Abstract
Aim
To assess the impact of UK specialist and primary care‐based stop smoking support on socio‐economic inequalities in cessation.
Methods
Systematic review and narrative synthesis, with a national equity analysis of stop smoking services (SSS). Ten bibliographic databases were searched for studies of any design, published since 2012, which evaluated specialist or primary care‐based stop smoking support by socio‐economic status (SES) or within a disadvantaged group. Studies could report on any cessation‐related outcome. National Statistics were combined to estimate population‐level SSS reach and impact among all smokers by SES. Overall, we included 27 published studies and three collated, national SSS reports for England, Scotland and Northern Ireland (equivalent data for Wales were unavailable).
Results
Primary care providers and SSS in the United Kingdom were particularly effective at engaging and supporting disadvantaged smokers. Low SES groups were more likely to have their smoking status assessed, to receive general practitioner brief cessation advice/SSS referral and to attempt a quit with SSS support. Although disadvantaged SSS clients were less successful in quitting, increased service reach offset these lower quit rates, resulting in higher service impact among smokers from low SES groups. Interventions that offer tailored and targeted support have the potential to improve quit outcomes among disadvantaged smokers.
Conclusions
Equity‐orientated stop smoking support can compensate for lower quit rates among disadvantaged smokers through the use of equity‐based performance targets, provision of targeted services and the development of tailored interventions.
Keywords: Cessation, disadvantage, primary care, smoking, socio‐economic inequalities, systematic review
Introduction
Throughout high‐income countries, inequalities in smoking contribute substantially to the unequal distribution of health by socio‐economic status (SES) 1. The need to reduce smoking among disadvantaged groups is therefore at the heart of UK tobacco control strategies 2, 3, 4, 5. As the only country in the world to have developed a national state‐funded system of cessation support, the United Kingdom provides a unique source of evidence on the effectiveness of such systems in tackling smoking inequalities.
Smokers in the United Kingdom who want to quit are able to access evidence‐based pharmacotherapy and behavioural support (delivered by specialist or community practitioners in a one‐to‐one or group format) through a network of stop smoking services (SSS) located in multiple settings, including pharmacies, general practitioner (GP) surgeries, community centres and work‐places 6. While these services are known to be effective in supporting cessation 7, systematic reviews consistently suggest an equity‐negative effect, with low SES service users having poorer quit rates than high SES users 7, 8, 9. Performance measures that encompass all smokers (not just SSS users), however, reveal a different picture. Bauld et al. 10, for instance, additionally examined SSS reach (the proportion of smokers making an SSS‐supported quit attempt) and SSS impact (the proportion of smokers making a successful SSS‐supported quit attempt). They found that, while quit rates were lower in more compared to less deprived areas (52.6 versus 57.9%), SSS reach was higher (16.7 versus 13.4%), giving an overall equity‐positive effect in relation to SSS impact (8.8 versus 7.8%). A systematic review by Brown et al. 8, moreover, reported similar findings, concluding that SSS can help to reduce smoking inequalities through the successful targeting and recruitment of disadvantaged smokers.
Alongside the SSS, the National Institute for Health and Care Excellence (NICE, the UK body responsible for national health‐care guidance) recommends that health professionals should seek to engage with smokers at every opportunity, checking the smoking status of patients, advising those who smoke to quit and, where appropriate, making a referral to a stop smoking service 11. Primary care provides a key setting for such brief interventions and in 2004 the Quality and Outcomes Framework (QOF) was introduced which included incentivizing general practitioners to record patient smoking status and to offer cessation advice and/or an SSS referral 12. To our knowledge, no systematic review has yet been undertaken to explore SES differences in the delivery of such brief cessation interventions within primary care.
In recent years, there has been a marked change in patterns of SSS use and reach. The number of people setting a quit date with English services has fallen from approximately 725 000 (8.7% of all smokers) in 2012–13 to 275 000 (4.1% of smokers) in 2017–18 13. Similar declines in service use/reach have been shown in Scotland 14 and Northern Ireland 15, although the reverse trend has been seen in Wales, where the proportion of smokers making an SSS‐supported quit attempt increased from 1.1% in 2012–13 16 to 3.1% in 2017–18 17. SSS quit rates, in contrast, have remained broadly stable, with 4‐week abstinence rates of approximately 50–51% being reported, for example, in England 13. The net combined effect of these trends on SSS impact is unclear.
We provide here an updated and extended assessment of the contribution of UK stop smoking support to reducing socio‐economic inequalities in smoking. Building on the work of Brown et al. 8 and Bauld et al. 10, we combine a systematic review of the published literature with a separate national equity analysis of SSS reach and impact, also broadening the scope of our review to cover GP brief interventions as well as SSS. We address the following research questions:
How does (a) delivery of GP brief cessation interventions, (b) SSS use and quit rates and (c) SSS reach and impact, vary by smoker SES in the United Kingdom?
Which innovative stop smoking interventions demonstrate potential for improving cessation outcomes among low SES smokers?
Methods
Systematic review
This review was underpinned by a conceptual model of the cessation pathway describing the various steps involved in a successful quit attempt (Fig. 1), and was written according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA): Equity Reporting Guidelines 18 (Supporting information, Appendix S1). The study protocol can be found at: http://doi.org/10.13140/RG.2.2.17572.17286.
Figure 1.
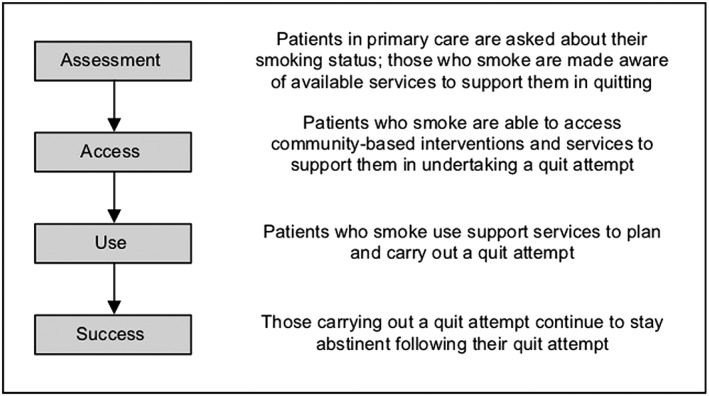
Conceptual model of the cessation pathway
Eligibility criteria
Study eligibility criteria were: evaluated UK specialist or primary care‐based stop smoking support, published since 2012 in English, focused on adult participants (≥ 16 years) and reported at least one pathway‐related outcome (Table 1), and compared this outcome among two or more SES groups (or presented the findings for a specific disadvantaged group). The 2012 cut‐off was chosen for several reasons. Brown et al.'s systematic review 8 covered 13 UK SSS studies published between 2003 and 2012, predominantly reporting on data collected between 2000 and 2007. As no review of GP brief cessation interventions had previously been undertaken, a 2012 cut‐off gave a balance between minimizing overlap with the Brown review and including sufficient years to adequately capture latest evidence on GP brief interventions. Moreover, we intended to explore implications of the SSS transfer from National Health Service (NHS) to local authority control in 2013 19, and thus sought to include evidence gathered prior to this move. Ultimately, such analyses proved impossible, as the majority of eligible SSS studies were based on data collected between 2008 and 2013, with only three official statistics releases containing more recent information. Although two GP studies incorporated data back to the early 2000s, these studies also included longer‐term trend data to 2008–09, so we retained them in our analysis.
Table 1.
Scope of systematic search.
| Pathway‐related outcomes | Ascertainment of smoking status; receipt of brief cessation advice; engagement with services; quit attempts; use of behavioural support and/or pharmacotherapy; quit success | |
| Bibliographic databases | Medline; Web of Science (Core Collection and BIOSIS); EMBASE; PsycINFO; ASSIA; CINAHL Plus; IBSS; Sociological Abstracts; Cochrane Library | |
| Summary search terms | Block 1: Socio‐economic indicators | Education (including levels of literacy); income; occupational class; social grade; composite measures of individual disadvantage; area‐based measures of deprivation [including Carstairs, Townsend and Indices of Multiple Deprivation for England (IMD), Scotland (SIMD) and Northern Ireland (NIMDM)]; Mosaic consumer classification; prescription fee exemption, receipt of state benefits |
| Block 2: Cessation interventions | GP brief interventions (including those delivered through NHS Health Check and QOF); stop smoking services (including behavioural support and pharmacotherapy); innovative GP and SSS‐based interventions (e.g. financial incentive schemes) | |
| Block 3: UK‐based | UK; Great Britain; England; Scotland; Wales; Northern Ireland | |
| Research designs | Randomized controlled trials (RCTs); non‐randomized trials; cohort studies; cross−sectional surveys |
Search strategy and study selection
Ten electronic bibliographic databases (Table 1) were searched on 14 April 2017, using three blocks of search terms covering socio‐economic inequalities, smoking cessation and UK‐based research (Table 1 and Supporting information, Appendix S2A). Eligible papers had to appear in all three blocks, but there were no restrictions on the research designs employed. Relevant grey literature was sourced through key informants and online searches of SSS official statistics.
Duplicates were removed in Endnote by matching on combinations of four identifiers (title, author, year, journal) and manually reviewing possible matches. Titles and abstracts were screened by C.E.S. to identify those evaluating cessation interventions by SES or within a disadvantaged group. Selected articles were then subject to full‐text review to determine whether they met the study eligibility criteria. Results were independently checked by at least one other author, with any disagreements resolved through discussion.
Data extraction and analysis
Standardized data extraction sheets were used to record the following for each eligible study: research design, location, years of data collection, sample characteristics, intervention type and setting, SES measures, cessation pathway steps and intervention outcomes by SES (Supporting information, Appendix S2B). Study quality was assessed using a modified version of the Critical Appraisal Skills Programme (CASP) tools 20, where checklists for randomized controlled trials (RCTs), cohort and case–control studies were combined into a single instrument (Supporting information Appendix S2C). Data extraction and quality appraisal was undertaken by C.E.S. Details were checked by A.A. or S.E.H., who also assessed each paper's overall value to the review (H: high; H/M: high/medium; M: medium; M/L: medium/low; L: low), taking into account both the individual CASP ratings and the relevance of the findings to our research questions. Quality appraisal results for each study are in Supporting information, Appendix S2D.
Wide variation in intervention types and outcomes meant that a meta‐analysis was not feasible. Findings are instead presented via narrative synthesis, with results reported separately by broad intervention type (GP, SSS, innovation) and pathway stage (assessment, access, use, success). Intervention equity impact was assessed for each SES indicator/outcome measure, using an adaptation of the criteria developed by Brown et al. 8 (Table 2). A similar rating system was used to classify the effectiveness of interventions targeted at disadvantaged groups. Equity impact ratings for each study finding can be found in Supporting information, Appendix S2E. Throughout the narrative synthesis, the overall value rating for the paper and the individual equity impact score for each finding (e.g. H,++) are included to indicate the strength and direction of evidence for that result.
Table 2.
Equity impact classification criteria.
| Positive [++] |
Strong evidence that lower SES groups are relatively more responsive to intervention (either a robust measure from a national data set or supported by a formal statistical comparison showing a significant difference between groups) Example: NRT prescription in most versus least deprived: OR = 1.41, 95% CI = 1.11–1.80 (Blane et al. 23) |
| Possibly positive [+] |
Some evidence that lower SES groups are relatively more responsive to intervention (either a weak measure from a national data set or a large difference between groups but study underpowered/no formal statistical analysis undertaken) Example: Smoking status recorded in most versus least deprived: pre‐QOF OR = 1.07, 95% CI = 0.93–1.23; post‐QOF OR = 1.35, 95% CI = 1.21–1.49 (Taggar et al. 12) |
| Neutral [o] |
No evidence that intervention had differential impact across low and high SES groups (must be supported by a formal statistical analysis with reasonable power) Example: Quit success per unit increase in deprivation: OR = 0.98, 95% CI = 0.96–1.01 (Brose et al. 22) |
| Possibly negative [−] |
Some evidence that higher SES groups are relatively more responsive to intervention (either a weak measure from a national data set or a large difference between groups but study underpowered/no formal statistical analysis undertaken) Example: GP cessation advice in most versus least deprived: OR = 0.80, 95% CI = 0.62–1.02 (Blane et al. 21) |
| Negative [– –] |
Strong evidence that higher SES groups are relatively more responsive to intervention (either a robust measure from a national data set or supported by a formal statistical comparison showing a significant difference between groups) Example: Quit success in least versus most deprived: OR = 1.4, 95% CI = 1.1–1.9 (Bauld et al. 32) |
| Unclear [?] |
Not able to assess intervention equity impact based on available evidence Example: Interaction between treatment type and SES non‐significant but OR/CIs not reported so unable to assess power. Wide CIs in main effect analysis of treatment type (Stapleton et al. 24) |
OR = odds ratio; CI = confidence interval; NRT = nicotine replacement therapy; SES = socio‐economic status.
National equity analysis: SSS reach and impact
Estimates of SSS reach and impact, broken down by SES, were calculated by combining data from several nationally representative reporting systems, including annual mid‐year population estimates, survey‐based estimates of smoking prevalence and SSS official statistics. Separate estimates were produced for each UK constituent nation (England, Scotland and Northern Ireland), but could not be generated for Wales as SES‐level data were unavailable. Comparison of each measure across the lowest and highest SES groups allowed an assessment of SSS equity impact by country. Sensitivity analyses explored the effect of missing SES data and coding inconsistencies on the robustness of the equity impact analysis. Full details (including data sources used) are in Supporting information, Appendix S2F.
Results
Systematic review
Bibliographic searches identified 3944 references which reduced to 1767 papers after removal of duplicates (Fig. 2). Initial screening of titles and abstracts led to 1673 articles being excluded, mainly because they did not involve UK data or did not focus on smoking cessation. Full‐text review of the remaining 94 papers identified 27 eligible articles.
Figure 2.
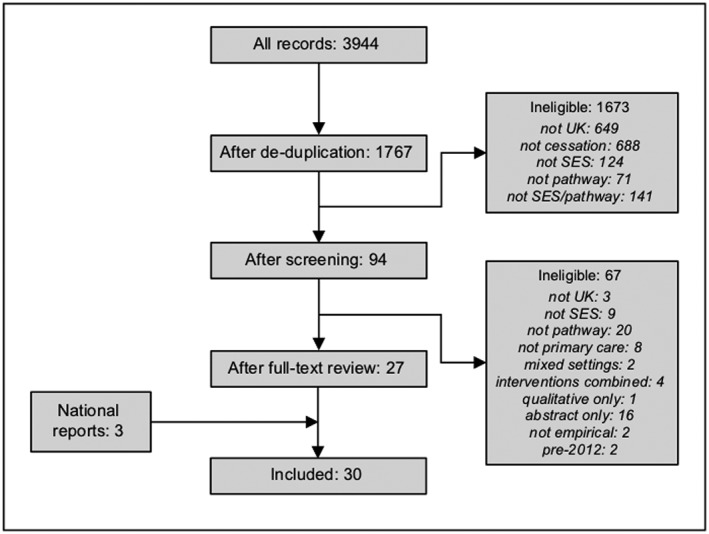
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram
Key informants pointed to seven possible further reports, but none contained data by SES. Online searches of SSS official statistics found 25 reports and workbooks. Two covered services in Wales, but neither presented findings by SES. The remaining 23 were collated to produce summary reports for England, Scotland and Northern Ireland, incorporating data for the time‐period 2009–17. Combined results from the academic and grey literature thus yielded 30 papers (27 academic articles; three national reports) for inclusion in the analysis. Table 3 provides brief study characteristics, the overall value rating and a summary equity impact assessment for each study (the full table of results is in Supporting information, Appendix S2E).
Table 3.
Characteristics and summary findings of included studies.
| Study design | Population | Location | Years for SES analysis | Intervention type | Cessation‐related outcomes | SES measuresa | Value to review2 | Equity impact | |
|---|---|---|---|---|---|---|---|---|---|
| GP brief interventions | |||||||||
| Blane et al. (2017) 21 | Cross‐sectional | Smokers aged ≥ 25 with CHD | Scotland | 2006–07 | Routine care | Advice; prescription | Carstairs | H/M | Mixed |
| Dhalwani et al. (2013) 25 | Before & after | Pregnant females aged 15–49 | UK | 2000–09 | QOF | Smoking status | Townsend | H | Positive |
| Dhalwani et al. (2014) 26 | Cross‐sectional | Pregnant smokers aged 15–49 | UK | 2006–12 | Routine care | Prescription | Townsend | H | Positive |
| Douglas & Szatkowski (2013) 27 | Cross‐sectional | Smokers aged ≥ 16 | UK | 2008–10 | Routine care | Advice; prescription | Townsend; Mosaic | H/M | Positive |
| Forster et al. (2016) 28 | Case–control | Healthy adults aged 40–74 | England | 2010–13 | NHS Health Check | Smoking status | IMD | H | Possibly positive |
| Hamilton et al. (2016) 29 | Before & after |
Healthy adults aged ≥15 |
London | 2006–11 | QOF+ | Smoking status; advice | IMD | H/M | Mixed |
| Hardy et al. (2014) 30 | Cross‐sectional | Pregnant smokers aged 15–49 | UK | 2006–09 | Routine care | Advice | Townsend | H/M | Positive |
| Taggar et al. (2012) 12 | Before & after | Adults aged ≥ 15 | UK | 2002, 2004 & 2008 | QOF | Smoking status; advice | Townsend | H/M | Possibly positive |
| Stop smoking services | |||||||||
| Bauld et al. (2012) 31 | Cohort | Clients who set quit date | Liverpool & Knowsley | 2009 | Drop‐in rolling group | Success (52 weeks) | Composite | H | Negative |
| Bauld et al. (2016) 23 | Cohort | Clients aged ≥ 16 who set quit date | England (9 areas) | 2012–13 | Mixed | Success (52 weeks) | Composite | H | Negative |
| Brose et al. (2012) 22 | Cohort | Clients who make quit attempt | England | 2009–11 | One‐to‐one | Success (4 weeks) | Occupation; IMD; free prescription | H/M | Mixed |
| Brose et al. (2013) 32 | Cohort | Clients who make quit attempt | England | 2009–11 | Mixed | Medication type; success (4 weeks) | Free prescription | H/M | Negative |
| Brose & McEwen (2016) 33 | Cohort | Clients who make quit attempt | England | 2009–12 | Mixed | Compliance; medication type; success (4 weeks) | IMD; free prescription | H | Negative |
| DoH NI (2016) 34 | Cohort | Clients who make quit attempt | Northern Ireland | 2009–16 | Mixed |
Attempts; success (4 weeks) |
NIMDM | H | Mixed |
| Hiscock et al. (2013) 35 | Cohort | Clients who make quit attempt | England | 2010–11 | Mixed | Support type; success (4 weeks) | Occupation; free prescription | H/M | Mixed |
| Hiscock et al. (2015) 36 | Cohort | Clients aged ≥16 who set quit date | England (9 areas) | 2012–13 | Mixed | Support type; success (52 weeks) | Composite | H/M | Mixed |
| ISD Scotland (2017) 37 | Cohort | Clients who make quit attempt | Scotland | 2009–17 | Mixed | Attempts; success (4 & 12 weeks) | SIMD | H | Mixed |
| McAlpine et al. (2015) 38 | Cohort | Clients aged ≥ 18 who set quit date | London | 2013–14 | Mixed | Success (4 weeks) | Occupation | L | Unclear |
| NHS Digital (2017) 39 | Cohort | Clients who make quit attempt | England | 2009–17 | Mixed |
Attempts; success (4 weeks) |
Occupation | H | Mixed |
| West et al. (2013) 40 | Cross‐sectional | Clients who set quit date | England | 2008–11 | Mixed | Attempts | Free prescription | M/L | Possibly positive |
| Innovations | |||||||||
| Bennett et al. (2015) 41 | RCT | Smokers aged 18–65 registered with GP | UK | 2007–08 | GP communications | Success (3 months) | Literacy level | M | Possibly positive |
| Gilbert et al. (2017) 42 | RCT | Smokers aged ≥ 16 registered with GP | England | 2011–14 | GP communications |
Uptake; success (6 months) |
IMD | M | Possibly negative |
| Maskrey et al. (2015) 43 | RCT | SSS clients who abstinent at 4 weeks | East of England | 2011–13 | SSS relapse prevention booklet | Abstinence (12 months) | Education; free prescription | H/M | Unclear |
| Stapleton et al. (2013) 24 | RCT | SSS clients | South East England | 2004–07 | Pharmacotherapy | Success (6 months) | Education; state benefits | L | Unclear |
| Turner et al. (2013) 44 | Cohort | SSS clients who abstinent at 8 weeks | Nottingham | 2010–11 | NRT for relapse prevention | Accept extended course of NRT | Occupation; free prescription | M/L | Mixed |
| Venn et al. (2016) 45 | Non‐randomized | Smokers who live or work in area | Nottingham | 2011 | Mobile SSS versus one‐to‐one SSS |
Uptake; success (4 weeks) |
Multiple | M | Mixed |
| Kassim et al. (2016) 46 | Cohort | Healthy ethnic minority smokers aged ≥18 | London | 2007–08 | Community outreach SSS | Success (4 weeks) | Deprived area | M | Possibly positive |
| Ormston et al. (2015) 47 | Quasi‐experiment | Smokers from deprived areas | Dundee | 2007–11 | Incentives (mixed settings) | Attempts; success (1, 3 & 12 months) | Deprived area | H/M | Mixed |
| Radley et al. (2013) 48 | Cohort | Pregnant smokers | Tayside | 2007–09 | Incentives (pharmacy) | Attempts; success (4 & 12 weeks) | Deprived area | M/L | Positive |
| Tappin et al. (2015) 49 | RCT | Pregnant smokers aged ≥16 | Glasgow | 2011–13 | Incentives (SSS) | Attempts; success (8 weeks & 6 months) | Deprived area | H/M | Mixed |
Details of the SES measures used can be found in Table 1.
Value to review rating—H: high; H/M: high/medium; M: medium; M/L: medium/low; L: low. CHD = coronary heart disease; GP = general practitioner; SES = socio‐economic status; RCT = randomized controlled trial; IMD = index of multiple deprivation; DoH NI = Department of Health Northern Ireland; ISD = Information Services Division; QOF = Quality and Outcomes; SSS = Stop Smoking Secvices.
Characteristics of included studies
Two‐thirds of included studies investigated the equity impact of existing stop smoking support, with eight assessing delivery of GP brief interventions (through both routine care and specific initiatives such as the NHS Health Check) and 12 focusing on SSS. The remaining 10 evaluated innovative interventions in diverse settings. A wide variety of outcome measures were considered, covering all stages of the cessation pathway: assessment (recording smoking status), access (receiving cessation advice and engaging with interventions), use (quit attempts and support usage) and success (quit rates).
Delivery of GP brief interventions (eight studies)
Four papers assessed the recording of smoking status in patients’ GP notes (Fig. 3a), with three evaluating the impact of the Quality and Outcomes Framework (QOF), a scheme which incentivized GPs to record smoking status and give brief cessation advice (among other performance indicators) 12. UK‐wide studies by Dhalwani et al. 25 (H,++) and Taggar et al. 12 (H/M,+) found that, after introduction of QOF, the greatest improvement in recording of smoking status was seen for residents of the most disadvantaged areas. In contrast, an enhanced local version of the scheme (QOF+) in one London borough had a negative equity impact (H/M,–) 29. Forster et al. 28 meanwhile examined the effect of the NHS Health Check (a national preventive programme to reduce cardiovascular morbidity) in England, showing that SES inequalities in recording smoking status were no longer apparent after the programme was implemented (H,+).
Figure 3.
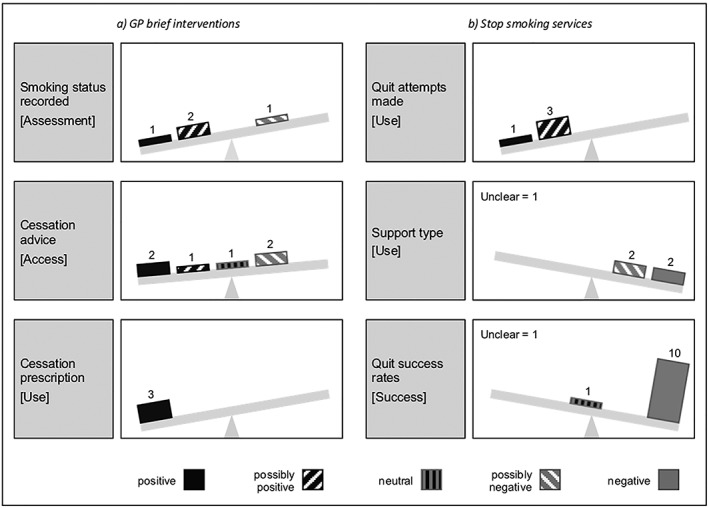
Equity impact of existing stop smoking support
Of the five papers examining provision of brief cessation advice (including SSS referral), two national studies [Douglas & Swatkowski 27 (H/M,++); Taggar et al. 12 (H/M,+)] showed that advice was more commonly recorded in notes for smokers from the most deprived areas of the United Kingdom. Some variation was apparent across patient subgroups: at a UK‐level, Hardy et al. 30 (H/M,++) found brief cessation advice during pregnancy was more likely to be given to low SES smokers; while in Scotland, Blane et al. 21 (H/M,–) showed that patients diagnosed with coronary heart disease (CHD) were less likely to receive cessation advice if they lived in disadvantaged areas. The London‐based enhanced QOF+ (H/M) 29 had a neutral equity impact in males but a negative impact in females.
Finally, three GP studies investigated prescriptions for cessation medication. Here, disadvantaged smokers were more likely to receive a prescription for nicotine replacement therapy both among pregnant patients in the United Kingdom 26 (H,++) and among patients with CHD in Scotland 21 (H/M,++). More broadly, low SES smokers in the United Kingdom were more likely to be prescribed cessation medication of any kind 27 (H/M,++).
SSS use and quit rates (12 studies)
Evidence relating to quit attempts (service use) came primarily from the collated official statistics, with all three reports showing that services in England 39 (H,+), Scotland 37 (H,++) and Northern Ireland 34 (H,+) succeeded in attracting more low than high SES smokers (Fig. 3b). A separate analysis of service monitoring data for English SSSs 40 (M/L,+) similarly reported an equity‐positive effect.
Four papers investigated variations in use of pharmacotherapy and behavioural support. Several studies showed that varenicline was less commonly prescribed for low SES smokers 32, 33, 36 (H/M,– –; H,– –;H/M,–). Findings were more equivocal with respect to behavioural support: one study 36 (H/M,–) found that disadvantaged clients were more likely to use the less effective drop‐in services, but another 35 (/M,?) demonstrated similar patterns of engagement throughout SES groups (although this latter finding was not subject to formal statistical testing).
The most frequently evaluated outcome measure was quit success (service quit rates), with 11 papers assessing socio‐economic differences in quit rates among SSS clients. In addition to the three national reports 34, 37, 39 (H (3)], six studies reported data for England based on a sample of services 22, 23, 32, 33, 35, 36 [H (2); H/M (4)]. Almost all these analyses indicated a negative equity impact over a range of time‐points (from 4 to 52 weeks) and SES indicators. The one exception was Brose et al. 22 (H/M,o/− −), who found that 4‐week quit rates for one‐to‐one support did not vary by the index of multiple deprivation 50 (IMD), although a negative equity effect was apparent by occupational status. Two further studies focused on single services within deprived areas, one reporting falling quit rates with increasing disadvantage for users of drop‐in rolling support groups in Liverpool 31 (H,– –), and the other presenting descriptive data only for a SSS in London 38 (L,?).
Innovative stop smoking interventions (10 studies)
Studies of innovative interventions were divided between those comparing outcomes across SES groups and those focusing solely on disadvantaged smokers (Table 4). Of the six studies assessing equity impact, two investigated interventions tailored towards low SES smokers. Bennett et al. 41 (M,+) conducted an RCT of GP‐endorsed cessation advice where computer‐tailored reports were matched to the smoker's literacy level. The intervention effect on quit rates was greater for the easy‐reading than the standard‐reading group, although wide confidence limits meant differences were not statistically significant. Venn et al. 45 (M) evaluated a mobile stop smoking service (MSSS), which toured deprived areas of Nottingham. This gave mixed results in relation to access, with an equity‐positive effect (++) in terms of the proportion of service users from manual occupations compared to the standard SSS for the same area, but no equity impact (o) for two further SES measures (area deprivation and prescription fee exemption). Among MSSS users, quit rates were also higher (+) for manual workers than for all clients, although quit rates across all client groups were worse compared to the standard service. Four comparative studies explored non‐tailored interventions, with only one 44 (M/L) finding limited evidence of an equity‐positive effect: SSS clients from manual occupations were more likely to use nicotine replacement therapy (NRT) for relapse prevention than those from professional groups (+) or the unemployed (– –).
Table 4.
Details of innovative interventions.
| Studies of equity impact | |
|---|---|
| Bennett et al. (2015) 41 | Customized cessation advice matched to smoker's reading level plus brief endorsement letter from GP (SES tailored) |
| Gilbert et al. (2017) 42 | Customized risk letter from GP plus invitation to attend a no‐commitment taster session at a local stop smoking service |
| Maskrey et al. (2015) 43 | Pack of relapse prevention booklets distributed through stop which aimed to help quitters recognize high‐risk relapse situations and give them the skills to cope in such situations |
| Stapleton et al. (2013) 24 | RCT of three forms of pharmacotherapy (NRT alone, bupropion alone, and combination NRT + bupropion) delivered through stop smoking services (SSS) |
| Turner et al. (2013) 44 | Extended course of NRT for relapse prevention given to SSS clients who remained successfully quit at 4 weeks |
| Venn et al. (2016) 45 | Mobile drop‐in, community‐based stop smoking service which sought to improve reach among disadvantaged smokers (SES tailored) |
| Studies of interventions targeted at disadvantaged groups | |
| Kassim et al. (2016) 46 | Community‐based outreach stop smoking service with opportunity to receive support in smoker's native language from adviser of same gender |
| Ormston et al. (2015) 47 | Financial incentives scheme (quit4u) targeted at smokers living in deprived areas delivered across a range of primary care settings |
| Radley et al. (2013) 48 | Financial incentives scheme (Give It Up for Baby) targeted at pregnant smokers in deprived areas delivered through community pharmacies |
| Tappin et al. (2015) 49 | Financial incentives scheme targeted at pregnant smokers in deprived areas delivered through community‐based stop smoking services |
GP = general practitioner; RCT = randomized controlled trial; NRT = nicotine replacement therapy; SES = socio‐economic status.
The remaining four papers assessed the efficacy of innovations targeting smokers from disadvantaged areas. Three explored the impact of financial incentive schemes in Scotland: a cohort study of a pharmacy‐based intervention for pregnant smokers 48 (M/L), an RCT of an SSS‐administered scheme for pregnant smokers 49 (H/M) and a quasi‐experimental evaluation of a programme for all residents delivered across various primary care settings 47 (H/M). Only Radley et al. 48 found an improvement in quit attempts, but all three schemes demonstrated higher quit success rates than those reported across a range of other comparator interventions. The final targeted innovation 46 (M,+) was a community outreach SSS for smokers from a minority ethnic group (British Bangladeshis), offering one‐to‐one cessation support to clients in their native language from gender‐matched community workers. This reported better quit outcomes than the standard SSS.
National equity analysis: SSS reach and impact
Robust estimates of SSS reach and impact by SES were only available for Scotland. Here, smokers living in the most deprived areas (SIMD1 and 2) were more likely to attempt to quit with SSS support than those in the least disadvantaged areas (SIMD5), with an equity‐positive effect on reach being evident throughout the period 2009–17 (Fig. 4a). SSS impact at 4 weeks (Fig. 4b) was initially higher for the most affluent smokers, but this pattern reversed from 2011 onwards, following the introduction of deprivation‐based equity targets for Scottish SSSs (HEAT targets) 51. In contrast, 3‐month SSS impact remained equity‐negative (apart from briefly during 2011) until further changes to the SSS equity targets in 2014 (shifting the focus to more sustained quitting) saw the rate for disadvantaged smokers overtake that for affluent smokers (Fig. 4c). These results suggest that SSS in Scotland may have an equity‐positive effect on smoking inequalities, with successive refinements of the equity targets possibly playing a role.
Figure 4.
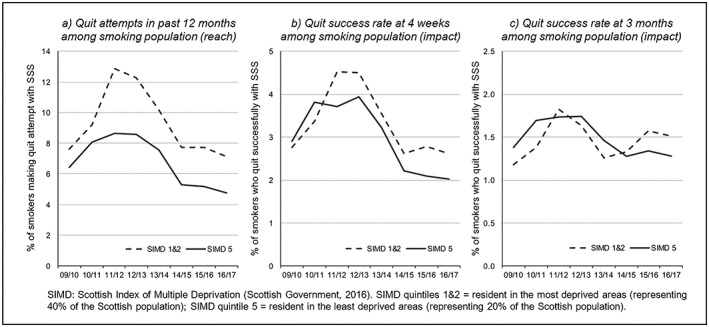
Reach and impact of stop smoking services (SSSs) in Scotland by socio‐economic status (SES), 2009–17
Equivalent SSS reach and impact analyses for English SSSs were inconclusive, due to issues with availability and consistency of SES measures among source data sets. Results in Northern Ireland were similarly affected by missing SES data, although recent improvements in recording meant that more reliable estimates could be produced for 2015–16. Here, comparison of the most and least disadvantaged areas suggests that SSS in Northern Ireland may also have an equity‐positive effect on service reach and impact. Full details of the national equity/sensitivity analyses for England and Northern Ireland are in Supporting information, Appendix S2(F).
Discussion
Our review, covering 27 academic articles and three national reports, suggests that stop smoking support in the United Kingdom plays an important role in addressing socio‐economic inequalities in smoking through a combination of reach and support. GP brief interventions were equity‐positive in terms of identifying disadvantaged smokers and encouraging them to quit: low SES groups were more likely to have their smoking status recorded, be offered brief cessation advice and/or SSS referral and be provided with cessation medication. SSS attracted higher numbers of disadvantaged smokers, although results were less positive in relation to quit rates which were consistently lower among deprived client groups. There was also some evidence that low SES smokers were less likely to be prescribed varenicline, the most effective form of pharmacotherapy 52. While evidence was more limited regarding SSS reach and impact, equity results were nevertheless encouraging. Increased SSS reach among low SES smokers in Scotland, and possibly also Northern Ireland, more than compensated for lower quit rates, resulting in an overall equity‐positive effect on impact. Several innovative approaches showed promise, including interventions that could be offered through existing channels (e.g. incentive schemes for smokers 47, 48, 49, tailored advice matched to literacy levels 41) and interventions targeted at disadvantaged groups (e.g. mobile 45 or outreach 46 services in low SES communities).
Ours is the first systematic review, to our knowledge, to examine socio‐economic differences in the delivery of brief cessation interventions within primary care, and we demonstrate that GPs in the United Kingdom have been particularly successful at engaging and supporting low SES smokers. The QOF 12 was introduced in 2004 with the aim of incentivizing GPs to deliver such brief interventions, and our review suggests that QOF may have been especially effective at improving intervention rates in disadvantaged smokers, potentially helping to reduce inequalities in cessation and smoking. These advances are, however, under threat following the discontinuation of QOF in Scotland from 2016, and amid growing dissatisfaction with the framework in England 53. Alongside this, there have been significant recent declines in primary care prescriptions for smoking cessation medications throughout the United Kingdom, with some parts of England issuing guidance to GPs discouraging the prescription of such medications 54, possibly endangering the equity‐positive pattern of prescribing identified in the current review. A lack of evidence gathered since 2013 limits our ability to assess the effects of these policy developments, emphasizing the need for continued research investment.
In line with past studies 7, 8, 9, we show that quit success rates among disadvantaged SSS clients continue to lag behind those of their more affluent counterparts. Unlike the review by Brown et al. 8, we found no studies that examined equity effects in relation to SSS reach and impact, although we were able to produce such an analysis for Scotland. Despite steep declines in recent years in the numbers making an SSS‐supported quit attempt 14, we provide evidence that Scottish services have maintained a net equity‐positive effect on quit success rates in the smoking population. Our results also suggest a possible role for equity‐based SSS performance targets of the type introduced by the Scottish Government 51. The rapid drop in SSS use is apparent across the United Kingdom and, while specific reasons for this remain unclear, contributing factors may include falling investment in services 19, 55, the transfer of English SSS to local authority control (with some smokers no longer having access to a stop smoking service) 19, reduced use of mass media campaigns 55 and the emergence of e‐cigarettes as a cessation aid 56. Given the lack of recent data (particularly for England and Wales), and in light of changes in the organization, funding and use of SSS, research is required to determine whether services in all parts of the United Kingdom have been able to sustain their previous equity‐positive effect 8, 10 at the population level.
This systematic review was underpinned by a conceptual model of the cessation pathway and was comprehensive and inclusive in scope, encompassing a wide range of research designs, socio‐economic indicators and outcome measures. This approach enabled us to consider stop smoking support at every stage of the cessation pathway (including GP attempts to engage with smokers and encourage them to quit), and not just during the actual quit itself. Nevertheless, our study has several limitations. First, in keeping with previous reviews 8, 9, only a third of the identified studies were designed with the primary aim of evaluating equity impact, although several papers focused on the experiences of disadvantaged smokers. Thus, while the quality of many of the studies was high in relation to their main research question, we encountered problems (e.g. low statistical power and a lack of adequate comparators) when trying to assess socio‐economic differences in cessation support. Moreover, while we attempted to source relevant grey literature in order to reduce the potential impact of publication bias (the tendency of academic journals to publish research that demonstrates an intervention effect) 57, none of the reports identified by key informants contained SES data. It is possible that equity‐neutral findings are under‐represented within our review. Next, as we were unable to conduct a meta‐analysis due to wide variation in intervention types and outcome measures, we presented instead a narrative synthesis accompanied by a visual representation of the equity impact findings using a vote‐counting approach (Fig. 3). Here, we sought to mitigate difficulties with the interpretation of borderline or non‐statistically significant results 57 by using possibly positive‐/negative‐equity impact ratings for studies that were underpowered or that contained no formal statistical analysis. Nevertheless, caution in interpretation is still required, as this graphical approach assumes equal weighting of all study findings 57. Finally, our search identified only one qualitative paper 58 (exploring disadvantaged smokers’ perceptions of the mobile stop smoking service described by Venn et al. 45) which could not be usefully integrated into our analysis. This dearth of qualitative evidence somewhat restricts our understanding of the reasons why certain interventions might be more successful in achieving an equity‐positive effect than others.
In conclusion, this review highlights the potential of stop smoking support in helping to reduce socio‐economic inequalities in smoking. Primary care providers and stop smoking services can together provide support to smokers across all stages of a quit attempt, facilitating a ‘joined‐up’ approach to cessation that may be particularly important for those from lower socio‐economic groups. High levels of SSS uptake among low SES smokers are essential to compensate for their lower rates of quit success, and brief interventions by GPs that identify and channel disadvantaged smokers towards appropriate forms of behavioural support and pharmacotherapy are key to accomplishing this. Changing models of funding and service delivery can threaten the success of such support, emphasizing the need for sustained commitment and investment in the development and delivery of cessation support targeted at disadvantaged smokers.
Declaration of interests
None.
Supporting information
Acknowledgements
This study was commissioned and funded by Cancer Research UK ‐ Policy Research Centre for Cancer Prevention (ref: C3721/A25121). The views expressed are those of the authors and not necessarily those of Cancer Research UK. The funder had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation and approval of the manuscript. We would like to thank colleagues at the following organizations for their help in identifying possible sources of grey literature: Public Health England, Wakefield Council, Fresh North East, NHS Health Scotland, ASH Wales, Welsh Government, Public Health Wales and Cancer Research UK.
Smith, C. E. , Hill, S. E. , and Amos, A. (2020) Impact of specialist and primary care stop smoking support on socio‐economic inequalities in cessation in the United Kingdom: a systematic review and national equity initial review completed 22 January 2019; final version accepted 19 July 2019 analysis. Addiction, 115: 34–46. 10.1111/add.14760.
References
- 1. Jha P., Peto R., Zatonski W., Boreham J., Jarvis M. J., Lopez A. D. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet 2006; 368: 367–370. [DOI] [PubMed] [Google Scholar]
- 2. Department of Health. Towards a Smokefree Generation: a Tobacco Control Plan for England. London: Department of Health; 2017. [Google Scholar]
- 3. Scottish Government. Raising Scotland's Tobacco‐Free Generation: Our Tobacco‐Control Action Plan 2018. Edinburgh: Scottish Government; 2018. [Google Scholar]
- 4. Department of Health (DoH) and Social Services and Public Safety Northern Ireland (DHSSPS NI). Ten‐year Tobacco Control Strategy for Northern Ireland. Belfast: DoH NI; 2012. [Google Scholar]
- 5. Welsh Government . Tobacco Control Action Plan for Wales. Cardiff: Welsh Government; 2012. [Google Scholar]
- 6. Bauld L., Coleman T., Adams C., Pound E., Ferguson J. Delivering the English smoking treatment services. Addiction 2005; 100: 19–27. [DOI] [PubMed] [Google Scholar]
- 7. Bauld L., Bell K., McCullough L., Richardson L., Greaves L. The effectiveness of NHS smoking cessation services: a systematic review. J Public Health 2010; 32: 71–82. [DOI] [PubMed] [Google Scholar]
- 8. Brown T., Platt S., Amos A. Equity impact of European individual‐level smoking cessation interventions to reduce smoking in adults: a systematic review. Eur J Public Health 2014; 24: 551–556. [DOI] [PubMed] [Google Scholar]
- 9. Hill S., Amos A., Clifford D., Platt S. Impact of tobacco control interventions on socio‐economic inequalities in smoking: review of the evidence. Tob Control 2014; 23: e89–e97. [DOI] [PubMed] [Google Scholar]
- 10. Bauld L., Judge K., Platt S. Assessing the impact of smoking cessation services on reducing health inequalities in England: observational study. Tob Control 2007; 16: 400–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. National Institute for Health and Care Excellence (NICE) . Stop smoking interventions and services [NG92]. London: Public Health England, 2018. Available at: https://www.nice.org.uk/guidance/ng92 (accessed 16 March 2019). [Google Scholar]
- 12. Taggar J. S., Coleman T., Lewis S., Szatkowski L. The impact of the quality and outcomes framework (QOF) on the recording of smoking targets ion primary care medical records: cross‐sectional analyses from the health improvement network (THIN) database. BMC Public Health 2012; 12: 329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. NHS Digital . Statistics on NHS stop smoking services in England—April 2017 to March 2018. Leeds: NHS Digital; 2018, p. 2018. [Google Scholar]
- 14. Information Services Division (ISD). Scotland NHS Smoking Cessation Service Statistics (Scotland) 2017/18. Edinburgh: ISD Scotland; 2018. [Google Scholar]
- 15. Department of Health, Northern Ireland (DoH NI). Statistics on Smoking Cessation Services in Northern Ireland 2017/18. Belfast: DoH NI; 2018. [Google Scholar]
- 16. Stop Smoking Wales. Annual report 2012–2103. Pontypool: Public Health Wales; 2013. [Google Scholar]
- 17. StatsWales . NHS Smoking Cessation Services in Wales. Cardiff: Welsh Government, 2019. Available at: https://statswales.gov.wales/Catalogue/Health-and-Social-Care/NHS-Performance/smoking-cessation-services/welshresidentsmokersmadequitattemptvianhs-by-lhb-cumulativequarters (accessed 16 March 2019).
- 18. Welch V., Petticrew M., Tugwell P., Moher D., O'Neill J., Waters E. et al PRISMA‐equity 2012 extension: reporting guidelines for systematic reviews with a focus on health equity. PLOS Med 2012; 9: e1001333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cancer Research UK (CRUK). Action on Smoking and Health. Feeling the Heat—the Decline of Stop Smoking services in England. London: CRUK; 2018. [Google Scholar]
- 20. Critical Appraisal Skills Programme (CASP) . CASP Checklists. Oxford: CASP; 2017. Available at: http://www.casp-uk.net/checklists (accessed 9 March 2017). [Google Scholar]
- 21. Blane D. N., Mackay D., Guthrie B., Mercer S. W. Smoking cessation interventions for patients with coronary heart disease and comorbidities: an observational cross‐sectional study in primary care. Br J Gen Pract 2017; 67: e118–e129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brose L. S., McEwen A., West R. Does it matter who you see to help you stop smoking? Short‐term quit rates across specialist stop smoking practitioners in England. Addiction 2012; 107: 2029–2036. [DOI] [PubMed] [Google Scholar]
- 23. Bauld L., Hiscock R., Dobbie F., Aveyard P., Coleman T., Leonardi‐Bee J. et al English stop‐smoking services: one‐year outcomes. Int J Env Res Pub He 2016; 13: 1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stapleton J., West R., Hajek P., Wheeler J., Vangeli E., Abdi Z. et al Randomized trial of nicotine replacement therapy (NRT), cessation: effectiveness in clinical practice. Addiction 2013; 108: 2193–2203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dhalwani N. N., Tata L. J., Coleman T., Fleming K. M., Szatkowski L. Completeness of maternal smoking status recording during pregnancy in United Kingdom primary care data. PLOS ONE 2013; 8: e72218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dhalwani N. N., Szatkowski L., Coleman T., Fiaschi L., Tata L. J. Prescribing of nicotine replacement therapy in and around pregnancy: a population‐based study using primary care data. Br J Gen Pract 2014; 64: e554–e560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Douglas L., Szatkowski L. Socio‐economic variations in access to smoking cessation interventions in UK primary care: insights using the mosaic classification in a large data set of primary care records. BMC Public Health 2013; 13: 546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Forster A. S., Burgess C., Dodhia H., Fuller F., Miller F., McDermott L. et al Do health checks improve risk factor detection in primary care? Matched cohort study using electronic health records. J Public Health 2016; 38: 552–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hamilton F. L., Laverty A. A., Huckvale K., Car J., Majeed A., Millett C. Financial incentives and inequalities in smoking cessation interventions in primary care: before‐and‐after study. Nicotine Tob Res 2016; 18: 341–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hardy B., Szatkowski L., Tata L. J., Coleman T., Dhalwani N. Smoking cessation advice recorded during pregnancy in United Kingdom primary care. BMC Fam Pract 2014; 15: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bauld L., Ferguson J., McEwen A., Hiscock R. Evaluation of a drop‐in rolling‐group model of support to stop smoking. Addiction 2012; 107: 1687–1695. [DOI] [PubMed] [Google Scholar]
- 32. Brose L. S., West R., Stapleton J. A. Comparison of the effectiveness of varenicline and combination nicotine replacement therapy for smoking cessation in clinical practice. Mayo Clin Proc 2013; 88: 226–233. [DOI] [PubMed] [Google Scholar]
- 33. Brose L. S., McEwen A. Neighbourhood deprivation and outcomes of stop smoking support ‐ an observational study. PLoS One 2016; 11: e0148194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Department of Health, Northern Ireland (DoH NI) . Statistics on Smoking Cessation services in Northern Ireland 2015/16. Belfast: DoH NI; 2016. [Google Scholar]
- 35. Hiscock R., Murray S., Brose L. S., McEwen A., Leonardi‐Bee J., Dobbie F. et al Behavioural therapy for smoking cessation: the effectiveness of different intervention types for disadvantaged and affluent smokers. Addict Behav 2013; 38: 2787–2796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hiscock R., Dobbie F., Bauld L. Smoking cessation and socio‐economic status: an update of existing evidence from a national evaluation of English stop smoking services. Biomed Res Int 2015. 274056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Scotland Information Services Division (ISD). NHS Smoking Cessation Service Statistics (Scotland) 2016/17. Edinburgh: ISD Scotland; 2017. [Google Scholar]
- 38. McAlpine K., Kośmider L., Anastasi N., Rossabi J. Klinika w Whitechapel jako przykład efektywności angielskiego systemu walki z nałogiem palenia [Effectiveness of smoking cessation services in England—clinic in Whitechapel as an example]. Przegl Lek 2015; 72: 496–499. [PubMed] [Google Scholar]
- 39. NHS Digital. Statistics on NHS stop smoking services in England—April 2016 to March 2017. Leeds: NHS Digital; 2016, p. 2017. [Google Scholar]
- 40. West R., May S., West M., Croghan E., McEwen A. Performance of English stop smoking services in first 10 years: analysis of service monitoring data. BMJ 2013; 347: f4921. [DOI] [PubMed] [Google Scholar]
- 41. Bennett K., Gilbert H., Sutton S. Computer‐tailored smoking cessation advice matched to reading ability: perceptions of participants from the ESCAPE trial. Patient Educ Couns 2015; 98: 1577–1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gilbert H., Sutton S., Morris R., Petersen I., Galton S., Wu Q. et al Effectiveness of personalised risk information and taster sessions to increase the uptake of smoking cessation services (Start2quit): a randomised controlled trial. Lancet 2017; 389: 823–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Maskrey V., Blyth A., Brown T. J., Barton G. R., Notley C., Aveyard P. et al Self‐help educational booklets for the prevention of smoking relapse following smoking cessation treatment: a randomized controlled trial. Addiction 2015; 110: 2006–2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Turner J., McNeill A., Coleman T., Leonardi‐Bee J., Agboola S. Feasibility of offering nicotine replacement therapy as a relapse prevention treatment in routine smoking cessation services. BMC Health Serv Res 2013; 13: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Venn A., Dickinson A., Murray R. L., Jones L., Li J., Parrott S. et al Effectiveness of a mobile, drop‐in stop smoking service in reaching and supporting disadvantaged UK smokers to quit. Tob Control 2016; 25: 33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kassim S., al Haboubi M., Croucher R. Short‐term smoking cessation in English resident adults of Bangladeshi origin: a service review. Nicotine Tob Res 2016; 18: 410–415. [DOI] [PubMed] [Google Scholar]
- 47. Ormston R., van der Pol M., Ludbrook A., McConville S. Amos a. quit4u: the effectiveness of combining behavioural support, pharmacotherapy and financial incentives to support smoking cessation. Health Educ Res 2015; 30: 121–133. [DOI] [PubMed] [Google Scholar]
- 48. Radley A., Ballard P., Eadie D., MacAskill S., Donnelly L., Tappin D. Give it up for baby: outcomes and factors influencing uptake of a pilot smoking cessation incentive scheme for pregnant women. BMC Public Health 2013; 13: 343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tappin D., Bauld L., Purves D., Boyd K., Sinclair L., MacAskill S. et al Financial incentives for smoking cessation in pregnancy: randomised controlled trial. BMJ 2015; 350: h134. [DOI] [PubMed] [Google Scholar]
- 50. Department for Communities and Local Government. The English Indices of Deprivation 2015 statistical release. London: UK Government; 2015. [Google Scholar]
- 51. Scottish Government . H6: Smoking Cessation‐ HEAT Targets 14/15. Edinburgh: Scottish Government, 2016. Available at: http://www.gov.scot/About/Performance/scotPerforms/partnerstories/NHSScotlandperformance/smokingcessation (accessed 18 December 2017).
- 52. Cahill K., Stevens S., Perera R., Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta‐analysis. Cochrane Database Syst Rev 2013; 5: CD009329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Roland M., Guthrie B. Quality and outcomes framework: what have we learnt? BMJ 2016; 354: i4060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. British Lung Foundation. Less help to quit. What's happening to stop smoking prescriptions across Britain. London: British Lung Foundation; 2018. [Google Scholar]
- 55. Reid G., Rennick L., Laird Y., Arnot J., McAteer J. Review of ‘Creating a tobacco‐free generation: A Tobacco Control Strategy for Scotland’. Edinburgh: NHS Health Scotland; 2017. [Google Scholar]
- 56. West R., Brown J. Latest trends on smoking in England from the Smoking Toolkit Study. Powerpoint presentation, updated 27 February 2019. Available at: http://www.smokinginengland.info/latest-statistics/(accessed 17 March 2019).
- 57. Higgins J. P. T., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available at: http://www.handbook.cochrane.org (accessed 17 March 2019).
- 58. Bains M., Venn A., Murray R. L., McNeill A., Jones L. L. ‘You just went in and you got it all sorted straightaway’—what is the appeal of a community‐based mobile stop smoking service? J Smoking Cessat 2015; 10: 65–73. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


