Abstract
Objective
To present the diagnostic and clinical features of musculocutaneous neuropathy, propose possible conservative management strategies, and create awareness of this rare condition.
Case presentation
We present the case of a 24-year old competitive soccer athlete, who sought care for an unrelated lower extremity complaint. Upon examination, significant wasting of the right biceps was noted. The patient reported right arm pain and weakness that began six months prior, following a long sleep with his arm beneath him. Neurological examination revealed an absent deep tendon reflex of C5 on the right, diminished sensation on the right anterolateral forearm, and significant weakness in muscle testing of the biceps brachii on the right. The patient was referred to a neurologist to confirm suspicion of a musculocutaneous nerve injury. Electromyography and magnetic resonance imaging confirmed the diagnosis of musculocutaneous neuropathy and ruled out other differential diagnoses. The patient is currently awaiting confirmation to determine if he is a surgical candidate for a nerve transfer.
Summary
Musculocutaneous neuropathy is a rare condition. Recognition of the clinical presentation of this condition is important for early diagnosis and prompt intervention.
Keywords: chiropractic, atrophy, biceps, musculocutaneous nerve, neuropathy, weakness
Abstract
Objectif
Présenter les caractéristiques diagnostiques et cliniques de la neuropathie musculo-cutanee, proposer des stratégies de prise en charge conservatrices possibles et sensibiliser la population à cette maladie rare.
Présentation de cas
Nous présentons le cas d’un athlète de 24 ans pratiquant le soccer en compétition qui a reçu des soins pour une douleur d’un membre inférieur sans lien avec sa pratique sportive. L’examen a révélé une perte importante du biceps droit. Le patient a rapporté des douleurs et des faiblesses localisées au bras droit qui se sont manifestées six mois auparavant, après un long sommeil avec son bras positionné sous son corps. L’examen neurologique a révélé l’absence d’un réflexe tendineux profond de niveau C5 du tendon droit, une diminution de la sensation sur l’avant-bras antérolatéral droit et une faiblesse significative dans le test musculaire. Le patient a été envoyé chez un neurologue pour confirmer les soupçons d’une lésion du nerf musculo-cutané. L’électromyographie et l’imagerie par résonance magnétique ont confirmé le diagnostic de neuropathie musculo-cutanée et exclu d’autres diagnostics différentiels. Le patient attend actuellement une confirmation pour déterminer s’il est un candidat chirurgical à la réalisation d’un transfert de nerfs.
Résumé
La neuropathie musculo-cutané est une maladie rare. La reconnaissance de la présentation clinique de cette condition est importante pour un diagnostic précoce et une intervention rapide.
MOTS CLÉS: chiropratique, atrophie, biceps, nerf musculo-cutané, neuropathie, faiblesse
Introduction
Isolated injury to the musculocutaneous nerve is a rare occurrence. Associated signs and symptoms of an isolated musculocutaneous neuropathy may include weakness in elbow flexion or shoulder flexion, atrophy of the biceps brachii, and pain or paresthesia at the lateral forearm. Previous case studies have reported this condition following strenuous activity, trauma, in athletes who engaged in repetitive or contact sports, caused by anatomical anomalies, and following surgery to an unrelated body part.1–8 We report a case of musculocutaneous neuropathy following prolonged position of the arm beneath the body during sleep. It is important to understand the clinical presentation and diagnostic criteria to allow early diagnosis and intervention in this condition.
Case presentation
A healthy 24-year-old university student and competitive soccer player presented to the chiropractic clinic to undertake rehabilitation after dislocating his ankle which occurred six months prior while playing soccer. During this visit, the patient also complained of right shoulder and arm pain which began shortly after the ankle injury. At the time of the dislocation, he presented to a local emergency room department where the ankle was reduced. He was sent home with narcotic analgesics (acetaminophen with codeine). No other follow-up was suggested or arranged. He reported that he fell asleep on the couch lying on his right side with his right arm underneath his body. The following morning, he woke up after a 10-hour sleep with intense burning, tingling, numbness, and pain in the entire upper limb. He was unable to move his arm due to pain. He also reported significant neck pain and stiffness. He had no significant history of previous neck or upper limb injuries, and denied any prior neurological conditions. In the weeks following his injury, some of the symptoms improved – tingling and burning subsided, the intensity of the pain diminished, and numbness localized to the lateral aspect of the forearm primarily. He recovered some movement in his right upper limb at the elbow, but complained of weakness especially with lifting and push-ups. The patient had not noticed any muscle atrophy.
On observation, he was a tall lean male with visible atrophy of the right biceps, which was noticed on the first visit. There was no other muscle wasting noted elsewhere on the arm or forearm. The patient had full range of motion at the elbow. The deep tendon reflex (DTR) at the elbow over the biceps tendon was absent on the right, while all remaining upper limb DTR’s were found to be 2+. During sensory examination, he was unable to distinguish sharp and dull sensation located to the right anterolateral forearm, over the territory of the right lateral antebrachial cutaneous nerve, a branch of the musculocutaneous nerve. Active and passive range of motion of the elbow was full. There was significant weakness during manual muscle testing of the biceps, which was tested with the elbow flexed to ninety degrees and with the forearm supinated. Using McGee’s grading system for manual muscle testing, the patient was able to generate grade 4/5 strength in elbow flexion but it appeared to come entirely from brachioradialis contraction, as there was no fasciculation noted in the biceps muscle during testing.
Following this examination, the patient was referred to his family physician for consideration of a neurologist referral, to confirm our suspicion of a musculocutaneous nerve lesion as the chiropractor believed manual therapy and rehabilitation for the nerve would have been futile due to the advanced findings. The family physician referred the patient to a neurologist who confirmed our physical examination findings and ordered an electromyography (EMG) test and an MRI of the cervical spine and brachial plexus. The nerve conduction study showed an absent lateral antebrachial sensory response and during needle examination the right biceps showed no voluntary activity, but frequent fibrillation potentials. MRI of the cervical spine and brachial plexus was unremarkable. Based on these results the neurologist diagnosed this patient with a right musculocutaneous neuropathy. At the time of writing this case, the patient was waiting to determine if he was a surgical candidate for a possible nerve transfer. The time frame in which this diagnosis was reached, following the referral to the neurologist, took approximately six months. This was one year from the original insult.
Discussion
Anatomy and etiology
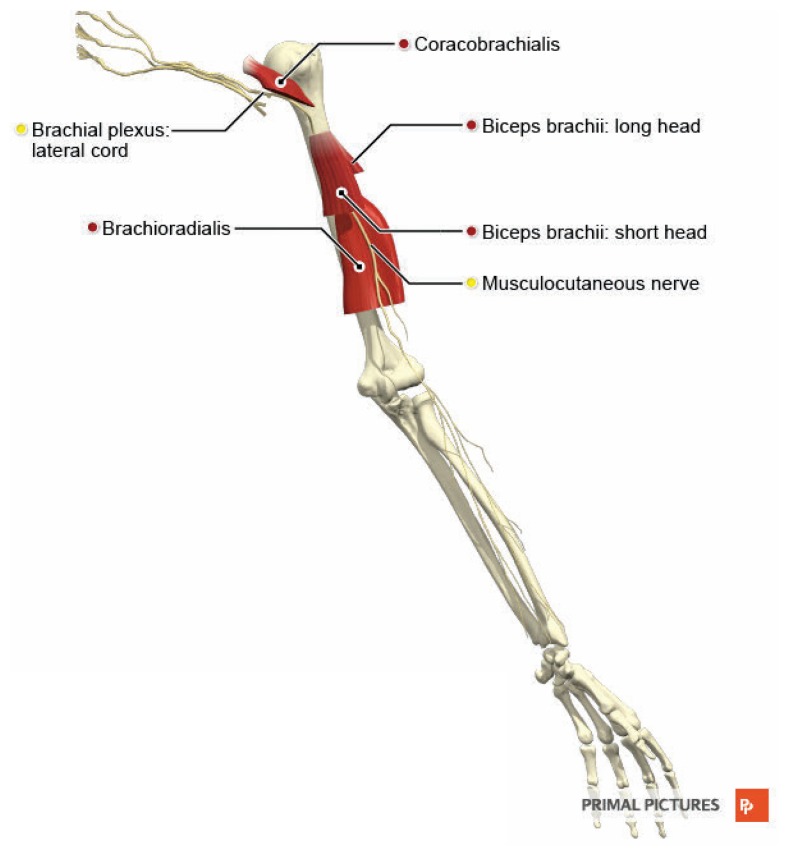
The musculocutaneous nerve is the terminal branch of the lateral cord of the brachial plexus. It receives fibres from the C5, C6, and C7 nerve roots. It branches off the lateral cord just distal to the coracoid process and exits the axilla by piercing the coracobrachialis (see Figure 1).9 It descends between the biceps brachii and brachialis, supplying both muscles. At the cubital fossa, specifically at the lateral margin of the biceps aponeurosis, it pierces the cutaneous fascia and continues as the lateral cutaneous nerve of the forearm, supplying sensory innervation to the skin of the lateral forearm.1
Figure 1.
Illustration of the musculocutaneous nerve and surrounding anatomy in the arm.
(© Informa UK Ltd (trading as Primal Pictures), 2020. Primal Pictures, an informa business www.primalpictures.com)
In the current literature, there are few reports of isolated musculocutaneous nerve injury. The clinical presentation of musculocutaneous nerve lesions in the literature is quite variable. Most case reports documented the following physical examination findings: grade 3 or 4 weakness in elbow flexion with motor testing, atrophy of the right biceps brachii, diminished deep tendon reflexes at C5, and paresthesia and/or sensory deficit at the anterolateral aspect of the forearm.1–3,6–8,10,11
Physical examination
Neurodynamic testing challenges the physical capabilities of the peripheral nervous system using multi-joint movements of the limbs in order to alter the length of the nerve.12 A “positive” test may suggest increased mechanosensitivity in neural tissues and the following have been proposed to distinguish a positive response: reproduction of the patient’s symptoms with movement of a distal body segment, differences (i.e. aching, burning, tingling, etc.) between involved and uninvolved side, and alteration in resistance perceived by the examiner.12 Positioning of the patient for nerve tension testing of the musculocutaneous nerve would include the following: shoulder girdle depression, elbow extension, shoulder extension, ulnar deviation of the wrist with thumb flexion, and either medial or lateral rotation of the arm. Palpation of the nerve (sustained or unsustained) and isometric contraction of a muscle supplied by the nerve may also identify enhanced mechanical sensitivity in neural structures.12–14
Manual muscle strength testing (MMST) can be a useful diagnostic tool to determine impairments in the strength of muscles that are innervated by the musculocutaneous nerve, including the biceps brachii, brachialis, and coracobrachialis. MMST is graded on a scale of 0 – 5 and descriptors of each grade are described as follows.15 A grade of 5 is assigned when the therapist cannot break the patient’s hold position when applying maximum resistance. Grade 4 designates a muscle that is able to complete a full range of motion against gravity but not able to hold the position against maximum resistance. A grade of 3 is assigned when the muscle can complete a full range of motion against gravity, but not additional resistance. Grade 2 designates muscle strength in a muscle that can complete a full range of motion in a position that minimizes gravity. A grade of 1 means some contractile activity is visible or palpable, however movement is not generated. Lastly, a grade 0 muscle is completely inert on palpation.
Tinel’s test is commonly used as a provocative test in peripheral neuropathy, however there is no specific literature on this test in musculocutaneous nerve entrapments. Tinel’s sign is the sensation of tingling felt at the site of the lesion or distally along the course of the nerve when it is percussed, particularly in the corresponding cutaneous distribution of the nerve.16 In musculocutaneous neuropathy, if the nerve is percussed at the suspected lesion site (e.g. where it pierces the coracobrachialis), tingling at the anterolateral forearm would indicate a positive Tinel’s sign.
Mechanism of injury
The mechanism of injury for musculocutaneous neuropathy described in the literature varies. Some describe iatrogenic causes secondary to prolonged positioning of the arm during an unrelated surgery, or direct injury to the nerve during surgery.1,17 Repetitive, vigorous upper extremity activity (e.g. lifting, throwing, or carrying), or a single forceful extension of the upper extremity (e.g. pushing or wrestling) are more commonly cited mechanisms of injury.2–4,6,7,10,18 Most reported injuries to the musculocutaneous nerve occur proximal to the biceps and brachialis muscles, most commonly at the coracobrachialis muscle, due to hypertrophy or strong contraction of the muscle, resulting in mechanical and/or ischemic nerve injury.3,4,10
Peripheral nerve injuries range in severity from neuropraxia to axonotmesis to neurotmesis.19 Neuropraxia injuries are most common, and involve a conduction block of motor or sensory function without damage to the neural elements and with intact connective tissue sheaths. This usually occurs due to compression, mild crush, traction, or local ischemia.20 Axonotmesis results in axonal injury and distal axon degeneration with an intact connective tissue sheath, and usually follows a more severe trauma which causes a crush injury.19 Neurotmesis is complete disruption of the nerve and nerve sheath caused by a transection or laceration of the nerve.19,21
Nerve regeneration and repair processes occur differ ently depending on the severity of the injury. With lesions that involve less than 20–30% of the axons, collateral sprouting from surviving axons occurs over 2–6 months.22 When more than 90% of axons are injured, nerve tissue regenerates from the injury site, and rate of recovery depends on the distance to the injury site. Proximal injuries can be problematic due to the longer distance to re-innervate distal muscles, and the regeneration and repair phases continue for months.22 Peripheral nerve regeneration typically occurs at a rate of 1–2mm per day.23,24
Differential diagnoses
Differential diagnoses for musculocutaneous nerve injuries include biceps tendon injury or rupture, strain or tear of the biceps or brachialis muscles, C5 or C6 radiculopathy, and brachial plexus injury.2,3,6,11,21 There are some specific signs and symptoms to be aware of to aid in differentiating the listed potential diagnoses. Biceps tendon injuries would present without sensory changes.2,6 Loss of contour of the biceps muscle belly, possible bunching of the muscle belly superiorly, and absence of the tendon in the antecubital fossa would also help differentiate a biceps tendon rupture.7 A diagnosis of C5 or C6 radiculopathy would present with pain and/or weakness in the sensory and motor distribution of the musculocutaneous nerve, but would also include weakness of other muscles supplied by the C5 or C6 nerve root, including serratus anterior, pectoralis major, and deltoid as well as neck pain.25 In addition, radicular pain may be exacerbated by manoeuvers that irritate the involved nerve root, such as coughing, sneezing, Valsalva, and certain movements and positions of the cervical spine.25 A brachial plexus injury would typically present with a wider distribution of sensory and motor involvement in the upper extremity, which could be confirmed with electrophysiological testing.
Diagnostic testing
While upper extremity entrapment neuropathies are typically diagnosed during the clinical assessment, a variety of diagnostic testing modalities can help to confirm clinical suspicion.26 Electrophysiological studies such as electromyography and nerve conduction studies can usually determine the location and severity of the injury, however they are mildly invasive, operator dependent, and are unable to determine structural causes of denervation.26,27 Ultrasonography and magnetic resonance imaging may be used to confirm the location and etiology of the nerve compression, or establish an alternative diagnosis.26
Motor and sensory nerve conduction studies (NCS) of the musculocutaneous nerve have been described in the literature. Standard techniques involve the measurement of nerve response amplitude and conduction velocity along the course of the nerve.28 Needle electromyography (EMG) involves inserting a fine needle electrode into the muscle. EMG may identify the presence of denervated muscles, showing absence or reduction of motor unit recruitment during voluntary movement, and fibrillation potentials at rest.29
Electrodiagnostic studies (NCS and EMG) should be performed 10–21 days after a peripheral nerve injury. At this time, the extent of axonal loss can be assessed and the extent of the lesion can be distinguished.28 Electrodiagnostic findings in musculocutaneous neuropathy may include absent lateral antebrachial cutaneous nerve and musculocutaneous motor responses and EMG abnormalities at the biceps brachii and brachialis, as well as coracobrachialis depending on the location of the lesion.5
Magnetic resonance imaging (MRI) can useful in demonstrating specific muscle denervation patterns, as it can identify muscle edema within 24–48 hours of denervation as well as map out denervated muscles in order to localize entrapment or compressive neuropathies.30 With chronic denervation, fatty atrophy of the muscle is demonstrable months later.31 In musculocutaneous nerve injuries, the nerve itself likely will not be visualized, however edema in the coracobrachialis, brachialis, and/or biceps brachii muscles would suggest involvement of the nerve.26 With muscle edema, MRI findings include increased signal intensity on T2-weighted images superimposed on an otherwise normal appearance of the involved muscle.32 Fatty infiltration is usually seen in association with muscle atrophy. MRI findings include increased quantities of fat with characteristic signal intensity within the involved muscle, usually with a decreased volume of muscle tissue.32 T1-weighted images are most reliable in revealing chronic muscle denervation changes.32 Due to the rarity of isolated musculocutaneous nerve injury, the literature on imaging findings is limited. However, we may be able to extrapolate findings from different peripheral nerve injuries.
Ultrasound is a cost-efficient, quick, non-invasive modality. It allows for dynamic evaluation and visualization of long nerve segments, however it can only depict superficially located nerves. 26 It can also be used to either demonstrate or rule out biceps tendon injury.
Magnetic resonance neurography (MRN) is a relatively new imaging modality that has been used to confirm clinical suspicion of peripheral neuropathy by clearly depicting peripheral nerve anatomy and pathology.33 MRN can demonstrate a nerve abnormality, nerve entrapment or impingement lesions, and diffuse peripheral nerve lesions, as well as detect incidental lesions that mimic neuropathy symptoms, or exclude a neuropathy diagnosis by showing normal nerves and muscles.33,34 MRN can reveal the morphological characteristics of nerves, such as calibre, contour, and continuity as well as relationships to other nerves or other non-neural structures such as muscle or bone.34 The technique uses a combination of two- and three-dimensional and diffusion imaging pulse sequences in order to image nerves directly.35 Injured nerves typically exhibit a hyperintense signal on T2-weighted images within 24 hours of the insult and the pattern is different for Sunderland Class I–V injuries.35,36 Class I–III injuries show a uniform hyperintense signal, Class IV injuries show a heterogenous nerve signal with focal fascicular abnormality, and Class V injuries show a discontinuous nerve.35 Muscle denervation typically occurs distal to the site of the injury, resulting in edema and atrophy, important findings in the diagnosis of neuropathy.35,37
Abnormally high signals in nerve fascicles correlate well with abnormal EMG/NCS studies that demonstrated nerve injuries such as traumatic injuries, compression neuropathies, or peripheral nerve tumours.34 These findings may significantly influence the management of peripheral neuropathies, as more severe injuries/conditions will likely be unresponsive to conservative care and should be referred to a specialist. While there is very limited literature on MRN in musculocutaneous neuropathy, likely due to the rarity of the condition, there is existing MRN research in other peripheral neuropathies that is promising.
Treatment
Similarly, there is very limited evidence for best management practices in the treatment of musculocutaneous neuropathies. Several treatment strategies, both surgical and non-surgical, have been used in cases of musculocutaneous nerve injury. Conservative management is typically used first, and surgical interventions follow when there is no improvement with conservative treatment. Non-operative management techniques include recommendations for relative rest and reduced activity, pharmacological agents (including non-steroidal anti-inflammatory drugs or anticonvulsants), local nerve inhibition methods (such as injection of corticosteroids or botulinum toxin), or physical therapy.2,3,6,7,10 Many cases in the literature reported full recovery with conservative management as described above. None of the cases reviewed for this condition described specific physical therapy techniques that were employed in order to treat musculocutaneous neuropathy. However, we may be able to extrapolate from the literature on peripheral nerve entrapments to propose possible treatment techniques that can be performed by manual/physical therapists.
Conservative management
Effective conservative management for peripheral neuropathies may include: education, soft tissue interventions, and neurodynamic mobilization techniques.12 Educating patients about the mechanism, presentation, and clinical behaviour of their pain can reduce the fear associated with their experience of pain, as well as influence emotional and cognitive components of pain. 12,38,39 It is also important to ensure that adjacent nonneural structures are functioning optimally in order to reduce nociceptive input.40 This may include interventions such as mobilization and/or manipulation of local joints, soft tissue therapy, taping to unload neural structures, or neuromuscular control retraining.12 Myofascial therapy techniques such as Active Release Technique (ART) ® may be effective in treating peripheral nerve entrapments, however much of the literature is low-level evidence comprising of case reports. ART® is described as a hands-on touch and case-management system that allows a practitioner to diagnose and treat soft-tissue injuries.41 It is performed by taking the target tissue from a shortened position to a lengthened position while the practitioner maintains tension longitudinally along the soft tissue fibres.41 One suggested mechanism of the ART® protocol in treating nerve entrapments is the movement of the tissues in such a way that causes relative motion between the entrapped nerve and the surrounding tissue.41 While not specifically reported in musculocutaneous neuropathy, the utilization of ART® as a therapeutic intervention has been reported in cases of pudendal nerve entrapment, carpal tunnel syndrome, saphenous nerve entrapment, and posterior interosseous nerve entrapment.42–46 It should be noted that more research is needed in order to fully understand the mechanism of myofascial therapy techniques in the treatment of peripheral nerve entrapments. Finally, neural tissue mobilizations have been hypothesized to have a positive impact on symptoms, however more research needs to be done in this area.12 Neural tissue mobilization techniques involve passive or active movements that focus on restoring the nervous system’s ability to tolerate compression, friction, and tension forces that are associated with daily activities.12 Nee and Butler proposed several neural mobilization techniques that may improve patients’ self-reported pain and disability, as well as physical signs of mechanosensitivity.12 Gliding techniques attempt to produce a sliding movement between neural tissues and adjacent tissues.40,47 Tensile loading techniques involve oscillatory movements of the limb in a fashion that puts tension on both the distal and proximal end of the nerve. The goal of these techniques is to improve the neural tissue tolerance to tension and lengthening.40
Operative management
If musculocutaneous nerve (or other peripheral nerve) injuries fail to respond with time and conservative treatment, then numerous surgical options have been described in the literature. These include epineurotomy, decompression, nerve graft, and nerve transfer, which will be described in this section. Surgical intervention is usually considered when there is no clinical or EMG evidence of reinnervation, typically within six months of the injury.22 The literature lacks a specific description of a release procedure for proximal musculocutaneous nerve injuries. Yilmaz et al. described a surgical epineurotomy procedure, where the epineurium was incised and interfascicular release was performed at the hyperemic and edematous segment of the nerve. This resulted in complete symptom relief following surgery and the patient was still symptom-free at one-year follow up.4 Surgical decompression may be advised if symptoms continue to persist 12 weeks after injury.1,11 This intervention involves the resection of a small triangular wedge of aponeurosis that overlies the nerve. Surgical management may be a more successful option depending on the type of nerve injury, the severity of the lesion, and time of delay in repair.48 Bhandari and Deb compared the outcomes of nerve grafts versus nerve transfers in the operative management of isolated musculocutaneous nerve injuries.49 It should be noted that all of the subjects in their study had neurotmesis injuries, and the authors acknowledge that most neuropraxia injuries improve with conservative management. Conventional nerve grafting involves replacing the damaged portion of the nerve with a graft from a sensory nerve elsewhere in the body, typically the sural nerve.49 Conversely, nerve transfer involves reconstructing the nerve by transferring fascicles from other nerves (such as the ulnar and median nerves) directly onto the motor branches of the musculocutaneous nerves. Bhandari and Deb reported that distal nerve transfer resulted in better functional outcomes than conventional nerve grafting.49 In this study, electromyography revealed the first sign of biceps reinnervation at 10 weeks in the nerve transfer group, compared with 20 weeks in the grafted group.49
Summary
The clinical presentation of the isolated musculocutaneous neuropathy in this case was typical of many reported cases in the literature. However, the mechanism of injury we report has not yet been described. Although this condition is rare, timely diagnosis is necessary in order to initiate proper treatment as soon as possible to avoid further insult to the nerve and associated muscle atrophy. The role of healthcare providers in a rare case such as this, is to recognize the signs and symptoms as early as possible, determine if a trial of conservative care is appropriate as a first-line treatment, and/or initiate referral to a specialist for further diagnostic testing and imaging. Electrodiagnostic studies such as electromyography and nerve conduction studies may aid in confirming the diagnosis. In most cases of neuropraxia, conservative management is successful and may include neurodynamic mobilization techniques, pain education, and treatment of adjacent nonneural structures using joint manipulation/mobilization, soft tissue therapy, taping, or muscle control training. However, when conservative management is unsuccessful, surgical intervention is required. In conclusion, early diagnosis of musculocutaneous neuropathies along with an appropriate intervention will help ensure the best possible outcome for the patient.
Footnotes
The authors have no disclaimers, competing interests, or sources of support or funding to report in the preparation of this manuscript.
The involved patient provided consent for case publication.
References
- 1.Besleaga D, Castellano V, Lutz C, Feinberg JH. Musculocutaneous neuropathy: case report and discussion. HSS J. 2010;6(1):112–116. doi: 10.1007/s11420-009-9143-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pecina M, Bojanic I. Musculocutaneous nerve entrapment in the upper arm. Int Orthop. 1993;17:232–234. doi: 10.1007/BF00194185. [DOI] [PubMed] [Google Scholar]
- 3.Papanikolaou A, Maris J, Tsampazis K. Isolated musculocutaneous nerve palsy after heavy physical activity. Inj Extra. 2005;36(11):486–488. [Google Scholar]
- 4.Yilmaz C, Eskandari MM, Colak M. Traumatic musculocutaneous neuropathy: a case report. Arch Orthop Trauma Surg. 2005;125(6):414–416. doi: 10.1007/s00402-005-0818-2. [DOI] [PubMed] [Google Scholar]
- 5.Merrell CA, Merrell KL. A variation of musculocutaneous neuropathy: implications for electromyographers. PM&R. 2010;2(8):780–782. doi: 10.1016/j.pmrj.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 6.Henry D, Bonthius DJ. Isolated musculocutaneous neuropathy in an adolescent baseball pitcher. J Child Neurol. 2011;26(12):1567–1570. doi: 10.1177/0883073811411189. [DOI] [PubMed] [Google Scholar]
- 7.Chabra T, Tahbildar P. Case report on isolated musculocutaneous nerve injury following a wrestling match. J Med Dent Sci. 2015;14(3):97–99. [Google Scholar]
- 8.Juel VC, Kiely JM, Leone KV, Morgan RF, Smith T, Phillips LH. Isolated musculocutaneous neuropathy caused by a proximal humeral exostosis. Neurology. 2000;54(2):494. doi: 10.1212/wnl.54.2.494. [DOI] [PubMed] [Google Scholar]
- 9.Moore KL, Dalley AF, Agur AM. Clinically Oriented Anatomy. 7th ed. Baltimore: Lippincott Williams & Wilkins; 2013. [Google Scholar]
- 10.DeFranco MJ, Schickendantz MS. Isolated musculocutaneous nerve injury in a professional fast-pitch softball player: a case report. Am J Sports Med. 2008;36(9):1821–1823. doi: 10.1177/0363546508317966. [DOI] [PubMed] [Google Scholar]
- 11.Davidson JJ, Bassett FH, Nunley JA. Musculocutaneous nerve entrapment revisited. J Shoulder Elbow Surg. 1998;7(3):250–255. doi: 10.1016/s1058-2746(98)90053-2. [DOI] [PubMed] [Google Scholar]
- 12.Nee RJ, Butler D. Management of peripheral neuropathic pain: Integrating neurobiology, neurodynamics, and clinical evidence. Phys Ther Sport. 2006;7(1):36–49. [Google Scholar]
- 13.Novak CB, Mackinnon SE. Evaluation of nerve injury and nerve compression in the upper quadrant. J Hand Ther. 2005;18(2):230–240. doi: 10.1197/j.jht.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 14.Elvey RL. Physical evaluation of the peripheral nervous system in disorders of pain and dysfunction. J Hand Ther. 1997;10(2):122–129. doi: 10.1016/s0894-1130(97)80066-x. [DOI] [PubMed] [Google Scholar]
- 15.Hislop H, Avers D, Brown M. Daniels and Worthingham’s Muscle Testing-E-Book: Techniques of Manual Examination and Performance Testing. Elsevier Health Sciences; 2013. [Google Scholar]
- 16.Tinel J. “Tingling” signs with peripheral nerve injuries. J Hand Surg. 2005;30(1):87–89. doi: 10.1016/j.jhsb.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 17.Abbott KM, Nesathurai S. Musculocutaneous nerve palsy following traumatic spinal cord injury. Spinal Cord. 1998;36(8):588. doi: 10.1038/sj.sc.3100653. [DOI] [PubMed] [Google Scholar]
- 18.Sander HW, Quinto CM, Elinzano H, Chokrouerty S. Carpet carrier’s palsy: musculocutaneous neuropathy. Neurology. 1997;48(6):1731–1732. doi: 10.1212/wnl.48.6.1731. [DOI] [PubMed] [Google Scholar]
- 19.Seddon H. Surgical Disorders of the Peripheral Nerves. Edinburgh, Scotland: Churchill Livingstone; 1972. [Google Scholar]
- 20.Dahlin LB, Wiberg M. Nerve injuries of the upper extremity and hand. EFORT Open Rev. 2017;2(5):158–170. doi: 10.1302/2058-5241.2.160071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duralde XA. Neurologic injuries in the athlete’s shoulder. J Athl Train. 2000;35(3):316–328. [PMC free article] [PubMed] [Google Scholar]
- 22.Campbell WW. Evaluation and management of peripheral nerve injury. Clin Neurophysiol. 2008;119(9):1951–1965. doi: 10.1016/j.clinph.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 23.Sunderland S. Rate of regeneration in human peripheral nerves: Analysis of the interval between injury and onset of recovery. Arch Neur Psych. 1947;58(3):251–295. doi: 10.1001/archneurpsyc.1947.02300320002001. [DOI] [PubMed] [Google Scholar]
- 24.Grinsell D, Keating C. Peripheral nerve reconstruction after injury: a review of clinical and experimental therapies. BioMed Res Int. 2014;698256:1–13. doi: 10.1155/2014/698256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abbed KM Coumans J-VCE. Cervical radiculopathy pathophysiology, presentation, and clinical evaluation. Neurosurgery. 2007;60(suppl1):S28–S34. doi: 10.1227/01.NEU.0000249223.51871.C2. [DOI] [PubMed] [Google Scholar]
- 26.Linda DD, Harish S, Stewart BG, Finlay K, Parasu N, Rebello RP. Multimodality imaging of peripheral neuropathies of the upper limb and brachial plexus. Radiographics. 2010;30(5):1373–1400. doi: 10.1148/rg.305095169. [DOI] [PubMed] [Google Scholar]
- 27.Andreisek G, Burg D, Studer A, Weishaupt D. Upper extremity peripheral neuropathies: role and impact of MR imaging on patient management. Eur Radiol. 2008;18(9):1953–1961. doi: 10.1007/s00330-008-0940-y. [DOI] [PubMed] [Google Scholar]
- 28.Quan D, Bird SJ. Nerve conduction studies and electromyography in the evaluation of peripheral nerve injuries. Univ Pa Orthop J. 1999;12:45–51. [Google Scholar]
- 29.Arancio O, Cangiano A, De Grandis D. Fibrillatory activity and other membrane changes in partially denervated muscles. Muscle Nerve. 1989;12(2):149–153. doi: 10.1002/mus.880120210. [DOI] [PubMed] [Google Scholar]
- 30.Kim S-J, Hong SH, Jun WS, Choi J-Y, Myung JS, Jacobson JA, et al. MR imaging mapping of skeletal muscle denervation in entrapment and compressive neuropathies. Radiographics. 2011;31(2):319–332. doi: 10.1148/rg.312105122. [DOI] [PubMed] [Google Scholar]
- 31.Andreisek G, Crook DW, Burg D, Marincek B, Weishaupt D. Peripheral neuropathies of the median, radial, and ulnar nerves: MR imaging features. Radiographics. 2006;26(5):1267–1287. doi: 10.1148/rg.265055712. [DOI] [PubMed] [Google Scholar]
- 32.May DA, Disler DG, Jones EA, Balkissoon AA, Manaster BJ. Abnormal signal intensity in skeletal muscle at MR imaging: patterns, pearls, and pitfalls. Radiographics. 2000;20(suppl1):S295–S315. doi: 10.1148/radiographics.20.suppl_1.g00oc18s295. [DOI] [PubMed] [Google Scholar]
- 33.Chhabra A, Andreisek G, Soldatos T, Wang KC, Flammang AJ, Belzberg AJ, et al. MR neurography: past, present, and future. Am J Roentgenol. 2011;197(3):583–591. doi: 10.2214/AJR.10.6012. [DOI] [PubMed] [Google Scholar]
- 34.Du R, Auguste KI, Chin CT, Engstrom JW, Weinstein PR. Magnetic resonance neurography for the evaluation of peripheral nerve, brachial plexus, and nerve root disorders. J Neurosurg. 2010;112(2):362–371. doi: 10.3171/2009.7.JNS09414. [DOI] [PubMed] [Google Scholar]
- 35.Chhabra A, Madhuranthakam AJ, Andreisek G. Magnetic resonance neurography: current perspectives and literature review. Eur Radiol. 2018;28(2):698–707. doi: 10.1007/s00330-017-4976-8. [DOI] [PubMed] [Google Scholar]
- 36.Sunderland S. A classification of peripheral nerve injuries producing loss of function. Brain. 1951;74(4):491–516. doi: 10.1093/brain/74.4.491. [DOI] [PubMed] [Google Scholar]
- 37.Filler AG, Kliot M, Howe F, Hayes CE, Saunders DE, Goodkin R, et al. Application of magnetic resonance neurography in the evaluation of patients with peripheral nerve pathology. J Neurosurg. 1996;85:299–309. doi: 10.3171/jns.1996.85.2.0299. [DOI] [PubMed] [Google Scholar]
- 38.Moseley G. A pain neuromatrix approach to patients with chronic pain. Man Ther. 2003;8(3):130–140. doi: 10.1016/s1356-689x(03)00051-1. [DOI] [PubMed] [Google Scholar]
- 39.Shacklock MO. Central pain mechanisms: a new horizon in manual therapy. Aust J Physiother. 1999;45(2):83–92. doi: 10.1016/s0004-9514(14)60340-8. [DOI] [PubMed] [Google Scholar]
- 40.Butler D. The sensitive nervous system. Adelaide, Australia: Noigroup Publications; 2000. [Google Scholar]
- 41.Leahy M. Active Release Techniques® Soft Tissue Management Systems for the Upper Extremity. 2nd edition. 2008. [Google Scholar]
- 42.Durante JA, MacIntyre IG. Pudendal nerve entrapment in an Ironman athlete: a case report. J Can Chiropr Assoc. 2010;54(4):276–281. [PMC free article] [PubMed] [Google Scholar]
- 43.George JW, Tepe R, Busold D, Keuss S, Prather H, Skaggs CD. The effects of active release technique on carpal tunnel patients: a pilot study. J Chiropr Med. 2006;5(4):119–122. doi: 10.1016/S0899-3467(07)60143-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robb A, Sajko S. Conservative management of posterior interosseous neuropathy in an elite baseball pitcher’s return to play: a case report and review of the literature. J Can Chiropr Assoc. 2009;53(4):300–310. [PMC free article] [PubMed] [Google Scholar]
- 45.Settergren R. Conservative management of a saphenous nerve entrapment in a female ultra-marathon runner. J Bodyw Mov Ther. 2013;17(3):291–301. doi: 10.1016/j.jbmt.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 46.Saratsiotis J, Myriokefalitakis E. Diagnosis and treatment of posterior interosseous nerve syndrome using soft tissue manipulation therapy: a case study. J Bodyw Mov Ther. 2010;14(4):397–402. doi: 10.1016/j.jbmt.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 47.Shacklock MO. Clinical neurodynamics: A new system of musculoskeletal treatment. Edinburgh, Scotland: Elsevier/Butterworth Heinemann; 2005. [Google Scholar]
- 48.Osborne AWH, Birch RM, Munshi P, Bonney G. The musculocutaneous nerve: results of 85 repairs. Bone Jt J. 2000;82(8):1140–1142. doi: 10.1302/0301-620x.82b8.10791. [DOI] [PubMed] [Google Scholar]
- 49.Bhandari PS, Deb P. Management of isolated musculocutaneous injury: comparing double fascicular nerve transfer with conventional nerve grafting. J Hand Surg. 2015;40(10):2003–2006. doi: 10.1016/j.jhsa.2015.06.122. [DOI] [PubMed] [Google Scholar]