Abstract
Improvements in sensor accuracy, greater convenience and ease of use, and expanding reimbursement have led to growing adoption of continuous glucose monitoring (CGM). However, successful utilization of CGM technology in routine clinical practice remains relatively low. This may be due in part to the lack of clear and agreed-upon glycemic targets that both diabetes teams and people with diabetes can work toward. Although unified recommendations for use of key CGM metrics have been established in three separate peer-reviewed articles, formal adoption by diabetes professional organizations and guidance in the practical application of these metrics in clinical practice have been lacking. In February 2019, the Advanced Technologies & Treatments for Diabetes (ATTD) Congress convened an international panel of physicians, researchers, and individuals with diabetes who are expert in CGM technologies to address this issue. This article summarizes the ATTD consensus recommendations for relevant aspects of CGM data utilization and reporting among the various diabetes populations.
Adoption of continuous glucose monitoring (CGM), which includes both real-time CGM (rtCGM) and intermittently scanned CGM (isCGM), has grown rapidly over the past few years as a result of improvements in sensor accuracy, greater convenience and ease of use, and expanding reimbursement. Numerous studies have demonstrated significant clinical benefits of CGM use in people with diabetes regardless of insulin delivery method (1–15). In many countries, the benefits and utility of CGM are now recognized by national and international medical organizations for individuals with insulin-requiring diabetes and/or those at risk for hypoglycemia (16–21). However, despite increased CGM adoption (22,23), successful utilization of CGM data in routine clinical practice remains relatively low. This may be due in part to the lack of clear and agreed-upon glycemic targets toward which both diabetes teams and people with diabetes can work.
In 2012 the Helmsley Charitable Trust sponsored the first expert panel to recommend the standardization of CGM metrics and CGM report visualization (24). This was followed by a series of CGM consensus statements refining the core CGM metrics, but the conclusions were never in alignment. In 2017, several articles supported use of systematic approaches to CGM data evaluation (18–20). To date, the key CGM metrics remain as unified recommendations in three separate peer-reviewed articles, yet formal adoption by diabetes professional organizations and guidance in the practical application of these metrics in clinical practice have been lacking (19).
In February 2019, the Advanced Technologies & Treatments for Diabetes (ATTD) Congress convened an international panel of individuals with diabetes and clinicians and researchers with expertise in CGM. Our objective was to develop clinical CGM targets to supplement the currently agreed-upon metrics for CGM-derived times in glucose ranges (within target range, below target range, above target range) in order to provide guidance for clinicians, researchers, and individuals with diabetes in using, interpreting, and reporting CGM data in routine clinical care and research. Importantly, in order to make the recommendations generalizable and comprehensive, the consensus panel included individuals living with diabetes and had international representation from physicians and researchers from all geographic regions.
The panel was divided into subgroups to review literature and provide recommendations for relevant aspects of CGM data utilization and reporting among the various diabetes populations. Long-term trials demonstrating how CGM metrics relate to and/or predict clinical outcomes have not been conducted, and many of the published reports assessed here are not at the highest evidence level (25). However, there is suggestive evidence from a number of recent studies, including a cross-sectional study correlating current retrospective 3-day time in target range with varying degrees of diabetes retinopathy (26) and an analysis of the 7-point self-monitored blood glucose (SMBG) data from the Diabetes Control and Complications Trial (DCCT) (27), showing correlations of time in target range (70–180 mg/dL [3.9–10.0 mmol/L]) with diabetes complications. Relationships between time in target range and A1C (26,27) and number of severe and nonsevere hypoglycemic events (28–32) have also been observed. Recommendations from each subgroup were presented to the full panel and voted upon. This article summarizes the consensus recommendations and represents the panel members’ evaluation of the issues.
Need for Metrics Beyond A1C
A1C is currently recognized as the key surrogate marker for the development of long-term diabetes complications in people with type 1 and type 2 diabetes and has been used as the primary end point for many CGM studies (1,3,4,6,33,34). While A1C reflects average glucose over the last 2–3 months, its limitation is the lack of information about acute glycemic excursions and the acute complications of hypo- and hyperglycemia. A1C also fails to identify the magnitude and frequency of intra- and interday glucose variation (35,36). Moreover, certain conditions such as anemia (37), hemoglobinopathies (38), iron deficiency (39), and pregnancy (40) can confound A1C measurements. Importantly, as reported by Beck et al. (41), the A1C test can fail at times to accurately reflect mean glucose even when none of those conditions are present. Despite these limitations, A1C is the only prospectively evaluated tool for assessing the risk for diabetes complications, and its importance in clinical decision making should not be undervalued. Rather, the utility of A1C is further enhanced when used as a complement to glycemic data measured by CGM.
Unlike A1C measurement, use of CGM allows for the direct observation of glycemic excursions and daily profiles, which can inform on immediate therapy decisions and/or lifestyle modifications. CGM also provides the ability to assess glucose variability and identify patterns of hypo- and hyperglycemia. However, potential drawbacks of CGM use include the need to be actively used in order to be effective; that it may induce anxiety; that it may have accuracy limitations, particularly with the delay in registering blood glucose changes in dynamic situations; and that it can provoke allergies. Another limitation of CGM is that this technology is not yet widely available in several regions of the world.
Effective use of CGM data to optimize clinical outcomes requires the user to interpret the collected data and act upon them appropriately. This requires 1) common metrics for assessment of CGM glycemic status, 2) graphical visualization of the glucose data and CGM daily profile, and 3) clear clinical targets.
Standardization of CGM Metrics
In February 2017, the ATTD Congress convened an international panel of expert clinicians and researchers to define core metrics for assessing CGM data (18) (Table 1).
Table 1.
Standardized CGM metrics
| 2017 international consensus on CGM metrics (18) |
|---|
| 1. Number of days CGM worn |
| 2. Percentage of time CGM is active |
| 3. Mean glucose |
| 4. Estimated A1C |
| 5. Glycemic variability (%CV or SD) |
| 6. Time >250 mg/dL (>13.9 mmol/L) |
| 7. Time >180 mg/dL (>10.0 mmol/L) |
| 8. Time 70–180 mg/dL (3.9–10.0 mmol/L) |
| 9. Time <70 mg/dL (<3.9 mmol/L) |
| 10. Time <54 mg/dL (<3.0 mmol/L) |
| 11. LBGI and HBGI (risk indices) |
| 12. Episodes (hypoglycemia and hyperglycemia) 15 min |
| 13. Area under the curve |
| 14. Time blocks (24-h, day, night) |
| Use of Ambulatory Glucose Profile (AGP) for CGM report |
CV, coefficient of variation; LBGI, low blood glucose index; HBGI, high blood glucose index.
The list of core CGM metrics has now been streamlined for use in clinical practice based on the expert opinion of this international consensus group (18). Of the 14 core metrics, the panel selected that 10 metrics that may be most useful in clinical practice (Table 2).
Table 2.
Standardized CGM metrics for clinical care: 2019
| 1. Number of days CGM worn (recommend 14 days) (42,43) | |
| 2. Percentage of time CGM is active (recommend 70% of data from 14 days) (41,42) | |
| 3. Mean glucose | |
| 4. Glucose management indicator (GMI) (75) | |
| 5. Glycemic variability (%CV) target ≤36% (90)* | |
| 6. Time above range (TAR): % of readings and time >250 mg/dL (>13.9 mmol/L) | Level 2 |
| 7. Time above range (TAR): % of readings and time 181–250 mg/dL (10.1–13.9 mmol/L) | Level 1 |
| 8. Time in range (TIR): % of readings and time 70–180 mg/dL (3.9–10.0 mmol/L) | In range |
| 9. Time below range (TBR): % of readings and time 54–69 mg/dL (3.0–3.8 mmol/L) | Level 1 |
| 10. Time below range (TBR): % of readings and time <54 mg/dL (<3.0 mmol/L) | Level 2 |
|
Use of Ambulatory Glucose Profile (AGP) for CGM report | |
Fundamental to accurate and meaningful interpretation of CGM is ensuring that adequate glucose data are available for evaluation. As shown in studies, >70% use of CGM over the most recent 14 days correlates strongly with 3 months of mean glucose, time in ranges, and hyperglycemia metrics (42,43). In individuals with type 1 diabetes, correlations are weaker for hypoglycemia and glycemic variability; however, these correlations have not been shown to increase with longer sampling periods (43). Longer CGM data collection periods may be required for individuals with more variable glycemic control (e.g., 4 weeks of data to investigate hypoglycemia exposure).
Time in Ranges
The development of blood glucose testing provided individuals with diabetes the ability to obtain immediate information about their current glucose levels and adjust their therapy accordingly. Over the past decades, national and international medical organizations have been successful in developing, harmonizing, and disseminating standardized glycemic targets based on risk for acute and chronic complications. CGM technology greatly expands the ability to assess glycemic control throughout the day, presenting critical data to inform daily treatment decisions and quantifying time below, within, and above the established glycemic targets.
Although each of the core metrics established in the 2017 ATTD consensus conference (18) provides important information about various aspects of glycemic status, it is often impractical to assess and fully utilize many of these metrics in real-world clinical practices. To streamline data interpretation, the consensus panel identified “time in ranges” as a metric of glycemic control that provides more actionable information than A1C alone. The panel agreed that establishing target percentages of time in the various glycemic ranges with the ability to adjust the percentage cut points to address the specific needs of special diabetes populations (e.g., pregnancy, high-risk) would facilitate safe and effective therapeutic decision making within the parameters of the established glycemic goals.
The metric includes three key CGM measurements: percentage of readings and time per day within target glucose range (TIR), time below target glucose range (TBR), and time above target glucose range (TAR) (Table 3). The primary goal for effective and safe glucose control is to increase the TIR while reducing the TBR. The consensus group agreed that expressing time in the various ranges can be done as the percentage (%) of CGM readings, average hours and minutes spent in each range per day, or both, depending on the circumstances.
Table 3.
Guidance on targets for assessment of glycemic control for adults with type 1 or type 2 diabetes and older/high-risk individuals
| Diabetes group | TIR |
TBR |
TAR |
|||
|---|---|---|---|---|---|---|
| % of readings; time per day | Target range | % of readings; time per day | Below target level | % of readings; time per day | Above target level | |
| Type 1*/type 2 | >70%; >16 h, 48 min | 70–180 mg/dL (3.9–10.0 mmol/L) | <4%; <1 h | <70 mg/dL (<3.9 mmol/L) | <25%; <6 h | >180 mg/dL (>10.0 mmol/L) |
| <1%; <15 min | <54 mg/dL (<3.0 mmol/L) | <5%; <1 h, 12 min | >250 mg/dL (>13.9 mmol/L) | |||
| Older/high-risk# type 1/type 2 | >50%; >12 h | 70–180 mg/dL (3.9–10 mmol/L) | <1%; <15 min | <70 mg/dL (<3.9 mmol/L) | <10%; <2 h, 24 min | >250 mg/dL (>13.9 mmol/L) |
Each incremental 5% increase in TIR is associated with clinically significant benefits for individuals with type 1 or type 2 diabetes (26,27).
*For age <25 years, if the A1C goal is 7.5%, set TIR target to approximately 60%. See the section clinical application of time in ranges for additional information regarding target goal setting in pediatric management.
#See the section older and/or high-risk individuals with diabetes for additional information regarding target goal setting.
It was agreed that CGM-based glycemic targets must be personalized to meet the needs of each individual with diabetes. In addition, the group reached consensus on glycemic cutpoints (a target range of 70–180 mg/dL [3.9–10.0 mmol/L] for individuals with type 1 diabetes and type 2 diabetes and 63–140 mg/dL [3.5–7.8 mmol/L] during pregnancy, along with a set of targets for the time per day [% of CGM readings or minutes/hours]) individuals with type 1 diabetes and type 2 diabetes (Table 3) and women during pregnancy (Table 4) should strive to achieve. It should be noted that premeal and postprandial SMBG targets remain for diabetes in pregnancy (44), in addition to the new CGM TIR targets for overall glycemia.
Table 4.
Guidance on targets for assessment of glycemic control during pregnancy
| Diabetes group | TIR |
TBR |
TAR |
|||
|---|---|---|---|---|---|---|
| % of readings; time per day | Target range | % of readings; time per day | Below target level | % of readings; time per day | Above target level | |
| Pregnancy, type 1§ | >70%; >16 h, 48 min | 63–140 mg/dL† (3.5–7.8 mmol/L†) | <4%; <1 h | <63 mg/dL† (<3.5 mmol/L†) | <25%; <6 h | >140 mg/dL (>7.8 mmol/L) |
| <1%; <15 min | <54 mg/dL (<3.0 mmol/L) | |||||
| Pregnancy, type 2/GDM§ | See pregnancy section | 63–140 mg/dL† (3.5–7.8 mmol/L†) | See pregnancy section | <63 mg/dL† (<3.5 mmol/L†) | See pregnancy section | >140 mg/dL (>7.8 mmol/L) |
| <54 mg/dL (<3.0 mmol/L) | ||||||
Although the metric includes TIR, TBR, and TAR, achieving the goals for both TBR and TIR would result in reduced time spent above range and thereby improve glycemic control. However, some clinicians may choose to target the reduction of the high glucose values and minimize hypoglycemia, thereby arriving at more time in the target range. In both approaches, the first priority is to reduce TBR to target levels and then address TIR or TAR targets.
Note that for people with type 1 diabetes, the targets are informed by the ability to reach the targets with hybrid closed-loop therapy (11), the first example of which is now commercially available with several more systems in final stages of testing. Importantly, recent studies have shown the potential of reaching these targets with CGM in individuals using multiple daily injections (6). In type 2 diabetes, there is generally less glycemic variability and hypoglycemia than in type 1 diabetes (45). Thus, people with type 2 diabetes can often achieve more time in the target range while minimizing hypoglycemia (4). As demonstrated by Beck et al. (4), individuals with type 2 diabetes increased their TIR by 10.3% (from 55.6% to 61.3%) after 24 weeks of CGM use with slight reductions in TBR. Most recently, the beneficial effects of new medications, such as sodium–glucose cotransporter 2 agents have helped individuals with type 1 diabetes increase TIR (46–48). Targets for type 1 diabetes and type 2 diabetes were close enough to combine into one set of targets, outside of pregnancy.
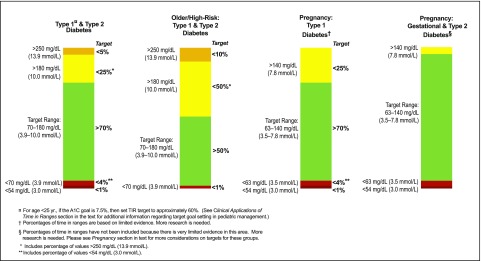
Another way to visualize the CGM-derived targets for the four categories of diabetes is shown in Fig. 1, which displays and compares the targets for TIR (green), TBR (two categories in light and dark red), and TAR (two categories in yellow and orange). It becomes clear at a glance that there are different expectations for the various time in ranges relating to safety concerns and efficacy based on currently available therapies and medical practice.
Figure 1.
CGM-based targets for different diabetes populations.
Clinical Validity of Measures
To fundamentally change clinical care with use of the new metrics, it would be important to demonstrate that the metrics relate to and predict clinical outcomes. In this regard, longer-term studies relating to time spent within specific CGM glycemic ranges, diabetes complications, and other outcomes are required. However, there is evidence from a number of recent studies that have shown correlations of TIR (70–180 mg/dL [3.9–10.0 mmol/L]) with diabetes complications (49,50) as well as a relationship between TIR and A1C (26,27). Although evidence regarding TIR for older and/or high-risk individuals is lacking, numerous studies have shown the elevated risk for hypoglycemia in these populations (51–56). Therefore, we have lowered the TIR target from >70% to >50% and reduced TBR to <1% at <70 mg/dL (<3.9 mmol/L) to place greater emphasis on reducing hypoglycemia with less emphasis on maintaining target glucose levels (Table 3).
Type 1 Diabetes and Type 2 Diabetes
Association With Complications
Associations between TIR and progression of both diabetic retinopathy (DR) and development of microalbuminuria were reported by Beck et al. (50), using 7-point blood glucose profiles from the DCCT data set to validate the use of TIR as an outcome measure for clinical trials. Their analysis showed that the hazard rate for retinopathy progression increased by 64% for each 10% reduction in TIR. The hazard rate for microalbuminuria development increased by 40% for each 10% reduction in TIR. A post hoc analysis of the same DCCT data set showed a link between glucose of <70 mg/dL (<3.9 mmol/L) and <54 mg/dL (<3.0 mmol/L) and an increased risk for severe hypoglycemia (57).
Similar associations between DR and TIR were reported in a recent study by Lu et al. (49) in which 3,262 individuals with type 2 diabetes were evaluated for DR, which was graded as non-DR, mild nonproliferative DR (NPDR), moderate NPDR, or vision-threatening DR. Results showed that individuals with more advanced DR spent significantly less time within target range (70–180 mg/dL [3.9–10.0 mmol/L]) and that prevalence of DR decreased with increasing TIR.
Relationship Between TIR and A1C
Analyses were conducted utilizing datasets from four randomized trials encompassing 545 adults with type 1 diabetes who had central laboratory measurements of A1C (26). TIR (70–180 mg/dL [3.9–10.0 mmol/L]) of 70% and 50% strongly corresponded with an A1C of approximately 7% (53 mmol/mol) and 8% (64 mmol/mol), respectively. An increase in TIR of 10% (2.4 h per day) corresponded to a decrease in A1C of approximately 0.5% (5.0 mmol/mol); similar associations were seen in an analysis of 18 randomized controlled trials (RCTs) by Vigersky and McMahon (27) that included over 2,500 individuals with type 1 diabetes and type 2 diabetes over a wide range of ages and A1C levels (Table 5).
Table 5.
Estimate of A1C for a given TIR level based on type 1 diabetes and type 2 diabetes studies
| Beck et al. (26) (n = 545 participants with type 1 diabetes) |
Vigersky and McMahon (27) (n = 1,137 participants with type 1 or type 2 diabetes) |
|||
|---|---|---|---|---|
| TIR 70–180 mg/dL (3.9–10.0 mmol/L) | A1C, % (mmol/mol) | 95% CI for predicted A1C values, % | TIR 70–180 mg/dL (3.9–10.0 mmol/L) | A1C, % (mmol/mol) |
| 20% | 9.4 (79) | (8.0, 10.7) | 20% | 10.6 (92) |
| 30% | 8.9 (74) | (7.6, 10.2) | 30% | 9.8 (84) |
| 40% | 8.4 (68) | (7.1, 9.7) | 40% | 9.0 (75) |
| 50% | 7.9 (63) | (6.6, 9.2) | 50% | 8.3 (67) |
| 60% | 7.4 (57) | (6.1, 8.8) | 60% | 7.5 (59) |
| 70% | 7.0 (53) | (5.6, 8.3) | 70% | 6.7 (50) |
| 80% | 6.5 (48) | (5.2, 7.8) | 80% | 5.9 (42) |
| 90% | 6.0 (42) | (4.7, 7.3) | 90% | 5.1 (32) |
| Every 10% increase in TIR = ∼0.5% (5.5 mmol/mol) A1C reduction |
Every 10% increase in TIR = ∼0.8% (8.7 mmol/mol) A1C reduction |
|||
The difference between findings from the two studies likely stems from differences in number of studies analyzed and subjects included (RCTs with subjects with type 1 diabetes vs. RCTs with subjects with type 1 or type 2 diabetes with CGM and SMBG).
Pregnancy
During pregnancy, the goal is to safely increase TIR as quickly as possible, while reducing TAR and glycemic variability. Data from the first study of longitudinal CGM use in pregnancy demonstrated a 13–percentage point increase in TIR (43% to 56% TIR 70–140 mg/dL [3.9–7.8 mmol/L]) (58). TBR <50 mg/dL was reduced from 6% to 4%, although the higher TBR <70 mg/dL was high (13–15%) using older-generation sensors. With improved sensor accuracy, recent type 1 diabetes pregnancy studies report a lower threshold of <63 mg/dL (<3.5 mmol/L) for TBR and ≥63 mg/dL (≥3.5 mmol/L) for TIR (59,60). Data from Sweden, and the Continuous Glucose Monitoring in Women With Type 1 Diabetes in Pregnancy Trial (CONCEPTT) control group, report 50% TIR in the first trimester, improving to 60% TIR in the third trimester, reflecting contemporary antenatal care. Of note, these data confirm that the TBR <63 mg/dL (<3.5 mmol/L) recommendation of <4% is safely achievable, especially after the first trimester. Furthermore, 33% of women achieved the recommendation of 70% TIR 63–140 mg/dL (3.5–7.8 mmol/L) in the final (>34) weeks of pregnancy. Preliminary data suggest that closed-loop systems may allow pregnant women to safely achieve 70% TIR at an earlier (>24 weeks) stage of gestation (61,62). Law et al. (63) analyzed data from two early CGM trials (64,65) describing the associations between CGM measures and risk of large-for-gestational-age (LGA) infants. Taken together, the Swedish and CONCEPTT data confirm that a 5–7% higher TIR during the second and third trimesters is associated with decreased risk of LGA and neonatal outcomes including macrosomia, shoulder dystocia, neonatal hypoglycemia, and neonatal intensive care admissions. More data are needed to define the clinical CGM targets for pregnant women with type 2 diabetes, who spend one-third less time hyperglycemic than women with type 1 diabetes and achieve TIR of 90% (58). Because of the lack of evidence on CGM targets for women with gestational diabetes mellitus (GDM) or type 2 diabetes in pregnancy, percentages of time spent in range, below range, and above range have not been included in this report. Recent data suggest that even more stringent targets (66) and greater attention to overnight glucose profiles may be required to normalize outcomes in pregnant women with GDM (63).
Older and/or High-Risk Individuals With Diabetes
Older and/or high-risk individuals with diabetes are at notably higher risk for severe hypoglycemia due to age, duration of diabetes, duration of insulin therapy, and greater prevalence of hypoglycemia unawareness (51–55). The increased risk of severe hypoglycemia is compounded by cognitive and physical impairments and other comorbidities (53,56). High-risk individuals include those with a higher risk of complications, comorbid conditions (e.g., cognitive deficits, renal disease, joint disease, osteoporosis, fracture, and/or cardiovascular disease), and those requiring assisted care, which can complicate treatment regimens (56). Therefore, when setting glycemic targets for high-risk and/or elderly people, it is important to individualize and be conservative, with a strong focus on reducing the percentage of time spent <70 mg/dL (<3.9 mmol/L) and preventing excessive hyperglycemia.
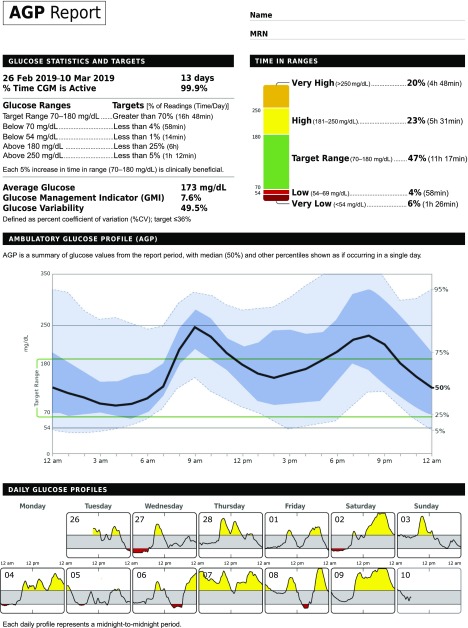
Standardization of CGM Data Presentation
As noted above, in 2013 a panel of clinicians with expertise in CGM published recommendations for use of the Ambulatory Glucose Profile (AGP) as a template for data presentation and visualization. Originally created by Mazze et al. (67), the standardized AGP report was further developed by the International Diabetes Center and now incorporates all the core CGM metrics and targets along with a 14-day composite glucose profile as an integral component of clinical decision making (24). This recommendation was later endorsed at the aforementioned international consensus conference on CGM metrics (18) and is referenced as an example in the American Diabetes Association 2019 “Standards of Medical Care in Diabetes” (16) and in an update to the American Association of Clinical Endocrinologists consensus on use of CGM (68). The AGP report, in slightly modified formats, has been adopted by most of the CGM device manufacturers in their download software. An example of the AGP report, updated to incorporate targets, is presented in Fig. 2. In the AGP report, glucose ranges are defined as “Very High” (Level 2), “High” (Level 1), “Low” (Level 1), and “Very Low” (Level 2). An “mmol/L” version is provided in Supplementary Fig. 1.
Figure 2.
Ambulatory Glucose Profile.
There is a general consensus that a useful CGM report is one that can be understood by clinicians and people with diabetes. While there may be some terms (e.g., glucose variability) that are less familiar to many people with diabetes, a single-page report that the medical team can review and file in the electronic medical record and that can be used as a shared decision-making tool with people with diabetes was considered to be of value (69–72). More detailed reports (e.g., adjustable data ranges, detailed daily reports) should remain available for individualized review by or with people with diabetes.
Clinical Application of Time in Ranges
Despite its demonstrated value, clinical utilization of CGM data has remained suboptimal. Although time constraints and reimbursement issues are clearly obstacles, clinician inexperience in data interpretation and lack of standardization software for visualization of CGM data have also played a role (73). The proposed standardized report enables clinicians to readily identify important metrics such as the percentage of time spent within, below, and above each individual’s target range, allowing for greater personalization of therapy through shared decision making.
Using the standardized report, the clinician can also address glucose variability (e.g., the coefficient of variation [%CV] metric) (74) or use the glucose management indicator (GMI) metric (75) to discuss the possible discrepancies noted in glucose exposure derived from CGM data versus the individual’s laboratory-measured A1C (41,76). With appropriate educational materials, time, and experience, clinicians will develop a systematic approach to CGM data analysis and the most effective ways to discuss the data with patients in person or remotely.
Goal Setting
Numerous studies have demonstrated the clinical benefits of early achievement of near-normal glycemic control in individuals with type 1 diabetes and type 2 diabetes (77–83). However, when advising people with diabetes, goal-setting must be collaborative and take into account the individual needs/capabilities of each patient and start with the goals that are most achievable. An early study by DeWalt et al. (84) found that setting small, achievable goals not only enhances people’s ability to cope with their diabetes, but that people with diabetes who set and achieved their goals often initiated additional behavioral changes on their own. One approach to consider is the SMART goal (Specific, Measurable, Achievable, Relevant, Time-bound) intervention, which is directly applicable to setting targets for time in ranges. First described by Lawlor and Hornyak in 2012 (85), this approach incorporates four key components of behavioral change relevant to goal setting: 1) the goal is specific and defines exactly what is to be achieved, 2) the goal is measurable and there is tangible evidence when it has been achieved, 3) the goal is achievable but stretches the patient slightly so that he/she feels challenged, and 4) the goal should be attainable over a short period of time.
Effective goals should utilize CGM data to identify specific instances for the patient to take measurable action to prevent hypoglycemia. Although analysis of the AGP reports provides an opportunity for meaningful discussion, individuals should be counseled to look at patterns throughout the day to see when low glucose events are occurring and make adjustments in their therapy to reduce these events.
When applying the CGM metrics in clinical practice, it may be more meaningful and motivating to communicate to people with diabetes the importance of working to reduce the time spent <70 mg/dL (<3.9 mmol/L) to less than 1 h per day and time spent <54 mg/dL (<3.0 mmol/L) to less than 15 min per day, rather than using <4% and <1%, respectively, as the goal. However, as discussed earlier, targets must be personalized to meet the needs and capabilities of each person, focusing on small steps and small successes. Individuals with diabetes should work with their provider and/or educator to develop a SMART goal to reduce TBR.
Individualized goals are particularly important for pediatric and young adult populations. The International Society for Pediatric and Adolescent Diabetes recommends that targets for individuals ≤25 years of age aim for the lowest achievable A1C without undue exposure to severe hypoglycemia or negative effects on quality of life and burden of care (86). An A1C target of 7.0% (53 mmol/mol) can be used in children, adolescents, and adults ≤25 years old who have access to comprehensive care (86). However, a higher A1C goal (e.g., <7.5% [<58 mmol/mol]) may be more appropriate in the following situations: inability to articulate hypoglycemia symptoms, hypoglycemia unawareness, history of severe hypoglycemia, lack of access to analog insulins and/or advanced insulin delivery technology, or inability to regularly check glucose (86). This would equate to a TIR target of ∼60% (Table 4).
The consensus group recognized that achieving the targets for the various time in ranges is aspirational in some situations, and many individuals will require ongoing support, both educational and technological, from their health care team. Importantly, as demonstrated by Beck et al. (26), Vigersky and McMahon (27), and Feig et al. (59), even small, incremental improvements yield significant glycemic benefits. Therefore, when advising individuals with diabetes (particularly children, adolescents, and high-risk individuals) about their glycemic goals, it is important to take a stepwise approach, emphasizing that what may appear to be small, incremental successes (e.g., 5% increase in TIR) are, in fact, clinically significant in improving their glycemia (26,27,59). However, when counseling women planning pregnancy and pregnant women, greater emphasis should be placed on getting to goal as soon as possible (59,60).
Conclusions
Use of CGM continues to expand in clinical practice. As a component of diabetes self-management, daily use of CGM provides the ability to obtain immediate feedback on current glucose levels as well as direction and rate of change in glucose levels. This information allows people with diabetes to optimize dietary intake and exercise, make informed therapy decisions regarding mealtime and correction of insulin dosing, and, importantly, react immediately and appropriately to mitigate or prevent acute glycemic events (87–89). Retrospective analysis of CGM data, using standardized data management tools such as the AGP, enables clinicians and people with diabetes to work collaboratively in identifying problem areas and then set achievable goals (70–72). We conclude that, in clinical practice, time in ranges (within target range, below range, above range) are both appropriate and useful as clinical targets and outcome measurements that complement A1C for a wide range of people with diabetes and that the target values specified in this article should be considered an integral component of CGM data analysis and day-to-day treatment decision making.
Supplementary Material
Article Information
Acknowledgments. The consensus group participants wish to thank the ATTD Congress for organizing and coordinating the meeting and Rachel Naveh (The Jesse Z and Sara Lea Shafer Institute for Endocrinology and Diabetes, National Center for Childhood Diabetes, Schneider Children’s Medical Center of Israel) for assistance in organizing the meeting. They also thank Courtney Lias from the U.S. Food and Drug Administration for her participation as an observer at the consensus conference.
Funding and Duality of Interest. Support for the CGM consensus conference and development of this consensus report was provided by the ATTD Congress. Abbott Diabetes Care, Astra Zeneca, Dexcom Inc., Eli Lilly and Company, Insulet Corporation, Medtronic, Novo Nordisk, Roche Diabetes Care, and Sanofi provided funding to ATTD to support the consensus meeting. Consensus participants were reimbursed for travel to the ATTD conference and one night of lodging; no honoraria were provided. ATTD provided funding to Christopher G. Parkin, CGParkin Communications, Inc., for his medical writing and editorial support. T.Ba. has received honoraria for participation on advisory boards for Novo Nordisk, Sanofi, Eli Lilly and Company, Boehringer, Medtronic, and Bayer Health Care and as a speaker for AstraZeneca, Eli Lilly and Company, Bayer, Novo Nordisk, Medtronic, Sanofi, and Roche. T.Ba. owns stocks of DreaMed Diabetes, and his institution has received research grant support and travel expenses from Abbott Diabetes Care, Medtronic, Novo Nordisk, GluSense, Sanofi, Sandoz, and Diamyd. T.D. has received speaker honoraria, research support, and consulting fees from Abbott Diabetes Care, Bayer, Bristol-Myers Squibb, AstraZeneca, Boehringer Ingelheim, Dexcom, Eli Lilly and Company, Medtronic, Novo Nordisk, Sanofi, and Roche Diabetes Care; and he is a shareholder of DreaMed Diabetes. S.A.A. has received honoraria for participation on advisory boards for Roche and Medtronic and has given a lecture funded by Sanofi. R.B. is an employee the Jaeb Center for Health Research, which has received grant support from Dexcom, Animas, Bigfoot, and Tandem; nonfinancial study support from Dexcom, Abbott Diabetes Care, and Roche Diabetes Care; and consulting fees from Eli Lilly and Company and Insulet. He has no personal financial arrangements with any company. R.M.B. has received research funding and served as a consultant and on advisory boards for Abbott Diabetes Care, Becton Dickinson, Dexcom, Eli Lilly and Company, Glooko, Helmsley Charitable Trust, Hygieia, Johnson & Johnson, Medtronic, Merck, Novo Nordisk, Roche, Sanofi, and Senseonics. His employer, nonprofit HealthPartners Institute, contracts for his services and no personal income goes to R.M.B. E.B. received honoraria for participation on advisory boards and speakers’ bureaus from Abbott Diabetes Care, AstraZeneca, Medtronic, Novartis, Roche, and Sanofi. B.A.B. is on medical advisory boards for Medtronic and Convatec and has received research funding from the National Institutes of Health, JDRF, the Leona M. and Harry B. Helmsley Charitable Trust, Medtronic Diabetes, ConvaTec, Dexcom, Tandem, and Insulet. K.L.C. is an employee of Close Concerns and The diaTribe Foundation, which receive funding from CGM manufacturers, including Medtronic, Dexcom, and Abbott Diabetes Care. C.C. reports 10 patents and patent applications related to continuous glucose sensors and artificial pancreas. E.D. has received consulting fees and honoraria for participation on advisory boards from Roche, Insulet, and Eli Lilly and Company and research support from Dexcom, Insulet, Animas, Xeris, and Roche. J.H.D. has received speaker honoraria and research support from and has consulted for Abbott Diabetes Care, Dexcom, Medtronic, Merck Sharp & Dohme, Novo Nordisk, Sanofi, Roche, Senseonics, and Zealand. F.J.D. has received consulting fees from ModeAGC and research support from Dexcom, Insulet, Animas, and Xeris. S.G. has received consulting fees and honoraria for participation on advisory boards for Medtronic, Roche Diabetes Care, Merck, Lexicon, Novo Nordisk, Sanofi, MannKind, Senseonics, Zealand, and Eli Lilly and Company and research grants from Eli Lilly and Company, Novo Nordisk, Merck, Lexicon, Medtronic, Dario, the National Cancer Institute, T1D Exchange, the National Institute of Diabetes and Digestive and Kidney Diseases, JDRF, Animas, Dexcom, and Sanofi. G.G. has received research support from Novo Nordisk and Medtronic and honoraria for participation on speakers’ bureaus from Novo Nordisk, Eli Lilly and Company, Boehringer Ingelheim, and Sanofi. S.H. has served as a consultant or speaker for Eli Lilly and Company, Novo Nordisk, Takeda, Boehringer Ingelheim, MannKind, Sanofi, Zealand Pharma, and UNEEG. L.H. is a consultant for companies developing novel diagnostic and therapeutic options for diabetes. He is a shareholder of Profil Institut für Stoffwechselforschung GmbH and ProSciento. I.B.H. receives research funding from Medtronic Diabetes and has received consulting fees from Abbott Diabetes Care, Bigfoot, Roche, and Becton Dickinson. R.H. reports having received speaker honoraria from Eli Lilly and Company, Novo Nordisk, and AstraZeneca, serving on an advisory panel for Eli Lilly and Company and Novo Nordisk, and receiving license fees from B. Braun and Medtronic. O.K. received honoraria from Amring, Eli Lilly and Company, Novo Nordisk, and Sanofi and owns shares from DreaMed Diabetes. B.K. declares research support handled by the University of Virginia from Dexcom, Roche, Sanofi, and Tandem; patent royalties handled by the University of Virginia from Johnson & Johnson, Sanofi, and Dexcom; and has served as a consultant for Sanofi and Tandem and on a speakers’ bureau for Dexcom. B.L. is an employee of Close Concerns and The diaTribe Foundation, which receive funding from CGM manufacturers, including Medtronic, Dexcom, and Abbott Diabetes Care. C.M. serves or has served on the advisory panel or speakers’ bureau for Novo Nordisk, Sanofi, Merck Sharp & Dohme, Eli Lilly and Company, Novartis, AstraZeneca, Boehringer Ingelheim, Hanmi Pharmaceuticals, Roche, Medtronic, ActoBio Therapeutics, Pfizer, Dianax, and UCB. Financial compensation for these activities has been received by KU Leuven. H.R.M. received honoraria from participation on advisory boards for Medtronic and research support from Dexcom, Medtronic, Abbott Diabetes Care, and Johnson & Johnson. R.N. received honoraria for participation on the speakers’ bureau of Novo Nordisk, Pfizer, Eli Lilly and Company, and Sanofi. R.N. owns DreaMed stock and reports two patent applications. K.N. owns shares in Novo Nordisk and has received consulting fees from Medtronic, Abbott Diabetes Care, and Novo Nordisk; speaker honoraria from Medtronic, Roche Diabetes Care, Rubin Medical, Sanofi, Novo Nordisk, Zealand Pharma, and Bayer; and research support from Novo Nordisk, Zealand Pharma, Medtronic, and Roche Diabetes Care. C.G.P. has received consulting fees from Dexcom, Diasome, Onduo, Proteus, Roche Diabetes Care, and Senseonics. E.R. has received consulting fees from A. Menarini Diagnostics, Abbott Diabetes Care, Air Liquide SI, Becton Dickinson, Cellnovo, Dexcom, Eli Lilly and Company, Insulet, Johnson & Johnson, Medtronic, Novo Nordisk, Roche, and Sanofi and research support from Abbott Diabetes Care, Dexcom, Insulet, Tandem, and Roche. D.R. has received consulting fees from Eli Lilly and Company and Better Therapeutics. K.S. is an employee of dQ&A Market Research, Inc., whose clients include several device and pharmaceutical companies in the diabetes field. S.A.W. has received consulting fees from Eli Lillyand Company, Sanofi, and Zealand and speaker honoraria from Medtronic, Insulet, and Tandem. M.P. is a member of the advisory board of AstraZeneca, Sanofi, Medtronic, Eli Lilly and Company, Novo Nordisk, and Insulet and is a consultant to RSP Systems A/S, Qulab Medical, and Pfizer. The institute headed by M.P. received research support from Medtronic, Novo Nordisk, Eli Lilly and Company, Dexcom, Sanofi, Insulet, OPKO Health, DreaMed Diabetes, Bristol-Myers Squibb, and Merck. M.P. is a stockholder/shareholder of DreaMed Diabetes, NG Solutions, and Nutriteen Professionals and reports two patent applications. No other potential conflicts of interest relevant to this article were reported.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dci19-0028/-/DC1.
This international consensus report has been endorsed by the American Diabetes Association, American Association of Clinical Endocrinologists, American Association of Diabetes Educators, European Association for the Study of Diabetes, Foundation of European Nurses in Diabetes, International Society for Pediatric and Adolescent Diabetes, JDRF, and Pediatric Endocrine Society.
References
- 1.Lind M, Polonsky W, Hirsch IB, et al. Continuous glucose monitoring vs conventional therapy for glycemic control in adults with type 1 diabetes treated with multiple daily insulin injections: the GOLD randomized clinical trial. JAMA 2017;317:379–387 [DOI] [PubMed] [Google Scholar]
- 2.Aleppo G, Ruedy KJ, Riddlesworth TD, et al.; REPLACE-BG Study Group . REPLACE-BG: A randomized trial comparing continuous glucose monitoring with and without routine blood glucose monitoring in adults with well-controlled type 1 diabetes. Diabetes Care 2017;40:538–545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beck RW, Riddlesworth T, Ruedy K, et al.; DIAMOND Study Group . Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections: The DIAMOND randomized clinical trial. JAMA 2017;317:371–378 [DOI] [PubMed] [Google Scholar]
- 4.Beck RW, Riddlesworth TD, Ruedy K, et al.; DIAMOND Study Group . Continuous glucose monitoring versus usual care in patients with type 2 diabetes receiving multiple daily insulin injections: a randomized trial. Ann Intern Med 2017;167:365–374 [DOI] [PubMed] [Google Scholar]
- 5.Polonsky WH, Hessler D, Ruedy KJ, Beck RW; DIAMOND Study Group . The impact of continuous glucose monitoring on markers of quality of life in adults with type 1 diabetes: further findings from the DIAMOND randomized clinical trial. Diabetes Care 2017;40:736–741 [DOI] [PubMed] [Google Scholar]
- 6.Šoupal J, Petruželková L, Flekač M, et al. Comparison of different treatment modalities for type 1 diabetes, including sensor-augmented insulin regimens, in 52 weeks of follow-up: a COMISAIR study. Diabetes Technol Ther 2016;18:532–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Beers CA, DeVries JH, Kleijer SJ, et al. Continuous glucose monitoring for patients with type 1 diabetes and impaired awareness of hypoglycaemia (IN CONTROL): a randomised, open-label, crossover trial. Lancet Diabetes Endocrinol 2016;4:893–902 [DOI] [PubMed] [Google Scholar]
- 8.Bolinder J, Antuna R, Geelhoed-Duijvestijn P, Kröger J, Weitgasser R. Novel glucose-sensing technology and hypoglycaemia in type 1 diabetes: a multicentre, non-masked, randomised controlled trial. Lancet 2016;388:2254–2263 [DOI] [PubMed] [Google Scholar]
- 9.Haak T, Hanaire H, Ajjan R, Hermanns N, Riveline JP, Rayman G. Flash glucose-sensing technology as a replacement for blood glucose monitoring for the management of insulin-treated type 2 diabetes: a multicenter, open-label randomized controlled trial. Diabetes Ther 2017;8:55–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choudhary P, Olsen BS, Conget I, Welsh JB, Vorrink L, Shin JJ. Hypoglycemia prevention and user acceptance of an insulin pump system with predictive low glucose management. Diabetes Technol Ther 2016;18:288–291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bergenstal RM, Garg S, Weinzimer SA, et al. Safety of a hybrid closed-loop insulin delivery system in patients with type 1 diabetes. JAMA 2016;316:1407–1408 [DOI] [PubMed] [Google Scholar]
- 12.Heinemann L, Freckmann G, Erdmann D, et al. Real-time continuous glucose monitoring use in adults with type 1 diabetes and impaired hypoglycaemia awareness or severe hypoglycaemia treated with multiple daily insulin injections (HypoDE): a multicentre, randomised controlled trial. Lancet 2018;391:1367–1377 [DOI] [PubMed] [Google Scholar]
- 13.Reddy M, Jugnee N, El Laboudi A, Spanudakis E, Anantharaja S, Oliver N. A randomised controlled pilot study of continuous glucose monitoring and flash glucose monitoring in people with type 1 diabetes and impaired awareness of hypoglycaemia. Diabet Med 2018;35:483–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Battelino T, Nimri R, Dovc K, Phillip M, Bratina N. Prevention of hypoglycemia with predictive low glucose insulin suspension in children with type 1 diabetes: a randomized controlled trial. Diabetes Care 2017;40:764–770 [DOI] [PubMed] [Google Scholar]
- 15.Dovc K, Cargnelutti K, Sturm A, Selb J, Bratina N, Battelino T. Continuous glucose monitoring use and glucose variability in pre-school children with type 1 diabetes. Diabetes Res Clin Pract 2019;147:76–80 [DOI] [PubMed] [Google Scholar]
- 16.American Diabetes Association 7. Diabetes technology: Standards of Medical Care in Diabetes—2019. Diabetes Care 2019;42(Suppl. 1):S71–S80 [DOI] [PubMed] [Google Scholar]
- 17.Fonseca VA, Grunberger G, Anhalt H, et al.; Consensus Conference Writing Committee . Continuous glucose monitoring: a consensus conference of the American Association of Clinical Endocrinologists and American College of Endocrinology. Endocr Pract 2016;22:1008–1021 [DOI] [PubMed] [Google Scholar]
- 18.Danne T, Nimri R, Battelino T, et al. International consensus on use of continuous glucose monitoring. Diabetes Care 2017;40:1631–1640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Petrie JR, Peters AL, Bergenstal RM, Holl RW, Fleming GA, Heinemann L. Improving the clinical value and utility of CGM Systems: issues and recommendations: a joint statement of the European Association for the Study of Diabetes and the American Diabetes Association Diabetes Technology Working Group. Diabetes Care 2017;40:1614–1621 [DOI] [PubMed] [Google Scholar]
- 20.Agiostratidou G, Anhalt H, Ball D, et al. Standardizing clinically meaningful outcome measures beyond HbA1c for type 1 diabetes: a consensus report of the American Association of Clinical Endocrinologists, the American Association of Diabetes Educators, the American Diabetes Association, the Endocrine Society, JDRF International, The Leona M. and Harry B. Helmsley Charitable Trust, the Pediatric Endocrine Society, and the T1D Exchange. Diabetes Care 2017;40:1622–1630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sherr JL, Tauschmann M, Battelino T, et al. ISPAD Clinical Practice Consensus Guidelines 2018: diabetes technologies. Pediatr Diabetes 2018;19(Suppl. 27):302–325 [DOI] [PubMed] [Google Scholar]
- 22.Foster NC, Beck RW, Miller KM, et al. State of type 1 diabetes management and outcomes from the T1D Exchange in 2016–2018. Diabetes Technol Ther 2019;21:66–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Foster NC, Miller K, Dimeglio L, et al. Marked increases in CGM use has not prevented increases in HbA1c levels in participants in the T1D Exchange (T1DX) clinic network (Abstract). Diabetes 2018;67(Suppl. 1):A451 [Google Scholar]
- 24.Bergenstal RM, Ahmann AJ, Bailey T, et al. Recommendations for standardizing glucose reporting and analysis to optimize clinical decision making in diabetes: the Ambulatory Glucose Profile (AGP). Diabetes Technol Ther 2013;15:198–211 [DOI] [PubMed] [Google Scholar]
- 25.American Diabetes Association Introduction: Standards of Medical Care in Diabetes—2017. Diabetes Care 2017;41(Suppl. 1):S1–S2 [DOI] [PubMed] [Google Scholar]
- 26.Beck RW, Bergenstal RM, Cheng P, et al. The relationships between time in range, hyperglycemia metrics, and HbA1c. J Diabetes Sci Technol. 13 January 2019. [Epub ahead of print]. DOI: 10.1177/1932296818822496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vigersky RA, McMahon C. The relationship of hemoglobin A1C to time-in-range in patients with diabetes. Diabetes Technol Ther 2019;21:81–85 [DOI] [PubMed] [Google Scholar]
- 28.Brod M, Christensen T, Thomsen TL, Bushnell DM. The impact of non-severe hypoglycemic events on work productivity and diabetes management. Value Health 2011;14:665–671 [DOI] [PubMed] [Google Scholar]
- 29.Brod M, Rana A, Barnett AH. Impact of self-treated hypoglycaemia in type 2 diabetes: a multinational survey in patients and physicians. Curr Med Res Opin 2012;28:1947–1958 [DOI] [PubMed] [Google Scholar]
- 30.Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care 2013;36:1384–1395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.International Hypoglycaemia Study Group Glucose concentrations of less than 3.0 mmol/L (54 mg/dL) should be reported in clinical trials: a joint position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2017;40:155–157 [DOI] [PubMed] [Google Scholar]
- 32.Novodvorsky P, Bernjak A, Chow E, et al. Diurnal differences in risk of cardiac arrhythmias during spontaneous hypoglycemia in young people with type 1 diabetes. Diabetes Care 2017;40:655–662 [DOI] [PubMed] [Google Scholar]
- 33.Battelino T, Conget I, Olsen B, et al.; SWITCH Study Group . The use and efficacy of continuous glucose monitoring in type 1 diabetes treated with insulin pump therapy: a randomised controlled trial. Diabetologia 2012;55:3155–3162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bergenstal RM, Tamborlane WV, Ahmann A, et al.; STAR 3 Study Group . Sensor-augmented pump therapy for A1C reduction (STAR 3) study: results from the 6-month continuation phase. Diabetes Care 2011;34:2403–2405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cox DJ, Kovatchev BP, Julian DM, et al. Frequency of severe hypoglycemia in insulin-dependent diabetes mellitus can be predicted from self-monitoring blood glucose data. J Clin Endocrinol Metab 1994;79:1659–1662 [DOI] [PubMed] [Google Scholar]
- 36.Qu Y, Jacober SJ, Zhang Q, Wolka LL, DeVries JH. Rate of hypoglycemia in insulin-treated patients with type 2 diabetes can be predicted from glycemic variability data. Diabetes Technol Ther 2012;14:1008–1012 [DOI] [PubMed] [Google Scholar]
- 37.National Institute of Diabetes and Digestive and Kidney Diseases Health Information Center. Sickle cell trait & other hemoglobinopathies & diabetes (for providers) [Internet]. Available from https://www.niddk.nih.gov/health-information/diagnostic-tests/sickle-cell-trait-hemoglobinopathies-diabetes. Accessed 12 January 2018
- 38.Bry L, Chen PC, Sacks DB. Effects of hemoglobin variants and chemically modified derivatives on assays for glycohemoglobin. Clin Chem 2001;47:153–163 [PubMed] [Google Scholar]
- 39.Ford ES, Cowie CC, Li C, Handelsman Y, Bloomgarden ZT. Iron-deficiency anemia, non-iron-deficiency anemia and HbA1c among adults in the US. J Diabetes 2011;3:67–73 [DOI] [PubMed] [Google Scholar]
- 40.Nielsen LR, Ekbom P, Damm P, et al. HbA1c levels are significantly lower in early and late pregnancy. Diabetes Care 2004;27:1200–1201 [DOI] [PubMed] [Google Scholar]
- 41.Beck RW, Connor CG, Mullen DM, Wesley DM, Bergenstal RM. The fallacy of average: how using HbA1c alone to assess glycemic control can be misleading. Diabetes Care 2017;40:994–999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xing D, Kollman C, Beck RW, et al.; Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group . Optimal sampling intervals to assess long-term glycemic control using continuous glucose monitoring. Diabetes Technol Ther 2011;13:351–358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Riddlesworth TD, Beck RW, Gal RL, et al. Optimal sampling duration for continuous glucose monitoring to determine long-term glycemic control. Diabetes Technol Ther 2018;20:314–316 [DOI] [PubMed] [Google Scholar]
- 44.American Diabetes Association 14. Management of diabetes in pregnancy. Standards of Medical Care in Diabetes—2019. Diabetes Care 2019;42(Suppl. 1):S165–S172 [DOI] [PubMed] [Google Scholar]
- 45.Rama Chandran S, Tay WL, Lye WK, et al. Beyond HbA1c: comparing glycemic variability and glycemic indices in predicting hypoglycemia in type 1 and type 2 diabetes. Diabetes Technol Ther 2018;20:353–362 [DOI] [PubMed] [Google Scholar]
- 46.Famulla S, Pieber TR, Eilbracht J, et al. Glucose exposure and variability with empagliflozin as adjunct to insulin in patients with type 1 diabetes: continuous glucose monitoring data from a 4-week, randomized, placebo-controlled trial (EASE-1). Diabetes Technol Ther 2017;19:49–60 [DOI] [PubMed] [Google Scholar]
- 47.Dandona P, Mathieu C, Phillip M, et al.; DEPICT-1 Investigators . Efficacy and safety of dapagliflozin in patients with inadequately controlled type 1 diabetes: the DEPICT-1 52-week study. Diabetes Care 2018;41:2552–2559 [DOI] [PubMed] [Google Scholar]
- 48.Mathieu C, Dandona P, Phillip M, et al.; DEPICT-1 and DEPICT-2 Investigators . Glucose variables in type 1 diabetes studies with dapagliflozin: pooled analysis of continuous glucose monitoring data from DEPICT-1 and -2. Diabetes Care 2019;42:1081–1087 [DOI] [PubMed] [Google Scholar]
- 49.Lu J, Ma X, Zhou J, et al. Association of time in range, as assessed by continuous glucose monitoring, with diabetic retinopathy in type 2 diabetes. Diabetes Care 2018;41:2370–2376 [DOI] [PubMed] [Google Scholar]
- 50.Beck RW, Bergenstal RM, Riddlesworth TD, et al. Validation of time in range as an outcome measure for diabetes clinical trials. Diabetes Care 2019;42:400–405 [DOI] [PMC free article] [PubMed]
- 51.Weinstock RS, DuBose SN, Bergenstal RM, et al.; T1D Exchange Severe Hypoglycemia in Older Adults With Type 1 Diabetes Study Group . Risk factors associated with severe hypoglycemia in older adults with type 1 diabetes. Diabetes Care 2016;39:603–610 [DOI] [PubMed] [Google Scholar]
- 52.Bremer JP, Jauch-Chara K, Hallschmid M, Schmid S, Schultes B. Hypoglycemia unawareness in older compared with middle-aged patients with type 2 diabetes. Diabetes Care 2009;32:1513–1517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Punthakee Z, Miller ME, Launer LJ, et al.; ACCORD Group of Investigators; ACCORD-MIND Investigators . Poor cognitive function and risk of severe hypoglycemia in type 2 diabetes: post hoc epidemiologic analysis of the ACCORD trial. Diabetes Care 2012;35:787–793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Giorda CB, Ozzello A, Gentile S, et al.; HYPOS-1 Study Group of AMD . Incidence and risk factors for severe and symptomatic hypoglycemia in type 1 diabetes. Results of the HYPOS-1 study. Acta Diabetol 2015;52:845–853 [DOI] [PubMed] [Google Scholar]
- 55.Cariou B, Fontaine P, Eschwege E, et al. Frequency and predictors of confirmed hypoglycaemia in type 1 and insulin-treated type 2 diabetes mellitus patients in a real-life setting: results from the DIALOG study. Diabetes Metab 2015;41:116–125 [DOI] [PubMed] [Google Scholar]
- 56.Abdelhafiz AH, Rodríguez-Mañas L, Morley JE, Sinclair AJ. Hypoglycemia in older people – a less well recognized risk factor for frailty. Aging Dis 2015;6:156–167 [DOI] [PMC free article] [PubMed]
- 57.Beck RW, Bergenstal RM, Riddlesworth TD, Kollman C. The association of biochemical hypoglycemia with the subsequent risk of a severe hypoglycemic event: analysis of the DCCT data set. Diabetes Technol Ther 2019;21:1–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Murphy HR, Rayman G, Duffield K, et al. Changes in the glycemic profiles of women with type 1 and type 2 diabetes during pregnancy. Diabetes Care 2007;30:2785–2791 [DOI] [PubMed] [Google Scholar]
- 59.Feig DS, Donovan LE, Corcoy R, et al.; CONCEPTT Collaborative Group . Continuous glucose monitoring in pregnant women with type 1 diabetes (CONCEPTT): a multicentre international randomised controlled trial. Lancet 2017;390:2347–2359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kristensen K, Ögge LE, Sengpiel V, et al. Continuous glucose monitoring in pregnant women with type 1 diabetes: an observational cohort study of 186 pregnancies. Diabetologia. 23 March 2019. [Epub ahead of print]. DOI: 10.1007/s00125-019-4850-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stewart ZA, Wilinska ME, Hartnell S, et al. Closed-loop insulin delivery during pregnancy in women with type 1 diabetes. N Engl J Med 2016;375:644–654 [DOI] [PubMed] [Google Scholar]
- 62.Stewart ZA, Wilinska ME, Hartnell S, et al. Day-and-night closed-loop insulin delivery in a broad population of pregnant women with type 1 diabetes: a randomized controlled crossover trial. Diabetes Care 2018;41:1391–1399 [DOI] [PubMed] [Google Scholar]
- 63.Law GR, Alnaji A, Alrefaii L, et al. Suboptimal nocturnal glucose control is associated with large for gestational age in treated gestational diabetes mellitus. Diabetes Care 2019;42:810–815 [DOI] [PubMed] [Google Scholar]
- 64.Murphy HR, Rayman G, Lewis K, et al. Effectiveness of continuous glucose monitoring in pregnant women with diabetes: randomised clinical trial. BMJ 2008;337:a1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Secher AL, Ringholm L, Andersen HU, Damm P, Mathiesen ER. The effect of real-time continuous glucose monitoring in pregnant women with diabetes: a randomized controlled trial. Diabetes Care 2013;36:1877–1883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Paramasivam SS, Chinna K, Singh AKK, et al. Continuous glucose monitoring results in lower HbA1c in Malaysian women with insulin-treated gestational diabetes: a randomized controlled trial. Diabet Med 2018;35:1118–1129 [DOI] [PubMed] [Google Scholar]
- 67.Mazze RS, Lucido D, Langer O, Hartmann K, Rodbard D. Ambulatory glucose profile: representation of verified self-monitored blood glucose data. Diabetes Care 1987;10:111–117 [DOI] [PubMed] [Google Scholar]
- 68.Fonseca V, Grunberger G. Letter to the editor: standard glucose reporting: follow-up to the February 2016 AACE CGM Consensus Conference. Endocr Pract 2017;23:629–632 [DOI] [PubMed] [Google Scholar]
- 69.Mullen DM, Bergenstal R, Criego A, Arnold KC, Goland R, Richter S. Time savings using a standardized glucose reporting system and ambulatory glucose profile. J Diabetes Sci Technol 2018;12:614–621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Carlson AL, Mullen DM, Bergenstal RM. Clinical use of continuous glucose monitoring in adults with type 2 diabetes. Diabetes Technol Ther 2017;19(Suppl. 2):S4–S11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hirsch IB, Verderese CA. Professional flash continuous glucose monitoring with ambulatory glucose profile reporting to supplement A1C: rationale and practical implementation. Endocr Pract 2017;23:1333–1344 [DOI] [PubMed] [Google Scholar]
- 72.Kruger DF, Edelman SV, Hinnen DA, Parkin CG. Reference guide for integrating continuous glucose monitoring into clinical practice. Diabetes Educ 2019;45(Suppl. 1):3S–20S [DOI] [PubMed] [Google Scholar]
- 73.Rodbard D. Continuous glucose monitoring: a review of successes, challenges, and opportunities. Diabetes Technol Ther 2016;18(Suppl. 2):S3–S13 [DOI] [PMC free article] [PubMed]
- 74.Rodbard D. Glucose variability: a review of clinical applications and research developments. Diabetes Technol Ther 2018;20(Suppl. 2):S25–S215 [DOI] [PubMed] [Google Scholar]
- 75.Bergenstal RM, Beck RW, Close KL, et al. Glucose management indicator (GMI): a new term for estimating A1C from continuous glucose monitoring. Diabetes Care 2018;41:2275–2280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cohen RM, Franco RS, Smith EP, Higgins JM. When HbA1c and blood glucose do not match: how much is determined by race, by genetics, by differences in mean red blood cell age? J Clin Endocrinol Metab 2019;104:707–710 [DOI] [PubMed] [Google Scholar]
- 77.Svensson E, Baggesen LM, Johnsen SP, et al. Early glycemic control and magnitude of HbA1c reduction predict cardiovascular events and mortality: population-based cohort study of 24,752 metformin initiators. Diabetes Care 2017;40:800–807 [DOI] [PubMed] [Google Scholar]
- 78.Safford MM, Shewchuk R, Qu H, et al. Reasons for not intensifying medications: differentiating “clinical inertia” from appropriate care. J Gen Intern Med 2007;22:1648–1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nathan DM, Genuth S, Lachin J, et al.; Diabetes Control and Complications Trial Research Group . The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 80.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 81.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HAW. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008;359:1577–1589 [DOI] [PubMed] [Google Scholar]
- 82.Ismail-Beigi F, Craven T, Banerji MA, et al.; ACCORD trial group . Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet 2010;376:419–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hayward RA, Reaven PD, Wiitala WL, et al.; VADT Investigators . Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2015;372:2197–2206 [DOI] [PubMed] [Google Scholar]
- 84.DeWalt DA, Davis TC, Wallace AS, et al. Goal setting in diabetes self-management: taking the baby steps to success. Patient Educ Couns 2009;77:218–223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lawlor KB, Hornyak MJ. SMART goals: how the application of SMART goals can contribute to achievement of student learning outcomes. Developments in Business Simulation and Experiential Learning: Proceedings of the Annual ABSEL Conference 2012;39:259–267 [Google Scholar]
- 86.DiMeglio LA, Acerini C, Codner E, et al. ISPAD Clinical Practice Consensus Guidelines 2018: glycemic control targets and glucose monitoring for children, adolescents, and young adults with diabetes. Pediatr Diabetes 2018;19:105–114 [DOI] [PubMed]
- 87.Aleppo G, Laffel LM, Ahmann AJ, et al. A practical approach to using trend arrows on the Dexcom G5 CGM system for the management of adults with diabetes. J Endocr Soc 2017;1:1445–1460 [DOI] [PMC free article] [PubMed]
- 88.Laffel LM, Aleppo G, Buckingham BA, et al. A practical approach to using trend arrows on the Dexcom G5 CGM system to manage children and adolescents with diabetes. J Endocr Soc 2017;1:1461–1476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kudva YC, Ahmann AJ, Bergenstal RM, et al. Approach to using trend arrows in the FreeStyle Libre Flash Glucose Monitoring Systems in adults. J Endocr Soc 2018;2:1320–1337 [DOI] [PMC free article] [PubMed]
- 90.Monnier L, Colette C, Wojtusciszyn A, et al. Toward defining the threshold between low and high glucose variability in diabetes. Diabetes Care 2017;40:832–838 [DOI] [PubMed] [Google Scholar]
- 91.Rodbard D. Hypo- and hyperglycemia in relation to the mean, standard deviation, coefficient of variation, and nature of the glucose distribution. Diabetes Technol Ther 2012;14:868–876 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.