Abstract
The intercession of widespread Internet access and use of mobile devices and wearables has increased the attention to the field of digital health as a novel means of providing patient care. Although substantial advancements have been made toward the development of novel technologies and identification of therapeutic areas of impact, the issue remains of how to educate future health professionals to work in an era of digital tools. This perspective piece seeks to highlight areas of concern related to subset areas of the digital health environment and provide potential educational pathways to prepare students.
Keywords: Digital health, education, mHealth, digital therapeutics
The advent of rapid technological development of mobile device and access to the Internet has drastically changed society. Nonetheless, health care itself is equally seeing multiple new inroads for technology while also outpacing integration. Although terms like e-health (electronic health) and mHealth (mobile health) have been around for more than 20 years, in the past decade the topic of digital health has come into precedence, in part, due to novel tools and devices which have come onto the market. Arguably, one of the biggest drivers has been a boon of health technology into the medical space, including products and services from traditional health-oriented companies as well as a slew of new start-ups and involvement from outside tech companies not traditionally thought to be interested in health care (eg, Apple, Google).1
Coupled with the issues of technology advancements, we are also facing the next generational shift among incoming students to our schools. The millennial generation is now past, and Gen Z (those born after 1997) are now leaving high school and entering higher education.2 These students, who may be starting predoctoral curriculums or other health sciences, are inclined to be “digital natives” in accepting the use of technology in their lives, though not necessarily well-versed in how to use it. The expectation for this generation to anticipate the use of technology may be beyond what their professors can envision in patient care.3
Taking this into consideration, the health sciences face a dilemma of how best to address the integration of digital health services into their educational curricula. Arguably, it is in the best interest for health professions to prepare the next generation of practitioners to work in a health landscape that may see significant disruption due to such technological upheavals. We only have to look at the current issues facing health profession schools looking to integrate electronic health record (EHR) systems into their teaching to appreciate the possible burden of taking on these other issues. It is the goal of this commentary piece to identify and posit means of addressing these challenges that will arise in the very near future.
What Are Digital Health Areas of Focus?
Currently, there is no universal, formal definition of digital health, though acceptable considerations such as those from the Food and Drug Administration (FDA) include categories such as health information technology (HIT), wearable devices, telehealth and telemedicine, personalized medicine, and general wellness.4 The FDA recognizes that digital health can decrease costs, increase scalability of access to medical care (through wireless interventions), and make medicine more personalized for patients.4 Although several of these areas have been discussed about in the medical community for more than a decade, the widespread adoption of mobile devices and Internet access has quickly moved these areas into practical applications of use. Other areas, aside from using digital health to reach patients for care, include the aspect of data use and the issue of prescribing software as medical care.5 In comparison, others have defined digital health in cultural contexts for stakeholders or a context for health care innovation.6-10 Taking these definitions and positions into account, Table 1 encompasses areas of digital health that health educators will likely focus on in relationship to clinical training their learners will undergo.
Table 1.
Areas of digital health.
| Topic area | Description |
|---|---|
| Mobile medical applications | “Medical devices that are mobile apps, meet the definition of a medical device, and are an accessory to a regulated medical device or transform a mobile platform into a regulated medical device”11 |
| Digital therapeutics | Regulated, evidence-based software intervention that can be independent or complementary to other therapies.10 |
| Telehealth | “Delivery and facilitation of health and health-related services including medical care, provider and patient education, health information services, and self-care via telecommunications and digital communication technologies”12 |
| Wearable devices and sensors | “Wearable electronics are devices that can be worn or mated with human skin to continuously and closely monitor an individual’s activities, without interrupting or limiting the user’s motion”13 |
| Digital biomarkers | Hardware-software based measurement of physiological data in real time for prognostic or diagnostic measurements14 |
What Are the Implications of Digital Health in Education?
Data, the new so-called “oil boom” of this century, are quickly being identified as the penultimate source of novel means of generating outcomes through asynchronous collection from patients as they go about their daily lives. With many companies tracking how their consumers use their smartphones (eg, search history), their geolocation and movement habits (ie, GPS), and thoughts and attitudes (eg, social media), it comes as no surprise that companies and organizations are looking toward the health aspects of this data. Questions are quickly being formed as to what data can be feasible to collect and generate about our patients, especially with the growth of adoption of wearable devices (eg, fitness trackers, smart watches). In addition, there are questions as to what meaningful use these data can have for clinical insights and actions. This, in turn, has led to a “Pandora’s box” regarding how to educate health students, as gaps in how patient care will be delivered are now becoming apparent.15-18 One axiom of medical training is not to order a test if you are unprepared to deal with the results. This inclination is regarding a health professional in the position of power to dictate what they want to know, assuming they are following standard clinical practice. However, in this digital age and with many of the technological issues that follow, we are now facing a point where patients may collect and choose to share data that we as clinicians were not prepared to take into account. Then, as an add-on, engaging with a patient through a digital mechanism (eg, teleservice) will need to be a function in which clinicians are comfortable engaging with their patients.19,20
For example, consider medication adherence. Traditionally, a medication may be prescribed and dispensed to a patient for them to self-actualize treatment through their self-administration. Clinical effectiveness is gauged based on response. When a response is not seen, a patient may be questioned on their adherence, such as in the case of hypertension where blood pressure may vary depending on medication use. Adherence may be assessed through a patient interview, but subjectivity is an issue based on patient recall bias. Other data may also be available, such as billing claims, which can be interpreted as a medication possession ratio. These data points can indicate if a patient has at least purchased a prescription. Aside from that limited data, the only way to directly confirm that a patient takes their medication is through directly observed therapy. However, novel technologies such as virtually observed therapy (VOT), bioingestible sensors,21 and even smart pill bottles and boxes, offer more objective data on patients’ self-administration habits. In the past, clinicians may have been “in the dark” on whether a patient takes their medication. Through technology today, we can now know. The consideration of how to navigate this new data set is troubling. For instance, outside of a hospital or a patient in a facility, clinicians are not trained to handle continuous clinical data. This will be an issue with the rise of real-time data transmission from patients electing to use wearable devices and apps that will transmit data as it is collected.
Aside from digital health compounding the present challenge of data overload, a further conundrum faces future clinicians: advanced data analysis methods. Current practitioners and educators do not foreseeably grasp this challenge today. Much talk is given to the use of “artificial intelligence” (AI) in much of the current software being developed. Whether these current technologies warrant to be called true “AI” is arguable, but machine learning and related topics are indeed making inroads into health care management. How should future practitioners deal with so-called AI-generated suggestions or analyses of their patients’ health status? Should future clinicians have a basic understanding of data analytics or HIT, currently not adopted by most institutions, for teaching accreditation or are we seeing a crossroads in how future clinicians should be taught?
Finally, the idea of prescribing and dispensing digital products for patients will also be a conundrum. Digital therapeutics is quickly being identified as a novel means of delivering care to patients that use much of the above identified technology.22 These evidence-based software, often delivered as apps on a mobile device, purport to manage and treat patient health conditions. This goes beyond prescribing a medication, where many students spend hours understanding the underlying pharmacology and pharmacokinetics of their active ingredients in the body based on their understanding of human anatomy and physiology. Rather, we are seeing the concept of software, whose inner workings most students could not grasp without an education in computer science, being prescribed for patient care. Considerations on how this impacts workflow and patient engagement still need to be processed with these technologies, which are now being cleared by the FDA for patient use.23,24
The digital health technologies available directly to patient consumers are outpacing the clinical integration of these technologies into practice. Sensors are quickly moving into the space of routinely worn wearables. The Apple Watch can measure electrocardiogram data and report if a patient is experiencing atrial fibrillation, which would need to be confirmed by a clinician.25 Data meaningful to medical practice, such as sleeping or daily exercise habits, have still not been adopted into traditional clinical guidelines or formally addressed in patient care training. This lack of integration in practice does not deter our current patients from tapping into these devices. Democratized health service is quickly reaching its peak, driving the need to understand how data are collected, assessed, and used.
Current Challenges
The above-mentioned issues present a real and present challenge to educators in the health sciences. Concurrently, these technological developments are expected to exponentially grow and expand their reach in health care and that leaves educators the responsibility of keeping up to date regarding current trends in digital health innovations. Although “futurism” itself is not the responsibility of an educator, it is reasonable to expect that adoption and understanding of landscape movements must be undertaken.
The life cycle of these technologies’ development and their ambiguous role in clinical effectiveness make for challenges in establishing standards for education regarding digital health. For future and present clinicians, there should be an emphasis on foundational skills regarding assessment of relevance for these technologies to contextualized clinical use.26 For example, a clinician would not need to know all medication reminder applications available for mobile phones. They should, however, be able to assess individual patient needs, such as history of diagnosis and digital literacy, to make a meaningful, actionable recommendation to patients. These foundational skills complement and extend current clinical skills in educational standards. This extension of skills also applies to topics such as policy and regulations. Just as students learn about the drug development and the FDA approval process incorporating chemists, statisticians, and lawyers, students should have a broad but functional understanding of the FDA medical device classification as it applies to digital health. New technologies will continue to emerge and fade in practice and the FDA will continue its challenge to define, regulate, and/or approve these technologies. The challenge will be for educators and practioners to incorporate these dynamic elements of digital health in practice.
The adoption of digital health topics in effective educational methods may consider and use multiple approaches, though each with a challenge to consider. One may adopt technological interventions into current didactic classes and laboratory assessments. This could be similar to a therapeutic discussion on medication management of a disease along with digital management. Hands-on training with devices and teleservices could similarly be used in laboratory and hands-on simulations, such as a remote objective structured clinical examination (OSCE) assessment. Issues that will be present with this approach include short technology life cycles. There would be question as to the use of teaching demos and relevance in the lab or classroom for a period of time without significant depreciation of value due to newer technologies coming to the market. Educators will need to make tactical decisions regarding what companies to possibly partner with regarding technology to teach about and be able to respond accordingly with adjustments in teaching models if such technologies become integral to a curriculum area. Second, patient interactions and e-professionalism must also be adopted and explored alongside students’ digital literacy and abilities as they are fundamental to the field of digital health. This could include appropriate body language and effective patient communication through virtual interactions. This will be increasingly relevant as changing markets toward telehealth services become predominant and the need for future practitioners fit the need of future employers. However, determining best practices are yet to be determined. Third, an expansion on real-time disease treatment and appreciation for data management can also be explored through clinical coursework regarding managing chronic and urgent patient conditions. Again, best practice on this approach must be discussed further and research will be needed to ascertain educational needs of future practitioners. This may be feasible by engaging current early adopters and health practitioners currently in the digital health space and identifying their frustrations and experiences that may be brought back into the curriculum. Finally, training faculty to understand and use digital health technologies will be key, but also a costly endeavor as no formal training process currently exists. These areas may include data analytics, machine learning, remote patient monitoring, and others relevant to the digital health space. Likely, in time, there will be a standard approach, but at this moment, institutions should identify key faculty with a mind-set conducive to teaching this material and enable their further training and knowledge to bring back to their health programs.
Current Academic Pursuits in Digital Health
The integration of digital health into formal education offers a novel means to engage in interprofessional education (IPE) opportunities. Students across multiple professions can work together to engage in digital health discussion activities that can aim to tackle health solutions and problems based on a technological focus and not necessarily on their clinical capabilities, while still bringing multiple views together.27 Nonetheless, another benefit may be also to use other schools, including computer science and business schools, for activities like a hackathon.28 This has been seen with many health-focused hackathons across the United States targeting multiple health professionals and those with an interest in health care to foster interprofessional insights and disruption in the health space.
Nonetheless, determining how to build out digital health education will be a topic of debate in the coming years.29 Although there have been certificates offered in health informatics, such as from Healthcare Information and Management Systems Society (HIMSS),30 digital health as a topic goes beyond their scopes. Several medical schools are already housing centers for digital health, and it comes as no surprise that they may seek to expand these out to formal educational outputs.31-39 We anticipate that different modalities will be offered based on early adopters currently broadcasting their services, summarized in Table 2. A certificate model may end up being a short-term solution for formal education, such as what UC San Diego will be offering to those with a bachelor’s degree to a scientific or technological field,36 what Tufts Public Health program offers as a Digital Health Communication certificate,37 or even Jefferson with 3 certificates offered in digital health.38 However, these certificates are more geared toward those with an interest in digital health and not necessarily need a health science background. This creates a limitation for health student learners from integrating their clinical knowledge sets with digital health. Conversely, creating a digital health mechanic to teach health students explicitly will be more difficult, especially considering scalability. As such, pursuing a track to digital health knowledge would likely be easier, and on a smaller scale, such as with the Rocky Vista University, which is offering a track in their allopathic medical school.39 Working with outside partners to facilitate expertise, rotations, and clinical experiences will also be a rate-limiting step for programs looking to engage in digital health.
Table 2.
An in-depth look at digital health educational options currently available.
| Institution/program | Program description | Curriculum integration |
|---|---|---|
| Brown Alpert Medical School | Prepare liberal medical education and medical students for an understanding of digital health. Uses student leaders under a faculty advisor with a digital health background. | Course elective in curriculum that students can engage with local experts in the digital health space. |
| Center for Digital Health Innovation (CDHI) at UCSF | CDHI provides expertise in data science, software development, product and project management, EHR integration, and digital health policy development. Works with digital health companies and integrates faculty and students. | No formal integration into curriculum, but offers digital health spot for faculty, staff, and students to be a part of development and innovation strategies. |
| Center for Digital Health at Stanford Medicine | Supports digital health projects and research at Stanford Medicine, along with hosting events and educational seminars. | No formal integration into curriculum. Host multiple elective courses with didactic and interactive sessions with academia and industry personnel providing input. |
| The Center for Digital Health at Icahn School of Medicine at Mount Sinai | Serves as a hub for innovation with clinical researchers, engineers, designers work with academia and industry to create digital health solutions. Focused primarily on research and development with clinical applicability. | No formal integration into curriculum. |
| Center for Digital Health & Data Science at Thomas Jefferson University | Digital health research center focused on design and developing resources for clinical and evaluative digital health research at Thomas Jefferson University, through collaborative work with academics, clinicians, and industry. Aimed at those with a background in health. | No formal integration into curriculum as didactic teaching, but students may work with the center as part of their mandatory scholarly inquiry component for the JeffMD curriculum. Offers 3 certificates, including “digital health design & communication certificate,” “Blockchain for healthcare certificate,” and “digital health entrepreneurship certificate” offered online over the course of 1 year offered through the Institute of Emerging Health Professions at Thomas Jefferson. |
| Rocky Vista University College of Osteopathic Medicine | Digital health track that trains students in AI, remote monitoring, ethics, informatics, telemedicine, analytics, and entrepreneurship. Available for medical students only. | Curriculum integration as a curricular track that students can elect to enroll on their formal medical education. Due to roll out in 2020. |
| Tufts School of Medicine | Digital Strategies for Health Communication certificate is offered using guest speakers that help learners to manage and evaluate the use of Web, social medial, and mobile technologies for health purposes. Aimed at those with a background in health. | No formal integration into curriculum. Certificate is offered in-person over 1 week during the summer. Limited to 20 students per offering. |
| UC San Diego Extension | Digital health certificate offered in collaboration with their school of medicine. Certificate program is focused on data science, mHealth, AI, regulatory, and ethics. Aimed at those with a background in health. | No formal integration into curriculum. Online program focused on public health, administration, ethics, and business commercialization. Certificate completion takes 12-18 months. |
| UMass Center for Digital Health (CDH) | The CDH is a multicampus partnership across the UMass space. Engages in research, education, and working with industry with a digital health focus. | No formal integration into curriculum. |
Abbreviation: EHR, electronic health record.
Future Directions and Curriculum Design Concepts
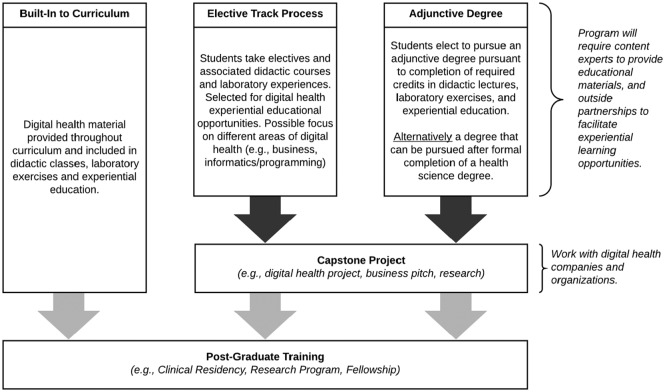
At this time, the most likely low-hanging fruits for digital health education with health science students as a focus would be a track or certificate program as they will be smaller in size and easier to manage. However, this will still require a sustainable model of technology to use in teaching, which could be cost-prohibitive (eg, wearables, VR technology), and appropriate faculty will still need to be recruited.40 Adjunctively, offering a master’s degree may also be a possibility for those seeking to gain further education through an online program during or after completion of their formal health degree. Although digital health is a topic increasingly growing today, it is inevitable that it will just be a part of the global health care education in the future. These ancillary degrees and certificates are an interim solution to the eventual adoption of digital health into the formal health curriculum. Taking that into consideration, we envision several pathways that could be pursued as seen in Figure 1. There may be a future where medical and health science programs will build into their curricula digital health topics as didactic courses, laboratory exercises, and with rotations or clinical experiences. Building digital health into a curriculum would allow learners to have a better grasp of digital health at large and understand implications for clinical practice on graduation instead of a snapshot approach which are limited in learning. Approaches for such components in a curriculum would include an elective track process. Pursuing an elective track conjunctively with the health program curriculum would offer students with an interest in digital health a more formalized approach to gaining knowledge and understanding, and not force learners who many not have an interest in digital health when it is not a mandate of current clinical practice at this time. One of the largest limitations compared with full integration into the curriculum would likely be experiential education, such as clinical rotations which students may not be able to participate and integrate their knowledge. As such, a capstone project may be an easy mechanic to create an output from an elective track process, which could be done with outside partners as well such as local companies or health systems with an interest in digital health. Alternatively, the creation of an adjunctive degree (eg, masters) in digital health could be done that students could due concurrently with their curriculum or offered to those postgraduation. Benefit is likely adoption of online learning to facilitate these learners experience, while also using a capstone project similar to an elective track, as rotations and experiential learning would likely be limited. An elective track or adjunctive degree seems more realistic in the short-term due, in part, to limitations of expanding a curriculum when accreditation bodies are not mandating digital health education at this time. Additional issues with these options include a lack of large digital health experts with backgrounds in education, which the schools would need to gather at scale to teach such a curriculum or be involved in an elective tract or adjunctive degree. It will come down to the health program to grow and foster these relationships or train them internally as discussed prior.
Figure 1.
Digital health training options.
Finally, although not a focus on this piece, education for current health practitioners will also be an issue. Although health programs may seek to build continuing education materials, the issue of digital health education will likely be taken up by health systems or health professional organizations who seek to capitalize on semi-formal education. This may, in turn, foster new opportunities in postgraduate education, like residency or fellowship positions which health students can pursue. However, there are debatable matters on how to best approach this. Continuing medical education (CME) may be the most feasible model to get current practitioners up to speed on digital health at this time. It can be expected that many pharmaceutical companies and digital health companies with products and services will likely seek to initiate many of these CMEs, unless health professional associations take it on themselves. This may lead to some associations or organizations to start creating their own learning suites on digital health, or possible certificate programs as well. It will come down to employer and workforce expectations in the near future to determine the need and viability of creating such educational outreaches. Other considerations include the creation of new organizations or societies that seek to address this current gap and offer their services to all health professionals in the future.
Conclusions
The clinical implications of digital health in patient care will force health science programs to determine the best means to introduce the topic to their learners. Although opportunities are plentiful, faculty development and experts to facilitate learning experiences may not be available at the same scale. The integration of digital health topics into the curriculum will be difficult and many programs may instead elect to offer tracks, certificates, or possible adjunctive degrees to interested students.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests:The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: T.D.A., PharmD, is an advisor for the Digital Therapeutics Alliance and consultant for Eli Lilly, Otsuka Pharmaceutical, and Teva Pharmaceutical. No disclosure or conflicts reported by Dr R.P.
Author Contributions: TDA and RP both equally contributed towards this manuscript.
ORCID iD: Timothy Dy Aungst  https://orcid.org/0000-0002-6914-0218
https://orcid.org/0000-0002-6914-0218
References
- 1. Elenko E, Underwood L, Zohar D. Defining digital medicine. Nat Biotechnol. 2015;33:456-461. [DOI] [PubMed] [Google Scholar]
- 2. Dimock M. Defining generations: where millennials end and generation Z begins. Pew Research Center. January 17, 2019. https://www.pewresearch.org/fact-tank/2019/01/17/where-millennials-end-and-generation-z-begins/. Accessed October 26, 2019.
- 3. Pathipati AS, Azad TD, Jethwani K. Telemedical education: training digital natives in telemedicine. J Med Internet Res. 2016;18:e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Digital health. Food and Drug Administration. https://www.fda.gov/medical-devices/digital-health. Accessed October 20, 2019.
- 5. Shuren J, Patel B, Gottlieb S. FDA regulation of mobile medical apps. JAMA. 2018;320:337-338. [DOI] [PubMed] [Google Scholar]
- 6. Mesko B, Drobni Z, Benyei E, Gergely B, Gyorffy Z. Digital health is a cultural transformation of traditional healthcare. mHealth. 2017;3:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gandhi M, Evans B. What digital health is (and isn’t). Rock Health. April 5, 2013. https://rockhealth.com/what-digital-health-is-and-isnt/. Updated 2017. Accessed December 18, 2019.
- 8. Iyawa GE, Herselman M, Botha A. Digital health innovation ecosystems: from systematic literature review to conceptual framework. 2016;100:244-252. [Google Scholar]
- 9. Sim I. Mobile devices and health. N Engl J Med. 2019;381:956-968. [DOI] [PubMed] [Google Scholar]
- 10. Digital therapeutics: combining technology and evidence-based medicine to transform personalized patient care. Digital Therapeutics Alliance. https://www.dtxalliance.org/wp-content/uploads/2018/09/DTA-Report_DTx-Industry-Foundations.pdf. Accessed October 26, 2019.
- 11. Device Software Functions Including Mobile Medical Applications. Food and Drug Administration. https://www.fda.gov/medical-devices/digital-health/device-software-functions-including-mobile-medical-applications. Accessed October 20, 2019.
- 12. What is Telehealth? NEJM Catalyst. February 1, 2018. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0268. Accessed December 20, 2019.
- 13. Haghi M, Thurow K, Stoll R. Wearable devices in medical internet of things: scientific research and commercially available devices. Healthc Inform Res. 2017;23(1):4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Coravos A, Khozin S, Mandl KD. Developing and adopting safe and effective digital biomarkers to improve patient outcomes. NPJ Digit Med. 2019;2(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Haag M, Igel C, Fischer MR. Digital Teaching and Digital Medicine: a national initiative is needed. GMS J Med Educ. 2018;35:Doc43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chandrashekar P. A digital health preclinical requirement for medical students. Acad Med. 2019;94:749. [DOI] [PubMed] [Google Scholar]
- 17. Vassar L. How to equip new doctors for the digital health frontier. American Medical Association. June 18, 2015. https://www.ama-assn.org/education/accelerating-change-medical-education/how-equip-new-doctors-digital-health-frontier. Accessed on October 26, 2019.
- 18. How to prepare the future generation of physicians. The Medical Futurist. July 24, 2018. https://medicalfuturist.com/how-to-prepare-the-future-generation-of-physicians/. Accessed on October 26, 2019.
- 19. Waseh S, Dicker AP. Telemedicine training in undergraduate medical education: mixed-methods review. JMIR Med Educ. 2019;5:e12515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wernhart A, Gahbauer S, Haluza D. eHealth and telemedicine: practices and beliefs among healthcare professionals and medical students at a medical university. PLoS ONE. 2019;14:e0213067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. FDA approves pill with sensor that digitally tracks if patients have ingested their medication. Food and Drug Administration. November 13, 2017. https://www.fda.gov/news-events/press-announcements/fda-approves-pill-sensor-digitally-tracks-if-patients-have-ingested-their-medication. Accessed October 20, 2019.
- 22. Byambasuren O, Sanders S, Beller E, Glasziou P. Prescribable mHealth apps identified from an overview of systematic reviews. NPJ Digit Med. 2018;1:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Digital Health Innovation Action Plan. Food and Drug Administration. https://www.fda.gov/media/106331/download. Accessed October 20, 2019.
- 24. Digital Health Software Precertification (Pre-Cert) Program. Food and Drug Administration. https://www.fda.gov/medical-devices/digital-health/digital-health-software-precertification-pre-cert-program. Accessed October 20, 2019.
- 25. Apple Watch Series 5 Health. Apple. https://www.apple.com/apple-watch-series-5/health/. Accessed October 26, 2019.
- 26. Car J, Carlstedt-Duke J, Tudor Car L, et al. Digital education in health professions: the need for overarching evidence synthesis. J Med Internet Res. 2019;21: e12913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Aungst TD, Lahoz MR, Evans PJ. Digital health evaluation workshop for interprofessional healthcare students. Digit Health. 2017;3:2055207617740089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Aungst TD. Using a hackathon for interprofessional health education opportunities. J Med Syst. 2015;39:60. [DOI] [PubMed] [Google Scholar]
- 29. McCall M, Spencer E, Owen H, et al. Characteristics and efficacy of digital health education: an overview of systematic reviews. Health Educ J. 2018;77: 497-514. [Google Scholar]
- 30. Healthcare Information and Technology Continuing Education. HIMSS. https://www.himss.org/health-it-certification/continuing-education. Accessed October 26, 2019.
- 31. BIOL 6677: Digital Health. Brown Alpert Medical School. https://www.brown.edu/academics/medical/education/biol-6677-digital-health. Accessed October 26, 2019.
- 32. Center for Digital Health. UCSF. https://www.centerfordigitalhealthinnovation.org/. Accessed October 26, 2019.
- 33. Center for Digital Health. Stanford Medicine. http://med.stanford.edu/cdh.html. Accessed October 26, 2019.
- 34. UMass Center for Digital Health (CDH). https://www.uml.edu/research/digital-health/. Accessed October 26, 2019.
- 35. Center for Digital Health. Icahn School of Medicine at Mount Sinai. https://icahn.mssm.edu/research/digital-health. Accessed October 26, 2019.
- 36. Digital Health. UC San Diego Extension. https://extension.ucsd.edu/courses-and-programs/digital-health. Accessed October 26, 2019.
- 37. Certificate in Digital Health Communication. Tufts School of Medicine. https://publichealth.tufts.edu/graduate-programs/certificates-professional-development/hcom-professional-development/digital. Accessed December, 18 2019.
- 38. Center for Digital Health & Data Science Academic Programs. Thomas Jefferson University; https://www.jefferson.edu/university/emerging-health-professions/centers/Digital-health/academic-programs.html. Accessed December 18, 2019. [Google Scholar]
- 39. Shoup M. Rocky Vista University announces first Digital Health Track to be offered in an osteopathic or allopathic medical school in U.S. St. George News. September 29, 2019. https://www.stgeorgeutah.com/news/archive/2019/09/29/mks-rocky-vista-university-announces-first-digital-health-track-to-be-offered-in-an-osteopathic-medical-school-in-u-s/#.XbTml5NKjOT. Accessed October 26, 2019.
- 40. Fernando J, Lindley J. Lessons learned from piloting mHealth informatics practice curriculum into a medical elective. J Am Med Inform Assoc. 2018;25(4):380-384. [DOI] [PMC free article] [PubMed] [Google Scholar]