adjusteda | Unadjusted | Multivariable-adjusteda | Unadjusted | Multivariable-adjusteda | |||||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| Age group | ||||||||||||
| 18-24 yrs | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||||
| 25-44 yrs | 1.45 (1.15,1.83) | .002 | 2.28 (1.74,2.99) | <.001 | 2.63 (1.77,3.92) | <.001 | 3.48 (2.25,5.40) | <.001 | 1.12 (.68,1.86) | .65 | 1.98 (1.08,3.62) | .03 |
| 45-64 yrs | 1.21 (.96,1.53) | .11 | 2.31 (1.75,3.04) | <.001 | 2.05 (1.39,3.02) | <.001 | 2.68 (1.73,4.15) | <.001 | .90 (.56,1.44) | .65 | 2.49 (1.30,4.77) | .006 |
| ≥65 yrs | .44 (.32,.60) | <.001 | .98 (.67,1.43) | .91 | .47 (.30,.74) | .001 | .67 (.38,1.18) | .17 | .58 (.30,1.11) | .10 | 1.64 (.69, 3.90) | .26 |
| Sex | ||||||||||||
| Male | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||||
| Female | .46 (.40,.53) | <.001 | .47 (.40,.55) | <.001 | .60 (.48,.74) | <.001 | .59 (.47,.74) | <.001 | .65 (.47,.91) | .01 | .70 (.49,.99) | .04 |
| Educational attainment | ||||||||||||
| < than HS | 1.20 (.95,1.52) | .13 | 2.43 (1.85,3.19) | <.001 | 3.61 (2.51,5.21) | <.001 | 5.41 (3.50,8.35) | <.001 | 1.27 (.78,2.08) | .34 | 3.03 (1.65,5.54) | <.001 |
| HS graduate | 1.18 (.93,1.51) | .18 | 1.51 (1.16,1.97) | .002 | 2.91 (2.01,4.20) | <.001 | 2.78 (1.85,4.17) | <.001 | 1.09 (.60,1.98) | .78 | 1.71 (.88,3.34) | .12 |
| Some college/technical school | 1.33 (1.04,1.71) | .02 | 1.37 (1.06,1.79) | .02 | 1.98 (1.34,2.90) | .001 | 1.91 (1.27,2.88) | .002 | 1.55 (.92,2.60) | .10 | 1.73 (1.00,2.99) | .05 |
| College graduate | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||||
| Health insurance status | ||||||||||||
| Insured | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||||
| Uninsured | 1.11 (.93,1.31) | .24 | 1.21 (1.00,1.46) | .05 | 1.23 (.86,1.75) | .26 | .98 (.68,1.41) | .91 | 1.61 (1.07,2.42) | .02 | 1.59 (1.00,2.52) | .049 |
| Household poverty | ||||||||||||
| <200% federal poverty level | .91 (.78,1.06) | .23 | 1.34 (1.12,1.60) | .001 | 1.75 (1.39,2.21) | <.001 | 1.77 (1.35,2.31) | <.001 | .70 (.50,.99) | .04 | 1.03 (.69,1.54) | .88 |
| ≥200% federal poverty level | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||||
| Acculturationb | ||||||||||||
| More acculturated | 3.26 (2.76,3.84) | <.001 | 5.82 (4.69,7.22) | <.001 | 2.67 (1.95,3.66) | <.001 | 3.17 (2.14,4.71) | <.001 | 3.84 (2.60,5.67) | <.001 | 7.68 (4.18,14.1) | <.001 |
| Bicultural | 1.70 (1.40,2.08) | <.001 | 2.68 (2.14,3.36) | <.001 | 2.00 (1.39,2.86) | <.001 | 2.21 (1.49,3.28) | <.001 | 1.76 (1.16,2.67) | .01 | 2.77 (1.71,4.48) | <.001 |
| Less acculturated | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||||
a. Mutually adjusted for all other variables in table.
b. More acculturated refers to respondents born in the 50 US states or DC who answered survey in English; bicultural refers to those born in the 50 US states or DC who answered in a language other than English or who were born outside the 50 US states and DC and answered in English; less acculturated refers to those born outside the 50 US states or DC who responded in a language other than English. For Hispanic/Latino respondents, excluded 3 respondents who answered in languages other than Spanish.
N reflects number of respondents with complete data who were included in multivariable-adjusted models.
Table 4. Odds ratios (OR) and 95% CI for demographic and socioeconomic variables among Central and South Americans, Other Hispanic/Latino heritage groups in the NYC CHS, 2012-2016.
| Central and South American, N=2,665 | Other Hispanic/Latino, N=2,032 | |||||||
| Unadjusted | Multivariable-adjusteda | Unadjusted | Multivariable-adjusteda | |||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| Age group | ||||||||
| 18-24 yrs | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||
| 25-44 yrs | .98 (.57, 1.69) | .95 | 1.04 (.55, 1.99) | .90 | 1.30 (.80, 2.12) | .29 | 1.71 (.94, 3.13) | .08 |
| 45-64 yrs | .66 (.37, 1.18) | .16 | .80 (.39, 1.66) | .56 | 1.26 (.70, 2.26) | .44 | 1.90 (.96, 3.76) | .07 |
| ≥65 yrs | .21 (.08, .51) | .001 | .31 (.11, .89) | .03 | .38 (.18, .83) | .01 | .83 (.33, 2.14) | .71 |
| Sex | ||||||||
| Male | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||
| Female | .36 (.25, .51) | <.001 | .38 (.26, .56) | <.001 | .18 (.12, .27) | <.001 | .19 (.12, .28) | <.001 |
| Education | ||||||||
| < than HS | .64 (.39, 1.04) | .07 | .65 (.36, 1.16) | .14 | .61 (.35, 1.06) | .08 | .88 (.44, 1.74) | .71 |
| HS graduate | .70 (.43, 1.15) | .16 | .66 (.39, 1.12) | .13 | .63 (.36, 1.10) | .11 | .73 (.39, 1.35) | .31 |
| Some college/technical school | 1.01 (.61, 1.66) | .97 | .96 (.56, 1.64) | .88 | 1.02 (.56, 1.88) | .94 | 1.18 (.61, 2.32) | .62 |
| College graduate | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||
| Health insurance status | ||||||||
| Insured | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||
| Uninsured | 1.39 (.97, 2.00) | .07 | 1.26 (.81, 1.96) | .30 | 1.11 (.78, 1.59) | .55 | 1.37 (.83, 2.26) | .21 |
| Household poverty | ||||||||
| <200% federal poverty level | .79 (.55, 1.13) | .20 | 1.05 (.68, 1.61) | .83 | .72 (.48, 1.07) | .10 | 1.04 (.69, 1.57) | .85 |
| ≥200% federal poverty level | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||
| Acculturationb | ||||||||
| More acculturated | 1.72 (1.10, 2.69) | .02 | 1.44 (.77, 2.67) | .25 | 2.17 (1.45, 3.25) | <.001 | 2.99 (1.61, 5.54) | .001 |
| Bicultural | 1.36 (.89, 2.09) | .16 | 1.16 (.68, 1.98) | .58 | 1.09 (.68, 1.75) | .72 | 1.33 (.75, 2.35) | .32 |
| Less acculturated | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||
a. Mutually adjusted for all other variables in table.
b. More acculturated refers to respondents born in the 50 US states or DC who answered survey in English; bicultural refers to those born in the 50 US states or DC who answered in a language other than English or who were born outside the 50 US states and DC and answered in English; less acculturated refers to those born outside the 50 US states or DC who responded in a language other than English. For Hispanic/Latino respondents, excluded 3 respondents who answered in languages other than Spanish.
N reflects number of respondents with complete data who were included in multivariable-adjusted models.
Puerto Ricans
In multivariable models, increased odds of current smoking were observed for Puerto Ricans aged 25-44 years and 45-64 years, relative to those aged 18-24. Females were less likely to currently smoke than males. A strong education gradient was observed, with fewer years of education associated with higher odds of smoking. Compared with college graduates, those with less than high school education were more than five times more likely to smoke, while those with some college or technical school were nearly twice as likely to smoke. Those with household income <200% FPL had higher odds of smoking compared with those with income ≥200% FPL. Puerto Ricans who were classified as more acculturated or bicultural had higher odds of smoking compared with those classified as less acculturated. No association with health insurance status was observed.
Dominicans
Compared with Dominicans aged 18-24 years, those aged 25-44 years and 45-64 years were more likely to currently smoke. Females were less likely than males to currently smoke. Compared with those who graduated college, those with less than high school education had a higher likelihood of smoking. Not having health insurance was also associated with higher likelihood of smoking, while no significant association with household poverty was observed. Compared with respondents who were classified as less acculturated, odds of smoking were higher among Dominicans who were classified as more acculturated or bicultural.
Central and South Americans
Central and South Americans aged ≥65 years were less likely than those aged 18-24 to currently smoke. Lower odds of smoking were observed among females compared with males. No significant associations were observed for educational attainment, health insurance status, household poverty, or acculturation.
Other Hispanic/Latinos
Among other Hispanic/Latinos, odds of smoking were lower among females compared with males. Odds of smoking were approximately threefold higher among respondents classified as more acculturated compared with those classified as less acculturated. No significant associations with current smoking were noted by age, educational attainment, or health insurance status.
Discussion
Using data from a population-based survey of adult NYC residents, we noted differences by Hispanic/Latino heritage group in time trends, prevalence, and correlates of current smoking. Despite decreases in smoking prevalence among Hispanic/Latinos overall between 2003 and 2016, no reductions were observed for Puerto Rican males. Puerto Ricans have a smoking prevalence that is highest among the predominant Hispanic/Latino heritage groups in NYC and higher than non-Hispanic/Latino Whites. In multivariable-adjusted models, the positive association between Puerto Rican heritage and current smoking was attenuated after accounting for sociodemographic variables; however, inverse associations with smoking persisted for Dominican and Central/South American heritage relative to non-Hispanic/Latino White ethnicity. For all heritage groups, female sex was inversely associated with likelihood of current smoking, and proxy measures of acculturation were positively associated with smoking among all heritage groups except Central and South Americans. A strong education gradient was noted for Puerto Ricans, with lower educational attainment associated with higher odds of smoking.
Owing to differential migration and dispersion patterns by national origin, the Hispanic/Latino population in NYC has a different distribution of heritage groups relative to the rest of the United States, allowing us to examine smoking prevalence and correlates among groups who have not been well represented in national survey data, particularly Dominicans. Nationally, Dominicans comprise <4% of the Hispanic/Latino population, compared with nearly 30% in NYC, and nearly 35% of the US Dominican community lives in NYC, primarily in areas of the Bronx and northern Manhattan.1,18 Previously, the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) characterized smoking prevalence in a sample of nearly 1,500 Dominicans residing primarily in the Bronx, between 2008 and 2011. Age-standardized smoking prevalence by sex among Dominican respondents in the HCHS/SOL was 11.0% and 11.7% for males and for females, respectively.10 Though the relationship between degree of acculturation and smoking has not been widely examined among Dominicans living in the United States, analyses of NHIS data have found higher prevalence of ever-smoking among US-born vs foreign-born Dominicans (28% vs 22%)4 and positive associations between acculturation and current smoking among Dominican males.22 Our data show both that the Dominican population in NYC is composed primarily of individuals born outside of the United States who are Spanish-speaking, and that higher markers of acculturation are positively associated with the likelihood of smoking among this heritage group. Taken together, these findings may account for the relatively low smoking prevalence among Dominicans in NYC; however, with increasing acculturation over time and generations, smoking may become a greater health risk among this group.
High prevalence of smoking among Puerto Ricans relative to most other Hispanic/Latino heritage groups has previously been noted,12,23,24 including in the HCHS/SOL, in which 35% and 32.6% of Puerto Rican males and females reported smoking, respectively.10 Similar to our findings, examination of national trends has revealed persistently high prevalence of smoking among Puerto Ricans over time despite reductions among Hispanic/Latinos overall. 25 Comparison of 2002-2005 and 2010-2013 data from the National Survey on Drug Use and Health revealed no significant decreases in current smoking among Puerto Ricans between 2002 and 2013 and reported similar prevalence estimates to those in our study (2002-2005: 31.5%; 2010-2013: 28.5%).9 As we examined trends in NYC during a time period in which the city implemented a suite of comprehensive tobacco control policies, leading to a nearly 40% reduction in adult smoking overall, the lack of progress in reducing smoking among Puerto Rican males is concerning. During the time period examined in our analysis, current smoking prevalence in Puerto Rico was substantially lower than among Puerto Rican New Yorkers and declined from 13.6% in 2003 to 10.6% in 2016.26 Reasons for this disparity have not been well studied, but may include targeted marketing efforts by the tobacco industry to Hispanic/Latino communities,27 and the experience of ethnic discrimination, which has been associated with smoking and nicotine dependence among Hispanic/Latino youth and adults.28,29 Both national7 and NYC-specific20 analyses have previously noted that among all Hispanic/Latino subgroups, Puerto Ricans report the highest prevalence of serious psychological distress, which is associated with higher likelihood of smoking.11 Better understanding of the factors contributing to high smoking prevalence among Puerto Ricans, particularly males, may aid in the design and implementation of more effective cessation programs.
Previous analyses that examined Hispanic/Latinos as a single, pan-ethnic category reported weaker associations between low educational attainment and smoking among this group relative to those observed for non-Hispanic/Latino Whites. Analysis of 2010 NHIS data showed that the prevalence of smoking among those with less than a high school education was fivefold higher than prevalence among those with a college degree among non-Hispanic/Latino Whites (53% vs 10%), but less than twofold higher among Hispanic/Latinos (15% vs 9).30 However, these national findings are not stratified by subgroup and they may primarily reflect individuals of Mexican heritage, who account for approximately two-thirds of the US Hispanic/Latino population.1 Recent analysis of 15 years of pooled NHIS data showed that while educational attainment was significantly inversely associated with current smoking among male immigrants from the combined regions of Mexico, Central American and the Caribbean, this education gradient in smoking was weaker than that observed among US-born males; no significant education gradient for smoking was observed for female immigrants from these regions.31 Few other studies have examined the education gradient in smoking among Hispanic/Latino heritage groups, though stratified analysis of 2000-2006 NHIS data showed that the inverse association between years of education and smoking was stronger among US-born Hispanic/Latinos compared with their foreign-born counterparts and was most pronounced among US-born Puerto Ricans.32 Our analysis did not stratify by country of birth, though we also observed a strong inverse relationship between educational attainment and smoking among Puerto Ricans. Though previous analyses have not examined this association among Dominicans, we also noted that low educational attainment was associated with higher likelihood of smoking in this group.
Study Limitations
Several limitations of our analysis should be noted. First, we did not have adequate sample size to examine smoking among all heritage groups, particularly Mexicans, who account for nearly 15% of the NYC Hispanic/Latino population. Similarly, we were not able to separately examine associations by national origin among Central and South Americans, as these data were not collected. The wording of CHS survey items also did not allow us to evaluate associations among respondents of multiple heritage groups. Though smoking intensity has been shown to vary by Hispanic/Latino heritage group, we were not able to separately examine light and heavy smoking due to small sample sizes. Although we examined a proxy measure of acculturation, we were unable to examine other potentially important markers, including length of time in the US. Lastly, this study of NYC residents may not be generalizable to Hispanic/Latinos living in other US regions.
Conclusion
NYC has been an innovator in tobacco control, beginning with the enactment of the city’s comprehensive Smoke-Free Air Act in 2002 and continuing with the subsequent implementation of pricing regulations and increases in the minimum purchasing age and hard-hitting media campaigns.33 These efforts have been accompanied by a decrease in the citywide smoking prevalence, from 21.5% in 2002 to 13.1% in 2016.19 While prevalence among all Hispanic/Latinos also decreased significantly during this period, this aggregation masks differences by heritage group, including lack of progress among Puerto Rican males. The inability of our comprehensive activities to thus far impact this group bears further reflection. Historically, our media campaigns have been developed with input from low-SES adults who smoke. These sessions have not suggested distinct issues faced by Puerto Rican adults. Activities that target based on cultural, historical, and sex differences may be successful in addressing the continuing disparity seen in this study.
References
- 1. US Census Bureau 2017. American Community Survey 1-Year Estimates: Hispanic or Latino by Specific Origin. Last accessed November 8, 2019 from https://factfinder.census.gov/bkmk/table/1.0/en/ACS/17_1YR/B03001.
- 2. Pinheiro PS, Callahan KE, Siegel RL, et al. Cancer mortality in Hispanic ethnic groups. Cancer Epidemiol Biomarkers Prev. 2017;26(3):376-382. 10.1158/1055-9965.EPI-16-0684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rodriguez F, Hastings KG, Boothroyd DB, et al. Disaggregation of cause-specific cardiovascular disease mortality among Hispanic subgroups. JAMA Cardiol. 2017;2(3):240-247. 10.1001/jamacardio.2016.4653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pabon-Nau LP, Cohen A, Meigs JB, Grant RW. Hypertension and diabetes prevalence among U.S. Hispanics by country of origin: the National Health Interview Survey 2000-2005. J Gen Intern Med. 2010;25(8):847-852. 10.1007/s11606-010-1335-8 10.1007/s11606-010-1335-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Daviglus ML, Talavera GA, Avilés-Santa ML, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308(17):1775-1784. 10.1001/jama.2012.14517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hajat A, Lucas JB, Kington R. Health outcomes among Hispanic subgroups: data from the National Health Interview Survey, 1992-95. Adv Data. 2000;(310):1-14. [PubMed] [Google Scholar]
- 7. Lucas JW, Freeman G, Adams PF. Health of Hispanic adults: United States, 2010–2014. NCHS data brief, no. 251. Hyattsville, MD: National Center for Health Statistics; 2016. [PubMed] [Google Scholar]
- 8. US Department of Health and Human Services The Health Consequences of Smoking-50 Years of Progress: a Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 9. Martell BN, Garrett BE, Caraballo RS Disparities in adult cigarette smoking -United States, 2002-2005 and 2010-2013. MMWR Morb Mortal Wkly Rep. 2016;65(30):753-758. https://doi.org/ 10.15585/mmwr. mm6530a1 PMID:27491017 [DOI] [PubMed]
- 10. Kaplan RC, Bangdiwala SI, Barnhart JM, et al. Smoking among U.S. Hispanic/Latino adults: the Hispanic community health study/study of Latinos. Am J Prev Med. 2014;46(5):496-506. 10.1016/j.amepre.2014.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jamal A, Phillips E, Gentzke AS, et al. Current cigarette smoking among adults – United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(2):53-59. 10.15585/mmwr.mm6702a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pérez-Stable EJ, Ramirez A, Villareal R, et al. Cigarette smoking behavior among US Latino men and women from different countries of origin. Am J Public Health. 2001;91(9):1424-1430. 10.2105/AJPH.91.9.1424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kondo KK, Rossi JS, Schwartz SJ, Zamboanga BL, Scalf CD. Acculturation and cigarette smoking in Hispanic women: A meta-analysis. J Ethn Subst Abuse. 2016;15(1):46-72. 10.1080/15332640.2014.1002878 10.1080/15332640.2014.1002878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bethel JW, Schenker MB. Acculturation and smoking patterns among Hispanics: a review. Am J Prev Med. 2005;29(2):143-148. https://doi.org/ 10.1016/j amepre.2005.04.014 PMID:16005811 [DOI] [PubMed]
- 15. Acevedo-Garcia D, Barbeau E, Bishop JA, Pan J, Emmons KM. Undoing an epidemiological paradox: the tobacco industry’s targeting of US Immigrants. Am J Public Health. 2004;94(12):2188-2193. 10.2105/AJPH.94.12.2188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rodriguez CJ, Allison M, Daviglus ML, et al. ; American Heart Association Council on Epidemiology and Prevention; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Cardiovascular and Stroke Nursing . Status of cardiovascular disease and stroke in Hispanics/Latinos in the United States: a science advisory from the American Heart Association. Circulation. 2014;130(7):593-625. 10.1161/CIR.0000000000000071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26(1):367-397. 10.1146/annurev.publhealth.26.021304.144615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. US Census Bureau 2017. American Community Survey 1-Year Estimates: Hispanic or Latino by Specific origin, New York City, New York. Last accessed November 8, 2019 from https://factfinder.census.gov/faces/tableservices/jsf/pages/ productview.xhtml?pid=ACS_17_1YR_ B03003&prodType=table.
- 19. New York City Department of Health and Mental Hygiene EpiQuery: NYC Interactive Health Data System [Community Health Survey 2002-2016]. Last accessed November 8, 2019 from http://nyc.gov/health/epiquery.
- 20. Greer S, Naidoo M, Hinterland K, Archer A, Lundy De La Cruz N, Crossa A, Gould LH Health of Latinos in NYC. 2017;1-32. Last accessed November 8, 2019 from https://www1.nyc.gov/assets/doh/downloads/pdf/episrv/2017-latino-health.pdf
- 21.New York City United Hospital Fund (UHF) Neighborhoods and NYC Zip Code Areas. Last accessed November 8, 2019 from https://www1.nyc.gov/assets/doh/downloads/pdf/survey/uhf_map_100604.pdf.
- 22. Rodriquez EJ, Fernández A, Livaudais-Toman JC, Pérez-Stable EJ. How does acculturation influence smoking behavior among Latinos? The role of education and national background. Ethn Dis. 2019;29(2):227-238. 10.18865/ed.29.2.227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Haynes SG, Harvey C, Montes H, Nickens H, Cohen BH. Patterns of cigarette smoking among Hispanics in the United States: results from HHANES 1982-84. Am J Public Health. 1990;80(suppl):47-53. 10.2105/AJPH.80.Suppl.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Caraballo RS, Yee SL, Gfroerer J, Mirza SA. Adult tobacco use among racial and ethnic groups living in the United States, 2002-2005. Prev Chronic Dis. 2008;5(3):A78. [PMC free article] [PubMed] [Google Scholar]
- 25. Blanco L, Garcia R, Pérez-Stable EJ, et al. National trends in smoking behaviors among Mexican, Puerto Rican, and Cuban men and women in the United States. Am J Public Health. 2014;104(5):896-903. 10.2105/AJPH.2013.301844 10.2105/AJPH.2013.301844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health BRFSS Prevalence & Trends Data. Last accessed November 8, 2019 from https://www.cdc.gov/brfss/brfssprevalence/.
- 27. Iglesias-Rios L, Parascandola M. A historical review of R.J. Reynolds’ strategies for marketing tobacco to Hispanics in the United States. Am J Public Health. 2013;103(5):e15-e27. 10.2105/AJPH.2013.301256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kendzor DE, Businelle MS, Reitzel LR, et al. Everyday discrimination is associated with nicotine dependence among African American, Latino, and White smokers. Nicotine Tob Res. 2014;16(6):633-640. 10.1093/ntr/ntt198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Unger JB, Soto DW, Baezconde-Garbanati L. Trajectories of perceived discrimination from adolescence to emerging adulthood and substance use among Hispanic youth in Los Angeles. Addict Behav. 2016;53:108-112. 10.1016/j.addbeh.2015.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Margerison-Zilko C, Cubbin C. Socioeconomic disparities in tobacco-related health outcomes across racial/ethnic groups in the United States: National Health Interview Survey 2010. Nicotine Tob Res. 2013;15(6):1161-1165. 10.1093/ntr/nts256 [DOI] [PubMed] [Google Scholar]
- 31. Pampel F, Khlat M, Bricard D, Legleye S. Smoking among immigrant groups in the United States: Prevalence, education gradients, and male-to-female ratios. Nicotine Tob Res. 2019;ntz022. 10.1093/ntr. Accessed November 8, 2019. [DOI] [PubMed] [Google Scholar]
- 32. Kimbro RT, Bzostek S, Goldman N, Rodríguez G. Race, ethnicity, and the education gradient in health. Health Aff (Millwood). 2008;27(2):361-372. 10.1377/hlthaff.27.2.361 [DOI] [PubMed] [Google Scholar]
- 33. Kilgore EA, Mandel-Ricci J, Johns M, et al. Making it harder to smoke and easier to quit: the effect of 10 years of tobacco control in New York City. Am J Public Health. 2014;104(6):e5-e8. 10.2105/AJPH.2014.301940 [DOI] [PMC free article] [PubMed] [Google Scholar]