Abstract
Premenstrual syndrome (PMS) encompasses a vast array of physical and psychological symptoms. Of the herbal supplements mentioned for remedy PMS symptoms, chamomile used as an effective herbal medicine. The overall purpose of this review was to determine the efficacy of chamomile on the treatment PMS. An extensive research review using Web of Science, the Cochrane Controlled Trials Register database, PubMed, Chinese Biomedical Database (CBM), CINAHL, China National Knowledge Infrastructure (CNKI), Psych INFO, Social Science Research Network, SID, Google Scholar, Iran Doc, Magiran and Iran Medex. Eligible studies were identified from English and Persian databases, published between 1990 and 2019. Studies were screened independently by two researchers who performed the data extraction. Of Twenty-seven studies identified, Eight RCTs met our inclusion criteria. Chamomile has been used to treat PMS relief because of therapeutic properties such as anti-inflammatory effects (Chamazulene and α-Bisabolol); anti-spasmodic effects (Apigenin, Quercetin, and Luteolin, Metoxicomarin, Matrisin, and Phytoestrogens); anti-anxiety effects (Glycine, Flavonoid). The results of this review show that Chamomile is effective for the treatment of PMS. Based on these results, we believe that Chamomile can be used as good herbal medicine to treat in women with PMS.
Keywords: chamomile, premenstrual syndrome, herbal medicine
1. Introduction
PMS is a collection of mostly physical symptoms or a state of negative mood or behavior [1]. PMS may affect women of any age, although it’s most common among women between their late 20s and early 40s [2]. The prevalence of PMS was estimated at about 30% and 50% [3]. The core symptoms of PMS are anxiety and depression and it is important to distinguish cyclical reports from a manifestation of clinical or trait anxiety and depression which may be exacerbated Premenstrually [4]. When symptoms are perceived to be sufficiently severe, the woman may be suffering from PMS [5].
The etiology of PMS is as yet unclear, but since PMS symptoms coincide with the hormonal fluctuations of the menstrual cycle [2], hormonal imbalance like estrogen excess and progesterone deficiency [6] have been proposed, although Serotonergic involvement is generally accepted as a key etiological factor [7]. Because there is no single clear and accepted etiology, a large number of possible treatments are prescribed and purchased [8]. The most commonly prescribed medications are SSRIs, based on the hypothesized role of serotonin, which can be taken solely in the Luteal phase [1]. However, women with PMS are often reluctant to take SSRIs, partly due to the side effects produced [9]. Therefore, many women turn to herbal remedies to treat their symptoms [10]. Herbal remedies may be very effective as a natural alternative to ease menstrual cramps, and other PMS symptoms [1, 3]. Various herbal remedies have been proposed to treat PMS [5]. One of the most common herbs used for the treatment of PMS is Chamomile [11]. Chamomile tea possesses anti-spasmodic properties, which can relieve the painful cramps associated with the menstrual periods [12]. A compound named Apigenin found in chamomile tea helps reduce the impact of excitatory neurotransmitter and hormones on the mind and body, helping to soother the over-firing sympathetic nervous system. Chamomile tea also helps modulate the actions of dopamine and serotonin, helping to offset or at least reduce the impact of depressive symptoms [4]. Apart from reducing the inflammatory response of the immune system, chamomile tea also works to reduce the sensation of pain by inhibiting the COX enzyme [11]. The anti-inflammatory and analgesic activities associated with chamomile have also been effectively used to alleviate managing symptoms of PMS [12]. Chamomile is listed on the FDA’s generally recognized as safe list [13]. It is known to be used in various forms of its preparations. The most common form is tea [14]. Chamomile tea possesses anti-spasmodic properties, which can relieve the painful cramps associated with the menstrual periods [11, 15]. Also, its tea helps modulate the actions of dopamine and serotonin, helping to offset or at least reduce the impact of depressive symptoms [11]. However, Chamomile essential oil has antispasmodic and relaxing properties which are useful in calming the symptoms associated with PMS [13].
Chamomile extract can be just as effective as Mefenamic Acid (MA) when it comes to relieving pain and regulating emotions [14]. A study from the Complementary Therapies in Clinical Practice Journal aimed to compare the effects of the popular anti-inflammatory medication, MA, found commonly in drugs like ibuprofen with chamomile extract for relieving PMS. Also, it acts similar to the MA in relieving physical symptoms [15].
Although Chamomile is widely consumed for PMS symptoms, rigorous scientific studies to test their efficacy are lacking. Therefore, this review aims to advance understanding regarding the effectiveness of the Chamomile in relieving symptoms of PMS.
2. Materials and Methods
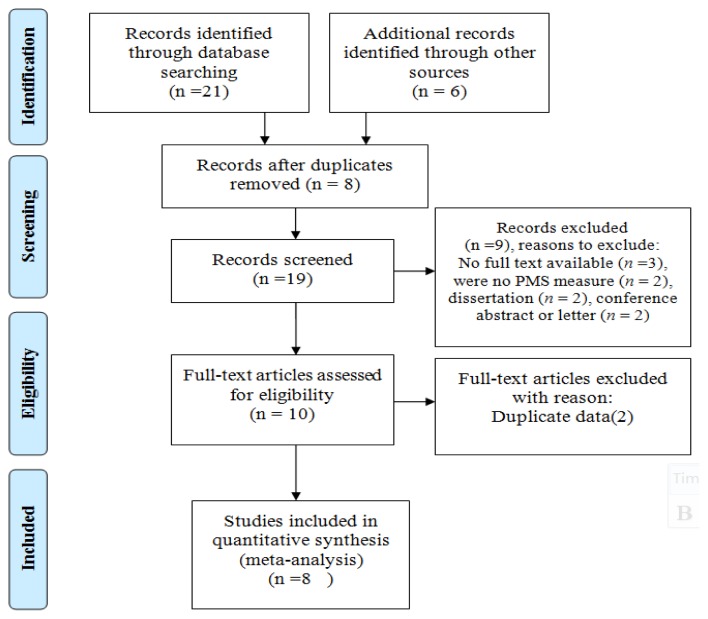
We conducted a comprehensive review of the literature published between 1990 and 2019 focusing on the efficacy of Chamomile on the treatment PMS. Preferred Reporting Items for Systematic Reviews (PRISMA) principle were used to extend the process explained in this review [16]. A search of the literature was carried out using Web of Science, the Cochrane Controlled Trials Register database, PubMed, Chinese Biomedical Database (CBM), CI-NAHL, China National Knowledge Infrastructure (CNKI), Psych INFO, and Social Science Research Network as databases for English papers and SID, Google Scholar, Iran Doc, Magiran and Iran Medex as databases for Persian papers. Gray literature search be conducted by the New York Academy of Medicine, PAIS, and the WHO Global Health Library. Studies were identified using the search terms “Premenstrual Syndrome”, “Premenstrual Tension”, “Premenstrual Dysphoria”, “Chamomile”, “Herbal medicines”, “Alternative Treatment”, “Premenstrual Dysphoric Disorder” according to the medical subject headings (MeSH). Manual reference checks of studies were performed to supplement the electronic search. The finds of the peer-reviewed search were entered into EndNote by Chamomile for PMS subject. In return, because of restrictions on the investigative capacity of the databases for gray literature, results of the gray search were entered into EndNote in relation to use of Chamomile for the treatment PMS more widely.
Two authors autonomously assessed every record caption for inclusion in the current review, and a third author adjudicated when disagreement occurred. Detailed records were made about the purpose of each study, participants, methodology, intervention type, data collection, and the outcomes of the study. We included studies meeting the following criteria: RCT that investigated the efficacy of Chamomile for the treatment of PMS, Published in English and Persian language. Published between 1990 to 2019. Studies were excluded that it was irrelevant to the Chamomile for the treatment of PMS or insufficient quantitative data were reported.
We assessed the methodology of each trial with a scale developed by Jadad and colleagues [17]. This scale assesses the randomization and double blinding and reports of dropouts and withdrawals.
The Consort Statement Checklist [18] used for evaluating ensuring reliability, and for drawing the right conclusions on randomized controlled trial (RCT). Whole duplicates studies were recognized and deleted. Two reviewers autonomously screened the title and abstracts of the article for eligibility. Then, the cause of removing studies was recorded.
3. Results
A total of Twenty-seven relevant trials were excluded from screening the title and abstract. Finally, Eight RCTs met the inclusion criteria. Reasons for record excluded were no PMS measure (n = 5), conference abstract or letter (n = 5), and unable to obtain full text (n = 2) (Fig. 1).
Figure 1.
Flowchart of the literature search
Most studies were conducted in Iran. Chamomile included four different forms (Tea, Capsule, extract, and Oil) in a variety of doses. Chamomile was compared with MA, placebo and no treatment.
Full details of the 8 included RTC are exposed in Table 1.
Table 1.
Characteristics of included RTC
| Author (Year) | Intervention form/mg | Type of control | Participants (N) | Tools | Outcome(s) |
|---|---|---|---|---|---|
| Jahanian et al (1999) [19] | Chamomile(Extract/ 30 drops) | 1st cycle as control | Students (70) | Visual Analogue Scales | Chamomile is more effective in relieving Dysmenorrhea if it is used before pain begins |
| Yazdani et al (2004) [20] | Chamomile(Extract/ 20 drops) | 1st cycle as control | Students (60) | Visual Analogue Scales | Using of Chamomile effectively reduces the severity of PMS symptoms than Foeniculum vulgar |
| Jenabi et al (2010) [21] | Chamomile (Tea/ two cups a day) | 1st cycle as control | Students (80) | Visual Analogue Scales | The PMS reduction was significantly greater in the chamomile tea group than in the control group |
| Modaress M et al (2011) [22] | Chamomile (Capsule/ 400 mg) | MA(250 mg/TDS*) | Students (80) | Visual Analogue Scales | Chamomile was more effective in reducing PMS symptoms than MA |
| Karimian et al (2013) [23] | Chamomile (Capsule / 250 mg) | MA(250 mg/TDS*) | Students (90) | McGill ruler | Chamomile is effective in decreasing the severity of physical symptoms of PMS as well as MA. |
| Sharifi F et al (2014) [24] | Chamomile (Capsule / 100 mg) | MA(250 mg/TDS*) | Students (90) | Daily Rating Form | The findings were shown a significantly greater reduction of emotional symptom in Chamomile users than the MA users |
| Dadfar F (2015) [25] | Chamomile (Extract/ 30 drops) | 1st cycle as control | Women (30) | Daily Record of Severity of Problems | The severity of retention and anxiety symptoms after consumption of Chamomile extract had significantly decreased than before consumption. |
| Najafi E et al (2018) [26] | Chamomile (Capsule / 250 mg) | Placebo | Students (118) | Premenstrual Symptoms, Screening Tool | Using of Chamomile is effective to relieve PMS symptoms |
TDS: Three times daily
4. Discussion
Although researchers conducted controlled trials aimed to determine the efficacy of Chamomile in the treatment of PMS, various forms and dosage of chamomile were used to did this that makes it difficult to draw conclusions.
Clearly, the amount of evidence about the effect of Chamomile is very little, albeit, existing studies have revealed Chamomile in the Menstrual pain reduction were more effective than placebo [19–26].
Presently, the world market has a chamomile drug with a variety of medicinal and therapeutic values [23]. Traditional herbal medicine in England used chamomile as one of the five “opening” herbs for the treatment of irregular menstruation [27]. As efficient methods for determining the drug constituents and effectiveness have been developed, the content of (−)-α Bisabolol and its oxides in the flowers have become a significant index of drug value and quality. Thus, chamomile of particular chemical composition is used as a drug, as it shows specific pharmacological activity [11]. Chamomile has anti-anxiety, antihistamine, anti-inflammatory, antioxidant, and antispasmodic properties. It is considered generally safe, but according to evidence should still take precaution nary measures [15].
Reviewing these studies indicated that most of the result of studies possess antidepressant effects through an anti-anxiety effect can reduce psychological signs of PMS [24, 25].
Laboratory tests on animals show that inhaling the vapors of essential oil of chamomile reduces the body’s production of the Adrenocorticotropic hormone, a stress hormone [28, 29]. The therapeutic value of the plant matter was assessed by the substance of essential oil. The quality of essential oil is verified by its color. As the name indicates, bluer the oil better is the quality, because the blue color serves as the chemical indicator for the existence of Flavonoids and Terpenoids, α-Bisabolol and Chamazulene [28]. For manufacturing chamomile extracts of Antiphlogistic effectiveness, only such types of chamomile should be used, which exhibit a high content of (−)-α-Bisabolol and the synthetic Bisabolol [29].
Studies on human have also shown that chamomile tea eases anxiety and irritability that can be caused by PMS [24, 25].
Glycine, Apigenin, Luteolin and also Flavonoid as CNS stimulating molecule is nerve relaxant, which may explain why chamomile is also effective for stress and anxiety relief [30].
Chamomile contains Spiroether, a very strong antispasmodic agent that relaxes aching, tense muscles and alleviates premenstrual pain [12]. A crossover study, Chamomile was compared with MA for treating PMS, that reported that Chamomile was more effective than the MA in reducing menstrual cramps [31]. Relaxing menstrual cramps occur due to an increase in serum Glycine levels following Chamomile tea using [15]. Chamomile seems to suppress pain through the effect of Matrisin, Metoxicomarin, Flavonoids, Phytostrogenic, and Apigenin on the central nervous system [13]. Also, its flowers contain Flavonoids which may responsible for antispasmodic [11]. Another clinical trial supplied the effectiveness of Chamomile at managing abdominal and pelvic pain [23].
5. Conclusion
In summary, the consequences of the current study propose an efficacy of Chamomile in the treatment PMS. This review has demonstrated that the chemical ingredients of the chamomile drug possess anti-inflammatory, antispasmodic, sedative, and anti-anxiety properties that significantly impact on painful menstruation, anxiety and psychological problems in the women of PMS sufferers. Since the Chamomile as traditional herbal medicine is well known and accessible in Iran, so it could be used easier than other herbs to relieve PMS symptoms. Because the randomized controlled trials could improve our understanding of what Chamomile is efficacious for PMS treatment. Further trials with different forms and doses of Chamomile, larger populations, longer durations, featuring comparisons with safe drugs and accurate descriptions of the involved molecular mechanisms are recommended to confirm the benefits of the procedures described and ensure the absence of complications.
One of the major strengths in this research was the extensive review and more than one researcher evaluate each document. Our study’s limitations include the Likelihood of removing a number of eligible studies.
Acknowledgment
MB and ZB contributed to the design of the study, review and summarized the papers, and evaluated the records for quality. MB and SP contributed to the reviewer of papers. ZB drafted the study. The study has been read and approved by all authors.
Footnotes
This paper meets the requirements of KS X ISO 9706, ISO 9706-1994 and ANSI/NISO Z39.48-1992 (Permanence of Paper).
Conflict of interes
We have no conflict of interest to declare.
References
- 1.Kapur N, Narula PS. Premenstrual symptoms and social disability. International Journal of Innovative Knowledge Concepts. 2016;4(1):1–11. [Google Scholar]
- 2.Bostani Khalesi Z, Abedinzade M, Safari A. Comparison of Acupressure Effect on Sanyinjiao Point with that of Vitamin E on Primary Dysmenorrhea. Amalgam-Danesh. 2009;3(55):36–43. [Google Scholar]
- 3.Farokheslamlou H, Nabilou B, Oshnoee S, Akbari E. The prevalence of premenstrual syndrome and its associated factors among medical students of Urima University of Medical Science. J Urmia Univ Med Sci. 2013;24(9):702–10. [Google Scholar]
- 4.Jang SH, Kim DI, Choi MS. Effects and treatment methods of acupuncture and herbal medicine for premenstrual syndrome/premenstrual dysphoric disorder: systematic review. BMC Complement Altern Med. 2014;14:11. doi: 10.1186/1472-6882-14-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bostani Khalesi Z, Simbar M, Azin SA. A qualitative study of sexual health education among Iranian engaged couples. African Health Sciences. 2017;17(2):382–390. doi: 10.4314/ahs.v17i2.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Panjalipour S, Bostani Khalesi Z, Mirhaghjoo SN. Iranian Female Adolescents’ Reproductive Health Needs: A Systematic Review. IJWHR. 2018;6:226–232. doi: 10.15296/ijwhr.2018.39. [DOI] [Google Scholar]
- 7.Dante G, Facchinetti F. Herbal treatments for alleviating premenstrual symptoms: a systematic review. J Psychosom Obstet Gynaecol. 2011;32(1):42–51. doi: 10.3109/0167482X.2010.538102. [DOI] [PubMed] [Google Scholar]
- 8.Chen HY, Huang BS, Lin YH, et al. Identifying Chinese herbal medicine for premenstrual syndrome: implications from a nationwide database. BMC Complement Altern Med. 2014;14:206. doi: 10.1186/1472-6882-14-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pattanittum P, Kunyanone N, Brown J, Sangkomkamhang US, Barnes J, Seyfoddin V, et al. Dietary supplements for Dysmenorrhoea. Cochrane Database of Systematic Reviews. 2016;3:CD002124. doi: 10.1002/14651858.CD002124.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gholami Z. The primary Dysmenorrhoea and complementary medicine in Iran: A systematic review. International Journal of Fertility & Sterility. 2015;9:107. [Google Scholar]
- 11.Amsterdam JD, Shults J, Soeller I, Mao JJ, Rockwell K, Newberg AB. Chamomile (Matricaria recutita) may provide antidepressant activity in anxious, depressed humans: an exploratory study. Altern Ther Health Med. 2012;18(5):44–49. [PMC free article] [PubMed] [Google Scholar]
- 12.Bhaskaran N, Shukla S, Srivastava JK, Gupta S. Chamomile: an anti-inflammatory agent inhibits inducible nitric oxide synthase expression by blocking RelA/p65 activity. Int J Mol Med. 2010;26(6):935–940. doi: 10.3892/ijmm_00000545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amsterdam JD, Li Y, Soeller I, Rockwell K, Mao JJ, Shults J. A randomized, double-blind, placebo-controlled trial of oral Matricaria recutita (chamomile) extract therapy for generalized anxiety disorder. J Clin Psychopharmacol. 2009;29(4):378–82. doi: 10.1097/JCP.0b013e3181ac935c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mirabia P, Alamolhodab SH, Esmaeilzadeha S, Mojabc F. Effect of medicinal herbs on primary Dysmenorrhoea: a systematic review. Iranian Journal of Pharmaceutical Research. 2014;13:757–767. [PMC free article] [PubMed] [Google Scholar]
- 15.McKay DL, Blumberg JB. A review of the bioactivity and potential health benefits of chamomile tea (Matricaria recutita L.) Phytother Res. 2006;20(7):519–30. doi: 10.1002/ptr.1900. [DOI] [PubMed] [Google Scholar]
- 16.PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement criteria. http://www.prisma-statement.org/statement.htm.
- 17.Jadad A, Moore M, Carrol D, Jenkinson C, Reynolds DJ, Gavaghan D. Assessing the quality of reports of randomized clinical trials; is blinding necessary? Controlled Clinical Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 18.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. BMJ. 2010;340:c332. doi: 10.1136/bmj.c332. [DOI] [PubMed] [Google Scholar]
- 19.Jahanian M, Rakhshandeh H, Teimuri M. The effect of Chamomile extract on Dysmenorrhoea. Med J Mashad Univ Med Sci. 1999;42(64):33–40. [Google Scholar]
- 20.Yazdani M, Shahriari M, Hamidi B. Comparison of fennel and chamomile extract and placebo in treatment of premenstrual syndromes and Dysmenorrhoea. Med J Hormozgan Univ. 2004;8:57e61. [Google Scholar]
- 21.Jenabi E, Ebrahimzadeh S. Chamomile tea for relief of Dysmenorrhoea. Iranian Journal of Obstetrics, Gynaecology and Infertility. 2010;13(1):39–42. [Google Scholar]
- 22.Modares M, Oshrieh Z, Mehran A. Comparison of the effect of Mefenamic acid and Matricaria Chamomilla capsules on primary Dysmenorrhoea. J Babol Uni Med Sci (JBUMS) 2011;13:50e8. [Google Scholar]
- 23.Karimian Z, Sadat Z, Abedzadeh M, Sarafraz N, Kafaei Atrian M, Bahrami N. Comparing the effect of Mefenamic acid and Matricaria Chamomilla on primary Dysmenorrhoea in Kashan Medical University Students. Journal of Ardabil University of Medical Sciences. 2013;13(4):413–20. [Google Scholar]
- 24.Sharifi F, Simbar M, Mojab F, Majd H. Comparison of the effects of Matricaria chamomile (Chamomile) extract and Mefenamic acid on the intensity of premenstrual syndrome. Complementary Therapies in Clinical Practice. 2014;20:81–88. doi: 10.1016/j.ctcp.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 25.Dadfar F. Effectiveness of Chamomile extracts on the reduction of Dysmenorrhoea and premenstrual syndrome symptoms. Der Pharm Let. 2015;7(21):454–8. [Google Scholar]
- 26.Najafi Mollabashi E, Ziaie T, Bostani Khalesi Z, Kazemnejad Leili E, Bekhradi R. Effect of Chamomile capsule on premenstrual syndrome symptom relief. 2018;21(7):72–80. [Google Scholar]
- 27.Sammon CJ, Nazareth I, Petersen I. Recording and treatment of premenstrual syndrome in UK general practice: a retrospective cohort study. BMJ Open. 2016;6:e010244. doi: 10.1136/bmjopen-2015-010244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keefe JR, Mao JJ, Soeller I, Li QS, Amsterdam JD. Short-term open-label chamomile therapy of moderate to severe generalized anxiety disorder. Phytomedicine. 2016;23(14):1699–1705. doi: 10.1016/j.phymed.2016.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mao JJ, Xie SX, Keefe JR, Soeller I, Li QS, Amsterdam JD. Long-term chamomile treatment for generalized anxiety disorder: A randomized clinical trial. Phytomedicine. 2016;23(14):1735–1742. doi: 10.1016/j.phymed.2016.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McIntyre E, Saliba AJ, Moran CC. Herbal medicine use in adults who experience anxiety: A qualitative exploration. International journal of qualitative studies on health and well-being. 2015;10:29275. doi: 10.3402/qhw.v10.29275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maleki-Saghooni N, Karimi FZ, Behboodi Moghadam Z, Mirzaii Najmabadi K. The effectiveness and safety of Iranian herbal medicines for treatment of premenstrual syndrome: A systematic review. Avicenna J Phytomed. 2018;8(2):96–113. [PMC free article] [PubMed] [Google Scholar]