Abstract
Background
Revision shoulder arthroplasty has become increasingly common as primary arthroplasty has become more widespread.
Questions/Purposes
We sought to answer two questions: What are the risks factors for revision shoulder arthroplasty? What are the complications associated with revision shoulder arthroplasty?
Methods
A retrospective search of a national insurance database from the years 2013 to 2016 was undertaken for billing codes of patients undergoing revision shoulder arthroplasty. The odds ratios for revision of various patient demographic characteristics and comorbidities were determined. The incidences of various complications within 90 days of revision were determined.
Results
A total of 824 cases of revision shoulder arthroplasty were found. Eighty-seven patients (10.5%) had infections prior to revision and 133 patients (16.1%) had dislocations prior to revision. Of the risk factors examined, smoking status was associated with the highest odds ratio for revision (8.1). Additionally, depression, Charlson Comorbidity Index (CCI), male gender, renal failure, and diabetes were significant risks factors for revision. The most common complication of revision shoulder arthroplasty was found to be surgical site infection, affecting 10.9% of patients. In the time period studied, 89 patients underwent more than one revision shoulder arthroplasty.
Conclusion
Despite limitations inherent in database studies, this data may have utility for surgeons in pre-operative counseling of patients on their risk.
Electronic supplementary material
The online version of this article (10.1007/s11420-019-09673-3) contains supplementary material, which is available to authorized users.
Keywords: revision shoulder arthroplasty, database study, complication rate, risk factors, demographic trends, comorbidities
Introduction
It has been reported that both primary and revision shoulder arthroplasties have become increasingly common procedures in the USA, growing by over 300% in the past 20 years [1, 17]. The growth rate of revision shoulder arthroplasty (14%) from 1993 to 2007 is higher than that of total shoulder arthroplasty (9.4%) and shoulder hemiarthroplasty (5.6%) [6]. Revision surgery has been reported to comprise up to 15% of all total shoulder arthroplasties performed [7].
A number of retrospective case series have reported on complication rates of shoulder arthroplasty. Complications include infection, peri-prosthetic fracture, component loosening, rotator cuff pathology, and shoulder instability [5, 8, 11, 12, 16, 18, 22]. A recent systematic review reports a decrease in overall complications between 2006 and 2015 when compared with 1996 to 2005 [3]. However, the confounding effects of small sample size in each individual study, regional bias, and reporting bias pose challenges in any such study that estimates the incidence of complications requiring reoperation for a given procedure [15, 20]. Such effects are particularly pronounced when the rate of revision shoulder arthroplasty is relatively low. To address this issue, large samples from diverse geographic regions, as can be obtained in database studies, may be used to reduce bias.
The purpose of this study was to investigate the incidence of and demographic trends in revision shoulder arthroplasty over time, as well as to determine the risk factors associated with these procedures. We wished to elucidate these issues so as to better inform orthopedic surgeons’ counseling of patients pre-operatively about risks and expectations regarding primary shoulder arthroplasty. Based on our clinical experience, we hypothesized that patients with comorbidities such as smoking, diabetes, and chronic renal failure would be more likely to undergo revision shoulder arthroplasty.
Methods
The billing codes of patients undergoing revision shoulder arthroplasty were searched using the PearlDiver patient record database (PearlDiver, Colorado Springs, CO, USA), a national insurance database of the Humana Group that from the years 2013 to 2016 contained 11 million patient records. Additionally, for the purposes of determining the dates of primary arthroplasties or prior revisions, records for these patients were available beginning in 2007. We were unable to distinguish between anatomic versus reverse total shoulder arthroplasty, as they do not have distinct Current Procedural Terminology (CPT®) codes. Patients under 40 years old were excluded because we suspect that patients undergoing arthroplasty at such a young age may be inherently different from the older population that typically undergoes shoulder arthroplasty. The CPT codes (23473 and 23474) and International Classification of Diseases, Ninth Revision (ICD-9) codes (P-81.97) for revision shoulder arthroplasty were searched. The type of procedure performed, date, and gender were identified for each patient.
To assess rates of each complication, ICD-9 and ICD-10 codes were queried for surgical site infection, stiffness, dislocation, nerve injury, acute kidney injury, cardiac arrest, deep vein thrombosis, pneumonia, pulmonary embolism, urinary tract infection, dehiscence, hematoma, and transfusion (Table 1). Risk factors examined included smoking status at the time of revision, depression, gender, renal failure, age, overweight status, and diabetes. The Charlson Comorbidity Index (CCI) was calculated for all patients [4], and this was also investigated as a risk factor for revision shoulder arthroplasty. Additionally, for patients who had revision shoulder arthroplasty between 2013 and 2016, the database was searched for any prior shoulder arthroplasties for those patients, in order to determine the time between index procedure and revision. The incidence of these diagnoses within 90 days of the revision shoulder arthroplasty was determined.
Table 1.
International Classification of Diseases, Ninth and Tenth Revisions (ICD-9 and ICD-10) codes searched for complications associated with revision shoulder arthroplasty
| Complication | ICD codes |
|---|---|
| Surgical site infection | ICD-9: 73001, 73011, 73021, 73091, 73081, 99666, 99667, 99851, 99859; ICD-10: K6811, M86119, M86219, M86619, M869, M90819, T814XXA, T8450XA, T8460XA, T847XXA |
| Stiffness | ICD-9: 71950, 71951; ICD-10: M2560, M25619 |
| Dislocation | ICD-9: 71821, 71831, 83100, 83109; ICD-10: M24419, M24319, S43006A, S43086A |
| Nerve injury | ICD-9: 3449, 34440, 34441, 34442, 7814, 907, 9550, 9551, 9552, 9553, 9554, 9555, 9556, 9557, 9558, 9559, |
| ICD-10: S4400XA, S4410XA, S4420XA, S4430XA, S4440XA, S4450XA, S5400XA, S5410XA, S5420XA, S5430XA, S6400XA, S6410XA, S6420XA, S6430XA, S6440XA, S448X9A, S4490XA | |
| Acute kidney injury | ICD-9: 5845, 5846, 5847, 5848, 5849, ICD-10: N170, N171, 172, 178, 179 |
| Cardiac arrest | ICD-9: 4275, 42741; ICD-10: I469, I4901 |
| Deep vein thrombosis | ICD-9: 4532, 4533, 4534, 45382, 45384, 45385, 45386; ICD-10: I82220, I82221, I823, I82629, I82A19, I82B19, I82C19 |
| Pneumonia | ICD-9: 4800, 4809, 481, 4820, 4821, 48230, 48231, 48232, 48239, 48240, 48241, 48242, 48249, 48281, 48282, 48283, 48284, 48289, 4829, 4830, 4831, 4838, 4841, 4843, 4845, 4846, 4847, 4848, 485, 486; ICD-10: A221, A3791, A481, B250, B440, J120, J121, J122, J1281, J1289, J129, J13, J181, J150, J151, J14, J154, J153, J1520, J15211, J15212, J1529, J154, J155, J156, J157, J158, J159, J160, J168, J17, J180, J189, J399 |
| Pulmonary embolism | ICD-9: 4151; ICD-10: I2690, II2699, T800XXA, T81718A, T8172XA, T82817A, T82818A |
| Urinary tract infection | ICD-9: 5990; ICD-10: N390 |
| Dehiscence | ICD-9: 99830,99831, 99832, 99833 |
| Hematoma | ICD-9: 99811, 99812, 99813; ICD-10: T8130XA, T8131XA, T8132XA, T8133XA |
| Transfusion | ICD-9: 9904; ICD-10: 30233N1, 30233P1, 30243N1, 30243P1, 30253N1, 30253P1, 30263N1, 30263P1 |
Statistical Analysis
The odds ratio (OR) was calculated for each risk factor by dividing the odds of undergoing a revision with a risk factor by the odds of undergoing a revision without the risk factor. Multivariate logistic regression was performed to test the significance of risk factors within the PearlDiver program. The R open source statistical software was used with the PearlDiver program, and p < 0.05 was considered statistically significant.
Results
A total of 824 patients undergoing revision shoulder arthroplasty were identified within the 4-year period from 2013 to 2016. The incidence of revision shoulder arthroplasties in that period did not increase with time (Fig. 1). Female patients accounted for 55.5% of the revisions. The ages of the patients undergoing revision arthroplasty are shown in Fig. 2. Eighty-seven patients (10.5%) had infections prior to revision and 133 patients (16.1%) had dislocations prior to revision. Of the revisions queried, 52% occurred within 180 days of the index shoulder arthroplasty, 91% occurred within 3 years, and all revisions occurred within 7 years (Fig. 3). Of the risk factors examined, smoking was associated with the highest odds ratio (8.1) for revision. Additionally, depression, CCI, male gender, renal failure, and diabetes were significant risks factors for revision, with ORs of 6.3, 4.7, 4.4, 2.4, and 1.9, respectively (Table 2). Older age and overweight were not found to correlate with increased risk of undergoing revision shoulder arthroplasty.
Fig. 1.
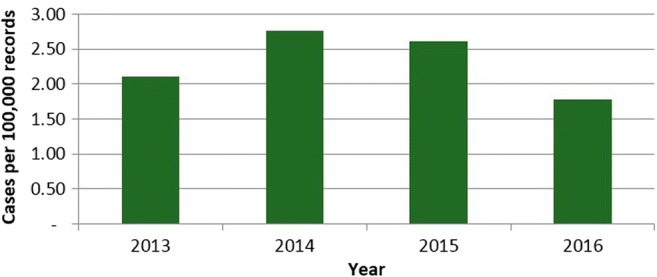
Incidence of revision shoulder arthroplasty by year from 2013 to 2016 in private insurance database.
Fig. 2.
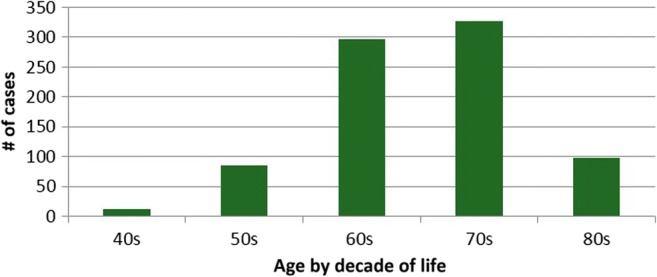
Distribution of revision shoulder arthroplasty procedures by age for 824 patients in private insurance database from 2013 to 2016.
Fig. 3.
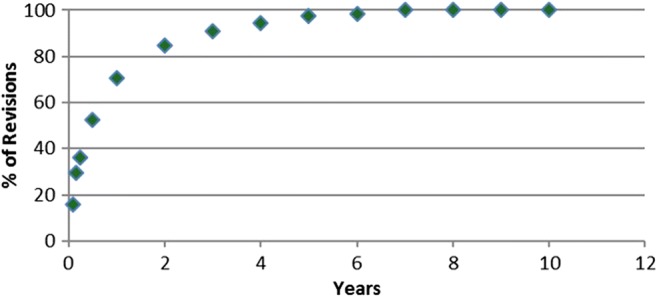
Time between primary arthroplasty and revision arthroplasty procedures. Eighty-five percent of revisions were performed by 2 years post-operatively, and all revisions in this database were performed by 7 years post-operatively.
Table 2.
Calculated odds ratios of various risk factors for revision total shoulder arthroplasty
| Risk factor | Odds ratio | p value |
|---|---|---|
| Smoking | 8.1 | < 0.001 |
| Depression | 6.3 | < 0.001 |
| Charlson Comorbidity Index | 4.7 | < 0.001 |
| Male gender | 4.4 | < 0.001 |
| Renal failure | 2.4 | 0.01 |
| Diabetes | 2.0 | 0.05 |
Of patients undergoing revision shoulder arthroplasty, 8.8% were readmitted to the hospital within 30 days of surgery, and 15.8% within 90 days. The most common complication within 90 days of revision shoulder arthroplasty was surgical site infection, affecting 10.9% of patients. Dislocation was found in 5.7% of patients, and stiffness was found in 4.6% of patients. In terms of medical complications, 6% of patients had a urinary tract infection, 3.2% had acute kidney injury, and 3.4% had pneumonia within 90 days of surgery (Table 3). Queries for nerve injury, cardiac arrest, thromboembolic events, and wound dehiscence did not return a sufficient number of patients; any queries resulting in fewer than 11 patients have results concealed to protect patient privacy.
Table 3.
Complications affecting patient undergoing revision total shoulder arthroplasty
| Complication | No. of patients | % of revision total shoulder arthroplasty patients |
|---|---|---|
| Surgical site infection | 90 | 10.9 |
| Urinary tract infection | 49 | 5.9 |
| Dislocation | 47 | 5.7 |
| Stiffness | 38 | 4.6 |
| Pneumonia | 28 | 3.4 |
| Acute kidney injury | 26 | 3.2 |
| Hematoma | 14 | 1.7 |
| Transfusion | 14 | 1.7 |
In the time period studied, 12,232 patients underwent primary shoulder arthroplasty and 89 patients underwent more than one revision shoulder arthroplasty. The two risk factors that were predictive of a second revision were renal failure (OR 3.66, p < 0.001) and smoking (OR 3.90, p < 0.001). CCI, diabetes, depression, age, gender, and overweight status were not associated with risk of second revision.
Discussion
We examined 824 cases of revision shoulder arthroplasty performed over a 4-year period and found that patients who were male or had comorbidities of smoking, renal failure, depression, diabetes, or overall higher CCI were at increased risk of revision shoulder arthroplasty. The most common complication following revision arthroplasty was surgical site infection. It should be noted that while 55.5% of revisions were in female patients, male gender was still found to be a risk factor due to the higher number of female patients undergoing primary shoulder arthroplasty.
This study is not without limitations. The use of a database of millions of orthopedic patients confers a level of statistical power to this study that simply cannot be achieved in conventional chart review studies [21]. Still, there are obvious limitations to this study inherent in the study design. Although the study included a search of over 11 million records across the USA, our results did not necessarily provide a representative sample of the US population. The patients included were insured by private insurers, indicating a cohort that may have better access to care than the population as a whole [9]. In addition, patient-specific information, operative report details, post-operative rehabilitation protocols, and outcomes data were unavailable. Thus, we were unable to determine whether a specific problem such as infection or dislocation directly contributed to the decision for revision. Also, data regarding regional differences in potential confounding factors such as body mass index and smoking habits was not available (it was determined whether patients were smokers but not how often and for how long they had smoked), and as with any database search using billing codes, the results are subject to error introduced by improper coding [13].
With regard to the complication rates, it is difficult to assess the rate of complications not requiring operative intervention, as more common issues such as stiffness may have simply been observed and not entered into the database. Furthermore, laterality is not known for patients with an ICD-9 code. Thus, we are unable to ascertain that a revision procedure definitively corresponds to the primary procedure during the study period. Also, for patients who underwent more than one revision, we cannot determine with certainty whether they underwent bilateral revisions or serial revisions in the same shoulder. Unfortunately, while we are able to ascertain the total number of shoulder arthroplasty procedures in the study period, as well as the total number of revision procedures, we are unable to calculate the revision rate because the primary procedures for which the revisions are reported were not necessarily in the time period of the study and vice versa. Likewise, we are unable to determine with certainty whether medical diagnoses such as urinary tract infection and pneumonia were related to the revision arthroplasty procedure. Additionally, because this database has data starting in 2007, information was not available regarding the timing of primary shoulder arthroplasties in all of the patients. Thus, if the primary arthroplasty occurred prior to 2007 or while the patient was covered by another insurance plan, we were unable to determine the duration of time from primary arthroplasty to revision.
Recently, Boddapati and colleagues employed the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database to examine the differences in complication rate between 10,371 primary and 496 revision total shoulder arthroplasties [2]. They reported an overall complication rate of 6.5% in primary arthroplasty and 10.7% in revision cases. Furthermore, they reported that age over 75 years, female gender, diabetes, chronic obstructive pulmonary disease, and American Society of Anesthesiologists classification of 3 or higher were associated with increased risk of any complication; smoking was associated with increased risk of wound complications. We found that diabetes was a risk factor for revisions, as was male gender. While Boddapati found a higher complication rate in females, these complications may not have led to revisions.
Schwartz et al. examined the National Hospital Discharge Database from 2001 to 2010 and found 1297 patients who had undergone primary total shoulder arthroplasties and 184 who had undergone revision total shoulder arthroplasties, as well as significantly increasing rates of both procedures over time [17]. Unlike our study, theirs found no differences due to gender but did find that patients undergoing primary procedures were older. Some of these differences may be attributable to the time period queried. Additionally, in recent years, more outpatient shoulder arthroplasties have been performed in carefully selected patients, which may not be captured in hospital discharge data. Matsen et al. analyzed data from the New York Statewide Planning and Research Cooperative System database on 457 cases of revision surgery among 17,311 index shoulder arthroplasties and found younger age groups and Hispanic populations to have the highest hazard ratios for revision surgery [10]. Our study found younger patients to have significantly reduced rates of revision, while older populations had the highest rates. This difference may be due to the present study’s exclusion of patients under age 40. Matsen et al. found that trauma, osteoarthritis, and inflammatory arthritis were the diagnoses with the greatest hazard ratios (3.16, 1.61, 1.60, respectively) for revision surgery [10], while our study found infection to be the diagnosis most associated with revision surgery. Geographic variability may be a key factor in differences in reported data. The rate of infection after primary or revision shoulder arthroplasty has not changed from 2002 to 2011, but more procedures are being performed and there is consequently a higher number of patients with infected arthroplasty, resulting in a greater economic burden attributed to infection overall [14]. Our finding of infection as the diagnosis most commonly associated with revision shoulder arthroplasty may further support this notion. Specific to explanted reverse total shoulder arthroplasties, a series of 50 retrieved implants had an average term of implantation of 20 months, with a range of 0 to 81 months [19], which is consistent with our study results.
Overall, we found that 70.4% of revision shoulder arthroplasties occurred within the first year following the index procedure, 84.8% by the second year, and 90.9% by the third year. With the limitations of the database in mind, this data suggests that there may be little use in following revision arthroplasty patients past 7 years post-operatively, given the small number of revisions occurring after 5 years.
In conclusion, despite the limitations inherent in most database studies [13], there is important information to be gleaned from our study. Overall, the incidence of revision shoulder arthroplasty in the patient population studied was relatively low. We found that patients who were male or had comorbidities of smoking, renal failure, depression, diabetes, or overall higher CCI were at increased risk of revision shoulder arthroplasty, and that surgical site infection was the most common complication following revision. Additionally, renal failure and smoking were risk factors for more than one revision. The information gleaned from this study may be useful in counseling patients on the likelihood they might require revision shoulder arthroplasty. These data may also be applied as a benchmark for the evaluation of newly adopted practices and technologies. Future studies are warranted to further study risk factors for multiply revised shoulder arthroplasties.
Electronic Supplementary Material
(PDF 153 kb)
Compliance with Ethical Standards
Conflict of Interest
Natalie L. Leong, MD, Shelby Sumner, MPH, and Ani Gowd, BS, declare that they have no conflicts of interest. Anthony A. Romeo, MD, reports personal fees from AANA and MLB; grants and personal fees from Arthrex; grants from Aesculap/B. Braun, Histogenics, Medipost, NuTech, OrthoSpace, Smith & Nephew, and Zimmer; royalties and personal fees from Saunders/Mosby-Elsevier; board membership, royalties, and financial support from SLACK Incorporated; board membership in AOSSM, ASES, Atreon Orthopaedics, Orthopedics Today, SAGE, and Wolters Kluwer Health-Lippincott Williams & Wilkins, outside the submitted work. Gregory P. Nicholson, MD, reports personal fees from Tornier, Innomed, Arthrosurface, and Wright Medical, and board membership from American Shoulder and Elbow Society, outside the submitted work. Nikhil N. Verma, MD, reports personal fees from MLB; grants from OrthoSpace, Mitek, Arthrex, Arthrosurface, Inc, DJ Orthopedics, Ossur, Athletico, ConMed Linvatec, and Miomed; publishing royalties and editorial board membership from Arthroscopy; stock or stock options from Cymedica and Omeros; stock or stock options and personal fees from Minivasive; grants, personal fees, and royalties from Smith & Nephew; personal fees and publishing royalties from Vindico Medical-Orthopedics Hyperguide; board membership in Arthroscopy Association Learning Center Committee, AOSSM, ASES, Journal of Knee Surgery, and SLACK Incorporated, all outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level IV: prognostic, retrospective study
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
5/1/2019
The name of author Anirudh K. Gowd was listed incorrectly in the original article. It is corrected here.
References
- 1.Bansal Ankit, Khatib Omar N., Zuckerman Joseph D. Revision Total Joint Arthroplasty: The Epidemiology of 63,140 Cases in New York State. The Journal of Arthroplasty. 2014;29(1):23–27. doi: 10.1016/j.arth.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 2.Boddapati V, Fu MC, Schairer WW, Gulotta LV, Dines DM, Dines JS. Revision total shoulder arthroplasty is associated with increased thirty-day postoperative complications and wound infections relative to primary total shoulder arthroplasty. HSS J. 2018;14(1):23–28. doi: 10.1007/s11420-017-9573-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bohsali KI, Bois AJ, Wirth MA. Complications of shoulder arthroplasty. J Bone Joint Surg Am. 2017;99(3):256–269. doi: 10.2106/JBJS.16.00935. [DOI] [PubMed] [Google Scholar]
- 4.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 5.Coste JS, Reig S, Trojani C, Berg M, Walch G, Boileau P. The management of infection in arthroplasty of the shoulder. J Bone Joint Surg Br. 2004;86(1):65–69. doi: 10.1302/0301-620X.86B1.14089. [DOI] [PubMed] [Google Scholar]
- 6.Day JS, Lau E, Ong KL, Williams GR, Ramsey ML, Kurtz SM. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg. 2010;19(8):1115–1120. doi: 10.1016/j.jse.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 7.Hollatz MF, Stang A. Nationwide shoulder arthroplasty rates and revision burden in Germany: analysis of the national hospitalization data 2005 to 2006. J Shoulder Elbow Surg. 2014;23(11):e267–274. doi: 10.1016/j.jse.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 8.KUMAR SANJAY, SPERLING JOHN W., HAIDUKEWYCH GEORGE H., COFIELD ROBERT H. PERIPROSTHETIC HUMERAL FRACTURES AFTER SHOULDER ARTHROPLASTY. The Journal of Bone and Joint Surgery-American Volume. 2004;86(4):680–689. doi: 10.2106/00004623-200404000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Leong Natalie L., Cohen Jeremiah R., Lord Elizabeth, Wang Jeffrey C., McAllister David R., Petrigliano Frank A. Demographic Trends and Complication Rates in Arthroscopic Elbow Surgery. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2015;31(10):1928–1932. doi: 10.1016/j.arthro.2015.03.036. [DOI] [PubMed] [Google Scholar]
- 10.Matsen Frederick A., Li Ning, Gao Huizhong, Yuan Shaoqing, Russ Stacy M., Sampson Paul D. Factors Affecting Length of Stay, Readmission, and Revision After Shoulder Arthroplasty. The Journal of Bone and Joint Surgery. 2015;97(15):1255–1263. doi: 10.2106/JBJS.N.01107. [DOI] [PubMed] [Google Scholar]
- 11.Miller BS, Joseph TA, Noonan TJ, Horan MP, Hawkins RJ. Rupture of the subscapularis tendon after shoulder arthroplasty: diagnosis, treatment, and outcome. J Shoulder Elbow Surg. 2005;14(5):492–496. doi: 10.1016/j.jse.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 12.Moeckel B H, Altchek D W, Warren R F, Wickiewicz T L, Dines D M. Instability of the shoulder after arthroplasty. The Journal of Bone & Joint Surgery. 1993;75(4):492–497. doi: 10.2106/00004623-199304000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Montgomery SR, Foster BD, Ngo SS, et al. Trends in the surgical treatment of articular cartilage defects of the knee in the United States. Knee Surg Sports Traumatol Arthrosc. 2014;22(9):2070–2075. doi: 10.1007/s00167-013-2614-9. [DOI] [PubMed] [Google Scholar]
- 14.Padegimas Eric M., Maltenfort Mitchell, Ramsey Matthew L., Williams Gerald R., Parvizi Javad, Namdari Surena. Periprosthetic shoulder infection in the United States: incidence and economic burden. Journal of Shoulder and Elbow Surgery. 2015;24(5):741–746. doi: 10.1016/j.jse.2014.11.044. [DOI] [PubMed] [Google Scholar]
- 15.Raiss P, Bruckner T, Rickert M, Walch G. Longitudinal observational study of total shoulder replacements with cement: fifteen to twenty-year follow-up. J Bone Joint Surg Am. 2014;96(3):198–205. doi: 10.2106/JBJS.M.00079. [DOI] [PubMed] [Google Scholar]
- 16.SANCHEZ-SOTELO JOAQUIN, SPERLING JOHN W., ROWLAND CHARLES M., COFIELD ROBERT H. INSTABILITY AFTER SHOULDER ARTHROPLASTY. The Journal of Bone and Joint Surgery-American Volume. 2003;85(4):622–631. doi: 10.2106/00004623-200304000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Schwartz Brian E., Savin David D., Youderian Ari R., Mossad David, Goldberg Benjamin A. National trends and perioperative outcomes in primary and revision total shoulder arthroplasty. International Orthopaedics. 2014;39(2):271–276. doi: 10.1007/s00264-014-2614-5. [DOI] [PubMed] [Google Scholar]
- 18.Sperling JW, Kozak TK, Hanssen AD, Cofield RH. Infection after shoulder arthroplasty. Clin Orthop Relat Res. 2001;382:206–216. doi: 10.1097/00003086-200101000-00028. [DOI] [PubMed] [Google Scholar]
- 19.Wiater BP, Baker EA, Salisbury MR, Koueiter DM, Baker KC, Nolan BM, Wiater JM. Elucidating trends in revision reverse total shoulder arthroplasty procedures: a retrieval study evaluating clinical, radiographic, and functional outcomes data. J Shoulder Elbow Surg. 2015;24(12):1915–1925. doi: 10.1016/j.jse.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 20.Yeranosian MG, Petrigliano FA, Terrell RD, Wang JC, McAllister DR. Incidence of postoperative infections requiring reoperation after arthroscopic knee surgery. Arthroscopy. 2013;29(8):1355–361. doi: 10.1016/j.arthro.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 21.Yeranosian Michael G., Arshi Armin, Terrell Rodney D., Wang Jeffrey C., McAllister David R., Petrigliano Frank A. Incidence of Acute Postoperative Infections Requiring Reoperation After Arthroscopic Shoulder Surgery. The American Journal of Sports Medicine. 2013;42(2):437–441. doi: 10.1177/0363546513510686. [DOI] [PubMed] [Google Scholar]
- 22.Young AA, Walch G, Pape G, Gohlke F, Favard L. Secondary rotator cuff dysfunction following total shoulder arthroplasty for primary glenohumeral osteoarthritis: results of a multicenter study with more than five years of follow-up. J Bone Joint Surg Am. 2012;94(8):685–693. doi: 10.2106/JBJS.J.00727. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 153 kb)


