Abstract
The American Diabetes Association and the European Association for the Study of Diabetes have briefly updated their 2018 recommendations on management of hyperglycemia, based on important research findings from large cardiovascular outcomes trials published in 2019. Important changes include: 1) the decision to treat high-risk individuals with a glucagon-like peptide 1 (GLP-1) receptor agonist or sodium–glucose cotransporter 2 (SGLT2) inhibitor to reduce major adverse cardiovascular events (MACE), hospitalization for heart failure (hHF), cardiovascular death, or chronic kidney disease (CKD) progression should be considered independently of baseline HbA1c or individualized HbA1c target; 2) GLP-1 receptor agonists can also be considered in patients with type 2 diabetes without established cardiovascular disease (CVD) but with the presence of specific indicators of high risk; and 3) SGLT2 inhibitors are recommended in patients with type 2 diabetes and heart failure, particularly those with heart failure with reduced ejection fraction, to reduce hHF, MACE, and CVD death, as well as in patients with type 2 diabetes with CKD (estimated glomerular filtration rate 30 to ≤60 mL min–1 [1.73 m]–2 or urinary albumin-to-creatinine ratio >30 mg/g, particularly >300 mg/g) to prevent the progression of CKD, hHF, MACE, and cardiovascular death.
The American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) requested a brief update of the 2018 recommendations on management of hyperglycemia (1,2), based on the important research findings published in 2019, with a particular focus on new data from large cardiovascular outcomes trials (CVOTs). The authors began work on the brief update in July 2019 and submitted it for publication in Diabetes Care and Diabetologia in October 2019. Work was conducted over a series of phone calls and by electronic interactions. This brief update provides a summary of the implications of this new evidence on recommendations for the management of hyperglycemia in type 2 diabetes (see text box), which will be addressed more fully in the ADA Standards of Medical Care in Diabetes—2020 (https://professional.diabetes.org/SOC). It should be considered in conjunction with the 2018 consensus report (1,2).
Changes to consensus recommendations
|
The Researching Cardiovascular Events with a Weekly Incretin in Diabetes (REWIND) trial of the glucagon-like peptide 1 (GLP-1) receptor agonist dulaglutide included a greater proportion of individuals with type 2 diabetes with high cardiovascular risk but without prior established cardiovascular disease (CVD) (68.5%) and with longer follow-up (median 5.4 years) than prior CVOTs (3). The primary major adverse cardiovascular event (MACE) outcome occurred in 2.7 per 100 patient-years with a hazard ratio (HR) of 0.88 (95% CI 0.79, 0.99) in favor of dulaglutide. There was no difference in the MACE effect in the subpopulations with and without a history of CVD, although the treatment effect of dulaglutide did not reach statistical significance when the groups were considered separately. Most other CVOTs with GLP-1 receptor agonists have included a minority of patients with risk factors only but without evidence of benefit on MACE outcomes in the lower-risk subgroups. Whether the differences in outcomes in trial subgroups without established CVD are related to study details or to the assigned therapy is uncertain. In REWIND, prior CVD was defined as a history of myocardial infarction, ischemic stroke, unstable angina with electrocardiogram (ECG) changes, myocardial ischemia on imaging or stress test, or coronary, carotid, or peripheral revascularization. We previously recommended that established CVD was a compelling indication for treatment with a GLP-1 receptor agonist or sodium–glucose cotransporter 2 (SGLT2) inhibitor. We now also suggest that to reduce risk of MACE, GLP-1 receptor agonists can also be considered in patients with type 2 diabetes without established CVD with indicators of high risk, specifically, patients aged 55 years or older with coronary, carotid, or lower extremity artery stenosis >50%, left ventricular hypertrophy, an estimated glomerular filtration rate (eGFR) <60 mL min–1 [1.73 m]–2, or albuminuria. To date, the level of evidence to support the use of GLP-1 receptor agonists for primary prevention is strongest for dulaglutide but lacking for other GLP-1 receptor agonists.
The Dapagliflozin Effect on Cardiovascular Events–Thrombolysis in Myocardial Infarction 58 (DECLARE–TIMI 58) trial compared the SGLT2 inhibitor dapagliflozin with placebo and also enrolled a greater proportion of participants with type 2 diabetes without prior established CVD but with multiple risk factors (59.4%) and with longer follow-up (median 4.2 years) than other SGLT2 inhibitor trials (4). Dapagliflozin demonstrated cardiovascular (CV) safety but not a benefit for the MACE end point (HR 0.93; 95% CI 0.84, 1.03). Dapagliflozin was associated with benefit for the coprimary efficacy end point of CV death or hospitalization for heart failure (hHF) with HR 0.83 (95% CI 0.73, 0.95) as well as renal end points. For MACE, the HR in the multiple risk factor group without established atherosclerotic vascular disease was 1.01, but this group had strong evidence for benefit for the composite of CV death or hHF. Meta-analysis of the SGLT2 inhibitor CVOTs suggests a class effect to reduce hHF and chronic kidney disease (CKD) progression across high and lower CVD risk subgroups with no effect on MACE in the absence of established atherosclerotic vascular disease (5).
Analysis of two SGLT2 inhibitor CVOTs, DECLARE–TIMI 58 (6) and the Canagliflozin Cardiovascular Assessment Study (CANVAS) Program (7), suggests that the benefits of SGLT2 inhibitors for hHF, MACE, and CV death are greatest for those individuals with preexisting heart failure with reduced ejection fraction (HFrEF) compared with those without HFrEF. It is important to note that hHF was a secondary outcome, relatively low numbers of patients had HF at baseline, and data on ejection fraction (EF) were only available for a proportion of patients. In DECLARE–TIMI 58, individuals with HF but no reduction of EF as well as those without HF did not seem to benefit from dapagliflozin treatment to lower MACE and CV death outcomes. The benefit for hHF was strongest for those who at baseline had an EF <30%, strong for those with an EF <45%, and marginal for those with an EF ≥45% or those without HF. The Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure (DAPA-HF) trial of dapagliflozin was the first heart failure outcome trial of a diabetes medication (8). Recruitment included patients with and without type 2 diabetes with heart failure and an EF ≤40% and demonstrated benefits for reduction of the primary composite end point of CV death, hHF, and urgent HF visits, as well as for HF events and mortality (CV and total) considered separately. We now suggest that SGLT2 inhibitors are recommended in patients with type 2 diabetes and HF, particularly those with HFrEF, to reduce hHF, MACE, and CV death.
The REWIND trial of the GLP-1 receptor agonist dulaglutide had no lower limit to HbA1c for eligibility and demonstrated equivalent efficacy for reduction of MACE above and below the median HbA1c of 55 mmol/mol (7.2%) (3). None of the CVOTs of SGLT2 inhibitors with primary MACE end points have recruited patients with an HbA1c <48 mmol/mol (<6.5%), and there is little data to inform clinical decision making for patients with an HbA1c <53 mmol/mol (<7%) (9). However, the outcome benefits observed in the CVOTs do not appear restricted to patients with an elevated HbA1c. That said, the DAPA-HF trial recruited patients with HFrEF with and without diabetes (8). The benefit for reduction of mortality rate and HF events with dapagliflozin was significant in both subgroups, suggesting that the effects of dapagliflozin on these end points is independent of HbA1c (8). We now recommend that in appropriate high-risk individuals with established type 2 diabetes, the decision to treat with a GLP-1 receptor agonist or SGLT2 inhibitor to reduce MACE, hHF, cardiovascular death, or CKD progression should be considered independently of baseline HbA1c or individualized HbA1c target. That said, there are no specific analyses addressing HbA1c <48 mmol/mol (<6.5%). We continue to recommend that substituting a drug with known CVD, CKD, and hHF benefit for one without known benefit in high-risk patients is reasonable when patients are at individualized glycemic targets.
The Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trial of the SGLT2 inhibitor canagliflozin was the first renal outcome trial of a diabetes medication (10) with a primary composite end point of end-stage kidney disease (dialysis, transplantation, or a sustained eGFR of <15 mL min–1 [1.73 m]–2), a doubling of the serum creatinine level, or death from renal or cardiovascular causes. The trial recruited patients with type 2 diabetes and CKD on the maximally tolerated dose of ACE inhibitors or angiotensin receptor blockers with a urinary albumin-to-creatinine ratio (UACR) of 300–5,000 mg/g and an eGFR of 30 to <90 mL min–1 [1.73 m]–2. This trial demonstrated a clear benefit of canagliflozin (100 mg) on multiple renal end points, including progression to end-stage kidney disease, and on cardiovascular mortality, MACE, and hHF. Furthermore, the CREDENCE results demonstrated that the benefits conferred by canagliflozin in terms of reducing MACE, hHF, cardiovascular mortality, and renal end points were similar regardless of baseline status for cardiovascular or CKD grade 2–3 (11). We now recommend that SGLT2 inhibitors should be used to prevent hHF, MACE, and CV death and the progression of CKD in patients with type 2 diabetes with CKD. The benefits are clear-cut for those with UACR >300 mg/g and eGFR 30–90 mL min–1 [1.73 m]–2 and less well established for lesser grades of CKD based on secondary end point analyses of the CVOT.
A concern in the CANVAS Program was the increased risk of amputation with canagliflozin compared with placebo (7). In CREDENCE (10), although the risk of amputation was higher overall than in other SGLT2 inhibitor trials, no significant increase in risk was observed with canagliflozin 100 mg versus placebo (HR 1.11; 95% CI 0.79, 1.56). This may be due to the risk mitigation strategies employed: exclusion of patients with a history of a traumatic amputation within 12 months of screening, or an active foot ulcer, osteomyelitis, gangrene, or critical ischemia of the lower extremity within 6 months of screening; and interruption of therapy for emergence of any of the above with careful consideration of the individual risks and benefits prior to restarting canagliflozin after resolution of the event. We now recommend that patients with foot ulcers or at high risk for amputation should only be treated with SGLT2 inhibitors after careful shared decision making around risks and benefits with comprehensive education on foot care and amputation prevention.
Based on the studies published thus far, we believe that for patients with type 2 diabetes and established atherosclerotic CVD (such as those with prior myocardial infarction, ischemic stroke, unstable angina with ECG changes, myocardial ischemia on imaging or stress test, or revascularization of coronary, carotid, or peripheral arteries) where MACE is the gravest threat, that the level of evidence for MACE benefit is greatest for GLP-1 receptor agonists.
The Peptide Innovation for Early Diabetes Treatment 6 (PIONEER 6) cardiovascular safety trial of oral semaglutide, a GLP-1 receptor agonist, involved 3,183 patients with type 2 diabetes followed for only a median of 16 months, but it provided adequate demonstration of cardiovascular safety (HR 0.79; 95% CI 0.57, 1.11) and a strong signal for reduction of CV mortality rate (HR 0.49; 95% CI 0.27, 0.92) (12). This formulation of semaglutide has been approved for marketing in the U.S. and a decision in the European Union is expected soon.
For patients with or without established atherosclerotic CVD, but with HFrEF or CKD (eGFR 30 to ≤60 mL min–1 [1.73 m]–2 or UACR >30 mg/g, particularly UACR >300 mg/g), the level of evidence for benefit is greatest for SGLT2 inhibitors. For patients with type 2 diabetes at low cardiovascular risk and without CKD, there have been no studies to examine the cardiovascular or renal benefit of GLP-1 receptor agonists or SGLT2 inhibitors.
Some meta-analyses (5,13,14) suggest the presence of heterogeneity in estimates for MACE and CV death with GLP-1 receptor agonists, although this is mostly due to the results of a single trial with lixisenatide. Likewise, there is some heterogeneity in the estimate for CV death with SGLT2 inhibitors. Whether differences in point estimates of benefits and harms are the result of differences in the effects of the medications, the design and conduct of the trials, or chance effects is uncertain. Attention to patient-specific factors and preferences, product labeling, meta-analyses, and the primary research reports should drive individualized clinical decision making with regard to prescribing particular medications within a class. For many patients, treatment with a GLP-1 receptor agonist or SGLT2 inhibitor in some health care settings involves considerable direct cost to them, and the impact of this on their overall well-being needs to be factored into decision making.
The Cardiovascular Outcome Study of Linagliptin Versus Glimepiride in Type 2 Diabetes (CAROLINA) trial randomized adults at high cardiovascular risk to receive the dipeptidyl peptidase 4 (DPP-4) inhibitor linagliptin or to receive the sulfonylurea glimepiride to evaluate a primary MACE end point. No between-group difference in the primary end point was demonstrated (HR 0.98; 95% CI 0.84, 1.14). At trial end, for linagliptin as compared with glimepiride, there was a 1.5-kg weight loss benefit, no difference in HbA1c or introduction of glucose-lowering medications postbaseline, and substantial benefits in terms of reductions in hypoglycemia, though serious hypoglycemic events were rare with glimepiride (0.45/100 patient-years) (15). Paired with other DPP-4 inhibitor CVOTs, including Cardiovascular and Renal Microvascular Outcome Study with Linagliptin (CARMELINA) (16), which demonstrated the CV safety of linagliptin, this is a reassuring safety signal for glimepiride, an inexpensive and effective sulfonylurea. It is unclear whether these findings extend to other sulfonylureas.
Whereas we previously stated that there was limited evidence for initial combination therapy, the Vildagliptin Efficacy in Combination with Metformin for Early Treatment of Type 2 Diabetes (VERIFY) trial provides additional information. The initial combination of the DPP-4 inhibitor vildagliptin and metformin was shown to provide for a lower rate of secondary failure of glycemic control to HbA1c ≥53 mmol/mol (≥7%) versus metformin alone or the sequential addition of metformin and vildagliptin (17). We now suggest that providers should engage in shared decision making around initial combination therapy in new-onset cases of type 2 diabetes.
There are several major questions regarding the optimal application of new diabetes drugs. One obvious question arising from recent trial results is whether combined use of GLP-1 receptor agonists and SGLT2 inhibitors provides additional benefit for the prevention of MACE, CV death, hHF, and CKD progression. Three trials have demonstrated the HbA1c-lowering and weight-reduction efficacy of the combination (18–20), but none addresses the impact of the combination of the two on cardiorenal end points. A second question that arises from the recent secondary analyses of SGLT2 inhibitor studies is whether there are subsets of patients who benefit disproportionately, or very little, from treatment with the newer diabetes drugs. The emerging evidence that SGLT2 inhibitors may be particularly useful in preventing adverse outcomes in patients with diabetes with HFrEF raises the possibility of more targeted use of these agents. Finally, the mechanism(s) of action by which GLP-1 receptor agonists and SGLT2 inhibitors confer cardiorenal benefit in diabetes are not understood. Research in this area will be very useful in optimizing the now clear potential of drugs for diabetes to mitigate the cardiovascular and renal complications of the disease.
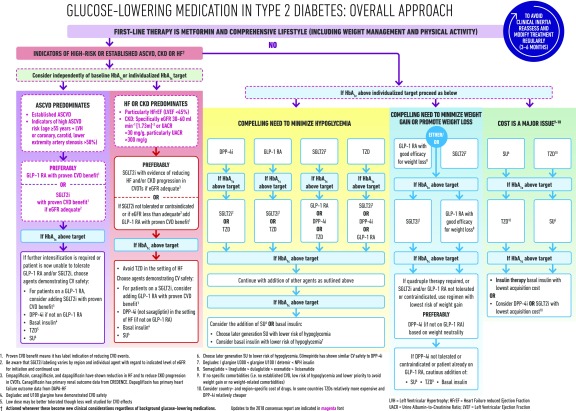
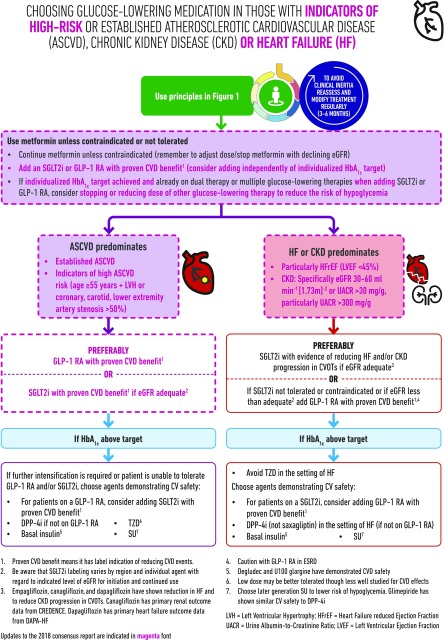
Modifications to the main figures of the prior publication are suggested as shown in Figs. 1 and 2.
Figure 1.
Glucose-lowering medication in type 2 diabetes: overall approach. RA, receptor agonist, SU, sulfonylureas; TZD, thiazolidinediones. Adapted from Davies et al. (1). © American Diabetes Association and European Association for the Study of Diabetes, 2018.
Figure 2.
Choosing glucose-lowering medication in those with indicators of high-risk or established atherosclerotic cardiovascular disease (ASCVD), chronic kidney disease (CKD), or heart failure (HF). RA, receptor agonist; SU, sulfonylureas; TZD, thiazolidinediones. Adapted from Davies et al. (1). © American Diabetes Association and European Association for the Study of Diabetes, 2018.
Article Information
Acknowledgments. The authors would like to thank William T. Cefalu (Director of the Division of Diabetes, Endocrinology, and Metabolic Diseases at the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health) for his review. The authors would like to acknowledge M. Saraco (Managing Director, Scientific & Medical Affairs) from ADA, as well as M. Hata (Executive Assistant) and P. Niemann (Executive Assistant) from EASD for their assistance. The authors would also like to acknowledge M. Bonar (Creative Director) and C. Franklin (Design Assistant) from the Leicester Diabetes Centre, Leicester, U.K., who provided considerable support in drafting and amending the figures. The authors also acknowledge the careful review and helpful suggestions of the members of the ADA Professional Practice Committee and the EASD Committee on Clinical Affairs.
Funding. This activity was funded by the American Diabetes Association and the European Association for the Study of Diabetes.
Duality of Interest. J.B.B. has provided consultation to Adocia, AstraZeneca, Eli Lilly, MannKind, NovaTarg, Novo Nordisk, Senseonics, and vTv Therapeutics with fees paid to the University of North Carolina. He has received grant support from Novo Nordisk, Sanofi, and vTv Therapeutics. He is a consultant to Cirius Therapeutics Inc., CSL Behring, and Neurimmune AG. He holds stock options in Mellitus Health, PhaseBio, Stability Health, and Pendulum Therapeutics. He is supported by a grant from the National Institutes of Health (UL1TR002489). D.J.W. reports serving on a Data Monitoring Committee for Novo Nordisk. A.T. reports nonfinancial support from EASD during the conduct of the study, grants and other from Boehringer Ingelheim, grants and other from Novo Nordisk, other from Novartis, grants and other from Sanofi, grants and other from AstraZeneca, grants from GlaxoSmithKline, and grants and other from the European Foundation for the Study of Diabetes (EFSD) outside the submitted work. P.R. reports grants, nonfinancial support, and other from Novo Nordisk, grants and other from AstraZeneca, other from Bayer, other from Boehringer Ingelheim, other from Merck Sharp & Dohme, and other from Eli Lilly during the conduct of the study. G.M. reports grants and personal fees from Novo Nordisk, personal fees from Johnson & Johnson, and personal fees from Fractyl Inc. during the conduct of the study. C.M. reports grants and fees from Novo Nordisk, grants and fees from Sanofi, grants and fees from Merck Sharp & Dohme, grants and fees from Eli Lilly and Company, grants and fees from Novartis, fees from AstraZeneca, grants and fees from Boehringer Ingelheim, fees from Roche Diagnostics, grants and fees from Medtronic, and grants and fees from ActoBio Therapeutics outside the submitted work, with all fees paid to her university. D.A.D’A. reports personal fees from Eli Lilly, Merck, Novo Nordisk, and Intarcia and grants from Merck and Ligand during the conduct of the study, personal fees from Lilly, Merck, Novo Nordisk, and Intarcia, and grants from Merck and Ligand outside the submitted work. M.J.D. reports personal fees and grants from Boehringer Ingelheim, Janssen, Novo Nordisk, and Sanofi and personal fees from AstraZeneca, Eli Lilly, Gilead Sciences Ltd., Intarcia/Servier, Merck Sharp & Dohme, Mitsubishi Tanabe Pharma Corporation, and Takeda Pharmaceuticals International Inc. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. All authors were responsible for drafting the article and revising it critically for important intellectual content. All authors approved the version as published.
Footnotes
M.J.D. and J.B.B. were co-chairs for the Consensus Statement Writing Group. D.D’A. and D.J.W. were the writing group members for the ADA. C.M., G.M., P.R., and A.T. were the writing group members for the EASD.
This article is being simultaneously published in Diabetologia (https://doi.org/10.1007/s00125-019-05039-w) and Diabetes Care (https://doi.org/10.2337/dci19-0066) by the European Association for the Study of Diabetes and the American Diabetes Association.
This article is featured in a podcast available at http://www.diabetesjournals.org/content/diabetes-core-update-podcasts.
References
- 1.Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2018;41:2669–2701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2018;61:2461–2498 [DOI] [PubMed] [Google Scholar]
- 3.Gerstein HC, Colhoun HM, Dagenais GR, et al.; REWIND Investigators . Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet 2019;394:121–130 [DOI] [PubMed] [Google Scholar]
- 4.Wiviott SD, Raz I, Bonaca MP, et al.; DECLARE–TIMI 58 Investigators . Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2019;380:347–357 [DOI] [PubMed] [Google Scholar]
- 5.Zelniker TA, Wiviott SD, Raz I, et al. Comparison of the effects of glucagon-like peptide receptor agonists and sodium-glucose cotransporter 2 inhibitors for prevention of major adverse cardiovascular and renal outcomes in type 2 diabetes mellitus. Circulation 2019;139:2022–2031 [DOI] [PubMed] [Google Scholar]
- 6.Kato ET, Silverman MG, Mosenzon O, et al. Effect of dapagliflozin on heart failure and mortality in type 2 diabetes mellitus. Circulation 2019;139:2528–2536 [DOI] [PubMed] [Google Scholar]
- 7.Figtree GA, Rådholm K, Barrett TD, et al. Effects of canagliflozin on heart failure outcomes associated with preserved and reduced ejection fraction in type 2 diabetes mellitus. Circulation 2019;139:2591–2593 [DOI] [PubMed] [Google Scholar]
- 8.McMurray JJV, Solomon SD, Inzucchi SE, et al.; DAPA-HF Trial Committees and Investigators . Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 21 November 2019 [Epub ahead of print]. DOI: 10.1056/NEJMoa1911303 [Google Scholar]
- 9.Inzucchi SE, Kosiborod M, Fitchett D, et al. Improvement in cardiovascular outcomes with empagliflozin is independent of glycemic control. Circulation 2018;138:1904–1907 [DOI] [PubMed] [Google Scholar]
- 10.Perkovic V, Jardine MJ, Neal B, et al.; CREDENCE Trial Investigators . Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med 2019;380:2295–2306 [DOI] [PubMed] [Google Scholar]
- 11.Mahaffey KW, Jardine MJ, Bompoint S, et al. Canagliflozin and cardiovascular and renal outcomes in type 2 diabetes mellitus and chronic kidney disease in primary and secondary cardiovascular prevention groups. Circulation 2019;140:739–750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Husain M, Birkenfeld AL, Donsmark M, et al.; PIONEER 6 Investigators . Oral semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2019;381:841–851 [DOI] [PubMed] [Google Scholar]
- 13.Giugliano D, Maiorino MI, Bellastella G, Longo M, Chiodini P, Esposito K. GLP-1 receptor agonists for prevention of cardiorenal outcomes in type 2 diabetes: an updated meta-analysis including the REWIND and PIONEER 6 trials. Diabetes Obes Metab 2019;21:2576–2580 [DOI] [PubMed] [Google Scholar]
- 14.Kristensen SL, Rørth R, Jhund PS, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol 2019;7:776–785 [DOI] [PubMed] [Google Scholar]
- 15.Rosenstock J, Kahn SE, Johansen OE, et al.; CAROLINA Investigators . Effect of linagliptin vs glimepiride on major adverse cardiovascular outcomes in patients with type 2 diabetes: the CAROLINA randomized clinical trial. JAMA. 19 September 2019 [Epub ahead of print]. DOI: 10.1001/jama.2019.13772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosenstock J, Perkovic V, Johansen OE, et al.; CARMELINA Investigators . Effect of linagliptin vs placebo on major cardiovascular events in adults with type 2 diabetes and high cardiovascular and renal risk: the CARMELINA randomized clinical trial. JAMA 2019;321:69–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Matthews DR, Paldánius PM, Proot P, Chiang Y, Stumvoll M, Del Prato S; VERIFY study group . Glycaemic durability of an early combination therapy with vildagliptin and metformin versus sequential metformin monotherapy in newly diagnosed type 2 diabetes (VERIFY): a 5-year, multicentre, randomised, double-blind trial. Lancet 2019;394:1519–1529 [DOI] [PubMed] [Google Scholar]
- 18.Zinman B, Bhosekar V, Busch R, et al. Semaglutide once weekly as add-on to SGLT-2 inhibitor therapy in type 2 diabetes (SUSTAIN 9): a randomised, placebo-controlled trial. Lancet Diabetes Endocrinol 2019;7:356–367 [DOI] [PubMed] [Google Scholar]
- 19.Ludvik B, Frías JP, Tinahones FJ, et al. Dulaglutide as add-on therapy to SGLT2 inhibitors in patients with inadequately controlled type 2 diabetes (AWARD-10): a 24-week, randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol 2018;6:370–381 [DOI] [PubMed] [Google Scholar]
- 20.Frías JP, Guja C, Hardy E, et al. Exenatide once weekly plus dapagliflozin once daily versus exenatide or dapagliflozin alone in patients with type 2 diabetes inadequately controlled with metformin monotherapy (DURATION-8): a 28 week, multicentre, double-blind, phase 3, randomised controlled trial. Lancet Diabetes Endocrinol 2016;4:1004–1016 [DOI] [PubMed] [Google Scholar]