Abstract
Background
In young and active patients, long head of biceps (LHB) tenodesis has become a common procedure for managing LHB pathology, but it remains unclear whether it is performed in isolation or along with other shoulder procedures and whether open and arthroscopic techniques produce different complications.
Questions/Purposes
We sought to determine and compare open and arthroscopic LHB tenodesis in terms of (a) trends in overall use, (b) trends in use in isolation and in association with rotator cuff repair (RCR) and superior labral tear from anterior-to-posterior (SLAP) debridement/repair, and (c) the rates of post-operative complications.
Methods
We performed a retrospective analysis of data from an insurance database to identify LHB tenodesis procedures performed from 2011 to 2014. The overall annual rates of open and arthroscopic LHB tenodesis were determined and then stratified according to concurrent RCR and SLAP repair/debridement. A multivariate logistic regression analysis that controlled for patient demographics (age, sex, comorbidity) was performed.
Results
Overall, 8547 patients underwent LHB tenodesis, of which 43.5% were open and 56.5% were arthroscopic procedures. There was a significant increase in the utilization of LHB tenodesis from 2011 to 2014. In isolation, open LHB tenodesis was the more common technique overall and by year. Arthroscopic LHB tenodesis was the most common tenodesis technique performed in conjunction with RCR and SLAP repair/debridement. The overall complication rate was 2.9%; only wound dehiscence demonstrated a difference between techniques.
Conclusions
The rates of open and arthroscopic LHB tenodesis procedures increased significantly from 2011 to 2014, with open techniques more common when LHB tenodesis is performed in isolation and arthroscopic techniques more common when performed as a concomitant procedure. Our use of a population database did not allow us to evaluate biomechanical or cost-related phenomena, and future research should examine these and other relevant differences between these two LHB tenodesis techniques.
Electronic supplementary material
The online version of this article (10.1007/s11420-018-9645-1) contains supplementary material, which is available to authorized users.
Keywords: long head biceps, biceps, tenodesis, open, arthroscopic, complications
Introduction
Pathology of the long head of biceps (LHB) is increasingly recognized as a source of anterior shoulder pain [5]. Management of LHB pathology includes non-operative and operative treatment. Two surgical techniques exist to manage LHB pathology: tenodesis and tenotomy [21]. In the young and active patient, LHB tenodesis has become more commonplace, with evidence suggesting it results in improved cosmesis and decreased biceps muscle cramping [11]. Two common techniques for LHB tenodesis are arthroscopic supra-pectoral tenodesis and open sub-pectoral tenodesis. To date, studies have demonstrated a rise in the overall and technique-specific use of LHB tenodesis, but these studies are limited to 2011, and it remains unclear in what clinical context LHB tenodesis is utilized—that is, performed in isolation or along with other common shoulder procedures, such as rotator cuff repair (RCR) or superior labrum anterior-to-posterior (SLAP) tear debridement or repair [22]. Additionally, while a number of clinical studies have failed to demonstrate a difference in clinical outcomes between arthroscopic and open LHB tenodesis [1], it remains largely unknown if there is a difference in complication rates, particularly in rare complications such as post-operative humeral shaft fractures; many studies examining this have been limited-to-small sample sizes or case reports [7, 13, 14, 17, 24]. There is difficulty in reporting rare complications in small cohorts, and thus, using a larger patient population—as a large population database provides—may better determine whether such rare complications exist and differ by technique.
We sought to determine and compare (a) trends in the use of arthroscopic and open LHB tenodesis techniques, (b) trends in their use in isolation and in association with RCR and SLAP debridement/repair, and (c) the rates of post-operative complications between open and arthroscopic techniques. Our hypothesis was that both open and arthroscopic LHB tenodesis procedures would be increasingly used, with the open technique being more common, regardless of its use in isolation or with other arthroscopic surgery, and that the rates of open and arthroscopic techniques would not be significantly different.
Methods
A retrospective review of the PearlDiver Humana database (PearlDiver, Warsaw, IN, USA) was performed to capture all open and arthroscopic LHB tenodesis procedures performed from 2011 through the end of 2014. Institutional review board (IRB) approval was not required as the data is anonymous and publically available. The PearlDiver Humana database is a commercially available, Health Insurance Portability and Accountability Act (HIPAA)-compliant national database containing individual patient records associated with Current Procedural Terminology (CPT) and International Classification of Diseases, Ninth Revision (ICD-9) codes related to orthopedic procedures. This technology has been utilized in numerous publications, including patient populations who have undergone orthopedic shoulder sports surgery, as with a recent assessment of the effect of concomitant biceps tenodesis on reoperation rates after arthroscopic RCR [8]. It represents 16 million records and includes Medicare and Medicare Advantage beneficiaries and private and commercially insured patients [4].
We identified all patients in the database with CPT codes 29,828 (arthroscopy, shoulder, surgical; biceps tenodesis) or 23,430 (tenodesis of long tendon of biceps; open treatment). Exclusion criteria included previous or concurrent humeral shaft fracture. Patient age, sex, and year of surgical procedure were available in the database. In addition, patient comorbidities were determined using ICD-9 diagnosis codes, which are listed in Table 2 in Appendix 1. All patients had a minimum of 90 days of follow-up.
Table 2.
ICD-9 codes for each comorbidity
| Comorbidity | ICD-9 code |
|---|---|
| Obesity | 278.00–278.03 |
| Smoking | 305.1 |
| Diabetes | 249.00, 250.00, 250.01, 790.2–290.29, 791.5, 791.6 |
| Coronary artery disease | 414.0–414.9 |
| Chronic kidney disease | 585.1–585.9 |
| Congestive heart failure | 398.91, 428.0–428.9 |
| Chronic obstructive pulmonary disease | 491.0–491.9, 492.0–492.9, 493.00–493.92, 494.0, 494.1, 495.0–495.9, 496 |
ICD-9 International Classification of Diseases, Ninth Revision
Post-operative complications were determined by identifying ICD-9 diagnosis codes for each complication arising within 90 days of the initial procedure, including deep vein thrombosis (DVT)/pulmonary embolism (PE), nerve injury, wound dehiscence, hematoma, and humerus fracture (Table 3 in Appendix 2). Associated CPT procedure codes were used to identify stiffness (open capsule release [23020], manipulation under anesthesia [MUA, 23700], and arthroscopic lysis of adhesions with MUA [29825] within 6 months) and surgical site infection (irrigation and debridement within 90 days [10,180, 20,000, 20,005, 10,140, 10,060, or 10,061]).
Table 3.
ICD-9 codes for each event
| Event | ICD-9 code |
|---|---|
| Thromboembolic event (DVT/PE) | 452, 453.0, 453.1, 453.2, 453.3, 453.40, 453.41, 453.42, 453.50, 453.51, 453.52, 453.6, 453.71, 453.72, 453.73, 453.74, 453.75, 453.76, 453.77, 453.79, 453.8, 453.81, 453.82, 453.83, 453.84, 453.85, 453.86, 453.87, 453.89, 453.9 |
| Nerve injury | 955.0, 955.1, 955.2, 955.3, 955.4, 955.5, 955.6, 955.7, 955.8, 955.9, 907.4 |
| Wound dehiscence | 998.30, 998.31, 998.32, 998.33 |
| Hematoma | 998.11, 998.12, 998.13 |
ICD-9 International Classification of Diseases, Ninth Revision, DVT deep venous thrombosis, PE pulmonary embolism
The characteristics of procedures performed concomitantly with open or arthroscopic biceps tenodesis were also collected, including RCR, with CPT codes 29,827 (arthroscopy, shoulder, surgical; with rotator cuff repair), 23,410 (repair of ruptured musculotendinous cuff [i.e., rotator cuff] open; acute), or 23,412 (repair of ruptured musculotendinous cuff [i.e., rotator cuff] open; chronic)] and SLAP repair/debridement, with CPT code 29807 (arthroscopy, shoulder, surgical; repair of SLAP lesion).
Statistical Analysis
Statistical analyses were conducted using R (R Foundation for Statistical Computing, Vienna, Austria). Pearson’s χ2 analyses were used to compare patient demographics between open and arthroscopic LHB tenodesis. Multivariate logistic regression was used to compare open and arthroscopic techniques in terms of adverse events, using arthroscopic cases as the reference. Multivariate analyses controlled for baseline patient characteristics, including age, sex, comorbidities, and year of operation. Trends across years for isolated LHB tenodesis, those performed with concomitant RCR or SLAP repair/debridement were determined using Cochran–Armitage tests for trend. All tests were two-tailed, and the statistical difference was established at a two-sided ά level of 0.05 (p < 0.05).
Results
Overall, we identified 8547 patients who underwent LHB tenodesis, of which 43.5% (n = 3717) underwent the open technique and 56.5% (n = 4830) underwent the arthroscopic technique. The typical patient who underwent LHB tenodesis was between the ages of 50 and 80 years (85.2%, n = 7282; p < 0.001) and male (58.3%, n = 4980; p < 0.001), irrespective of LHB tenodesis technique. Patients who underwent open LHB tenodesis were significantly younger than their arthroscopic counterparts (p < 0.001), but no other significant differences were seen in patient demographics (sex, obesity, diabetes, chronic obstructive pulmonary disease, coronary artery disease, congestive heart failure, chronic kidney disease, and smoking).
Trends
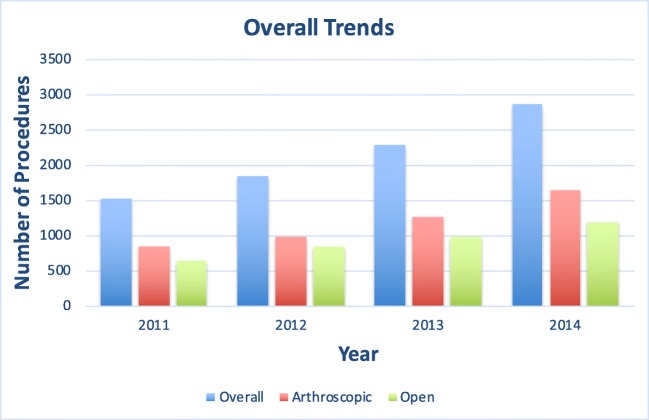
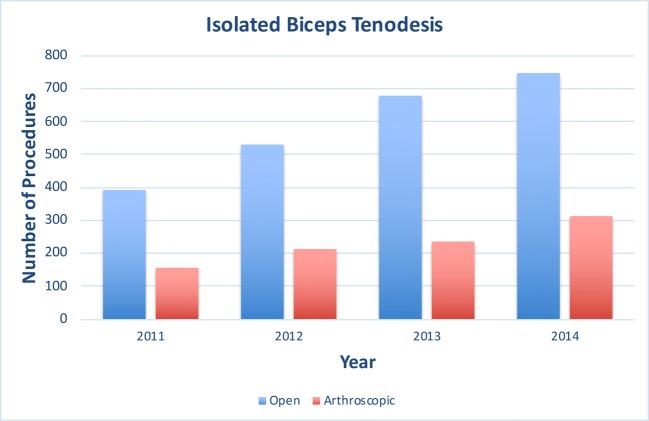
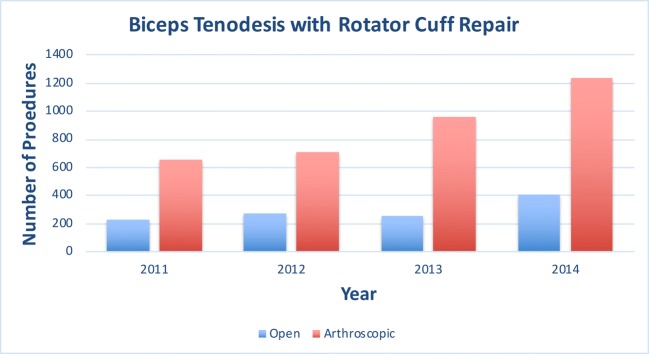
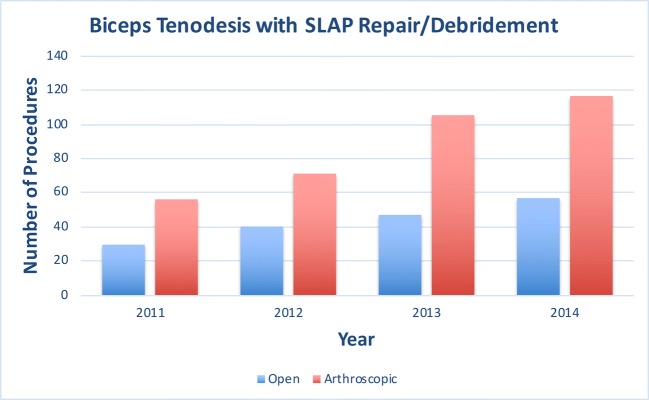
There was a significant increase in LHB tenodesis procedures from 2011 to 2014 (1525 out of 6,536,126 Humana beneficiaries in 2011 vs. 2875 out of 9,649,042 Humana beneficiaries in 2014, p ≤ 0.001) (Fig. 1). A similar rise in both arthroscopic and open LHB tenodesis procedures was observed from 2011 to 2014 (open LHB tenodesis, 654 vs. 1208, respectively; arthroscopic LHB tenodesis, 871 vs. 1667, respectively; Fig. 1). In isolation, open LHB tenodesis was the more common technique overall and by year. There was no significant comparative change in the number of isolated open and arthroscopic LHB tenodesis procedures performed annually between 2011 and 2014 (p = 0.78 and p = 0.95, respectively; Fig. 2). As a concomitant procedure, the arthroscopic LHB tenodesis technique was the most common tenodesis technique performed in conjunction with RCR and SLAP repair/debridement. Moreover, the number of arthroscopic LHB tenodesis procedures performed concurrently with RCR and SLAP repair/debridement annually between 2011 and 2014 increased significantly (in conjunction with RCR, p < 0.001; in conjunction with SLAP repair/debridement, p < 0.001). On the other hand, the annual number of open LHB tenodesis procedures performed with RCR and SLAP repair/debridement did not increase significantly between 2011 and 2014 (in conjunction with RCR, p = 0.26; in conjunction with SLAP repair/debridement, p = 0.05) (Figs. 3 and 4).
Fig. 1.
Overall trends in utilization of long head biceps tenodesis, 2011 to 2014.
Fig. 2.
Overall trends in performance of isolated long head biceps tenodesis, 2011 to 2014.
Fig. 3.
Overall trends in performance of concomitant long head biceps tenodesis with rotator cuff repair, 2011 to 2014.
Fig. 4.
Overall trends in performance of concomitant long head biceps tenodesis with slap repair/debridement, 2011 to 2014.
Complications
The overall complication rate was 2.9% for the LHB tenodesis procedure. No significant difference was seen in the complication rate following open versus arthroscopic LHB tenodesis (rate, 3.3% vs. 2.3%, respectively; p = 0.319). The rate of and odds ratio (OR) for wound dehiscence following LHB tenodesis were significantly greater following the open rather than the arthroscopic technique (rate, < 0.4% vs. < 0.3%, respectively; OR, 3.7; p = 0.042), with no other significant differences in wound dehiscence, infection, hematoma, stiffness, or thromboembolic events (Table 1).
Table 1.
Complications after long head biceps tenodesis
| Overall | Open | Arthroscopic | Multivariate | |||||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | Odds ratio | p value | |
| Any adverse event | 204 | 2.9 | 91 | 3.3 | 113 | 2.3 | 1.2 | 0.319 |
| Nerve injury | < 11 | < 0.2 | 11 | < 0.4 | < 11 | < 0.3 | 3.3 | 0.914 |
| Wound dehiscence | 13 | 0.2 | < 11 | < 0.4 | < 11 | < 0.3 | 3.7 | 0.042 |
| Hematoma | 21 | 0.3 | 10 | 0.4 | 11 | 0.2 | 1.1 | 0.991 |
| Stiffness | 62 | 0.9 | 29 | 1.0 | 33 | 0.7 | 1.3 | 0.295 |
| Humerus fracture | 23 | 0.3 | 12 | 0.4 | 11 | 0.2 | 1.8 | 0.215 |
| SSI | 28 | 0.4 | 11 | 0.4 | 17 | 0.4 | 1.0 | 0.941 |
No. number, SSI surgical site infection
Discussion
Overall, we observed trends suggesting that there was a significant increase in the use of LHB tenodesis over the included 3-year period. This continues the trends that Vellios et al. [20] and Werner et al. [22] found, with increasing number of biceps tenodesis cases between 2007 and 2011 and 2008 and 2011, respectively. It likely reflects a continued improvement in surgeon awareness of biceps tendon disease and a preference for tenodesis over tenotomy. In addition, while open LHB tenodesis was more common when performed as an isolated procedure, arthroscopic tenodesis is both more common and increasing yearly when performed concurrently with either RCR or SLAP repair/debridement. As nearly half of all LHB tenodesis cases are associated with rotator cuff pathology due to its association with tendinopathy of the LHB [2, 20, 25], this finding is not surprising. Furthermore, as arthroscopic (rather than open) treatment is most common for RCR or SLAP repair/debridement, surgeons may decide to tenodese the biceps in a similar fashion rather than perform a separate open incision [20]. As the instrumentation available for arthroscopic LHB tenodesis continues to improve, and as data suggests that the overall charges for arthroscopic tenodesis have increased at a rate significantly greater than that of open tenodesis [22], we may further expect these disparities to rise.
Our study is not without limitations. As with any study using an administrative database, our limitations include those due to reliance on data from a national registry of patients, which may not be representative of the overall population of patients who underwent LHB tenodesis. Any miscoding, undercoding, or absence of surgeon- or patient-specific variables recorded in the database could have affected our results. Additionally, details about the surgeries—including intra-operative details, tenodesis fixation components or surgical technique, or surgeon specifics—cannot be assessed with the PearlDiver database, and thus, we could not determine associations between such variables and the interventions or complications. The PearlDiver database does not disclose data when fewer than 11 patients are in a single group, out of concern for patient confidentiality. The ability to report exact patient information is thus prevented. The time these patients are followed may contribute to missed identification of complications that developed over a longer period, although this would be true for both cohorts. Additionally, we used a relatively short duration of time to generate a representative cohort and propose an extrapolated, generalized trend in LHB tenodesis. Furthermore, while our data provides information on trends, patient demographics, and complications, it does not comment on the efficacy of the procedure in terms of patient-reported outcomes or physical examination findings. Finally, as our data is limited through 2014, our findings may underestimate current trends in LHB tenodesis surgery, especially if large shifts in practice have been made in recent years.
The complication rate from LHB tenodesis—when performed arthroscopically or in an open fashion—is remarkably low. The comparison of techniques found no difference in overall complication rates, but it did reveal significantly greater OR (3.7) of a wound dehiscence following open LHB tenodesis. With exceedingly low rates of occurrence (< 0.4% vs. < 0.3%) in both groups, the clinical relevance of this statistical finding is suspect. In their systematic review comparing LHB tenodesis techniques, Abraham et al. [1] did not report any cases of frank wound dehiscence after arthroscopic or open LHB tenodesis, again highlighting its infrequency.
We saw no differences in any of the other post-operative complications, including humeral shaft fracture and stiffness. While humeral shaft fractures after LHB tenodesis are relatively infrequent—with mostly case reports or small series in the literature reporting its incidence—the repercussions can be devastating [7, 10, 12, 15, 16, 19]. Creation of the drill hole in the proximal humerus during open sub-pectoral tenodesis may predispose the humerus to fracture [3, 6, 7]. Ways of reducing the risk of fracture have been proposed, including the use of unicortical and concentric drilling in the humerus with the guide pin, careful reaming, non-absorbable screws (or polyether ether ketone [PEEK] screws rather than poly-l-lactide [PLLA] screws for slower biodegradation profiles) in lieu of absorbable, smaller screw sizes, suture anchors over interference screws, and delayed return to overhead activities [6, 7, 9, 10, 16, 18, 19]. Additionally, isolated clinical studies have suggested increased post-operative stiffness after arthroscopic LHB supra-pectoral tenodesis (17.9 vs. 5.6%)—most commonly in female patients and smokers—and that it may be related to the superiorly placed tenodesis site [24]. Our results challenge these findings and suggest that open LHB tenodesis does not result in greater rates of post-operative stiffness—in addition to a finding that the rates of this complication (open, 1.0%; arthroscopic, 0.7%) are far lower than previously reported. However, we acknowledge the difficulty of comparing dichotomous results from large databases to clinical studies in which range of motion is diligently recorded post-operatively.
That we found no differences in the remaining post-operative complications mirrors the available literature. A systematic review suggests that the rate of good or excellent outcomes with open and arthroscopic LHB tenodesis is high, with no identifiable difference between the two techniques [1]. We provide further evidence that both are safe with low complication rates. However, cadaveric comparisons have shown differences in the biomechanical properties of arthroscopic supra-pectoral and open sub-pectoral LHB tenodesis, including a tendency of interference screw constructs to overtension the biceps (by 2.15 cm) and significantly decrease ultimate load to failure [23]. Also, the charges (hospital and facility fees) have increased more rapidly over time for arthroscopic than for open LHB tenodesis, likely because of differences in the cost of implants, the variability in operating room time, and the inflation of hospital and surgical center fees [22]. Our use of a population database did not allow us to evaluate such biomechanical or cost-related phenomena, and thus, these may be areas of future clinical research to identify differences between the two techniques.
In conclusion, the annual rate of open and arthroscopic LHB tenodesis is increasing significantly over time, with open techniques more common when performed in isolation and arthroscopic techniques more common when performed as concomitant procedures. Complications post-operatively are exceedingly rare; while the rate of wound dehiscence is significantly higher after open techniques, the absolute difference is small. No significant differences were seen in the rates of other post-surgical complications.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)
(PDF 1225 kb)
Appendix
Compliance with Ethical Standards
Conflict of Interest
Timothy S. Leroux, MD; Eric J. Cotter, MD; Bryce Basques, MD; Justin Griffin, MD; and Rachel M. Frank, MD, declare that they have no conflicts of interest. Anthony A. Romeo, MD, reports board or committee membership at American Orthopaedic Society for Sports Medicine and American Shoulder and Elbow Surgeons; editorial or governing board membership at Orthopedics, Orthopedics Today, SAGE, and Wolters Kluwer Health; personal fees and governing board membership from SLACK Incorporated; personal fees from Arthrex, Inc., and Saunders/Mosby-Elsevier; and research support from DJO Surgical, Ossur, and Smith & Nephew, outside the submitted work. Bryan M. Saltzman, MD, reports personal fees from Nova Science Publishers and honoraria from Postgraduate Institute for Medicine, outside the submitted work. Nikhil N. Verma, MD, reports board or committee membership from American Orthopaedic Society for Sports Medicine, American Shoulder and Elbow Surgeons, and Arthroscopy Association Learning center committee; personal fees and editorial or governing board membership from Arthroscopy and SLACK Incorporated; editorial or governing board membership from Journal of Knee Surgery; personal fees and research support from Arthrex, Inc., and Smith & Nephew; personal fees from Vindico Medical-Orthopedics Hyperguide, Minivasive, and Orthospace; and research support from Arthrosurface, Athletico, ConMEd Linvatec, Miomed, Mitek, and DJO Surgical, outside the submitted work.
Human/Animal Rights
N/A
Informed Consent
N/A
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level III: Epidemiologic Study
References
- 1.Abraham Vineet Thomas, Tan Bryan H.M., Kumar V. Prem. Systematic Review of Biceps Tenodesis: Arthroscopic Versus Open. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2016;32(2):365–371. doi: 10.1016/j.arthro.2015.07.028. [DOI] [PubMed] [Google Scholar]
- 2.Arce G, Bak K, Bain G, Calvo E, Ejnisman B, Di Giacomo G, et al. Management of disorders of the rotator cuff: Proceedings of the ISAKOS upper extremity committee consensus meeting. Arthroscopy. 2013;29(11):1840–1850. doi: 10.1016/j.arthro.2013.07.265. [DOI] [PubMed] [Google Scholar]
- 3.Beason DP, Shah JP, Duckett JW, Jost PW, Fleisig GS, Cain EL., Jr Torsional fracture of the humerus after subpectoral biceps tenodesis with an interference screw: A biomechanical cadaveric study. Clin Biomech (Bristol, Avon) 2015;30(9):915–920. doi: 10.1016/j.clinbiomech.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 4.Bedard NA, Pugely AJ, Westermann RW, Duchman KR, Glass NA, Callaghan JJ. Opioid use after total knee arthroplasty: Trends and risk factors for prolonged use. J Arthroplasty. 2017;32(8):2390–2394. doi: 10.1016/j.arth.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 5.Chen CH, Hsu KY, Chen WJ, Shih CH. Incidence and severity of biceps long head tendon lesion in patients with complete rotator cuff tears. J Trauma. 2005;58(6):1189–1193. doi: 10.1097/01.TA.0000170052.84544.34. [DOI] [PubMed] [Google Scholar]
- 6.Chiang FL, Hong CK, Chang CH, Lin CL, Jou IM, Su WR. Biomechanical comparison of all-suture anchor fixation and interference screw technique for subpectoral biceps tenodesis. Arthroscopy. 2016;32(7):1247–1252. doi: 10.1016/j.arthro.2016.01.016. [DOI] [PubMed] [Google Scholar]
- 7.Dein EJ, Huri G, Gordon JC, McFarland EG. A humerus fracture in a baseball pitcher after biceps tenodesis. Am J Sports Med. 2014;42(4):877–879. doi: 10.1177/0363546513519218. [DOI] [PubMed] [Google Scholar]
- 8.Erickson BJ, Basques BA, Griffin JW, Taylor SA, O’Brien SJ, Verma NN, et al. The effect of concomitant biceps tenodesis on reoperation rates after rotator cuff repair: A review of a large private-payer database from 2007 to 2014. Arthroscopy. 2017;33(7):1301–1307. doi: 10.1016/j.arthro.2017.01.030. [DOI] [PubMed] [Google Scholar]
- 9.Euler SA, Smith SD, Williams BT, Dornan GJ, Millett PJ, Wijdicks CA. Biomechanical analysis of subpectoral biceps tenodesis: Effect of screw malpositioning on proximal humeral strength. Am J Sports Med. 2015;43(1):69–74. doi: 10.1177/0363546514554563. [DOI] [PubMed] [Google Scholar]
- 10.Friedel R, Markgraf E, Schmidt I, Donicke T. Proximal humerus shaft fracture as a complication after keyhole-plasty. A case report. Unfallchirurgie. 1995;21(4):198–201. doi: 10.1007/BF02588699. [DOI] [PubMed] [Google Scholar]
- 11.Ge H, Zhang Q, Sun Y, Li J, Sun L, Cheng B. Tenotomy or tenodesis for the long head of biceps lesions in shoulders: A systematic review and meta-analysis. PLoS One. 2015;10(3):e0121286. doi: 10.1371/journal.pone.0121286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gyulai M. Humeral fracture after keyhole tenodesis. Magy Traumatol Orthop Helyreallito Seb. 1990;33(3):234–236. [PubMed] [Google Scholar]
- 13.Nho SJ, Reiff SN, Verma NN, Slabaugh MA, Mazzocca AD, Romeo AA. Complications associated with subpectoral biceps tenodesis: Low rates of incidence following surgery. J Shoulder Elbow Surg. 2010;19(5):764–768. doi: 10.1016/j.jse.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 14.Oflazoglu K, Menendez ME, Ring D, O’Brien TM, Archibald JD. Axillary artery injury associated with subpectoral biceps tenodesis: A case report. J Shoulder Elbow Surg. 2016;25(1):e25–28. doi: 10.1016/j.jse.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 15.Provencher MT, LeClere LE, Romeo AA. Subpectoral biceps tenodesis. Sports Med Arthrosc. 2008;6(3):170–176. doi: 10.1097/JSA.0b013e3181824edf. [DOI] [PubMed] [Google Scholar]
- 16.Reiff SN, Nho SJ, Romeo AA. Proximal humerus fracture after keyhole biceps tenodesis. Am J Orthop (Belle Mead NJ) 2010;39(7):E61–63. [PubMed] [Google Scholar]
- 17.Rhee PC, Spinner RJ, Bishop AT, Shin AY. Iatrogenic brachial plexus injuries associated with open subpectoral biceps tenodesis: A report of 4 cases. Am J Sports Med. 2013;41(9):2048–2053. doi: 10.1177/0363546513495646. [DOI] [PubMed] [Google Scholar]
- 18.Rios DM, Martetschlaeger F, Horan MP, Millet PJ. Complications following subpectoral biceps tenodesis with interference screw fixation. J Shoulder Elbow Surg. 2013;22:e26. doi: 10.1016/j.jse.2013.07.007. [DOI] [Google Scholar]
- 19.Sears BW, Spencer EE, Getz CL. Humeral fracture following subpectoral biceps tenodesis in 2 active, healthy patients. J Shoulder Elbow Surg. 2011;20(6):e7–11. doi: 10.1016/j.jse.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 20.Vellios EE, Nazemi AK, Yeranosian MG, Cohen JR, Wang JC, McAllister DR, et al. Demographic trends in arthroscopic and open biceps tenodesis across the United States. J Shoulder Elbow Surg. 2015;24(10):e279–285. doi: 10.1016/j.jse.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 21.Walch G, Edwards TB, Boulahia A, Nove-Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: Clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;4(3):238–246. doi: 10.1016/j.jse.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 22.Werner BC, Brockmeier SF, Gwathmey FW. Trends in long head biceps tenodesis. Am J Sports Med. 2015;43(3):570–578. doi: 10.1177/0363546514560155. [DOI] [PubMed] [Google Scholar]
- 23.Werner BC, Lyons ML, Evans CL, Griffin JW, Hart JM, Miller MD, et al. Arthroscopic suprapectoral and open subpectoral biceps tenodesis: A comparison of restoration of length-tension and mechanical strength between techniques. Arthroscopy. 2015;31(4):620–627. doi: 10.1016/j.arthro.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 24.Werner BC, Pehlivan HC, Hart JM, Carson EW, Diduch DR, Miller MD, et al. Increased incidence of postoperative stiffness after arthroscopic compared with open biceps tenodesis. Arthroscopy. 2014;30(9):1075–1084. doi: 10.1016/j.arthro.2014.03.024. [DOI] [PubMed] [Google Scholar]
- 25.Wu PT, Jou IM, Yang CC, Lin CJ, Yang CY, Su FC, et al. The severity of the long head biceps tendinopathy in patients with chronic rotator cuff tears: Macroscopic versus microscopic results. J Shoulder Elbow Surg. 2014;23(8):1099–1106. doi: 10.1016/j.jse.2013.11.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)
(PDF 1225 kb)