Abstract
Objective
The aim of this study was to examine the association of county‐level food access, recreational opportunities, and natural amenities with participant engagement in a weight management program.
Methods
In this cohort study, participants in the Veterans Health Administration MOVE! weight management program between October 1, 2007, and September 30, 2013, were observed for 12 months after enrollment. Engagement was measured as the number of program visits per year at 12 months. Cross‐sectional analysis and spatial regression were used to examine county characteristics associated with greater participant engagement at 12 months.
Results
A total of 321,624 participants in 2,708 counties were included. Greater engagement was associated with older age, female sex, white race, being married, and being retired. After accounting for similarities between nearby communities, engagement at 12 months was 3.1 visits higher for each additional farmers’ market per 1,000 population (P = 0.01). Engagement was highest for participants living in counties with the most natural amenities (P < 0.001). Recreational opportunities had only a small effect on engagement in the program (β = 0.02 visits at 12 months; P = 0.002).
Conclusions
Consideration of a participant’s county characteristics in addition to other known demographics and program factors may help to explain variation in engagement in weight management programs.
Study Importance.
What is already known?
Engaging participants with overweight or obesity in a weight loss program is critical for improving cardiometabolic health.
Despite understanding many of the associated patient and provider barriers, engagement remains a significant challenge.
What does this study add?
Community characteristics differentially affect engagement in weight management programs.
Participant engagement is higher in communities with farmers’ markets and more natural amenities.
Introduction
Weight management programs and other lifestyle interventions are commonly used to treat patients with risk factors for cardiovascular disease 1, 2, 3. Engaging participants for extended periods of time in these interventions is key to their overall success 4. Unfortunately, weight management programs still face many challenges in continued engagement, which ultimately impacts their long‐term success 3, 4 Current research has shown that engagement in any lifestyle intervention varies between participants and tends to decline drastically in the first 12 months for all participants 5, 6.
The issue of waning engagement is evident even within successful nationwide programs such as the Veterans Health Administration’s (VHA’s) MOVE! program. Although more than 95% of eligible veterans are offered the MOVE! program each year, only 5% to 10% opt to participate, and the noncompletion rate is estimated to be as high as 74%, further stressing the importance of understanding and encouraging continued engagement after recruitment 5, 6, 7. When participants do complete the program, they see long‐term improvements in weight loss, diabetes, and hyperlipidemia 8, 9. Maintaining engagement continues to be a major challenge not only to MOVE! but also to nearly all weight management programs, regardless of program effectiveness 10.
Community characteristics may influence continued engagement with weight management programs but research in this area is lacking. Research in this field has been focused on the influence of community characteristics on obesity and not engagement 11, 12, 13. Jilcott et al. 11 used multilevel generalized linear regression to find an inverse association between supercenters/grocery stores per capita and county‐level obesity 11, 14. In 2013, the authors followed up with additional analyses showing an inverse association between recreational facilities per capita/natural resources and county‐level obesity 12, 14. In addition, Slack et al. 13 used spatial regression to demonstrate a negative association between obesity and fitness centers per capita, natural amenities, and fast food restaurants per capita. Several community characteristics, such as park density, natural amenities, and farmers’ markets, are associated with improved success at reaching weight loss goals 11, 15. However, the role that these community characteristics may play in continued engagement in a weight management program remains unknown 12.
Assessing community characteristics requires an understanding of any potential underlying spatial dependence or of the likelihood that nearby geographic areas influence each other 16. This is particularly important because independence between observations is one of the cornerstone assumptions of linear regression. Generalized estimating equations have the potential to address spatial dependence, but many of the standard correlation matrices are not appropriate for the types of spatial relationships that may occur 16.
The aim of this study is to explore the relationship of food access, recreational opportunities, and natural amenities with participant engagement in the MOVE! weight management program. We hypothesize that these community characteristics will be associated with participant engagement in the MOVE! program. Prior research has shown that there is substantial spatial dependence across communities, necessitating the use of spatial regression to address this question.
Methods
We used a cross‐sectional study design to identify participants enrolled in the MOVE! weight management program at VHA medical centers in the continental United States. Veterans enrolled in programs in Puerto Rico, the Philippines, Alaska, and Hawaii were excluded from this analysis because of the lack of county‐level health information for Puerto Rico and the Philippines and drastic differences in program access and county characteristics for Alaska and Hawaii compared with the continental states. This study was reviewed and approved by the Birmingham Department of Veterans Affairs (VA) Medical Center Institutional Review Board (IRB) with a waiver of informed consent. Additionally, exempt status was granted by the University of Alabama at Birmingham IRB because all data analyses were conducted at the Birmingham VA Medical Center. All research was conducted in accordance with the Declaration of Helsinki.
MOVE! program characteristics
The MOVE! program is an ongoing multifaceted weight management program integrated into primary care in the VHA 17. It was implemented nationwide in the VHA in 2008 17. It is available, free of cost, to all veterans. Veterans are screened at least once each year at their annual primary care visit and, if determined to be eligible, are offered the opportunity to participate in the program. Eligibility was originally defined as BMI ≥ 30 kg/m2. Additional qualifications for individuals with lower BMI, such as the presence of certain comorbidities or a high waist circumference (defined as > 35 inches for women and > 40 inches for men), were added as the program evolved over time 18.
Each program has the option to provide weight loss medications, intensive therapy, and bariatric surgery to MOVE! enrollees. Technology‐linked care and other more specific program options have also been added in recent years. Each hospital is allowed flexibility in determining what MOVE! components to add and how much emphasis is placed on each. The only required components are MOVE! staff support, meeting nationwide screening performance measures, and offering individual counseling sessions.
To better assess program implementation, an annual survey of program coordinators was completed in fiscal years 2008‐2011 and 2013 (5 years). The annual survey is designed and implemented by the VHA National Center for Health Promotion and Disease Prevention to monitor MOVE! progress. The survey assesses the types of program options in use (e.g., bariatric surgery or weight loss medication use) and staffing levels for disciplines involved in the program. Other items related to barriers and facilitators of implementation are included but vary by year. The survey is conducted by the National Center for Health Promotion and Disease Prevention early in the calendar year to reflect answers for the previous fiscal year (ending September 30). Results are typically made available via the MOVE! annual report by the end of the next fiscal year.
Study population
The study population for this analysis included all veterans enrolled in MOVE! between October 1, 2007, and September 30, 2013, with at least one MOVE! visit documented in the medical record (Figure 1). Participants with BMI < 30 (n = 113,871) were excluded from this analysis to accurately capture a population that is considered eligible to participate in the MOVE! program because of weight alone, irrespective of other comorbidities. In addition, participant visits to the program between October 1, 2011, and September 30, 2012, (fiscal year 2012; n = 67,298) were excluded from the analysis because the annual MOVE! survey on program characteristics was not conducted for that year.
Figure 1.
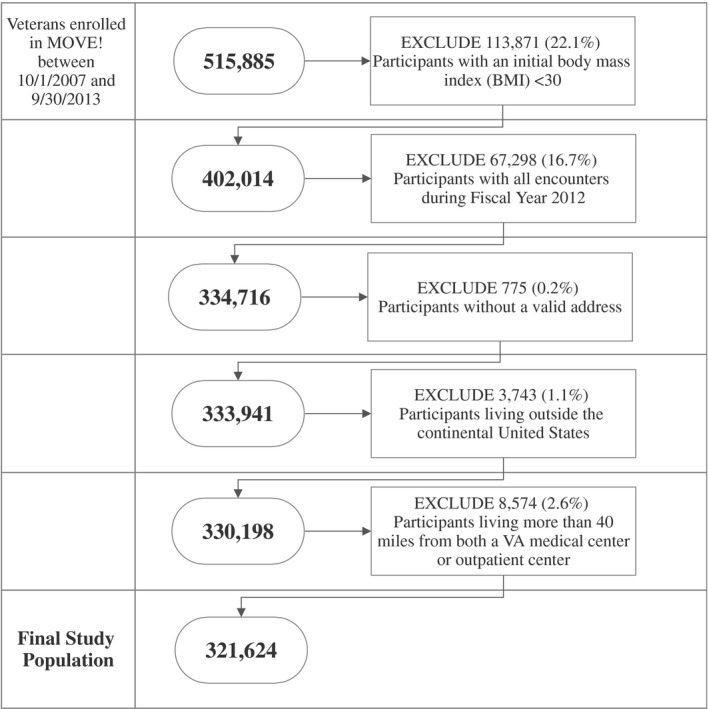
Study population flowchart.
Another 775 participants were excluded because they did not have a valid address, and 3,743 were excluded because they lived outside of the continental United States. Finally, participants living more than 40 miles from both a VA medical center and a VA community‐based outpatient clinic (n = 8,574) were excluded to capture patients with reasonable access to the MOVE! program. The study period was selected to incorporate results from the MOVE! program survey, which was conducted in fiscal years 2008‐2011 and 2013. The final study population included 321,624 MOVE! participants (Figure 1).
Data sources
This study used multiple VHA and non‐VHA data sources to describe participant, program, and county characteristics of the populations served by the MOVE! program. All MOVE! visits were identified using MOVE! program–specific clinic stop codes in the VHA Corporate Data Warehouse (CDW) outpatient domains.
Outcome
Participant engagement in MOVE! was defined as the number of MOVE! visits per year (VPY), with higher VPY indicating greater engagement. Visits were totaled across the 12‐month period, including the participant’s first documented MOVE! visit. The distribution of VPY was highly skewed, and so we categorized the variable as one, two to five, and six or more visits. We made this classification based on prior research of MOVE! engagement. In prior studies, MOVE! participants with six or more visits in a year have been considered “high‐intensity” users and are different from users with less than six visits 8. In addition, the MOVE! program defines participants with less than six visits in the first 6 months as “noncompleters” 5, 6.
Patient‐level variables
Participant demographics were identified in the CDW patient domain. These demographics included age, sex, race, marital status, and employment status at the time of the first MOVE! visit. Comorbidities included the Charlson Comorbidity Index 19 as well as several key cardiovascular risk factors: prior myocardial infarction, peripheral vascular disease, cerebrovascular disease, or diabetes with complications. All comorbidities were obtained from the CDW inpatient and outpatient domains. Baseline BMI was calculated from height and weight measurements in the CDW vital signs domain. The CDW outpatient domain was also used to obtain the patient’s zip code at the time of the first MOVE! visit. The zip code was then mapped to the county of residence and used to define regional location, rurality, and distance to the closest medical center and community‐based outpatient clinic. Patient rurality was defined using the US Department of Agriculture Economic Research Service Rural‐Urban Continuum Codes (2013 version). Nonmetropolitan counties with a population < 2,500 and nonmetropolitan counties with a population < 19,999 and not adjacent to a metropolitan county were considered rural counties.
Program‐level variables
Program characteristics are reported in the annual MOVE! survey available from the VHA Support Services Center. Survey data were available for fiscal years 2008‐2011 and 2013. The program characteristics included in this analysis were the annual number of patients seen, the annual number of new patients seen, the availability of intensive medical treatment, weight loss medication availability, bariatric surgery availability, and reported program staff support in hours per week.
Community‐level variables
County characteristics were obtained from the US Department of Agriculture Food Environment Atlas 20 and County Health Rankings and Roadmaps data 21. All non‐VHA data were linked to participants by the Federal Information Processing Standards code representing a county or county equivalent. County characteristics examined include population size, the number of recreational facilities per 1,000 population, and measures of food access such as the density of grocery stores, supercenters, convenience stores, full‐service restaurants, fast food restaurants, and farmers’ markets per 1,000 population.
The natural amenities index was used to estimate the natural resources available in each county 22. The natural amenities index was developed by the US Department of Agriculture and ranks a county’s natural amenities based on six measures: topographic variation, percentage of water area, average summer (July) and winter (January) temperatures, summer (July) humidity, average winter (January) hours with sun. Topographic variation is measured using a 21‐point scale ranging from flat plains 1 to plains with hills 9 and hills 17 or high mountains 20. The resulting index is the sum of the six measures after they are standardized to zero. Higher values represent more attractive amenities 22. The scale is categorized into seven categories based on deviations from the mean. For the purposes of this analysis, we reduced the scale to five categories as follows: low amenities: > 2 SDs below the mean; moderately low amenities: 0 to 2 SDs below the mean; average amenities: > 0 to 1 SD above the mean; moderately high amenities: > 1 to 3 SDs above the mean; and high amenities: > 3 SDs above the mean.
Statistical analyses
A cross‐sectional analysis of outcomes at 12 months after MOVE! enrollment was employed. The unit of analysis was the participant. We examined the distribution of baseline participant demographics, program characteristics, and county characteristics with univariate statistics. Many of the continuous program and county characteristics were highly skewed, and medians with interquartile ranges were reported for these covariates. Missing data were minimal (< 5%). Program data from the annual MOVE! survey during the year 2012 was missing completely. A complete case analysis excluding data from the year 2012 was undertaken for the remaining analyses.
We calculated the mean and SD, median and interquartile range, or number and percentage to describe the participant, program, and county characteristics by categories of engagement (one, two to five and six or more visits). χ2 tests were used to test for differences across categories of program engagement and categorical variables. ANOVA or Kruskal‐Wallis one‐way ANOVA was used to examine differences among continuous variables. All nonspatial analyses were completed using SAS version 9.4 (SAS Institute, Inc., Cary, North Carolina). α = 0.05 was considered statistically significant for all analyses.
Generalized linear regression with generalized estimating equations to account for clustering within counties was initially employed to understand the association between county characteristics and MOVE! program engagement. Covariates were included in the model if they were significant at α = 0.05 in bivariate analyses. Backwards stepwise regression was used to determine the most parsimonious model. All county characteristics were then forced back in, regardless of statistical significance.
Spatial analyses were then conducted to understand and account for spatial dependence. Moran’s I was used to test for evidence of spatial dependence. Moran’s I is a summary measure of how correlated participant engagement is across nearby locations. Moran’s I ranges from −1 to 1, and a significant value indicates evidence of spatial dependence or the likelihood that nearby geographic areas are more similar than geographic areas that are further apart 16. Finding evidence of spatial dependence would violate the assumption of independence in generalized linear regression.
After finding evidence of spatial dependence, data were aggregated to the Federal Information Processing Standards code level (county), and we conducted simultaneous autoregressive regression to understand the contribution of county characteristics to participant engagement. Simultaneous autoregressive models are similar to standard linear regression but incorporate a variance‐covariance matrix based on a spatial weights matrix 23. The spatial weights matrix is defined as the data with closer geographic areas receiving higher weights than geographic areas that are further away 24. Despite the expansive processing capabilities of the VA Informatics Networking and Computing Infrastructure, our entire model was too large to run as a whole. Bootstrapping methods were undertaken. The data were divided into 10 randomly selected data sets. A separate simultaneous autoregressive model was run on each data set. The final model estimates were calculated as the mean of the estimate across the 10 separate models, and bootstrap CIs were calculated. Spatial analyses were conducted in R using the spdep package (R Core Team, R Foundation for Statistical Computing, Vienna, Austria) 25, 26.
Results
This study included 321,624 participants from 2,708 counties enrolled at 126 MOVE! programs across the continental United States. Participants were observed for 12 months after enrollment in the program. Most participants had only one documented visit in their first year (42.9%), 33.5% had two to five visits in the first year, and 23.6% had six or more visits in their first year (Table 1). Participants with the greatest engagement, six or more visits in their first year versus five or fewer visits in the first year, were older (P < 0.01) and more likely to be white (P < 0.01) or married (P < 0.01) at the time of their first visit. These highly engaged participants also had a higher comorbidity burden (P < 0.01) and greater baseline BMI (P < 0.01). Full‐ or part‐time employment at the time of the first visit was associated with fewer visits in the year following (P < 0.01; Table 1).
Table 1.
MOVE! participant demographics and comorbidities at the baseline visit by participant engagement
| Overall | MOVE! visits in the first year of program participation | P value | |||
|---|---|---|---|---|---|
| 1 | 2‐5 | 6 or more | |||
| Number of participants | 321,624 | 138,013 (42.9%) | 107,724 (33.5%) | 75,887 (23.6%) | … |
| Age, y, mean (SD) a | 56.3 (12.0) | 55.3 (12.6) | 55.9 (11.9) | 58.5 (10.5) | < 0.001a |
| Sex, n (%) | < 0.001b | ||||
| Female | 39,061 (12.1) | 15,402 (11.2) | 14,008 (13.0) | 9,651 (12.7) | … |
| Male | 282,563 (87.9) | 122,611 (88.8) | 93,716 (87.0) | 66,236 (87.3) | … |
| BMI, mean (SD) a | 36.9 (5.4) | 36.4 (5.1) | 37.1 (5.4) | 37.6 (5.7) | < 0.001a |
| Race, n (%) | < 0.001b | ||||
| White | 218,328 (72.9) | 91,392 (71.6) | 72,949 (72.5) | 53,987 (75.8) | … |
| Black | 73,972 (24.7) | 33,011 (25.9) | 25,293 (25.1) | 15,668 (22.0) | … |
| Other | 7,213 (2.4) | 3,246 (2.5) | 2,424 (2.4) | 1,543 (2.2) | … |
| Rurality, n (%) | < 0.001b | ||||
| Metropolitan | 272,594 (84.8) | 118,812 (86.1) | 90,801 (84.3) | 62,981 (83.0) | … |
| Urban | 37,586 (11.7) | 14,713 (10.7) | 13,100 (12.2) | 9,773 (12.9) | … |
| Rural | 11,433 (3.6) | 4,482 (3.3) | 3,820 (3.6) | 3,131 (4.1) | … |
| Miles to closest medical center, mean (SD) a | 35.5 (39.2) | 35.9 (39.8) | 35.3 (40.1) | 35.3 (37.0) | < 0.001a |
| Miles to outpatient clinic, mean (SD) a | 10.2 (8.3) | 10.2 (8.2) | 10.2 (8.3) | 10.3 (8.5) | < 0.001a |
| Marital status, n (%) | < 0.001b | ||||
| Single | 40,773 (12.7) | 18,466 (13.4) | 13,652 (12.7) | 8,655 (11.4) | … |
| Married | 169,831 (52.9) | 71,208 (51.7) | 56,380 (52.5) | 42,243 (55.8) | … |
| Other | 110,292 (34.4) | 47,992 (34.9) | 37,464 (34.9) | 24,836 (32.8) | … |
| Employment status, n (%) | < 0.001b | ||||
| Employed | 91,075 (28.9) | 41,623 (30.8) | 30,497 (28.9) | 18,955 (25.4) | … |
| Retired | 85,117 (27.0) | 33,195 (24.6) | 27,990 (26.5) | 23,932 (32.1) | … |
| Not employed | 139,034 (44.1) | 60,233 (44.6) | 47,191 (44.7) | 31,610 (42.4) | … |
| Region, n (%) | < 0.001b | ||||
| Continental | 63,808 (19.6) | 27,019 (19.6) | 20,730 (19.2) | 15,331 (20.2) | … |
| Midwest | 73,095 (22.7) | 26,881 (19.5) | 26,060 (24.2) | 20,154 (26.6) | … |
| North Atlantic | 73,119 (22.7) | 32,770 (23.7) | 24,438 (22.7) | 15,911 (21.0) | … |
| Pacific | 56,587 (17.6) | 26,368 (19.1) | 18,638 (17.3) | 11,581 (15.3) | … |
| Southeast | 55,743 (17.3) | 24,975 (18.1) | 17,858 (16.6) | 12,910 (17.0) | … |
| Comorbidities | |||||
| CCI, mean (SD) a | 1.1 (1.5) | 1.1 (1.5) | 1.1 (1.5) | 1.2 (1.5) | < 0.001a |
| Myocardial infarction, n (%) | 5,786 (1.8) | 2,475 (1.8) | 1,872 (1.7) | 1,439 (1.9) | 0.04b |
| Peripheral vascular disease, n (%) | 12,716 (4.0) | 5,220 (3.8) | 4,206 (3.9) | 3,290 (4.3) | < 0.001b |
| Cerebrovascular disease, n (%) | 12,443 (3.9) | 5,293 (3.8) | 4,125 (3.8) | 3,025 (4.0) | 0.16b |
| Diabetes with complications, n (%) | 26,063 (8.1) | 9,921 (7.2) | 8,991 (8.4) | 7,151 (9.4) | < 0.001b |
ANOVA test.
χ2 test.
CCI, Charlson Comorbidity Index.
The association of program characteristics with engagement is shown in Table 2. Participants in programs seeing fewer patients per year or enrolling fewer new patients per year had more visits in their first year (P = −0.04; P < 0.001 for both). In addition, participants attending programs that offered weight loss medications or bariatric surgery were more likely to have six or more visits in their first year. Participants in programs with more hours per week of staff support also tended to have better engagement in their program as well (Table 2).
Table 2.
Program volume, offerings, and staff support of MOVE! programs at VHA medical centers by participant engagement (N = 321,624)
| Overall | MOVE! visits in the first year of program participation | ||||
|---|---|---|---|---|---|
| 1 | 2‐5 | 6 or more | P value | ||
| Number of participants | 321,624 | 138,013 (42.9%) | 107,724 (33.5%) | 75,887 (23.6%) | … |
| Patients seen each year, median (IQR) | 1,012 (592‐1,699) | 1,095 (598‐1,854) | 951 (580‐1,589) | 975 (598‐1,500) | < 0.001a |
| New patients seen each year, median (IQR) | 746 (455‐1,223) | 790 (481‐1,378) | 686 (440‐1,182) | 738 (440‐1,132) | < 0.001a |
| Program offerings, n (%) | |||||
| Intensive medical treatment | 69,787 (21.8) | 30,418 (22.1) | 22,619 (21.1) | 16,750 (22.2) | < 0.001b |
| Weight loss medications | 245,777 (76.4) | 103,852 (75.3) | 82,304 (76.4) | 59,621 (78.6) | < 0.001b |
| Bariatric surgery | 154,481 (48.2) | 67,800 (49.2) | 48,926 (45.6) | 37,755 (49.9) | < 0.001b |
| Staff support, median (IQR), h/wk c | |||||
| Administrative | 10.0 (4.0‐20.0) | 8.0 (4.0‐20.0) | 10.0 (4.0‐20.0) | 10.0 (4.0‐24.0) | < 0.001a |
| Primary care | 6.0 (0.5‐25.3) | 6.0 (0.5‐25.3) | 6.0 (0.5‐26.0) | 6.0 (0.5‐25.3) | < 0.001a |
| Behavioral health | 4.0 (1.3‐10.0) | 3.5 (1.0‐10.0) | 3.7 (1.2‐10.0) | 4.5 (1.5‐12.0) | < 0.001a |
| Dietitian | 34.0 (19.0‐65.0) | 34.0 (20.0‐65.0) | 32.0 (18.0‐64.0) | 35.0 (20.0‐65.5) | < 0.001a |
| Physical activity | 2.0 (0.5‐9.0) | 2.0 (0.5‐9.0) | 2.0 (0.5‐9.0) | 2.0 (0.6‐9.0) | < 0.001a |
Kruskal‐Wallis one‐way ANOVA.
χ2 test.
Staff support defined as number of hours worked per week on MOVE! program–related tasks.
IQR, interquartile range.
County characteristics
The association of county characteristics with participant engagement is shown in Table 3. The median county population size in 2008 was 349,778 (interquartile range = 110,491‐910,058), with an average of 9.1 recreational facilities per 10,000 population. Full‐service restaurants were the most prevalent food establishment, with an average of 72.7 restaurants per 10,000 population, followed by fast food restaurants at 70.5 per 10,000 population. There was also a wide range of natural amenities across the study area, with 41.6% of participants in areas with moderate to low access to natural amenities, 28.0% of participants in areas with average access to natural amenities, and 30.4% of participants in areas with moderately high to high access to natural amenities.
Table 3.
Community characteristics associated with participant engagement (N = 321,624)
| Overall | MOVE! visits in the first year of program participation | P value | |||
|---|---|---|---|---|---|
| 1 | 2‐5 | 6 or more | |||
| Number of participants | 321,624 | 138,013 (42.9%) | 107,724 (33.5%) | 75,887 (23.6%) | … |
| County population (2008), median (IQR) | 349,778 (110,491‐910,058) | 405,660 (125,081‐1,009,832) | 325,166 (106,398‐894,401) | 299,489 (98,385‐868,068) | < 0.001a |
| Recreational facilities, per 10,000 population, median (IQR) | 8.7 (6.7‐11.6) | 8.6 (6.5‐11.5) | 8.8 (6.7‐11.7) | 8.8 (6.7‐11.6) | < 0.001a |
| Community food outlets, per 10,000 population, median (IQR) | |||||
| Grocery stores | 17.7 (13.9‐22.1) | 17.9 (14.0‐22.4) | 17.6 (13.6‐22.0) | 17.3 (13.5‐21.6) | < 0.001a |
| Supercenters | 1.7 (1.1‐2.4) | 1.7 (1.1‐2.3) | 1.7 (1.1‐2.4) | 1.7 (1.1‐2.4) | < 0.001a |
| Convenience stores | 37.8 (30.6‐48.7) | 37.5 (29.6‐47.4) | 38.4 (31.2‐48.8) | 38.7 (31.6‐49.6) | < 0.001a |
| Specialty‐food stores | 6.1 (4.4‐8.1) | 6.2 (4.6‐8.1) | 6.1 (4.3‐8.1) | 6.1 (4.3‐8.1) | < 0.001a |
| Fast food restaurants | 70.7 (61.8‐80.5) | 70.5 (62.1‐80.2) | 70.7 (62.3‐80.9) | 70.6 (61.3‐81.3) | < 0.001a |
| Full‐service restaurants | 69.8 (58.1‐81.7) | 69.8 (57.6‐81.7) | 69.6 (58.6‐81.8) | 69.6 (57.6‐81.4) | < 0.001a |
| Farmers’ markets | 1.8 (1.0‐3.1) | 1.8 (1.0‐3.0) | 1.8 (1.1‐3.2) | 2.0 (1.1‐3.3) | < 0.001a |
| Environmental factors | |||||
| Natural amenities ranking, n (%) c | < 0.001b | ||||
| Few | 639 (0.2) | 169 (0.1) | 228 (0.2) | 242 (0.3) | … |
| Moderately few | 131,321 (41.4) | 53,190 (39.0) | 45,546 (43.0) | 32,585 (43.3) | … |
| Average | 88,984 (28.0) | 38,642 (28.4) | 30,212 (28.5) | 20,130 (26.8) | … |
| Moderately high | 78,801 (24.8) | 36,243 (26.6) | 24,314 (23.0) | 18,244 (24.3) | … |
| Many | 17,601 (5.6) | 8,005 (5.9) | 5,618 (5.3) | 3,978 (5.3) | … |
| January temperature, °F, median (IQR) c | 2.3 (−2.7‐9.2) | 3.0 (−2.2‐10.3) | 2.3 (−2.8‐8.5) | 1.4 (−3‐8.4) | < 0.001a |
| January hours of sunlight, median (IQR) c | 152.0 (130.0‐184.0) | 153.0 (130.0‐186.0) | 151.0 (129.0‐181.0) | 153.0 (130.0‐185.0) | < 0.001a |
| July temperature, °F, median (IQR) c | 24.7 (22.2‐27.4) | 24.9 (22.2‐27.6) | 24.7 (22.2‐27.3) | 24.5 (22.2‐27.3) | < 0.001a |
| July humidity, %, median (IQR) c | 61.0 (51.0‐68.0) | 62.0 (50.0‐68.0) | 61.0 (51.0‐68.0) | 61.0 (55.0‐68.0) | < 0.001a |
| Proportion of county that is water, %, median (IQR) c | 2.8 (0.8‐12.1) | 2.8 (0.9‐12.2) | 2.7 (0.8‐10.6) | 2.5 (0.8‐12.2) | < 0.001a |
| Topography, n (%) c | < 0.001b | ||||
| Hills and mountains | 107,354 (33.8) | 46,603 (34.2) | 36,933 (34.9) | 23,818 (31.7) | … |
| Plains | 155,896 (49.1) | 65,989 (48.4) | 51,660 (48.8) | 38,247 (50.9) | … |
| Plains with hills | 27,573 (8.7) | 11,677 (8.6) | 8,905 (8.4) | 6,991 (9.3) | … |
| Tablelands | 26,523 (8.4) | 11,980 (8.8) | 8,420 (8.0) | 6,123 (8.1) | … |
| Daily fine‐particulate matter, µg/m3, median (IQR) | 11.1 (9.9‐12.4) | 11.0 (9.8‐12.3) | 11.2 (9.9‐12.4) | 11.2 (9.8‐12.4) | < 0.001a |
Kruskal‐Wallis one‐way ANOVA.
χ2 test.
As reported from US Department of Agriculture’s natural amenities scale, which ranks county’s natural amenities based on six measures: topographic variation, percentage of water area, average summer and winter temperatures, summer humidity, and average winter days with sun. Resulting index is sum of six measures after standardization to zero. Higher values represent more attractive amenities 22 .
IQR, interquartile range.
Although differences were small, there were several county characteristics notably associated with higher participant engagement in bivariate analyses. Larger numbers of recreational facilities (P = 0.02; P < 0.001) and farmers’ markets (P = 0.03; P < 0.001) were associated with higher participant engagement. In contrast, larger numbers of grocery stores (P = −0.01; P < 0.001) and the most natural amenities (P = −0.03; P < 0.001) were associated with lower participant engagement (Table 3).
Generalized linear regression identified greater engagement among participants living in counties with more recreational facilities, fast food restaurants, or farmers’ markets and fewer convenience stores and full‐service restaurants. However, there was strong evidence for spatial dependence across this nationwide sample (Moran’s I = 0.21; P < 0.001), necessitating the use of spatial regression. In the final spatial regression model, accounting for this dependence, only a greater density of farmers’ markets, fewer full‐service restaurants, and the most natural amenities were associated with greater engagement in the MOVE! weight management program (Table 4).
Table 4.
Factors associated with number of MOVE! visits per person 12 months after program enrollment (N = 321,624)
| Generalized linear regression with generalized estimating equations | Spatial regression | |||
|---|---|---|---|---|
| β (95% CI) | P | β (95% CI) | P | |
| Community characteristics | ||||
| Recreational facilities, per 1,000 population | 0.01 (0.00 to 0.03) | 0.04 | 0.02 (0.01 to 0.04) | 0.002 |
| Grocery stores, per 1,000 population | 0.00 (0.00 to 0.00) | 0.99 | 0.00 (−0.01 to 0.00) | 0.23 |
| Supercenters, per 1,000 population | 2.34 (−0.24 to 4.92) | 0.08 | 3.63 (−3.56 to 10.82) | 0.24 |
| Convenience stores, per 1,000 population | −0.02 (−0.04 to −0.01) | 0.002 | −0.02 (−0.05 to 0.01) | 0.12 |
| Specialty‐food stores, per 1,000 population | −0.06 (−0.89 to 0.77) | 0.89 | 0.56 (−0.67 to 1.78) | 0.27 |
| Fast food restaurants, per 1,000 population | 0.25 (0.03 to 0.46) | 0.02 | 0.43 (−0.06 to 0.91) | 0.09 |
| Full‐service restaurants, per 1,000 population | −0.26 (−0.39 to −0.14) | < 0.001 | −0.35 (−0.60 to −0.09) | 0.01 |
| Farmers’ markets, per 1,000 population | 2.38 (1.42 to 3.34) | < 0.001 | 3.08 (0.92 to 5.23) | 0.01 |
| Natural amenities index | ||||
| High | Reference | … | Reference | … |
| Moderately high | −0.25 (−0.41 to −0.09) | 0.003 | −0.59 (−0.93 to −0.26) | < 0.001 |
| Average | −0.14 (−0.30 to 0.02) | 0.09 | −0.76 (−1.03 to −0.49) | < 0.001 |
| Moderately low | 0.14 (−0.01 to 0.30) | 0.07 | −0.66 (−0.99 to −0.34) | < 0.001 |
| Low | 1.40 (0.86 to 1.94) | < 0.001 | 1.25 (−0.25 to 2.75) | 0.11 |
| Additional covariates | ||||
| Patient characteristics at baseline | ||||
| Age, per 1 year | 0.04 (0.04 to 0.05) | < 0.001 | 0.04 (0.04 to 0.05) | < 0.001 |
| Sex | ||||
| Male | Reference | … | Reference | … |
| Female | 0.66 (0.60 to 0.72) | < 0.001 | 0.67 (0.53 to 0.81) | < 0.001 |
| BMI, per 1 unit | 0.07 (0.07 to 0.07) | < 0.001 | 0.07 (0.06 to 0.08) | < 0.001 |
| CCI, per 1 point | −0.01 (−0.02 to 0.01) | 0.41 | 0.01 (−0.04 to 0.05) | 0.38 |
| Race | ||||
| White | Reference | … | Reference | … |
| Black | −0.14 (−0.19 to −0.10) | < 0.001 | −0.26 (−0.39 to −0.12) | < 0.001 |
| Other | −0.18 (−0.29 to −0.06) | 0.002 | −0.07 (−0.41 to 0.27) | 0.37 |
| Marital status | ||||
| Married | Reference | … | Reference | … |
| Single | 0.01 (−0.05 to 0.07) | 0.67 | 0.00 (−0.19 to 0.19) | 0.40 |
| Other | −0.22 (−0.26 to −0.18) | < 0.001 | −0.22 (−0.32 to −0.12) | < 0.001 |
| Employment status | ||||
| Employed | Reference | … | Reference | … |
| Retired | 0.23 (0.19 to 0.27) | < 0.001 | 0.20 (0.08 to 0.32) | 0.001 |
| Not employed | 0.20 (0.15 to 0.24) | < 0.001 | 0.20 (0.15 to 0.24) | < 0.001 |
| Rurality | ||||
| Rural | Reference | … | Reference | … |
| Urban | −0.03 (−0.08 to 0.03) | 0.37 | −0.12 (−0.28 to 0.04) | 0.14 |
| Distance to outpatient center, per 10 miles | −0.01 (−0.01 to 0.00) | 0.01 | −0.01 (−0.01 to 0.00) | 0.03 |
| Program characteristics | ||||
| Offers weight loss medications | 0.16 (0.10 to 0.21) | < 0.001 | 0.18 (0.06 to 0.29) | 0.004 |
| Offers bariatric surgery | 0.06 (0.01 to 0.11) | 0.02 | 0.06 (−0.04 to 0.15) | 0.21 |
| Hours per week of staff support | ||||
| Administrative, per 8 hours | 0.09 (0.08 to 0.10) | < 0.001 | 0.10 (0.07 to 0.13) | < 0.001 |
| Primary care, per 8 hours | 0.01 (0.00 to 0.01) | 0.04 | 0.00 (−0.02 to 0.02) | 0.37 |
| Behavioral health, per 8 hours | 0.18 (0.15 to 0.20) | < 0.001 | 0.24 (0.18 to 0.29) | < 0.001 |
| Dietetics, per 8 hours | 0.04 (0.03 to 0.04) | < 0.001 | 0.01 (0.00 to 0.03) | 0.04 |
| Physical activity, per 8 hours | −0.06 (−0.08 to −0.05) | < 0.001 | −0.04 (−0.07 to −0.01) | 0.02 |
CCI, Charlson Comorbidity Index.
Participant engagement at 12 months was 3.1 visits higher for each additional farmers’ market per 1,000 population (P = 0.01). In addition, participant engagement was 0.59 to 0.76 visits lower for participants with access to moderately high or average natural amenities compared with participants with access to the most natural amenities on the natural amenities index (P < 0.001). The addition of 1 full‐service restaurant per 1,000 population in a county resulted in an overall decrease of 0.35 visits at 12 months (P = 0.01), and, although statistically significant, participant engagement at 12 months only improved by 0.02 visits for every additional recreational facility per 1,000 population (P = 0.002).
Discussion
This study examined the association of food access, recreational opportunities, and natural amenities at the county‐level with participant engagement in the nation’s largest population‐based weight management program, MOVE!. Consistent with prior research, we found that older age, higher baseline BMI, white race, female sex, and married or retired status are important participant‐level predictors of greater engagement in the program 6, 18. Adding to the current literature, we found that participants in communities with a higher density of farmers’ markets and the most natural resources had more visits to the MOVE! program in their first year, even after taking into account significant spatial dependence.
Identifying community characteristics associated with engagement in weight management programs offers two opportunities to intervene in the obesity epidemic. First, it provides a better understanding of how existing interventions could be better tailored to specific community characteristics. In light of our findings, program coordinators could identify nearby farmers’ markets or natural resources to highlight in their educational group meetings or individual counseling sessions. Second, a better understanding of community characteristics can provide support for policy initiatives geared toward infrastructure improvements that support these lifestyle interventions 27. Our findings support policy initiatives that provide support to developing and improving access to local farmers’ markets and natural resources such as public parks.
The nationwide MOVE! program offers the ideal opportunity to study how aspects of a community affect weight management program participants. It is offered free to veterans, mitigating some barriers to access, such as cost. It also includes annual reminders for veterans who receive their primary care at the VA, thus mitigating several other barriers related to recruitment and engagement. Nonetheless, engagement in MOVE! is still a challenge. In our analyses, we identified a greater density of farmers’ markets and more natural resources as important predictors of greater participant engagement in the MOVE! program.
Our study is one of only a few studies to date examining community characteristics in addition to participant and program characteristics. Recently, the Weight and Veterans Environment Study (WAVES), which also examines MOVE!, reported results on the effect of community characteristics on enrollment in MOVE! but not engagement 28. Although WAVES was limited to metropolitan communities and only examined a few county‐level characteristics (supermarkets, convenience stores, fast food restaurants, fitness facilities, and park area in acres) the authors found that the impact of these select characteristics on MOVE! enrollment was relatively small. Our findings were similar for MOVE! engagement for all factors apart from recreational facilities. The WAVES study found that greater access to fitness facilities resulted in a much greater increase in MOVE! enrollment in contrast to the minute increase in engagement of 0.02 visits at 12 months that we found. However, the WAVES study used a different definition, accessing only commercial fitness centers within a 1‐mile radius 28.
An important strength of our study is its use of spatial regression to account for spatial dependence. Prior research is flawed by the exclusion of this important consideration. Apparent community‐level effects may be due to analyses that do not take into account the significant spatial dependence that occurs when examining community‐level effects 29. In sensitivity analyses, we identified several county‐level characteristics using generalized linear regression that were associated with engagement, including the density of grocery stores and fast food restaurants. After using spatial regression to account for spatial dependence, only the density of farmers’ markets and the availability of natural amenities remained associated with MOVE! engagement.
Farmers’ markets in the United States have been on a steady rise, increasing by 76% from 2008 to 2014 30. There is very little research on the role of farmers’ markets in health behaviors, weight management, and program engagement, but Jilcott et al. 11 found that an increased the density of farmers’ markets in nonmetropolitan counties was associated with a reduction in county‐level obesity rates. Farmers’ markets may be the only source of fresh food in some communities, particularly those of low income 31. For MOVE! participants, having better access to a farmers’ market may be instrumental in encouraging participants to continue to engage in the program because many group sessions in MOVE! are geared toward a healthy diet. Alternatively, the density of farmers’ markets may be a marker of healthier communities with environments supportive of weight management.
Our findings have some interesting implications for dissemination and implementation research in weight management programs moving forward. The MOVE! program is a highly successful evidence‐based intervention that has been adopted nationwide by the VA. Many studies are currently underway to further improve its delivery and effectiveness in our veteran population. Our findings suggest that new studies should consider the availability of fresh and healthy food options to participants along with access to natural resources such as topography, temperature, humidity, and sunlight hours. Future dissemination research should examine these factors in more detail to better understand their contributions to weight management program participation and engagement.
This study is unique in its assessment of 126 programs distributed nationwide, but it is also limited in generalizability to characteristics of the veteran population. The veteran population is majority male, and thus these results may not be generalizable to women or nonveterans. In prior research on weight management programs, women were more likely than men to participate 32, 33. We have attempted to control for these differences by adjusting for sex in our analyses; however, the small number of women limited our ability to examine sex effects. It is also important to note that our results represent the experiences of veterans who opt to participate in the MOVE! program. Only 5% to 10% of eligible veterans opt to participate in the MOVE! program 7. Prior studies have shown that these patients are more likely to be women, unmarried, and younger and are more likely to have a higher baseline BMI 19, 32, 33.
It is also important to keep in mind that the program characteristics are self‐reported and subject to inaccuracies in reporting. Also, community characteristics in our analyses are linked to the participant’s county of residence and may not represent the actual community environment of the participant. A common limitation of many spatial analyses is the modifiable area unit problem, in which bias arises from aggregation of spatial data 34. Although we have done our best to address issues of spatial dependence, the areal units in our study defined by county code could potentially be reaggregated at different units, such as census tracts or zip code levels, and lead to different results. As with all spatial analyses, interpretation of our spatial model results should take this limitation into consideration.
Finally, it is important to consider the role that socioeconomic status plays in our findings. We attempted to control for some aspects of socioeconomic status, such as employment, but this certainly falls short of describing the true socioeconomic status of the participant. Some community characteristics examined in this manuscript may be socially patterned and thus a proxy for certain levels of socioeconomic status. This is particularly true for farmer’s markets and could potentially explain some of our findings.
Conclusion
Community characteristics differentially affected engagement in weight management programs such that participant engagement was higher in communities with farmers’ markets and the most natural amenities. Our results indicate that plans to optimize participant engagement in weight management programs may consider community characteristics in addition to other known demographics and program factors.
Funding agencies: This study was funded by the American Heart Association (grant 16MCPRP2967).
Disclosure: EBL receives research funding from Amgen unrelated to this work, has served on Amgen advisory boards, and has served as a consultant for a Novartis‐funded research project. APC receives research funding from Amgen unrelated to this work. The other authors declared no conflict of interest.
References
- 1. Kinsinger LS, Jones KR, Kahwati L, et al. Design and dissemination of the MOVE! weight‐management program for veterans. Prev Chronic Dis 2009;6:A98 http://www.cdc.gov/pcd/issues/2009/jul/08_0150.htm [PMC free article] [PubMed] [Google Scholar]
- 2. Byrne NM, Meerkin JD, Laukkanen R, Ross R, Fogelholm M, Hills AP. Weight loss strategies for obese adults: personalized weight management program vs. standard care. Obesity (Silver Spring) 2006;14:1777‐1788. [DOI] [PubMed] [Google Scholar]
- 3. Graffagnino CL, Falko JM, La Londe M, et al. Effect of a community‐based weight management program on weight loss and cardiovascular disease risk factors. Obesity (Silver Spring) 2006;14:280‐288. [DOI] [PubMed] [Google Scholar]
- 4. Honas JJ, Early JL, Frederickson DD, O’Brien MS. Predictors of attrition in a large clinic‐based weight‐loss program. Obes Res 2003;11:888‐894. [DOI] [PubMed] [Google Scholar]
- 5. Funderburk JS, Arigo D, Kenneson A. Initial engagement and attrition in a national weight management program: demographic and health predictors. Transl Behav Med 2016;6:358‐368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Spring B, Sohn MW, Locatelli SM, Hadi S, Kahwati L, Weaver FM. Individual, facility, and program factors affecting retention in a national weight management program. BMC Public Health 2014;14:363. doi: 10.1186/1471-2458-14-363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Del Re AC, Maciejewski ML, Harris AH. MOVE: weight management program across the Veterans Health Administration: patient‐ and facility‐level predictors of utilization. BMC Health Serv Res 2013;13:511. doi: 10.1186/1472-6963-13-511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chan SH, Raffa SD. Examining the dose‐response relationship in the Veterans Health Administration’s MOVE!® weight management program: A nationwide observational study. J Gen Intern Med 2017;32(suppl 1):18‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jackson SL, Long Q, Rhee MK, et al. Weight loss and incidence of diabetes with the Veterans Health Administration MOVE! lifestyle change programme: an observational study. Lancet Diabetes Endocrinol 2015;3:173‐180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jackson SL, Safo S, Staimez LR, et al. Reduced cardiovascular disease incidence with a national lifestyle change program. Am J Prev Med 2017;52:459‐468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jilcott SB, Keyserling T, Crawford T, McGuirt JT, Ammerman AS. Examining associations among obesity and per capita farmers’ markets, grocery stores/supermarkets, and supercenters in US counties. J Am Diet Assoc 2011;111:567‐572. [DOI] [PubMed] [Google Scholar]
- 12. Jilcott Pitts SB, Edwards MB, Moore JB, Shores KA, DuBose KD, McGranahan D. Obesity is inversely associated with natural amenities and recreation facilities per capita. J Phys Act Health 2013;10:1032‐1038. [DOI] [PubMed] [Google Scholar]
- 13. Slack T, Myers CA, Martin CK, Heymsfield SB. The geographic concentration of US adult obesity prevalence and associated social, economic, and environmental factors. Obesity (Silver Spring) 2014;22:868‐874. [DOI] [PubMed] [Google Scholar]
- 14. Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription opioid analgesics commonly unused after surgery: a systematic review. JAMA Surg 2017;152:1066‐1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Armstrong B, Lim CS, Janicke DM. Park density impacts weight change in a behavioral intervention for overweight rural youth. Behav Med 2015;41:123‐130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Albert PS, McShane LM. A generalized estimating equations approach for spatially correlated binary data: applications to the analysis of neuroimaging data. Biometrics 1995;51:627‐638. [PubMed] [Google Scholar]
- 17. US Department of Veterans Affairs . MOVE! weight management program. https://www.move.va.gov/. Updated September 11, 2019. Accessed June 17, 2019.
- 18. Maciejewski ML, Shepherd‐Banigan M, Raffa SD, Weidenbacher HJ. Systematic review of behavioral weight management program MOVE! for veterans. Am J Prev Med 2018;54:704‐714. [DOI] [PubMed] [Google Scholar]
- 19. Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index . J Clin Epidemiol 1994;47:1245‐1251. [DOI] [PubMed] [Google Scholar]
- 20. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373‐383. [DOI] [PubMed] [Google Scholar]
- 21. Rivers EP. Point: adherence to early goal‐directed therapy: does it really matter? Yes. After a decade, the scientific proof speaks for itself. Chest 2010;138:476‐480; discussion 484‐485. [DOI] [PubMed] [Google Scholar]
- 22. McGranahan DA. Natural amenities drive rural population change. Agricultural Economic Report no. 781. Washington, DC: US Economic Research Service; 1999. [Google Scholar]
- 23. Cressie N. Statistics for spatial data. Terra Nova 1992;4:613‐617. [Google Scholar]
- 24. Ullah A, Giles DEA, eds. Handbook of Applied Economic Statistics. New York, NY: Marcel Dekker; 1998. [Google Scholar]
- 25. Hill AB. The environment and disease: association or causation? Proc R Soc Med 1965;58:295‐300. [PMC free article] [PubMed] [Google Scholar]
- 26. Bivand R, Hauke J, Kossowski T. Computing the Jacobian in Gaussian spatial autoregressive models: an illustrated comparison of available methods. Geogr Anal 2013;45:150‐179. [Google Scholar]
- 27. Lyn R, Aytur S, Davis TA, et al. Policy, systems, and environmental approaches for obesity prevention: a framework to inform local and state action. J Public Health Manag Pract 2013;19(3 suppl 1):S23‐S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zenk SN, Tarlov E, Powell LM, et al. Weight and Veterans’ Environments Study (WAVES) I and II: rationale, methods, and cohort characteristics. Am J Health Promot 2018;32:779‐794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Arcaya MC, Tucker‐Seeley RD, Kim R, Schnake‐Mahl A, So M, Subramanian SV. Research on neighborhood effects on health in the United States: a systematic review of study characteristics. Soc Sci Med 2016;168:16‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. US Department of Agriculture . New data reflects the continued demand for farmers markets. https://www.usda.gov/media/press-releases/2014/08/04/new-data-reflects-continued-demand-farmers-markets. Published August 4, 2014.
- 31. Young C, Karpyn A, Uy N, Wich K, Glyn J. Farmers’ markets in low income communities: impact of community environment, food programs and public policy . Community Dev (Columb) 2011;42:208‐220. [Google Scholar]
- 32. Robertson C, Avenell A, Boachie C, et al. Should weight loss and maintenance programmes be designed differently for men? A systematic review of long‐term randomised controlled trials presenting data for men and women: the ROMEO project. Obes Res Clin Pract 2016;10:70‐84. [DOI] [PubMed] [Google Scholar]
- 33. Ahlgren C, Hammarström A, Sandberg S, et al. Engagement in new dietary habits‐obese women’s experiences from participating in a 2‐year diet intervention. Int J Behav Med 2016;23:84‐93. [DOI] [PubMed] [Google Scholar]
- 34. Duncan DT, Kawachi I, Subramanian SV, Aldstadt J, Melly SJ, Williams DR. Examination of how neighborhood definition influences measurements of youths’ access to tobacco retailers: a methodological note on spatial misclassification. Am J Epidemiol 2014;179:373‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]


