Abstract
Introduction
Migraine attacks associated with menstruation are generally perceived as more severe than attacks outside this period.
Aim and Objective
The study aimed at determining the frequency of menstrual-related headaches among a cohort of senior secondary school girls in Abeokuta, Nigeria. We also determined its burden among these school girls.
Methodology
This study was cross-sectional using a validated adolescent headache survey questionnaire. A self-administration of the instrument was done during a school visit. A headache was classified using the ICHD-II criteria.
Results
Of the 183 students interviewed, 123(67.2%) had recurrent headaches. Mean age ±SD, 16.18±1.55 (range 12–19). The prevalence of definite migraine was 17.5% while the prevalence of probable migraine was 6.0%. The prevalence of tension-type headache was 41.0%. Migraine was significantly menstrual-related (p=0.001, 95% CI=1.06–6.63). Median pain severity score was higher among MRH group (p=0.043). The median number of days of reduced productivity and missed social activities was significantly higher in the MRH group; p= 0.001 and p=0.03, respectively. Subjects with MRH were more incapacitated by their headaches (p= 0.003).
Conclusion
Menstrually related headache is prevalent even among the adolescent and it has adversely affected their productivity and social life. Care of adolescent with headaches should be intensified.
Keywords: headache, adolescence, migraine, menstruation, menstrually related
Introduction
Over 37 million Nigerians are adolescents (between the ages of 10–19 years) and they constitute over 20% of the general population. Roughly half of these are females.1 Adolescence is a phase of life characterized by rapid and ample physical, biological, psychosocial and neurodevelopmental changes 2 One of the biological changes that characterize this period is the attainment of menarche; a milestone that is greatly influenced by the genetic makeup and environmental factors of the individual and one that is accompanied by menstrually associated disorders3 apart from other psychosocial issues. The adolescent population is therefore faced with specific health and developmental needs.
Migraine headache, the 7th disabling disease4 is probably as common among the adolescent population as in the adult5 although our current understanding of headache pathophysiology among children and adolescents is based on extrapolations from studies conducted among adults.6 Migraine is twice as prevalent in females as in male genders especially after puberty. Among adolescents just like in adults, chronic migraine has been found to be strongly associated with depression, irritability, missed school/works as well as missed social activities thereby increasing the total burden of headaches in this population.7 Menstrual disorders have been found to be significant among adolescents who reported headache or dizziness during their menstrual period.8
According to the international classification of headache disorders 2nd version (ICHD-II),9 menstrually related migraine (MRM) is defined as attacks of menstrually related migraine without aura that has an onset during the peri-menstrual time period (2 days before to 3 days after the onset of menstruation) and this pattern must be confirmed in two-thirds of menstrual cycles, but other attacks may occur at other times of the menstrual cycle (Table 1). Migraine attacks associated with menstruation are generally perceived as more severe, more disabling and refractory to abortive medications than those outside this period.10
Table 1.
ICHD-2 Diagnostic Criteria for Menstrual Migraine
| Diagnostic Criteria for Pure Menstrual Migraine Without Aura (A1.1.1) |
| A. Attacks, in a menstruating woman, fulfilling the criteria for migraine without aura |
| B. Attacks that occur exclusively from days −2 to +3 of menstruation in at least two out of three menstrual cycles and at no other times of the cycle. |
| Diagnostic Criteria for Menstrually-Related Migraine Without Aura (A1.1.2) |
| A. Attacks, in a menstruating woman, fulfilling the criteria for migraine without aura |
| B. Attacks that occur exclusively from days −2 to +3 of menstruation in at least two out of three menstrual cycles, and additionally at other times of the menstrual cycle. |
Notes: The first day of menstruation is day +1, and the preceding day is day −1; there is no day 0. In ICHD-3, menstruation is considered to be endometrial bleeding resulting from either the normal menstrual cycle or from the withdrawal of exogenous progestogens, as in the use of combined oral contraceptives or cyclical hormone replacement therapy.9
There is paucity of data-driven scientific reports from sub-Saharan African on the burden of menstrually related migraine, especially among adolescents. The need for individualized therapy, provision and optimization of effective abortive therapy and improvement in the overall quality of life of adolescent migraineurs calls for this survey. We hypothesized that menstrually related headaches will be prevalent among Nigerian high school adolescent girls. Our study aimed therefore, at determining the frequency of menstrually related headaches among a cohort of senior secondary school girls in Abeokuta, southwestern Nigeria. We also set out to document headache burden among these school girls.
Methodology
This was a cross-sectional observational study that was conducted in four secondary schools in Abeokuta south local government area (LGA), Abeokuta, south-western Nigeria in October 2010. Abeokuta is a southwestern Nigerian city with a population of 593,100 according to the 2006 census. It is situated at elevation 64 m above sea level and lies in longitude 3.35and latitude 7.16.11 Abeokuta is made up of two local governments namely Abeokuta south and Abeokuta north LGA. Abeokuta south was selected for the study by balloting. Of the 20 public secondary schools in the local government, four secondary schools (20%of the sample frame) were randomly selected for the survey.
To obtain the lifetime prevalence of migraine and tension-type headache from this adolescent population, the minimum sample size to be studied was estimated to be 142. This was based on a standard normal deviate of 1.96 and a degree of accuracy of 0.05 while the proportion of high school students with migraine was put at 10.3% based on a previous study among Nigerian undergraduates.12 The study protocol was approved by the research and ethics committee (REC) of Federal Medical Centre Abeokuta (FMCA). The authorities of the secondary schools approved the study and informed verbal consent was obtained from the participants. Individual parental informed consent was not obtained. The school authority served as proxy for the parents in this regard. This modification of the protocol was approved by the REC of FMCA. A validated self-administered headache questionnaire developed by Ojini et al13 was used for the survey. The questionnaires were anonymized while the students were assured of the confidentiality of their responses. The questionnaire were distributed to the participants by the residents rotating through the neurology unit of the medical department of our hospital after a pilot study with 20 students showed excellent clarity. The 29 item questionnaire is made up of three sections.
The first section assessed socio-demographic variables. The second section evaluated headache-related variables including the association of headache with menstruation in the past 3 months. The third section assessed headache disability using the migraine disability assessment scale (MIDAS). The headache-related items were developed to incorporate diagnostic items for migraine and tension-type headaches according to the International Classification of Headaches Disorders (ICHD-II) classification.9 The survey was conducted in trickles during school hours at the end of class from October 1, 2010 to October 20, 2010. Although the questionnaires were self- administered, the authors were on hand to give clarifications where necessary. Six hundred questionnaires were distributed in all. The males had 350 questionnaires while 250 questionnaires were distributed to the female students based on their availability in the school on the day of interview. Sub-analysis of the female respondents was performed for this report.
Statistical Analysis
Statistical analysis was performed with Statistical Package for the Social Sciences version 20.0.0 (SPSS Inc., Chicago). Data were summarized and presented as frequencies and percentages. Categorical data were compared using chi-square test. Normally distributed numerical variables were summarized as mean with standard deviation and between groups comparison was performed with student’s t-test. Skewed numerical data were summarized with median (interquartile range) and non-parametric Kruskal–Wallis test was used for between group comparisons. The level of significance was set at p<0.05.
Results
Characteristics of the Respondents and Prevalence of Menstrually Related Headaches
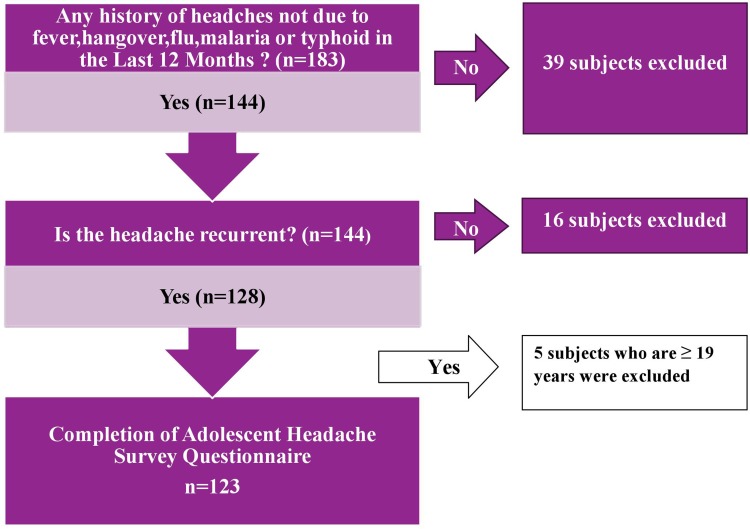
One hundred and eighty-three (183) out of the 250 questionnaires distributed to the female students were returned (response rate 73.2%). Of the 183 respondents, 39 subjects (21.3%) had headaches considered to be due to systemic infection like malaria, typhoid or flu. Of those whose headaches were not due to the factors above, 16 (8.7%), had non-recurrent headaches. Five subjects who had recurrent headaches but were older than 19 years of age were excluded from the analysis. Figure 1 shows the algorithm of subjects’ selection for the analysis.
Figure 1.
Algorithm for screening for recurrent headaches among the subjects.
The prevalence of all primary headache type was 67.2% (123/183). Thirty-two subjects (17.5%) satisfied the ICHD-II criteria for the diagnosis of migraine while 11(6.0%) satisfied the criteria for probable migraine. The prevalence of Tension Type Headache (TTH) was 41.0% (75/183). Five patients (2.7%) could not be classified.
The prevalence of menstrually related headache was 14.2% (26/183).The prevalence of definite menstrually related migraine was 6.6% (12/183). When probable migraine was added, the prevalence of all menstrually related migraine was 8.7% (16/183). There was no significant age difference between the cohorts with and without menstrually related headaches (Table 2). Although the difference was also insignificant, subjects with menstrually related headaches tend to have a positive family history of headaches. Nausea and photophobia were significantly prevalent among subjects with menstrually related headaches (p<0.05) and these subjects were more likely to consult a doctor for their headaches (p<0.05). Table 2 shows the baseline characteristics of those with recurrent headaches. Table 3 shows the frequency of menstrually related primary headaches. Migraine was significantly menstrually related (p=0.001, 95% CI=1.06–6.63) while TTH was significantly non-menstrually related (p=0.007, 95% CI=1.25–5.32).
Table 2.
Sociodemography and Baseline Characteristics of the Subjects
| Variables | All Primary Headaches sn=123 (100%) | Non-MRH n=97(100%) | MRH n=26(100%) | Test Statistics | P value |
|---|---|---|---|---|---|
| Age | |||||
| 12–14 | 12(9.8) | 9(9.3) | 3(11.5) | 1.90# | 0.386 |
| 15–17 | 80(65.0) | 66(68.0) | 14(53.8) | ||
| 18–19 | 31(25.2) | 22(22.7) | 9(34.6) | ||
| Family history of headaches | 51(41.5) | 38(39.6) | 13(50.0) | 0.91# | 0.375 |
| Frequency | 5.89# | 0.435 | |||
| Daily | 2(1.6) | 2(2.1) | 0(0.0) | ||
| 3x/week | 25(20.3) | 20(20.8) | 5(20.0) | ||
| 2x/week | 16(13.0) | 14(14.6) | 2(8.0) | ||
| 1/week | 19(15.4) | 15(15.6) | 4(16.0) | ||
| 2x/month | 15(12.2) | 12(12.5) | 3(12.0) | ||
| 1/month | 21(21) | 13(13.5) | 8(32.0) | ||
| 3–6/year | 23(18.7) | 20(20.8) | 3(12.0) | ||
| Severity of Pain on VAS, Median (IQR) | 5.0(10.0) | 2.0(10.0) | 5.5(8.25) | 930† | 0.185 |
| Presence of nausea | 21(17.1) | 12(12.5) | 9(36.0) | 7.64# | 0.006* |
| Presence of photophobia | 41(33.3) | 30(31.9) | 11(42.3) | 0.98# | 0.323 |
| Presence of phonophobia | 89(72.4) | 64(66.7) | 25(96.2) | 9.02# | 0.003* |
| Consultation | |||||
| Consult a doctor | 43(35.0) | 29(30.9) | 14(53.8) | 4.68# | 0.030* |
| Self-medication | 75(61.0) | 55(59.1) | 20(76.9) | 2.76# | 0.097 |
| Prayers | 10(8.1) | 8(8.2) | 2(7.8) | – | – |
| Frequently used medication | |||||
| Aspirin | 3(2.4) | 2(2.1) | 1(3.8) | – | – |
| PCM | 83(67.5) | 66(68.0) | 17(65.4) | – | – |
| Other NSAID | 6(4.9) | 4(4.1) | 2(7.7) | – | – |
| Sedative | 3(2.4) | 1(1.03) | 2(7.7) | – | – |
Notes: #Chi-Square Test; †Mann–Whitney U-Test;*Significant value (P< 0.05).
Table 3.
Frequency of Primary Headache and Its Association with Menstruation
| Non MRH n=97(100) | MRH n=26(100) | χ2 | RR (95% CI) | P value | |
|---|---|---|---|---|---|
| Migraine | 20(20.6) | 12(46.2) | 6.95 | 3.30(1.32–8.24) | 0.008* |
| Probable migraine | 7(7.2) | 4(15.3) | 1.68 | 2.34(0.63–8.69) | 0.195 |
| All migraine | 27(27.8) | 16(61.5) | 10.24 | 2.65(1.06–6.63) | 0.001* |
| TTH | 66(68.04) | 9(34.6) | 9.63 | 0.25(0.10–0.62) | 0.002* |
| Unclassifiable | 4(4.1) | 1(3.5) | 1.00ǂ | 1.06(0.18–6.33) | 0.715 |
Notes: ǂFishers exact chi–square; *Significant value (P< 0.05).
Abbreviation: TTH, tension-type headache.
Burden of Menstrually Related Headaches
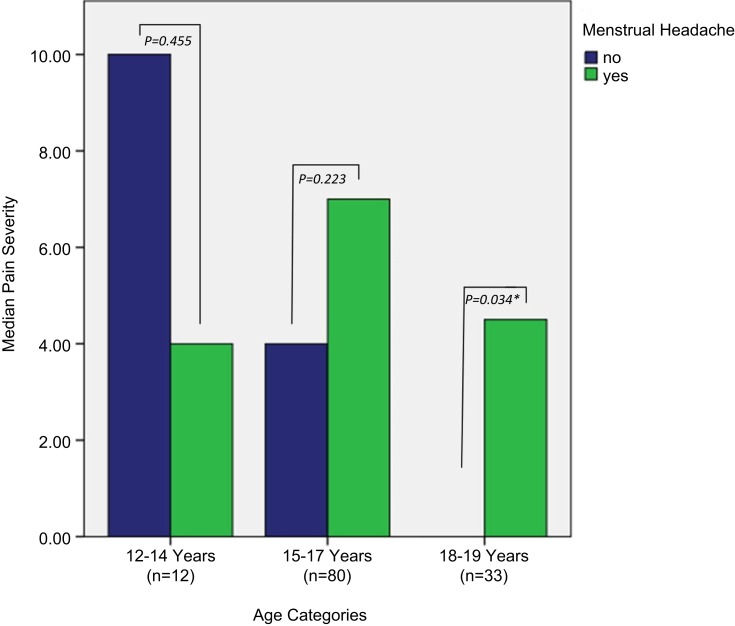
When severity of headaches was compared across age groups, there was a significantly higher median headache severity score among 18–19 years old with menstrually related headaches (p=0.034). (Figure 2).No statistically significant difference in median headache severity scores was noted between those with or without menstrually related headache in the other age groups (Figure 2).
Figure 2.
Clustered bar charts showing severity of headaches in subjects with and without menstrual headaches. *significant value (P<0.05).
Table 4 shows the comparison of each item of the MIDAS scale between subjects with and without menstrually related headaches. Median number of days of missed social activities and reduced productivity was significantly higher among the cohort with menstrually related headaches; p-values 0.047 and 0.004, respectively. There was no difference in the median number of days of missed social activities, reduced productivity or reduced house works between the cohort of menstrually related migraine and other menstrually related headaches. The cohort with menstrually related migraine, however, demonstrated more severe headaches (p value =0.006) as well as more number of headache days in the last three months (p value=0.007).
Table 4.
Comparison of MIDAS Items Between Patients with and Without MRH and MRM
| Variables, Median (IQ-Range) | Non-MRH (n=97) | MRH (n=26) |
P value | Non-MRM(21) | MRM (11) | P value |
|---|---|---|---|---|---|---|
| Days of missed school/work | 0.0(1.0) | 0.0(0.5) | 0.669 | 0.0(1.0) | 0.0(1.0) | 0.984 |
| Days of reduced productivity (work/school) | 0.0(2.0) | 0.0(1.3) | 0.830 | 0.0(3.5) | 0.0(2.0) | 0.631 |
| Days of missed social activities | 0.0(2.0) | 2.0(3.3) | 0.047* | 0.0(2.0) | 0.0(2.0) | 0.861 |
| Days of reduced productivity (housework) | 0(2.0) | 2.0(5.5) | 0.004* | 0.0(2.5) | 1.0(5.0) | 0.715 |
| Days of missed house works | 1.0(3.0) | 0.5(3.0) | 0.393 | 1.0(3.0) | 3.0(4.0) | 0.108 |
| Headaches days/3 months | 0.0(4.0) | 2.0(5.5) | 0.650 | 2.0(2.0) | 5.0(4.0) | 0.006* |
| Pain Severity | 2.0(10.0) | 6.0(7.5) | 0.323 | 3.0(9.75) | 10.0(7.5) | 0.007* |
Note: *Significant value (P< 0.05).
Abbreviations: MRH, menstrually related headaches; MRM, menstrually related migraine.
Table 5 shows the degree of headache disability according to the total MIDAS score. A score of 0–5 was graded as little or no disability (grade I), 6–10 as mild disability (grade II), 11–20 as moderate disability (grade III) while >20 was defined as severe disability (grade IV). Significantly higher proportion of patients with menstrually related headaches had moderate disability (p=0.003).
Table 5.
Headache Disability in Relation to Menstruation
| MIDAS Scale | Overall (n=123) | Non-MRH (n=97) | MRH (n=26) | χ2 | OR | 95% CI | P-value |
|---|---|---|---|---|---|---|---|
| Grade I | 42(34.1) | 37(38.1) | 5(19.2) | 3.26 | 0.37 | 0.13–1.11 | 0.071 |
| Grade II | 17(13.8) | 16(16.5) | 1(3.8) | 2.75 | 0.20 | 0.03–1.60 | 0.097 |
| Grade III | 26(21.1) | 15(15.4) | 11(42.3) | 8.86 | 4.01 | 1.55–10.39 | 0.003* |
| Grade IV | 38(30.9) | 29(29.8) | 9(34.6) | 0.21 | 1.24 | 0.50–3.11 | 0.644 |
Note: *Significant value (P< 0.05).
Abbreviations: MRH, menstrually related headaches; MRM, menstrually related migraine; MIDAS, migraine disability assessment scale.
Discussion
Research on small and specific populations of headache sufferers has the added advantage of aiding in the identification of factors that influence the frequency and severity of various subtypes of headache13 thereby enabling effective planning and organization of health services. From a planning point of view, gender-specific data, from clinical and epidemiological studies have the potential to bridge the knowledge gap that fosters the neglect of vulnerable groups such as adolescents.
Globally, the estimated overall mean prevalence of headache among adolescents is 54.4% (95% CI 43.1–65.8) and the overall mean prevalence of migraine is 9.1% (95% CI 7.1–11.1).14 Among this cohort of female adolescents, the prevalence of headache was 67.2%.14,15 Our study found a higher prevalence compared to the study by Ofovwe and Ofili who reported a prevalence of 19.5% in a survey of secondary school students in south-south Nigeria.16 Ofovwe and Ofili, however, reported a migraine prevalence of 13.5% which is comparable to the prevalence rate of 11.5% that we found in this study. As pointed out by Wöber-Bingöl, there is a paucity of population-based studies of adolescent headaches from low and low-middle income countries15 hence there are limited studies to compare our findings with. When compared with studies among young undergraduates, our study found a higher prevalence of headache than Mitsicostas as et, who reported a prevalence of 50.3% among female undergraduate.14 Krogh et al17 however, reported a prevalence of 88%; a rate higher than what we found in this cohort. The relatively modest sample size in our study as well as regional/racial differences in headache epidemiology could have been responsible for these differences even though we used the same diagnostic criteria as the earlier quoted studies. The prevalence rate in this study is however comparable to the prevalence rate of 62.8% in the female cohorts of the survey by Ojini et al in a sample of Nigerian undergraduates.13
The prevalence of menstrually related headache was 14.2% in this survey of which menstrually related migraine was 8.7% when all migraine (definite and probable migraine) was summed up. Among the female adult population, the prevalence of menstrually related migraine without aura ranges from 20-51% while that of pure menstrual migraine without aura varies from 7-19%.18,19 There is paucity of literature on menstrually related migraine in adolescents. In a study of 896 girls between 9 and 18 years, Crawford et al reported a prevalence rate of 36.9%.20 This value no doubt is higher than what we found. While the value of Crawford et al approaches that of the female adult population, the prevalence of MRM in this study lags behind that of the female adult population as well as that of the Caucasian adolescent population. This finding suggests that perhaps the adolescent Caucasian or African American adolescents attain menarche earlier, and that their hypo-thalamo-pituitary-ovarian (HPO)functions mature faster than native African adolescents.
By way of pathophysiology, the decline in serum estradiol levels that occur soon before and during the peri-menstrual time period is the most plausible trigger for menstrual migraine. Other contributor to MM includes the release of prostaglandins from a shedding endometrium that sensitizes peripheral nociceptors, and the declines in serum magnesium levels. A decrease in the inhibitory neurotransmitter systems that modulate neuronal firing rates within second-order neurons of the trigeminal system may also augment the initiation of MM.21 Therefore, the more developed the HPO function is, the more readily the adult pattern of menstruation is established. The above hypothesis is buttressed by our findings of higher median pain severity score among older girls aged 18–19 years (Figure 2). This relatively higher pain severity score also agrees with the finding of Stewart et al22 who in a rigorous prospective survey of 81 migraineurs women from the general population, found a slight increase in the severity of attacks occurring the first 2 days of menses. However, these authors did not find any other significant characteristical difference between menstrual and non-menstrual migraine attacks.
A significant proportion of adolescents with MRH sought a doctor for their headaches (Table 1). Although the difference was not significant, the MRH cohort was more likely to self-medicate. It is possible that this treatment-seeking pattern is dictated by the severity of the headache attacks. We recorded no use of abortive therapies such as triptans and ergot preparations in this study. Our finding mirrors the report by other authors in our environment.12,13,16,23 Oshinaike et al, also recorded no patient with triptans prescription, but up to 32% of those who sought medical consultation had ergot prescription.23 The study population (hospital staff members) however was not comparable with ours hence the difference in the treatment pattern. Our finding clearly underscores the fact that headaches in general, are undertreated in our environment and menstrually related headaches in particular, does not enjoy any special attention as far as treatment is concerned.
Our results show that menstrually related headaches are clearly more disabling especially when moderate to severe disability are considered. Crawford et al20 found no difference in disability between girls with a menstrual pattern and those without a menstrual pattern although girls with MM reported increased associated symptoms compared with girls without MM. In our cohort, however, girls with MM reported more headache days in 3 months and higher pain severity suggesting that girls with MM are likely more incapacitated by their headaches. Just like we have established, the American Migraine Prevalence and Prevention (AMPP) study found that women with MM were more impaired by attacks while women with MAM had overall highest burden, likely due to experiencing migraines on additional days.24
Limitations and Strength of Study
Our study is limited by its modest sample size and cross-sectional design. However, its strength lies in the fact that there is paucity of MRH-specific data from SSA. In addition, we have studied a population of educated/enlightened girls; hence, the influence of cultural beliefs on reporting MRH is less likely.
Conclusion
Our study found that menstrually related headache is prevalent among adolescent Nigerian girls. When compared with similar studies among whites, it appears less prevalent but undoubtedly more disabling. Unfortunately, health-care facilities are poorly accessed and the headache is poorly treated in that approved medications are seldom used by the migraineurs. More headache education and awareness programs need to be instituted and possibly incorporated into adolescent and school health programs. Headache advocacy among this vulnerable group should be escalated as this might have a long-lasting impact on reducing the burden of menstrually related headaches in our environment.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
- 1.Statistics | At a glance: Nigeria | UNICEF. [cited April13, 2016] Available from: http://www.unicef.org/infobycountry/nigeria_statistics.html. Accessed December20, 2019.
- 2.Adolescence: a period needing special attention - recognizing-adolescence. [cited April13, 2016] Available from: http://apps.who.int/adolescent/second-decade/section2/page1/recognizing-adolescence.html. Accessed December20, 2019.
- 3.Abdelmoty HI, Youssef MA, Abdallah S, et al. Menstrual patterns and disorders among secondary school adolescents in Egypt. A cross-sectional survey. BMC Womens Health. 2015;15:70. doi: 10.1186/s12905-015-0228-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Steiner TJ, Stovner LJ, Birbeck GL. Migraine: the seventh disabler. J Headache Pain. 2013;14:1. doi: 10.1186/1129-2377-14-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brna PM, Dooley JM. Headaches in the pediatric population. Semin Pediatr Neurol. 2006;13(4):222–230. doi: 10.1016/j.spen.2006.09.003 [DOI] [PubMed] [Google Scholar]
- 6.Matar AK, Kerem NC, Srugo I, Genizi J. Primary headache in children and adolescents–diagnosis and treatment. Harefuah. 2015;154(12):795–8, 803. [PubMed] [Google Scholar]
- 7.Arita JH, Lin J, Pinho RS, et al. Adolescents with chronic migraine commonly exhibit depressive symptoms. Acta Neurol Belg. 2013;113(1):61–65. doi: 10.1007/s13760-012-0135-9 [DOI] [PubMed] [Google Scholar]
- 8.Titilayo A, Agunbiade OM, Banjo O, Lawani A. Menstrual discomfort and its influence on daily academic activities and psychosocial relationship among undergraduate female students in Nigeria. Tanzan J Health. 2009;11(4):181–188. [DOI] [PubMed] [Google Scholar]
- 9.Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24 Suppl 1:9–160. doi: 10.1111/j.1468-2982.2003.00824.x [DOI] [PubMed] [Google Scholar]
- 10.MacGregor EA, Hackshaw A. Prevalence of migraine on each day of the natural menstrual cycle. Neurology. 2004;63(2):351–353. doi: 10.1212/01.WNL.0000133134.68143.2E [DOI] [PubMed] [Google Scholar]
- 11.Where is Abeokuta, Nigeria?/Where is Abeokuta, Nigeria Located in The World?/Abeokuta Map - WorldAtlas.com. [cited April14, 2016] Available from: http://www.worldatlas.com/af/ng/og/where-is-abeokuta.html. Accessed December20, 2019.
- 12.Wahab KW, Ugheoke AJ. Migraine: prevalence and associated disability among Nigerian undergraduates. Can J Neurol Sci. 2009;36(2):216–221. doi: 10.1017/S0317167100006570 [DOI] [PubMed] [Google Scholar]
- 13.Ojini FI, Okubadejo NU, Danesi MA. Prevalence and clinical characteristics of headache in medical students of the University of Lagos, Nigeria. Cephalalgia. 2009;29(4):472–477. doi: 10.1111/j.1468-2982.2008.01766.x [DOI] [PubMed] [Google Scholar]
- 14.Mitsikostas DD, Gatzonis S, Thomas A, Kalfakis N, IIias A, Papageoergiou C. An epidemiological study of headaches among medical students in Athens. Headache. 1996;36(9):561–564. doi: 10.1046/j.1526-4610.1996.3609561.x [DOI] [PubMed] [Google Scholar]
- 15.Wöber-Bingöl C. Epidemiology of migraine and headache in children and adolescents. Curr Pain Headache Rep. 2013;17(6):341. doi: 10.1007/s11916-013-0341-z [DOI] [PubMed] [Google Scholar]
- 16.Ofovwe GE, Ofili AN. Prevalence and impact of headache and migraine among secondary school students in Nigeria. Headache. 2010;50(10):1570–1575. doi: 10.1111/hed.2010.50.issue-10 [DOI] [PubMed] [Google Scholar]
- 17.Krogh A-B, Larsson B, Salvesen Ø, Linde M. Assessment of headache characteristics in a general adolescent population: a comparison between retrospective interviews and prospective diary recordings. J Headache Pain. 2016;17(1):14. doi: 10.1186/s10194-016-0602-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vetvik KG, Macgregor EA, Lundqvist C, Russell MB. Prevalence of menstrual migraine: a population-based study. Cephalalgia. 2014;34(4):280–288. doi: 10.1177/0333102413507637 [DOI] [PubMed] [Google Scholar]
- 19.Granella F, Sances G, Allais G, et al. Characteristics of menstrual and nonmenstrual attacks in women with menstrually related migraine referred to headache centres. Cephalalgia. 2004;24(9):707–716. doi: 10.1111/j.1468-2982.2004.00741.x [DOI] [PubMed] [Google Scholar]
- 20.Crawford MJ, Lehman L, Slater S, et al. Menstrual migraine in adolescents. Headache. 2009;49(3):341–347. doi: 10.1111/hed.2009.49.issue-3 [DOI] [PubMed] [Google Scholar]
- 21.Martin VT, Behbehani M. Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis–part 2. Headache. 2006;46(3):365–386. doi: 10.1111/hed.2006.46.issue-3 [DOI] [PubMed] [Google Scholar]
- 22.Stewart WF, Lipton RB, Chee E, Sawyer J, Silberstein SD. Menstrual cycle and headache in a population sample of migraineurs. Neurology. 2000;55(10):1517–1523. doi: 10.1212/WNL.55.10.1517 [DOI] [PubMed] [Google Scholar]
- 23.Oshinaike O, Ojo O, Okubadejo N, Ojelabi O, Dada A. Primary headache disorders at a tertiary health facility in Lagos, Nigeria: prevalence and consultation patterns. Biomed Res Int. 2014;2014:782915. doi: 10.1155/2014/782915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pavlović JM, Stewart WF, Bruce CA, et al. Burden of migraine related to menses: results from the AMPP study. J Headache Pain. 2015;16:24. doi: 10.1186/s10194-015-0503-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Statistics | At a glance: Nigeria | UNICEF. [cited April13, 2016] Available from: http://www.unicef.org/infobycountry/nigeria_statistics.html. Accessed December20, 2019.