Abstract
Objective
To illustrate the conservative clinical management of Morel-Lavallée lesion.
Clinical features
A 34 year-old male presented with a forced flexion induced right knee injury that was diagnosed as a Morel-Lavallée lesion by way of Magnetic Resonance Imaging (MRI).
Intervention and outcome
The patient was co-managed by a sports medicine physician and a chiropractor with a combination of percutaneous aspiration, dry needling, soft tissue therapy, extracorporeal shockwave therapy (ESWT), and corrective exercise.
Summary
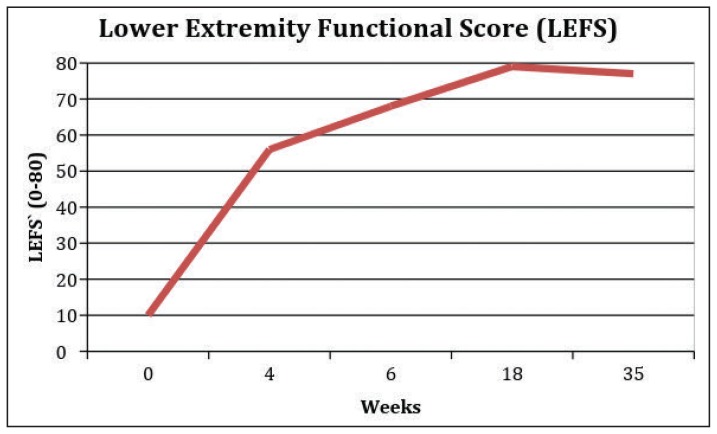
The patient experienced improved function throughout chiropractic care. Almost complete resolution was achieved at 18 weeks after injury and maintained at 35 weeks after injury. Further research is needed to understand if this improvement in function is better than the natural history of this condition.
Keywords: chiropractic, extracorporeal shockwave therapy, conservative management, electroacupuncture, fascial abrasion tool, Morel-Lavallée lesion
Abstract
Objectif
Illustrer la prise en charge conservatrice clinique de la lésion de Morel-Lavallée.
Caractéristiques cliniques
Un homme de 34 ans s’est présenté avec une blessure au genou droit provoquée par une flexion forcée qui a été diagnostiquée comme une lésion de MorelLavallée grâce à l’imagerie par résonance magnétique (IRM).
Intervention et résultats
Le patient a été pris en charge conjointement par un médecin du sport et un chiropraticien avec une combinaison d’aspiration percutanée, d’aiguilles sèches, de thérapie des tissus mous, de thérapie par ondes de choc extracorporelles et d’exercices correctifs.
Résumé
L’état du patient s’est amélioré tout au long des soins chiropratiques. Une guérison presque complète a été atteinte 18 semaines après la blessure et 35 semaines après la blessure, le patient été guéri. D’autres recherches sont nécessaires pour comprendre si cette amélioration de la fonction est meilleure que l’histoire naturelle de cette condition.
MOTS CLÉS: chiropratique, thérapie par ondes de choc extracorporelles, prise en charge conservatrice, électro-acupuncture, outil d’abrasion du fascia, lésion de MorelLavallée
Introduction
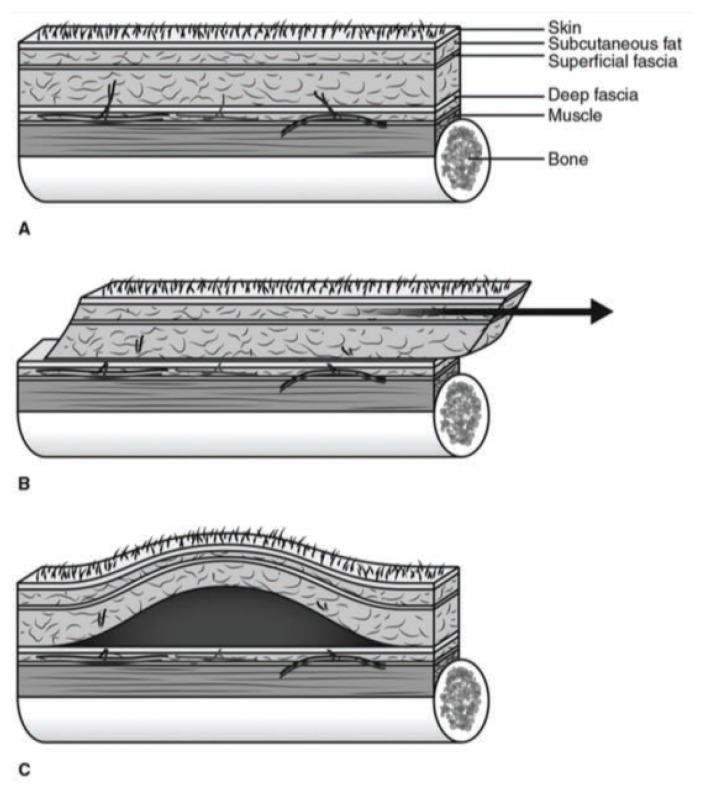
The Morel-Lavallée lesion (MLL) is a closed soft tissue injury usually sustained from trauma.1,2 It can be described as a degloving injury, as the injury involves shearing forces and separation of the hypodermis from the underlying fascia, similar to removing a glove.2 This causes disruption of the vasculature and lymphatic structures resulting in hemolymphatic fluid collection between the tissue layers. This injury needs to be diagnosed, preferably with Magnetic Resonance Imaging (MRI), and managed in a timely fashion as to prevent infection, pseudocyst formation, cosmetic deformity, and musculoskeletal dysfunction.1,2 There is a gap in the academic literature in regards to the conservative management of this condition and no clinical guidelines currently present. The purpose of this case study is to present the successful results of a multimodal conservative treatment approach that focuses on both the local lesion and the movement compensations associated with it.
Case presentation
A 34 year-old male presented to a chiropractic clinic with right knee pain and bruising of the inferomedial aspect of their thigh and lower leg. The patient had not seen a health care provider prior to this visit. The patient stated that this pain and bruising began after a traumatic sliding maneuver that involved sudden flexion of his right knee playing American football five days prior. There was no audible “pop” or “snap” with this sudden flexion. He was unable to continue playing due to pain. Swelling and bruising began the next day. The patient described their pain as dull, with a severity of 5/10, localized to the medial aspect of the knee and was causing a limp while walking. There was no distal pain, paresis, or paresthesia described. Since the injury, but prior to the physical examination, the patient had travelled on an airplane and attempted to play golf, but was unable to continue due to knee pain. The patient had not taken any medication and the patient’s systems review, family history, and medical history were unremarkable
On gait examination, the patient’s gait was antalgic but was able to weight bear with minimal pain. The patient was unable to extend their right hip and right knee during the gait cycle. Right ankle dorsiflexion was also limited as compared to the asymptomatic side during the gait assessment. Observation revealed bruising on the inferomedial thigh and medial ankle (see Figures 1 and 2) but no edema. Minimal tenderness was noted on palpation of the bruised area, however there was tenderness of the right semitendinosis tendon and medial joint line. The pedal pulse was palpated bilaterally. Lower limb sensory, motor, and reflex testing revealed normal neurological findings bilaterally. Range of motion testing revealed active and passive knee flexion were reduced, as compared to the asymptomatic side. Active knee flexion range of motion (ROM) was measured at 110° and passive knee flexion ROM at 115°. This limitation was due to superficial tension in the anterior quadricep musculature as described by the patient. Muscle testing of the trunk, hip, and thigh musculature was performed isometrically in a supine position and revealed a weak right gluteus maximus (3/5) when tested in a neutral hip position with 90 degrees of knee flexion as well as a weak right quadratus lumborum (3/5). Left hip, leg, and trunk musculature tested strong (5/5) with isometric muscle testing with the patient in a supine position.
Figure 1.
Inferomedial thigh bruising present five days after trauma.
Figure 2.
Lower leg bruising present five days after trauma.
Orthopedic testing of the right knee included Lachman, McMurray, anterior drawer, posterior drawer, Thessaly’s, pivot-shift, varus, and valgus stress tests were within normal limits. A lower extremity functional scale (LEFS) outcome measure was completed at each visit (see Table 1). A score of 10/80 was recorded at the initial visit indicating severe disability.
Table 1.
Lower Extremity Functional Scale (LEFS) results
| Visit | Date | LEFS Score |
|---|---|---|
| Initial Visit | Feb 6, 2018 | 10/80 |
| Follow Up 1 | March 2, 2018 | 56/80 |
| Follow Up 2 | March 21, 2018 | 68/80 |
| Follow Up 3 | June 14, 2018 | 79/80 |
| Follow Up 4 | October 10, 2018 | 77/80 |
Due to the significant ecchymosis, the patient was referred to a sports medicine physician (SMP). The patient was seen by the SMP the same day and was referred for a right knee radiographic series and diagnostic ultrasound. The imaging results were found to be negative two days later and the patient was then sent by the SMP for an MRI. The results of the MRI performed nine days later revealed:
No meniscal, cruciate, or collateral ligament tears but potential low grade sprain of proximal portion of ACL and MCL
Large subcutaneous fluid collections (10 cm x 12 cm) superficial to fascia and within the subcutaneous compartments in keeping with the degloving MLL
Question raised of deep vein thrombosis of the popliteal vein
Upon receiving these results and an urgent call from the radiologist, the SMP ordered a venous doppler of the right lower extremity to rule out deep venous thrombosis, which the patient had performed the same day. The results of the venous doppler received two days later revealed no evidence of deep vein thrombosis above or below the right knee. Two days after the venous doppler, and approximately three weeks post-injury, the patient presented to the SMP and it was noted that the area was not red or hot. The SMP explained the risks and benefits of needle aspiration of the area to remove fluid and reduce pressure. The patient consented to treatment and the SMP removed 100 ml of non-purulent blood. The patient was advised to follow up in five days and in the meantime wear a compressive sleeve, monitor the area for signs and symptoms of infection, and begin rehabilitation with the initiating chiropractor. That week the patient was unable to see the chiropractor due to work travel.
The patient presented to the SMP five days later and reported reduced pain and increased ROM. The patient was advised to begin riding a stationary bike and see the chiropractor for manual therapy and corrective exercise. The patient was again advised to monitor the area for signs and symptoms of infection.
Upon follow-up with the chiropractor 8 days after the aspiration and approximately four weeks post-injury, the patient was more functional with a LEFS score of 56/80. Their pain had decreased and passive knee flexion ROM was 125 degrees, an improvement of 10 degrees since the first visit. There was slight tenderness superficially on palpation of the patella and bruised area but no heat or erythema present. Superficial fluid was still present proximal and medial to the right patella. The chiropractor used soft tissue therapy and a fascial abrasion tool (FAT tool) to reduce tension in the hip flexor myofascia, anterior and posterior thigh myofascia, and calf myofascia for the purpose of improving hip extension ROM and ankle dorsiflexion ROM that were found to be reduced during initial gait assessment. The chiropractor also used dry needling with electrical stimulation at a current frequency of 2 Hz into the right hip capsule, anterior portion of gluteus medius, tensor fascia latae, right vastus lateralis, right vastus medialis, right saphenous nerve, right common peroneal nerve, and the right recurrent genicular nerve for the purpose of trigger point release and pain reduction.3–6 The chiropractor avoided needling areas of effusion or bruising. The patient was given common corrective exercises to be performed in between visits (Box 1). One set of ten repetitions of half of the prescribed exercises were to be done every other day. The lesser known retlouping exercise (Figure 3), typically used for postsurgical knee patients, was performed to improve hamstring flexibility and knee extension ROM. Sliding lunges were performed in all planes of movement to a ROM within the patient’s pain tolerance.
Box 1. Exercise prescription.
Hip flexor stretching in a lunge position
Two legged glute bridge
Box squat
Sliding lunge
Retlouping (see Figure 3)
Kettlebell swings (20 lbs)
Kettlebell front squats (20 lbs)
Goblet squat (20 lbs)
Sumo deadlift
Bulgarian split squat (no weight)
Figure 3.
Retlouping exercise.
Four days later the patient presented to the SMP and the right knee ROM was now full with only slight pain at full flexion. Cycling and corrective exercises had been well tolerated. A superficial edema region measuring 3 cm in diameter just above the patella was noted. No tenderness, heat, or erythema noted. A follow up visit in two weeks was advised.
The patient presented to the chiropractor for their second follow up visit at seven weeks post-injury and four weeks post-aspiration, and reported no pain in the knee with day-to-day activity and had now attempted jogging, the elliptical machine, lunging, and squats successfully without pain. A LEFS score of 68/80 was recorded. The chiropractor again used soft tissue techniques including manual therapy and a FAT tool to reduce tension in the hip flexor myofascia, anterior and posterior thigh myofascia, and calf myofascia. The chiropractor also used dry needling with electrical stimulation at a current of 2 Hz into the right hip capsule, anterior portion of gluteus medius, tensor fascia latae, right vastus lateralis, vastus medialis, right saphenous nerve, right common peroneal nerve, and the right recurrent genicular nerve. The chiropractor still avoided needling areas of effusion or bruising. The patient was encouraged to gradually increase the load with his strength training and was prescribed trunk and hip focused exercises including the dead bug exercise, bird dog exercise, and front and side planks.
The third follow up visit was approximately 19 weeks post-injury and 16 weeks post-aspiration. At this visit the patient presented with almost complete function and a LEFS score of 79/80. There was still lingering sensitivity on the superficial aspect of the patella, but the patient reported they were very functional with activities of daily living. The chiropractor again used soft tissue techniques including manual therapy and a FAT tool to reduce tension in the hip flexor myofascia, anterior and posterior thigh myofascia, and calf myofascia. The chiropractor again used dry needling with electrical stimulation at a current of 2 Hz into the right hip capsule, anterior gluteus medius, tensor fascia latae, right vastus lateralis, vastus medialis, right saphenous nerve, right common peroneal nerve, and the right recurrent genicular nerve.
The patient presented to the chiropractor 17 weeks later (36 weeks post-injury and 33 weeks post-aspiration) with slight discomfort proximal to the patella and a LEFS score of 77/80, a possible slight regression since the previous visit. However this slight regression was less than the minimum clinically important difference of 9 points for the LEFS.7 The distal quadricep musculature slightly proximal to the patella was palpably hardened as compared to the left quadricep. Due to suspected “scarring” of the underlying myofascia, the chiropractor advised using Extracorporeal Shockwave Therapy (ESWT) in the region and the patient consented. An ESWT session (Storz MP100 unit) of 2000 hits at 15 Hz with an intensity of 2 bars was used. The patient reported slight discomfort during the ESWT application but insisted it was manageable. Long-term outcomes after this visit and beyond 17 weeks post-injury were not available for the purposes of this study.
Management
Treatment interventions for this condition were performed by the chiropractor and the SMP and included percutaneous fluid aspiration, soft tissue manual therapy, instrument-assisted soft tissue mobilization, dry needling with electrical stimulation, corrective exercise and radial extracorporeal shockwave therapy.
Percutaneous Fluid Aspiration
Percutaneous aspiration of 100 ml of fluid was performed three weeks post injury by the SMP.8
Soft-Tissue Manual Therapy
Myofascial soft tissue therapy was applied to the hip myofascia, anterior and posterior thigh myofascia, and calf myofascia bilaterally to improve ROM of these tissues and the associated joints.9,10
Instrument-Assisted Soft Tissue Mobilization (IASTM)
IASTM has been shown to be an effective tool for reducing the pain pressure threshold of a myofascial trigger point which involves pain, weakness, and dysfunction.11 A FAT tool was used on the anterior thigh and calf musculature on the ipsilateral side of the lesion for the purpose of improved myofascial ROM and pain reduction.11,12
Dry Needling With Electrical Stimulation
Dry needling involves the insertion of acupuncture needles without injectate into or around nerves, muscles, and or connective tissue for the management of pain and dysfunction in neuromusculoskeletal conditions by way of neurohumoral response.3–6 Dry needling was not used around the bruised lesion or in areas with edema, but was used proximal and distal to this region. Needle insertion sites during the initial visit included the proximal quadriceps on the ipsilateral side for pain control and muscular tension reduction. Subsequent visits involved needle insertion into the right hip capsule, anterior gluteus medius, tensor fascia latae, right vastus lateralis, vastus medialis, adjacent to the right saphenous nerve, right common peroneal nerve, and the right recurrent genicular nerve. These dry needling points were chosen as they displayed hypertonicity on palpation, reflective of trigger points.6
Corrective Exercise
A corrective exercise approach with the goal of returning to right lower extremity function involved trunk, hip, knee, and foot mobility and stability exercises. These were used in conjunction with a gradual progression of cycling, elliptical, and running.13
Extracorporeal Shockwave Therapy (ESWT)
Radial ESWT was applied to the lesion during the final visit (35 weeks after the initial visit) as the lesion had been chronic at this stage and ESWT can significantly improve the healing process of chronic wounds.14
Follow-up and Outcomes
The LEFS was used as an outcome measure. The questionnaire was completed at the start of each chiropractic visit. The long-term follow-up beyond 35 weeks was not included in this document as it was still ongoing (see Figure 4).
Figure 4.
Lower Extremity Functional Scale.
Discussion
Epidemiology
MLL is uncommon and has been reported to be involved in 8.3% of pelvic traumas.15 It is often associated with acetabulum and pelvic fractures but can also be related to knee trauma, which is less severe.15–17 However, over the period of 14 NFL seasons, one team reported 27 MLLs in 24 American football athletes, which may suggest the injury is more common than once thought.17
Pathology
MLL occurs due to a shearing of superficial subcutaneous tissue away from underlying fascial layers (see Figure 4). Areas of mobile overlying skin and tough underlying fascia like the proximal lateral thigh and quadriceps fascia proximal to the knee are more prone to this condition.16,17 Following tissue separation, blood and lymph tissue are able to travel more freely and often pool in between layers of tissue.1,2, 15–17 Blood within these cavities begins to resorb leaving a seroanguinous fluid surrounded by a haemosiderin layer which induces inflammation and leads to a fibrous capsule. If not intervened promptly, this capsule will lead to a chronic MLL.16
Signs and symptoms
MLL typically presents as enlarged, tight, and tender tissue that may contain ecchymosis, erythema, and surface abrasion of the skin. An important clinical feature is the presence of fluctuance within the lesion. Potential differential diagnoses to consider include haematoma, fat necrosis, haemangioma, soft tissue sarcoma, early myositis ossificans, or bursitis. MLL can typically be discerned based on the mechanism of injury and the progression of symptoms.
Investigations
When trauma and the signs and symptoms mentioned above are present, MLL should be ruled out with diagnostic imaging.16,18 Diagnostic ultrasound is an inexpensive initial investigative tool and typically demonstrates the lesion as anechoic relative to hyperechoic mass.19 MRI is the imaging modality of choice and should be ordered urgently, as done in this case. Diagnostic ultrasound is less useful but Doppler ultrasound can be used to rule out a suspicion of vascular compromise such as deep vein thrombosis, as done in this case.16 Computed Tomography (CT) does not provide value in the assessment of MLL.18
Classification
Mellado and Bercandino20 have proposed a classification system for MLL based on size, MRI characteristics, and capsular presence. Shen et al. have more recently suggested using a more simplified classification system identifying MLL as either acute or chronic. According to Shen et al., MLL can be diagnosed as chronic when the lesion contains a capsule.8
Complications
Since the mechanism of injury is commonly traumatic, bacterial infection can be a concern in MLL due to an open lesion of the skin. While infection rates with MLL are inconclusive, due to the severity of the potential complications with infected tissue, this should be the primary concern with this lesion.
Management
Management decisions for MLL are based on the volume of the cavity created in the lesion, as well as the chronicity of the lesion. There are currently no management guidelines for the management of MLL. Many small cohort studies have investigated the efficacy of conservative management, percutaneous aspiration, sclerodesis, and open surgery, but there is currently no high quality evidence to support any one treatment strategy over the other.1,2,15,16 As for conservative management measures, compression is thought to flush out the inevitable edema in the area and has shown good effects in knee related MLL.8,17,18 High recurrence rates of MLL have been shown after percutaneous aspiration of the lesion. MLL with a volume greater than 50 ml has a higher likelihood of recurring than those with less than 50 ml of fluid.8 This patient had 100 ml aspirated, was informed of this higher likelihood of recurrence and yet did not present with a recurrence while under care. Sclerodesis to close off the cavity has been successfully used in MLL. The sclerodesis agents cause cell destruction within the periphery of the lesion, which then induces fibrosis.8 Doxycycline as a sclerodesis agent has shown the best results and is recommended in a recent review.1,21 Sclerodesis has been shown to be efficacious in lesions up to 700 ml in volume, with the mean volume of treated lesions being approximately 400 ml.22 Surgical intervention reduces recovery time as compared to compression therapy on its own, other than in cases of acute MLL around the knee.12 Open drainage and mass resection are also options that can be used if there is a larger volume or if not responding to more conservative strategies. The clinical decisions made by the SMP were to use minimally invasive strategies like aspiration and compression and the outcomes along with chiropractic care were successful.
The treatment interventions chosen by the chiropractor and described in the management section above were with the goals of first managing pain, mobilizing the soft tissue structures above and below the MLL lesion, preventing scarring of the lesion, increasing muscle strength, and improving function.4–12
Summary
The MLL is an uncommon soft tissue degloving injury that should be considered as a differential diagnosis for any patient who has sustained a serious traumatic injury. A wide variety of treatment interventions have been proposed in the literature, yet none considering soft tissue conservative management including dry needling with electrical stimulation, soft tissue manual therapy, instrument-assisted soft tissue therapy, corrective exercise and ESWT. The treatment(s) chosen by a health care practitioner for a patient presenting with MLL should be made on an individualized basis based on the size and chronicity of the lesion. This case study illustrates that conservative soft tissue treatment options may be considered for patient’s presenting with MLL if the lesion is relatively small (less than or equal to 100 ml) and in the acute stage. The successful conservative management of this patient, more prone to recurrence due to a percutaneous aspiration greater than 50 ml, demonstrated the potential for improving function and preventing recurrence with a multimodal conservative treatment approach. Long term follow-up with this patient, beyond 35 weeks, would allow for comment on longer term efficacy of the interventions. Future research is warranted to consider if these treatment strategies would also be helpful to improve function, reduce symptoms and prevent recurrence for larger MLL lesions or those in the chronic stage, either on their own, or in addition to less conservative options such as percutaneous aspiration or sclerodesis.
Figure 5.
Cross-section of tissue from skin to bone (image reproduced with permission of Scolaro et al.2).
Footnotes
The authors have no disclaimers, competing interests, or sources of support or funding to report in the preparation of this manuscript.
The involved patient provided consent for case publication.
References
- 1.Singh R, Rymer B, Youssef B, Lim J. The Morel-Lavallée lesion and its management: a review of the literature. J Orthopaed. 2018;15:917–921. doi: 10.1016/j.jor.2018.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scolaro JA, Chao T, Zamorano DP. The Morel-Lavallée lesion: diagnosis and management. J Am Acad Orthop Surg. 2016;24(10):667–672. doi: 10.5435/JAAOS-D-15-00181. [DOI] [PubMed] [Google Scholar]
- 3.Dunning J, Butts R, Mourad F, Young I, Flannagan S, Perreault T. Dry needling: a literature review with implications for clinical practice guidelines. Phys Ther Rev. 2014;19(4):252–265. doi: 10.1179/108331913X13844245102034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C, Wang Y, Han JS, Wan Y. Characteristics of electroacupuncture-induced analgesia in mice: variation with strain, frequency, intensity and opioid involvement. Brain Res. 2002;945(1):20–25. doi: 10.1016/s0006-8993(02)02503-9. [DOI] [PubMed] [Google Scholar]
- 5.Ulett GA, Han S, Han JS. Electroacupuncture: mechanisms and clinical application. Biologic Psychiatr. 1998;44(2):129–138. doi: 10.1016/s0006-3223(97)00394-6. [DOI] [PubMed] [Google Scholar]
- 6.Gattie E, Cleland JA, Snodgrass S. The effectiveness of trigger point dry needling for musculoskeletal conditions by physical therapists: a systematic review and metaanalysis. J Orthopaed Sports Phys Ther. 2017;47(3):133–149. doi: 10.2519/jospt.2017.7096. [DOI] [PubMed] [Google Scholar]
- 7.Binkley JM, Stratford PW, Lott SA, Riddle DL. The lower extremity functional scale (LEFS): scale development, measurement properties, and clinical application. Physical Ther. 1999;79:371–383. [PubMed] [Google Scholar]
- 8.Shen C, Peng J, Chen X. Efficacy of treatment in peri-pelvic Morel-Lavallée lesion: a systematic review of the literature. Arch Orthop Trauma Surg. 2013;133(5):635–640. doi: 10.1007/s00402-013-1703-z. [DOI] [PubMed] [Google Scholar]
- 9.Tak S, Lee Y, Choi W, Lee G. The effects of active release technique on the gluteus medius for pain relief in persons with chronic low back pain. Physical Ther Rehabil Sci. 2013;2(1):27–30. [Google Scholar]
- 10.Piper S, et al. The effectiveness of soft-tissue therapy for the management of musculoskeletal disorders and injuries of the upper and lower extremities: a systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Manual Therapy. 2015;21:18–34. doi: 10.1016/j.math.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 11.Gulick D. Instrument-assisted soft tissue mobilization increases myofascial trigger point pain threshold. J Bodywork Movement Ther. 2018;22(2):341–345. doi: 10.1016/j.jbmt.2017.10.012. [DOI] [PubMed] [Google Scholar]
- 12.Cheatham SW, Lee M, Cain M, Baker R. The efficacy of instrument assisted soft tissue mobilization: a systematic review. J Can Chiropr Assoc. 2016;60(3):200–211. [PMC free article] [PubMed] [Google Scholar]
- 13.Kristensen J, Franklyn-Miller A. Resistance training in musculoskeletal rehabilitation: a systematic review. Brit J Sports Med. 2012;46(10):719–726. doi: 10.1136/bjsm.2010.079376. [DOI] [PubMed] [Google Scholar]
- 14.Zhang L, Weng C, Zhao Z, Fu X. Extracorporeal shock wave therapy for chronic wounds: a systematic review and meta-analysis of randomized controlled trials. Wound Repair Regen. 2017;25:697–706. doi: 10.1111/wrr.12566. [DOI] [PubMed] [Google Scholar]
- 15.Nickerson T, Zielinski M, Jenkins D, Schiller H. The Mayo Clinic experience with Morel-Lavallée lesion: establishment of a practice management guideline. J Trauma Acute Care Surg. 2014;76(2):493–497. doi: 10.1097/TA.0000000000000111. [DOI] [PubMed] [Google Scholar]
- 16.Bonilla-Yoon I, Masih S, Patel D, et al. Morel-Lavallée lesion: pathophysiology, clinical presentation, imaging features, and treatment options. Emerg Radiol. 2014;21(1):35–43. doi: 10.1007/s10140-013-1151-7. [DOI] [PubMed] [Google Scholar]
- 17.Tejwani S, Cohen S, Bradley J. Management of Morel-Lavallee lesion of the knee: twenty-seven cases in the national football league. Am J Sports Med. 2007;35(7):1162–1167. doi: 10.1177/0363546507299448. [DOI] [PubMed] [Google Scholar]
- 18.Nair A, Nazar P, Sekhar R, Ramachandran P, Moorthy S. Morel-Lavallée lesion: a closed degloving injury that requires real attention. Indian J Radiol Imag. 2014;24(3):288–290. doi: 10.4103/0971-3026.137053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gilbert BC, Bui-Mansfield LT, Dejong S. MRI of a Morel-Lavallee Lesion. Am J Roenten. 2004;182:1347–1348. doi: 10.2214/ajr.182.5.1821347. [DOI] [PubMed] [Google Scholar]
- 20.Mellado JM, Bencardino JT. Morel-Lavallée lesion: review with emphasis on MR imaging. Magn Reson Imaging Clin N Am. 2005;13:775–782. doi: 10.1016/j.mric.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 21.Bansal A, Bhatia N, Singh A, Singh A. Doxycycline sclerodesis as a treatment option for persistent Morel-Lavallée lesions. Injury. 2013;44(1):66–69. doi: 10.1016/j.injury.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 22.Penaud A, Quignon R, Danin A, Bahe L, Zakine G. Alcohol sclerodhesis: an innovative treatment for chronic Morel-Lavallée lesions. J Plast Reconstr Aesthetic Surg. 2011;64(10):262–264. doi: 10.1016/j.bjps.2011.06.012. [DOI] [PubMed] [Google Scholar]