Abstract
We used path analysis to investigate complex pathways from HIV status disclosure without consent, physical/verbal violence and depression, social support, and HIV medication self-efficacy through mediators of HIV stigma among women living with HIV in Canada. In the final model, internalized stigma fully mediated the relationship between physical/verbal violence and reduced medication self-efficacy. Enacted stigma fully mediated the relationship between HIV status disclosure without consent and depression. Internalized stigma (β = 0.252; p < 0.001) had a significant negative direct effect on medication self-efficacy. Enacted stigma had a significant direct effect on depression (β = 0.162; p = 0.037). Findings will help improve services and interventions to promote quality of life and well-being of women living with HIV.
Keywords: adherence, HIV, self-efficacy, social support, stigma, women’s health
Introduction
Worldwide, women comprised 51 percent of all adults living with HIV in 2015, with the incidence of HIV among women continuing to increase since the beginning of the HIV epidemic (Consolidated guideline on sexual and reproductive health and rights of women living with HIV, 2017). In Canada, women constitute approximately one-quarter of the total number of people living with HIV (HIV in Canada: Surveillance summary tables, 2014–2015, 2016). In the province of British Columbia in 2016, approximately 1833 women are living with HIV (18% of the total population living with HIV), with 89 percent of women linked to care and 66 percent of women on highly active antiretroviral therapy (HAART; Women and HIV in British Columbia, 2017). Gendered gaps in antiretroviral therapy (ART) adherence and viral load suppression remain in this setting, for women relative to men (Women and HIV in British Columbia, 2017).
With improvements in access to HIV treatment and medications themselves, women living with HIV (WLWH) live increasingly longer and healthier lives (Teeraananchai et al., 2017). Growing attention has focused on understanding how to support WLWH’s positive emotional, psychological and social-cognitive well-being. High prevalence of psychiatric conditions including depression (Morrison et al., 2002), anxiety, and post-traumatic stress disorder (e.g. 5-fold as high rates in the United States (Machtinger et al., 2012), have been reported among WLWH. WLWH experience high levels of trauma across their lifetimes both prior to and following their HIV diagnoses, including physical, sexual and verbal/emotional abuse in both childhood and adulthood (LeGrand et al., 2015), as well as HIV discrimination and stigma (Logie et al., 2018). In Canada, Indigenous women are overrepresented among WLWH, and continue to experience ongoing and multi-generational mental health, quality of life and well-being effects related to the trauma of settler colonialism and residential schools (Benoit et al., 2016). Suicide ideation and attempts, isolation, limited social support, coping challenges, substance use, reduced medication self-efficacy and HIV medication adherence challenges are common for women following an HIV diagnosis (Machtinger et al., 2012).
Some of these markers of emotional, psychological and social-cognitive well-being have been found to have particularly strong direct associations with HIV treatment and care outcomes. Depression and depressive symptoms are associated with HIV medication non-adherence in systematic reviews (Uthman et al., 2014). Medication self-efficacy, defined as the confidence that one has in taking medications as prescribed, is a social-cognitive measure that has been identified as important along the pathway to HIV outcomes including HIV medication adherence (Langebeek et al., 2014). Social support has been associated with adherence to medication regimes in a review and meta-analysis (Langebeek et al., 2014). Thus, in addition to being critical to investigate on their own in relation to women’s well-being, these outcomes can also play important roles in supporting women’s health related to living with HIV more broadly.
Multiple forms of HIV stigma have been identified as barriers to depression, social support, and medication self-efficacy. The effects of HIV stigma remain a global concern for WLWH and are deeply embedded within these relationships. HIV stigma has been associated with higher depression and reduced social support (Rueda et al., 2016), and reduced HIV medication self-efficacy (Sweeney and Vanable, 2016). HIV stigma has also been associated with HIV treatment and care outcomes including reduced adherence to HIV medication (Sweeney and Vanable, 2016), Many mechanisms of HIV stigma have been characterized, and include anticipated stigma—referring to fear or anticipation of mistreatment and rejection following disclosure of one’s HIV positive status; internalized stigma—acceptance of negative feelings and societal beliefs about persons living with HIV (PLWH), and perceived stigma—awareness of negative beliefs and values toward PLWH in one’s society and community (Turan et al., 2017). Enacted stigma refers to acts of mistreatment due to HIV status, and can include discrimination (Turan et al., 2017).
Growing but very limited attention has been drawn to exploring the definitions and specific effects of two types of enacted stigma, including violence (e.g. verbal, physical) related to HIV status, and involuntary disclosure of HIV status/ HIV status disclosure without consent (Barreto, 2017; Duff et al., 2018). However, there is some evidence that these types of HIV stigma could have important impacts on other forms of HIV stigma as well as health and well-being outcomes for PLWH. While voluntary disclosure of HIV status has been shown to be positively correlated with social support (Loutfy et al., 2016), as well as quality of life (Loutfy et al., 2016), and reduced levels of depression or depressive symptoms among WLWH (Vyavaharkar et al., 2011), from a human rights perspective, it is imperative to recognize the potential and realized harms to women from disclosure (Obermeyer et al., 2011), particularly when disclosure is involuntary. These harms can include isolation, abandonment, other stigma, discrimination, and violence (Krüsi et al., 2018; Varga et al., 2006). No quantitative research to our knowledge has been conducted on relationships between HIV status disclosure without consent and important emotional, psychological, and social-cognitive well-being outcomes including depression, social support, or HIV medication self-efficacy; our research aims to fill this research gap.
We are also unaware of any studies that look at the relationship between verbal or physical violence perceived as being related to HIV status on these outcomes. Many studies with women (both living and not living with HIV) have found a relationship between violence and depression; for example, a meta-analysis of studies largely from the United States suggested an increased risk of major depressive disorder (2- to 3-fold), elevated depressive symptoms, and post-partum depression (1.5- to 2-fold increased odds) among women exposed to intimate partner violence relative to those not exposed (Beydoun et al., 2012). Recent trauma has been associated with having a detectable viral load (⩾75 copies/mm) and reduced self-reported antiretroviral use among cis and trans women (Machtinger et al., 2012), and gender-based violence against WLWH has been associated with reduced ART adherence in our study setting (Barreto, 2017). WLWH with a history of physical and sexual violence were significantly more likely to experience negative social and physical consequences following HIV disclosure (Gielen et al., 2000). Research with women suggests that experiences with intimate partner violence have been associated with lower perceived social support (Thompson et al., 2000). Among adolescents, violence has been associated with reduced peer status (Cook et al., 2010), as well as loss of friends/reduced social networks, with this relationship stronger among girls (Wallace and Ménard, 2017).
The factors through which these two rarely examined forms of enacted HIV stigma – HIV disclosure without consent and verbal/physical violence related to HIV status – act on emotional, psychological, and social-cognitive well-being outcomes is not well-understood. Previous research in our study setting has identified direct associations between disclosure of HIV status without consent and anticipated, enacted and perceived HIV stigma and between verbal and physical violence associated with HIV-positive status (“HIV-related violence”) and enacted, internalized, and perceived HIV stigma (Deering et al., 2019). The current study draws on this analysis and the literature to test a conceptual model using path analysis and investigate pathways from HIV disclosure without consent, HIV-related physical and verbal violence, and depression, social support, and HIV medication self-efficacy through mediators of other HIV-related stigma dimensions (other enacted, anticipated, internalized and perceived HIV stigma) among WLWH currently taking ART in Vancouver, Canada.
Methods
Study design and sampling
Data were drawn from 2 years of follow-up (four follow-up surveys) from a longitudinal community-based participatory open cohort of 325+ cis or trans WLWH who lived and/or accessed care in Metro Vancouver, Canada (2014-present; Sexual Health and HIV/AIDS: Women’s Longitudinal Needs Assessment “SHAWNA”). SHAWNA is a partnership of more than 20 women’s HIV and community service providers and is guided by a Community Stakeholder Advisory Board that meets annually and a Positive Women’s Advisory Board of WLWH that meets every 2–3 months. SHAWNA was developed based on over 6 months of community consultations with WLWH, HIV care providers, and policy experts, with the main objective to longitudinally assess the needs and priorities identified by WLWH in Metro Vancouver.
Eligibility for SHAWNA includes being aged 14 or older and living and/or accessing HIV/AIDS services in Metro Vancouver. Various recruitment methods based on community-based research principles were used to recruit participants, including: self-referrals and referrals from HIV care providers, peer researchers, HIV/AIDS service organizations, and clinical outreach, including British Columbia’s primary referral center for WLWH (Oak Tree Clinic, based at BC Women’s Hospital; Kestler et al., 2018). Participants who have provided informed consent completed a semi-annual peer or community interviewer-administered questionnaire at baseline and 6-month follow-ups. The questionnaire covers social-demographics and structural vulnerability (e.g. experiences of violence, food insecurity, sex work, and drug use). Participants then respond to a second questionnaire, administered by a sexual health research nurse, that covers various aspects of sexual and reproductive health access and outcomes, as well as questions related to HIV status.
Participants also receive voluntary viral load/CD4 measurements and serology for sexually transmitted infections/Hepatitis C Virus serology by one of the project’s sexual health nurses. Participants are offered treatment by project nurses onsite, if needed, for symptomatic STI infections and Papanicolaou testing, regardless of enrolment in the study. At each visit, participants receive CA$50 remuneration for their time, travel, and expertise. SHAWNA holds ethical approval through Providence Health/University of British Columbia Research Ethics Board and BC Women’s Hospital.
Primary outcomes and explanatory variables in the path analysis model
All of the following variables were updated every 6 months (time-dependent), with the last 6 months (“recent”) as a reference point.
Our three main outcomes included: (1) depression (defined as a response of “yes” to a survey item asking if participants had been diagnosed with, had been treated for, or had received counseling for depression); (2) social support (defined as responding “a lot,” on a four-point response to the single survey item question “In general, how satisfied are you with the overall support you get from family/friends?”); and (3) and HIV medication self-efficacy (defined as responding “extremely sure” or “very sure,” on a four-point response to the single survey item question “How sure are you that you will be able to take all or most of your medication as directed?”).
Key explanatory variables in the path analysis model included HIV disclosure without consent (“outed” for being HIV-positive), and experiencing verbal or physical violence related to HIV status (being verbally or physically abused by a perpetrator because they knew or suspected the participant was HIV-positive). As in a previous study (Deering et al., 2019), HIV stigma was measured using nine questions from Wright’s shortened 10-item version (Wright et al., 2007) of Berger’s HIV-stigma scale (Berger et al., 2001). All stigma measures were considered continuous in path analysis. Table 1 presents the survey items that comprise each sub-scale.
Table 1.
Characteristics of participants at baseline in our study of women living with HIV in Metro Vancouver, Canada (SHAWNA; N = 208).
| Characteristic | Prevalence (N) or median, interquartile range | Missing |
|---|---|---|
| Age (years) | 47 (40–53) | 0 |
| Duration since diagnosed with HIV (years) | 15 (9–21) | 11 |
| Identify as sexual minority | 38.9% (81) | 0 |
| Identify as trans/gender minority | 10.6% (22) | 0 |
| Ethnicity—Indigenous | 57.2% (119) | 0 |
| Ethnicity—Other minority | 8.7% (18) | |
| Ethnicity—White | 34.1% (71) | |
| Immigrant to Canada | 6.3% (13) | 0 |
| High school graduation | 46.2% (96) | 0 |
| Homeless/living on the streeta | 10.1% (21) | 0 |
| Sex worka | 23.6% (49) | 0 |
| Injection drug usea | 44.2% (92) | 2 |
| Non-injection drug usea | 47.1% (98) | 1 |
| HIV disclosure without consenta | 13.5% (28) | 8 |
| Verbal/physical HIV violencea | 9.6% (20) | 1 |
| Anticipated HIV stigmaa,b | ||
| Careful who I tell I have HIV | 64.4% (134) | 3 |
| Worry that people will tell others I have HIV | 43.3% (90) | 6 |
| Enacted HIV stigmaa,b | ||
| Hurt by people’s reactions to learning I have HIV | 24.5% (51) | 7 |
| Stopped socializing with people from reactions to learning I have HIV | 27.4% (57) | 8 |
| Lost friends by telling them I have HIV | 23.6% (49) | 11 |
| Internalized HIV stigmaa,b | ||
| Feel I am not as good a person because I have HIV | 16.8% (35) | 3 |
| Feel unclean because I have HIV | 22.1% (46) | 2 |
| Feel I am a bad person because I have HIV | 9.6% (20) | 2 |
| Perceived stigmaa,b | ||
| Feel most people with HIV are rejected | 36.1% (75) | 12 |
| Depressiona | 19.2% (40) | 0 |
| Satisfied with social support | 56.3% (117) | 2 |
| HIV medication self-efficacy | 87.5% (182) | 2 |
SHAWNA: Sexual Health and HIV/AIDS: Women’s Longitudinal Needs Assessment.
In the last 6 months.
Each HIV stigma measure separately (for each measure, “yes” included responses of “strongly agree” or “agree” vs “no,” which included responses of “neither agree nor disagree,” “disagree” or “strongly disagree”).
Confounders in the multivariable path analysis model
Potential confounders for the final path analysis model included variables chosen based on a priori knowledge gathered from previous research and through ongoing discussions with peer researchers and members of our Community Stakeholder Advisory Board and Positive Women’s Advisory Board of WLWH. Socio-demographic variables included the following: age (continuously in years); duration since first diagnosed with HIV (continuously in years); identifying as a member of the sexual minority community (i.e. identifying as any of “gay,” “lesbian,” “bisexual,” “two-spirit,” “asexual,” “queer,” “other,” vs “straight”); identifying as a member of the gender minority community (identifying as any of “transgender,” “intersex,” “transexual,” “two-spirit,” “genderqueer,” “other,” vs “cisgender”); ethnicity (defined as Indigenous (First Nations, Métis, or Inuit), other visible/ethnic minority (African/Caribbean/Black/other minority), vs White); im/migrant to Canada (vs born in Canada); and education (graduated high school vs did not). With the exception of age, duration since HIV diagnosis, identifying as sexual minority and identifying as gender minority, all of the social-demographic variables listed were considered time-independent variables. The remaining variables were considered time-dependent and updated every 6 months. In addition to those just described, additional time-dependent variables examined as potential confounders included, in the last 6 months, being homeless, being in jail overnight or longer, sex work, injection drug use, and non-injection drug use.
Statistical analysis
Descriptive statistics were calculated for the overall sample of WLWH on ART and included frequencies and proportions for categorical variables, and measures of central tendencies (i.e. mean, medians, and interquartile ranges (IQRs)) for continuous data.
We used path analysis to investigate pathways from HIV disclosure without consent and HIV-related violence to depression, social support and HIV medication self-efficacy through mediators of other HIV-related stigma dimensions (other enacted from the HIV Stigma Scale, anticipated, internalized, and perceived HIV stigma). Path analysis is a form of multiple regression statistical analysis that is used to evaluate causal models by examining the relationships between one or several outcomes and two or more explanatory variables (Muthen et al., 1997). Path analysis was conducted using a weighted least-squares approach, with mean and variance adjustment to evaluate the hypothesized model (Muthen et al., 1997). We tested direct relationships between HIV disclosure without consent and physical/verbal violence associated with participant’s HIV-positive status, and three outcomes: depression, social support, and medication self-efficacy. We tested indirect relationships via four HIV-related stigma dimensions (other enacted from the HIV Stigma Scale, anticipated, internalized, and perceived HIV stigma). In the final models, we adjusted for the variables that were identified as confounders, described above. Standardized coefficients, standard errors, critical ratios, and p-values are presented for each direct relationship investigated. In path analysis, standardized coefficient estimates are presented to remove scaling and allow for the comparison of all parameters within the model. Standardized coefficients represent the strength and direction of direct and indirect effects. Path analysis model fit was assessed using chi-square, root mean square error of approximation (RMSEA), and comparative fit index (CFI). A score of <0.05 for RMSEA and a score >0.90 for CFI indicate an acceptable model fit (Mueller and Hancock, 2008).
Statistical significance was set at p < 0.05 level, and observations with missing responses on exogenous variables were excluded from the path analysis. All p-values are two-sided. Statistical Analysis System (SAS) software version 9.4 (SAS Institute Inc., Cary, NC, USA) and Mplus version 8 (Muthén & Muthén, Los Angeles, CA, USA) were used for all statistical analyses.
Results
Characteristics of participants
Overall, our study included 208 participants on ART who responded to ⩾1 follow-up survey during the 2 years of follow-up (max: four follow-up surveys). Table 1 presents characteristics of participants at their baseline survey. The median age of participants was 47 years (IQR: 40–53 years), with a median of 15 years (IQR: 9–21) since first diagnosed with HIV (Table 1). Indigenous women were over-represented in the sample (57.2%) relative to the BC population (5% in 2011), with 34.1 percent of participants reporting being White and 8.7 percent reporting another ethnicity. Overall, 38.9 percent of the sample reported identifying as sexual minority and 10.6 percent reported identifying as gender minority. In total, 6.3 percent reported having immigrated/migrated to Canada and 46.2 percent reported high school graduation. In the last 6 months, 10.1 percent reported being homeless, 23.6 percent reported sex work, and 44.2 percent and 47.1 percent reported injection and non-injection drug use, respectively (Table 1).
In the last 6 months, 13.5 percent of participants had their HIV status disclosed without their consent, and 9.6 percent reported physical or verbal violence related to their HIV status. With respect to outcomes, 19.2 percent of participants reported being diagnosed with, treated for, or received counseling for depression in the last 6 months, 56.3 percent reported being satisfied with their social support and 87.5 percent reported having HIV medication self-efficacy, as measured by feeling able to take ART as prescribed.
Path analysis
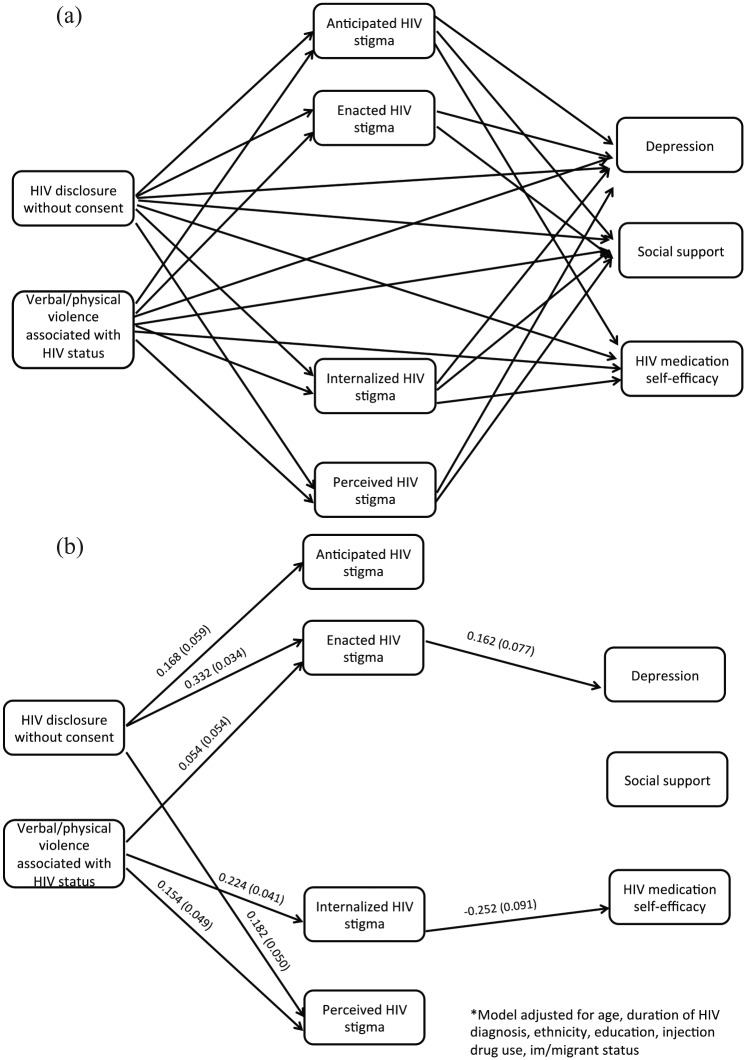
Path analysis was conducted to examine the direct and indirect effects of disclosure of HIV status without consent, physical, or verbal violence perceived as associated with HIV status and depression, social support, and HIV medication self-efficacy. After missing data were excluded, 194 participants with 464 observations over 2 years of follow-up were included in the final model. Final model fit indices suggest the model fit well to the data (χ2 = 2.856; p = 0.240; CFI = 0.997; RMSEA = 0.030). Figure 1(a) illustrates all of the tested path models. Figure 1(b) presents the path diagram with standardized coefficients as well as the pathways for relationships that were significant on a p < 0.05 level, and standard errors in parentheses.
Figure 1.
(a) Initial path diagram with hypothesized pathways. (b) Final path diagram including only pathways for relationships that were significant on a p < 0.05 level, with standardized coefficients and standard errors (parentheses).
Table 2 presents the results of the final model. In the final model, the direct paths from HIV disclosure without consent and physical/verbal violence associated with participant’s HIV-positive status to the three outcomes (depression, social support, and HIV medication self-efficacy) were not significant. In the final model, internalized stigma (β =−0.252, p < 0.001) had a significant negative direct effect on HIV medication self-efficacy. The direct path from enacted stigma to depression was positive and significant (β = 0.162; p = 0.037; Figure 1(b); Table 2). Internalized stigma fully mediated the relationship between physical/verbal violence associated with participant’s HIV status and medication self-efficacy. Enacted stigma fully mediated the relationship between HIV disclosure without consent and depression.
Table 2.
Final path analysis model parameter estimates of depression, social support and medication self-efficacy among women living with HIV in Metro Vancouver, Canada (N = 194).a,b.
| Parameter | Standardized coefficient | Standard error | Critical ratio | p |
|---|---|---|---|---|
| Depression | ||||
| Disclosure without consent | 0.093 | 0.208 | 0.449 | 0.653 |
| Violence related to HIV status | 0.297 | 0.193 | 1.535 | 0.125 |
| Anticipated HIV stigma | 0.078 | 0.078 | 1.001 | 0.317 |
| Enacted HIV stigma | 0.162 | 0.077 | 2.090 | 0.037 |
| Internalized HIV stigma | 0.086 | 0.085 | 1.016 | 0.310 |
| Perceived HIV stigma | −0.039 | 0.085 | −0.456 | 0.649 |
| Satisfied with social support | ||||
| Disclosure without consent | −0.296 | 0.188 | −1.579 | 0.114 |
| Violence related to HIV status | −0.046 | 0.209 | −0.218 | 0.828 |
| Anticipated HIV stigma | −0.120 | 0.067 | −1.776 | 0.076 |
| Enacted HIV stigma | −0.139 | 0.077 | −1.811 | 0.070 |
| Internalized HIV stigma | −0.115 | 0.062 | −1.868 | 0.062 |
| Perceived HIV stigma | 0.056 | 0.071 | 0.786 | 0.432 |
| Medication self-efficacy | ||||
| Disclosure without consent | −0.353 | 0.209 | −1.687 | 0.092 |
| Violence related to HIV status | 0.047 | 0.225 | 0.210 | 0.833 |
| Anticipated HIV stigma | −0.133 | 0.090 | −1.477 | 0.140 |
| Enacted HIV stigma | 0.142 | 0.094 | 1.506 | 0.132 |
| Internalized HIV stigma | −0.252 | 0.069 | −3.630 | <0.001 |
| Perceived HIV stigma | −0.012 | 0.091 | −0.133 | 0.894 |
| Anticipated HIV stigma | ||||
| Disclosure without consent | 0.472 | 0.165 | 2.854 | 0.004 |
| Violence related to HIV status | 0.169 | 0.169 | 0.997 | 0.319 |
| Enacted HIV stigma | ||||
| Disclosure without consent | 0.932 | 0.091 | 10.217 | <0.001 |
| Violence related to HIV status | 0.697 | 0.125 | 5.564 | <0.001 |
| Internalized HIV stigma | ||||
| Disclosure without consent | 0.117 | 0.144 | 0.810 | 0.418 |
| Violence related to HIV status | 0.540 | 0.155 | 3.485 | <0.001 |
| Perceived HIV stigma | ||||
| Disclosure without consent | 0.512 | 0.140 | 3.660 | <0.001 |
| Violence related to HIV status | 0.481 | 0.151 | 3.192 | 0.001 |
All results were adjusted by age, education, ethnicity, immigrant/migrant status, duration since first diagnosed with HIV and injection drug use.
Each HIV stigma measure separately (for each measure, “yes” included responses of “strongly agree” or “agree” vs “no,” which included responses of “neither agree nor disagree,” “disagree” or “strongly disagree”).
HIV disclosure without consent had a significant direct effect on anticipated stigma (β = 0.472; p = 0.004), enacted stigma (β = 0.932; p < 0.001), and perceived stigma (β = 0.512; p < 0.001), while physical/verbal violence associated with HIV status had a significant direct effect on enacted stigma (β = 0.697; p < 0.001), internalized stigma (β = 0.540; p < 0.001), and perceived stigma (β = 0.481; p = 0.001).
Discussion
Study findings suggested that two dimensions of HIV-related stigma play important mediating roles along the pathways to HIV medication self-efficacy and depression, and two important outcomes for PLWH that have emerged from the field of psychological health. Internalized HIV stigma mediated the relationship between physical/verbal violence associated with participant’s HIV status and reduced medication self-efficacy, while enacted HIV stigma mediated the relationship between HIV disclosure without consent and heightened depression. These results offer key insights into the psychological health and well-being of WLWH.
Our finding that internalized HIV stigma was a mediator in the relationship between HIV-related physical/verbal violence and reduced HIV medication self-efficacy provides insight into results from growing research indicating that trauma and violence is associated with reduced ART use, adherence to medication and viral load (Hatcher et al., 2015; Mugavero et al., 2006), including in our setting (Barreto, 2017). Relative to other psychological social-cognitive adherence variables, including attitudes and norms surrounding medication use, HIV medication self-efficacy has been identified as a critical determinant of adherence to medication (Langebeek et al., 2014). Medication self-efficacy describes an individual’s belief that they possess the ability to take medication (Schwarzer, 1992). In our study, as in many others, the strength of self-efficacy, or an individual’s confidence in the estimate of efficacy, is measured (Schwarzer, 1992). In our study setting, violence was associated with increased internalized stigma, that in turn was associated with reduced medication self-efficacy. These results are in line with previous research suggesting that internalized HIV stigma is associated with reduced ART initiation (Logie et al., 2018) and treatment adherence (Livingston and Boyd, 2010), and that medication self-efficacy is a mediator between internalized stigma and medication adherence (Seghatol-Eslami et al., 2017). Internalized stigma occurs when people apply their perceptions of negative social or public attitudes by others regarding a characteristic they imbue to their own perceptions of themselves (Earnshaw et al., 2013). Through its established influence on factors such as reduced self-esteem, hope, empowerment, and social connectedness/support (Livingston and Boyd, 2010), for example, internalized HIV stigma could have a negative impact on women’s confidence or ability to take HIV medication regularly. As with all stigma mechanisms, internalized stigma needs to be contextualized within larger social and structural inequalities experienced. Further qualitative research on how internalized HIV stigma and medication self-efficacy can be addressed could help inform tailored interventions to address internalized HIV stigma alongside structural interventions.
Physical violence and verbal abuse related to HIV status is a particularly harmful example of enacted HIV stigma and more research is needed to better understand how to intervene. In the shorter term, results suggest that individual and broader community interventions to reduce HIV stigma should recognize the risk of abuse and violence among WLWH. As with other groups who experience high rates of trauma (A Treatment Improvement Protocol: Trauma-Informed Care in Behavioral Health Services, 2014), approaches guided by trauma-informed care principles that recognize the prevalence of violence against WLWH and intersections with HIV stigma and impact on health outcomes, including those related to HIV medication use and adherence, are critical. Limited previous studies suggest various coping strategies can be used to help reduce internalized HIV stigma (Rael et al., 2017; Rao et al., 2012b). Coping strategies can include safe HIV disclosure (e.g. developing feelings of control over disclosure of HIV status), education/dispelling myths about HIV for participants and others, working toward viewing HIV as a manageable chronic condition, and facilitating support from family and friends and peer support (Rael et al., 2017; Rao et al., 2012b). Studies have used various approaches to support women in developing coping skills, including role-plays, modeling of behaviors through video, discussions on triggering events, social support, and contact with peers (Rael et al., 2017; Rao et al., 2012b). Cognitive-behavioral therapeutic interventions have had positive results for improving the psychological health of WLWH through these pathways, for example, an intervention based on an understanding of themes related to women’s experiences with HIV and stigma (feelings of powerlessness, feelings of guilt and anger about the past, behavioral patterns and responses, experiences of reactions of others, and uncertainty about the future) was found to be associated with reduced internalized HIV stigma and coping, as well as depression (Tshabalala and Visser, 2011). Additional social-structural strategies could include ensuring that women have opportunities to be connected to support groups for WLWH, supportive HIV/AIDS service organizations and facilitating opportunities for women to be advocates for others with HIV.
Our results suggest that other enacted HIV stigma was a mediator in the relationship between HIV status disclosure without consent and depression, a key measure of psychological well-being. Since enacted HIV stigma (including discrimination) reflects discriminatory societal views of HIV that are translated into actions (Earnshaw et al., 2013), interventions tailored for and with WLWH to address mental health and counter enacted HIV stigma could use approaches that aim to mobilize social change and address HIV stigma on a community level (Prinsloo et al., 2017). On an intrapersonal level, support in building resilient coping skills could help women develop strategies to reduce the personal and emotional impact caused by the negative stigmatizing actions of others (Logie et al., 2013). Higher resilience has also been associated with reduced depression symptoms among WLWH, alongside other factors that could act along the pathway from internalized HIV stigma to depression (e.g. self-efficacy, self-esteem; Dale et al., 2019). Among many different populations in a systematic review, psychological resilience interventions based on a combination of cognitive-behavioral therapy and mindfulness techniques had a positive impact on individual resilience; more interventions should be tailored by and with WLWH (Joyce et al., 2018). Results also highlight the importance of eliminating situations where women may have their HIV status disclosed involuntarily and without their consent as an approach to addressing women’s mental health. It is critical that medical information of WLWH remain confidential, including in healthcare settings, where health professionals have a duty of confidentiality toward clients/patients. Protection of privacy is a fundamental human right and WLWH ought to be able to rely on their health information remaining private, especially when accessing health services and because disclosure of medical information relating to HIV can have uniquely negative consequences for individuals living with HIV relative to other health conditions. Continuing to work toward ensuring women’s privacy can help reduce opportunities for non-consensual disclosure of HIV status. Furthermore, given the potential benefits of safe HIV disclosure on women’s health and well-being, future research should investigate how interventions to support safe disclosure can be designed and evaluated to minimize the impact of disclosure on enacted HIV stigma (Kennedy et al., 2015). Research into how Canada’s punitive HIV disclosure laws promote HIV disclosure without consent, stigma and violence and the benefits of repealing such laws, should be continued and supported (Krüsi et al., 2018).
This study had several limitations as well as strengths. Our study’s smaller sample size may not provide power to detect some associations. However, because we are able to make use of multiple measurements over time in our longitudinal study approach, effective sample size is increased. Our study may not be representative of all WLWH in Metro Vancouver nor be generalizable to other settings. However, recruitment of study participants for SHAWNA is achieved by broad coverage of diverse AIDS Service Organizations and clinical settings by our peer research associates and clinical outreach, and we feel that our sample reflects the diversity of WLWH. Our study includes self-report data, which can be subject to social desirability bias, as well as recall bias (Althubaiti, 2016). However, we are confident in the training and experience of our peer, community, and clinical research interviewers in safe and supportive interview approaches to minimize these biases. We have investigated several key pathways out of many potential pathways to explore. While we considered depression, social support, and medication self-efficacy as separate outcomes, evidence suggests that these variables may be related in some study populations. For example, social support may be a mediator between HIV stigma and depression (Rao et al., 2012a); in supplementary analysis, we did not find social support to be a mediator between HIV stigma and depression, with the model with this pathway having worse fit than the model presented here. We are limited in our ability to detect causation, with reverse causation possible for some relationships (e.g. HIV stigma and depression).
HIV stigma dimensions emerged as important mediators in relationships between HIV disclosure without consent, violence and the wellbeing of WLWH, including depression and medication self-efficacy. Findings provide important insights for WLWH and implications for policy and practice, and can help improve the services and interventions, as well as promote the psychological quality of life and well-being for WLWH.
Acknowledgments
We thank all those who contributed their time and expertise to this project, particularly participants, community partners, the SHAWNA Positive Women’s Advisory Board and Community Advisory Board, and the SHAWNA Project team: Sarah Moreheart, Brittany Udall, Jennifer Morris, Flo Ranville, Heidi Safford, Lauren Martin, Ray Croy, Bridgette Simpson, Anita Dhanoa, Monique Desroches, Lydia Hamel, Lulu Gurney, and Patience Chamboko. We also acknowledge Abby Rolston, Sylvia Machat, Peter Vann, Erin Seatter, and Patricia McDonald for their research and administrative support.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the Canadian Institutes of Health Research.
References
- A Treatment Improvement Protocol: Trauma-Informed Care in Behavioral Health Services (2014) Available at: https://store.samhsa.gov/shin/content//SMA14-4816/SMA14-4816.pdf [PubMed]
- Althubaiti A. (2016) Information bias in health research: Definition, pitfalls, and adjustment methods. Journal of Multidisciplinary Healthcare 9: 211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barreto DFL. (2017) The impact of structural inequities and interpersonal violence on food security and HIV care among women living with and affected by HIV in a Canadian setting. MSc Thesis, The University of British Columbia, Vancouver, BC, Canada. [Google Scholar]
- Benoit AC, Cotnam J, Raboud J, et al. (2016) Experiences of chronic stress and mental health concerns among urban Indigenous women. Archives of Women’s Mental Health 19(5): 809–823. [DOI] [PubMed] [Google Scholar]
- Berger BE, Ferrans CE, Lashley FR. (2001) Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health 24(6): 518–529. [DOI] [PubMed] [Google Scholar]
- Beydoun HA, Beydoun MA, Kaufman JS, et al. (2012) Intimate partner violence against adult women and its association with major depressive disorder, depressive symptoms and postpartum depression: A systematic review and meta-analysis. Social Science & Medicine 75(6): 959–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consolidated guideline on sexual and reproductive health and rights of women living with HIV (License: CC BY-NC-SA 3.0 IGO) (2017). Geneva: World Health Organization. [PubMed] [Google Scholar]
- Cook CR, Williams KR, Guerra NG, et al. (2010) Predictors of bullying and victimization in childhood and adolescence: A meta-analytic investigation. School Psychology Quarterly 25(2): 65–83. [Google Scholar]
- Dale SK, Reid R, Safren SA. (2019) Factors associated with resilience among Black women living with HIV and histories of trauma. Journal of Health Psychology. Epub ahead of print 8 April. DOI: 10.1177/1359105319840690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deering KN, Logie C, Krusi A, et al. (2019) Prevalence and correlates of HIV stigma among women living with HIV in Metro Vancouver. AIDS and Behavior, Revisions in progress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duff P, Kestler M, Chamboko P, et al. (2018) Realizing women living with HIV’s reproductive rights in the era of ART: The negative impact of non-consensual HIV disclosure on pregnancy decisions amongst women living with HIV in a Canadian Setting. AIDS and Behavior 22(9): 2906–2915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Smith LR, Chaudoir SR, et al. (2013) HIV stigma mechanisms and well-being among PLWH: A test of the HIV stigma framework. AIDS and Behavior 17(5): 1785–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gielen AC, Fogarty L, O’Campo P, et al. (2000) Women living with HIV: Disclosure, violence, and social support. Journal of Urban Health 77(3): 480–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher AM, Smout EM, Turan JM, et al. (2015) Intimate partner violence and engagement in HIV care and treatment among women: A systematic review and meta-analysis. AIDS 29(16): 2183–2194. [DOI] [PubMed] [Google Scholar]
- HIV in Canada: Surveillance summary tables, 2014-2015 (2016). Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/hiv-in-canada-surveillance-summary-tables-2014-2015.html?_ga=2.36148512.1854480409.1511201895-982402930.1509048385
- Joyce S, Shand F, Tighe J, et al. (2018) Road to resilience: A systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 8: e017858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy CE, Haberlen S, Amin A, et al. (2015) Safer disclosure of HIV serostatus for women living with HIV who experience or fear violence: A systematic review. Journal of the International AIDS Society 18(6S5): 20292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kestler M, Murray M, Money D, et al. (2018) The Oak Tree Clinic: The envisioned model of care for women living with human immunodeficiency virus in Canada. Women’s Health Issues 28(2): 197–198. [DOI] [PubMed] [Google Scholar]
- Krüsi A, Ranville F, Gurney L, et al. (2018) Positive sexuality: HIV disclosure, gender, violence and the law—A qualitative study. PLoS ONE 13(8): e0202776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langebeek N, Gisolf EH, Reiss P, et al. (2014) Predictors and correlates of adherence to combination antiretroviral therapy (ART) for chronic HIV infection: A meta-analysis. BMC Medicine 12(1): 142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeGrand S, Reif S, Sullivan K, et al. (2015) A review of recent literature on trauma among individuals living with HIV. Current HIV/AIDS Reports 12(4): 397–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston JD, Boyd JE. (2010) Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Social Science & Medicine 71(12): 2150–2161. [DOI] [PubMed] [Google Scholar]
- Logie C, James L, Tharao W, et al. (2013) Associations between HIV-related stigma, racial discrimination, gender discrimination, and depression among HIV-positive African, Caribbean, and Black Women in Ontario, Canada. AIDS Patient Care and STDs 27(2): 114–122. [DOI] [PubMed] [Google Scholar]
- Logie CH, Lacombe-Duncan A, Wang Y, et al. (2018) Pathways from HIV-related stigma to antiretroviral therapy measures in the HIV care cascade for women living with HIV in Canada. JAIDS Journal of Acquired Immune Deficiency Syndromes 77(2): 144–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loutfy M, Johnson M, Walmsley S, et al. (2016) The association between HIV disclosure status and perceived barriers to care faced by women living with HIV in Latin America, China, Central/Eastern Europe, and Western Europe/Canada. AIDS Patient Care and STDs 30(9): 435–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machtinger EL, Haberer JE, Wilson TC, et al. (2012) Recent trauma is associated with antiretroviral failure and HIV transmission risk behavior among HIV-positive women and female-identified transgenders. AIDS and Behavior 16(8): 2160–2170. [DOI] [PubMed] [Google Scholar]
- Machtinger EL, Wilson TC, Haberer JE, et al. (2012) Psychological trauma and PTSD in HIV-positive women: A meta-analysis. AIDS and Behavior 16(8): 2091–2100. doi: 10.1007/s10461-011-0127-4. [DOI] [PubMed] [Google Scholar]
- Morrison MF, Petitto JM, Ten Have T, et al. (2002) Depressive and anxiety disorders in women with HIV infection. American Journal of Psychiatry 159(5): 789–796. doi: 10.1176/appi.ajp.159.5.789. [DOI] [PubMed] [Google Scholar]
- Mueller RO, Hancock GR. (2008) Best Practices in Structural Equation Modeling. Thousand Oaks, CA: SAGE. [Google Scholar]
- Mugavero M, Ostermann J, Whetten K, et al. (2006) Barriers to antiretroviral adherence: The importance of depression, abuse, and other traumatic events. AIDS Patient Care and STDs 20(6): 418–428. [DOI] [PubMed] [Google Scholar]
- Muthen BO, du Toit SHC, Spisic D. (1997) Robust inference using weighted least squares and quadratic estimating equations in latent variable modeling with categorical and continuous outcomes. Working paper. University of California, Los Angeles.
- Obermeyer CMD, Baijal PMA, Pegurri EM. (2011) Facilitating HIV disclosure: Facilitating HIV disclosure across diverse settings: A review. American Journal of Public Health 101(6): 1011–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prinsloo CD, Greeff M, Kruger A, et al. (2017) HIV stigma experiences and stigmatisation before and after a HIV stigma-reduction community “hub” intervention. African Journal of AIDS Research 16(3): 203–213. [DOI] [PubMed] [Google Scholar]
- Rael CT, Carballo-Diéguez A, Norton R, et al. (2017) Identifying strategies to cope with HIV-related stigma in a group of women living with HIV/AIDS in the Dominican Republic: A qualitative study. AIDS and Behavior 21(9): 2589–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao D, Chen WT, Pearson CR, et al. (2012. a) Social support mediates the relationship between HIV stigma and depression/quality of life among people living with HIV in Beijing, China. International Journal of STD & AIDS 23(7): 481–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao D, Desmond M, Andrasik M, et al. (2012. b) Feasibility, acceptability, and preliminary efficacy of the unity workshop: An internalized stigma reduction intervention for African American women living with HIV. AIDS Patient Care and STDs 26(10): 614–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rueda S, Mitra S, Chen S, et al. (2016) Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: A series of meta-analyses. BMJ Open 6(7): e011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzer R. (1992) Self-Efficacy in the Adoption and Maintenance of Health Behaviours: Theoretical Approaches and a New Model. New York: Taylor & Francis. [Google Scholar]
- Seghatol-Eslami VC, Dark HE, Raper JL, et al. (2017) Brief report: Interpersonal and intrapersonal factors as parallel independent mediators in the association between internalized HIV stigma and ART adherence. JAIDS Journal of Acquired Immune Deficiency Syndromes 74(1): e18–e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeney SM, Vanable PA. (2016) The association of HIV-related stigma to HIV medication adherence: A systematic review and synthesis of the literature. AIDS and Behavior 20(1): 29–50. [DOI] [PubMed] [Google Scholar]
- Teeraananchai S, Kerr S, Amin J, et al. (2017) Life expectancy of HIV-positive people after starting combination antiretroviral therapy: A meta-analysis. HIV Medicine 18(4): 256–266. [DOI] [PubMed] [Google Scholar]
- Thompson MP, Kaslow NJ, Kingree JB, et al. (2000) Partner violence, social support, and distress among inner-city African American women. American Journal of Community Psychology 28(1): 127–143. [DOI] [PubMed] [Google Scholar]
- Tshabalala J, Visser M. (2011) Developing a cognitive behavioural therapy model to assist women to deal with HIV and stigma. South African Journal of Psychology 41(1): 17–28. doi: 10.1177/008124631104100103. [DOI] [Google Scholar]
- Turan B, Hatcher AM, Weiser SD, et al. (2017) Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. American Journal of Public Health 107(6): 863–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uthman OA, Magidson JF, Safren SA, et al. (2014) Depression and adherence to antiretroviral therapy in low-, middle- and high-income countries: A systematic review and meta-analysis. Current HIV/AIDS Reports 11(3): 291–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varga CA, Sherman GG, Jones SA. (2006) HIV-disclosure in the context of vertical transmission: HIV-positive mothers in Johannesburg, South Africa. AIDS Care 18(8): 952–960. [DOI] [PubMed] [Google Scholar]
- Vyavaharkar M, Moneyham L, Corwin S, et al. (2011) HIV-disclosure, social support, and depression among HIV-infected African American women living in the rural southeastern united states. AIDS Education and Prevention 23(1): 78–90. [DOI] [PubMed] [Google Scholar]
- Wallace LN, Ménard KS. (2017) Friendships lost: The social consequences of violent victimization. Journal of Aggression, Maltreatment & Trauma 26(2): 116–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Women and HIV in British Columbia (2017). Available at: http://www.cfenet.ubc.ca/sites/default/files/uploads/HIV-pulse/hiv-pulse-issue-4.pdf
- Wright K, Naar-King S, Lam P, et al. (2007) Stigma scale revised: Reliability and validity of a brief measure of stigma for HIV+ youth. Journal of Adolescent Health 40(1): 96–98. [DOI] [PMC free article] [PubMed] [Google Scholar]