Abstract
Background
Blade plates are frequently used for internal fixation following proximal femoral varus rotational osteotomy to treat hip dysplasia in children with cerebral palsy. Recently, cannulated blade plates with the option for a proximal locking screw have demonstrated ease of insertion and low complication rates. Although there are two commonly used blade plates with a proximal screw option, no comparison of their biomechanical profiles has been undertaken.
Questions/Purposes
Our study sought to compare the structural properties under axial loading, as well as the biomechanical contribution of a proximal screw, of two different 90° cannulated blade plates designed for pediatric proximal femurs. Plate A has a hole distal to the blade designed to attach a plate inserter, through which a 3.5-mm non-locking cortical screw could be placed. Plate B has a threaded hole distal to the blade designed to accept a 3.5-mm locking screw.
Methods
Plate A and plate B were inserted into 33 left pediatric synthetic proximal femurs. Axial loading to failure of plate A with and without a proximal screw was compared to that of plate B with and without a proximal screw. An additional 10 samples using plate B, with and without a proximal locking screw, were tested in tension to quantify the effect of the proximal screw on pullout strength.
Results
Plate B failed at a higher axial load than plate A. The addition of a proximal screw did not affect the axial load to failure for either plate. Pullout testing revealed that blade plates fixed with the proximal screw failed in tension at a significantly higher load (856.3 ± 120.9 N) than those without proximal fixation (68.1 ± 9.3 N, p < 0.001).
Conclusions
Plate B failed at a higher axial load in biomechanical testing, likely related to differences in its design. The addition of a proximal screw did not increase the axial loading properties of the blade plate construct but did increase the pullout strength by a factor of 12. These results may be used to influence implant selection and post-operative rehabilitation following proximal femoral osteotomies in children.
Electronic supplementary material
The online version of this article (10.1007/s11420-019-09675-1) contains supplementary material, which is available to authorized users.
Keywords: biomechanics, blade plate, pediatric orthopedics, proximal femoral osteotomy
Introduction
Several options exist for internal fixation following pediatric proximal femur osteotomy. These include hip screw-side plate devices [7], locking compression plates [9, 10, 13], and blade plates [1, 6, 7]. Fixed-angle blade plates are a common choice for internal fixation following femoral varus rotational osteotomy (VRO) used in treating hip dysplasia in children with cerebral palsy. Given the complex nature of such surgeries, the presence of comorbidities, and the often bilateral nature of these procedures, early post-operative mobilization has been proposed [1, 4] as a method of limiting the disuse atrophy, osteoporosis, and skin/vascular complications associated with recumbency and prolonged immobility [3]. Some authors [13] have advocated for an intra-operative assessment of fixation stability of the implant–bone construct in determining the need for spica casting and dictating post-operative mobilization protocols. A decision to forgo a period of non-weight bearing with immobilization of adjacent joints limits the time for bony healing at the osteotomy site, along with its associated stability; as a result, a greater reliance is placed upon the strength of the blade plate and the stability of its fixation.
Implant-related complications such as varus collapse with loss of fixation or blade pullout, although rare [5, 11], can have serious consequences and often require reoperation. Recently, the introduction of cannulated blade plates with the option for a proximal locking screw have demonstrated ease of insertion and low complication rates in their early use [13]. Other blade plate designs with an option for additional fixation in the proximal segment may provide biomechanical advantages such as increased loads to failure and pullout strengths. Currently, there are at least two commonly used blade plate implants designed with a proximal screw hole; however, to date there remains no comparison of their biomechanical profiles.
The primary aim of this study was to compare the load to failure of these two commercially available blade plate implants when tested under axial compression. Additional aims were to determine whether adding a proximal screw strengthens the bone–implant construct when subjected to axial stresses and to quantify how it affects pullout strength of the implant from the proximal segment of bone. We hypothesized that the load to failure would be equal between the competing blade plates but that the addition of a proximal screw would increase the overall axial strength of the construct, while greatly enhancing the pullout strength of the blade.
Materials and Methods
Our study tested two 90° cannulated blade plates designed for pediatric proximal femurs and produced by two manufacturers: plate A (Smith & Nephew, Memphis, TN, USA) and plate B (OrthoPediatrics, Warsaw, IN, USA). The specifications of each plate are listed in Table 1. Plate A samples were purchased using institutional funds, and plate B samples were donated by OrthoPediatrics for use in the study. Among the differences in the plate design, an important discrepancy exists in the nature of the most proximal hole. Plate A (Fig. 1) has a hole just distal to the blade designed to attach a plate inserter, through which a 3.5-mm non-locking, cortical screw can be placed. Plate B (Fig. 2) has a threaded hole distal to the blade designed to accept a 3.5-mm locking screw. Thirty-three left pediatric synthetic femurs (Sawbones, Vashon Island, WA, USA) with bone mineral density representative of pediatric patients with cerebral palsy [8] (0.5 g/cm2) were utilized for biomechanical testing. The femurs were osteotomized 1 cm below the blade, while the distal segment of the synthetic femur was discarded, in order to isolate the inherent properties of the plate and blade–bone interface independent of the distal fixation or differences in stability imparted by potential differences in the proximal bone–distal bone apposition. In fact, both plates are standard small fragment 3.5-mm plates distally and would be expected to provide very similar if not identical distal fixation. The proximal fixation was the area of interest in this study.
Table 1.
Select specifications of each blade plate
| Plate | Shoulder region thickness (mm) | Width (mm) | Plate length (mm) | Blade length (mm) | Number of holes |
|---|---|---|---|---|---|
| Plate A | 3.05 | 11 | 40 | 35 | 3 distal, 1 proximal |
| Plate B | 3.25 | 11 | 40 | 35 | 3 distal, 1 proximal |
mm millimeters
Fig. 1.

Front and side profile views of plate A.
Fig. 2.

Front and side profile views of plate B.
To perform axial load testing, all plates were inserted into the synthetic femurs using the same standard technique. A guide wire was first inserted in the proximal lateral femur with a starting point 5 mm below the greater trochanteric apophysis and centered in the sagittal plane. The wire was then driven into a central position in the neck and confirmed fluoroscopically. A chisel was then passed over the wire to create the path for the blade. An osteotomy was made 1 cm below the chisel insertion site, with the distal portion of the femur discarded. The chisel was then removed and the blade plate inserted into its path. Four different groups were tested: plate A with (n = 9) and without (n = 9) a proximal cortical screw and plate B with (n = 5) and without (n = 10) a proximal locking screw. Each specimen was placed in a vise which allowed for contact and testing using a servohydraulic load frame (Fig. 3). The vise was angled 5° from vertical to account for physiologic axial loading of the femur. Specimens were ramped to failure at 10 mm/min, where failure was defined as a 10° decrease in femoral neck-shaft angle. Since the horizontal distance between the contact point on the head and lateral femur was set at 54 mm for all specimens, change in femoral neck-shaft angle was calculated to be 9.5 mm of piston motion (tan (10°) = 54 mm/piston motion). Load and actuator displacement were recorded continuously throughout testing.
Fig. 3.
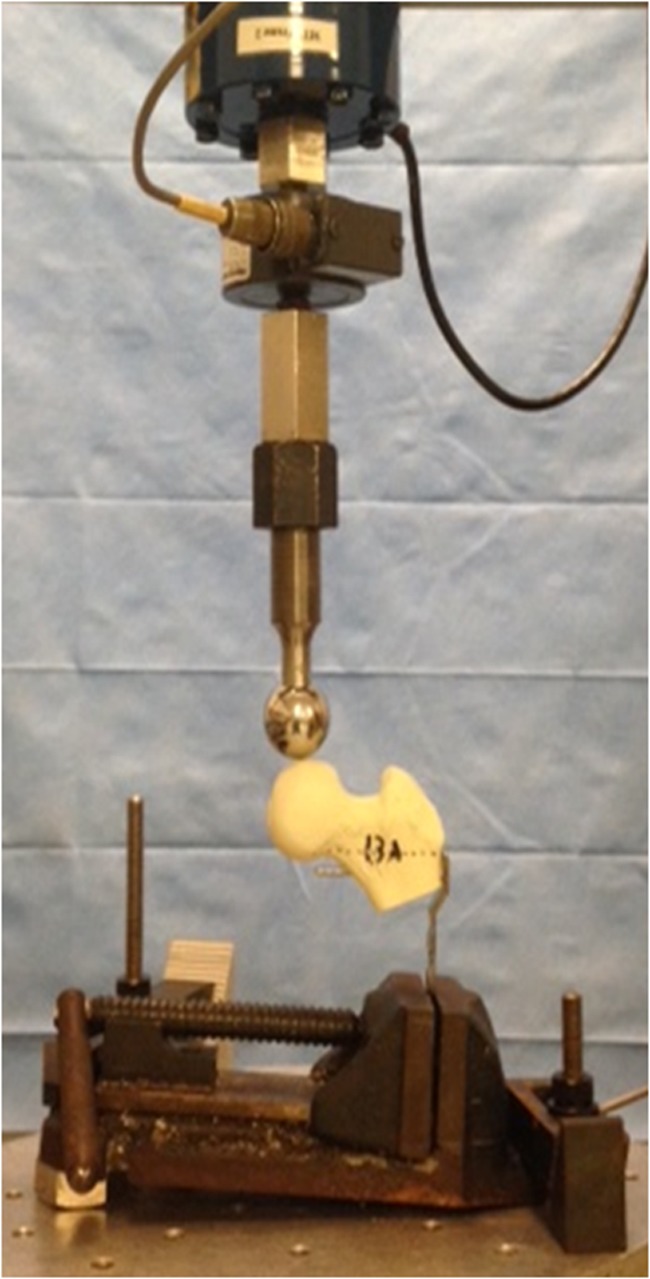
Experimental setup for axial load testing.
To perform pullout testing, an additional 10 left pediatric synthetic femurs were prepared in the same manner described above for axial load testing with the group B plates. Only group B plates were used, as the goal of this phase of the trial was to assess the pullout strength imparted by the addition of a proximal screw and not to compare plates. A proximal 3.5-mm locking screw was inserted in five femurs, and the proximal screw hole was left empty in the remaining five femurs. Pullout testing was performed using a servohydraulic load frame configured to apply a lateral tension force. The blade–proximal femur constructs were statically fixed to the load frame apparatus using 1.25-mm Kirschner wires in a triangular configuration to ensure rotational stability, and the blade was oriented parallel to the axis of the applied load. A steel cable attached to the load frame was tethered around the proximal portion of the blade plate (Fig. 4). The load to failure in tension was directed parallel to the axis of the proximal screw. Specimens were ramped to failure at 10 mm/min, with failure defined as 5 mm of blade pullout.
Fig. 4.
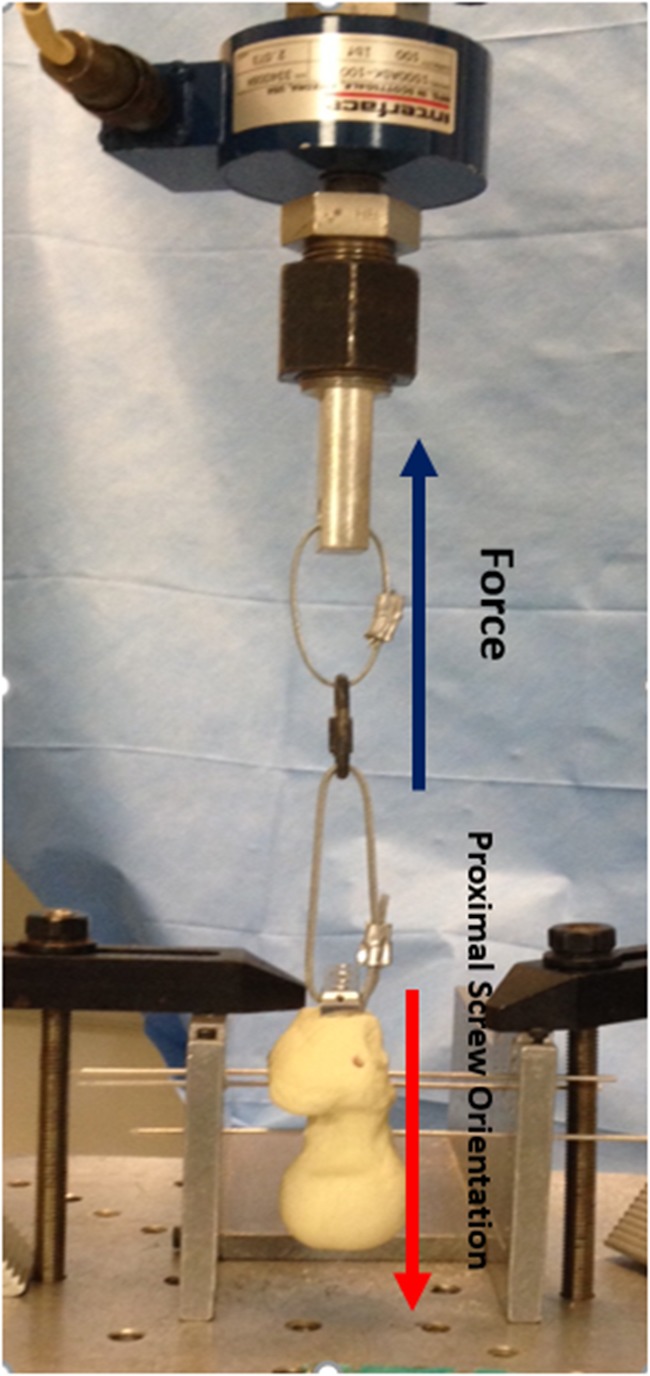
Experimental setup for pullout testing.
Statistics
A one-way analysis of variance was used to compare loads to failure between all groups with a Tukey post hoc test. A student’s t test was used to compare the pullout force of the group B plates with and without proximal locking screws. Normality of the data was assessed using the Shapiro-Wilk test. Alpha was set at 0.05 for all tests. SigmaPlot (version 13.0) software from Systat Software, Inc. (San Jose, CA, USA), was used for the analysis.
Results
With respect to axial load testing, the plate B group without a proximal locking screw had a higher load to failure than the plate A group without a proximal locking screw (p = 0.011). Additionally, the plate B group without a proximal locking screw had a higher load to failure than the plate A group with a proximal locking screw (p = 0.035). In both of the above comparisons, an approximately 20% higher load was achieved. The addition of a proximal screw did not affect the load to failure for either plate B or plate A (Table 2). With respect to the results of pullout testing, the cohort of blade plate B fixed with the proximal locking screw failed at a 12-fold higher load (856.3 ± 120.9 N) compared to those without proximal fixation (68.1 ± 9.3 N, p < 0.001).
Table 2.
Comparison of the two blade plates in load to failure in Newtons (N) in axial load testing
| Axial load testing | |||
|---|---|---|---|
| Comparison | Mean difference in load to axial failure (N) | p value | |
| Plate B without screw | Plate A with screw | 12.6 | 0.035 |
| Plate B without screw | Plate A without screw | 12.5 | 0.011 |
| Plate B without screw | Plate B with screw | 0.2 | 1.00 |
| Plate B with screw | Plate A with screw | 12.5 | 0.078 |
| Plate B with screw | Plate A without screw | 12.4 | 0.040 |
| Plate A without screw | Plate A with screw | 0.1 | 1.00 |
Discussion
Blade plate fixation of proximal femur VROs in pediatric patients with cerebral palsy has been used for decades [1, 12]. These constructs are frequently protected with post-operative spica casting or prolonged periods of immobilization. As a strategy to reduce both complications and hospital stays, early mobilization after surgery has become a priority in this patient population. Despite their potential advantages, immediate range of motion and early weight bearing post-operatively increase the stresses placed upon the blade plate construct, especially before bony healing commences. Given the benefits of early mobilization [12], the aim of this study was to compare the biomechanical properties of two commonly used blade plates, in addition to a novel screw configuration, with an ultimate goal of designing an optimal construct for early rehabilitation. Plate B withstood a 20% greater load prior to failure under axial loading than did plate A. Although not specifically tested, this difference could have implications for osteotomy unions and hardware failures when applied clinically.
The use of synthetic femurs is a limitation of our study. Although the specific synthetic femurs used are designed to mimic the bone density of femurs in children with cerebral palsy, these biomechanical results act merely as an estimation of time-zero mechanics. The in vivo bone–implant interface likely behaves differently. Furthermore, although extrapolating the results to the immediate post-operative period is reasonable, the synthetic femur model cannot account for mechanical properties after post-operative healing occurs at the osteotomy site. Another limitation involves the simple unidimensional mode of testing. In addition to axial loading and pullout forces, these blade plates experience other biomechanical stresses in vivo, including flexion, extension, torsion, and cyclic loading. However, given the most common modes of failure and implications for immediate weight-bearing, axial loading, and pullout strength were chosen to be the focus of this analysis. Lastly, the irregular numbers of plates tested in each group can be viewed as a limitation. Given that an odd number of group B plates were available, but allocation required distribution among four separate groups (two groups for axial-load testing and two groups for pullout testing), we decided to divide the plates into four unequal groups (n = 10, 5, 5, 5). Because significant differences were found for both pullout strength and load to failure, these irregular group sizes confirmed that the study was adequately powered despite these slight differences in group sizes.
The differences in loads to failure can likely be explained by the physical characteristics of the plates and their designs. Plate B was cut from a sheet of stainless steel, whereas plate A was “formed”—essentially, the stainless steel plate was bent to its current configuration through plastic deformation. Despite equal blade lengths (Table 1) and intended patient population, plate A had a thickness throughout its shoulder region that was 0.2 mm less than that of plate B. Since bending rigidity is proportional to plate thickness to the third power [2], this small difference in thickness was likely the most important feature affecting the plates’ resistance to bending.
Contrary to our hypothesis, the addition of a proximal screw, whether locking or cortical, had no effect on the strength of the construct in axial compression. The proximal screw sits parallel and directly adjacent to the blade. Under axial stresses, force is transmitted through the apex of the femoral head through the blade to the shoulder region of the blade plate. The proximal screw is not being loaded under such conditions of axial stress, and as a result the screw does little to the construct to contribute to overall resistance to axial compression. Although not specifically tested, this screw does likely impart some degree of rotational stability to the proximal fragment by providing a second point of fixation. Failure under conditions of cyclic loading and torsional stresses can be tested in future biomechanical studies.
Contrary to its effect on axial loading, however, the addition of a proximal screw increases the pullout strength by 12 times that of the blade in isolation. Given that post-operative mobilization and perineal hygiene often require hip abduction and adduction and their associated coronally based force vectors, stronger fixation in the proximal segment will reduce the risk of blade plate pullout and catastrophic failure.
In conclusion, proximal femoral osteotomies fixed with plate B failed at higher axial loads than those fixed with plate A, independent of the presence of proximal screw fixation. The addition of a proximal screw significantly increased the implant’s pullout strength, further supporting the superiority of plate B’s design. In a clinical context, greater resistance to deformation in the immediate post-operative period following VRO can help support earlier weight bearing and mobilization, but future biomechanical studies are needed to elucidate the effects of different loading patterns and repetitive stresses.
Electronic Supplementary Material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1.19 MB)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)
Funding
No direct funding was provided for this study, although OrthoPediatrics provided some of the blade plates used.
Compliance with Ethical Standards
Conflict of Interest
Joseph J. Ruzbarsky, MD, Ishaan Swarup, MD, Matthew R. Garner, MD, Kathleen Meyers, MS, Folorunsho Edobor-Osula, MD, Roger Widmann, MD, and David M. Scher, MD, report that OrthoPediatrics provided some of the blade plates used in this study. David M. Scher, MD, also reports receiving personal fees as a consultant from OrthoPediatrics, during the conduct of this study.
Human/Animal Rights
N/A
Informed Consent
N/A
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
References
- 1.Beauchesne R, Miller F, Moseley C. Proximal femoral osteotomy using the AO fixed-angle blade plate. J Pediatr Orthop. 1992;12:735–740. doi: 10.1097/01241398-199211000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Browner Bruce D., Jupiter Jesse B., Levine Alan M., Trafton Peter G., Krettek Christian. Skeletal Trauma. 2009. Pharmacologic Management of the Orthopaedic Trauma Patient; pp. 253–285. [Google Scholar]
- 3.DiFazio R, Vessey J, Zurakowski D, Hresko MT, Matheney T. Incidence of skin complications and associated charges in children treated with hip spica casts for femur fractures. J Pediatr Orthop. 2011;31:17–22. doi: 10.1097/BPO.0b013e3182032075. [DOI] [PubMed] [Google Scholar]
- 4.Dreher T, Wolf SI, Heitzmann D, et al. Long-term outcome of femoral derotation osteotomy in children with spastic diplegia. Gait Posture. 2012;36:467–470. doi: 10.1016/j.gaitpost.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 5.Forward DP, Doro CJ, O’Toole RV, et al. A biomechanical comparison of a locking plate, a nail, and a 95 degrees angled blade plate for fixation of subtrochanteric femoral fractures. J Orthop Trauma. 2012;26:334–340. doi: 10.1097/BOT.0b013e3182254ea3. [DOI] [PubMed] [Google Scholar]
- 6.Grant AD, Lehman WB, Strongwater AM, Atar D. Cannulated blade plate for proximal femoral varus osteotomy. Clin Orthop Relat Res. 1990;259:111–113. [PubMed] [Google Scholar]
- 7.Hau R, Dickens DR, Nattrass GR, O'Sullivan M, Torode IP, Graham HK. Which implant for proximal femoral osteotomy in children? A comparison of the AO (ASIF) 90 degree fixed-angle blade plate and the Richards intermediate hip screw. J Pediatr Orthop. 2000;20:336–343. [PubMed] [Google Scholar]
- 8.Henderson RC, Lin PP, Greene WB. Bone-mineral density in children and adolescents who have spastic cerebral palsy. J Bone Joint Surg Am. 1995;77:1671–1681. doi: 10.2106/00004623-199511000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Khouri N, Khalife R, Desailly E, Thevenin-Lemoine C, Damsin JP. Proximal femoral osteotomy in neurologic pediatric hips using the locking compression plate. J Pediatr Orthop. 2010;30:825–831. doi: 10.1097/BPO.0b013e31820156f2. [DOI] [PubMed] [Google Scholar]
- 10.Rutz E, Brunner R. The pediatric LCP hip plate for fixation of proximal femoral osteotomy in cerebral palsy and severe osteoporosis. J Pediatr Orthop. 2010;30:726–731. doi: 10.1097/BPO.0b013e3181efb86b. [DOI] [PubMed] [Google Scholar]
- 11.Ruzbarsky JJ, Beck NA, Baldwin KD, Sankar WN, Flynn JM, Spiegel DA. Risk factors and complications in hip reconstruction for nonambulatory patients with cerebral palsy. J Child Orthop. 2013;7:487–500. doi: 10.1007/s11832-013-0536-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schaefer MK, McCarthy JJ, Josephic K. Effects of early weight bearing on the functional recovery of ambulatory children with cerebral palsy after bilateral proximal femoral osteotomy. J Pediatr Orthop. 2007;27:668–670. doi: 10.1097/BPO.0b013e3181373d63. [DOI] [PubMed] [Google Scholar]
- 13.Zhou L, Camp M, Gahukamble A, Khot A, Graham HK. Cannulated, locking blade plates for proximal femoral osteotomy in children and adolescents. J Child Orthop. 2015;9:121–127. doi: 10.1007/s11832-015-0649-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1.19 MB)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)


