Abstract
Background
Acetabular component position alone has not been predictive of stability after total hip arthroplasty (THA). Combined anteversion of the acetabulum and femur has the potential of being more predictive of stability. Unfortunately, femoral component position is difficult to measure on plain radiographs. Computed tomography (CT) is the gold standard for measuring implant position post-operatively, but CT exposes patients to a substantial amount of radiation.
Questions/Purposes
We sought to determine whether biplanar low-dose radiography can be used to accurately measure both acetabular and femoral implant position after THA.
Methods
Twenty patients underwent standing low-dose biplanar spine-to-ankle radiographs and supine CT scans 6 weeks after THA. Measurements of acetabular inclination, acetabular anteversion, and femoral anteversion were performed by two blinded observers and compared.
Results
The average absolute differences between biplanar radiographs and CT scans were 2° ± 2° for acetabular inclination, 3° ± 2° for acetabular anteversion, and 4° ± 4° for femoral anteversion between EOS measurements and CT measurements. Interobserver agreement was good for acetabular inclination, acetabular anteversion, and femoral anteversion (Cronbach’s α = 0.90) using biplanar low-dose imaging.
Conclusion
Biplanar radiography is a reliable low-radiation alternative for measuring acetabular inclination, acetabular anteversion, femoral version, and thus combined anteversion compared to CT. Femoral anteversion had the most variability but is still clinically relevant.
Electronic supplementary material
The online version of this article (10.1007/s11420-018-09659-7) contains supplementary material, which is available to authorized users.
Keywords: total hip arthroplasty, imaging, implant position, computed tomography, anteversion
Introduction
Implant position plays a major role in mechanical stability and accelerated bearing wear after total hip arthroplasty (THA) [20, 32, 35]. The standard modality for assessing implant position after THA is a two-dimensional (2D) anteroposterior (AP) radiograph, due to low radiation dose and low cost. Acetabular component position (inclination and anteversion) can be measured relative to the coronal reference frame defined by the radiograph itself. Alternatively, a cross table lateral may also be useful when determining acetabular anteversion [24, 27]. However, recent studies have demonstrated that the traditional “safe zone” for acetabular component position on an AP radiograph may not reduce the risk of dislocation [1, 8]. The acetabular position accounts for only half of the hip replacement; femoral implant position is an essential element in determining impingement-free arc of motion [6, 28]. Unfortunately, a shortcoming of conventional radiographs is their inability to measure femoral anteversion.
Femoral anteversion can be measured using three-dimensional (3D) imaging technologies, such as computed tomography (CT), where it is possible to choose a coronal reference frame according to femoral landmarks, such as the posterior condylar axis. But most surgeons do not routinely order CT scans post-operatively to measure implant position due to clinical practicality, cost, and radiation concerns. The ability to measure femoral stem anteversion in THA patients routinely may be beneficial to surgeons as they consider the role of combined anteversion (both acetabular and femoral anteversion) on THA stability [6, 28].
Biplanar radiography has recently started to be used as a means for measuring hip component position [17, 18]. Biplanar radiography can calculate 3D patient information from two simultaneous frontal and lateral radiographs of a standing patient without stitching or vertical distortion and has been shown to be more reliable than conventional 2D radiographs for lower extremity measurements [11]. Previous studies have validated biplanar imaging for 3D reconstruction of lower limbs in adults and children [2, 3, 10, 25, 29, 30]. However, only one study has reported on the accuracy of biplanar radiography for measurement of THA implant position [14]. A major limitation of this study was the use of dry bone models, which do not have the additional tissues that could limit visibility of anatomic landmarks in patients. Therefore, the purpose of this prospective study was to assess the accuracy and reproducibility of measuring hip component position using biplanar radiography compared to the gold standard method of CT in a series of patients who underwent THA.
Materials and Methods
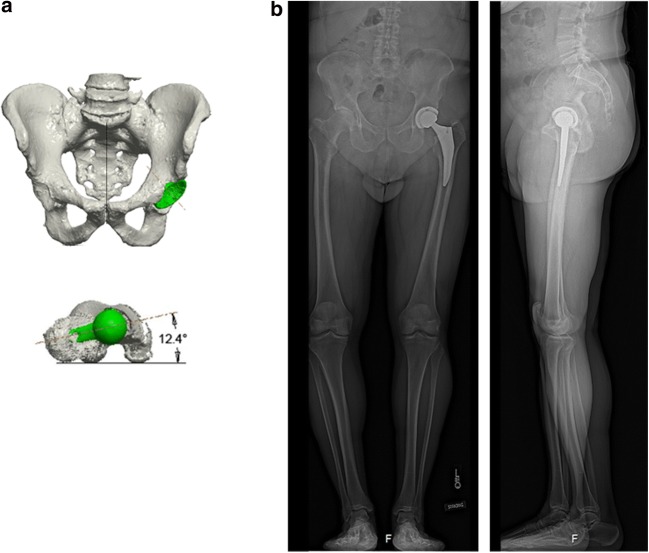
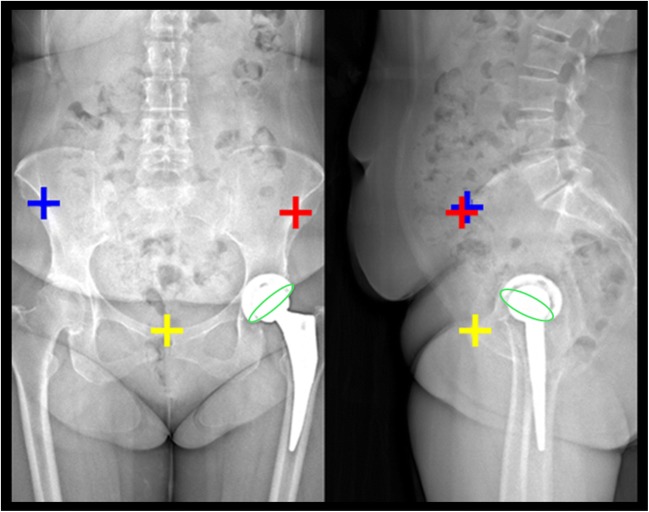
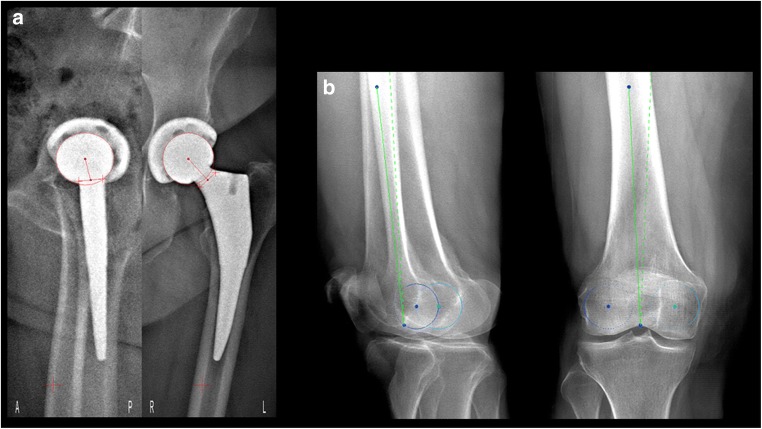
After institutional review board approval, 20 patients undergoing unilateral cementless THA consented to this analysis of post-operative THA alignment. All patients had supine CT scans and standing EOS biplanar radiography taken 6 weeks post-operatively (Fig. 1). CT images of the pelvis and femur were segmented using Mimics software (Materialise, Leuven, Belgium), and component position was measured using Geomagic Studio (Morrisville, NC, USA) and Creo Parametric (PTC Creo, Needham, MA, USA). CT reconstruction methods have been shown to be accurate for determining acetabular cup orientation [4, 15, 21, 31]. Post-operative acetabular angles (acetabular inclination and anteversion) and femoral angles (femoral anteversion) were measured on biplanar radiographs using sterEOS® software (EOS Imaging Acquisition System, EOS Imaging Inc., Paris, France). Anatomic references were used to define acetabular and femoral component position on both biplanar radiographs and CT in order to avoid angular differences that can occur with pelvic tilt or femoral rotation in supine or standing positions (changes in functional implant alignment). The anterior pelvic plane (APP) (defined by the two anterior superior iliac spines and the pubic symphysis) was used as an anatomic reference for acetabular inclination and anteversion (Fig. 2). The most posterior part of the femoral condyles was used as an anatomic reference for femoral anteversion (defined as the angular difference between the axis of the femoral neck and the posterior bi-condylar axis; Fig. 3). Two blinded observers (C.E., T.M.), a musculoskeletal radiologist and an experienced user engineer, measured hip angles using sterEOS software. For the purpose of this study, a senior musculoskeletal radiologist (T.M.) and an expert user engineer (C.E.), trained prior to the start of this study to identify the necessary anatomic landmarks, performed the measurements. The primary outcomes were acetabular inclination, acetabular anteversion, and femoral anteversion measured using biplanar radiography compared to the gold standard CT method in the same patients.
Fig. 1.
a 3D computed tomography (CT) reconstruction of pelvis (coronal view) and femur (transverse view). Implants are shown in green; CT femoral anteversion in this patient was 12.4°. b Simultaneous and orthogonal acquisition of these standing anteroposterior and lateral radiographs allowed for 3D implant position measurements (cup inclination, cup anteversion, and femoral anteversion).
Fig. 2.
Cup position on radiographs was measured using the sterEOS workstation which requires users to manually identify anatomic and implant landmarks including the anterior superior iliac spines (blue and red +) and the ring of the acetabular component (green circles).
Fig. 3.
a Sagittal and anteroposterior views of the femoral stem where the neck axis (in red) is manually identified to measure femoral anteversion. b Sagittal and anteroposterior views of a right knee, where the medial (light blue) and lateral (dark blue) femoral condyles of the knee to measure femoral anteversion.
We calculated the deviations in cup inclination, cup anteversion, and femoral anteversion found using biplanar radiographs from the reference CT values and stated the means and standard deviations of the respective amounts. The differences in these means were tested for statistical significance by the Mann–Whitney Rank Sum Test. To check the accuracy of the biplanar radiographic measurement method, we determined the Pearson correlation between the paired results of two measurements. Correlation coefficients greater than 0.8 were assessed as good and hence as confirming the high reliability of the measurement procedure. Interobserver reliability was calculated using the Cronbach’s α (∝) coefficient of reliability. In each case, the significance level was set at p < 0.05. All statistical tests were performed with SPSS Statistics, Version 25 (IBM, New York, NY, USA).
Results
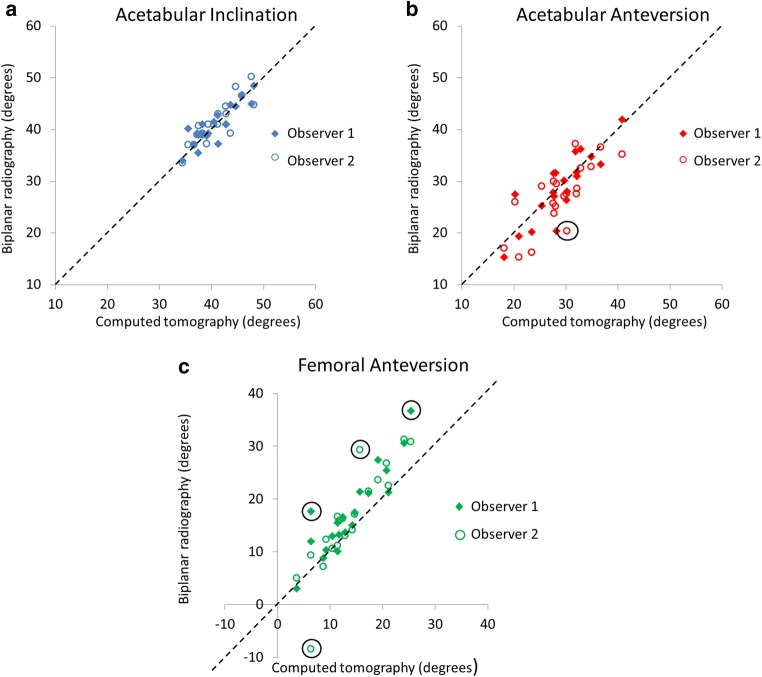
The mean absolute differences between biplanar radiography and CT measurements were 2° ± 2° for acetabular inclination, 3° ± 2° for acetabular anteversion, and 4° ± 4° for femoral anteversion. There was no significant difference in these errors (Table 1). Measurements by two observers showed good correlations to CT values, with Pearson correlation coefficients greater than 0.78 for all hip angles (Table 1). While measurement with biplanar radiograph was only slightly different than reference values, substantial outliers have to be taken into account. In one measurement of acetabular anteversion and four measurements of femoral anteversion, there were greater than 10° difference between biplanar radiography and CT measurements (highlighted by black circles in Fig. 4). The two observers made an error in femoral anteversion measurements in two different patients. This may be explained by users incorrectly identifying anatomic landmarks, such as the anterior superior iliac spines on the pelvis or the posterior femoral condyles on the knees (Fig. 3). Interobserver agreement was good for acetabular inclination (Cronbach’s α = 0.83), acetabular anteversion (Cronbach’s α = 0.89), and femoral components (Cronbach’s α = 0.89) using EOS imaging.
Table 1.
Summary of measurement errors comparing computed tomography (CT) to biplanar radiography for hip angles
| Measure | Observer 1 Cup inclination (°) |
Observer 2 Cup inclination (°) |
Observer 1 Cup anteversion (°) |
Observer 2 Cup anteversion (°) | Observer 1 Femoral anteversion (°) | Observer 2 Femoral anteversion (°) |
|---|---|---|---|---|---|---|
| Mean absolute difference | 0.24 | 0.65 | − 0.13 | − 1.72 | 3.67 | 2.47 |
| Standard deviation | 1.97 | 2.01 | 3.43 | 4.04 | 3.65 | 5.28 |
| Range |
4.6 − 4.0 |
3.7 − 4.4 |
7.3 − 7.8 |
5.8 − 9.8 |
11.3 − 1.3 |
13.6 − 14.8 |
| 95% confidence interval range |
1.10 − 0.63 |
1.53 − 0.23 |
1.37 − 1.63 |
0.05 − 3.49 |
5.27 2.07 |
4.79 0.16 |
| Pearson correlation coefficient* |
r = 0.87, p < 0.01 |
r = 0.89, p < 0.01 |
r = 0.85, p < 0.01 |
r = 0.78, p < 0.01 |
r = 0.91, p < 0.01 |
r = 0.88, p < 0.01 |
*Reliability of biplanar radiography measurements compared to reference CT measurements
Fig. 4.
Scatter plots showing computed tomography (CT) and biplanar radiography measurements for cup inclination (a), cup anteversion (b), and femoral anteversion (c) in the same 20 patients. If CT and biplanar radiography measurements are a perfect match for a patient, a data point falls on the dotted black line. Black circles identify data points where biplanar radiography measurements differed from CT measurements by more than 10°.
Discussion
While CT scans are the gold standard for measuring total hip component positions, they are not obtained during weight-bearing and cannot be used routinely in clinical practice due to cost and high radiation exposure. Therefore, this study sought to consider whether biplanar radiography can accurately and reliably measure acetabular and femoral component position in patients after THA, while exposing patients to lower X-ray emission compared to conventional techniques [22].
Our study has limitations. Landmarks can be difficult to identify and in five patients, we had an error greater than 10° in either acetabular or femoral anteversion. In addition, we were limited by our study size of 20 patients. However, we determined that 20 patients were required to achieve 80% power to detect a minimum proportion of 70% positive tests (versus null kappa of 0.00) between two groups using intraclass correlation coefficients. Also, we did not analyze the reproducibility of the CT measurements that we performed in this study, but it has previously been shown that intraobserver and interobserver agreement in CT measurements is high [24].
Training and practice are necessary to identify anatomic landmarks correctly on biplanar radiographs. Biplanar radiography has been compared to 2D radiographs for lower extremity measurements [11], to CT for assessment of limb length [7], to CT for measuring femoral and tibial rotational alignment [10], to conventional radiographs or saw bones for THA acetabular component position [14, 18], and to conventional radiographs for femoral offset [19]. One study has validated biplanar radiography for measuring acetabular component position using four pelvic phantom models [5], and another study has validated it for measuring femoral stem position using 28 femoral stems implanted in composite femurs [12]. We found an expected error of 2° for acetabular anteversion, 3° for acetabular anteversion, and 4° for femoral anteversion in patients, which should be clinically significant and provide useful information to the surgeon without requiring a CT scan. Conventional radiographs may be useful for measuring varus or valgus stem alignment [16], but cannot be used to measure femoral anteversion. While we found the greatest error associated with measuring femoral anteversion, we feel that biplanar radiography can provide information on whether a patient has high or low femoral stem anteversion, and this additional information may be useful as the patient is followed after THA. For the purpose of this study, a senior musculoskeletal radiologist and an engineer performed the measurements and they were trained prior to the start of this study to identify the necessary anatomic landmarks. In one patient, there was an error of more than 10° in acetabular anteversion and in four patients, there was an error of more than 10° in femoral anteversion (see black circles in Fig. 4). Error can occur from incorrectly identifying landmarks such as the anterior superior iliac spines on the pelvis (Fig. 2) or the posterior femoral condyles on the knees (Fig. 3b). However, if a user is properly trained, biplanar radiography can replace CT imaging for measuring THA component position. Training to gain competence should be done with a musculoskeletal radiologist in order to properly identify bony landmarks and implant landmarks, such as the rim of the metal acetabular component. We recommend evaluating user competence with a set of biplanar images where acetabular and femoral component position is known from additional CT imaging or sawbone models, to gain confidence in a new user’s ability to make measurements on biplanar radiographs.
Biplanar imaging allows measurement not only of anatomic definitions of component position but also functional component position in standing or sitting [9, 23]. Therefore, we may be able to start to consider the impact of pelvic tilt and femoral torsion on functional combined anteversion. Few studies have been able to report on the impact of combined anteversion on hip dislocation, since most centers do not obtain post-operative CT scans of THA patients. One study has shown that a combined anteversion technique reduced the rate of dislocation by six times in cementless THA [26]. Hip surgeons understand well the importance of femoral anteversion, and CT studies have shown that femoral stem anteversion is highly variable [6]. In our study, femoral stem anteversion ranged from 3 to 25° on CT, while other studies have shown the range of cementless femoral component version to be as extreme as 30° retroversion to 45° anteversion [34]. The concept of combined anteversion was introduced by Ranawat et al. in 1991 [28], suggesting the sum of the cup anteversion and stem anteversion should be 45° for women and between 20 and 30° for men. Subsequently, several mathematical models were developed to determine the combination of cup inclination and anteversion, and stem anteversion providing the greater range of motion and lower risk of cup-stem impingement [13, 33, 35]. However, future studies need to consider variability in post-operative femoral anteversion and whether femoral anteversion can be predicted pre-operatively.
Dislocation continues to be one of the leading causes of revision surgery, and variations in both acetabular and femoral implant position may contribute to the risk. We believe that biplanar imaging will be an important tool for considering the impact of implant position on hip stability, since we can now collect data on a large series of patients to identify patient outliers who have extreme retroversion or anteversion of either the acetabular or the femoral component.
Electronic Supplementary Material
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
Compliance with Ethical Standards
Conflict of Interest
Christina I. Esposito, PhD, and Kaitlin M. Carroll, BS, declare that they have no conflicts of interest. David J. Mayman, MD, reports stock or stock options from Imagen Technologies and OrthAlign; personal fees for consultancy, lectures, and grants from Smith & Nephew; and board membership with the Knee Society. Douglas E. Padgett, MD, reports board membership with American Joint Replacement Registry, Journal of Arthroplasty, and Hip Society; personal fees and royalties from DJ Orthopaedics and PixarBio; and stock or stock options from PixarBio. Joseph D. Lipman, MS, reports royalties from Exactech, Inc., LimaCorporate, Mathys Ltd., and Ortho Development Corporation. Seth A. Jerabek, MD, reports personal fees, speakers’ fees, royalties, and grants from Stryker and stock and stock options from Imagen Technologies. Theodore T. Miller, MD, reports educational fees from Amirsys Publishing Co.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was obtained from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level II: Diagnostic Study.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abdel MP, von Roth P, Jennings MT, Hanssen AD, Pagnano MW. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop. 2016;474:386–391. doi: 10.1007/s11999-015-4432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buck FM, Guggenberger R, Koch PP, Pfirrmann CWA. Femoral and tibial torsion measurements with 3D models based on low-dose biplanar radiographs in comparison with standard CT measurements. Am J Roentgenol. 2012;199:W607–612. doi: 10.2214/AJR.11.8295. [DOI] [PubMed] [Google Scholar]
- 3.Chaibi Y, Cresson T, Aubert B, et al. Fast 3D reconstruction of the lower limb using a parametric model and statistical inferences and clinical measurements calculation from biplanar X-rays. Comput Methods Biomech Biomed Engin. 2012;15:457–466. doi: 10.1080/10255842.2010.540758. [DOI] [PubMed] [Google Scholar]
- 4.Craiovan B, Renkawitz T, Weber M, Grifka J, Nolte L, Zheng G. Is the acetabular cup orientation after total hip arthroplasty on a two dimension or three dimension model accurate? Int Orthop. 2014;38:2009–2015. doi: 10.1007/s00264-014-2336-8. [DOI] [PubMed] [Google Scholar]
- 5.Demzik AL, Alvi HM, Delagrammaticas DE, Martell JM, Beal MD, Manning DW. Inter-rater and intra-rater repeatability and reliability of EOS 3-dimensional imaging analysis software. J Arthroplasty. 2016;31:1091–1095. doi: 10.1016/j.arth.2015.11.026. [DOI] [PubMed] [Google Scholar]
- 6.Dorr LD, Malik A, Dastane M, Wan Z. Combined anteversion technique for total hip arthroplasty. Clin Orthop. 2009;467:119–127. doi: 10.1007/s11999-008-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Escott BG, Ravi B, Weathermon AC, et al. EOS low-dose radiography: a reliable and accurate upright assessment of lower-limb lengths. J Bone Joint Surg Am. 2013;95:e1831–1837. doi: 10.2106/JBJS.L.00989. [DOI] [PubMed] [Google Scholar]
- 8.Esposito CI, Gladnick BP, Lee Y-Y, et al. Cup position alone does not predict risk of dislocation after hip arthroplasty. J Arthroplasty. 2014;30(1):109–113. doi: 10.1016/j.arth.2014.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Esposito CI, Carroll KM, Sculco PK, Padgett DE, Jerabek SA, Mayman DJ. Total hip arthroplasty patients with fixed spinopelvic alignment are at higher risk of hip dislocation. J Arthroplasty. 2018;33(5):1449–1454. doi: 10.1016/j.arth.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 10.Folinais D, Thelen P, Delin C, Radier C, Catonne Y, Lazennec JY. Measuring femoral and rotational alignment: EOS system versus computed tomography. Orthop Traumatol Surg Res. 2013;99:509–516. doi: 10.1016/j.otsr.2012.12.023. [DOI] [PubMed] [Google Scholar]
- 11.Guenoun B, Zadegan F, Aim F, Hannouche D, Nizard R. Reliability of a new method for lower-extremity measurements based on stereoradiographic three-dimensional reconstruction. Orthop Traumatol Surg Res. 2012;98:506–513. doi: 10.1016/j.otsr.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 12.Guenoun B, El Hajj F, Biau D, Anract P, Courpied J-P. Reliability of a new method for evaluating femoral stem positioning after total hip arthroplasty based on stereoradiographic 3D reconstruction. J Arthroplasty. 2015;30:141–144. doi: 10.1016/j.arth.2014.07.033. [DOI] [PubMed] [Google Scholar]
- 13.Hisatome T, Doi H. Theoretically optimum position of the prosthesis in total hip arthroplasty to fulfill the severe range of motion criteria due to neck impingement. J Orthop Sci. 2011;16:229–237. doi: 10.1007/s00776-011-0039-1. [DOI] [PubMed] [Google Scholar]
- 14.Journé A, Sadaka J, Bélicourt C, Sautet A. New method for measuring acetabular component positioning with EOS imaging: feasibility study on dry bone. Int Orthop. 2012;36:2205–2209. doi: 10.1007/s00264-012-1650-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim Y-H, Cho K-H, Park Y-G. Is the acetabular cup orientation after total hip arthroplasty on a two-dimensional or three-dimensional model accurate? Int Orthop. 2015;39:819–820. doi: 10.1007/s00264-015-2697-7. [DOI] [PubMed] [Google Scholar]
- 16.Kutzner KP, Freitag T, Donner S, Kovacevic MP, Bieger R. Outcome of extensive varus and valgus stem alignment in short-stem THA: clinical and radiological analysis using EBRA-FCA. Arch Orthop Trauma Surg. 2017;137:431–439. doi: 10.1007/s00402-017-2640-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lazennec JY, Brusson A. Rousseau M-A. THA patients in standing and sitting positions: a prospective evaluation using the low-dose “full-body” EOS® imaging system. Semin Arthroplasty. 2012;23:220–225. doi: 10.1053/j.sart.2013.01.005. [DOI] [Google Scholar]
- 18.Lazennec JY, Rousseau MA, Rangel A, et al. Pelvis and total hip arthroplasty acetabular component orientations in sitting and standing positions: measurements reproductibility with EOS imaging system versus conventional radiographies. Orthop Traumatol Surg Res. 2011;97:373–380. doi: 10.1016/j.otsr.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Lazennec JY, Brusson A, Dominique F, Rousseau M-A, Pour AE. Offset and anteversion reconstruction after cemented and uncemented total hip arthroplasty: an evaluation with the low-dose EOS system comparing two- and three-dimensional imaging. In Orthop. 2015;39:1259–1267. doi: 10.1007/s00264-014-2616-3. [DOI] [PubMed] [Google Scholar]
- 20.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. doi: 10.2106/00004623-197860020-00014. [DOI] [PubMed] [Google Scholar]
- 21.Lin F, Lim D, Wixson RL, Milos S, Hendrix RW, Makhsous M. Validation of a computer navigation system and a CT method for determination of the orientation of implanted acetabular cup in total hip arthroplasty: a cadaver study. Clin Biomech Bristol Avon. 2008;23:1004–1011. doi: 10.1016/j.clinbiomech.2008.04.015. [DOI] [PubMed] [Google Scholar]
- 22.Mahboub-Ahari A, Hajebrahimi S, Yusefi M, Velayati A. EOS imaging versus current radiography: a health technology assessment study. Med J Islam Repub Iran. 2016;30:331. [PMC free article] [PubMed] [Google Scholar]
- 23.Maratt JD, Esposito CI, McLawhorn AS, Jerabek SA, Padgett DE, Mayman DJ. Pelvic tilt in patients undergoing total hip arthroplasty: when does it matter? J Arthroplasty. 2015;30(3):387–391. doi: 10.1016/j.arth.2014.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McArthur B, Cross M, Geatrakas C, Mayman D, Ghelman B. Measuring acetabular component version after THA: CT or plain radiograph? Clin Orthop. 2012;470:2810–2818. doi: 10.1007/s11999-012-2292-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morvan G, Guerini H, Carré G, Vuillemin V. Femoral torsion: impact of femur position on CT and stereoradiography measurements. Am J Roentgenol. 2017;209:W93–W99. doi: 10.2214/AJR.16.16638. [DOI] [PubMed] [Google Scholar]
- 26.Nakashima Y, Hirata M, Akiyama M, et al. Combined anteversion technique reduced the dislocation in cementless total hip arthroplasty. Int Orthop. 2014;38:27–32. doi: 10.1007/s00264-013-2091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nunley RM, Keeney JA, Zhu J, Clohisy JC, Barrack RL. The reliability and variation of acetabular component anteversion measurements from cross-table lateral radiographs. J Arthroplasty. 2011;26:84–87. doi: 10.1016/j.arth.2011.03.039. [DOI] [PubMed] [Google Scholar]
- 28.Ranawat CS, Maynard MJ. Modern techniques of cemented total hip arthroplasty. Tech Orthop. 1991;6:17–25. doi: 10.1097/00013611-199109000-00004. [DOI] [Google Scholar]
- 29.Rosskopf AB, Pfirrmann CWA, Buck FM. Assessment of two-dimensional (2D) and three-dimensional (3D) lower limb measurements in adults: comparison of micro-dose and low-dose biplanar radiographs. Eur Radiol. 2016;26:3054–3062. doi: 10.1007/s00330-015-4166-5. [DOI] [PubMed] [Google Scholar]
- 30.Rosskopf AB, Buck FM, Pfirrmann CWA, Ramseier LE. Femoral and tibial torsion measurements in children and adolescents: comparison of MRI and 3D models based on low-dose biplanar radiographs. Skeletal Radiol. 2017;46:469–476. doi: 10.1007/s00256-017-2569-x. [DOI] [PubMed] [Google Scholar]
- 31.Tsai T-Y, Dimitriou D, Li G, Kwon Y-M. Does total hip arthroplasty restore native hip anatomy? three-dimensional reconstruction analysis. Int Orthop. 2014;38:1577–1583. doi: 10.1007/s00264-014-2401-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wan Z, Boutary M, Dorr LD. The influence of acetabular component position on wear in total hip arthroplasty. J Arthroplasty. 2008;23:51–56. doi: 10.1016/j.arth.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 33.Widmer K-H, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–821. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 34.Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty. 2006;21:696–701. doi: 10.1016/j.arth.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 35.Yoshimine F. The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech. 2006;39:1315–1323. doi: 10.1016/j.jbiomech.2005.03.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)