Abstract
Background
Appendicitis is the most common general surgical emergency worldwide, but its diagnosis remains challenging. The aim of this study was to determine whether existing risk prediction models can reliably identify patients presenting to hospital in the UK with acute right iliac fossa (RIF) pain who are at low risk of appendicitis.
Methods
A systematic search was completed to identify all existing appendicitis risk prediction models. Models were validated using UK data from an international prospective cohort study that captured consecutive patients aged 16–45 years presenting to hospital with acute RIF in March to June 2017. The main outcome was best achievable model specificity (proportion of patients who did not have appendicitis correctly classified as low risk) whilst maintaining a failure rate below 5 per cent (proportion of patients identified as low risk who actually had appendicitis).
Results
Some 5345 patients across 154 UK hospitals were identified, of which two‐thirds (3613 of 5345, 67·6 per cent) were women. Women were more than twice as likely to undergo surgery with removal of a histologically normal appendix (272 of 964, 28·2 per cent) than men (120 of 993, 12·1 per cent) (relative risk 2·33, 95 per cent c.i. 1·92 to 2·84; P < 0·001). Of 15 validated risk prediction models, the Adult Appendicitis Score performed best (cut‐off score 8 or less, specificity 63·1 per cent, failure rate 3·7 per cent). The Appendicitis Inflammatory Response Score performed best for men (cut‐off score 2 or less, specificity 24·7 per cent, failure rate 2·4 per cent).
Conclusion
Women in the UK had a disproportionate risk of admission without surgical intervention and had high rates of normal appendicectomy. Risk prediction models to support shared decision‐making by identifying adults in the UK at low risk of appendicitis were identified.
Women in the UK had a disproportionate risk of admission without surgical intervention and had high rates of normal appendicectomy. Risk prediction models to support shared decision‐making were identified by identifying UK adults at low risk of appendicitis. An online calculator is available (http://appy-risk.org). WCC, white cell count; CRP, C‐reactive protein; AIRS, Appendicitis Inflammatory Response Score; AAS, Adult Appendicitis Score.
Important differences between men and women
Antecedentes
La apendicitis es la urgencia quirúrgica de cirugía general más frecuente en todo el mundo, pero su diagnóstico sigue siendo un desafío. El objetivo de este estudio fue determinar si los modelos de predicción de riesgo existentes pueden identificar de manera fiable a los pacientes del Reino Unido que se presentan en el hospital con dolor agudo en la fosa ilíaca derecha (right iliac fossa, RIF) con bajo riesgo de apendicitis.
Métodos
Se realizó una búsqueda sistemática para identificar todos los modelos existentes de predicción de riesgo de apendicitis. Los modelos se validaron utilizando los datos del Reino Unido de un estudio International prospectivo de cohortes que incluía pacientes consecutivos de 16 a 45 años que se presentaron en el hospital con dolor agudo en RIF entre marzo y junio de 2017. El criterio de valoración principal fue la mejor especificidad que era posible alcanzar con el modelo (proporción de pacientes que no tenían apendicitis correctamente clasificados como de bajo riesgo) manteniendo una tasa de fracaso < 5% (proporción de pacientes identificados como de bajo riesgo que realmente tuvieron apendicitis).
Resultados
Se identificaron 5.345 pacientes en 154 hospitales del Reino Unido, de los cuales dos tercios (67,6%, 3.613/5.345) eran mujeres. Las mujeres tenían más del doble de probabilidades de someterse a una apendicectomía con un apéndice histológicamente normal (28,2%; 272/964) en comparación con los varones (12,1%; 120/993, riesgo relativo 2,33 (i.c. del 95% 1,92‐2,84), P < 0,001)). Entre los 15 modelos de predicción de riesgo validados, el sistema de puntuación de apendicitis en adultos (Adult Appendicitis Score) fue el que obtuvo la mejor predicción (punto de corte ≤ 8, especificidad 63%, tasa de fracaso 3,7%). El sistema de puntuación de la respuesta inflamatoria de apendicitis (Appendicitis Inflammatory Response Score) fue el que obtuvo la mejor predicción en los varones (punto de corte ≤ 2, especificidad 25%, tasa de fracaso 2,4%).
Conclusión
Las mujeres del Reino Unido tuvieron un riesgo desproporcionado de ingreso sin intervención quirúrgica, así como porcentajes elevados de apendicectomías blancas. Se encontraron modelos de predicción de riesgos para apoyar la toma de decisiones compartida mediante la identificación de adultos del Reino Unido con bajo riesgo de apendicitis.
Introduction
Acute appendicitis is the most common general surgical emergency worldwide1, but its diagnosis remains challenging, particularly in young women for whom there is a broader range of differential diagnoses than for men2. A key concern is overtreatment, in the form of normal appendicectomy (removal of a histologically normal appendix), which may be associated with increased postoperative complications, duration of hospital stay and healthcare costs compared with diagnostic laparoscopy alone3, 4, 5. There is little consensus on optimal diagnostic pathways for patients presenting with acute right iliac fossa (RIF) pain in the UK. Traditionally, concerns over the radiation exposure associated with CT have limited its routine use6. Although modern low‐dose protocols have reduced radiation exposure whilst maintaining diagnostic performance7, 8, CT rates are lower in the UK than in many other high‐income countries, and this is associated with higher normal appendicectomy rates (NARs)9.
To improve diagnosis of appendicitis, international guidelines10, 11 recommend routine clinical risk scoring. Although the Appendicitis Inflammatory Response (AIRS) and Alvarado scores are recommended most frequently, there is little evidence to support their application, as they have been inconsistently and poorly validated12. None is in routine clinical use13. Consequently, although guidelines recommend that patients at low risk of appendicitis should not be admitted routinely to hospital13, diagnostic uncertainty may lead to patients being admitted for observation, increasing the likelihood of overtreatment and healthcare‐related costs. Robustly validated risk prediction models that identify groups at low risk of appendicitis could help to standardize clinical assessment and inform patient and doctor decision‐making. In turn, this may reduce hospital admissions, overtreatment and healthcare costs14.
To influence wide‐scale change, a prospective multicentre study including patients presenting with RIF pain was developed to assess whether existing risk prediction models can identify low‐risk patients suitable for ambulatory management. This study represents the first planned analysis from the Right Iliac Fossa Treatment (RIFT) Study Group15. The aim of this study was to identify the optimal risk prediction model to identify young patients (aged 16–45 years) in the UK at low risk of acute appendicitis. Children and adults aged over 45 years follow distinct management pathways and will be addressed in subsequent preplanned analyses.
Methods
This study was undertaken in two parts. First, a systematic literature search was performed to identify all available risk prediction models for acute appendicitis. This is reported according to the PRISMA guidelines16. Second, a multicentre prospective observational cohort study was performed to collect accurate data for validation of these risk prediction models. This is reported according to Standards for Reporting Diagnostic Accuracy (STARD) guidelines17 for diagnostic accuracy studies.
The RIFT Study15 captured data in the UK, Italy, Portugal, Republic of Ireland and Spain. Clinical risk score validation was preplanned to be performed in the UK for patients presenting with acute RIF pain. National differences in clinical pathways mean that analyses must be stratified by country. At the time of planning the analysis, the NAR was anticipated to be around 20 per cent in the UK18, but under 5 per cent in other European countries14, 19. Given the low baseline NAR, there is little clinical need for risk scoring in European populations, so validation of risk scores in those patients would be unlikely to change clinical practice. Therefore, clinical risk score validation was preplanned to be performed in the UK only, although observed NARs from across all participating countries are presented for context. Future analyses are planned to explore variation in imaging rates across Europe.
Identifying risk scoring models
Systematic searches of MEDLINE and Web of Science were performed using the search terms [‘appendicitis’ OR ‘appendectomy’ OR ‘appendicectomy’] AND [‘score’ OR ‘model’ OR ‘scoring’ OR ‘nomogram’]. These results were supplemented by additional unstructured searches of Google Scholar. Reference lists from relevant articles were hand‐searched for eligible studies, as were recent World Society of Emergency Surgery and Royal College of Surgeons (England) Emergency Surgery guidelines10, 13. No date restrictions were set. The search was last updated on 25 July 2018.
Studies were eligible for inclusion if they described a risk prediction model for the diagnosis of acute appendicitis that used clinical data and/or routine laboratory tests (full blood count, C‐reactive protein, liver function tests). As the aim of the study was to identify model(s) that could be used at initial surgical assessment, models were excluded if they relied on radiological investigations or non‐routine laboratory tests that are not typically available at the point of first surgical contact. Models that aimed to differentiate simple from complex appendicitis were also excluded. Only English‐language articles that provided sufficient information to replicate their clinical risk model algorithm were included. Titles and abstracts were screened, followed by review of full texts of relevant articles. Study selection and data extraction were completed independently by two authors, with any disagreements resolved through discussion with a third author.
Study dissemination
Data collection was conducted according to a prespecified, published protocol15. The protocol was disseminated through surgical trainee‐led research collaboratives. Any hospital providing acute general surgical services was eligible to participate.
Study approval
As this observational study collected routine, anonymized data with no change to clinical care pathways, lead investigators at participating UK centres registered the study locally as either clinical audit or service evaluation. In the Republic of Ireland, Italy, Portugal and Spain, local lead investigators were responsible for arranging research ethics committee or institutional approval locally, as appropriate.
Patient selection
Eligible patients were identified from participating centres during one of four prespecified 2‐week study periods between 13 March 2017 and 18 June 2017. During each interval, all consecutive patients referred by a general practitioner or emergency physician to the on‐call surgeon's team with suspected appendicitis or acute RIF pain were identified at the point of admission to the surgical unit. Patients who had previously undergone either a therapeutic appendicectomy or an incidental appendicectomy as part of another procedure were excluded. Pregnant women have significantly different clinical needs to other patients and were therefore excluded. Pregnancy was identified by patients' self‐report. The possibility of pregnancy was further excluded by most women undergoing urinalysis. Patients who underwent appendicectomy for whom histological findings were not available were excluded, as it was not possible to determine the underlying diagnosis (appendicitis versus normal appendicectomy) for them. Patients who were managed without surgery for acute appendicitis following a positive CT or MRI diagnosis of appendicitis were also excluded, as the diagnosis was not confirmed histologically.
Diagnosis of appendicitis
A diagnosis of acute appendicitis was confirmed if within 30 days of enrolment in the study the patient had excision of the appendix with postoperative histological examination confirming acute appendicitis. Patients who underwent right hemicolectomy for presumed acute appendicitis were pooled with those who had appendicectomy. Based on the original histopathology report, patients were classified as having either simple or complex (gangrenous, perforated) appendicitis2. The NAR was calculated as patients with normal appendix histology as a proportion of all patients who had an appendicectomy. Patients with appendix pathology other than appendicitis (such as appendix tumour) were included in the denominator but not the numerator.
Data collection
Data were collected using standardized case report forms (CRFs) by teams of up to three investigators per 2‐week period. The CRF was designed to be completed at the patient bedside. A large number of variables have been proposed to predict appendicitis. Therefore, to ensure feasibility of data collection, the CRF was designed to collect the data points required for the four most common adult risk prediction models identified in international guidelines10. Patient‐level variables collected included age, sex, clinical symptoms and examination findings, urinalysis and blood test results. Data were collected on ultrasound, CT or MRI use, and whether these tests were positive for appendicitis (diagnosis of appendicitis in the formal radiology report). If the patient had surgery, the procedure, operative findings and histopathology results were recorded. Patients were followed during their initial admission, during any subsequent hospital admissions within 30 days of initial presentation, and then at 30 days after initial presentation using a combination of electronic and paper hospital records.
Data integrity
Multiple strategies were used to ensure accurate data collection. A supervising consultant surgeon at each hospital oversaw study conduct and was responsible for overall quality assurance of submitted data. To ensure data completeness, before locking of the online database, local lead investigators were contacted with specific details of missing data. Participating sites voluntarily identified independent data validators who had not been involved in the initial data collection. Data accuracy was determined by review of the following key data fields against the original clinical records for enrolled patients: whether the patient had undergone surgery; whether the patient had been readmitted within 30 days of index admission; and histopathological results, if applicable. The data accuracy rate was defined as the proportion of validated data fields that was recorded correctly. Where incorrect data were identified, validators were asked to amend those data points on the study database.
Validation of risk prediction models and statistics
The development of the statistical analysis plan is summarized in Appendix S2 (supporting information).
Risk prediction models were validated if patients could be scored with the data points available. As there are distinct differential diagnoses for RIF pain in women, it was preplanned to stratify risk prediction model validation by sex.
For maximum clinical impact, the ideal risk score would classify as many patients as possible as being at low risk of appendicitis (true negatives), but not at the expense of missing significant numbers of patients with appendicitis (false negatives). The clinical performance of each score was therefore evaluated in terms of failure rate and specificity. The failure rate is the false‐negative rate: the proportion of patients stratified to the low‐risk group who actually have appendicitis (false negatives/(true negatives + false negatives)). Before analysis, a modified Delphi exercise (Appendix S2 , supporting information) amongst 24 experienced UK general surgeons agreed the maximum acceptable failure rate to be 5 per cent. Specificity is the proportion of patients who do not have appendicitis who were stratified to the low‐risk group (true negatives/(true negatives + false positives)).
The main outcome measure for evaluating each risk prediction model was the best achievable specificity whilst maintaining a failure rate of less than 5 per cent. The overall ability of the risk prediction models to discriminate between patients with and without acute appendicitis was determined by calculation of the area under the receiver operating characteristic (ROC) curve (AUC).
Analyses were carried out in Stata® version 15 (StataCorp, College Station, Texas, USA).
Handling of missing data
As surgical collaborative cohort studies have been completed with very low rates of missing data, an overall incomplete data rate of under 2·5 per cent was anticipated. Therefore, there was no plan to impute missing data. A complete case analysis (list‐wise deletion) was performed, and preplanned sensitivity analyses: missing data points scored as zero, representing what would happen in normal clinical practice and providing a scenario that would underestimate appendicitis risk; missing data were scored with maximum applicable points.
Results
The systematic search identified 26 risk prediction models (Fig. 1). Fifteen of these could be validated with the data collected in the cohort study20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34 (Table 1). These risk prediction models were based on 17 clinical parameters (Table S1 , supporting information). The other 11 models could not be validated owing to the data set lacking specific variables35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45 (Table S2 , supporting information).
Figure 1.
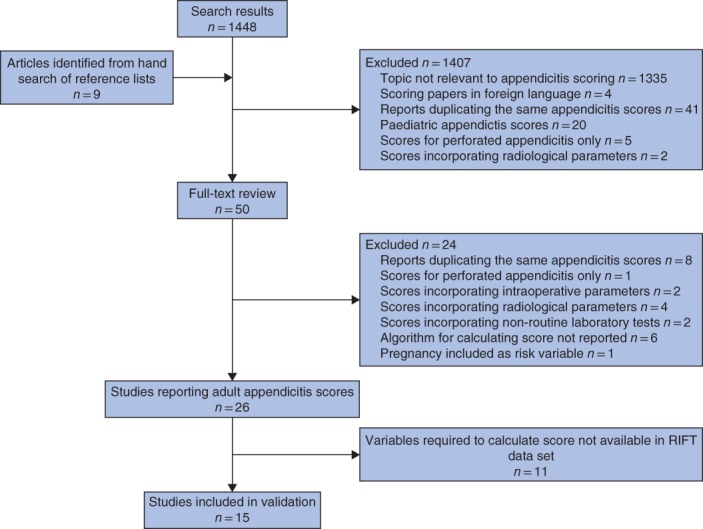
Flow diagram of study inclusion in the systematic review
Table 1.
Characteristics of risk prediction models identified in systematic review
| Model | Year | Country | Derivation cohort | Patients included in derivation cohort |
|---|---|---|---|---|
| Van Way et al.34 | 1982 | USA | Retrospective single‐centre | 476 patients who underwent appendicectomy; included children and adults, and both sexes* |
| Alvarado20 | 1986 | USA | Retrospective single‐centre |
305 patients presenting with abdominal pain; age range 4–80 years, 42% of patients were women |
| Izbicki et al.28 | 1992 | Germany | Retrospective single‐centre | 536 patients who underwent appendicectomy; included both sexes* |
| Eskelinen et al.25 | 1992 | Finland | Prospective multicentre | 1333 patients presenting with abdominal pain; mean age 38 years, 52 per cent of patients were women |
| Christian and Christian24 | 1992 | India | Prospective single‐centre | 58 patients presenting with abdominal pain; age range 10–56 years, 22% of patients were women |
| Modified Alvarado29 | 1994 | UK | n.a.† | n.a.† |
| Eskelinen et al.26 | 1994 | Finland | Prospective multicentre | 636 patients presenting with abdominal pain; included men only* |
| van der Broek et al.33 | 2002 | Holland | Prospective single‐centre | 577 patients presenting with abdominal pain; all patients aged above 10 years, 59% of patients were women |
| Birkhahn et al.22 | 2006 | USA | Prospective single‐centre | 439 patients presenting with abdominal pain; age range 3–93 years, 65% of patients were women |
| AIRS21 | 2008 | Sweden | Prospective multicentre |
316 patients presenting with abdominal pain; mean age 26 years, 54% of patients were women |
| RIPASA score23 | 2010 | Brunei | Retrospective single‐centre | 312 patients who underwent appendicectomy; mean age 26 years, 42% of patients were women |
| Ting et al.32 | 2010 | Taiwan | Retrospective single‐centre | 532 patients who underwent appendicectomy; 39% of patients were women* |
| AAS31 | 2014 | Finland | Prospective single‐centre | 725 patients presenting with abdominal pain; age range 16–97 years, 58% of patients were women |
| Goh27 | 2017 | China | n.a.† | n.a.† |
| Mikaere et al.30 | 2018 | New Zealand | Retrospective single‐centre | 885 patients presenting with abdominal pain; all patients aged over 15 years, 59% of patients were women |
Overall age and/or sex information not reported.
Not applicable (n.a.) as modification of a previously published score (no derivation cohort). AIRS, Appendicitis Inflammatory Response Score; RIPASA, Raja Isteri Pengiran Anak Saleha Appendicitis; AAS, Adult Appendicitis Score.
Normal appendicectomy rate benchmarking across participating countries
The overall NAR in patients aged 16–45 years was 20·0 per cent (392 of 1957) in the UK and 6.2 per cent (54 of 868) in the other countries. In women aged 16–45 years, the NAR was 28·2 per cent (272 of 964) in the UK, 5·0 per cent (6 of 121) in Italy, 6 per cent (3 of 51) in Portugal, 25 per cent (15 of 59) in the Republic of Ireland and 10·1 per cent (18 of 179) in Spain. In men in the same age group, the NAR was 12·1 per cent (120 of 993) in the UK, 0·6 per cent (1 of 157) in Italy, 6 per cent (2 of 32) in Portugal, 3·4 per cent (7 of 208) in the Republic of Ireland and 3·3 per cent (2 of 61) in Spain. As anticipated, the NAR was higher in the UK than in other countries, so risk score validation proceeded in UK patients. All of the following data are for UK patients only.
Data integrity
A total of 5345 patients were included in the study (Fig. 2), from across 154 UK hospitals. Of the 17 clinical parameters required to validate the risk prediction models, 0·9 per cent (794 of 90 865) were missing. Some 35·3 per cent (4461 of 12 647) of eligible data fields were assessed by independent data validators, finding overall data accuracy to be 98·3 per cent (4384 of 4461).
Figure 2.
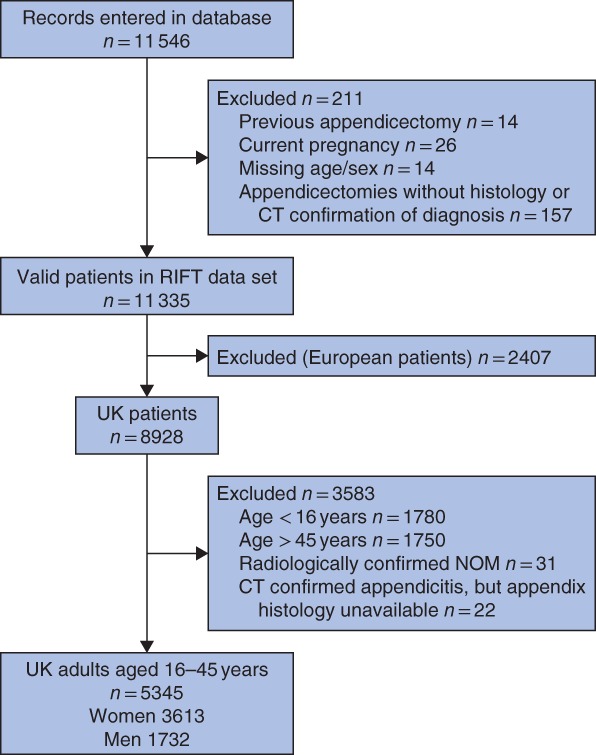
Flow diagram of patient inclusion in the cohort study
NOM, non‐operative management of appendicitis.
Patient characteristics and outcomes
Two‐thirds (3613 of 5345, 67·6 per cent) of patients were women (Table 2). Women were less likely to undergo any surgery than men (32·0 versus 59·8 per cent respectively; relative risk 0·53, 95 per cent c.i. 0·50 to 0·57, P < 0·001). Amongst women undergoing appendicectomy, 97·6 per cent (941 of 964) had a laparoscopic procedure, of which 2·2 per cent (21 of 941) were converted to an open operation. Amongst men undergoing appendicectomy, 93·9 per cent (932 of 993) had a laparoscopic procedure, of which 6·0 per cent (56 of 932) were converted to an open procedure.
Table 2.
Patient management stratified by sex
| Women (n = 3613) | Men (n = 1732) | |
|---|---|---|
| No. who had surgery | 1156 (32·0) | 1036 (59·8) |
| No. of appendicectomies performed | 964 of 1156 (83·4) | 993 of 1036 (95·8) |
| Confirmed appendicitis | 625 (64·8) | 841 (84·7) |
| Other appendix pathology | 67 (7·0) | 32 (3·2) |
| Histologically normal appendix | 272 (28·2) | 120 (12·1) |
| No. not operated on | 2457 (68·0) | 696 (40·2) |
Values in parentheses are percentages.
The NAR was higher in women than in men (28·2 versus 12·1 per cent respectively; relative risk 2·33, 95 per cent c.i. 1·92 to 2·84, P < 0·001). Within the 30‐day follow‐up, 27·4 per cent (1466 of 5345) of all patients presenting with acute RIF pain had undergone appendicectomy and been confirmed to have appendicitis on histological examination. Of all patients presenting with RIF pain, women were less likely to have a confirmed diagnosis of appendicitis than men (17·3 versus 48·6 per cent respectively; relative risk 0·36, 0·33 to 0·39, P < 0·001).
Clinical use of risk prediction models
Only 0·6 per cent of patients (32 of 5345) were recorded as having been formally risk‐scored on admission by their clinical team. When performed, the Alvarado score was used most frequently (29 of 32, 91 per cent).
Validation of risk prediction models
Of the 15 risk prediction models, 11 showed consistently good discrimination for identifying appendicitis (AUC above 0·7) across both women and men (Fig. 3 and Table 3). In women, the Adult Appendicitis Score31 (AAS) achieved the highest specificity whilst maintaining a failure rate of less than 5 per cent in low‐risk patients (Table 3). At a cut‐off score of 8 or less, the AAS triaged 63·1 per cent of women who did not have appendicitis to the low‐risk group (specificity), and amongst all women in the low‐risk group 3·7 per cent in fact had appendicitis (failure rate). In men, the optimal model was the Appendicitis Inflammatory Response Score21 (AIRS), with a cut‐off score of 2 or less associated with a specificity of 24·7 per cent and a failure rate of 2·4 per cent.
Figure 3.
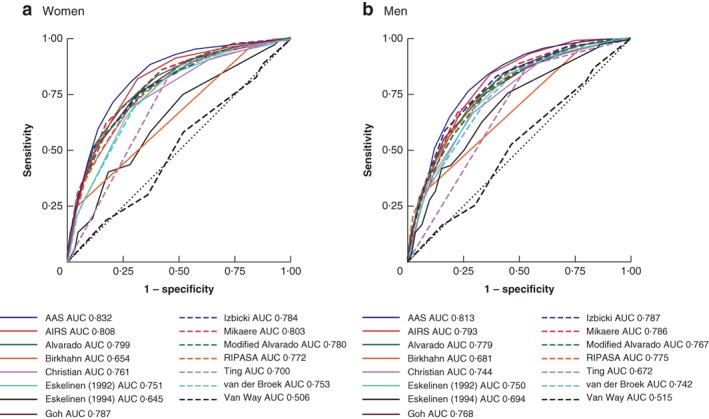
Receiver operating characteristic (ROC) curves for 15 appendicitis risk prediction models in women and men
a Women; b men. These receiver operating characteristic (ROC) curves are based on a complete‐case analysis for all 15 risk prediction models. As a result they may be based on fewer patients than when each model was validated individually (Table 3). This accounts for any minor discrepancies between the data presented here and those in Table 3. AAS, Adult Appendicitis Score; AUC, area under the ROC curve; AIRS, Appendicitis Inflammatory Response Score; RIPASA, Raja Isteri Pengiran Anak Saleha Appendicitis.
Table 3.
Validation and identification of optimal thresholds for risk prediction models, stratified by sex
| Model | AUC | Optimal threshold | Failure rate (%) | Specificity (%) |
|---|---|---|---|---|
| AAS 31 | ||||
| Women | 0·83 (0·82, 0·85) | ≤ 8 | 3·7 | 63·1 |
| Men | 0·81 (0·79, 0·83) | ≤ 6 | 5·0 | 20·4 |
| AIRS 21 | ||||
| Women | 0·81 (0·79, 0·83) | ≤ 3 | 3·5 | 51·6 |
| Men | 0·79 (0·77, 0·82) | ≤ 2 | 2·4 | 24·7 |
| Alvarado 20 | ||||
| Women | 0·80 (0·78, 0·82) | ≤ 3 | 3·7 | 40·8 |
| Men | 0·78 (0·76, 0·80) | ≤ 1 | 0 | 6·2 |
| Birkhahn et al. 22 | ||||
| Women | 0·66 (0·64, 0·67) | 1 | 3·8 | 18·1 |
| Men | 0·68 (0·66, 0·70) | 1 | 10·1 | 21·6 |
| Christian and Christian 24 | ||||
| Women | 0·76 (0·74, 0·78) | 0 | 0·9 | 3·9 |
| Men | 0·75 (0·72, 0·77) | 0 | 2·1 | 5·5 |
| Eskelinen et al. 25 | ||||
| Women | 0·76 (0·74, 0·78) | ≤ 45·3 | 4·4 | 9·6 |
| Men | 0·75 (0·73, 0·78) | ≤ 39·4 | 1·4 | 8·4 |
| Eskelinen et al. 26 | ||||
| Women | 0·65 (0·62, 0·67) | ≤ − 5·8 | 3·6 | 6·4 |
| Men | 0·70 (0·67, 0·72) | ≤ − 7·7 | 10·5 | 2·0 |
| Goh 27 | ||||
| Women | 0·79 (0·77, 0·81) | ≤ 2 | 4·1 | 46·3 |
| Men | 0·77 (0·75, 0·79) | 0 | 5·3 | 8·4 |
| Izbicki et al. 28 | ||||
| Women | 0·79 (0·77, 0·80) | ≤ 1 | 3·3 | 21·2 |
| Men | 0·79 (0·77, 0·81) | ≤ 1 | 6·1 | 3·6 |
| Mikaere et al. 30 | ||||
| Women | 0·80 (0·78, 0·82) | ≤ 1 | 4·9 | 57·9 |
| Men | 0·79 (0·76, 0·81) | ≤ 1 | 4·3 | 21·7 |
| Modified Alvarado 29 | ||||
| Women | 0·78 (0·76, 0·80) | ≤ 3 | 4·5 | 43·6 |
| Men | 0·77 (0·75, 0·79) | ≤ 2 | 11·8 | 25·4 |
| RIPASA score 23 | ||||
| Women | 0·77 (0·75, 0·79) | ≤ 5·5 | 4·7 | 44·2 |
| Men | 0·78 (0·76, 0·80) | ≤ 4 | 0 | 3·8 |
| Ting et al. 32 | ||||
| Women | 0·70 (0·68, 0·72) | 0 | 19·8 | 46·9 |
| Men | 0·67 (0·65, 0·69) | 0 | 4·8 | 52·5 |
| van der Broek et al. 33 | ||||
| Women | 0·76 (0·74, 0·77) | 0 | 3·3 | 24·6 |
| Men | 0·75 (0·72, 0·77) | ≤ 2 | 14·3 | 23·1 |
| Van Way et al. 34 | ||||
| Women | 0·51 (0·48, 0·53) | 32 | 15·5 | 12·9 |
| Men | 0·52 (0·49, 0·54) | 32 | 42·9 | 16·4 |
Values in parentheses are 95 per cent confidence intervals. AUC, area under the curve; AAS, Adult Appendicitis Score; AIRS, Appendicitis Inflammatory Response Score; RIPASA, Raja Isteri Pengiran Anak Saleha Appendicitis.
Sensitivity analyses
Overall, 0·9 per cent (294 of 32 517) of the variables required to calculate AAS were missing in women. The main complete‐case analysis was based on the 95·0 per cent (3433 of 3613) of women for whom all variables were available. In sensitivity analysis, the failure rate was found to range from 3·6 to 3·8 per cent, if missing variables were scored with either the maximum or minimum possible point value respectively. Specificity was found to range from 61·3 to 64·2 per cent respectively.
In total, 1·0 per cent (156 of 15 588) of the variables required to calculate AIRS were missing in men. The complete‐case analysis was based on the 93·9 per cent (1627 of 1732) of men for whom all variables were available. In sensitivity analysis, the failure rate ranged between 2·4 and 2·9 per cent, and specificity from 23·3 to 26·4 per cent.
Patients stratified to low‐risk groups
Of the 1856 women identified as low risk by the AAS in the complete‐case analysis, 1560 (84·1 per cent) did not undergo surgery (Table 4). Of women who either did not undergo surgery or had a procedure other than appendicectomy, at 30 days the final diagnoses were non‐specific abdominal pain (851 of 1627, 52·3 per cent), benign gynaecological pathology (430 of 1627, 26·4 per cent), urinary tract infection (99 of 1627, 6·1 per cent) and miscellaneous other (247 of 1627, 15·2 per cent). A full breakdown of diagnoses is provided in Table S3 (supporting information).
Table 4.
Management and readmissions in patients scored as low risk, stratified by sex
| Women with AAS ≤ 8 (n = 1856) | Men with AIRS ≤ 2 (n = 209) | |
|---|---|---|
| Patient management | ||
| No. who had surgery | 296 (15·9) | 35 (16·7) |
| No. of appendicectomies performed | 229 of 296 (77·4) | 34 of 35 (97) |
| Simple appendicitis | 60 (26·2) | 5 (15) |
| Complex appendicitis | 9 (3·9) | 0 (0) |
| Other appendix pathology | 28 (12·2) | 4 (12) |
| Histologically normal appendix | 132 (57·6) | 25 (74) |
| No. not operated on | 1569 (84·1) | 174 (83·3) |
| Readmission | ||
| Ongoing RIF pain in patients not operated on in index admission | 130 of 1586 (8·2) | 13 of 178 (7·3) |
| Postoperative complications following appendicectomy on index admission | 14 of 207 (6·8) | 7 of 31 (23) |
Values in parentheses are percentages. AAS, Adult Appendicitis Score; AIRS, Appendicitis Inflammatory Response Score; RIF, right iliac fossa.
Amongst the 12·3 per cent (229 of 1856) of women who underwent appendicectomy, 57·6 per cent (132 of 229) had a normal appendicectomy, 26·2 per cent (60 of 229) had simple appendicitis, 3·9 per cent (9 of 229) had complex appendicitis and 12·2 per cent (28 of 229) had other abnormal appendix pathology. Amongst the 28 women with other pathology, four were found to have carcinoid and one to have Crohn's disease. The readmission rate for ongoing RIF pain amongst low‐risk women who were not operated on in their index admission was 8·2 per cent (130 of 1586). Of the women who had undergone appendicectomy on index admission, 6·8 per cent (14 of 207) were readmitted with postoperative complications.
In the complete‐case analysis, AIRS identified 209 men as being at low risk (Table 4). Of these, only 34 (16·3 per cent) had an appendicectomy and one man (0·5 per cent) underwent non‐appendix surgery. At 30 days, the final diagnosis for most men who did not undergo appendicectomy was non‐specific pain (110 of 175, 62·9 per cent) (Table S4 , supporting information). Of men who had an appendicectomy, five were found to have appendicitis on histological examination, with no complex appendicitis identified. The NAR in low‐risk men was 74 per cent (25 of 34). The readmission rate for ongoing RIF pain in low‐risk men who were not operated on in their index admission was 7·3 per cent (13 of 178), and the readmission rate for postoperative complications among those who had an appendicectomy was 23 per cent (7 of 31).
Imaging
Most women (2638 of 3613, 73·0 per cent) had either ultrasound or CT preoperative imaging. The imaging modality used most frequently was ultrasonography (2289 of 3613, 63·4 per cent). Low overall sensitivity (0·36) indicated that triage based solely on ultrasound imaging would misclassify most patients with appendicitis as being low risk. The failure rate for ultrasonography was 8·4 per cent. Stratifying women by AAS score, the AUC for ultrasound imaging was modest in both the low‐risk (AUC 0·63) and high‐risk (AUC 0·68) groups (Table 5). Although CT was performed in only 15·1 per cent (547 of 3613) of women overall, this imaging modality was sensitive (0·92), with a low failure rate (2·1 per cent). Stratifying by AAS score, the AUC for CT was excellent in both the low‐risk (AUC 0·99) and high‐risk (AUC 0·93) groups.
Table 5.
Use of imaging and performance, stratified by sex and risk category
| Women | Men | |||
|---|---|---|---|---|
| Low risk (AAS ≤ 8) (n = 1856) | High risk (AAS > 8) (n = 1577) | Low risk (AIRS ≤ 2) (n = 209) | High risk (AIRS > 2) (n = 1418) | |
| Ultrasound imaging | 1291 (69·6) | 916 (58·1) | 59 (28·2) | 205 (14·5) |
| AUC* | 0·63 (0·57, 0·70) | 0·68 (0·65, 0·71) | 1·00 (n.a.) | 0·66 (0·60, 0·72) |
| Sensitivity | 0·28 | 0·38 | 1·00 | 0·37 |
| Specificity | 0·99 | 0·98 | 1·00 | 0·95 |
| NPV | 0·97 | 0·82 | 1·00 | 0·74 |
| PPV | 0·54 | 0·84 | 1·00 | 0·79 |
| CT | 208 (11·2) | 316 (20·0) | 41 (19·6) | 341 (24·0) |
| AUC* | 0·99 (0·98, 1·00) | 0·93 (0·90, 0·96) | 1·00 (n.a.) | 0·92 (0·90, 0·95) |
| Sensitivity | 1·00 | 0·92 | 1·00 | 0·94 |
| Specificity | 0·97 | 0·95 | 1·00 | 0·91 |
| NPV | 1·00 | 0·96 | 1·00 | 0·94 |
| PPV | 0·62 | 0·91 | 1·00 | 0·90 |
| No imaging | 434 (23·4) | 456 (28·9) | 111 (53·1) | 910 (64·2) |
Values in parentheses are percentages unless indicate otherwise;
values in parentheses are 95 per cent confidence intervals. AAS, Adult Appendicitis Score; AIRS, Appendicitis Inflammatory Response Score; AUC, area under the receiver operating characteristic (ROC) curve; n.a., not applicable; NPV, negative predictive value; PPV, positive predictive value.
Overall, only 36·2 per cent (627 of 1732) of men underwent preoperative imaging. Ultrasound imaging (276 of 1732, 15·9 per cent) was performed less frequently than CT (398 of 1732, 23·0 per cent). The overall sensitivity of ultrasonography (0·38) was low, with a high failure rate (18·8 per cent). In men stratified as high risk by AIRS, ultrasound imaging had a poor AUC (0·66). In contrast, the overall sensitivity of CT (0·94) was high, with a failure rate of 4·5 per cent. In high‐risk men, CT had an excellent AUC (0·92). Analysis of the performance of ultrasound and CT imaging in low‐risk men was limited by low numbers (Table 5).
AAS and AIRS performance across participating countries
Overall, 17·3 per cent (625 of 3613) of women and 48·6 per cent (841 of 1732) of men in the UK presenting with appendicitis had a histological diagnosis of appendicitis, compared with 42·5 per cent (361 of 849) of women and 68·5 per cent (442 of 645) of men in Ireland, Italy, Portugal and Spain.
To test the potential for international application of risk‐scoring, performance of the AAS and AIRS was tested in the Irish, Italian, Portuguese and Spanish data. In women, the AAS (cut‐off score 8 or below) had a specificity of 57·5 per cent (226 of 393), with a failure rate of 17·5 per cent (48 of 274). In men, the AIRS (cut‐off score 2 or less) had a specificity of 15·6 per cent (25 of 160), with a failure rate of 32 per cent (12 of 37).
Discussion
This study found that women in the UK who presented with acute RIF pain had a disproportionately high rate of admission without surgical intervention. Women who did undergo surgery had high rates of normal appendicectomy. Using the AAS31 (cut‐off score 8 or less) it was possible to stratify almost two‐thirds of UK women aged 16–45 years who presented with RIF pain into a low‐risk group. This low‐risk group had an overall one in 27 risk of appendicitis and one in 200 risk of complex appendicitis. Similarly, the AIRS21 (cut‐off score 2 or less) identified a smaller group of UK men who were at low risk of appendicitis. The performance of ultrasound imaging for diagnosis of appendicitis was poor in both men and women, whereas CT was both sensitive and specific across all subgroups.
The overall NAR in UK adults aged 16–45 years was 20·0 per cent, significantly higher than the rate recorded in other countries that participated in the RIFT Study. This represents one of the world's highest NARs9, 18, 19. Although simple and complex appendicitis may represent distinct pathologies46, some surgeons believe that delaying surgery may increase the risk of appendiceal perforation. This leads to some surgeons having a low threshold for surgery, preferring for patients with equivocal presentations to undergo early appendicectomy rather than a period of clinical observation. This may result in potentially unnecessary operations (removal of histologically normal appendices) with associated postoperative morbidity3, 4, 5. However, leaving a macroscopically normal looking appendix in situ may risk missing microscopic inflammation47 and is associated with an increased readmission rate48. These conflicting considerations have resulted in variations in practice, with some surgeons routinely leaving a macroscopically normal appendix in situ 49. Improved preoperative diagnosis could potentially reduce both overtreatment and heterogeneity in practice.
A large number of risk prediction models for acute appendicitis have been published. Few have been validated robustly, with most validation studies relying on small single‐centre retrospective data sets12. In the present study of 5345 patients across 154 UK hospitals, most models were unable safely to identify significant numbers of patients at low risk of appendicitis. Given the clinical importance of identifying low‐risk patients, this study was preplanned to focus on validating models' prediction of patients who do not have appendicitis (true negatives) rather than prediction of acute appendicitis (true positives), whereas most previous studies have prioritized identification of high‐risk patients. In addition to differences in baseline case mix, this explains why the optimal cut‐off scores identified in this study differ from those proposed in the original AAS (original study proposed cut‐off score of 11 or less versus 8 or below identified in the present study) and AIRS (original study proposed cut‐off score of 5 or less versus 2 or less identified in this study) studies21, 31. Identification of the optimal cut‐off scores for use in the UK population will increase the likelihood of risk prediction models being disseminated widely and implemented safely in the UK National Health Service. Routine risk scoring has been found in prospective studies to be associated with reduced need for imaging and hospital admission, and to reduce the NAR14, 50.
Ultrasound imaging is used frequently in women as it allows effective visualization of gynaecological organs. However, in this national UK cohort it was found to perform poorly in the identification of appendicitis in both women and men. Although CT was performed highly selectively, consistent with previous studies7, 8 it demonstrated excellent discrimination for appendicitis. Routine CT may decrease NARs, but exposes patients to radiation51. In the past it has been estimated that there may be one excess cancer for every 12 normal appendicectomies avoided by routine CT6, but these concerns are less prominent in the era of low‐dose CT protocols. Nonetheless, low‐risk patients, particularly women of childbearing age, may choose to avoid ionizing radiation, if there is a low index of suspicion of appendicitis. This study excluded older, postmenopausal women, who are more likely to benefit from routine CT to exclude colonic pathology such as malignancy and diverticulitis10.
This is the largest prospective multicentre cohort study worldwide of RIF pain in the era of laparoscopic surgery. A total of 154 hospitals contributed data, representing around two‐thirds of UK hospitals that provide general surgery52. The study's findings are therefore broadly generalizable across the UK. The CRF was designed to be completed at the patient's bedside during their initial assessment. This minimized measurement and recall bias, leading to high data completeness (99·1 per cent) and accuracy (98·3 per cent) rates, ensuring high internal validity.
Previous trainee‐led prospective cohort studies achieved high levels of case ascertainment53, but it is possible that a small number of eligible patients were missed during the study inclusion windows. Follow‐up was limited to the index hospital where patients initially presented, so some patients discharged without having undergone appendicectomy may have been readmitted and operated on at another hospital, although this is likely to be infrequent. There is weak epidemiological evidence indicating that there may be seasonal variation in the incidence of appendicitis54. Year‐long data collection would maximize the study's generalizability, but high‐quality data collection within a multicentre collaborative study would not be sustainable for protracted periods.
An additional 15 data items (Table S2 , supporting information) were required to validate all existing risk prediction models, but collecting these items for each patient would have placed an impractical burden on participating centres. As a consequence, 11 existing models could not be validated. None of these is in clinical use, but there is a hypothetical possibility that one or more may have outperformed AAS and AIRS if tested.
Risk stratification can be performed by the first clinician in contact with the patient, who has blood test results available. However, as this study captured patients at the point of assessment by surgical teams, its findings do not directly support the implementation of risk scoring by general practitioners and emergency physicians. As the incidence of appendicitis in patients presenting to general practice or the emergency department with abdominal pain is lower than that in patients reviewed by surgical teams, it is likely that risk prediction models would perform better in these settings, but further evaluation is required.
The UK has one of the world's highest NARs14, 18, 19, so the predefined aim for this study was to evaluate the potential for routine risk scoring to identify low‐risk UK patients who are unlikely to have appendicitis. It was predicted that the NAR would be lower in the other participating countries and there would be no need for appendicitis risk scoring. As anticipated, the overall NAR in Italy, Portugal, Republic of Ireland and Spain was lower than that in the UK (10·2 versus 28·2 per cent respectively in women, and 2·6 versus 12·1 per cent in men). An unexpected finding, however, was that in those countries a greater proportion of all patients who were admitted with RIF pain had a final diagnosis of appendicitis than in the UK (42·5 versus 17·3 per cent respectively in women, and 68·5 versus 48·6 per cent in men). The differences in the prevalence of appendicitis between the UK and other settings may explain why the failure rates (reciprocal of negative predictive value) were unacceptably high in the Irish, Italian, Portuguese and Spanish patients. Therefore, this study's results should be extrapolated cautiously to settings outside the UK. It is possible that in other countries with high baseline NAR, such as Australia55, and lower appendicitis prevalence amongst patients admitted with RIF pain there may be a role for clinical risk scoring, but local validation studies are needed.
Risk prediction models, stratified by sex, may act as adjuncts to high‐quality serial clinical assessment of patients, rationalizing exposure to ionizing radiation to those patients most likely to benefit from CT. AAS and AIRS can be implemented easily, as they require only simple clinical information and routine blood tests, which were already performed for most patients in the present observational cohort.
The authors propose that all adults presenting with acute RIF pain or suspected appendicitis should be scored routinely using the appropriate risk prediction model. To support calculation and application of appropriate cut‐off scores at the patient's bedside, a mobile‐, tablet‐ and desktop‐compatible web application has been developed (http://appy-risk.org).
To mitigate against the high risk of normal appendicectomy in low‐risk patients, if a patient is stratified as low risk and suspicion of appendicitis remains, low radiation dose CT should be undertaken to confirm the diagnosis before a decision to operate. Ultrasound imaging is preferable in women if the principal differential diagnosis is gynaecological pathology. A very small proportion of low‐risk women and men (Tables S3 and S4 , supporting information) presenting with RIF pain have serious conditions such as colitis. Therefore, patients with unclear diagnosis or markers of significant illness (such as fever or significantly raised C‐reactive protein level) should be admitted for observation and potentially for inpatient radiological investigation. Patients who are clinically well with a low index of suspicion of pathology requiring inpatient treatment may choose to be managed at home with the safety net of prompt ambulatory reassessment. Ambulatory management reduces rates of inpatient admission and CT56, and may in turn reduce unnecessary surgery and NARs. A clinical algorithm proposed by the authors is shown in Fig. 4.
Figure 4.
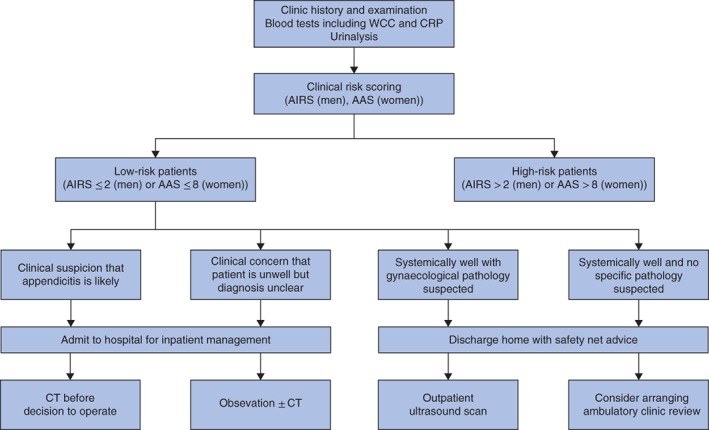
Proposed clinical algorithm for patients presenting with suspected appendicitis or right iliac fossa pain, stratified as low risk
WCC, white cell count; CRP, C‐reactive protein; AIRS, Appendicitis Inflammatory Response Score; AAS, Adult Appendicitis Score.
When diagnostic failure does occur in patients stratified to low‐risk groups, the risk of complex appendicitis is very low. Previous studies have suggested that a short delay to appendicectomy does not increase the risk of perforation57. It is likely that many patients in these studies were administered antibiotics while they awaited surgery, and it is not known whether patients with appendicitis who initially receive a period of ambulatory management are at increased risk of perforation, so this should be investigated in future studies.
Collaborators
Writing Group: D. Nepogodiev, J. H. Matthews, G. L. Morley, D. N. Naumann, A. Ball, P. Chauhan, S. Bhanderi, I. Mohamed, J. C. Glasbey, R. J. W. Wilkin, T. M. Drake, J. Clements, N. S. Blencowe, P. J. J. Herrod, F. Pata, M. Frasson, R. Blanco‐Colino, A. S. Soares, A. Bhangu.
Supporting information
Table S1 Clinical components of validated risk prediction models
Table S2 Appendicitis risk prediction models that could not be validated, with tabulation of specific missing data points that would have been required to complete validation
Table S3 Final diagnoses in low‐risk women who did not undergo appendicectomy (n = 1627)
Table S4 Final diagnoses in low‐risk men who did not undergo appendicectomy (n = 175)
Appendix S1 Co‐authors of the study
Appendix S2 Statistical analysis plan
Acknowledgements
The authors are grateful to the Birmingham Surgical Trials Consortium at the University of Birmingham for the use of their servers for secure online data collection.
Disclosure: The authors declare no conflict of interest.
Presented to the 13th Scientific and Annual Meeting of the European Society of Coloproctology, Nice, France, September 2018, and the 2018 International Surgical Conference of the Association of Surgeons in Training, Edinburgh, UK, April 2018; published in abstract form as Colorectal Dis 2018; 20(Suppl 4): 76
Contributor Information
A. Bhangu, Email: a.a.bhangu@bham.ac.uk
RIFT Study Group on behalf of the West Midlands Research Collaborative:
D Nepogodiev, JH Matthews, GL Morley, DN Naumann, A Ball, P Chauhan, S Bhanderi, I Mohamed, JC Glasbey, RJW Wilkin, TM Drake, J Clements, NS Blencowe, PJJ Herrod, F Pata, M Frasson, R Blanco‐Colino, AS Soares, A Bhangu, D Nepogodiev, A Bhangu, JH Matthews, GL Morley, S Bhanderi, A Ball, P Chauhan, S Jain, I Mohamed, T Amuthalingam, R Tyler, JC Glasbey, RJW Wilkin, F Pata, M Frasson, R Blanco‐Colino, AS Soares, A Bhangu, D Nepogodiev, EA Griffiths, TD Pinkney, O Gee, DG Morton, A Beggs, D Beral, A Bhangu, NS Blencowe, D Bowley, N Cruickshank, I Daniels, E Griffiths, ST Hornby, JN Lund, P Marriott, TD Pinkney, P Singh, NJ Smart, D Speake, C Thompson, J Torkington, A Torrance, R Vohra, O Warren, RJW Wilkin, DC Winter, F Pata, G Pellino, A Sgrò, A Simioni, V Farina, M Podda, S Di Saverio, A Birindelli, S Pasquali, ITSurg, AS Soares, PT Surg, R Blanco‐Colino, M Frasson, NS Blencowe, W Bolton, CJ Bradshaw, CS Chean, G Harris, JB Haddow, NB Jamieson, S McCain, J Mason, D Milgrom, GR Nana, MS Noor Mohamed, JO Brien, JCH Pearce, M Rabie, K Sahnan, P Sarmah, C Skerritt, MA Ghazanfar, L Sreedharan, S Kabwama, RT Gray, IW Kamande, S Nazarian, FA Dar, AT Misky, S Arunachalam, CS Twum‐Barima, IM Mohamed, KL Connor, PO Coe, A Kosti, M Elshaer, DA Colvin, MP Charalambous, KTD Yeung, LAG Merker, TEM Morrison, AJ Thaventhiran, TM Gilbert, JM Clements, G Hicks, S Afshar, NC Mckinley, N Assaf, T Hanna, EGE Macinnes, N Thavanesan, AS Dubois, LK Palani‐Velu, S Tezas, LPS Yow, RW Radwan, NB Jamieson, M Abdelrahman, KA Lee, Z A Zarka, NA Mcdowall, CY Tan, ML Venn, DL Ashmore, SE Whitehorn, AM Golder, A Reddy, C Delimpalta, OH Kay, P Sarmah, SM Shah, I Eiben, C Doyle, V Tudyka, E Issa, H West, HK Brewer, EZ Farrow, NS Taylor, CJ Smart, NP Griffiths, C Halkias, P Vitish‐Sharma, SR Knight, NG Mowbray, JB Olivier, KJ Lee, KD Clement, DRR Chrastek, N Panda, MJ Connor, SE Fahmy, ES Bryan, WS Ngu, SO Adegbola, EM Vaughan, W Stupalkowska, LFC Simmonds, A Malik, A Hussein, MJ Karim, T Singhal, R Ormiston, D Nepogodiev, VWS Kung, MA Rabie, JH Park, N Lal, D Worku, M D'Auria, A Ang, M Orizu, E Gammeri, ECS Clough, CH Choy, PJJ Herrod, S Lawday, AJ Hann, D Robinson, BG Wardle, D Mcdonnell, DG Rutherford, LM Hickey, AG Garg, S Rezvani, CR Bell, F Mahmood, S Rehman, G Donaldson, A Peleki, L Pearce, OL Sharp, S Jain, S Singh, DB Thompson, O El‐Tayar, M Hollyman, SN Rupasinghe, DB Toomey, MP Murray, N Amtul, RJ Mersh, RC Newton, W Al‐Khyatt, GF Stephens, SH Abbas, MR Iqbal, CE Brown, S Renshaw, KA Hureibi, UP Pullabatla‐Venkata, N O Donohoe, A Myatt, RJ Egan, K Rangarajan, M Trail, SC Mckay, NFT Engall, E Jerome, DC Townsend, BY Patel, S Pronin, N Chandratreya, JH Choong, TM Mohamed, NJ Hudson‐Peacock, R Manson, S Bhanderi, KRM Hebbar, BS Mothe, CR Weegenaar, M Saad, CR Bowman, F Serventi, F Fleres, C Foppa, G Pata, G Baronio, D Pertile, A Lucchi, A Sagnotta, I Maretto, T Campagnaro, M Gatti, EGJ Gjoni, F Roscio, M Inama, F Coccolini, A Sgrò, F Colombo, A Avanzolini, S Aresu, A De‐Manzoni‐Garberini, DA Merlini, A Chessa, N Tamini, S Mulas, N Cillara, D Coletta, J Atzeni, E Erdas, G Gallo, E Francone, P Di Gioia, A Birindelli, CL Bianchi, F Ferrara, A Biancafarina, M Podda, S Scabini, L Marano, A Miegge, D Sasia, G Savino, F Pata, M Scatizzi, FE D'Amico, GA Arcuri, L Gavagna, G Salamone, F Tatulli, E Goldin, ML Matos, AB Caldeira, J Romano, J Pereira, JGM Azevedo, JM Azevedo, JFF Simoes, ACQ Silva, AS Soares, DP O'Leary, ND Kennedy, EM Quinn, AY Zhang, PM Neary, JA De‐Marchi, BR O'Connor, K Wijesundera, NM Foley, J Wong, ND Kennedy, LA Tiedt, JC Bolger, TM Connelly, OS Ahmed, V Vigorita, V García, J Arredondo, E Redondo, B Sainz, I Aldrey, A Landaluce‐Olavarria, A De Andrés Gómez, E Cordoba, MN Sánchez‐Fuentes, C Cerdán‐Santacruz, J Beltran‐De‐Heredia, MTGM García, T Veres, A García‐Novoa, A Melero Abellán, L García‐Catalá, M Ruiz‐Marín, P Menendez, S Roldán‐Ortiz, JA Navas‐Cuéllar, D Sabia, JC Gomez‐Rosado, M Serrano Navidad, C Caula, ER Sanchez, E Espin‐Basany, D Fernández‐Martínez, AF Bravo‐Gutiérrez, C Payá‐Llorente, P Dujovne, F Lima, V Soria‐Aledo, CJ Gomez, I Pascual‐Miguelañez, M Muinelo, C Magadan Alvarez, HJ Vargas‐Pierola, M Vallve‐Bernal, JM Hidalgo‐Rosas, JJ Arenal‐Vera, F Sena‐Ruiz, L Sanchez‐Guillen, P Villarejo‐Campos, L Tallon‐Aguilar, A Garcea, JM Bennett, L Whittaker, AL Gidwani, CK Byrnes, SMF Saunders, MH Shiwani, N Ashraf, AK Venkatasubramaniam, KE Bevan, D Mcarthur, AK Mustafa, JP Griffith, JM Blazeby, A Charalabopoulos, W Campbell, G Reese, OJ Warren, M Peacock, D Menzies, D Jenner, NJ Eardley, S Yoong, M Abulafi, H Avalapati, R Thompson, P Nastro, R Kochupapy, D Beral, BM Stubbs, R McIntyre, J Crozier, PK Patel, V Pento, WD Beasley, CSD Roxburgh, ST Hornby, H Youssef, R Alexander, S Denley, F Di Franco, A Quddus, A Saha, I Hunter, JAF Hannay, A Reddy, VR Velchuru, GEL Bond‐Smith, Y Salama, A Bhargava, SP Panagiotopoulos, N Watson, V Tudyka, G Garcea, AP Boddy, PG Dunning, Geraint Lloyd, SV Gurjar, CJ Smart, J Hill, B Andrews, A Singh, F Ruzvidzo, G Shingler, D Mahon, S Elgaddal, CJ Payne, IA Shaikh, S Dalmia, MS Nair, JG Finch, KS Chapple, S Bawa, J Watfah, CA Carden, R Makhija, M Rao, J Sarveswaran, V Vijay, S Rekhraj, T Singhal, B Knight, TD Pinkney, MN Siddiqui, JF Sebastian, P Glen, S Vakis, H Ebied, R Vohra, R Rajaram, J Gray, D Mcgrath, G Faulkner, S Gopalswamy, JN Lund, NJ Smart, M Varcada, A Woodward, GL Williams, K Szentpali, R Ravindran, C Bronder, MA Thaha, A Rate, V Daya Shetty, VSR Rao, MS Sajid, B Clements, RT Patel, C Mason, G Branagan, A Torrance, K Maude, G Kaur, A Lyons, P Ainsworth, R Hagger, AZ Zadi, SU Maslekar, J Kinross, S Irukulla, W Hawkins, S Wheatstone, T Magro, STR Bailey, G Marshall, J Mccullough, G Marangoni, EL Leung, CM Borg, S Gopinath, J Torkington, J Kirkby‐Bott, S Yalamarthi, S Mirza, M Brett, S Ramcharan, V Pandey, B Thava, D Speake, N Chandratreya, SM Andreani, SJ Sahay, B Aravind, M Downey, D Nicol, P Whitehouse, A Sharma, N Francis, P Chitsabesan, DJ Stewart, GG Norcia, E Cucinotta, F Cianchi, U Fumagalli Romario, L Taglietti, P Capelli, G Garulli, A Parisi, D Nitti, A Guglielmi, A Alonzo, IS Scandroglio, F Roscio, G Moretto, L Ansaloni, A Pietrabissa, D Foschi, N Vettoretto, G Ercolani, M Coppola, E Colangelo, E Morandi, A Chessa, N Tamini, P Niolu, M Pala, M Coletti, A Pisanu, A Nicolosi, G Sammarco, S Berti, P Soliani, V Tonini, CL Bianchi, M Stella, G Ceccarelli, C De Nisco, S Scabini, G Castagnoli, P De Nardi, F Borghi, F Agresta, A Benevento, S Cantafio, FE D'Amico, MC Cesari, M Rubbini, G Salamone, G Chetta, F De Marchi, MF Nora, HS Sousa, CA Nascimento, CAO Casimiro, SD Costa, MJ Rosa, NMD Carvalho, JCF Correia, AP Gomes, AD Hill, TN Walsh, MA Aremu, J Mulsow, S El‐Masry, J Gillick, J Garvin, M Caldwell, B Mehigan, DC Winter, CB Peirce, F Cooke, K Mealy, A Ruano, G Ais, J Fueyo, E Redondo, B Sainz, AE Parajó, A Landaluce‐Olavarria, JC Bernal‐Sprekelsen, E Cordoba, JA Monzón‐Abad, C Cerdán‐Santacruz, F Blanco, T Veres, A Melero Abellán, A Arroyo, M Ruiz‐Marín, P Menendez, MC Bazán‐Hinojo, JA Navas‐Cuéllar, MI Ramos‐Bernado, JA Lopez‐Ruiz, T Golda, D Julià, MM Cuadrado, E Espin‐Basany, D Fernández‐Martínez, AF Bravo‐Gutiérrez, SA Gómez‐Abril, P Dujovne, J Martinez, JL Aguayo, M Millan, M Alvarez‐Gallego, M Muinelo‐Lorenzo, JI Martin Parra, E Muñoz‐Muñoz, PE González De Chaves‐Rodríguez, G Cánovas‐Moreno, M Rodriguez‐Lopez, JJ Segura‐Sampedro, A García‐Granero, FJ Redondo‐Calvo, L Tallon‐Aguilar, A Garcea, S Dyson, D Thakur, L Sreedharan, C Swords, O Siaw, M Zelazek, R Woo, A Badran, N Aruparayil, P Christopoulos, B Chambers, N O'Neill, RH Long, RT Gray, P Mccaughey, MJ Lynch Wong, RS Mccain, HC Lennox‐Warburton, C Moore, KM Manektella, IW Kamande, S Mcilwaine, S Rupani, DJ Simpson, J Wauchope, M Ng, L Christian, A Crone, JB Haddow, R Sacks, S Nazarian, NRA Symons, A Lazzaro, SD Patil, FA Dar, S Roomi, I Silva, JM Hodgson, C Ly, AT Misky, H Froud, H Patel, S Arunachalam, P Cay, RS Karwal, S Arunachalam, D Danquah‐Boateng, BJM Berry, HD Esmail, CS Twum‐Barima, H Maripi, D Bilku, MA McKelvie, K Miller, A Maina, R Velho, R Hasan, R Clingan, SMH Jah, K Waite, A Jones, S Buckley‐Jones, L Lecky‐Thompson, KL Connor, N Saghir, S Mansoor, D Mistry, R Brown, A Wong, S Gurung, F Wensley, TA Fleming, RKL Griggs, A Kosti, S Haines, S Bedoya, A Beverstock, J Johnson, M Elshaer, G Govind, O Niaz, DA Colvin, ARS Dyal, E Tokidis, S Punj, A Leusink, KTD Yeung, I Rudland, M Kelly, R Morgan, S Al‐Musawi, C Lek, A Gilbert, A Gosal, R Mahoney, I Parwaiz, TEM Morrison, MJ Mitchard, B Ribeiro, H Merai, EA Dean, S Khan, A Baginski, C Mann, W Foers, L Jones, B Woodward, DM Mcwhirter, AT Thomas, TG Gilbert, LW Weatherburn, JP Pilkington, FC Cameron, TM Gilbert, CS Chean, JM Clements, JD Clements, C Mccann, S Davidson, L Hackney, JS Clements, A Martin, G Hicks, DT Du, Z Shakoor, SK Yen, M Adnan, S Ranathunga, S Sana, YH Tay, MY Chin, M Gillespie, AG Brown, U Campbell, N Assaf, M Chatzikonstantinou, B Mahendran, T Flack, M Chowdhary, JM Lim, EGE Macinnes, E Whiteman, JA Shepherd, A Pedder, N Thavanesan, KL Siggens, CW Lai, V Morrison‐Jones, Z Hayat, AS Dubois, I Nehikhare, C Macleod, HC Quinn, A Brown, G Neagle, LK Palani‐Velu, SM Chok, FM Carrano, OA Abbassi, GA Divekar, S Halmer, LPS Yow, V Pento, RE Adams, PL Davies, SY Wong, R Amarasinghe, LE Tague, E Jones, RW Radwan, A Martin, E Jones, NB Jamieson, J Singh, K Boza, SD Kelly, F Morrison, W Hei Chan, NS Blencowe, M Abdelrahman, EJ Wilson, OO Awokoya, SN Griffiths, EN Kirkham, AE Cotton, A Adimonye, PA Leighton, KA Lee, A Abdelrahman, H Cartwright, Z Gates, M Miguras, ZA Zarka, K Khan, C Louw, T Grove, T Badenoch, J Mckeon, NA Mcdowall, CS Wood, RP Leitch, P Sgardelis, MI Perera, D Nagarajan, Y Malam, K Theodoropoulou, ML Venn, S Rajagopal, S Kaptanis, D Popova, O Olagbaiye, S Tayeh, S Rigby, DL Ashmore, MP Harris, SE Whitehorn, KZ Ren, G Liaw, S Zhou, F White, AM Golder, CM Marshall, JH Mitchell, DJ Anderson, V Kanakala, A Hollingsworth, KR Paramasevon, J Milward, S Ahmed, C Delimpalta, BF Fanibi, N Ferguson, EA Dickson, AV Shaw, OH Kay, F Dixon, S Morrish, R Dandy, P Fooks, P Sharma, N Islam, V Tabain, R Keegan, P Sarmah, J Ahel, T Alhammali, J Graveston, EJ Balai, J Graveston, SM Shah, K Rothnie, GP Pankin, IE Eiben, NJ Jackson, M Dhar, D Nash, C Doyle, S Dharamavaram, M Seth, F Chowdhury, M Rezacova, N Seneviratne, EJ Turner, C Currow, E Issa, JD Isherwood, BM Hobson, H West, DH Lui, GR Nana, V Rodger, N Ting, HK Brewer, D Photiou, EZ Farrow, D Taze, S Lodhia, L Earnshaw, K Kumar, A Neale, J Bastianpillai, M Cipparrone, A Barrie, NS Taylor, Z Nash, L Anandan, K Tailor, Z Vinnicombe, S Krivan, R Kuo, A Giorga, H Habib, K Malik, M Bogdan, FP Mahon‐Daly, MJ Athersmith, JA Strange, NP Griffiths, C Wheeler, L Summerfield, RA Khaw, O Ashour, E Iosif, M Fadel, K Gopalakrishnan, N Orme, S Williams, M Rashid, A Sultana, N Patel, SR Knight, R Pearson, T Yasin, V Bevan, NG Mowbray, B Al‐Sarireh, JB Olivier, M Brown, N Mohd, EE Howie, M Poudevigne, C Paget, H Rallage, K Chui, F Fawzi, S Layman, E Okorocha, GM Jama, P Orawiec, O Kouli, A Hassane, KD Clement, J Kilkenny, AA Devine, M Laurenson, I Slezak, T Barker, EYL Lau, M Limbada, J O'Brien, J Weaver, T Barker, N Panda, S Hajibandeh, J Shah, MM Mansour, SN Malik, S Davis, F Trew, SK Bandyopadhyay, K Dart, MJ Connor, S Guru‐Naidu, R Callan, MK Nair, M Alani, E Sezen, S Salim, SE Fahmy, J Shurlock, K Siddique, A Forouzanfar, R Brews, WS Ngu, A Acharya, A Jain, SO Adegbola, K Sahnan, PJ Tozer, J Warusavitarne, KM Emslie, O Collier‐Wakefield, P Sivaloganathan, C Dobson, M Elseedawy, EM Vaughan, W Stupalkowska, L McNally, M Williams, FH Motiwala, S Choi, A Ahmad Asmadi, D Burnside, A Everden, S Suriyakumar, L Sandu, DA Kent, J Bowen, LFC Simmonds, P Long, A Khair, A Malik, K Shah, L Phelan, R Pierre, AA Dhari, A Hussein, M Hoff, MJ Karim, S Nickson, T Setshwaelo, A Chalk, MJ Parkola, A Harlinska, TCW Chan, JG Dudek, R Rolph, M Allen, H Pollard, R Ormiston, R Gormely, H Finlayson, G Ljungqvist, C Peponis, JC Glasbey, R Tyler, MMA Rahman, S Dhesi, MS Noor Mohamed, F Arshad, RJW Wilkin, AR Faris, T Sooriyamoorthy, VWS Kung, EL Springate, W Barnieh, AS Patel, ZA Siddiqui, IA Chishti, J Ayube‐Brown, MR Rabie, L Blake, E Yardimci, S Nagendram, JH Park, GI Neophytou, L Henderson, MMH Farhan‐Alanie, CY Kong, R Ghazala, N Lal, J Evans, N Hussain, M Kabir, D Worku, I Hraishawi, M D'Auria, M Cox, JA Bailey, N Muhibullah, F Yanni, A Ang, M Orizu, R Stevenson, A Nair, C Murphy, O Mcgucken, E Gammeri, R Pandya, H Bowerman, G Lafaurie, GI Van Boxel, K Shanmugarajah, D Maragouthakis, Z Hanif, JD Evans, S Yoganathan, TD Richardson, CH Choy, V Cook, GL Clark, B Rigney, E O'Neill, J Guliani, PJJ Herrod, D Chan, F Harper, T Sian, C Boereboom, JEM Blackwell, E Hardy, H Boyd‐Carson, DG Couch, CA Barter, SN Thoukididou, JR Hatt, CS Jones, S Dean, N Rajaretnam, S Lawday, M Masood, N Thakral, D Griffith, C Doherty, A Longshaw, D Peprah, G Mathew, AJ Hann, A Hook, D Robinson, J Vance‐Daniel, YMS Ibrahim, BG Wardle, KJ Walters, HE Whewell, MA Sherif, M Mckenna, JCH Pearce, D O'Sullivan, C Woodrow, S Gill, A Johnstone, R Gentry, R Irwin, A Forgie, S Welsh, LM Hickey, P Ivey, JK Bullivant, WJ English, A Osterberg, A Morowala, Z Al‐Faham, S Islam, E Tan, AG Garg, S Sadek, N Sihra, D Shrestha, B Chong, A Nadeem, JA Fasuyi, MM Patel, R Daureeawoo, B Okekunle, M Cheruvu, E Mazumdar, F Mahmood, A Hussain, C Patel, M Mcquaid, A Banks, A Robinson, MS Khan, W Riaz, M Verroiotou, JA Cohen, E Kouroumpas, S Rehman, G Donaldson, I Ghaffari, J Moradzadeh, A Peleki, M Kamal, M Gulamhussein, L Pearce, E Gaines, S Ghatorae, S Clark, OL Sharp, A Savill, B Hutchinson, J Chapman, F Wu, W Creasy, M Raymond, S Grosvenor, A Odeh, Y Malik, H Bansal, C Grant, A Raofi, B Ahmed, D Mai, DB Thompson, JEH Souter, RN Hamelmann, S Ikram, O El‐Tayar, A De‐Manzoni‐Garberini, M Hollyman, M Durbacz, N Gilliland, A Salem, D Chudek, SN Rupasinghe, N Ladwa, R Storey, C Fontaine, D Toomey, B Miller, A Robinson, M Oakey, H Smoker, N Amtul, SJ Chapman, SC O'Hagan, W Tahir, GJA Wilcox, A Ahmad, F Akram, TS Baddams, PR Boshier, M Fehervari, S Easdon, RJ Mersh, T Ilozue, ME Adam, RC Newton, S Jokhan, A Foster, K Nambiar, P Bohra, S Janardanan, V Shanmuganathan, F Maqboul, C Ettles, SD Wardle, E Martinou, GF Stephens, A Khasria, R Bagga, D Motter, N Mundkur, Y Pan, SH Abbas, K Akbari, SM Farrell, A Rahim, A Gummaraju, MR Iqbal, A Mahmoud, O Akinsola, N Smallcombe, M Tarazi, C Hanley, CE Brown, UM Campbell, NC Mckinley, S Renshaw, D Franklin, JR Davidson, KA Hureibi, SS Raza, A Krishnamoorthy, Y Rajjoub, M Ali, TC Seddon, RE Payne, A Das, LM Martin, KN Naismith, UP Pullabatla Venkata, VM Manda, N O Donohoe, KM Burns, J Huang, M Samuel, JA Docherty, WL Cheah, R Ooi, M Nyeko‐Lacek, L Marsh, A Prideaux, CH Li, A Poacher, M Lee, M Muzaffar, RJ Egan, A Kara, E Walsh, A Kara, H Sunter, NPG Roth, C Roy, D Mcmorran, A Turnbull, M Trail, GR Layton, JE Archer, P Yang, NFT Engall, L Henderson, E Douka, V Amin, K Borghol, P Marriott, DC Townsend, OD Blackford, S Bond, B Baker, WO Mohamed, R Williams, J Garnham, BY Patel, HD Robb, J Allington, L Cloney, A Tamborska, K Kalia, EJM Fung, Z Johnston, L Lynch, A Christides, HL Tan, G Cynthia, B Tsang, C Rossi, M Kaubrys, N Al‐Khafaji, M Jenkins, JH Choong, SM Chok, GB Peiris, TM Mohamed, S Gunning, E Nimako, D Pandya, P Hever, A Amayo, C Bull, NJ Hudson‐Peacock, C Clements, M Al‐Sheikh, F Savioli, M Long, E Horsfield, C Robertson, S Ogboru, AC Mcilwrath, S Bhanderi, S Bailey, J Bell, KRM Hebbar, C Limb, N Obeid, JE Rich, A Balasubramaniam, BS Mothe, R Mashar, M Taylor, JR Schuster Bruce, CR Weegenaar, G Dennison, NJ Curtis, M Saad, E Ezerska, B Ellis, M Brown, S Wiggill, A Tee, S Ng, CFW Carder, A Abdelwahed, CR Bowman, SB Chandler, BJ Tinsley, G Savino, E Finotti, F Serventi, G Occhioni, F Cossu, I Vulcano, F Viscosi, G Pata, G Baronio, M Michelini, B Compagnoni, C Sepe, SM Isolani, G Regina, D Pertile, A Lucchi, V Alagna, G Martorelli, C Gabbianelli, P Moroni, M Zuin, S Conci, T Campagnaro, G Lazzari, D Costamagna, JH Choong, TZ Zurleni, MA Altomare, EGJ Gjoni, J Desiderio, A Sagnotta, A Di Cintio, A Gemini, S Trastulli, FM Carrano, CE Brown, E Viviani, M Inama, F Coccolini, M Tomasoni, G Montori, A Sgrò, G Harder, F Argenti, S Malabarba, P Checcacci, P Montanelli, F Guerra, I Skalamera, F Staderini, S Grandi, T Nelli, F Coratti, L Sorrentino, A Maffioli, F Colombo, D Cavallo, A Bondurri, G Groppo, R Curti, L Solaini, A Xidas, S Aresu, T Manias, D Delogu, A Vacca, L Solinas, A De‐Manzoni‐Garberini, C Corbellini, L Fiore, A Nigro, L Santurro, M Angrisani, N Tamini, S Mulas, C Sparta, A Lorettu, FA Mura, GV Ruggiu, PF Pirari, R Pau, M Melis, F Piu, S Patti, A Deserra, N Cillara, D Coletta, D Angelieri, C Del Basso, D Rossi, I Iannone, C De Padua, C Giubilo, F Falaschi, B Cirillo, L Gordini, F Podda, S Sanna, E Erdas, A Saba, G Poillucci, E Pinna, A Messina, G Sena, G Sammarco, R Cardona, G Gallo, E De Luca, R Sacco, G Vescio, M Ammendola, R Romano, A Bianco, P Bonfante, L D'Ambra, C Feleppa, E Francone, A Gennai, V Lizzi, E Moggia, M Imperatore, S Bolzon, N Assaf, M Chatzikonstantinou, A Birindelli, A Belvedere, E Amaducci, MC Ripoli, E Segalini, M Cervellera, S Vaccari, CO Eretta, R O'Neill, O Llewelyn, NFT Engall, N Jones, F Clerici, M Ballabio, F Ferrara, E Andolfi, M Angelini, A Biancafarina, A Fontani, E Miranda, M Scricciolo, G Provenza, GA Pellicanò, F Pulighe, M Podda, G Argenio, A Melis, F Balestra, M Anania, A Cruccu, C Massaiu, ML Murru, A Martino, AP Luzzi, G La Valle, S Scabini, CI Zapana Chillitupa, A Bartoli, D Conti, L Marano, A Spaziani, R Bellochi, C Listorti, G Castagnoli, MC Salandini, A Miegge, P De Nardi, M Carlucci, F Pata, SM Tenconi, M Cannavò, D Sasia, A Marano, MC Giuffrida, G Cannata, L Pellegrino, G Giraudo, M Baraghini, A Garzi, R Giudicissi, T Zalla, L Romoli, A Vannucchi, I Giani, F Feroci, M Calussi, M Ribaudo, A Fiorot, T Stecca, FE D'Amico, C Nistri, C Fornasier, GA Arcuri, SV Valiani, DB Brunelli, LE Evoli, NG Giuliani, AC Contine, CR Renzi, CV Feo, G Anania, L Gavagna, P Carcoforo, F Aisoni, G Salamone, L Licari, R Tutino, G Cocorullo, V Silvestri, P De Marco, T Fontana, G Orlando, N Falco, M Baseggio, S Napetti, A Mella, GM Rossi, A Chimetto, E Goldin, M Cosci, M Bonomo, G Scialandrone, N Chetta, ML Matos, LC Carvalho, JS Magalhães, AM Pereira, C Fernandes, A Fareleira, D Gonçalves, M Pais, A Pereira, FM Resende, D Correia, D Cardoso, AFS Tojal, S Catarino Santos, LCS Barbosa, HC Louro, F Bairos, FM Martins, FM Messias, MS Ferreira, FC Borges, P Botelho, MJRT Lima, PM Valente, AA João, JM Guimarães, AS Soares, R Rocha, ST Nogueira, U Kabir, CLL Wong, LS Rahmani, S Tan, S Chng, B Jasinski, SA Cheng, S Mardhiah, K McGlynn, E Hannan, J Burke, ND Kennedy, Z Haveliwala, M O'Neill, M Boland, C Hayes, AMW Fox, A Zaborowski, RM Mitru, JA De‐Marchi, A Mc‐Dermott, D Coyle, I Stoica, SV McMahon, BR O'Connor, D Mc Laughlin, M Kannegieser‐Bailey, R Murphy, A Muntean, S Shet, L Thomas, S De Freitas, S Quill, A Aljorfi, NM Foley, BWT Soh, JJ Law, J Hartnett, T Jansen, JET Gilgan, J Jung, K Scanlon, A Szucs, J Wong, DP Ahern, AE Redmond, A Szucs, SE Edwards, LA Tiedt, P Manoharan, S Brennan, JC Bolger, AM Abdelgadir, KL Mckevitt, MA Zarog, G Ahmed, W Bukhari, A Ahad, OS Ahmed, M Paniagua, C Samartin, JC Primo, L Garrido, M Lopez, E Rufo, I Trostchansky, L Rodriguez, H Infante, A Acosta, P Cremades, A Cidoncha, V Olmos, I Oliva, C Santamaria, A Cavero, H Calvo, CA Suero, VM Maderuelo, P Galvez, A Hernando, I Eguaras, AC Recreo, M García‐Carrero, R Moreda, M García, U De Andres, E Del Pozo, M Calvo, C Navarro Moratalla, R Núñez Ronda, R Gómez Contreras, C Báez De Burgos, GF Valderas Cortés, C Cifre Martínez, A Rios Agudo, J Tárraga Soriano, XM Hernández Ramos, E Echazarreta, M Elia, A Hernaez, L Sanchez, C Vallejo‐Bernad, JR Oliver, M Sánchez‐Rubio, HK Kälviäinen, S Genzor, T González‐Nicolás, E Puerta, E Laviano, T Gimenez, C Cerdán‐Santacruz, A Fermiñán, P Muriel‐Álvarez, JE Sierra‐Grañón, J Escoll‐Rufino, E Cuello‐Guzmán, N Mestres‐Petit, M Merichal‐Resina, A Pinillos‐Somalo, Z Gomez‐Carmona, AP Vazquez‐Fernandez, JJ Trujillo‐Diaz, JLRC Rodríguez Couso, MIDR Darriba Fernández, E Riera, J Espinosa, A García‐Novoa, M Carral‐Freire, R Martínez‐Almeida, S Santarrufina‐Martínez, JC Sebastián‐Tomás, P Gonzálvez‐Guardiola, E Corral Fernández, A Sánchez Mozo, T Ivanov Stoyanov, P Casado Santamaría, E García Grimaldo, L García‐Catalá, A Fernández‐Candela, C Curtis‐Martínez, SR Del‐Valle‐Ruiz, A Sánchez‐Cifuentes, M Ramírez‐Faraco, AJ Fernández López, C Leon, S Kumar, M Fornell‐Ariza, S Ayllón‐Gámez, C Peña‐Barturen, L Ojea‐Ruiz‐Yherla, M Saavedra‐Chacón, JA Navas‐Cuéllar, J Perez‐Calvo, H Gomez‐Facundo, L Riba‐Combatti, O Crusellas Manas, B De‐Soto‐Cardenal, P De‐La‐Herranz‐Guerrero, C Dominguez‐Sanchez, JC Gamero‐Huaman, A Suarez‐Cabrera, AA Ramirez‐Redondo, Y Lara‐Fernandez, B Bascuas‐Rodrigo, BL Lopez‐Duran, C Caula, A Pigem, J Gil, H Salvador, P Planellas, R Farrés, ER Sanchez, A Caballero, M Arnau, R Blanco‐Colino, I Tapiolas, N Ridaura, L Sobrino Roncero, F Collado‐Roura, L Martinez Fijo, M Serrano Navidad, O Barrios Cormenzana, N Lluís Viñas, M Sorribas Grifell, M Alberich Prats, A Alvarez Torrado, S Sanz‐Navarro, E Contreras‐Saiz, L Solar‐García, M Moreno‐Gijón, A Suárez‐Sánchez, T Díaz‐Vico, D Fernández‐Martínez, JL Rodicio‐Miravalles, C García‐Gutierrez, U Pila, S Melone, L Martin‐Prieto, JA Rojo, M Gonzalez, L Zorrilla, V Soria‐Aledo, JA Garcia‐Marin, M Baeza‐Murcia, E Pellicer‐Franco, MA Jimenez‐Ballester, L Asensio‐Gomez, S Gortazar‐De‐Las‐Casas, J Guevara‐Martinez, M Lopez, L Ramirez, S Verea, F Anguita, G Navarro, A Del Castillo Criado, M Cañon Lara, E Toledo Martinez, A Sanchez‐Martinez, L Hernandez‐Gimenez, M Galofre‐Recasens, I Ferrer‐Vilela, LE Pérez‐Sanchez, M Burneo Esteves, A Menéndez‐Moreno, C Baz‐Figueroa, A Rosat, M Savoie Hontoria, N Alonso García, R Gracia‐Roman, M Pascua‐Sole, O Pino‐Perez, JM García‐Pérez, C Pineño‐Flores, D Ambrona‐Zafra, L Sanchez‐Guillen, J Sancho‐Muriel, E Alvarez, A García‐Granero, R Jiménez‐Rosellón, O Daga, A Alberca‐Paramo, S Sanchez‐Garcia, E García‐Santos, F Pareja‐Ciuró, C Olivares‐Oliver, L Navarro‐Morales, MJ Tamayo‐López, J Tinoco‐González, CO García‐Rivera, I Alarcón‐Del Agua, F Moreno‐Suero, E Pereira‐Mosquera, C Zerpa, E Llacer, A Diaz, A Caro, F Feliu, M Franco, J Escuder, M Abellan, E Padilla, M Rodriguez‐Lopez, S Mambrilla‐Herrero, KT Plua‐Muniz, M Bailon‐Cuadrado, FJ Tejero‐Pintor, E Choolani‐Bhojwani, C Vila‐Zarate, LJ Delgado‐Plasencia, L Ponchietti, G Pata, L Cousins, A Busuttil, C Baird, N Drye, OD Brown, S Mansour, O Anderson, B Woodward, R Mahapatra, JA Clements, N D'Souza, R Thompson, DJ Littlehales, AM Tang, BE Byrne, CY Tan, P Cunha, C Ogbuokiri, T Alhammali, P Eiben, F Chowdhury, G Gravante, H Kho, S Lodhia, S Dobbs, T Doulias, JCK Ng, MSJ Wilson, R Venugopal, N Panda, J Wolff, K Akhtar, HD Walji, JM Tognarelli, KA Knight, A Ansari, SA Hussaini, E Wright, E Gammeri, H Brewer, S Rinkoff, RL Harries, CJ Fairfield, LM Hickey, TEF Abbott, A Jackson, HL Wright, U Walters, K Carney, PC Logan, Z Mughal, E Strachan, M Boland, SM Andreani, B Chasty, A Sharma, JKY Ma, C Mazzeo, B Badii, A Armellini, M Grassia, A Perin, A Ruzzenente, F Roscio, M Magnoli, A Avanzolini, S Mulas, N Cillara, N Depalma, A Longheu, M Papandrea, L Dova, M De Prizio, GP Gusai, L Di Zitti, P Geretto, A Azabdaftari, G Chianese, C Elbetti, C Ruffolo, S Giaccari, G Salamone, V Devezas, JS Ferreira, RSA Peixoto, AD Hill, A Alshafei, G Ais, V Simo, H San José, B Ugarte‐Sierra, A De Andrés Gómez, C Cerdán‐Santacruz, J Beltran‐De‐Heredia, MC Bazán‐Hinojo, JA Navas‐Cuéllar, JC Gomez‐Rosado, A Bravo Salva, N Gómez, F Marinello, V Medina‐Arana, C Payá‐Llorente, L Vega, M Mengual Ballester, B Espina, MI Prieto‐Nieto, M Lopez, E Caballero Rodríguez, M Rodriguez‐Lopez, M Frasson, D Padilla‐Valverde, and VM Duran‐Muñoz‐Cruzado
References
- 1. GlobalSurg Collaborative . Mortality of emergency abdominal surgery in high‐, middle‐ and low‐income countries. Br J Surg 2016; 103: 971–988. [DOI] [PubMed] [Google Scholar]
- 2. Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet 2015; 386: 1278–1287. [DOI] [PubMed] [Google Scholar]
- 3. Bijnen CL, Van Den Broek WT, Bijnen AB, De Ruiter P, Gouma DJ. Implications of removing a normal appendix. Dig Surg 2003; 20: 115–121. [DOI] [PubMed] [Google Scholar]
- 4. Lee M, Paavana T, Mazari F, Wilson TR. The morbidity of negative appendicectomy. Ann R Coll Surg Engl 2014; 96: 517–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mock K, Lu Y, Friedlander S, Kim DY, Lee SL. Misdiagnosing adult appendicitis: clinical, cost, and socioeconomic implications of negative appendectomy. Am J Surg 2016; 212: 1076–1082. [DOI] [PubMed] [Google Scholar]
- 6. Rogers W, Hoffman J, Noori N. Harms of CT scanning prior to surgery for suspected appendicitis. Evid Based Med 2015; 20: 3–4. [DOI] [PubMed] [Google Scholar]
- 7. Kim K, Kim YH, Kim SY, Kim S, Lee YJ, Kim KP et al Low‐dose abdominal CT for evaluating suspected appendicitis. N Engl J Med 2012; 366: 1596–1605. [DOI] [PubMed] [Google Scholar]
- 8. Yoon HM, Suh CH, Cho YA, Kim JR, Lee JS, Jung AY et al The diagnostic performance of reduced‐dose CT for suspected appendicitis in paediatric and adult patients: a systematic review and diagnostic meta‐analysis. Eur Radiol 2018; 28: 2537–2548. [DOI] [PubMed] [Google Scholar]
- 9. van Rossem CC, Bolmers MD, Schreinemacher MH, Bemelman WA, van Geloven AA, Pinkney TD et al Diagnosing acute appendicitis: surgery or imaging? Colorectal Dis 2016; 18: 1129–1132. [DOI] [PubMed] [Google Scholar]
- 10. Di Saverio S, Birindelli A, Kelly MD, Catena F, Weber DG, Sartelli M et al WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg 2016; 11: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gorter RR, Eker HH, Gorter‐Stam MA, Abis GS, Acharya A, Ankersmit M et al Diagnosis and management of acute appendicitis. EAES consensus development conference 2015. Surg Endosc 2016; 30: 4668–4690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kularatna M, Lauti M, Haran C, MacFater W, Sheikh L, Huang Y et al Clinical prediction rules for appendicitis in adults: which is best? World J Surg 2017; 41: 1769–1781. [DOI] [PubMed] [Google Scholar]
- 13. Royal College of Surgeons of England . Commissioning Guide: Emergency General Surgery (Acute Abdominal Pain); 2014. https://www.rcseng.ac.uk/%E2%88%92/media/files/rcs/standards-and-research/commissioning/commissioning-guide--egs-published-v3.pdf [accessed 5 February 2018].
- 14. Andersson M, Kolodziej B, Andersson RE; STRAPPSCORE Study Group . Randomized clinical trial of appendicitis inflammatory response score‐based management of patients with suspected appendicitis. Br J Surg 2017; 104: 1451–1461. [DOI] [PubMed] [Google Scholar]
- 15. RIFT Study Group on behalf of the West Midlands Research Collaborative . Right Iliac Fossa Pain Treatment (RIFT) Study: protocol for an international, multicentre, prospective observational study. BMJ Open 2018; 8: e017574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP et al The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. BMJ 2009; 339: b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cohen JF, Korevaar DA, Altman DG, Bruns DE, Gatsonis CA, Hooft L et al STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ Open 2016; 6: e012799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. National Surgical Research Collaborative . Multicentre observational study of performance variation in provision and outcome of emergency appendicectomy. Br J Surg 2013; 100: 1240–1252. [DOI] [PubMed] [Google Scholar]
- 19. Sartelli M, Baiocchi GL, Di Saverio S, Ferrara F, Labricciosa FM, Ansaloni L et al Prospective Observational Study on acute Appendicitis Worldwide (POSAW). World J Emerg Surg 2018; 13: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med 1986; 15: 557–564. [DOI] [PubMed] [Google Scholar]
- 21. Andersson M, Andersson RE. The appendicitis inflammatory response score: a tool for the diagnosis of acute appendicitis that outperforms the Alvarado score. World J Surg 2008; 32: 1843–1849. [DOI] [PubMed] [Google Scholar]
- 22. Birkhahn RH, Briggs M, Datillo PA, Van Deusen SK, Gaeta TJ. Classifying patients suspected of appendicitis with regard to likelihood. Am J Surg 2006; 191: 497–502. [DOI] [PubMed] [Google Scholar]
- 23. Chong CF, Adi MI, Thien A, Suyoi A, Mackie AJ, Tin AS et al Development of the RIPASA score: a new appendicitis scoring system for the diagnosis of acute appendicitis. Singapore Med J 2010; 51: 220–225. [PubMed] [Google Scholar]
- 24. Christian F, Christian GP. A simple scoring system to reduce the negative appendicectomy rate. Ann R Coll Surg Engl 1992; 74: 281–285. [PMC free article] [PubMed] [Google Scholar]
- 25. Eskelinen M, Ikonen J, Lipponen P. A computer‐based diagnostic score to aid in diagnosis of acute appendicitis. A prospective study of 1333 patients with acute abdominal pain. Theor Surg 1992; 7: 86–90. [Google Scholar]
- 26. Eskelinen M, Ikonen J, Lipponen P. Sex‐specific diagnostic scores for acute appendicitis. Scand J Gastroenterol 1994; 29: 59–66. [DOI] [PubMed] [Google Scholar]
- 27. Goh PL. A simplified appendicitis score in the diagnosis of acute appendicitis. Hong Kong J Emerg Med 2017; 17: 230–235. [Google Scholar]
- 28. Izbicki JR, Knoefel WT, Wilker DK, Mandelkow HK, Müller K, Siebeck M et al Accurate diagnosis of acute appendicitis: a retrospective and prospective analysis of 686 patients. Eur J Surg 1992; 158: 227–231. [PubMed] [Google Scholar]
- 29. Kalan M, Talbot D, Cunliffe WJ, Rich AJ. Evaluation of the modified Alvarado score in the diagnosis of acute appendicitis: a prospective study. Ann R Coll Surg Engl 1994; 76: 418–419. [PMC free article] [PubMed] [Google Scholar]
- 30. Mikaere H, Zeng I, Lauti M, Kularatna M, MacCormick AD. Derivation and validation of the APPEND score: an acute appendicitis clinical prediction rule. ANZ J Surg 2018; 88: E303–E307. [DOI] [PubMed] [Google Scholar]
- 31. Sammalkorpi HE, Mentula P, Leppaniemi A. A new adult appendicitis score improves diagnostic accuracy of acute appendicitis – a prospective study. BMC Gastroenterol 2014; 14: 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ting HW, Wu JT, Chan CL, Lin SL, Chen MH. Decision model for acute appendicitis treatment with decision tree technology – a modification of the Alvarado scoring system. J Chin Med Assoc 2010; 73: 401–406. [DOI] [PubMed] [Google Scholar]
- 33. van den Broek WT, Bijnen BB, Rijbroek B, Gouma DJ. Scoring and diagnostic laparoscopy for suspected appendicitis. Eur J Surg 2002; 168: 349–354. [DOI] [PubMed] [Google Scholar]
- 34. Van Way CW III, Murphy JR, Dunn EL, Elerding SC. A feasibility study of computer aided diagnosis in appendicitis. Surg Gynecol Obstet 1982; 155: 685–688. [PubMed] [Google Scholar]
- 35. Ahn S, Lee H, Choi W, Ahn R, Hong JS, Sohn CH et al Clinical importance of the heel drop test and a new clinical score for adult appendicitis. PLoS One 2016; 11: e0164574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fenyö G. Routine use of a scoring system for decision‐making in suspected acute appendicitis in adults. Acta Chir Scand 1987; 153: 545–551. [PubMed] [Google Scholar]
- 37. Jahn H, Mathiesen FK, Neckelmann K, Hovendal CP, Bellstrøm T, Gottrup F. Comparison of clinical judgment and diagnostic ultrasonography in the diagnosis of acute appendicitis: experience with a score‐aided diagnosis. Eur J Surg 1997; 163: 433–443. [PubMed] [Google Scholar]
- 38. Jawaid A, Asad A, Motiei A, Munir A, Bhutto E, Choudry H et al Clinical scoring system: a valuable tool for decision making in cases of acute appendicitis. J Pak Med Assoc 1999; 49: 254–259. [PubMed] [Google Scholar]
- 39. Lindberg G, Fenyo G. Algorithmic diagnosis of appendicitis using Bayes' theorem and logistic regression. Bayesian Stat 1988; 3: 665–668. [Google Scholar]
- 40. Ramirez JM, Deus J. Practical score to aid decision making in doubtful cases of appendicitis. Br J Surg 1994; 81: 680–683. [DOI] [PubMed] [Google Scholar]
- 41. Teicher I, Landa B, Cohen M, Kabnick LS, Wise L. Scoring system to aid in diagnoses of appendicitis. Ann Surg 1983; 198: 753–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wilasrusmee C, Siribumrungwong B, Phuwapraisirisan S, Poprom N, Woratanarat P, Lertsithichai P et al Developing and validating of Ramathibodi Appendicitis Score (RAMA‐AS) for diagnosis of appendicitis in suspected appendicitis patients. World J Emerg Surg 2017; 12: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Arnbjörnsson E. Scoring system for computer‐aided diagnosis of acute appendicitis. The value of prospective versus retrospective studies. Ann Chir Gynaecol 1985; 74: 159–166. [PubMed] [Google Scholar]
- 44. Fente BG, Echem RC. Prospective evaluation of the Bengezi and Al‐Fallouji modified Alvarado score for presumptive accurate diagnosis of acute appendicitis in University of Port Harcourt Teaching Hospital, Port Harcourt. Niger J Med 2009; 18: 398–401. [DOI] [PubMed] [Google Scholar]
- 45. Ohmann C, Franke C, Yang Q. Clinical benefit of a diagnostic score for appendicitis: results of a prospective interventional study. German Study Group of Acute Abdominal Pain. Arch Surg 1999; 134: 993–996. [DOI] [PubMed] [Google Scholar]
- 46. Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg 2007; 245: 886–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Strong S, Blencowe N, Bhangu A; National Surgical Research Collaborative . How good are surgeons at identifying appendicitis? Results from a multi‐centre cohort study. Int J Surg 2015; 15: 107–112. [DOI] [PubMed] [Google Scholar]
- 48. Bhangu A, Begaj I, Ray D. Population level analysis of diagnostic laparoscopy versus normal appendicectomy for acute lower abdominal pain. Int J Surg 2014; 12: 1374–1379. [DOI] [PubMed] [Google Scholar]
- 49. Van Vlodrop V, Pattyn P, Ceelen W. Management of the 'normal' appendix during surgery for right fossa syndrome: proposed clinical algorithm. Acta Chir Belg 2007; 107: 8–11. [DOI] [PubMed] [Google Scholar]
- 50. Sammalkorpi HE, Mentula P, Savolainen H, Leppäniemi A. The introduction of adult appendicitis score reduced negative appendectomy rate. Scand J Surg 2017; 106: 196–201. [DOI] [PubMed] [Google Scholar]
- 51. Lahaye MJ, Lambregts DM, Mutsaers E, Essers BA, Breukink S, Cappendijk VC et al Mandatory imaging cuts costs and reduces the rate of unnecessary surgeries in the diagnostic work‐up of patients suspected of having appendicitis. Eur Radiol 2015; 25: 1464–1470. [DOI] [PubMed] [Google Scholar]
- 52. Nepogodiev D, Chapman SJ, Kolias AG, Fitzgerald JE, Lee M, Blencowe NS; National Surgical Research Collaborative . The effect of trainee research collaboratives in the UK. Lancet Gastroenterol Hepatol 2017; 2: 247–248. [DOI] [PubMed] [Google Scholar]
- 53. CholeS Study Group, West Midlands Research Collaborative . Population‐based cohort study of outcomes following cholecystectomy for benign gallbladder diseases. Br J Surg 2016; 103: 1704–1715. [DOI] [PubMed] [Google Scholar]
- 54. Fares A. Summer appendicitis. Ann Med Health Sci Res 2014; 4: 18–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Arthur T, Gartrell R, Manoharan B, Parker D; QUEST Collaboration . Emergency appendicectomy in Australia: findings from a multicentre, prospective study. ANZ J Surg 2017; 87: 656–660. [DOI] [PubMed] [Google Scholar]
- 56. Pidgeon TE, Shariff U, Devine F, Menon V. A report on an acute, in‐hours, outpatient review clinic with ultrasonography facilities for the early evaluation of general surgical patients. Ann R Coll Surg Engl 2016; 98: 468–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. United Kingdom National Surgical Research Collaborative , Bhangu A. Safety of short, in‐hospital delays before surgery for acute appendicitis: multicentre cohort study, systematic review, and meta‐analysis. Ann Surg 2014; 259: 894–903. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Clinical components of validated risk prediction models
Table S2 Appendicitis risk prediction models that could not be validated, with tabulation of specific missing data points that would have been required to complete validation
Table S3 Final diagnoses in low‐risk women who did not undergo appendicectomy (n = 1627)
Table S4 Final diagnoses in low‐risk men who did not undergo appendicectomy (n = 175)
Appendix S1 Co‐authors of the study
Appendix S2 Statistical analysis plan


