Supplemental Digital Content is Available in the Text.
Key Words: acetabular fracture, pararectus approach, ilioinguinal approach, radiological results, clinical results
Objectives:
To evaluate radiological fracture reduction and clinical results using the pararectus approach in complex acetabular fractures involving the anterior column.
Design:
Retrospective database analysis of prospectively collected data.
Setting:
Level 1 trauma center.
Patients/Participants:
61 patients (48 male and 13 female) with a median age of 55 (range 17–91) years were included. According to the chosen surgical approach, they were divided into 2 groups. The P-group included 43 patients, among them 32 male and 11 female patients with a median age of 55 (range 17–90) years. Eighteen patients [16 male, 2 female; median age: 53 (range 23–91) years] were treated through the ilioinguinal approach (I-group).
Intervention:
Anterior surgical procedures through the pararectus or the ilioinguinal approach.
Main Outcome Measured:
Reduction results were rated according to the modified Matta criteria using a measurement protocol of hip joint gaps and steps in computed tomography scans. Operation time, complications, and clinical outcomes median one year postoperatively were compared.
Results:
In the pararectus group reduction was anatomical in 21 out of 40 analyzed patients (52.5%), imperfect in 11 patients (27.5%), and poor in 8 patients (20%). The mean joint step reduction was 3.7 mm, and the mean joint gap reduction was 12.1 mm. In the ilioinguinal group reduction was anatomical in 9 out of 18 patients (50%), imperfect in 4 patients (22%), and poor in 5 patients (28%). The mean joint step reduction was 1 mm, and the mean joint gap reduction was 7 mm. Operation time was significantly shorter in the P-group (mean: 49 minutes; P < 0.001).
Conclusions:
This study indicates that acetabular fracture reduction using the pararectus approach is at least comparable with the ilioinguinal approach independent of patients' age. A relevant advantage of the pararectus approach was seen in a significantly shorter operation time.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
INTRODUCTION
In acetabular fracture management, the choice of the appropriate approach is based on a correct fracture classification and on the evaluation of the extent of dislocation.1–4 Fracture reduction without an articular step is crucial for good functional outcome. Using the classical ilioinguinal approach, the anterior column can be addressed directly.5 However, limitations are clearly given for pathologies beyond the arcuate line. In this regard, the quadrilateral plate can only be addressed indirectly. The modified Stoppa approach overcomes some of these limitations.6 Introduction of the pararectus approach opened a new option to surgically stabilize acetabular fractures involving the quadrilateral plate allowing for better visualization of the acetabular dome (see Figure, Supplemental Digital Content 1, http://links.lww.com/JOT/A847; Figure, Supplemental Digital Content 2, http://links.lww.com/JOT/A848).7 Options to use the pararectus approach have been seen in anterior column with or without posterior hemitransverse, both column, T-shaped, transverse, and anterior wall fractures.
Despite the obvious practical advantages in visualization and reduction of acetabular fractures involving the anterior column (Fig. 1), there are only little data available on whether using the pararectus approach results in similar fracture reduction compared with the ilioinguinal approach. In this regard, only one study providing radiological results preoperatively and postoperatively comparing the pararectus and the ilioinguinal approach outside the research group by the first describer has been published.7,8
FIGURE 1.
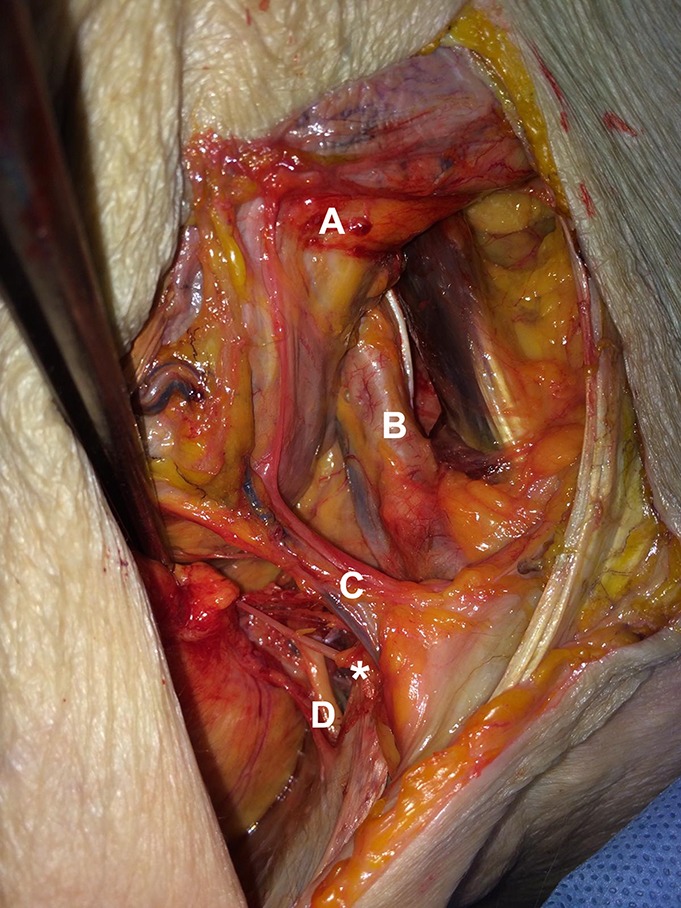
Postmortem surgical exposure developed through the pararectus approach lateral to the rectus abdominis muscle: mobilized peritoneum (A), external iliac vessels (B), vas deferens and inferior epigastric vessels (C), corona mortis (*), and obturator nerve and vessels (D). Editor's Note: A color image accompanies the online version of this article.
The aim of the current study was to evaluate acetabular fracture reduction using the pararectus approach compared to the ilioinguinal approach including measurement of the hip joint step and gap preoperatively versus postoperatively. The analysis included further relevant data such as mechanism of trauma, surgical details, complications, and the need for total hip arthroplasty (THA) due to posttraumatic arthritis as a primary indicator for short-term outcome.
PATIENTS AND METHODS
This retrospective analysis of prospectively collected data was conducted according to ICMJE guidelines and has been registered with the German Clinical Trials Register (ID: DRKS00011308). Table 1 provides an overview of patients' data. All patients with acetabular fractures who underwent anterior surgical procedures through the pararectus approach and the ilioinguinal approach between January 2013 and December 2015 at a single Level 1 trauma center were included (n = 296). One-hundred ten patients were treated surgically using anterior pelvic approaches by 3 senior surgeons with experience of more than 20 years each in pelvic surgery. Patients were assigned to the pararectus approach group (P-group) or to the ilioinguinal approach group (I-group) based on surgeon's experience and decision. Because of fracture classification, the ideal approach to surgically manage the fracture was chosen. Only patients with complete follow-up data sets were included in this study. Finally, 61 patients (48 male and 13 female) with a median age of 55 (range 17–91) years were included. According to the chosen surgical approach, they were divided into 2 groups. The P-group included 43 patients, among them 32 male and 11 female patients with a median age of 55 (range 17–90) years. Eighteen patients [16 male, 2 female; median age: 53 (range 23–91) years] were treated through the ilioinguinal approach (I-group). This group included one patient who had received primary insufficient stabilization of the acetabular fracture elsewhere. General patients' demographic data including mechanism of injury, fracture classification, surgical details, and complications were evaluated. Acetabular fractures were classified according to the Judet and Letournel classification as well as to the OTA/AO pelvic classification.9,10 Complications were noted intraoperatively and postoperatively. The following surgical details were listed: time interval between trauma and surgical intervention, operation time, and fixation method. One year after surgery, all patients were evaluated in terms of a need for secondary THA according to post-traumatic joint arthritis. The study was not designed to investigate secondary THA in a subgroup analysis.
TABLE 1.
Patients' Data Overview

Measurement Parameters
To analyze fracture reduction, the joint step and joint gap were measured in preoperative and postoperative computed tomography (CT) scans. Therefore, a fracture-specific 3D reconstruction including the weight-bearing region of the acetabulum was performed in each case. The joint gap was measured in a circular area which correlated with the largest circumference of the femoral head (Fig. 2). The middle of the circle was formed by the tip of the acetabular dome. The measurement of the joint step was performed in the transversal plane and was defined to be the largest dehiscence in a 90 degrees angular position in relation to the main fracture line (Fig. 3).
FIGURE 2.

Measurement of the hip head diameter in the transversal plane in the CT scan.
FIGURE 3.

Measurement of the largest joint gap at the tip of the acetabular dome in the transversal plane of the CT scan within a circle with the size of the hip head diameter.
In 11 cases of the P-group and in 3 cases of the I-group, the preoperative step had to be measured outside the previously described circle because fracture dehiscence was larger than the circle and therefore located outside the circumference. Starting from the tip of the acetabular dome, the largest step was measured in CT scans and recorded for further analysis. The joint step was measured in the coronal and sagittal planes: In the sagittal plane until 60 degrees to the dorsal side and until 45 degrees to the frontal side (see Figure, Supplemental Digital Content 3, http://links.lww.com/JOT/A849), and in the coronal plane completely to the lateral side and until 45 degrees to the medial side (see Figure, Supplemental Digital Content 4, http://links.lww.com/JOT/A850). Angles were measured related to a straight line through the tip of the acetabular dome that had a 90 degrees angle to a straight line through both tips of the acetabular domes. Those areas scanned for the largest step are corresponding to the main weight-bearing area of the acetabulum as indicated elsewhere.11
Statistical Analysis
Statistical data analysis for preoperative and postoperative CT measurements and duration of surgery was performed using SPSS version 19.0 (SPSS Inc, Chicago, IL). Testing for normality was performed using Kolmogorov–Smirnov test. Because normal distribution of each measurement parameter was not confirmed for both groups, the Mann–Whitney test was used for between-group comparisons. The level of significance was set at P < 0.05.
Ethical Approval
The study was approved prospectively and provided by the institutional as well as by the national ethics committee (Bavarian State Chamber of Physicians; ID 16043). All procedures performed in this study involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments.
RESULTS
Preoperative Results
The most common accidents leading to acetabular fracture were falls of less than 3 m, followed by traffic accidents. In total, 28 both column fractures (OTA/AO type C1), 11 anterior column with posterior hemitransverse (ACPHT) fractures (OTA/AO type B3), 10 T-shaped fractures (OTA/AO type B2), 6 transverse fractures (OTA/AO type B1-1), and 6 anterior column fractures (OTA/AO type A3-2) were taken into account. In the P-group, the median range of time between injury and surgery was 4.8 (range 0–19) days for patients secondarily transferred from other hospitals and 3.6 (range 0–9) days for patients with primary admission to our setting. In the I-group, median time interval between injury and surgery was 5 (range 0–14) days for transferred patients and 3.8 (range 3–5) days for patients with primary admission (P > 0.05).
Intraoperative Results
The mean operation time was 2 hours and 32 minutes in the P-group (n = 37) and 3 hours and 21 minutes in the I-group (n = 17). This revealed a highly statistically significant difference of 49 minutes between both approaches (P < 0.001). Data from patients without additional surgical treatment in the same session were used for this analysis only. In the P-group, fracture fixation using 2 plates was performed in 28 patients. The remaining 15 patients obtained one or three 3.5-mm small fragment plates and optionally additional lag screw fixation. In the I-group, one small fragment plate was applied in all patients, whereas in 3 patients, auxiliary cerclage wiring was used.12
CT Measurements
In the P-group, the preoperative fracture step was measured in 41 patients. In 2 transferred patients with imaging from other hospitals, the quality of the external radiographic CT data sets did not allow for 3D reconstructions as needed for correct analysis. The mean step was 5.4 ± 4 mm. The mean joint gap was 14 ± 8.5 mm while, in 12 cases, one measuring point was outside the above-described circle (see Patients and Methods).
In the I-group, the mean preoperative joint step was 3.1 mm, and in 3 cases, measurement was aggravated due to a large joint gap. The mean joint gap was 9.8 ± 6.8 mm and was measured in 3 cases outside the previously described circle (see Patients and Methods). Data of 17 of the 18 patients were used, as for one patient, a paper print of the preoperative CT was available only, which could not be analyzed digitally.
Forty out of 43 patients in the P-group underwent a postoperative CT scan. The mean joint step was 1.7 ± 2.2 mm with a mean reduction of 3.7 mm and the gap 1.9 ± 2.5 mm with a mean reduction of 12.1 mm. After the modified Matta criteria, reduction was anatomical in 21 patients (52.5%), imperfect in 11 patients (27.5%), and poor in 8 patients (20%). Twenty-three patients had postoperative X-ray images demonstrating no dislocation of the fixation material.
In the I-group, 18 patients obtained a postoperative CT scan. The mean joint step was 2.1 ± 2.6 mm with a mean reduction of 1 mm, and the gap was 3.0 ± 4.9 mm with a mean reduction of 7 mm. According to the modified Matta criteria, reduction was anatomical in 9 patients (50%), imperfect in 4 patients (22.2%), and poor in 5 patients (27.8%). Ten patients received postoperative X-rays that did not demonstrate any dislocation of the fixation material.
Fig. 4 illustrates the radiological gap and step values preoperatively and postoperatively comparing both study groups. Comparison of treatment groups demonstrated no statistically significant differences regarding both, joint step and joint gap (P > 0.05).
FIGURE 4.

Radiographic distances in patients treated through the pararectus approach (P-group) and the ilioinguinal approach (I-group). White: preoperative gap; shaded: preoperative step; gray: postoperative gap; dotted: postoperative step.
Complications
Intraoperative complications in the P-group were as follows: One case of accidental lesion of the peritoneum without any injury to intra-abdominal structures and one injury of the iliac vein. In both cases, lesions were immediately addressed by simple repair and without any consequences for the patient during further clinical course. Postoperatively, 4 patients survived acute lung embolism despite heparin prophylaxis, and one patient developed an acute ileus with the need for protective stoma surgery. No deep wound infection was seen in this group.
In the I-group, there was one case of an intraoperative lung embolism based on deep vein thrombosis. Postoperatively, there was one other patient suffering lung embolism, despite adequate heparin prophylaxis. One 73-year-old male patient with an ACPHT fracture showed signs of postoperative deep wound infection caused by Staphylococcus epidermidis. After fixation material removal, femoral head resection, microbial eradication, and finally THA were necessary. Alcohol abuse was detected as relevant risk factor for this patient.
Within 1 year after trauma, THA was necessary in 4 patients of the P-group (2 ACPHT fractures, 2 both column fractures). Median age in these patients was 76 (range 72–80) years.
DISCUSSION
In reconstructive acetabular surgery, sufficient intraoperative visualization of key structures of the acetabulum is mandatory. In addition, the necessity to fix both columns in comminuted acetabular fractures is another surgical challenge that has been addressed insufficiently through classical approaches. To overcome these shortcomings, the pararectus approach has been established.7,13 However, there is only one more study reporting radiological and clinical results after acetabular fracture fixation using the pararectus approach other than the results provided by the describer.8
Radiological Results
The main target of acetabular fracture fixation is anatomical joint reconstruction according to the modified Matta criteria.14,15 The remaining fracture step is considered with <1 mm as anatomical, with 1–3 mm as imperfect and with >3 mm as poor. This classification represents one of the main prognostic factors for the need of THA.16 In the current study, we were able to demonstrate that there was no relevant difference between the ilioinguinal and the pararectus approach in terms of reduction results according to the modified Matta criteria. This was despite the fact that patients who underwent surgery in our setting through the pararectus approach demonstrated a higher degree of preoperative fracture dislocation compared with those treated through the ilioinguinal approach. Our data may indicate that the pararectus approach is at least equal in terms of reduction results compared with the ilioinguinal approach and can even be used in cases with significant fracture dislocation. This is supported by the results of Märdian et al8 who indicated a significantly better reduction of the joint gap using the pararectus approach while having an equal rate of complications. However, the radiological reduction results provided by Märdian et al8 can only be compared limitedly with the results of the current study. They also included patients who obtained an additional fixation using the Kocher Langenbeck approach (17.9% in the I-group, 20.5% in the P-group). In addition, they did not focus particularly on the weight-bearing area of the acetabulum in their radiographic evaluation.
Comparing the percentage of imperfect and poor results with the original publications of Letournel,14 at first, it appears that the results of the current study are not as optimal. However, there are several explanations for this: First of all, Letournel used conventional X-rays to evaluate fracture reduction radiologically. In the current study, CT scans and particularly an exact protocol including 3D reconstructions of the relevant areas of the acetabulum were used, clearly providing greater sensitivity in detecting postoperative gaps and steps compared with conventional 2D films. Furthermore, Letournel's series included comminuted fracture configurations in 80% of all cases and thereby ACPHT fractures and both column fractures in particular. For these fracture patterns, Letournel reported a rate of perfect fracture reduction of 85% and 73%, respectively. In our series, comminuted fracture configurations accounted for as high as 88% of all cases. Among them ACPHT fractures and both column fractures were found in 72% of patients. Fracture reduction using the pararectus approach lead to anatomical results even in these displaced fracture patterns in more than 50%. In summary, positive effects of a quick and anatomical fracture reduction are most likely due to clear visualization using the pararectus approach with good access to the acetabular dome, the quadrilateral plate, and the option to indirectly place screws to fix the posterior column in various directions.
Clinical Results
In 2014, Keel et al13 published clinical results after acetabular fracture fixation through the pararectus approach and achieved a Harris hip score of 88 points which is graded as a good functional result for daily activities, and 9 points for the modified Merle d'Aubignè score that is a medium absolute score. Nevertheless, there was a lack of comparison with other approaches. In addition, our recent studies demonstrated good to excellent functional results.5 Another positive effect of the pararectus approach is the absence of inguinal herniation, which has been reported for the ilioinguinal approach.17 Even injuries to the lateral cutaneous nerve due to traction caused by hooks using the ilioinguinal approach can be prevented by the pararectus approach keeping the ilioinguinal canal intact.18 However, through the pararectus approach the obturator nerve may be affected, which already has been described by the Bernese group.12 In a relevant earlier study which included all types of displaced acetabular fractures independent of the approach, the need for THA after nonanatomical fracture reduction 2 years postoperatively was 70%–80%.19 But still, there is no general indication for primary THA in acetabular fractures.20 The decision for primary THA should mainly depend on bone quality, on additional injury of the femoral neck, on pathological fractures, and on preexisting arthritis of the acetabular joint.21 Comparing the fractures resulting in secondary need for THA, 50% ACPHT fractures and 50% both column fractures occurred in our collective.
In the current study, a significantly shorter operation time could be achieved using the pararectus approach compared with the ilioinguinal approach. One may criticize that shorter operation time through the pararectus approach was achieved due to a more frequent use of this approach. To counter this, patients were treated by 3 senior surgeons with experience in pelvic surgery of more than 20 years each. These surgeons performed the ilioinguinal approach among others including Matta's learning curve long before the pararectus approach was introduced.2 Therefore, the significant difference in operation time probably is not a question how frequently an approach is used. Although in the current study the difference in operation time was significant, it might be concluded that this results in less stress for the patient gaining quicker fracture reduction and shorter duration of general anesthesia. This is even more important since there are an increasing number of older patients suffering comminuted acetabular fracture configurations involving the anterior column during recent decades.22 With the rising number of elderly patients and the growing number of osteoporotic fractures, it was pointed out recently that there is an increasing population of patients requiring stabilization of the acetabulum for short-term THA to follow.23 In these patients, a minimally invasive surgical approach seems beneficial, and due to the planned secondary THA anatomical fracture reduction might not be necessarily the primary goal.
Overall, the pararectus approach is an anatomical approach but implies the risk of perforating the peritoneum potentially leading to damage of intraperitoneal organs.24 In the current study, one case of accidental perforation of the peritoneum and one accidental lesion of the iliac vein occurred.
In principle, our data support earlier recommendations to use the pararectus approach in surgical acetabular fracture management.8 While in the study provided by Märdian et al8 the key aspect was a better reduction of the fracture gap, in the current study the reduced operation time using the pararectus approach was superior compared with the ilioinguinal approach. In our setting, the pararectus approach is now considered as gold standard with more than 80% of the fractures treated through this access.
CONCLUSIONS
In conclusion, the results of this study demonstrate that acetabular fracture reduction using the pararectus approach is at least comparable with the ilioinguinal approach independent of patients' age. Furthermore, the use of the pararectus approach can be recommended in fractures with a significantly larger fracture gap. Besides, a relevant advantage of the pararectus approach is seen in a significantly shorter operation time compared with the ilioinguinal approach.
Supplementary Material
Footnotes
L. Wenzel and C. von Rüden contributed equally to this work.
The authors report no conflict of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jorthotrauma.com).
REFERENCES
- 1.Matta JM, Anderson LM, Epstein HC, et al. Fractures of the acetabulum. A retrospective analysis. Clin Orthop Relat Res. 1986;205:230–240. [PubMed] [Google Scholar]
- 2.Matta JM, Mehne DK, Roffi R. Fractures of the acetabulum. Early results of a prospective study. Clin Orthop Relat Res. 1986;205:241–250. [PubMed] [Google Scholar]
- 3.Matta JM, Merritt PO. Displaced acetabular fractures. Clin Orthop Relat Res. 1988;230:83–97. [PubMed] [Google Scholar]
- 4.Routt ML, Jr, Swiontkowski MF. Operative treatment of complex acetabular fractures: combined anterior and posterior exposures during the same procedure. J Bone Joint Surg Am. 1990;72:897–904. [PubMed] [Google Scholar]
- 5.von Rüden C, Wenzel L, Becker J, et al. The pararectus approach for internal fixation of acetabular fractures involving the anterior column: evaluating the functional outcome. Int Orthop. 2019;43:1487–1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Verbeek DO, Ponsen KJ, van Heijl M, et al. Modified Stoppa approach for operative treatment of acetabular fractures: 10-year experience and mid-term follow-up. Injury. 2018;49:1137–1140. [DOI] [PubMed] [Google Scholar]
- 7.Keel MJ, Ecker TM, Cullmann JL, et al. The pararectus approach for anterior intrapelvic management of acetabular fractures: an anatomical study and clinical evaluation. J Bone Joint Surg. 2012;94:405–411. [DOI] [PubMed] [Google Scholar]
- 8.Märdian S, Schaser KD, Hinz P, et al. Fixation of acetabular fractures via the ilioinguinal versus pararectus approach: a direct comparison. Bone Joint J. 2015;97-B:1271–1278. [DOI] [PubMed] [Google Scholar]
- 9.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. preliminary report. J Bone Joint Surg Am. 1964;46:1615–1646. [PubMed] [Google Scholar]
- 10.Marsh JL, Slongo TF, Agel J, et al. Fracture and Dislocation Classification Compendium - 2007: Orthopaedic Trauma Association Classification, Database and Outcomes Committee. J Orthop Trauma. 2007;21(suppl 10):S1–S163. [DOI] [PubMed] [Google Scholar]
- 11.Yoshida H, Faust A, Wilckens J, et al. Three-dimensional dynamic hip contact area and pressure distribution during activities of daily living. J Biomech. 2006;39:1996–2004. [DOI] [PubMed] [Google Scholar]
- 12.Erichsen CJ, von Rüden C, Hierholzer C, et al. Auxiliary cerclage-wiring in internal fixation of displaced acetabular fractures. Unfallchirurg. 2015;118:35–41. [DOI] [PubMed] [Google Scholar]
- 13.Keel MJ, Tomagra S, Bonel HM, et al. Clinical results of acetabular fracture management with the pararectus approach. Injury. 2014;45:1900–1907. [DOI] [PubMed] [Google Scholar]
- 14.Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993;292:62–76. [PubMed] [Google Scholar]
- 15.Griffin DB, Beaulé PE, Matta JM. Safety and efficacy of the extended iliofemoral approach in the treatment of complex fractures of the acetabulum. J Bone Joint Surg Br. 2005;87:1391–1396. [DOI] [PubMed] [Google Scholar]
- 16.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–1645. [PubMed] [Google Scholar]
- 17.Rommens PM, Hessmann MH. Acetabulum fractures. Unfallchirurg. 1999;102:591–610. [DOI] [PubMed] [Google Scholar]
- 18.Helfet DL, Schmeling GJ. Management of complex acetabular fractures through single nonextensile exposures. Clin Orthop Relat Res. 1994;305:58–68. [PubMed] [Google Scholar]
- 19.Tannast M, Najibi S, Matta JM. Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg Am. 2012;94:1559–1567. [DOI] [PubMed] [Google Scholar]
- 20.Sermon A, Broos F, Vanderschot P. Total hip replacement for acetabular fractures. Results in 121 patients operated between 1983 and 2003. Injury. 2008;39:914–921. [DOI] [PubMed] [Google Scholar]
- 21.De Bellis UG, Legnani C, Calori GM. Acute total hip replacement for acetabular fractures: a systematic review of the literature. Injury. 2014;45:356–361. [DOI] [PubMed] [Google Scholar]
- 22.Ferguson TA, Patel R, Bhandari M, et al. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br. 2010;92:250–257. [DOI] [PubMed] [Google Scholar]
- 23.Perl M, von Rüden C, Wenzel L, et al. Acetabular fractures – when and how to perform hip replacement? What are the outcomes? Trauma Berufskrankh. 2017;19:141–147. [Google Scholar]
- 24.Ponsen KJ, Joosse P, Schigt A, et al. Internal fracture fixation using the Stoppa approach in pelvic ring and acetabular fractures: technical aspects and operative results. J Trauma. 2006;61:662–667. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


